Abstract
Background
The addition of a chemotherapy drug or drugs to an established regimen is one method used to increase the dose and intensity of treatment for metastatic breast cancer.
Objectives
To assess the effects of adding one or more chemotherapy drugs to an established regimen in women with metastatic breast cancer.
Search methods
We searched the Cochrane Breast Cancer Group's Specialised Register (to August 2009) using the codes for "advanced breast cancer" and "chemotherapy". This review is an update of the original Cochrane Review (Issue 3, 2006).
Selection criteria
Randomised trials with a first line regimen of at least two chemotherapy drugs compared to the same regimen plus the addition of one or more chemotherapy drugs in women with metastatic breast cancer.
Data collection and analysis
Two authors extracted data independently from published trials. We derived hazard ratios (HR) from time‐to‐event outcomes where possible, and used a fixed‐effect model for meta‐analysis. We analysed response rates as dichotomous variables and extracted toxicity data where available.
Main results
We identified 17 trials reporting on 22 treatment comparisons (2674 patients randomised). Fifteen trials (20 treatment comparisons) reported results for tumour response and 11 trials (14 treatment comparisons) published time‐to‐event data for overall survival. There were 1532 deaths in 2116 women randomised to trials of the addition of a drug to the regimen and control (the regimen alone). There was no detectable difference in overall survival between these patients, with an overall HR of 0.96 (95% confidence interval (CI) 0.87 to 1.07, P = 0.47) and no significant heterogeneity. We found no difference in time to progression between these regimens, with an overall HR of 0.93 (95% CI 0.81 to 1.07, P = 0.31) and no significant heterogeneity. Addition of a drug to the regimen was favourably associated with overall tumour response rates (odds ratio 1.21, 95% CI 1.01 to 1.44, P = 0.04) although we observed significant heterogeneity for this outcome across the trials. Where measured, acute toxicities such as alopecia, nausea and vomiting and leucopenia were more common with the addition of a drug.
Authors' conclusions
The addition of one or more drugs to the regimen shows a statistically significant advantage for tumour response in women with metastatic breast cancer but the results suggest no difference in survival time or time to progression. The positive effect on tumour response was also associated with increased toxicity.
Plain language summary
Addition of drugs to a chemotherapy regimen for metastatic breast cancer
Advanced breast cancer is treatable but not curable. Women with advanced breast cancer have an average survival of about 2 years, although some women may live for many years beyond this. Therefore, it is important to investigate different chemotherapy treatment options. Chemotherapy can improve survival for women with metastatic breast cancer, but it can also cause toxic side effects. Of interest is whether there is any benefit by adding additional chemotherapy drugs, particularly given the potential harm caused by more dose‐intensive treatment. This review investigated the value of adding one or more chemotherapy drugs to a chemotherapy regimen. We found that the addition of chemotherapy drug/s to a regimen caused greater shrinkage of the tumour seen with imaging but increased toxicity. There is insufficient evidence to determine if there is an impact on time to disease progression and overall survival.
Background
Description of the condition
Breast cancer is the most common type of cancer in women, and the most common cause of cancer‐related death in women. In 2002, there were 1.15 million new cases of breast cancer reported worldwide. In the same year, there were approximately 410,712 deaths as a result of breast cancer; with an age‐standardised death rate (ASR) of 13.2 (per 100,000). ASRs of 25 or greater were recorded in 2002 by Barbados (25.53), Belgium (27.7), Botswana (25), Cyprus (29.6), Denmark (27.8), Ireland (25.5), Malta (29.6), Philippines (27.1) and the Netherlands (27.5) (Ferlay 2004).
While treatable, metastatic breast cancer is rarely curable at present. Some women with metastatic breast cancer live for many years; however, the median survival ranges from 18 to 24 months (Stockler 2000). Chemotherapy is considered by many to be the appropriate first treatment option for women with multiple sites of recurrence, or in women whose cancer is hormone refractory, or expected to be hormone resistant (Esteva 2001). See Table 1 for a list of chemotherapeutic agents and their site of action.
1. Chemotherapeutic Agents (adapted from Table 1.1 in The Chemotherapy Source Book).
| Type of Agent | Action | Includes |
| Agents that damage the DNA template | by alkylation: nitrogen mustards | cyclophosphamide, melphalan, ifosfamide, chlorambucil |
| by alkylation: nitrosureas | carmustine (BCNU), lomustine (CCNU) | |
| by alkylation: other agents | thitepa, mitomycin C | |
| by platinum coordination cross‐linking | cisplatin, carboplatin | |
| by antibiotics | doxorubicin, daunorubicin, mitoxantrone, idarubicin, epirubicin, amsacrine | |
| by podophyllotoxins | etoposide, teniposide | |
| by intercalation | dactinomycin | |
| by uncertain mechanisms | bleomycin | |
| Spindle poisons | vinca alkaloids | vincristine, vinblastine, vendesine, vinorelbine |
| taxanes | taxol, taxotere | |
| Antimetabolites | thymidylate synthase | 5‐fluorouracil |
| dihydrofolate reductase | methotrexate |
Description of the intervention
Most chemotherapeutic agents used in the treatment of cancer show a steep dose‐response curve. This has led to the conclusion that increasing the intensity of treatment will result in an increase in the rate and duration of response, and hence to improvements in survival (Hryniuk 1987). One widely accepted theory is that combining chemotherapy agents will produce regimens that are more active, thereby improving tumour response and overall survival.
How the intervention might work
The concurrent addition of a drug to a chemotherapy regimen is one method used to increase the dose and intensity of treatment. In the management of metastatic disease, it is important to understand if combination therapy offers a survival advantage over other treatment options (Hamilton 2005). Of interest is whether there is any benefit to increasing the dose intensity of a regimen, particularly given the potential harm caused by more dose‐intensive treatment. If palliation is the primary goal of treatment, and anticipated survival is limited, then toxicity and quality of life become important factors when deciding on a treatment regimen.
Why it is important to do this review
This review expands further on the potential benefit, or lack thereof, of the addition of a drug to a regimen containing two or more drugs in women with metastatic breast cancer. Single agent versus combination chemotherapy for metastatic breast cancer (Carrick 2005) is one such review in this series and this review of the addition of a drug to a regimen further complements these results. Compared with single‐chemotherapy agents, combination regimens show a statistically significant advantage for tumour response and time to progression in women with metastatic breast cancer, a modest improvement in overall survival and significantly worse toxicities (Carrick 2005). This updated review examines the potential benefit, or lack thereof, of the addition of a drug to a regimen, by comparing regimens that contain at least two chemotherapy drugs, in comparison to that same regimen with the concurrent addition of one or more chemotherapy drugs in women with metastatic breast cancer. We considered all chemotherapy agents regardless of their mechanism of action including antimetabolites, spindle poisons and agents that damage the DNA template.
There is a clear need to summarise the current research and to determine if the addition of one or more drugs to the regimen provides a survival benefit to aid decision making when choice of chemotherapy regimen is being considered for a woman with metastatic breast cancer.
Objectives
To assess the value of adding a drug (or drugs) to the regimen of at least two chemotherapy drugs in the management of women with metastatic breast cancer. Throughout this review, this addition of a drug arm is defined as 'Regimen A + drugn' and the regimen alone defined as 'Regimen A'.
Methods
Criteria for considering studies for this review
Types of studies
Properly randomised controlled clinical trials (see 'Methodological quality of included studies').
Types of participants
-
Women diagnosed with advanced breast cancer in accordance with the following criteria:
advanced breast cancer was defined as metastatic disease;
women with loco‐regional disease only were excluded*.
Women randomised to receive chemotherapy for advanced disease as first line treatment (i.e. no previous chemotherapy given except as adjuvant therapy).
We applied no age restrictions.
*We included trials which randomised both women with metastatic disease and women with loco‐regionally recurrent disease but only if women with isolated loco‐regional recurrence comprised less than 20% of the total group, or the trials stratified by stage so that metastatic disease data could be extracted.
Types of interventions
Intervention group:
(Regimen A + drug) A chemotherapy regimen of at least two cytotoxic drugs (Regimen A) plus the addition of one or more cytotoxic drugs (drug).
Comparator:
(Regimen A) Any chemotherapy regimen containing at least 2 cytotoxic drugs.
Following publication of the protocol, but prior to assessing trial eligibility, we decided to exclude sequential or alternating regimens which were defined as adding a drug to a regimen with a delay of more than five weeks (see table Characteristics of excluded studies: Aisner 1995Cocconi 1999; Costanza 1999Creagan 1984).
We included studies using endocrine therapy if both treatment groups received it.
Trials could specify or not specify recommended treatment upon disease progression/initial treatment failure.
Types of outcome measures
1. Overall survival. 2. Quality of life measures (trial specific instruments). 3. Progression‐free survival (time to disease progression, death or both). 4. Tumour response (World Health Organization [WHO], Response Evaluation Criteria In Solid Tumours [RECIST] or individual protocol criteria). 5. Toxicity (WHO criteria or individual protocol based definition). 6. Time to treatment failure (treatment stopped due to progressive disease, toxicity or death).
Primary outcomes
1. Overall survival.
Secondary outcomes
1. Quality of life measures. 2. Progression‐free survival. 3. Tumour response. 4. Toxicity. 5. Time to treatment failure.
Search methods for identification of studies
See: Breast Cancer Group methods used in reviews.
There will be no language restrictions on included studies and we will arrange to translate any potentially eligible studies if required.
Electronic searches
We will search the following databases:
(a) The Cochrane Breast Cancer Group's (CBCG's) Specialised Register and identify studies and code references as outlined in the CBCG's module (www.mrw.interscience.wiley.com/cochrane/clabout/articles/BREASTCA/frame.html). Trials coded with the key words 'advanced' and 'chemotherapy ' will be extracted and considered for inclusion in the review.
(b) EMBASE (via Embase.com) (2002 ‐ August 2009).
(c) Pubmed (January 1966 ‐ August 2009).
(d) The WHO International Clinical Trials Registry Platform (ICTRP) search portal (http://apps.who.int/trialsearch/Default.aspx) for all prospectively registered and ongoing trials (see Appendix 1 for details).
(e) Health on the Net Northern Ireland (HONNI) (January 1966 ‐ August 2009) which is an Internet based search engine for worldwide journal articles provided by Queen's University Belfast.
We obtained a copy of the full article for each reference reporting a potentially eligible trial.
Searching other resources
(a) Bibliography Searching
We will try to identify further studies from reference lists of identified relevant trials, reviews and other related literature reviews (such as those by Fossati et al (Fossati 1998), and Stockler et al (Stockler 2000)). A copy of the full article for each reference reporting a potentially eligible trial will be obtained, where possible. Where this is not possible, attempts will be made to contact authors to provide additional information.
(b) Handsearching of Journals
We will search for abstracts published in scientific meetings relevant to metastatic breast cancer such as Proceedings of the American Assoication for Cancer Research and Symposium for Breast Cancer Research.
Data collection and analysis
We performed the analysis in accordance with the guidelines published in the Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 (Higgins 2008).
Selection of studies
At least two individuals applied the selection criteria (including the quality of randomisation) to each reference identified by the search strategy, masked to the study results. A third reviewer resolved any discrepancies regarding eligibility or quality. The types of studies selected were randomised controlled clinical trials. At least two groups needed to be included in the trial, one group needed a chemotherapy regimen of at least two cytotoxic drugs (Regimen A), the other group needed Regimen A with the addition of at least one new cytotoxic drug. Other criteria for selection required at least 80% of the study group to have metastatic breast cancer and the chemotherapy regimens needed to be first line.
Data extraction and management
Data were extracted directly from the trial publications by two individuals and entered into results tables using Review Manager 5.
We extracted the hazard ratio (HR) and associated variances directly from the trial publication/s. If not reported, we obtained these data indirectly using the methods described by Parmar 1998 et al, either using other available summary statistics or from data extracted from published Kaplan‐Meier curves.
The pooled HR from the derived observed (O)‐expected (E) number of events and the variance for each trial using the fixed‐effect model (Yusuf 1985). The pooled HR represents the overall risk of an event on chemotherapy regimens with the addition of a drug versus control regimens (non‐addition of a drug). We used Chi2 tests to test for heterogeneity of trials (see the Cochrane Handbook for Systematic Reviews of Interventions Higgins 2008).
We analysed response rates as dichotomous variables (complete or partial versus stable disease or no response) and derived a pooled relative risk. As trialists generally report response for both randomised and assessable patients, we have done the same in this review.
We extracted toxicity data and added up the total number of WHO grade III or IV events and number at risk across trials. We used these data to calculate a crude odds ratio (OR) (with 95% confidence intervals). Five trials did not utilise the WHO toxicity criteria, defining toxicity only as 'severe'. We decided to assume that trials which used the definition 'severe' assessed toxicity in the same manner as trials with toxicity WHO grade III or IV. We have, therefore, reported these toxicity data for WHO grade III and IV alone, and toxicity defined as 'severe' alone, and then all together as combined results. Following publication of the protocol and prior to data extraction, we decided to extract the total number of toxic events for leukopenia, nausea or vomiting and alopecia (hair loss) (see Table 2).
2. Acute Toxicity Grade III‐IV.
| Site of toxicity | No. of trials | Add events (patients)/n | Control (patients)/n | OR (95% CI) |
| ASSESSABLE PATIENTS | ||||
| Trials with toxicity defined by WHO criteria Grade III and IV | ||||
| Alopecia | 1 | 0/51 | 2/54 | |
| Leucopenia* | 7 | 224/517 | 166/494 | 1.51 (1.17‐1.95) |
| Nausea/Vomiting** | 4 | 53/282 | 23/271 | 2.50 (1.48‐4.18) |
| Trials with criteria not defined. Trial grades the toxicity as 'severe' | ||||
| Alopecia | 3 | 96/118 | 52/117 | 5.45 (3.02‐9.84) |
| Leucopenia* | 0 | 0 | 0 | |
| Nausea/Vomiting** | 4 | 52/286 | 40/280 | 1.33 (0.85‐2.09) |
| If it is assumed that trials which defined toxicity as 'severe' have assessed toxicity the same as trials with toxicity WHO criteria grade III or IV, then these results can be combined (as below) | ||||
| All trials | ||||
| Alopecia | 4 | 96/169 | 54/171 | 2.85 (1.83‐4.44) |
| Leucopenia* | 7 | 224/517 | 166/494 | 1.51 (1.17‐1.95) |
| Nausea/Vomiting** | 8 | 105/568 | 63/551 | 1.76 (1.25‐2.46) |
| * data on grade III or IV neutropenia was included if data on leucopenia not reported | ||||
| **data on vomiting included if nausea and vomiting reported separately |
None of the studies included in this review reported quality of life data.
Assessment of risk of bias in included studies
We assessed risk of bias using the Cochrane Colloboration assessment tool (Table 8.5a, Cochrane Handbook for Systematic Reviews of InterventionsHiggins 2008). The quality of six domains of risk of bias was assessed in each publication by two individuals. The domains were:
sequence generation;
allocation concealment;
blinding of participants, personnel and outcome assessors;
incomplete outcome data;
selective outcome reporting; and
other sources of bias such as comparability between groups.
We graded the quality of each domain as A ‐ clearly adequate, B ‐ possibly adequate, C ‐ clearly inadequate (see table Characteristics of included studies). It was not possible to accurately assess all domains in most studies due to the lack of information in the published articles.
Measures of treatment effect
Treatment effect was measured by overall survival, percentage of patients achieving tumour response (partial or complete), incidence of toxicity and the mean time to treatment failure or tumour progression.
Unit of analysis issues
There were no issues regarding unit of analysis in most studies, however, Creech 1979 was a cross‐over trial (cyclophosphamide, methotrexate, fluorouracil (CMF) patients crossed over to doxorubicin on progression).
Dealing with missing data
We used statistical models to allow for missing data, either using other available summary statistics or by extracting data from published Kaplan‐Meier curves, as described by Parmar 1998. To allow for immature follow‐up, we adjusted the numbers at risk based upon estimated minimum and maximum follow‐up times. If these were not reported in any of the reports available, we estimated minimum follow‐up using the estimated time taken to complete treatment, and maximum follow‐up was estimated using the last event reported in the relevant time‐to‐event curve. We have recorded these follow‐up estimates in the table Characteristics of included studies under "Notes". No attempt was made to contact trial investigators for additional information.
Assessment of heterogeneity
Heterogeneity was assessed formally using the Chi2 test. There was significant heterogeneity for overall response of all trials (P heterogeneity = 0.03, I2 = 42.1%). There was also observed significant heterogeneity in other overall response subgroups, however, no heterogeneity was observed in any time‐to‐event and toxic related death data.
Assessment of reporting biases
Reporting bias was assessed using the Cochrane Colloboration assessment tool (Table 8.5a, Cochrane Handbook for Systematic Reviews of InterventionsHiggins 2008).
Data synthesis
We used a fixed‐effect model for meta‐analysis. Response rates were analysed as dichotomous variables and derived a pooled relative risk.
Subgroup analysis and investigation of heterogeneity
As outlined in the protocol, we extracted all of these outcomes, where available, from all trial publications. We completed pre‐specified subgroup analysis for: (a) first line trials, (b) dose adjustment in addition of a drug arm, and (c) addition of a drug now considered less active (vincristine, dibromodulcitol and ICRF‐159) compared to the addition of drugs considered more active (e.g. doxorubicin, cyclophosphamide and 5‐fluorouracil). We did not carry out planned subgroup analysis by menopausal status, hormone receptor status and stage of disease, due to the lack of data available in the included trials for these subgroups.
We conducted the following post hoc subgroup analyses: addition of an anthracycline; and addition of one, or two or more, drugs to a regimen. We planned these analyses, prior to pooling of results, with one of the authors who is a medical oncologist (NW) who was blinded to results of individual studies and was not involved in eligibility assessment and data extraction. We provided NW with details of the drugs, dosages and schedules compared in each trial to determine a meaningful way to group the studies. We applied Chi2 tests for interaction to these subgroup analyses. No attempt was made to contact trial investigators for additional information.
Sensitivity analysis
All of the trials designated as eligible trials comprised women randomised to receive chemotherapy for metastatic disease as first line treatment. We conducted a sensitivity analysis for trials in which the line of treatment was not entirely clear (see table Characteristics of included studies). The sensitivity analysis demonstrated comparable results to those found in the primary analysis so we decided to include all trials in the primary analysis.
Results
Description of studies
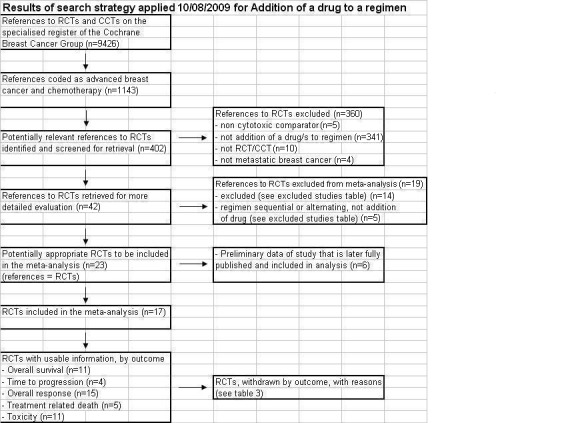
We searched the specialised register of the Cochrane Breast Cancer Group on 16 March 2009, with an updated search on 10 August 2009. Of the 9426 references included in the register, 1143 were coded as references to studies of chemotherapy and advanced breast cancer (Figure 1). Of these, 402 were references that reported the comparison of two different chemotherapy combinations in metastatic breast cancer, of which 360 were not eligible for this review based on information in the abstract. We obtained the complete paper for 42 references; this led to the exclusion of a further 19 references, which we considered ineligible for the review (see table Characteristics of included studies). The remaining 23 references reported the results of 17 randomised trials; six of these references were the preliminary data of a trial that was later fully published and included in this review. The 17 eligible trials reported on 22 treatment comparisons summarised in Table 3. The trials included in the forest plots were labelled by primary author and date of publication.
1.
3. Chemotherapy Details.
| Trial Name | Arm I | Arm II |
| Ahmann 1976a | Arm I: AC = doxorubicin 40 mg/m2 and cyclophosphamide 500 mg/m2 both day 1. Cycles repeated every 5 weeks. Number of cycles not reported. | Arm II: CAF = cyclophosphamide 400 mg/m2 + doxorubicin 40 mg/m2 (both day 1) + 5‐fluorouracil 150 mg/m2 (day 1‐3). Cycles repeated every 5 weeks. Number of cycles not reported. |
| Ahmann 1976b | Arm I: CFP = cyclophosphamide 150 mg/m2 + 5‐fluorouracil 300 mg/m2 both days 1 through 5 + prednisone. Cycles repeated every 5 weeks. Number of cycles not reported. | Arm II: CAF = cyclophosphamide 400 mg/m2 + doxorubicin 40 mg/m2 (both day 1) + 5‐fluorouracil 150 mg/m2 (day 1‐3). Cycles repeated every 5 weeks. Number of cycles not reported. |
| Aisner 1987a | Arm I: CAF = cyclophosphamide 100 mg/m2/day days 1‐14 + doxorubicin 25 mg/m2 days 1 & 8 (after total dose of 450 mg/m2 replaced with methotrexate 40 mg/m2 days 1 & 8)+ 5‐fluorouracil 500 mg/m2 days 1 & 8. 28 day cycle. | Arm II: CAFVP = cyclophosphamide 100 mg/m2/day, days 1‐14 + doxorubicin 25 mg/m2 days 1 & 8 (after total dose 450 mg/m2 replaced with methotrexate 40 mg/m2 days 1 & 8) + 5‐fluorouracil 500 mg/m2 days 1 & 8 + vincristine 10 mg/m2 days 1 & 8 + prednisone 40 mg/m2/day days 1‐14. 28 day cycle. |
| Aisner 1987b | Arm I: CAF+MER = cyclophosphamide 100 mg/m2/day days 1‐14 + doxorubicin 25 mg/m2 days 1 & 8 (after total dose of 450 mg/m2 replaced with methotrexate 40 mg/m2 days 1 & 8) + 5‐fluorouracil 500 mg/m2 days 1 & 8 + MER 200 micrograms days 1 & 8. 28 day cycle. | Arm II: CAFVP+MER = cyclophosphamide 100 mg/m2/day, days 1‐14 + doxorubicin 25 mg/m2 days 1 & 8 (after total dose 450 mg/m2 replaced with methotrexate 40 mg/m2 days 1 & 8) + 5‐fluorouracil 500 mg/m2 days 1 & 8 + vincristine 10 mg/m2 days 1 & 8 + prednisone + MER 200 micrograms days 1 & 8. 28 day cycle. |
| Cavalli 1983a | Arm I: CLB+MFP = chlorambucil 5 mg/m2/day days 1‐14 + methotrexate 10 mg/m2/wk days 1 & 8 + 5‐fluorouracil 500 mg/m2/wk days 1 & 8 + prednisone. 4 weeks cycles for 6 months. | Arm II: CLB+AMFP = chlorambucil 5 mg/m2/day days 1‐14 + methotrexate 40 mg/m2/wk days 1 & 8 + 5‐fluorouracil 600 mg/m2/wk days 1 & 8 + prednisone 30 mg/m2/day days 1‐14 (then decreasing) + doxorubicin 60 mg/m2 day 28. 8 week cycles for 6 months. |
| Cavalli 1983b | Arm I: CLB+MFP = chlorambucil 5 mg/m2/day days 1‐14 + methotrexate 10 mg/m2/wk days 1 & 8 + 5‐fluorouracil 500 mg/m2/wk days 1 & 8 + prednisone. 4 weeks cycles for 6 months. | Arm II: CLB+MFVP = chlorambucil 5 mg/m2/day days 1‐14 + methotrexate 15 mg/m2/wk days 1‐3 & 8‐10 + 5‐fluorouracil 500 mg/m2/wk days 15 & 22 + vincristine 1.2 mg/m2/wk days 15 & 22 + prednisone. 4 week continuous cycle for 6 months. |
| Chlebowski 1983 | Arm I: A‐CCNU = doxorubicin (25‐40 mg/m2) every 3 weeks + CCNU (65‐90 mg/m2) every 6 weeks. | Arm II: A‐CCNU‐V = doxorubicin (25‐40 mg/m2) every 3 weeks + CCNU (65‐90 mg/m2) every 6 weeks + vincristine (1.4 mg/m2 with individual dosage not exceeding 2 mg) every 3 weeks. |
| Creech 1979 | Arm I: CMF = cyclophosphamide 50 mg/m2 days 1‐14 + methotrexate 20 mg/m2 days 1 & 8 + 5‐fluorouracil 300 mg/m2 days 1 & 8. 28 day cycle. | Arm II: CAMF = cyclophosphamide 50 mg/m2 days 1‐14 + doxorubicin 20 mg/m2 days 1 & 8 + methotrexate 20 mg/m2 days 1 & 8 + 5‐fluorouracil 300 mg/m2 days 1 & 8. 28 day cycle. |
| Cummings 1981a | Arm I: AV = doxorubicin 60 mg/m2 + vincristine 1.2 mg/m2; Cycles repeated every 3 weeks until progressive disease | Arm II: AVD = doxorubicin 45 mg/m2 + vincristine 1.2 mg/m2 + dibromodulcitol 140 mg/m2. Cycles repeated every 4 weeks (AVD) until progressive disease. |
| Cummings 1981b | Arm I: AV = doxorubicin 60 mg/m2 + vincristine 1.2 mg/m2; Cycles repeated every 3 weeks until progressive disease | Arm II: AVI = doxorubicin 45 mg/m2 + vincristine 1.2 mg/m2 + ICRF‐159 250 mg/m2. Cycles repeated every 4 weeks (AVI) until progressive disease. |
| Inoue 1984 | Arm I: ACF = doxorubicin 40 mg/m2 day 1 + cyclophosphamide 130 mg/m2 day 1‐5 + ftorafur 500 mg/m2 daily, 21 day cycle. | Arm II: ACFM = doxorubicin 40 mg/m2 day 1 + cyclophosphamide 130 mg/m2 day 1‐5 + ftorafur 500 mg/m2 daily + methotrexate 10‐15 mg/m2 day 1 & 5, 21 day cycle. |
| Kennealey 1978 | Arm I: AC = doxorubicin 40 mg/m2 + cyclophosphamide 1.0 mg/m2 | Arm II: ACMF = doxorubicin 40 mg/m2 + cyclophosphamide 1.0 mg/m2 + methotrexate 30‐40 mg/m2 + 5‐fluorouracil 400‐600 mg/m2. |
| Lokich 1977 | Arm I: MA = melphalan 2.0 mg/m2 + doxorubicin 50 mg/m2. | Arm II: MAC = melphalan 1.0 mg/m2 + doxorubicin 50 mg/m2 + cyclophosphamide 250 mg/m2 ‐ to maximum dose doxorubicin 450 mg/m2, then maintenance CMF every 4 weeks. |
| Marschke 1989 | Arm I: CFP = cyclophosphamide 150 mg/m2 + 5‐fluorouracil 300 mg/m2 + prednisone. | Arm II: CMFP = cyclophosphamide 100 mg/m2 + methotrexate 40 mg/m2 (< 65 yrs; 30 mg/m2 if ≥ 65 yrs) + 5‐fluorouracil 600 mg/m2 (< 65 yrs; 400 mg/m2 if ≥ 65 yrs) + prednisone. |
| Nemoto 1982a | Arm I: CFP = cyclophosphamide 150 mg/m2 days 1‐5 + 5‐fluorouracil 300 mg/m2 days 1‐5 + prednisone. Number of cycles not specified. | Arm II: CFP‐CA = Alternating regimens: cyclophosphamide 150 mg/m2 days 1‐5 + 5‐flurouracil 300 mg/m2 days 1‐5 + prednisone. 5 week cycle then cyclophosphamide 500 mg/m2 + doxorubicin 40 mg/m2 every nine weeks. Maximum cumulative dose of Adriamycin 500 mg/m2. |
| Nemoto 1982b | Arm I: AC = doxorubicin 40 mg/m2 day 1 + cyclophosphamide 500 mg/m2 day 1. | Arm II: CAF = cyclophosphamide 400 mg/m2 day 1 + 5‐fluorouracil 200 mg/m2 days 1‐3 + doxorubicin 40 mg/m2 day 1. |
| Pannuti 1984 | Arm I: CMF = cyclophosphamide 100 mg/m2 days 1‐14 + methotrexate 40 mg/m2 day 1 & 8 + 5‐fluorouracil 600 mg/m2 day 1 & 8. 28 day cycle. | Arm II: R14 = cyclophosphamide 2 mg/kg + vincristine 0.01 mg/kg + vinblastine 0.1 mg/kg all on day 1 and then on day 2, 5‐fluorouracil 5 mg/kg + methotrexate 0.7 mg/kg + doxorubicin 0.5 mg/kg. Cycle every 21 days. |
| Rosner 1989 | Arm I: CFP = cyclophosphamide 150 mg/m2 + 5‐fluorouracil 300mg/m2 + prednisone every 5 weeks. | Arm II: CFPMV = 5‐fluorouracil 500 mg + methotrexate 25 mg + vincristine 1 mg (all weekly) + cyclophosphamide 50 mg + prednisone. |
| Segaloff 1985 | Arm I: CMFP = cyclophosphamide 100 mg/day + methotrexate 25 mg/week + 5‐fluorouracil 500 mg/week + prednisone. | Arm II: CMFVP = cyclophosphamide 100 mg/day + methotrexate 25 mg/week + 5‐fluorouracil 500 mg/week + vincristine 1 mg/week + prednisone. |
| Stein 1992 | Arm I: 2M = mitozantrone 6.5 mg/m2, methotrexate 30 mg/m2 every 3 weeks. | Arm II: 3M = mitozantrone 6.5 mg/m2, methotrexate 30 mg/m2 every 3 weeks & mitomycin C 6.5 mg/m2 every 6 weeks. |
| Tranum 1982 | Arm I: AC = doxorubicin 40 mg/m2 + cyclophosphamide 200 mg/m2 (p.o) on day 3, 4, 5, 6 every 3 weeks for 3 courses, then ever 4 weeks. Number of cycles not reported | Arm II: FAC = doxorubicin 50 mg/m2 + cyclophosphamide 500 mg/m2 + 5‐fluorouracil 500 mg/m2 every 4 weeks |
| Vogel 1984 | Arm I: CAF = cyclophosphamide 500 mg/m2 + doxorubicin 50 mg/m2 + 5‐fluorouracil 500 mg/m2. 3 week cycle | Arm II: CAF+CAMELEON = CAF (as arm I) alternating cycle with CAMELEON at 3 weekly intervals. CAMELEON: vincristine 1.4 mg/m2 + methotrexate 30 mg/m2 (three additional doses of per os methotrexate given at 6 hourly intervals) + cytosine arabinoside 300 mg/m2 + leucovorin 17.5 mg/m2. |
Where a trial included more than one comparison we labelled these alphabetically (a, b, c). Five of the included studies (Ahmann 1976a; Ahmann 1976b; Aisner 1987a; Aisner 1987b; Cavalli 1983a; Cavalli 1983b; Cummings 1981a; Cummings 1981b; Nemoto 1982a; Nemoto 1982b) published two or more comparisons that were included in this review (3‐arm trials). In 3‐arm trials (e.g. drugs CMFD versus CMF versus CMFV), comparisons of interest were arm 1 versus arm 2 for addition of drug D and arm 2 versus arm 3 for addition of drug V. To avoid double counting of patients in arm 2, the number of included patients in that arm was halved and the proportion with the outcome of interest was assumed to be the same in each half as that observed in the whole group. The exception to this method was for the Ahmann 1976a; Ahmann 1976b paper. The number of included patients in the arm to be halved was an odd number (N = 23), in this case the number of patients was rounded up (Ahmann 1976a, N = 12; Ahmann 1976b, N = 12 Forest plots 3.1 to 3.6).
Risk of bias in included studies
The 'Risk of bias' tables for each study are given in the table Characteristics of included studies. Figure 2 shows a summary of methodological quality as judged by the authors.
2.

Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
Allocation
Sequence generation was clearly reported in two trials (Aisner 1987a; Aisner 1987b; Marschke 1989), unclear in 14 trials (Ahmann 1976a; Ahmann 1976b; Cavalli 1983aCavalli 1983bChlebowski 1983Creech 1979; Cummings 1981a; Cummings 1981b; Inoue 1984; Lokich 1977; Nemoto 1982aNemoto 1982bPannuti 1984Rosner 1989Segaloff 1985Stein 1992Tranum 1982Vogel 1984 and inadequately generated in one trial (Kennealey 1978).
In this review, we graded one trial as having clearly adequate allocation concealment (grade A; Aisner 1987a; Aisner 1987b). We graded 15 trials as having possibly adequate allocation concealment and having good comparability of baseline characteristics and adequate reporting of outcomes (grade B; Ahmann 1976a; Ahmann 1976bCavalli 1983aCavalli 1983bChlebowski 1983Creech 1979Cummings 1981aCummings 1981bInoue 1984Lokich 1977Marschke 1989Nemoto 1982a; Nemoto 1982b; Pannuti 1984; Rosner 1989; Segaloff 1985; Stein 1992; Tranum 1982; Vogel 1984). One trial (Kennealey 1978) reported on randomised patients and non‐randomised patient data. The data for both were pooled and it was not possible to distinguish between randomised and non‐randomised patients for inclusion in this review (Table 4).
4. Included RCTs withdrawn, by outcome, with reasons.
| Trial ID | Outcome | Reason not included |
| Ahman 1976 | Toxicity | Does not report toxicity in sufficient detail to enable the data to be used in the review |
| Aisner 1987 | Time‐to‐event data (survival and time to treatment failure) | Time‐to‐event data not extracted from published curves for inclusion in the review as unable to do so accurately to replicate reported study findings |
| Cavalli 1983 | Toxicity | Does not report toxicity in sufficient detail to enable the data to be used in the review |
| Cummings 1981 | Toxicity | Does not report toxicity in sufficient detail to enable the data to be used in the review |
| Inoue 1984 | Toxicity | Does not report toxicity in sufficient detail to enable the data to be used in the review |
| Kennealey 1978 | All outcomes | This paper included 42 randomised patients plus 15 non‐randomised patients from a pilot study. The data for both was pooled and it was not possible to distinguish between randomised and non‐randomised |
| Pannuti 1984 | Toxicity | Does not report toxicity in sufficient detail to enable the data to be used in the review |
| Rosner 1989 | Toxicity | Does not report toxicity in sufficient detail to enable the data to be used in the review |
| Segaloff 1985 | Response, Toxicity | Does not report response and toxicity in sufficient detail to enable the data to be used in the review |
Blinding
For all trials, it was unclear as to whether there was blinding of study participants or outcome assessors.
Incomplete outcome data
Five trials displayed adequate completeness of all outcome data (Ahmann 1976a; Ahmann 1976bAisner 1987aAisner 1987bKennealey 1978Marschke 1989; Vogel 1984), however, in two trials it was unclear for all outcome data (Cummings 1981aCummings 1981bSegaloff 1985). In the remaining trials the majority of outcomes had adequate completeness although there was at least one outcome in which it was unclear (Figure 3). One trial was inadequate for completeness of one outcome (Nemoto 1982aNemoto 1982b): there was conflicting information in the paper clearly stating that all 126 patients had been included in analysis whereas the survival graph displayed 120 patients.
3.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Selective reporting
In three trials (Ahmann 1976a; Ahmann 1976bAisner 1987aAisner 1987bNemoto 1982aNemoto 1982b) there was uncertainty regarding selective outcome reporting whereas the other 14 trials showed no evidence. Some trials had other sources of bias such as group variations in menopausal status (Chlebowski 1983Cummings 1981b) and severity of metastatic disease (Inoue 1984Lokich 1977).
Other potential sources of bias
All of the trials designated as eligible trials comprised women randomised to receive chemotherapy for metastatic disease as first line treatment. We conducted a sensitivity analysis for trials in which the line of treatment was not entirely clear (see table Characteristics of included studies). The sensitivity analysis demonstrated comparable results to those found in the primary analysis so we decided to include all trials in the primary analysis.
Effects of interventions
NOTE: ratios of treatment effects for time‐to‐event outcomes are reported so that hazard ratios (HRs) less than 1.0 favour the addition of one or more drugs to the regimen and values greater than 1.0 favour the control group (that is, the regimen alone). We have reported ratios of treatment effects for response so that odds ratio (OR) greater than 1.00 favour addition of one or more drugs to the regimen.
We have detailed results for the pooled data from all trials (with extractable data) first, followed by the four subgroup analyses. When interpreting the plots for all trials, readers may want to refer to the analyses plots 1.1, 2.1, 3.1 and 4.1, and plots 1.2 to 1.6, 2.2 to 2.6 and so on for the subgroup analyses.
Addition of one or more drugs to a regimen ‐ all trials The 17 trials (22 treatment comparisons) included in this review randomised 2674 women. Time‐to‐event data were extractable for overall survival from 11 trials (14 treatment comparisons, 79% of all patients randomised) and progression‐free survival from four trials (six treatment comparisons, 34% of all patients randomised). Readers should interpret the results of the meta‐analysis with this information in mind. Tumour response rates based on assessable patients were available for 15 trials (20 treatment comparisons, 82% of all patients randomised). Overall survival ‐ all trials There were 1532 deaths in 2116* randomised women, we found no detectable difference in overall survival between the addition of one or more drugs to the regimen and control (the regimen alone). The overall HR was 0.96 (95% CI 0.87 to 1.07, P = 0.47) and we found no statistically significant heterogeneity (P heterogeneity = 0.89, I2 = 0%) (Forest plot 1.1). *There is conflicting information in Nemoto 1982, it is clearly stated that all 126 patients have been included in survival analysis, however, the graph displays N = 120. For the purposes of this review, N = 120 has been used for survival statistics from Nemoto 1982 Time to progression ‐ all trials We found no difference in time to progression between these regimens, with an overall HR of 0.93 (95% CI 0.81 to 1.07, P = 0.31) and no statistically significant heterogeneity (P heterogeneity = 0.83, I2 = 0% ) (Forest plot 2.1).
Overall tumour response ‐ all trials Addition of one or more drugs to the regimen was favourably associated with overall tumour response rates in comparison to the control (OR 1.21, 95% CI 1.01 to 1.44, P = 0.04) although we observed statistically significant heterogeneity for this outcome across the trials (P heterogeneity = 0.04, I2 = 40%) (Forest plot 3.1).
Toxicity ‐ all trials Treatment‐related deaths were reported in three per cent of participants across the four trials (five treatment comparisons reporting on this outcome) (Forest plot 4.1). Of the 27 treatment‐related deaths reported, eight occurred in the addition of a drug arm and eight occurred in the control arm, (OR 1.03, 95% CI 0.39 to 2.69, P = 0.96). It was not possible to identify the treatment arm for an additional 11 toxicity‐related deaths.
Toxicity data were not reported consistently across the included trials. Of the 17 eligible trials, 10 provided extractable data on grade III or IV toxicity. Of these (Table 2), seven trials reported on leucopenia (1011 patients), four on hair loss (340 patients) and eight on nausea and vomiting (1119 patients). Overall, addition of a drug to a regimen appeared to be associated with increased likelihood of leucopenia (white blood cell count less than 2000 x 109/litre) (OR 1.51, 95% CI 1.17 to 1.95), severe nausea and vomiting (OR 1.76, 95% CI 1.25 to 2.46) and hair loss (OR 2.85, 95% CI 1.83 to 4.44) in assessable patients.
Quality of life data were not reported in any of the included studies in this review.
We completed funnel plots for all treatment comparisons. These plots did not demonstrate any obvious asymmetry, suggesting it is unlikely that publication bias is an issue in this review.
Sensitivity analysis: First line trials Thirteen trials (17 treatment comparisons) were clearly first line treatment for metastatic breast cancer, with seven of these reporting on time‐to‐event outcomes. We excluded four trials (Chlebowski 1983; Cummings 1981a; Cummings 1981b; Segaloff 1985; Vogel 1984) from this sensitivity analysis because it was not entirely clear that these were trials of first line treatment (reported in the table Characteristics of included studies). However, because of this uncertainty, it was not clear that these trials were definitely second line either; therefore, we have not excluded them from the overall analysis. Overall survival ‐ first line trials First line trials documented 840 deaths in 1229 randomised women. A statistically significant difference in survival was not evident between addition of one or more drugs to the regimen and control, with an overall HR of 0.95 (95% CI 0.82 to 1.09, P = 0.46) and no statistically significant heterogeneity (P heterogeneity = 0.69, I2 = 0%) (Forest plot 1.2).
Time to progression ‐ first line trials We found no detectable difference in time to progression between these regimens (three comparisons, 465 patients), with an overall HR of 0.90 (95% CI 0.74 to 1.09, P = 0.29) and no statistically significant heterogeneity (P heterogeneity = 0.76, I2 = 0%) (Forest plot 2.2). Overall tumour response ‐ first line trials Addition of one or more drugs to the regimen had a significantly positive effect on overall tumour response (OR 1.38, 95% CI 1.14 to 1.68, P = 0.001) and no statistically significant heterogeneity was observed for this outcome across the trials (P heterogeneity = 0.21, I2 = 22%) (Forest plot 3.2).
Toxicity ‐ first line trials There were three trials (four treatment comparisons) that reported treatment‐related deaths. Of the 14 treatment‐related deaths reported, seven occurred in the addition of a drug arm and seven occurred in the control arm, (OR 0.99, 95% CI 0.35 to 2.75, P = 0.98) (Forest plot 4.2).
The sensitivity analysis revealed that the results are consistent, both for all trials and for the sensitivity analysis which looks at first line trials only. Therefore, the analyses by subgroup is based on all included trials (17 trials; 22 treatment comparisons; 2674 randomised women).
Addition of a 'less active' versus 'more active' drug We conducted this pre‐specified subgroup analysis to investigate the treatment effect with the addition of a drug/s now considered less active (vincristine, dibromodulcitol and ICRF‐159) compared to the addition of drug/s considered more active (e.g. doxorubicin, cyclophosphamide and 5‐fluorouracil). The addition of less active drug/s was investigated in five trials (seven treatment comparisons, 1086 patients), four of which reported survival outcomes. The addition of more active drug/s was considered in 12 trials (14 treatment comparisons, 1524 patients).
Overall survival ‐ 'less active' versus 'more active' There were 653 deaths observed in 837 women randomised to trials where the additional drug to a regimen was a less active drug and time‐to‐event outcomes were reported. There was no detectable difference in overall survival between addition of a less active drug regimen and control, with a HR of 0.94 (95% CI 0.81 to 1.10, P = 0.47) and no statistically significant heterogeneity (P heterogeneity = 0.55, I2 = 0%) (Forest plot 1.3).
Data from the eight trials (nine treatment comparisons) where the additional drug was more active, and where time‐to‐event outcomes were reported, revealed no detectable difference in overall survival (HR 0.98, 95% CI 0.85 to 1.12, P = 0.75) and no significant heterogeneity (P heterogeneity = 0.85, I2 = 0%) (Forest plot 1.3).
A test for interaction between the two groups for overall survival revealed no significant interaction (P = 0.73).
Overall tumour response ‐ 'less active' versus 'more active' Addition of a less active drug to the regimen did not have a significant effect on overall tumour response in comparison to control (OR 1.03, 95% CI 0.74 to 1.43, P = 0.86), with no statistically significant heterogeneity (P heterogeneity = 0.11, I2 = 44%) (Forest plot 3.3).
In comparison, the addition of a more active agent provided a significantly positive effect on overall tumour response (OR 1.34, 95% CI 1.09 to 1.65, P = 0.006). Heterogeneity was statistically significant for this outcome across the trials (P heterogeneity = 0.05, I2 = 43%) (Forest plot 3.3).
A test for interaction between the two groups for overall response revealed no significant interaction (P = 0.21).
Due to the small number of trials that reported time to progression and toxicity data in this subgroup, we did not complete this analysis.
Dose adjustment present in the addition of a drug arm versus no dose adjustment This pre‐specified subgroup analysis investigated Regimen A versus Regimen A (same dose) plus additional cytotoxic drug/s, and also Regimen A versus Regimen A (lesser dose) plus addition cytotoxic drug/s. Dose adjustment in the addition of a drug arm occurred in nine trials (12 treatment comparisons, 1483 patients), seven of which (nine treatment comparisons) reported survival outcomes.
Overall survival ‐ dose adjustment versus no dose adjustment There were 982 deaths observed in 1401 randomised women in trials with adjustment of dose in the addition of a drug arm. No detectable difference in survival was observed in these patients, with an overall HR of 0.94 (95% CI 0.83 to 1.07, P = 0.36) and no statistically significant heterogeneity (P heterogeneity = 0.86, I2 = 0%) (Forest plot 1.4).
There were 550 deaths in 715 women randomised in trials which did not adjust the dose of the agents in the addition of a drug arm. Similarly, no detectable difference in survival was observed in these patients in comparison to control (HR 1.00, 95% CI 0.84 to 1.18, P = 1.00) with no statistically significant heterogeneity (P heterogeneity = 0.56, I2 = 0%) (Forest plot 1.4).
A test for interaction between the two groups for overall survival revealed no significant interaction (P = 0.58). Overall tumour response ‐ dose adjustment versus no dose adjustment When the dose of a regimen was adjusted with the addition of a cytotoxic drug/s, a conventionally significant effect on overall tumour response was demonstrated (OR 1.27, 95% CI 1.01 to 1.58, P = 0.04), with no significant heterogeneity observed (P heterogeneity = 0.13, I2 = 33%) (Forest plot 3.4).
In comparison, when no dose adjustment was present, no detectable effect on overall tumour response was observed (OR 1.10, 95% CI 0.81 to 1.50, P = 0.54), however, significant heterogeneity was observed for this outcome across the trials (P heterogeneity = 0.05, I2 = 50%) (Forest plot 3.4).
A test for interaction between the two groups for overall response revealed no significant interaction (P = 0.46).
Toxicity and time to progression analysis was not appropriate due to the small number of trials that reported these outcomes in this subgroup.
Addition of an anthracycline versus addition of a non‐anthracycline We conducted post hoc subgroup analyses to investigate the treatment effect with the addition of an anthracycline. The addition of an anthracycline was investigated in five trials (352 patients), three of which reported survival outcomes.
Overall survival ‐ addition of an anthracycline There were 144 deaths observed in 193 women randomised to 3 of the 5 trials where the addition of a drug/s included an anthracycline and time‐to‐event outcomes were reported. There was no detectable difference in overall survival between anthracycline‐containing regimens and control (HR 0.87, 95% CI 0.61 to 1.24, P = 0.44) and no statistically significant heterogeneity (P heterogeneity = 0.63, I2 = 0%) (Forest plot 1.5).
Data from the 10 trials (11 treatment comparisons) where the drug added was a non‐anthracycline and where time‐to‐event data was reported, revealed no detectable difference in overall survival (HR 0.97, 95% CI 0.87 to 1.08, P = 0.60) and no statistically significant heterogeneity (P heterogeneity = 0.82, I2 = 0%) (Forest plot 1.5).
A test for interaction between the two groups for overall survival revealed no significant interaction (P = 0.55).
Overall tumour response ‐ addition of an anthracycline Addition of an anthracycline drug to a regimen had a significantly positive effect on overall tumour response in comparison to control (OR 1.87, 95% CI 1.22 to 2.86, P = 0.004). There was no statistically significant heterogeneity (P heterogeneity = 0.15, I2 = 41.0% (Forest plot 3.5).
In comparison, the addition of a non‐anthracycline did not have a statistically significant effect on overall tumour response (OR 1.13, 95% CI 0.94 to 1.37, P = 0.20) with no significant heterogeneity observed for this outcome across the trials (P heterogeneity = 0.06, I2 = 39%) (Forest plot 3.5).
A test for interaction for overall tumour response reveals significant interaction (P = 0.04). This suggests that the addition of an anthracycline has a greater effect on tumour response in those trials randomising patients to addition of an anthracycline to the regimen, in comparison to randomising patients to the addition of a non‐anthracycline.
Toxicity and time to progression analysis was not appropriate due to the small number of trials that reported these outcomes in this subgroup.
Addition of one drug versus the addition of two or more drugs We conducted post hoc subgroup analyses to investigate the treatment effect with the addition of one drug in comparison to the addition of two or more drugs. The addition of only one drug was investigated in 13 trials (17 treatment comparisons, 2301 patients), of which eight reported survival outcomes.
Overall survival ‐ addition of one drug versus the addition of two or more drugs There were 1754 women randomised to the addition of one drug to the regimen trials, 1269 deaths were observed in this group with no detectable difference in overall survival observed (HR 0.95, 95% CI 0.85 to 1.06, P = 0.35) and no statistically significant heterogeneity (P heterogeneity = 0.73, I2 = 0%) (Forest plot 1.6).
There were 263 deaths in 362 women randomised to trials of the addition of two or more drugs to the regimen, with an overall HR of 1.05 (95% CI 0.81 to 1.35, P = 0.73) and no statistically significant heterogeneity (P heterogeneity = 0.88, I2 = 0%) (Forest plot 1.6).
A test for interaction between the two groups for overall survival reveals no significant interaction (P = 0.49).
Overall tumour response ‐ addition of one drug versus the addition of two or more drugs The addition of one drug to the regimen in comparison to the regimen alone, had a significant impact on overall tumour response (OR 1.22, 95% CI 1.01 to 1.48, P = 0.04), with no significant heterogeneity observed (P heterogeneity = 0.17, I2 = 25%). (Forest plot 3.6).
In comparison, the addition of two or more drugs to the regimen (in comparison to the regimen alone) did not have a significant effect on tumour response (OR 1.12, 95% CI 0.70 to 1.81, P = 0.64), and statistically significant heterogeneity was observed (P heterogeneity = 0.01, I2 = 73%). (Forest plot 3.6).
A test for interaction between the two groups for overall response reveals no significant interaction (P = 0.69).
Due to the small number of trials that reported time to progression and toxicity in this subgroup, we did not complete this analysis.
Discussion
This review did not find a statistically significant benefit in overall survival or time to progression for the addition of one or more drugs to the regimen over control (that is, the regimen alone) in the first line treatment of metastatic breast cancer.
Despite the lack of evidence of a survival or time to progression benefit, this review demonstrated that addition of one or more drugs to the regimen provided a statistically significant advantage in tumour response compared to control. All eligible trials provided response data for 2101 assessable patients, for an OR of 1.21 (95% CI 1.01 to 1.44, P = 0.04). The favourable effect on response was consistent and statistically significant in regimens where an anthracycline was used as an additional agent (five treatment comparisons; 352 patients) which is consistent with an earlier review of 33 trials (5284 patients) (Lord 2004). This favourable effect on response was also observed in exploratory subgroup analysis with addition of a drug considered 'more active' (such as 5‐fluorouracil and anthracyclines) (14 treatment comparisons; 1518 patients), dose adjustment in the addition of a drug arm (12 treatment comparisons, 1483 patients) and in trials that added just one agent to a regimen (16 comparisons, 1772 patients).
Such a benefit in response rate, however, comes at the cost of toxicity. Where measured, acute toxicities such as alopecia, nausea and vomiting and leucopenia were more common with the addition of a drug.
This review includes 22 clinically diverse regimens, which differ in dose, activity and potency (e.g. the addition of vincristine versus the addition of doxorubicin). Despite this diversity, there is a significant benefit in overall response rates with the addition of drug/s to the regimen. We observed statistically significant heterogeneity for overall response of all trials (P heterogeneity = 0.04, I2 = 40%). We also observed significant heterogeneity in other overall response subgroups; however, no heterogeneity was observed in any time‐to‐event and toxic related death data.
It must be noted that many of the trials included in this review are not recent, and, therefore, new drug groups such as the addition of a taxane to a regimen have not been explored in this review. We found no recent research matching the eligibility study criteria for this review. Such research has been considered, and the addition of a taxane to a single agent regimen was examined in Ghersi 2004 et al.
The subgroup analyses lead to speculation about what type of drug may be beneficial in the addition of a drug regimen. The results of subgroup analysis suggest that adding a drug or drugs to a regimen produces a positive impact on tumour response. This may, in fact, be primarily due to the addition of an anthracycline, the addition of a more active drug and the addition of one drug only.
Addition of one or more drugs to a regimen does not have a positive impact on survival or time to response. If the addition of drugs to the regimen (such as those added) does not appear to benefit overall survival, the same clinical effect may potentially be achieved by administering three drugs all at once (A+B+C), as by administering them over time (A, then over time B, then over time C). The results of this review, however, do not answer this question with confidence. Furthermore, there is a lack of papers with quality of life and toxicity data. The results and limitations of this review demonstrate the necessity for further research in this field. This review will be updated as and when trials using current therapies are completed, at this stage the authors are not aware of such trials being conducted. More research is required in this area to fully understand the benefit, or lack thereof, of the addition of drugs to the regimen in order to understand the overall question of chemotherapy intensity for the treatment of metastatic breast cancer.
Authors' conclusions
Implications for practice.
Addition of one or more drugs to the regimen does not provide a survival benefit compared to control (the regimen alone), nor does addition of one or more drugs to the regimen have a positive impact on time to progression. The addition of a drug/s to the regimen does produce a benefit in overall response in comparison to control (the regimen alone), but this benefit needs to be considered against the increased risk of toxicity.
Implications for research.
We did not examine sequential therapy and alternating therapy in this review. A review of trials which examine the addition of a drug in a sequential or alternating regimen in the treatment of metastatic breast cancer may provide further information as to the benefit of addition of one or more drugs to the regimen.
What's new
| Date | Event | Description |
|---|---|---|
| 6 February 2018 | Review declared as stable | This review question is broad and no longer reflects the clinical management of breast cancer. Today, chemotherapy decisions are based on the molecular subtype of the breast cancer. As the trials in this Review include women diagnosed with unselected metastatic breast cancer, this Review will no longer be updated. |
History
Protocol first published: Issue 4, 2001 Review first published: Issue 3, 2006
| Date | Event | Description |
|---|---|---|
| 11 February 2011 | Amended | Changed the address of the first author. |
| 15 February 2010 | New citation required but conclusions have not changed | No new studies included. New authors joined the author team. |
| 9 September 2009 | Amended | Converted to new review format. |
| 10 August 2009 | New search has been performed | Performed search for new studies on the 10th August 2009. |
Acknowledgements
We would like to thank Nicole Holcroft for her work in the identification of studies through the Cochrane Breast Cancer Group's specialised register. We would also like to thank Sharon Parker for her work editing and revising this review. We also acknowledge the initial contribution made to the original concept for this review by Craig Henderson, Kathleen Pritchard, Martin Tattersall, Martin Stockler, Christine Brunswick, Roldano Fossati, Russell Basser, Franco Nole and Alessandro Liberati. We would also like to thank Stephane Heritier for providing statistical guidance.
Appendices
Appendix 1. WHO ICTRP Search Portal
Host: http://apps.who.it/trialsearch/ 8 July 2010 Advanced search (with Recruitment set at ALL):
Search 1. Condition field: metastatic breast cancer Intervention field: addition of chemotherapy drug to a chemotherapy regimen OR addition of chemotherapy drugs to a chemotherapy regimen
Search 2. Condition field: metastatic breast cancer Intervention field: addition of cytotoxic drug to a chemotherapy regimen OR addition of cytotoxic drugs to a chemotherapy regimen
Search 3. Condition field: metastatic breast cancer Intervention field: chemotherapy
Search 4 Condition field: advance breast cancer Intervention field: addition of chemotherapy drug to a chemotherapy regimen OR addition of chemotherapy drugs to a chemotherapy regimen
Search 5. Condition field: advance breast cancer Intervention field: addition of cytotoxic drug to a chemotherapy regimen OR addition of cytotoxic drugs to a chemotherapy regimen
Search 6. Condition field: advance breast cancer Intervention field: chemotherapy
Data and analyses
Comparison 1. Overall survival.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Overall survival (all trials) | 14 | 2116 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 0.96 [0.87, 1.07] |
| 1.2 Overall survival (sensitivity analysis) | 9 | 1229 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 0.95 [0.82, 1.09] |
| 1.3 Overall survival (addition of 'less active' drug vs addition of 'more active' drug) | 14 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | Subtotals only | |
| 1.3.1 Addition of 'less active' drug | 5 | 837 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 0.94 [0.81, 1.10] |
| 1.3.2 Addition of 'more active' drug | 9 | 1279 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 0.98 [0.85, 1.12] |
| 1.4 Overall survival (adjusted dose in addition of drug arm vs no dose adjustment) | 14 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | Subtotals only | |
| 1.4.1 Adjusted dose in addition of a drug arm | 9 | 1401 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 0.94 [0.83, 1.07] |
| 1.4.2 Dose not adjusted in addition of a drug arm | 5 | 715 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 1.00 [0.84, 1.18] |
| 1.5 Overall survival (addition of anthracycline vs addition of non‐anthracycline) | 14 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | Subtotals only | |
| 1.5.1 Addition of an anthracycline | 3 | 193 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 0.87 [0.61, 1.24] |
| 1.5.2 Addition of a non‐anthracycline | 11 | 1923 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 0.97 [0.87, 1.08] |
| 1.6 Overall survival (addition of 1 agent vs addition of 2 or more agents) | 14 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | Subtotals only | |
| 1.6.1 Addition of 1 agent | 10 | 1754 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 0.95 [0.85, 1.06] |
| 1.6.2 Addition of 2 or more agents | 4 | 362 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 1.05 [0.81, 1.35] |
1.1. Analysis.

Comparison 1: Overall survival, Outcome 1: Overall survival (all trials)
1.2. Analysis.

Comparison 1: Overall survival, Outcome 2: Overall survival (sensitivity analysis)
1.3. Analysis.

Comparison 1: Overall survival, Outcome 3: Overall survival (addition of 'less active' drug vs addition of 'more active' drug)
1.4. Analysis.

Comparison 1: Overall survival, Outcome 4: Overall survival (adjusted dose in addition of drug arm vs no dose adjustment)
1.5. Analysis.

Comparison 1: Overall survival, Outcome 5: Overall survival (addition of anthracycline vs addition of non‐anthracycline)
1.6. Analysis.

Comparison 1: Overall survival, Outcome 6: Overall survival (addition of 1 agent vs addition of 2 or more agents)
Comparison 2. Time to progression.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Time to progression (all trials) | 6 | 890 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 0.93 [0.81, 1.07] |
| 2.2 Time to progression (sensitivity analysis) | 3 | 465 | Hazard Ratio (Exp[(O‐E) / V], Fixed, 95% CI) | 0.90 [0.74, 1.09] |
2.1. Analysis.

Comparison 2: Time to progression, Outcome 1: Time to progression (all trials)
2.2. Analysis.

Comparison 2: Time to progression, Outcome 2: Time to progression (sensitivity analysis)
Comparison 3. Overall response (assessable patients).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Overall response (all trials) | 20 | 2101 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.21 [1.01, 1.44] |
| 3.2 Overall response (sensitivity analysis) | 16 | 1682 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.38 [1.14, 1.68] |
| 3.3 Overall response (addition of 'less active' drug vs addition of 'more active' drug) | 20 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.3.1 Addition of 'less active' drug | 6 | 659 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.74, 1.43] |
| 3.3.2 Addition of 'more active' drug | 14 | 1518 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.34 [1.09, 1.65] |
| 3.4 Overall response (adjusted dose in addition of a drug arm vs no dose adjustment) | 20 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.4.1 Dose adjusted in addition of drug arm | 12 | 1381 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.27 [1.01, 1.58] |
| 3.4.2 Dose not adjusted in addition of drug arm | 8 | 722 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.81, 1.50] |
| 3.5 Overall response (addition of anthracycline vs addition of non‐anthracycline) | 20 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.5.1 Addition of an anthracycline | 5 | 352 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.87 [1.22, 2.86] |
| 3.5.2 Addition of a non‐anthracycline | 15 | 1847 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.94, 1.37] |
| 3.6 Overall response (addition of 1 agent vs addition of 2 or more agents) | 20 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.6.1 Addition of 1 agent | 16 | 1772 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.22 [1.01, 1.48] |
| 3.6.2 Addition of 2 or more agents | 4 | 331 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.70, 1.81] |
3.1. Analysis.

Comparison 3: Overall response (assessable patients), Outcome 1: Overall response (all trials)
3.2. Analysis.

Comparison 3: Overall response (assessable patients), Outcome 2: Overall response (sensitivity analysis)
3.3. Analysis.

Comparison 3: Overall response (assessable patients), Outcome 3: Overall response (addition of 'less active' drug vs addition of 'more active' drug)
3.4. Analysis.

Comparison 3: Overall response (assessable patients), Outcome 4: Overall response (adjusted dose in addition of a drug arm vs no dose adjustment)
3.5. Analysis.

Comparison 3: Overall response (assessable patients), Outcome 5: Overall response (addition of anthracycline vs addition of non‐anthracycline)
3.6. Analysis.

Comparison 3: Overall response (assessable patients), Outcome 6: Overall response (addition of 1 agent vs addition of 2 or more agents)
Comparison 4. Treatment‐related deaths.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 All trials | 5 | 821 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.39, 2.69] |
| 4.2 All trials (sensitivity analysis) | 4 | 664 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.35, 2.75] |
4.1. Analysis.

Comparison 4: Treatment‐related deaths, Outcome 1: All trials
4.2. Analysis.

Comparison 4: Treatment‐related deaths, Outcome 2: All trials (sensitivity analysis)
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ahmann 1976a.
| Study characteristics | ||
| Methods | Accrual dates: not reported Sample size: 68 USA Randomisation method: not reported Baseline comparability: not reported | |
| Participants | Female % first line not reported unclear % metastatic breast cancer (MBC) (72% had visceral dominant disease) Age and ethnicity not stated | |
| Interventions | AC vs CFP vs CAF (+/‐ calusterone)
Arm 1: (AC) doxorubicin + cyclophosphamide
Arm 2: (CFP) cyclophosphamide + 5‐fluorouracil + prednisone
Arm 3: (CAF) cyclophosphamide + doxorubicin + 5‐fluorouracil Ahmann 1976a = AC vs CAF |
|
| Outcomes | Regression (defined as ≥ 50% reduction in tumour mass) Mean response duration Toxicity | |
| Notes | Abstract only available Reports on 68/68 randomised patients Toxicity related death not reported Doses of the same chemotherapy agent are reduced in the addition of a drug arm | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | B ‐ Unclear |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Toxicity | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Time to progression | Low risk | A ‐ Adequate |
| Selective reporting (reporting bias) | Unclear risk | B ‐ Unclear |
| Other bias | Unclear risk | B ‐ Unclear |
Ahmann 1976b.
| Study characteristics | ||
| Methods | As for Ahmann 1976a | |
| Participants | As for Ahmann 1976a | |
| Interventions | Ahmann 1976b = CF (with Prednisone) vs CAF | |
| Outcomes | As for Ahmann 1976a | |
| Notes | As for Ahmann 1976a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | B ‐ Unclear |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Toxicity | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Time to progression | Low risk | A ‐ Adequate |
| Selective reporting (reporting bias) | Unclear risk | B ‐ Unclear |
| Other bias | Unclear risk | B ‐ Unclear |
Aisner 1987a.
| Study characteristics | ||
| Methods | Accrual dates October 1976 to February 1980 Multicentre national trial (USA) Sample size: 432 Randomisation by sealed envelope using a Latin square design balancing across and within institutions. Baseline comparability: No significant imbalance apparent or reported | |
| Participants | Female Over 80% had visceral or osseous metastatic disease 100% first line Median age: 57 (CAF), 55 (CAFVP) | |
| Interventions | CAF vs CMF vs CAFVP vs CAF+MER vs CMF+MER vs CAFVP+MER Arm I: (CAF) cyclophosphamide + doxorubicin + 5‐fluorouracil Arm II: (CAFVP) cyclophosphamide + doxorubicin + fluorouracil + vincristine + prednisone Arm III: (CMF) cyclophosphamide + 5‐fluorouracil + methotrexate Arm IV, V, VI as above each with the addition of MER Aisner 1987a: CAF vs CAFVP |
|
| Outcomes | Overall survival Time to treatment failure Response Toxicity | |
| Notes | 395/432 evaluable. 37 patients were unevaluable: ineligible (20), protocol violations (10), early deaths (4), inadequate records (2), improper randomisation(1) 6 arm trial. Randomisation to chemoimmunotherapy ceased after an interim evaluation showed no benefit & increased toxicity. Analysis was conducted using 395 evaluable patients (260/283 patients randomised to chemotherapy, 135/149 patients randomised to chemoimmunotherapy). Time‐to‐event data not extracted from published curves for inclusion in this review as unable to do so accurately to replicate reported study findings. Follow‐up details not reported. Estimated minimum follow‐up = 2 months. Estimated maximum follow‐up = 36 months. 8 treatment‐related deaths: 5 due to infection in arms CAF+MER, CAFVP+MER, CAF, CAFVP (2); 2 due to haemorrhage in arms CAF+MER, CMF; 1 due to cardiac toxicity in CAF arm. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A ‐ Adequate, Latin square design |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate, closed envelope |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Toxicity | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Time to progression | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Overall survival | Low risk | A ‐ Adequate |
| Selective reporting (reporting bias) | Unclear risk | B ‐ Unclear, time to treatment failure results not included |
| Other bias | Low risk | A ‐ Other sources of bias not identified in methods |
Aisner 1987b.
| Study characteristics | ||
| Methods | As for Aisner 1987a | |
| Participants | As for Aisner 1987a | |
| Interventions | Aisner 1987b: CAF+MER vs CAFVP+MER | |
| Outcomes | As for Aisner 1987a | |
| Notes | As for Aisner 1987a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A ‐ Adequate, Latin square design |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate, closed envelope |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Toxicity | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Time to progression | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Overall survival | Low risk | A ‐ Adequate |
| Selective reporting (reporting bias) | Unclear risk | B ‐ Unclear, time to treatment failure results not included |
| Other bias | Low risk | A ‐Adequate, other sources of bias not identified in methods |
Cavalli 1983a.
| Study characteristics | ||
| Methods | Multicentre national Accrual: September 1975 ‐ December 1980 Sample size: 230 Randomisation method not defined Baseline comparability: no significant difference apparent or reported | |
| Participants | Female 100% MBC 100% first line Median age: 57.2‐57.9 years | |
| Interventions | CLB+AMFP vs CLB+MFP vs CLB+MFVP Arm I: (CLB+AMFP) chlorambucil, methotrexate, 5‐fluorouracil, prednisone, doxorubicin Arm II: (CLB+MFP) chlorambucil, methotrexate, 5‐fluorouracil plus prednisone Arm III: (CLB+MFVP) chlorambucil plus methotrexate plus prednisone plus 5‐fluorouracil plus vincristine Cavalli 1983a = CLB+AMFP vs CLB+MFP |
|
| Outcomes | Survival Time to progression Response (defined as ≥ 50% reduction in tumour size) Toxicity | |
| Notes | 464 patients entered in study and randomised to receive tamoxifen/oophorectomy or tamoxifen/oophorectomy plus concurrent chemotherapy. The 230 patients assigned to the chemotherapy arm were further randomised to 3 different chemotherapy regimens. 216/230 patients evaluable: excluded for major protocol violations (10), poorly evaluable tumour parameters (2) and early death (2). Minimum reported follow‐up= 17 months Maximum reported follow‐up = 80 months Time‐to‐event analyses calculated from entrance in to the study. Time‐to‐event data extracted directly from time‐to‐event curve. Toxicity related deaths were not reported. Doses of the same chemotherapy agent are increased in the addition of a drug arm, however, cycles are less frequent. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | B ‐ Unclear |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Toxicity | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Time to progression | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Overall survival | Low risk | A ‐ Adequate |
| Selective reporting (reporting bias) | Low risk | A ‐ Adequate, all outcomes reported |
| Other bias | Unclear risk | B ‐ Unclear, mean age of pre‐ and post‐menopausal groups not mentioned in each treatment group |
Cavalli 1983b.
| Study characteristics | ||
| Methods | As for Cavalli 1983a | |
| Participants | As for Cavalli 1983a | |
| Interventions | Cavalli 1983b = CLB+MFVP vs CLB+MFP | |
| Outcomes | As for Cavalli 1983a | |
| Notes | As for Cavalli 1983a except doses of the same chemotherapy agent are increased in the addition of a drug arm (cycles remain the same between treatment arms) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | B ‐ Unclear |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Toxicity | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Time to progression | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Overall survival | Low risk | A ‐ Adequate |
| Selective reporting (reporting bias) | Low risk | A ‐ Adequate, outcomes reported |
| Other bias | Unclear risk | B ‐ Unclear, mean age of pre‐ and post‐menopausal groups not mentioned in each treatment group |
Chlebowski 1983.
| Study characteristics | ||
| Methods | Accrual dates: not reported (accepted for publication May 1982) Sample size: 35 Number of centres: unknown (USA) Randomisation method: not reported Baseline comparability: no significant imbalance apparent or reported | |
| Participants | Female 100% MBC Unclear if this is a first line trial for MBC: 'patients admitted to study if they had failed an initial combination chemotherapy program' 'all patients received prior chemotherapy with at least cyclophosphamide and 5‐FU'. However, patients typically received prior chemotherapy of CMF or CMFP which are typically adjuvant regimens. Age range 24‐74 years Median 50 (both groups) | |
| Interventions | A‐CCNU vs A‐CCNU‐V Arm I: (A‐CCNU) Doxorubicin + CCNU (lomustine) Arm II: (A‐CCNU‐V) Doxorubicin + CCNU (lomustine) + vincristine |
|
| Outcomes | Overall survival (not defined) Response (objective response, defined as ≥ 50% reduction in tumour size) Toxicity | |
| Notes | 35/35 evaluable for toxicity and response. Follow‐up details not reported. ‐ estimated minimum 30 months ‐ estimated maximum 30 months Presents survival as life tables not Kaplan‐Meier curves. Time‐to‐event data extracted directly from time‐to‐event curve. Toxicity related deaths not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | B ‐ Unclear |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Toxicity | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Overall survival | Unclear risk | B ‐ Unclear |
| Selective reporting (reporting bias) | Low risk | A ‐ Adequate, outcomes reported |
| Other bias | High risk | C ‐ difference between groups in proportion of pre/post menopausal patients |
Creech 1979.
| Study characteristics | ||
| Methods | Accrual dates: not reported (Accepted for publication March 1978) Sample size: 78 Number of centres: Unknown (USA) Randomisation method not reported Patients were stratified according to poor or good risk Baseline comparability: no significant imbalance apparent or reported | |
| Participants | 100% women with visceral MBC Age range: 34‐79 years CAMF arm; 32‐87 years CMF arm Median age: 56 both arms | |
| Interventions | CMF vs CAMF Arm I: (CMF) cyclophosphamide + methotrexate + 5‐fluorouracil Arm II: (CAMF) as arm I plus doxorubicin |
|
| Outcomes | Response (defined as ≥ 50% reduction in tumour size) Survival (reported by response status) Progression‐free survival (reported by response status) Toxicity | |
| Notes | 78/78 evaluable. ITT analysis. CMF patients crossed over to doxorubicin on progression. ‐ estimated minimum follow‐up = 5 months ‐ estimated maximum follow‐up = 39 months Overall survival and time to progression were reported for subsets of patients by response status and not extracted for this review. No statistically significant difference between CAMF and CMF were reported for time‐to‐event data. Median survival for PR/CR patients was 20 months in CAMF arm vs 19 months in CMF arm. Treatment related deaths were not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | B ‐ Unclear |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Toxicity | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Time to progression | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Overall survival | Unclear risk | B ‐ Unclear |
| Selective reporting (reporting bias) | Low risk | A ‐ Adequate, outcomes reported |
| Other bias | Low risk | A ‐Adequate, other sources of bias not identified in methods |
Cummings 1981a.
| Study characteristics | ||
| Methods | Accrual dates: not reported (before 1981) Sample size: 268 Number of centres: unknown (USA) Randomisation method: 'randomly allocated' but method not described Baseline comparability: no significant imbalance apparent or reported other than AVI group with higher percentage postmenopausal women and diagnosis more than 5 years before entry | |
| Participants | Female Age range: under 70 82% dominant metastatic site visceral or bone 100% had prior chemotherapy but unclear if adjuvant or for MBC | |
| Interventions | AV vs AVD vs AVI
Arm I: (AV) doxorubicin + vincristine
Arm II: (AVD) doxorubicin + vincristine + dibromodulcitol
Arm III: (AVI) doxorubicin + vincristine + ICRF‐159 Cummings 1981a = AV vs AVD |
|
| Outcomes | Overall survival Time to treatment failure (TTF) (date entry to date progression or death from breast cancer within 6 weeks of ceasing therapy) Response (defined as ≥ 50% reduction in tumour size) Toxicity | |
| Notes | 230/268 evaluable: patient withdrew from study or died without objective progression within 8 weeks (26), reason for drop out not reported (12). Follow up details not reported. Based on median TTF: ‐ estimated minimum 3.5 months ‐ estimated maximum 24 months Time‐to‐event data extracted directly from time‐to‐event curve.Toxicity related deaths not reported. Doses of the same chemotherapy agent are reduced in the addition of a drug arm. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | B ‐ Unclear |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Toxicity | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Time to progression | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Overall survival | Unclear risk | B ‐ Unclear |
| Selective reporting (reporting bias) | Low risk | A ‐ Adequate, all outcomes reported |
| Other bias | High risk | C ‐ Higher proportion of premenopausal patients in AV group |
Cummings 1981b.
| Study characteristics | ||
| Methods | As for Cummings 1981a | |
| Participants | As for Cummings 1981a | |
| Interventions | Cummings 1981b = AV vs AVI | |
| Outcomes | As for Cummings 1981a | |
| Notes | As for Cummings 1981a | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | B ‐ Unclear |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Toxicity | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Time to progression | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Overall survival | Unclear risk | B ‐ Unclear |
| Selective reporting (reporting bias) | Low risk | A ‐ Adequate, all outcomes reported |
| Other bias | High risk | C ‐ Higher proportion of premenopausal patients in AV group |
Inoue 1984.
| Study characteristics | ||
| Methods | Accrual dates: 01/03/1979 to not reported (date closed to accrual not reported, study closed 30/04/1983 and date submitted for publication 25/11/1983) Unknown (Japan) Sample size:58 Randomisation method: Envelope system Baseline comparability: no significant imbalance apparent or reported | |
| Participants | Female 100% MBC 100% first line Age range: 31‐69 years Median age Arm I: 55 years, arm II: 49 years Anthracycline naive | |
| Interventions | ACF vs ACFM Arm I: ACF doxorubicin + cyclophosphamide + ftorafur Arm II ACFM: arm I + methotrexate |
|
| Outcomes | Overall survival Response (defined as ≥ 50% reduction in tumour size) Toxicity | |
| Notes | 58/60 evaluable. 2 patients excluded (ACF arm) due to protocol violation. Survival measured from start of chemotherapy. Follow‐up details not reported. Based on accrual and date of submission: ‐ estimated minimum follow‐up 1 month ‐ estimated maximum follow‐up 51 months Time‐to‐event data extracted directly from time‐to‐event curve. Toxicity related deaths not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | B ‐ Unclear |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate, envelope |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Toxicity | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Overall survival | Unclear risk | B ‐ Unclear |
| Selective reporting (reporting bias) | Low risk | A ‐ Adequate, outcomes reported |
| Other bias | High risk | C ‐ 37% ACFM group had ≥3 organs involved compared to 14% in ACF group |
Kennealey 1978.
| Study characteristics | ||
| Methods | Accrual dates: September 1974 to July 1976 Sample size: 42 randomised (+15 on pilot) Number of centres: unknown (USA) Randomisation method: not reported Baseline comparability: more patients in AC group had prior chemotherapy and endocrine therapy, although this is based on all patients not just randomised patients | |
| Participants | Female Age range: median 58 (AC) and 54 (ACMF) 100% MBC 100% not first line | |
| Interventions | AC vs ACMF Arm I: (AC) doxorubicin + cyclophosphamide Arm II: (ACMF) doxorubicin + cyclophosphamide + methotrexate + 5‐fluorouracil | |
| Outcomes | Response Toxicity | |
| Notes | Not possible to distinguish between randomised and non‐randomised patients (on pilot) therefore study outcomes not included in this review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | C ‐ Inadequate, 15 patients not randomised |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Toxicity | Low risk | A ‐ Adequate |
| Selective reporting (reporting bias) | Low risk | A ‐ Adequate, outcomes reported |
| Other bias | High risk | C ‐ 15/48 patients were not randomised, more patients in AC group (21/26) had prior hormonal therapy compared to ACMF (13/22) |
Lokich 1977.
| Study characteristics | ||
| Methods | Accrual dates: April 1975 to March 1976 Sample size: 43 Number of centres: unknown (USA) Randomisation method: not reported Baseline comparability: imbalance reported with more patients in MA group having skin metastases (15 vs 10), longer disease‐free interval (27 (range 0‐72) vs 8 (range 0‐48) months) and duration of metastases | |
| Participants | Female Age range 39‐78 years (median 53 (MA) and 59 (MAC)) 100% MBC 100% first line unclear: 9/43 had received prior chemotherapy but unclear if this was for metastatic disease | |
| Interventions | MA vs MAC Arm I: (MA) melphalan + doxorubicin Arm II: (MAC) melphalan + doxorubicin + cyclophosphamide | |
| Outcomes | Response (defined as ≥ 50% reduction in tumour size) Duration of response Toxicity | |
| Notes | 40/43 evaluable: reason for exclusion, early death at 3 weeks (1), low dosage of drug therapy with death at 6 weeks (1), absence of measurable disease at 7 weeks (1). 1 treatment related death: severe sepsis (MAC arm) Doses of the same chemotherapy agent are reduced in the addition of a drug arm. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | B ‐ Unclear |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Toxicity | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Duration of response | Unclear risk | B ‐ Unclear |
| Selective reporting (reporting bias) | Low risk | A ‐ Adequate, outcomes reported |
| Other bias | High risk | C ‐ Inadequate, MA group had longer disease free interval and more skin metastases compared to MAC group. |
Marschke 1989.
| Study characteristics | ||
| Methods | Accrual dates: June 1982 to December 1987 Sample size: 345 Multicentre: USA and Canada | |
| Participants | Female Age range: 22‐82 years (median 59‐60) 100% MBC 100% first line | |
| Interventions | CFP vs CMFP Arm I: (CFP) cyclophosphamide + 5‐fluorouracil + prednisone Arm II: (CMFP) cyclophosphamide + methotrexate + 5‐fluorouracil + prednisone | |
| Outcomes | Overall survival Time to progression Response (defined as ≥ 50% reduction in tumour size) Duration of response Toxicity | |
| Notes | Follow‐up details not reported. Based on length of chemotherapy: ‐ estimated minimum 5 months ‐ estimated maximum 48 months 345 randomised: 9 ineligible (5 CFP, 4 CMFP). Time to progression defined as date randomised to date of progression. Time‐to‐event data estimated from statistics presented in trial publication. 6 toxic related deaths: severe myelosuppression (3 from each treatment arm) Doses of the same chemotherapy agent are reduced (C) or increased (5‐FU) in the addition of a drug arm. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A ‐ Pocock‐Simon procedure |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Toxicity | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Time to progression | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Overall survival | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Duration of response | Low risk | A ‐ Adequate |
| Selective reporting (reporting bias) | Low risk | A ‐ Adequate |
| Other bias | Low risk | A ‐ Adequate |
Nemoto 1982a.
| Study characteristics | ||
| Methods | Accrual dates: July 1974 to October 1975 Sample size: 126 Multicentre: 2 sites in USA Randomisation method: 'closed envelopes' kept at one of the centres (unclear how randomisation was achieved) Baseline comparability: no imbalance apparent or reported | |
| Participants | Female Age range not reported (> 50 to < 70 years) 100% MBC 100% first‐line | |
| Interventions | AC vs CFP vs CAF vs CFP‐CA
Arm I: (AC) cyclophosphamide + doxorubicin
Arm II: (CFP) cyclophosphamide + 5‐fluorouracil + prednisone
Arm III: (CAF) cyclophosphamide + doxorubicin + 5‐fluorouracil
Arm IV: (CFP‐CA) CFP as above, then cyclophosphamide + doxorubicin Nemoto 1982a = CFP vs CFP‐CA |
|
| Outcomes | Overall survival Time to progression (TTP) Response (defined as ≥ 50% reduction in tumour size) Toxicity | |
| Notes | 117/126 evaluable: reason for exclusion, 9 withdrawn due to early death or withdrawal from study (no reason given). There is conflicting information in the paper, it is clearly stated that all 126 patients have been included in analysis, however, the graph displays N = 120 with the groups as follows CFP 18; CFP‐CA 20; CAF 40; CA 42. The group numbers as detailed which total to 120 (CFP 18; CFP‐CA 20; CAF 40; CA 42) have been used in this review. Follow‐up details not reported. Based on median TTP: ‐ estimated minimum 12 months ‐ estimated maximum 54 months Time‐to‐event data extracted directly from time‐to‐event curve. Reported that no toxic deaths occurred. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | B ‐ Unclear |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate, closed envelope |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Toxicity | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Time to progression | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Overall survival | High risk | C ‐ Inadequate |
| Selective reporting (reporting bias) | Unclear risk | B ‐ Unclear |
| Other bias | Low risk | A ‐ Adequate |
Nemoto 1982b.
| Study characteristics | ||
| Methods | As for Nemoto 1982a | |
| Participants | As for Nemoto 1982a | |
| Interventions | Nemoto 1982b = AC vs CAF | |
| Outcomes | As for Nemoto 1982a | |
| Notes | As for Nemoto 1982a except doses of the same chemotherapy agent are reduced in the addition of a drug arm | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | B ‐ Unclear |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate, closed envelope |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Toxicity | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Time to progression | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Overall survival | High risk | C ‐ Inadequate |
| Selective reporting (reporting bias) | Unclear risk | B ‐ Unclear |
| Other bias | Low risk | A ‐ Adequate |
Pannuti 1984.
| Study characteristics | ||
| Methods | Accrual dates: not reported Sample size: 46 Randomisation method not reported Baseline comparability: no significant imbalance apparent or reported | |
| Participants | Female 100% MBC (87% with metastases of bone or viscera) Unclear if prior chemotherapy received by 17% was for MBC Age range: 36‐74 years Median age: 55 (both arms) | |
| Interventions | CMF vs R14 Arm I: (CMF) cyclophosphamide + methotrexate + 5‐fluorouracil Arm II: (R14) arm I + vincristine + vinblastine + doxorubicin |
|
| Outcomes | Overall survival Response (defined as ≥ 50% reduction in tumour size) Toxicity | |
| Notes | 46/46 included in analysis Follow‐up details not reported: ‐estimated minimum follow‐up 5.5 months ‐estimated maximum follow‐up 45 months (from survival curve) Time‐to‐event data extracted directly from time‐to‐event curve. Treatment related deaths not reported. Doses of the same chemotherapy agent are markedly different between treatment arms. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | B ‐ Unclear |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Toxicity | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Overall survival | Unclear risk | B ‐ Unclear |
| Selective reporting (reporting bias) | Low risk | A ‐ Adequate, outcomes reported |
| Other bias | High risk | C ‐ Inadequate, higher proportion of R14 group premenopausal, small study groups |
Rosner 1989.
| Study characteristics | ||
| Methods | Accrual dates: September 1981 to December 1987 Sample size: 182 Number of centres: unknown (USA) Randomisation method not reported Baseline comparability: no significant imbalance reported | |
| Participants | Female Age range: mean 53 years 100% MBC 100% first line | |
| Interventions | AC vs CFP vs CFPMV
Arm I: (AC) doxorubicin + cyclophosphamide
Arm II: (CFP) cyclophosphamide + 5‐fluorouracil + prednisone
Arm III: (CFPMV) cyclophosphamide + 5‐fluorouracil + prednisone + methotrexate + vincristine Rosner 1989 = CFP vs CFPMV |
|
| Outcomes | Overall survival Response Remission duration Toxicity | |
| Notes | Follow‐up details not reported. Based on median time of remission: ‐ estimated minimum 6 months ‐ estimated maximum 36 months All patients included in time‐to‐event analyses. Time‐to‐event data extracted directly from time‐to‐event curve. Survival from start of chemotherapy Toxicity related deaths not reported Doses of the same chemotherapy agent are reduced (C) or increased (5‐FU) in the addition of a drug arm | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | B ‐ Unclear |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Toxicity | High risk | C ‐ Inadequate |
| Incomplete outcome data (attrition bias) Overall survival | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Duration of response | Unclear risk | B ‐ Unclear |
| Selective reporting (reporting bias) | Low risk | A ‐ Adequate, outcomes reported |
| Other bias | Low risk | A ‐ Adequate |
Segaloff 1985.
| Study characteristics | ||
| Methods | Accrual dates: July 1971 to October 1976 Sample size: 427 Number of centres: 11(USA) Randomisation method: 'randomised from a central statistical office' Baseline comparability: no significant imbalance apparent or reported | |
| Participants | Female Age range: > 40 to 65+ years 91% MBC, 9% locally advanced Unclear if a first line trial for MBC 'patients eligible if they had a trial with 1 or 2 single agents' | |
| Interventions | CMFP vs CMFVP Arm I: (CMFP) Cyclophosphamide + methotrexate + 5‐fluorouracil + prednisone Arm II: (CMFVP) arm I + vincristine |
|
| Outcomes | Overall survival Response Toxicity | |
| Notes | All randomised patients included in analyses. Mean follow‐up times reported, 17 months CMFP arm and 19 months CMFVP arm. Survival curve calculated using life table methodology. Time‐to‐event data estimated from statistics presented in trial publication. Toxic related deaths not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | B ‐ Unclear |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear, patients less than 1 year postmenopausal were centrally randomised |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Toxicity | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Overall survival | Unclear risk | B ‐ Unclear |
| Selective reporting (reporting bias) | Low risk | A ‐ Adequate, outcomes reported |
| Other bias | Low risk | A ‐ Adequate |
Stein 1992.
| Study characteristics | ||
| Methods | Accrual dates: March 1987 to May 1990 Sample size: 114 Number of centres: unknown (UK) Randomisation method: not reported Baseline comparability: no significant imbalance apparent or reported | |
| Participants | Female Age range: mean 61‐62 years Unclear % MBC (advanced and progressive disease) Approx 90% first line for MBC | |
| Interventions | 2M vs 3M Arm I: (2M) mitozantrone + methotrexate Arm II: (3M) mitozantrone + methotrexate + mitomycin‐C | |
| Outcomes | Response Toxicity | |
| Notes | 107/114 eligible: reason for exclusion, randomised in error (4), primary site of cancer in doubt (3). Toxic related deaths not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | B ‐ Unclear |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Toxicity | Unclear risk | B ‐ Unclear |
| Selective reporting (reporting bias) | Low risk | A ‐ Adequate, outcomes reported |
| Other bias | Low risk | A ‐ Adequate |
Tranum 1982.
| Study characteristics | ||
| Methods | Accrual dates: not reported Sample size: 497 Multicentre, national (USA) Randomisation method not reported Baseline comparability: reported as balanced (no baseline data included in article) | |
| Participants | Female Age range not reported (34% < 50 years) 100% MBC 100% first‐line | |
| Interventions | AC vs FAC vs A+CMFVP
Arm I AC: doxorubicin plus cyclophosphamide
Arm II FAC: 5‐fluorouracil, doxorubicin plus cyclophosphamide
Arm III A+CMFVP: doxorubicin, cyclophosphamide, methotrexate, 5‐fluorouracil, vincristine plus prednisone Tranum 1982a = AC vs FAC |
|
| Outcomes | Overall survival Response Toxicity | |
| Notes | 448/497 evaluable: reasons given for exclusion, did not satisfy eligibility (13), major protocol violation or inadequate data or too recent entry onto study (36). Follow‐up details not reported. Based on minimum length of response: ‐ estimated minimum 7.25 months ‐ estimated maximum 39 months Unclear if time‐to‐event analyses included all patients randomised. Time‐to‐event outcomes not defined. Time‐to‐event data extracted directly from time‐to‐event curve. 11 toxic related deaths reported, however, these could not be included in the review as it is unclear in which arm the treatment deaths occurred. Doses of the same chemotherapy agent are reduced in the addition of a drug arm. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | B ‐ Unclear |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Toxicity | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Overall survival | Unclear risk | B ‐ Unclear |
| Selective reporting (reporting bias) | Low risk | A ‐ Adequate, outcomes reported |
| Other bias | Unclear risk | B ‐ Unclear, no details of baseline characteristics given (e.g. disease free interval, number metastatic sites, ER status) |
Vogel 1984.
| Study characteristics | ||
| Methods | Accrual dates: not reported (submitted for publication August 1983, accepted for publication December 1983) Number of centres unknown (USA) Sample size: 187 Randomisation method not defined. 'projected 2:1 randomisation in favour of CAF+CAMELEON arm Baseline comparability: 'no significant differences reported' ‐ baseline characteristics not displayed | |
| Participants | Female Age range: not reported 100% visceral MBC % first‐line not reported. Unclear if this is a first‐line trial for MBC 'prior chemotherapy with any of the study drugs rendered a patient ineligible' | |
| Interventions | CAF vs CAF+CAMELEON Arm I CAF: cyclophosphamide + doxorubicin + 5‐fluorouracil Arm II CAF+CAMELEON: arm I plus cytosine arabinoside + methotrexate + oncovin |
|
| Outcomes | Overall survival Response Toxicity Overall duration of disease control Remission duration | |
| Notes | 157/187 evaluable ‐ 8 on CAF arm and 22 on CAF+CAMELEON arm inevaluable. Reasons for this include patient ineligibility (2 CAF, 6 CAF+CAMELEON), early removal from study (4 CAF, 5 CAF+CAMELEON), patient refusal (3 CAF+CAMELEON), insufficient data (1 CAF, 1 CAF+CAMELOEN), protocol violation (1 CAF, 6 CAF+CAMELEON), drug toxicity (1 CAF+CAMELEON). Follow‐up details not reported. Evaluable patients only included in time‐to‐event analyses. Time‐to‐event calculated from date of entry into study. Time‐to‐event data estimated from statistics presented in trial publication. Follow‐up details not reported. Overall duration of disease control will be interpreted as progression free survival. 2 toxic related deaths reported, 1 due to renal failure (CAF+CAMELEON arm) and 1 due to granulocytopenia and sepsis (CAF arm). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | B ‐ Unclear |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | B ‐ Unclear |
| Incomplete outcome data (attrition bias) Response | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Toxicity | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Overall survival | Low risk | A ‐ Adequate |
| Incomplete outcome data (attrition bias) Duration of response | Low risk | A ‐ Adequate |
| Selective reporting (reporting bias) | Low risk | A ‐ Adequate, outcomes reported |
| Other bias | Low risk | A ‐ Adequate |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ahmann 1974a | Unclear that subjects allocated to addition of a drug arm were correctly randomised ‐ 'vincristine was administered by random distribution to half of the control group.' |
| Ahmann 1974b | Subjects allocated to addition of a drug arm were not randomised. |
| Ahmann 1975 | Unclear that subjects allocated to addition of vincristine arm were correctly randomised ‐ 'the other 50% of patients were treated on a random basis'. |
| Aisner 1981 | Unclear how many subjects randomised to each study arm. In addition, unclear how many subjects dropped out from each study arm and reason for drop out. |
| Aisner 1995 | The eligible arms are VATH versus VATH +CMFVP, but the CMFVP is not given on the third arm until the 3rd cycle (28 day cycles) and then cycles 5, 7, 9 etc. This delay of over 70 days of CMFVP treatment does not meet the definition of addition of a drug for this review. |
| Brown 1976 | Unclear how many subjects properly randomised and how many automatically allocated favourable treatment. All subjects (both randomised and allocated) are included in results so not possible to distinguish how many randomised and how many not randomised. |
| Brown 1977 | Not clear how many patients randomised to each arm ('patients assessed'). Unequal distribution between treatment arms are reported, however, the number of patient drop outs from each arm is not reported. No baseline data are reported. Over half the participants received prior chemotherapy but it is unclear if this was for MBC. |
| Cocconi 1990 | Trial of delayed chemotherapy. All patients receive first line CMF for 6 cycles. Therefore, this is not a trial of first line treatment. At point of randomisation, only patients with stable disease were randomised, which raises the issue of generalisation. |
| Cocconi 1999 | Trial of rotational cross‐over and sequential intensification which does not meet the definition of addition of a drug to a regimen for this review. |
| Costanza 1999 | The eligible arms in this study are CAF versus one of a number of single agents + CAF. In the addition of a drug arm, the single agent is given every 21 days for up to four cycles and then patients are given CAF. This delay of over 80 days for the single agent + CAF treatment does not meet the definition of addition of a drug for this review. |
| Creagan 1984 | The eligible arms in this study are CFP versus CAP‐CFP. In the addition of a drug arm, CFP is administered following four cycles (28 days cycles) of CAP. This delay of over 80 days of CFP treatment does not meet the definition of addition of a drug for this review. |
| Horton 1975 | Preliminary data only reported. Not all randomised subjects evaluated for response at time of publication. |
| Milano 1985 | Exploratory study, a subset of which have metastatic breast cancer. Only outcome reported is urinary polyamine levels. |
| Mukaiyama 1989 | Quality and conduct of the study questionable. Difficult to ascertain results from study as survival curve suggests no events for at least four months, response is reported as % of induction therapy and there is a small number of patients randomised (total N = 47). |
| Priestman 1975 | Exploratory study. Both loco‐regional and metastatic breast cancer patients are included, unclear how many MBC patients in trial. |
| Saeki 2007 | Dofequidar Fumarate not a chemotherapy agent. |
| Venturino 2000 | 2nd line chemotherapy trial. Patients had received one course of prior chemotherapy for metastatic disease (including CMF, CEF). |
| Von Minckwitz 2005 | The treatment arm did not add another chemotherapy agent, cyclophosphamide in the first study arm was switched to bendamustine. |
| Zhao 1986 | Overall quality of the trial is questionable. Unclear if first line trial, a large percentage of patients received prior chemotherapy, but unclear if for metastatic disease. 23% of patients lost to follow up and it is unclear why these patients dropped out of the study before the completion of two courses of the regimen. In addition, analysis was not by intention‐to‐treat. |
Differences between protocol and review
None.
Contributions of authors
DG designed the review and wrote the protocol. D B, with input from DG, collected the data for the review. D B wrote the results and discussion for the review in collaboration with NW and DG.
SK and PT updated the review.
Sources of support
Internal sources
NHMRC Clinical Trials Centre, Australia
External sources
U.S. Army Medical Research Acquisition Activity, USA
Declarations of interest
DB wrote the review published in May 2006 while u ndertaking her Masters course at The University of Sydney. Following its publication, DB was employed by the Clin ical Research Organisation Parexel (UK) from August 2006 until October 2009 and worked on a variety of oncology studies including breast cancer. DB was not involved in updating the review during 2009 and 2010 but it should be mentioned that DB wa s s till affiliated with Parexel in 2009.
Stable (no update expected for reasons given in 'What's new')
References
References to studies included in this review
Ahmann 1976a {published data only}
- Ahmann DL, O'Connell MJ, Bisel HF. An evaluation of Cytoxan/Adriamycin (CA) vs. Cytoxan/Adriamycin/5-Fluorouracil (CAF) vs. Cytoxan/5-Fluorouracil/Prednisone (CFP) in advanced breast cancer. In: Proceedings of the American Association for Cancer Research. Vol. 17. 1976:278.
Ahmann 1976b {published data only}
- Ahmann DL, O'Connell MJ, Bisel HF. An evaluation of Cytoxan/Adriamycin (CA) vs. Cytoxan/Adriamycin/5-Fluorouracil (CAF) vs. Cytoxan/5-Fluorouracil/Prednisone (CFP) in advanced breast cancer. In: Proceedings of the American Association for Cancer Research. Vol. 17. 1976:278.
Aisner 1987a {published data only}
- Aisner J, Weinberg V, Perloff M, Weiss R, Perry M, Korzun A, et al. Chemotherapy versus chemoimmunotherapy (CAF v CAFVP v CMF each +/- MER) for metastatic carcinoma of the breast: a CALGB study. Cancer and Leukemia Group B. Journal of Clinical Oncology 1987;5(10):1523-33. [DOI] [PubMed] [Google Scholar]
Aisner 1987b {published data only}
- Aisner J, Weinberg V, Perloff M, Weiss R, Perry M, Korzun A, et al. Chemotherapy versus chemoimmunotherapy (CAF v CAFVP v CMF each +/- MER) for metastatic carcinoma of the breast: a CALGB study. Cancer and Leukemia Group B. Journal of Clinical Oncology 1987;5(10):1523-33. [DOI] [PubMed] [Google Scholar]
Cavalli 1983a {published data only}
- Cavalli F, Pedrazzini A, Martz G, Jungi WF, Brunner KW, Goldhirsch A, et al. Randomized trial of 3 different regimens of combination chemotherapy in patients receiving simultaneously a hormonal treatment for advanced breast cancer. European Journal of Cancer and Clinical Oncology 1983;19(11):1615-24. [DOI] [PubMed] [Google Scholar]
Cavalli 1983b {published data only}
- Cavalli F, Pedrazzini A, Martz G, Jungi WF, Brunner KW, Goldhirsch A, et al. Randomized trial of 3 different regimens of combination chemotherapy in patients receiving simultaneously a hormonal treatment for advanced breast cancer. European Journal of Cancer and Clinical Oncology 1983;19(11):1615-24. [DOI] [PubMed] [Google Scholar]
Chlebowski 1983 {published data only}
- Chlebowski RT, Pugh R, Weiner JM, Block JB, Bateman JR. Doxorubicin and CCNU with or without vincristine in patients with advanced refractory breast cancer. A randomized trial. Cancer 1983;52(4):606-9. [DOI] [PubMed] [Google Scholar]
- Chlebowski RT, Pugh R, Weiner JM, Block JB, Bateman JR. Influence of vincristine on survival in advanced refractory breast cancer. Breast Cancer Research and Treatment 1981;1(1):171. [Google Scholar]
Creech 1979 {published data only}
- Creech R, Harris D, Grotzinger P, Engstrom P. Low dose therapy of metastatic breast cancer with CAMF vs. sequential CMF and adriamycin. Proceedings of the American Association for Cancer Research 1977;Mar 16-17:300.
- Creech R, Holroyde C, Catalano R, Koons L, Miller D, Engstrom P. Low dose CMF vs. CAMF treatment for metastatic breast cancer. Proceedings of the American Association for Cancer Research 1976;17:259.
- Creech RH, Catalano RB, Harris DT, Engstrom PF, Grotzinger PJ. Low dose chemotherapy of metastatic breast cancer with cyclophosphamide, adriamycin, methotrexate, 5-fluorouracil (CAMF) versus sequential cyclophosphamide, methotrexate, 5-fluorouracil (CMF) and adriamycin. Cancer 1979;43:51-9. [DOI] [PubMed] [Google Scholar]
Cummings 1981a {published data only}
- Cummings FJ, Gelman R, Tormey DC, DeWys W, Glick J. Adriamycin plus vincristine alone or with dibromodulcitol or ICRF-159 in metastatic breast cancer. Cancer Clinical Trials 1981;4:253-60. [PubMed] [Google Scholar]
Cummings 1981b {published data only}
- Cummings FJ, Gelman R, Tormey DC, DeWys W, Glick J. Adriamycin plus vincristine alone or with dibromodulcitol or ICRF-159 in metastatic breast cancer. Cancer Clinical Trials 1981;4:253-60. [PubMed] [Google Scholar]
Inoue 1984 {published data only}
- Inoue K, Ogawa M, Inagaki J, Horikoshi N, Miyamoto H, Ikeda K, et al. A randomized trial of adriamycin, cyclophosphamide, ftorafur (ACF) and adriamycin, cyclophosphamide, ftorafur, methotrexate (ACFM) in patients with advanced breast cancer. Cancer Chemotherapy and Pharmacology 1984;13:95-9. [PubMed] [Google Scholar]
Kennealey 1978 {published data only}
- Kennealey GT, Boston B, Mitchell MS, Knobf MK, Bobrow SN, Pezzimenti JF, et al. Combination chemotherapy for advanced breast cancer: two regimens containing adriamycin. Cancer 1978;42(1):27-33. [DOI] [PubMed] [Google Scholar]
Lokich 1977 {published data only}
- Lokich JJ, Skarin AT, Mayer RJ, Henderson IC, Blum RH, Frei E. Adriamycin plus alkylating agents in the treatment of metastatic breast cancer. Cancer 1977;40(6):2801-5. [DOI] [PubMed] [Google Scholar]
Marschke 1989 {published data only}
- Marschke RF Jr, Ingle JN, Schaid DJ, Krook JE, Mailliard JA, Cullinan SA, et al. Randomized clinical trial of CFP versus CMFP in women with metastatic breast cancer. Cancer 1989;63(10):1931-7. [DOI] [PubMed] [Google Scholar]
Nemoto 1982a {published data only}
- Horton J, Dao T, Cunningham T, Nemoto T, Sponzo R, Rosner D, et al. Alternating combination therapy for metastatic breast cancer. Proceedings of the American Association for Cancer Research 1976;17:247.
- Nemoto T, Horton J, Simon R, Dao TL, Rosner D, Cunningham T, et al. Comparison of four-combination chemotherapy programs in metastatic breast cancer: comparison of multiple drug therapy with cytoxan, 5-FU and prednisone versus cytoxan and adriamycin, versus cytoxan, 5-FU and adriamycin, versus cytoxan, 5-FU and prednisone alternating with cytoxan and adriamycin. Cancer 1982;49(10):1988-93. [DOI] [PubMed] [Google Scholar]
Nemoto 1982b {published data only}
- Nemoto T, Horton J, Simon R, Dao TL, Rosner D, Cunningham T, et al. Comparison of four-combination chemotherapy programs in metastatic breast cancer: comparison of multiple drug therapy with cytoxan, 5-FU and prednisone versus cytoxan and adriamycin, versus cytoxan, 5-FU and adriamycin, versus cytoxan, 5-FU and prednisone alternating with cytoxan and adriamycin. Cancer 1982;49(10):1988-93. [DOI] [PubMed] [Google Scholar]
Pannuti 1984 {published data only}
- Pannuti F, Iafelice G, Martoni A, Fruet F, Angelelli B, Casadei M. A new six-drug antiblastic regimen (R 14) at low doses (micropolychemotherapy) compared to CMF in the treatment of metastatic breast cancer: phase III study. Chemioterapia 1984;3(4):216-9. [PubMed] [Google Scholar]
Rosner 1989 {published data only}
- Rosner D, Lane WW, Nemoto T. Differential response to chemotherapy in metastatic breast cancer in relation to estrogen receptor level. Results of a prospective randomized study. Cancer 1989;64(1):6-15. [DOI] [PubMed] [Google Scholar]
- Rosner D, Nemoto T, Lane WW. A randomized study of intensive versus moderate chemotherapy programs in metastatic breast cancer. Cancer 1987;59(5):874-83. [DOI] [PubMed] [Google Scholar]
Segaloff 1985 {published data only}
- Segaloff A, Hankey BF, Carter AC, Escher GC, Ansfield FJ, Talley RW. An evaluation of the effect of vincristine added to cyclophosphamide, 5-fluorouracil, methotrexate, and prednisone in advanced breast cancer. Breast Cancer Research and Treatment 1985;5(3):311-9. [DOI] [PubMed] [Google Scholar]
Stein 1992 {published data only}
- Stein RC, Bower M, Law M, Bliss JM, Barton C, Gazet JC, et al. Mitozantrone and methotrexate chemotherapy with and without mitomycin C in the treatment of advanced breast cancer: a randomised clinical trial. European Journal of Cancer 1992;28A(12):1963-5. [DOI] [PubMed] [Google Scholar]
Tranum 1982 {published data only}
- Tranum B. Treatment of advanced breast cancer: A 3-arm prospective study. Proceedings of the American Association for Cancer Research 1977;Mar 16-17:274.
- Tranum BL, McDonald B, Thigpen T, Vaughn C, Wilson H, Maloney T, et al. Adriamycin combinations in advanced breast cancer. A Southwest Oncology Group Study. Cancer 1982;49(5):835-9. [DOI] [PubMed] [Google Scholar]
Vogel 1984 {published data only}
- Vogel CL, Smalley RV, Raney M, Krauss S, Carpenter J, Velez Garcia E, et al. Randomized trial of cyclophosphamide, doxorubicin, and 5- fluorouracil alone or alternating with a "cycle active" non-cross-resistant combination in women with visceral metastatic breast cancer: a Southeastern Cancer Study Group project. Journal of Clinical Oncology 1984;2:643-51. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Ahmann 1974a {published data only}
- Ahmann DL, Bisel HF, Hahn RG. Phase II clinical trial of isophosphamide (NSC-109724) in patients with advanced breast cancer. Cancer Chemotherapy Reports - Part 1 1974;58(6):861-5. [PubMed] [Google Scholar]
Ahmann 1974b {published data only}
- Ahmann DL, Bisel HF, Eagan RT, Edmonson JH, Hahn RG. Controlled evaluation of adriamycin (NSC-123127) in patients with disseminated breast cancer. Cancer Chemotherapy Reports 1974;58(6):877-82. [PubMed] [Google Scholar]
Ahmann 1975 {published data only}
- Ahmann DL, Bisel HF, Hahn RG, Eagan RT, Edmonson JH, Steinfeld JL, et al. An analysis of a multiple-drug program in the treatment of patients with advanced breast cancer utilizing 5-fluorouracil, cyclophosphamide, and prednisone with or without vincristine. Cancer 1975;36(6):1925-35. [DOI] [PubMed] [Google Scholar]
Aisner 1981 {published data only}
- Aisner J, Weinberg V, Perloff M, Weiss R, Raich P, Perry M, et al. Chemoimmunotherapy for advanced breast cancer: A randomized comparison of 6 combinations (CMF, CAF vs CAFVP) each with or without MER immunotherapy. A CALGB study. In: Proceedings of the American Association of Cancer Research. 1981:C-433.
Aisner 1995 {published data only}
- Aisner J, Cirricione C, Perloff M, Perry M, Budman D, Abrams J, et al. Combination chemotherapy for metastatic or recurrent carcinoma of the breast - A randomised phase III trial comparing CAF versus VATH versus VATH alternating with CMFVP: Cancer and Leukemia Group B study 8281. Journal of Clinical Oncology 1995;13(6):1443-52. [DOI] [PubMed] [Google Scholar]
Brown 1976 {published data only}
- Brown I, Ward HW. Doxorubicin in the treatment of advanced breast cancer; comparative studies of three combination chemotherapy regimes. Clinical Oncology 1976;2(2):105-11. [PubMed] [Google Scholar]
Brown 1977 {published data only}
- Brown I, Arthur K, Banks AJ, Bond WH, Chowdhury MS, Freeman WE, et al. The polychemotherapeutic treatment of advanced breast cancer. Clinical Oncology 1977;3(2):183-9. [PubMed] [Google Scholar]
Cocconi 1990 {published data only}
- Cocconi G, Bisagni G, Bacchi M, Buzzi F, Canaletti R, Carpi A, et al. A comparison of continuation versus late intensification followed by discontinuation of chemotherapy in advanced breast cancer. A prospective randomized trial of the Italian Oncology Group for Clinical Research (G.O.I.R.C.). Annals of Oncology 1990;1(1):36-44. [DOI] [PubMed] [Google Scholar]
Cocconi 1999 {published data only}
- Cocconi G, Bisagni G, Bella M, Acito L, Anastasi P, Carpi A, et al. Comparison of CMF (cyclophosphamide, methotrexate and 5-fluorouracil) with a rotational crossing and a sequential intensification regimen in advanced breast cancer. A prospective randomised study. American Journal of Clinical Oncology 1999;22(6):593-600. [DOI] [PubMed] [Google Scholar]
Costanza 1999 {published data only}
- Costanza ME, Korzun AH, Norton L, Rice MA, Wood WC. A fair trial for trimetrexate (TMTX) in advanced breast cancer. In: Breast cancer research and treatment. Vol. 12. 1988:125.
- Costanza ME, Weiss RB, Henderson C, Norton L, Berry DA, Cirricione C, et al. Safety and efficacy of using a single agent or a phase II agent before instituting standard combination chemotherapy in previously untreated metastatic breast cancer patients: report of a randomised study - Cancer and Leukemia Group B 8642. Journal of Clinical Oncology 1999;17(5):1397-1406. [DOI] [PubMed] [Google Scholar]
Creagan 1984 {published data only}
- Creagan ET, Green SJ, Ahmann DL, Ingle JN, Edmonson JH, Marschke RF. A phase III clinical trial comparing the combination cyclophosphamide, adriamycin, cisplatin with cyclophosphamide, 5-fluorouracil, prednisone in patients with advanced breast cancer. Journal of Clinical Oncology 1984;2(11):1260-5. [DOI] [PubMed] [Google Scholar]
Horton 1975 {published data only}
- Horton J, Dao T, Cunningham T, Nemoto T, Sponzo R, Rosner D. A comparison of 4 combination chemotherapies for metastatic breast cancer. Proceedings of the American Association for Cancer Research 1975;16:240.
Milano 1985 {published data only}
- Milano G, Thyss A, Caldani C, Renée N, Buray L, Lesbats G, et al. Treatment of human carcinoma by alpha-difluoromethylornithine: Effect on polyamine levels. Journal of Experimental and Clinical Cancer Research 1985;4:25-30. [Google Scholar]
Mukaiyama 1989 {published data only}
- Mukaiyama T, Ogawa M, Horikoshi N, Inoue K, Tada A, Ueno K, et al. [A randomized trial comparing ACF (adriamycin, cyclophosphamide, ftorafur) and ACF/MVMF (mitomycin C, vincristine, methotrexate, ftorafur)--a non-cross-resistant alternating chemotherapy of recurrent and advanced breast cancer]. [Japanese]. Gan to Kagaku Ryoho [Japanese Journal of Cancer & Chemotherapy] 1989;16(3 Pt 1):327-32. [PubMed] [Google Scholar]
Priestman 1975 {published data only}
- Priestman TJ. Results of a prospective clinical trial comparing two cytotoxic regimes containing adriamycin in women with advanced breast cancer. Clinical Oncology 1975;1(3):207-11. [PubMed] [Google Scholar]
Saeki 2007 {published data only}
- Saeki T, Nomizu T, Toi M, Ito M, Noguchi S, Kobayashi T, et al. Dofequidar fumarate (MS-209) in combination with cyclophosphamide, doxorubicin, and fluorouracil for patients with advanced recurrent breast cancer. Journal of Clinical Oncology 2007;25(4):411-7. [DOI] [PubMed] [Google Scholar]
Venturino 2000 {published data only}
- Venturino A, Comandini D, Simoni C, Merlini L, Naso C, Palumbo R, et al. Is salvage chemotherapy for metastatic breast cancer always effective and well tolerated? A phase II randomized trial of vinorelbine versus 5-fluorouracil plus leucovorin versus combination of mitoxantrone, 5-fluorouracil plus leucovorin. Breast Cancer Research and Treatment 2000;60(3):195-200. [DOI] [PubMed] [Google Scholar]
Von Minckwitz 2005 {published data only}
- Von Minckwitz G, Chernozemsky I, Sirakova L, Chilingirov P, Souchon R, Marschner N, et al. Bendamustine prolongs progression-free survival in metastatic breast cancer (MBC): a phase III prospective, randomized, multicentre trial of bendamustine hydrochloride, methotrexate and 5-fluorouracil (BMF) versus cyclophosphamide, methotrexate and 5-fluorouracil (CMF) as first-line treatment of MBC. Anti-Cancer Drugs 2005;16(8):871-7. [DOI] [PubMed] [Google Scholar]
Zhao 1986 {published data only}
- Zhao TP, Ding GX, Gao HY, Shen ZZ, Li KY. A clinical trial of homoharringtonine in the treatment of advanced breast cancer. Tumori 1986;72:395-8. [DOI] [PubMed] [Google Scholar]
Additional references
Carrick 2005
- Carrick S, Parker S, Wilcken N, Ghersi D, Marzo M, Simes J. Single agent versus combination chemotherapy for metastatic breast cancer. Cochrane Database of Systematic Reviews 2005, Issue 2. Art. No: CD003372. [DOI: 10.1002/14651858.CD003372.pub2] [DOI] [PubMed] [Google Scholar]
Esteva 2001
- Esteva FJ, Valero V, Pusztai L, Boehnke-Michaud L, Buzdar AU, Hortobagyi GN. Chemotherapy of metastatic breast cancer: What to expect in 2001 and beyond. The Oncologist 2001;6(2):133-46. [DOI] [PubMed] [Google Scholar]
Ferlay 2004
- Ferlay J, Bray F, Pisani P, Parkin DM. Cancer incidence, mortality and prevalence worldwide. GLOBOCAN, version 2.0;IARC CancerBase No. 5. Lyon, IARCPress, 2004: http://www-dep.iarc.fr/globocan/globocan.html.
Fossati 1998
- Fossati R, Confalonierir C, Torri V, Ghislandi E, Penna A, Pistotti V, et al. Cytotoxic and hormonal treatment for metastatic breast cancer: a systematic review of published randomized trials involving 31,510 women. Journal of Clinical Oncology 1998;16(10):3439-60. [DOI] [PubMed] [Google Scholar]
Ghersi 2004
- Ghersi D, Wilcken N, Simes J, Donoghue E. Taxane containing regimens for metastatic breast cancer. Cochrane Database of Systematic Reviews 2004, Issue 3. Art. No: CD003366. [DOI: 10.1002/14651858.CD003366.pub2] [DOI] [PubMed] [Google Scholar]
Hamilton 2005
- Hamilton A, Hortobagyi G. Chemotherapy: What progress in the last 5 years? Journal of Clinical Oncology 2005;23(8):1760-75. [DOI] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions. Chichester: John Wiley & Sons, 2008. [Google Scholar]
Hryniuk 1987
- Hryniuk WA, Figueredo A, Goodyear M. Applications of dose intensity to problems in chemotherapy of breast and colorectal cancer. Seminars in Oncology 1987;11(Suppl 4):3-11. [PubMed] [Google Scholar]
Lord 2004
- Lord S, Ghersi D, Gattellari M, Wortley S, Wilcken N, Simes J. Antitumour antibiotic containing regimens for metastatic breast cancer. Cochrane Database of Systematic Reviews 2004, Issue 4. Art. No: CD003367. [DOI: 10.1002/14651858.CD003367.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Parmar 1998
- Parmar MKB, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Statistics in Medicine 1998;17:2815-34. [DOI] [PubMed] [Google Scholar]
Stockler 2000
- Stockler M, Wilcken NRC, Ghersi D, Simes RJ. Systematic reviews of chemotherapy and endocrine therapy in metastatic breast cancer. Cancer Treatment Reviews 2000;26:151-68. [DOI] [PubMed] [Google Scholar]


