Abstract
Background
Plastic surgery is a transversal discipline that many people misunderstand, including general practitioners, medical students, paramedics and the public. Plastic surgeons often collaborate with physiotherapists for post-acute care and rehabilitation. They ensure optimal post-operative recovery of the patient. Herein, the authors assessed the medical knowledge and perceptions of plastic surgery by physiotherapists working outside health centers and explored their attitudes towards classic reconstructive surgery scenarios.
Methods
To assess physiotherapists’ medical knowledge and perceptions of plastic surgery, the authors conducted an online questionnaire survey. A total of 1,262 physiotherapists responded.
Results
The physiotherapists confirmed the suspected lack of knowledge regarding the plastic surgery field. Although they were generally aware that plastic surgeons perform cosmetic procedures and treat burns, they were largely unaware that plastic surgeons perform hand surgeries and microsurgical operations. More than 70% of them stated that they did not have the necessary knowledge to properly manage patients in this specialty. This lack of knowledge can sometimes have a negative impact on patients’ recovery, particularly for fear of making a mistake.
Conclusions
Physiotherapists, outside the hospital, have an incomplete conception of plastic surgery. They would need a specific plastic surgery training in order to manage these patients in an optimal way.
Keywords: Physiotherapists, surgical physiotherapy, plastic surgery, rehabilitation, perception
Introduction
Plastic surgery is the field of excellence in managing complex tissue defects. All types of soft tissues (muscle, fat, skin) can be used to cover visceral organ or bones (no spontaneous healing if exposed). It can be defined as “surgery of form” (1). This surgical specialty involves the restoration and reconstruction of the human body. It can be divided into two categories. The first is reconstructive surgery which includes a wide range of subspecialty as craniofacial surgery, hand surgery, microsurgery, ophthalmology and the treatment of burns. The other is cosmetic or aesthetic surgery (2,3).
Plastic surgeons work in healing and if necessary, can make a flap (local or free) to cover the tissue defect (4). Flap surgery is a technique in reconstructive surgery where any type of tissue is lifted from a donor site and moved to a recipient site preserving the pedicle (artery and vein). This is distinct from a graft, which does not have an intact blood supply and therefore relies on growth of new blood vessels. This is performed to fill a defect such as a wound resulting from injury or surgery when the remaining tissue is unable to support a graft, or to rebuild more complex anatomic structures such as breast or jaw (5).
Plastic surgeons collaborate with physiotherapists to improve functional and aesthetic results in post-operative care, particularly by following the healing process of burn scars.
Physical therapy (PT) is an allied health profession based on scientific evidence. It focuses on the biomechanics, range of motion and the pain of the person. PT is based on a functional assessment for therapeutic aims, using educational, manual and instrumental techniques. It promotes the maintenance or improvement of physical, mental and social health, disability management and wellness (6).
Physiotherapists ensure optimal post-operative recovery of the patient. Physiotherapy in a private practice offers many advantages extends the care outside the hospital. Thus, they have an important role on the recovery of plastic surgery patients, in particular in the fight against stiffness in hand surgery and against the appearance of disabling retractions in patients with burns (7). In France, private practice physiotherapists represent more than 80% of the type of exercise (this population is 85,223 in 2017) (8).
In our society, plastic surgeons tend to be considered mostly as “cosmetic surgeons” (9-11). This perception is also shared by some health care professionals (9,12-16). However, we did not find any studies concerning physiotherapists’ perception of plastic surgery.
The objective of this study was to evaluate the perception of plastic surgery by physiotherapists and the impact on patient care.
Method
Data was collected through a standardized questionnaire distributed through a social network.
The study was conducted from April 5, 2019 to June 5, 2019 and two reminders of these questionnaires were posted on social network over these three months.
No ethics approval was required for this type of study (survey). The answer to the questionnaire was considered as the physiotherapist’s consent to participate in the study.
The inclusion criteria was all private practice physiotherapists working in France who participated to the online questionnaire.
The exclusion criteria were physiotherapists working in the hospital and current students.
This questionnaire was self-reported and anonymous and consisted of 15 questions in 2 parts (Appendix 1).
The first part of the questionnaire was about respondent’s characteristics (age, sex, region of practice, number of years of practice).
The second part dealt with questions related to the subject of study (knowledge of plastic surgery by physiotherapists, their contact with plastic surgery patients, practical aspect in the management of plastic surgery patients and training of physiotherapists for plastic surgery).
The descriptive analysis was done by indicating the mean and standard deviation for quantitative variables and the percentage for qualitative variables.
The analyses were carried out using Excel software.
Results
The main results are available in the table (Table 1).
Table 1. Summary table (physiotherapist characteristic enrolled in this study).
| Physiotherapist characteristic | Result |
|---|---|
| Average age | 31.4 years |
| Gender | 68.7% female |
| Years of professional experience in private practice | 9.4 years |
| Lack of knowledge in plastic surgery | 37.7% |
| Extracurriculars knowledge in plastic surgery specialty | >60% (including 15% media) |
| Uninformed about the hand surgery activity performed by plastic surgeon | 83.1% |
| Uninformed about the microsurgery performed by plastic surgeon | 71.1% |
| Uninformed about the craniofacial surgery activity performed by plastic surgeon | 40.3% |
| Ignorance or vague notion of the flap surgery | 54% |
| Care management of plastic surgery patients | 74.6% |
| Uncomfortable with the management of a patient post conventional reconstruction surgery | 41.9% |
| Need to contact a surgeon to learn about the rehabilitation instructions | 80.8% |
| Avoidance of providing a physical therapy session by fear of making a mistake | 57.6% |
| Insufficient prerequisites during their training to properly manage plastic surgery patients | 70.4% |
| Usefulness of having more information on plastic surgery during their training | 96.2% |
Demographic and professional characteristics of the sample
We obtained 1,262 answers to the questionnaires The average age of the health professionals who responded to the questionnaire was 31.4 years; 68.7% of physiotherapists were women.
The health professionals who answered the questionnaire had an average of 9.4 years of private practice experience.
More than 80% of the French regions were represented. The largest participation was the Ile de France region (15.8%), the New Aquitaine region (15.6%), the Auvergne-Rhône-Alpes region (11.9%) and the Occitanie region (11.5%).
Knowledge of plastic surgery by physiotherapists
62% of the professionals surveyed consider that they know what plastic surgery is, more than a quarter (37.7%) admit to having a poorly defined vision of plastic surgery. No professional reported not knowing.
The majority of all health professionals surveyed (more than 60%) have an extracurricular knowledge of plastic surgery and 15.4% of physiotherapists responded that their main source of knowledge of plastic surgery is from the media. Vocational training remains the most frequent source of training (34% of physiotherapists). In 27.6% of cases, personal background of the non-professional’s career made it possible to acquire knowledge of the discipline. 10.1% of the respondents became aware of the plastic surgeon’s profession through their personal research and 9.9% through discussions with acquaintances outside the medical field (Figure 1).
Figure 1.
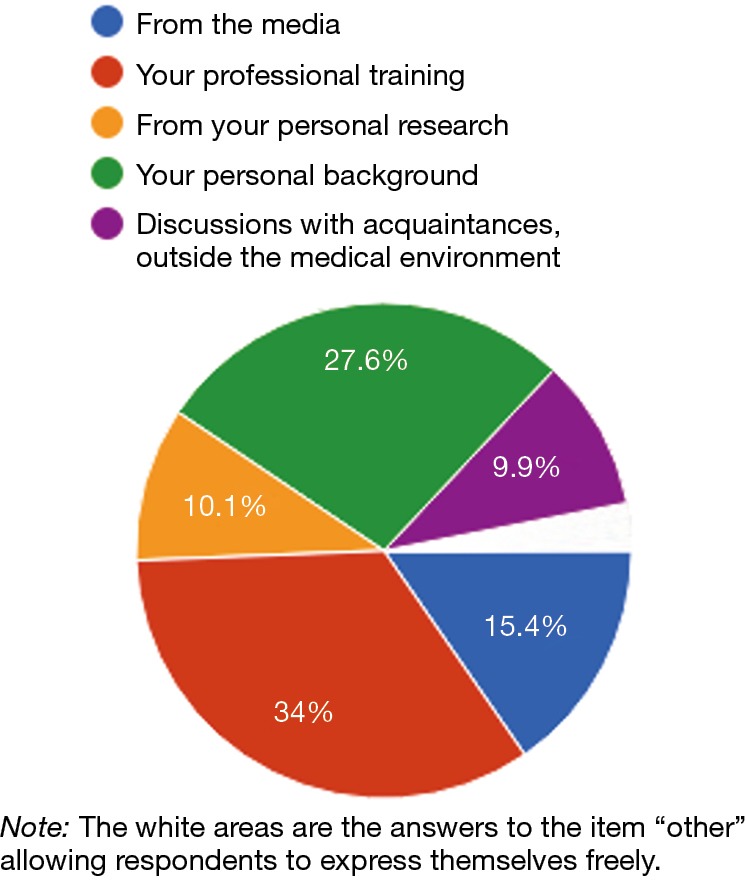
Main source of knowledge of plastic surgery by the paramedics interviewed.
While the reconstructive activity of the physical and aesthetic deformations of plastic surgery is well known (>90%), its craniofacial surgery activity is much less known (59.7%) by the paramedical professionals asked. We found a significant lack of knowledge about some of the sub-disciplines of plastic surgery. More than ¾ of these professionals (83.1%) were unaware that it included hand surgery and only 28.9% were aware of its activity as a micro-vessel surgery for the skin. Its activity in the management of weight loss sequelae, burns and scarring was relatively well known (>80%). These results are presented in Figure 2.
Figure 2.
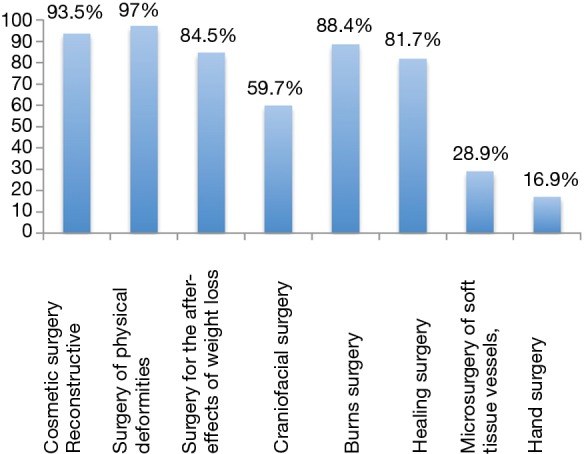
Activities associated with plastic surgery reported by the paramedics interviewed.
The flap, a surgery specific to the plastic surgeon’s profession, is not known or a vague concept for more than half of the physiotherapists (54%).
Contact with plastic surgery patients
The vast majority of the health workers questioned occasionally treat plastic surgery patients (74.6%). 10.2% of physiotherapists treat them frequently. Some professionals, even if they are in a minority, do not know if they have already managed this type of patient (4%).
A flap picture was presented with questions for the caregivers. This photo represents a patient’s arm who received a large dorsal flap to reconstruct a significant loss of right brachial substance caused by the removal of a large sarcoma. The patient, 6 weeks before the surgery, had been referred for physiotherapy at home.
Most of the healthcare surveyed (69.7%) had never managed patients who had this surgery. However, 29.1% have already had to manage these patients.
Caregivers were interviewed about their attitude towards the pathology of the patient to be cared for that was presented to them (whether or not they had already been confronted with this type of patient). Faced with a picture, 41.9% of private practice physiotherapists would have felt uncomfortable with the situation. Thus, it means that almost half of the caregivers who could have been called upon to take care of this patient would have experienced difficulties.
Management of plastic surgery patients
The vast majority of physiotherapists (80.8%) need to contact a surgeon to learn about rehabilitation instructions (“occasionally” in 69.8% of cases and “often” in 11% of cases).
Nearly half of the physiotherapists surveyed (49.52%) perform written care on prescriptions. More than half of the physiotherapists surveyed (50.55%) believe that surgeons’ prescriptions are often insufficient to properly provide the treatment.
More than half of physiotherapists (57.6%) have already avoided providing a treatment for fear of making a mistake. Thus, almost half of the caregivers surveyed (42.4%) did not provide prescribed care for the patient for fear of the consequences (Figure 3).
Figure 3.
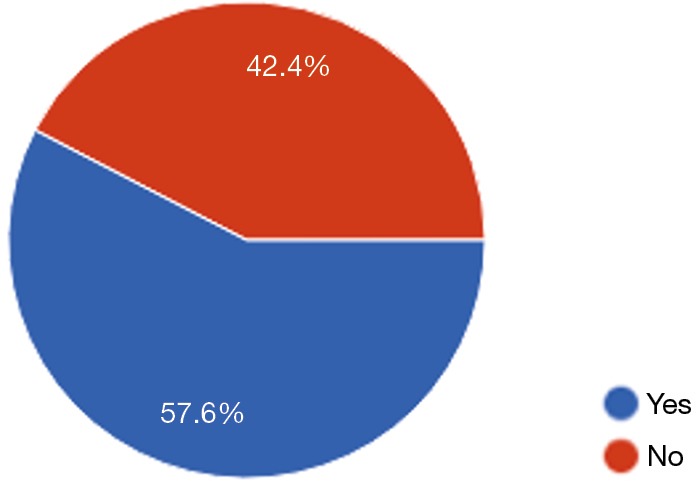
Avoidance of a treatment for fear of making a mistake.
Almost ¾ of professionals surveyed (70.4%) do not believe they have the necessary prerequisites during their training to properly manage plastic surgery patients.
The 1,262 professionals interviewed were almost unanimous on the usefulness of having more information on plastic surgery during their training (1,214/1,262 physiotherapists). Indeed, 96.2% of respondents agreed with this perspective.
Discussion
Public perception of plastic surgery is strongly influenced by the media and may not reflect the broad scope of work within the specialty (17). Studies have shown that this incomplete vision is also present in the medical profession, namely general practitioners (who are care coordinators and gatekeepers of specialist services), and medical students who are the next generation of general practitioners and hospital colleague (9).
If the perception of plastic surgery amongst the public and colleagues, present and future, is important, it is even more so with paramedical specialties, as they are categories of caregiver being the closest to patients.
Leonardo da Vinci said, ‘All our knowledge has its origins in our perceptions’, which illustrates well the impact that simple perceptions can have on a person’s reality.
Thus, plastic surgery is still a poorly known discipline (12,13) and our study confirms this fact in physiotherapists. Indeed, more than a quarter (37.7%) of the professionals admitted to having a biased vision of plastic surgery. The sources of plastic surgery knowledge by these health professionals are not always reliable (18-20).
Indeed, most of all the paramedical professionals questioned (66%) have an extra-professional origin of their knowledge of plastic surgery. The media is the main source of knowledge in plastic surgery for 15.4% of physiotherapists. The media on plastic surgery are often the source of clichés (TV plastic surgery series, TVreality channel, high-profile celebrity who abused plastic surgery, failed plastic surgery scandal). Thus, the media is still a strong vector of knowledge of plastic surgery, even with these health professions, which can be a source of misperception of the discipline with the spread of unrepresentative stigma (14). Furthermore, these media’s workers are rarely health professionals (20).
Although the large majority of the respondents occasionally treat plastic surgery patients (74.6%), some aspects of plastic surgery are largely unknown. So, we found that more than ¾ of the professionals surveyed (83.1%) were unaware that it included hand surgery and only 28.9% were aware of its microsurgical activity. Craniofacial activity was known to only 59.7% of caregivers. This lack of knowledge of the plastic surgeon as a hand, nerve and craniofacial surgeon has also been highlighted among medical interns (21-24). The flap, a surgery specific to the plastic surgeon’s profession, is not known or a vague concept for more than half of the professionals surveyed (54%). Our study showed that confronted with a specific situation of plastic surgery, almost half (41.9%) of the caregiver encountered difficulties. We noticed a marked lack of training in the discipline and almost all the professionals surveyed (70.4%) do not consider that they had the necessary prerequisites during their training to properly manage plastic surgery patients. Almost all respondents (96.2%) would find it useful to have more information in their training on plastic surgery.
Standard physiotherapy protocols are available for many of the most common reconstructive and orthopedic surgeries, such as anterior crucial ligament repair, breast reconstruction and carpal tunnel release (7). However, the availability of specific protocols for less common surgeries is limited. Thus, the rehabilitation program is based on the clinical experience and judgement of the physiotherapist, and consultation with the surgeon (7). If the physiotherapist does not have a good understanding of the pathology he is treating, then this rehabilitation program cannot be optimal.
This lack of knowledge can lead to negative impact on patients care. Indeed, almost half of the caregivers surveyed (42.4%) have already failed to follow prescriptions for fear of making a mistake.
The stage of the rehabilitation process, at which the physiotherapists treat the patient, may be dependent on their clinical setting. In the acute setting physiotherapists will see patients’ pre and post op, whereas in the primary care setting the patients will present at any stage from 2–6 weeks post operatively. The stages of rehabilitation are largely dependent on the healing process and the structure being repaired. Rehabilitation begins with the pre-op assessment and prescription of advice and exercise, and follows through to the patients’ return to normal activity, including higher level of functions (including sport participation). What the clinician needs to be aware of is the healing process of the repaired structure, the requirements of the repair pre-discharge from hospital and outpatient physiotherapy, the goals of the rehabilitation process and the safety precautions (7). This information can only be given accurately by the patient’s surgeon. Thus, we wondered about a possible link between this fear of making mistakes in the patient’s rehabilitation and a hypothetical difficulty of contact with surgeons, which provides essential information about the patient for physiotherapists. As we expected, we found a lack of communication between surgeons and these professionals. Less than half of the physiotherapists surveyed (49.52%) perform their care based on prescriptions and more than half of the physiotherapists surveyed (50.55%) believe that surgeons’ prescriptions are often insufficient to properly provide care. While the large majority of caregivers occasionally need to contact a surgeon for patient management (80.4%), this communication is sometimes difficult (25,26).
Health professional today acknowledge that poor communication is perhaps one of the most prevalent problems in medicine. A number of studies have looked into the causes and outcomes of poor communication (27).
Communication failures may be attributed to ineffective closed-loop communication, information lost in the transition of care.
We thought about different solutions that could improve the knowledge of paramedical health professionals regarding plastic surgery and the information that the surgeon wanted to transmit to the physiotherapists. The dissemination of information on the existence of reliable books and publications adapted to the caregiver’s specialty explaining the discipline can be a reliable first step in the discovery of plastic surgery (7,28,29). The creation of simple and informative factsheets of key concepts in the management of patients’ disease can also improve the situation. These factsheets could be given to patients leaving the hospital, for paramedical professionals who take care of them at home. In addition to that, promotion of appropriate university degrees for paramedical professionals is a way to familiarize yourself with the specialty. However, these trainings require time and often significant travel. Given the frequency of this situation, a reform of the initial training program for physiotherapy with more courses on the discipline, integrated into their training curriculum could be considered, with courses promoted by surgeons. Finally, the participation in conferences intended for multidisciplinary discussion on patient care can be an attractive way to discover the specialty. For example, the congress of the French Society of Burn with workshops and oral communications carried out and intended for physiotherapists, rehabilitation doctors, anesthetists and plastic surgeons.
Conclusions
This study shows for the first time the perception of private practice physiotherapists of plastic surgery. It appears a lack of knowledge of plastic surgery by private practice physiotherapists. This can have negative consequences on patient care.
A better knowledge of plastic surgery and the development of methods of communication would improve the management of plastic surgery patients.
Acknowledgments
We wish to thank Ms. Clara Baranger and Ms. Virginia Clark for their outstanding dynamism, inspiring energy and support.
Funding: None.
Appendix 1.
ANONYMOUS QUESTIONNAIRE TO PRIVATE PRACTICE PHYSIOTHERAPISTS:
Age (in years old):
Sex:
Number of years of liberal practice:
Place of exercise: (scrolling menu)
1. Do you think you know what the profession of plastic surgeon is all about? (One possible answer)
A. Yes
B. No
2. For you, plastic surgery is about: (One or more possible answers)
A. Cosmetic surgery
B. Reconstructive surgery of physical deformities
C. Surgery for the after-effects of weight loss
D. Craniofacial surgery
E. Burn surgery
F. Healing surgery
G. Microsurgery of soft tissue vessels, non-visceral
H. Hand surgery
Other
Specify:
3. Your knowledge of plastic surgery comes mainly from: (One or more possible answers)
A. From the media
B. Your professional training
C. From your personal research
D. Your personal background
E. Discussions with acquaintances, outside the medical environment
Other
Details:
4. Have you ever had to manage a patient who has had plastic surgery? (One possible answer)
A. Yes, frequently
B. Yes, occasionally
C. No
D. I do not know if I have taken care of plastic surgery patients
5a. About the picture below, have you ever been confronted with this type of patient to be cared for?(One possible answer)

A. Yes, often
B. Yes, occasionally
C. No
5b. If yes, have you ever been reluctant to take care of this type of patient at home: (One possible answer)
A. Yes
B. No
5c. If not, would you be reluctant to deal with this type of patient? (One possible answer)
A. Yes
B. No
6. Do you need to contact a surgeon for rehabilitation instructions: (One possible answer)
A. Yes, often
B. Yes, occasionally
C. No
7. In the context of a rehabilitation prescription prescribed by a surgeon: (One or more possible answers)
A. You do as prescribed
B. You rarely do as prescribed
C. Surgeons’ prescriptions are often sufficient to deliver proper treatment
D. Surgeons’ prescriptions are often insufficient to deliver proper care
E. Other
Details:
8. Have you ever omitted to provide care for fear of making a mistake? (One possible answer)
A. Yes
B. No
9. Do you think you know what a flap in plastic surgery is? (One possible answer)
A. Yes, I think I know exactly
B. Pretty much yes, but it isn’t clear
C. No
10. Do you think you have the necessary prerequisites during your training to properly manage plastic surgery patients? (One possible answer)
A. Yes
B. No
11. Would you find it useful to have more information in your training in plastic surgery? (One possible answer)
A. Yes
B. No
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Footnotes
Conflicts of Interest: AGL serves as an unpaid editorial board member of ATM from Dec 2018 to Nov 2020. The other authors have no conflicts of interest to declare.
References
- 1.Revol M, Binder JP, Danino A, et al. Manuel de chirurgie plastique reconstructrice et esthétique. 2ème édition. Sauramps Medical. 2009:882. [Google Scholar]
- 2.Neal S. The Art of Plastic Surgery. JAMA 2016;316:2072-3. 10.1001/jama.2016.17592 [DOI] [PubMed] [Google Scholar]
- 3.Grover R, Sanders R. Recent advances: Plastic surgery. BMJ 1998;317:397-400. 10.1136/bmj.317.7155.397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Buchanan PJ, Kung TA, Cederna PS. Evidence-Based Medicine: Wound Closure. Plast Reconstr Surg 2016;138:257S-70S. 10.1097/PRS.0000000000002775 [DOI] [PubMed] [Google Scholar]
- 5.Song DH, Ginard H, Russell RR, et al. Plastic Surgery: Essentials for Students. Plastic Surgery Education Foundation. 2007. Chapter 2: Grafts and Flaps. [Google Scholar]
- 6.Enhanced recovery after surgery and implications for nurse education- Art & Science, july 13,vol 25 no 45, 2011 - Mark Foss, lecturer and course director, MSc advanced clinical practice, School of Nursing, Midwifery and Physiotherapy, Queen’s Medical Centre, Nottingham. [DOI] [PubMed]
- 7.Hale A, O’Donovan R, Diskin S, et al. Impairment and disability short course Physiotherapy in burns, plastics and Reconstructive surgery. 2013. University of Limerick (IE).
- 8.Conseil National de l’Ordre des Masseurs-Kinésithérapeutes. Paris. Available online: www.ordremk.fr
- 9.Dunkin CS, Pleat JM, Jones SA, et al. Perception and reality-a study of public and professional perceptions of plastic surgery. Br J Plast Surg 2003;56:437-43. 10.1016/S0007-1226(03)00188-7 [DOI] [PubMed] [Google Scholar]
- 10.Hamilton GS, 3rd, Carrithers JS, Karnell LH. Public perception of the terms "cosmetic," "plastic," and "reconstructive" surgery. Arch Facial Plast Surg 2004;6:315-20. 10.1001/archfaci.6.5.315 [DOI] [PubMed] [Google Scholar]
- 11.Reid AJ, Malone PS. Plastic Surgery in the Press. J Plast Reconstr Aesthet Surg 2008;61:866-9. 10.1016/j.bjps.2008.06.012 [DOI] [PubMed] [Google Scholar]
- 12.Kim DC, Kim S, Mitra A. Perceptions and misconceptions of the plastic and reconstructive surgeon. Ann Plast Surg 1997;38:426-30. 10.1097/00000637-199704000-00020 [DOI] [PubMed] [Google Scholar]
- 13.Park AJ, Scerri GV, Benamore R, et al. What do plastic surgeons do? J R Coll Surg Edinb 1998;43:189-93. [PubMed] [Google Scholar]
- 14.Tanna N, Nitin J, Patel MD, et al. Professional perceptions of plastic and reconstructive surgery: what primary care physicians think. Plast Reconstr Surg 2010;126:643-50. 10.1097/PRS.0b013e3181de1a16 [DOI] [PubMed] [Google Scholar]
- 15.Fraser SJ, Al Youha S, Rasmussen PJ, et al. Medical Student Perception of Plastic Surgery and the Impact of Mainstream Media. Plast Surg (Oakv) 2017;25:48-53. 10.1177/2292550317694844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rogers AD, Dos Passos G, Hudson DA. The scope of plastic surgery. S Afr J Surg 2013;51:106-9. 10.7196/sajs.1792 [DOI] [PubMed] [Google Scholar]
- 17.de Blacam C, Kilmartin D, Mc Dermott C, et al. Public perception of Plastic Surgery. J Plast Reconstr Aesthet Surg 2015;68:197-204. 10.1016/j.bjps.2014.10.008 [DOI] [PubMed] [Google Scholar]
- 18.Chopan M, Sayadi L, Clark EM, et al. Plastic Surgery and Social Media: Examining Perceptions. Plast Reconstr Surg 2019;143:1259-65. 10.1097/PRS.0000000000005445 [DOI] [PubMed] [Google Scholar]
- 19.Callé SC, Evans JT. Plastic surgery in the cinema, 1917-1993. Plast Reconstr Surg 1994;93:422-33. 10.1097/00006534-199402000-00035 [DOI] [PubMed] [Google Scholar]
- 20.Branford OA, Kamali P, Rohrich RJ, et al. #PlasticSurgery. Plast Reconstr Surg 2016;138:1354-65. 10.1097/PRS.0000000000002814 [DOI] [PubMed] [Google Scholar]
- 21.Agarwal JP, Mendenhall SD, Moran LA, et al. Medical student perceptions of the scope of plastic and reconstructive surgery. Ann Plast Surg 2013;70:343-9. [DOI] [PubMed] [Google Scholar]
- 22.Agarwal JP, Mendenhall SD, Hopkins PN. Medical student perceptions of plastic surgeons as hand surgery specialists. Ann Plast Surg 2014;72:89-93. 10.1097/SAP.0b013e3182583f3b [DOI] [PubMed] [Google Scholar]
- 23.Denadai R, Muraro CA, Raposo-Amaral CE. Residents' Perceptions of Plastic Surgeons as Craniofacial Surgery Specialists. J Craniofac Surg 2015;26:2334-8. 10.1097/SCS.0000000000002081 [DOI] [PubMed] [Google Scholar]
- 24.Kling RE, Nayar HS, Harhay MO, et al. The scope of plastic surgery according to 2434 allopathic medical students in the United States. Plast Reconstr Surg 2014;133:947-56. [DOI] [PubMed] [Google Scholar]
- 25.Espin SL, Lingard LA. Time as a Catalyst for Tension in Nurse-Surgeon Communication. AORN J 2001;74:672-82. 10.1016/S0001-2092(06)61766-3 [DOI] [PubMed] [Google Scholar]
- 26.Taran S. An Examination of the Factors Contributing to Poor Communication Outside the Physician-Patient Sphere. Mcgill J Med 2011;13:86. [PMC free article] [PubMed] [Google Scholar]
- 27.Longstaffe R, Slade Shantz J, Leiter J, et al. Surgeon-Therapist Communication: Do All Members See Eye-to-Eye? Phys Sportsmed 2015;43:381-7. 10.1080/00913847.2015.1077096 [DOI] [PubMed] [Google Scholar]
- 28.Crestinu J. Chirurgie plastique-esthétique à l’usage des kinésithérapeutes. Spek, 1993:72. [Google Scholar]
- 29.Ferrand G, Hebting JM. Kinésithérapie de la face, du crâne et du cou. Elsevier Masson, 2015:216. [Google Scholar]


