Abstract
Background
Surgery is sometimes recommended for persistent lateral elbow pain where other less invasive interventions have failed.
Objectives
To determine the benefits and safety of surgery for lateral elbow pain.
Search methods
We searched CENTRAL (The Cochrane Library), MEDLINE, EMBASE, CINAHL and Web of Science unrestricted by date or language (to 15 December 2010).
Selection criteria
Randomised and controlled clinical trials assessing a surgical intervention compared with no treatment or another intervention including an alternate surgical intervention, in adults with lateral elbow pain.
Data collection and analysis
Two authors independently selected trials for inclusion, assessed risk of bias and extracted data.
Main results
We included five trials involving 191 participants with persistent symptoms of at least five months duration and failed conservative treatment. Three trials compared two different surgical procedures and two trials compared surgery to a non‐surgical treatment. All trials were highly susceptible to bias. Meta‐analysis was precluded due to differing comparator groups and outcome measures. One trial (24 participants) reported no difference between open extensor carpi radialis brevis (ECRB) surgery and radiofrequency microtenotomy, although reanalysis found that pain was significantly lower in the latter group at three weeks (MD ‐2.80 points on 10 point scale, 95% CI ‐5.07 to ‐0.53). One trial (26 participants) reported no difference between open ECRB surgery and decompression of the posterior interosseous nerve in terms of the number of participants with improvement in pain pain on activity, or tenderness on palpation after an average of 31 months following surgery. One trial (45 participants) found that compared with open release of the ERCB muscle, percutaneous release resulted in slightly better function. One trial (40 participants) found comparable results between open surgical release of the ECRB and botulinum toxin injection at two years, although we could not extract any data for this review. One trial (56 participants) found that extracorporeal shock wave therapy (ESWT) improved pain at night compared with percutaneous tenotomy at 12 months (MD 5 points on 100 point VAS, 95% CI 1.12 to 8.88), but there were no differences in pain at rest or pain on applying pressure.
Authors' conclusions
Due to a small number of studies, large heterogeneity in interventions across trials, small sample sizes and poor reporting of outcomes, there was insufficient evidence to support or refute the effectiveness of surgery for lateral elbow pain. Further well‐designed randomised controlled trials and development of standard outcome measures are needed.
Plain language summary
Surgery for elbow pain (tennis elbow)
This summary of a Cochrane review presents what we know from research about the effect of surgery for lateral elbow pain, also known as tennis elbow. The review shows the following.
In people with lateral elbow pain:
‐ percutaneous (smaller incision) surgery may slightly improve the ability to use your arm normally, compared with open surgery (in people who have had pain for a year or more and have failed to improve with non‐surgical treatments);
‐ radiofrequency microtenotomy applied to the affected tendon probably results in quicker pain improvement in the short term but results are the same in the long term when compared with open surgery;
‐ there was not enough information in the included studies to tell if surgery would make a difference in quality of life compared with not having surgery or compared with non‐surgical treatments.
There was no information about side effects in the included studies. Side effects of surgery may include infection, nerve damage, or loss of ability to straighten the arm.
What is lateral elbow pain and what is surgery?
Lateral elbow pain, or tennis elbow, can occur for no reason or be caused by too much stress on the tendon at the elbow. It can cause the outside of the elbow (lateral epicondyle) and the upper forearm to become painful and tender to touch. Pain can last for six months to two years, and may get better on its own. Many treatments have been used to treat elbow pain but it is not clear whether these treatments work or if the pain simply goes away on its own.
If the pain does not go away by itself or with various treatments like steroid injections or physiotherapy or both, surgery can be performed. Surgery on your elbow can include making a small cut in the arm and trimming damaged tissue from the tendon that joins the extensor carpi radialis brevis (ECRB) to the bone in the elbow (called an ECRB tenotomy), or releasing the tendon from the bone with a scalpel (called an ECRB release). The tenotomy may be done 'percutaneously', with a much smaller (1 cm) incision in the skin, or arthroscopically from within the joint. The ECRB tendon can also be detensioned further down in the mid‐forearm with a Z lengthening tenotomy. Another type of surgery that doesn't directly treat the ECRB tendon involves releasing the posterior interosseous nerve (PIN) that might be being compressed by the muscle (PIN decompression).
Best estimate of what happens to people with lateral elbow pain who have surgery
Pain (higher scores mean worse or more severe pain): ‐ people who had percutaneous (smaller incision) surgery with radio waves applied to the sore part of the elbow (radiofrequency microtenotomy) compared with open surgery (larger incision) rated their pain to be 3 points lower on a scale of 0 to 10 after 3 weeks (28% absolute improvement); ‐ people who had percutaneous surgery rated their pain to be 3.5 on a scale of 0 to 10 after 3 weeks; ‐ people who had open surgery rated their pain to be 6.5 on a scale of 0 to 10.
Physical function and disabilty (higher scores mean worse physical function or more disability): ‐ people who had percutaneous (smaller incision) surgery compared with open surgery (larger incision) rated their disability to be 4 points lower on a scale of 0 to 100 after 12 months (4% absolute improvement); ‐ people who had percutaneous surgery rated their disability to be 49 on a scale of 0 to 100; ‐ people who had open surgery rated their disability to be 53 on a scale of 0 to 100.
Summary of findings
Background
This is an update of a previous Cochrane review of surgery for lateral elbow pain (Buchbinder 2002).
Description of the condition
'Lateral elbow pain' is described by many analogous terms in the literature, including tennis elbow, lateral epicondylitis, rowing elbow, tendonitis of the common extensor origin, and peritendinitis of the elbow. For the purposes of this review the term lateral elbow pain will be used as it best describes the site of the pain and will allow for greater clarity of inclusion.
Lateral elbow pain is common (population prevalence 1% to 3%) (Allander 1974) and its peak incidence is at 40 to 50 years of age. Although the condition is self‐limiting it is associated with considerable morbidity. Typically an episode lasts between six months and two years (Murtagh 1988) with almost 80% of patients who present to primary care being completely recovered or much improved after six months (Bisset 2005; Smidt 2002a), increasing to 90% after one year (Bisset 2006; Smidt 2002a). Some patients however experience symptoms for much longer (Hudak 1996). The cost is therefore high, both in terms of loss of productivity and healthcare utilisation.
Many treatment options for lateral elbow pain have been proposed including non‐steroidal anti‐inflammatory drugs (Green 2001); orthotic devices (Borkholder 2004; Struijs 2002); physiotherapeutic modalities such as deep friction massage, exercises, laser and ultrasound therapy (Bisset 2005; Bjordal 2008; Brosseau 2002; Herd 2008; Kohia 2008; Smidt 2003); corticosteroid injections (Assendelft 1996; Smidt 2002b); shock wave therapy (Buchbinder 2005); acupuncture (Green 2002); and surgery (Buchbinder 2002; Lo 2007).
Treatment is usually conservative in the first instance. Surgery is generally reserved for the minority of people with persisting symptoms who have not responded to non‐operative treatment. Less than 10% of people eventually undergo surgery (Nirschl 1979), although reliable data on surgical rates in unselected patients are lacking.
Description of the intervention
Operative procedures for lateral elbow pain may be broadly grouped into the three main categories of open, percutaneous, and arthroscopic (Lo 2007); and various operations have been described based upon the surgeon's concept of the pathological entity (Goldberg 1987). For example, Nirschl and Pettrone proposed that the basic underlying lesion involves the attachment of extensor carpi radialis brevis (ECRB) muscle to the lateral epicondyle where overuse results in microscopic rupture and subsequent tendinous non‐repair with immature reparative tissue (Nirschl 1979). On this basis, the most described surgical procedures for lateral elbow pain involve excision of the identified lesion within the origin of the ECRB or release of the ECRB from the lateral epicondyle region, or both (Boyer 1999; Calvert 1985; Friden 1994; Goldberg 1987; Newey 1994; Nirschl 1979; Posch 1978; Spencer 1953; Yerger 1985).
Other pathology that has been described includes degeneration or stenosis of the orbicular ligament, chronic impingement of the redundant synovial fold between the radial head and the humerus, compression of the radial or posterior interosseous nerves or both, irritation of the articular branches of the radial nerve, traumatic periostitis of the lateral epicondyle, calcific tendinitis of the extensor muscles and chondromalacia of the radial head and capitellum (Bosworth 1955; Boyd 1973; Coonrad 1973; Cyriax 1936; Friedlander 1967; Gardner 1970; Goldberg 1987; La Freniere 1979; Osgood 1922; Trethowan 1929; Wittenberg 1992). Therefore, additional procedures that have been described include release of the anterior capsule, removal of inflamed synovial folds, resection of one third of the orbicular ligament, debridement of articular damage, release of the posterior interosseous nerve, denervation of the lateral epicondyle, denervation of the radiohumeral joint and excision of a radiohumeral bursa (Bosworth 1965; Boyd 1973; Coonrad 1973; Kaplan 1959; Osgood 1922; Trethowan 1929; Wilhelm 1996; Wittenberg 1992). Most of these procedures have been described as open operations.
Percutaneous release of the lateral epicondyle muscular attachments has also been reported (Yerger 1985), as has arthroscopic debridement of the lateral elbow area and release of the ECRB attachment.
Why it is important to do this review
Surgery may be recommended for people with persistent symptoms of lateral elbow pain who have failed to respond to non‐surgical management. While numerous uncontrolled trials have been performed and suggest beneficial outcomes, it is important to note that these studies do not take into account the favourable natural history of the condition, the tendency for people to regress to the mean; they also do not control for the placebo effect, which may be more profound with a surgical intervention. Our original Cochrane review of surgery for lateral elbow pain, published in 2001, failed to identify a single randomised controlled trial (Buchbinder 2002). Since then, several trials have been published and an update to review the available evidence on the effectiveness and safety of surgery for this condition is therefore warranted.
Objectives
To determine the effectiveness and safety of surgery in the treatment of patients with lateral elbow pain.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) or quasi‐randomised controlled clinical trials (CCTs) with methods of allocating participants to a treatment which are not strictly random, for example date of birth, hospital record number or alternation, were eligible for inclusion in this systematic review.
Types of participants
Inclusion in this review was restricted to trials with participants that met the following criteria: a) lateral elbow pain. Pain should be maximal over the lateral epicondyle, increased by pressure on the lateral epicondyle, and evident on resisted dorsiflexion of the wrist or middle finger, or both; b) no history of significant trauma or systemic inflammatory conditions such as rheumatoid arthritis; c) studies of various soft tissue diseases and pain due to tendinitis at all sites were included provided that the lateral elbow pain results were presented separately or > 90% of participants in the study had lateral elbow pain.
Types of interventions
All randomised controlled comparisons of surgical procedures versus no treatment (or placebo), another modality, or another surgical procedure were eligible for inclusion and comparisons established according to the intervention.
Types of outcome measures
All clinically relevant outcomes that were measured in the included trials at all time point were included.
Major, primary outcomes included pain, function or disability, and adverse effects.
Secondary outcomes included range of motion, quality of life, return to work, measures of participant and outcome assessor perception of overall effect (for example participant satisfaction), and grip strength.
We included pain, disability or function, and adverse events in our 'Summary of findings' tables.
Search methods for identification of studies
In the original review, we searched the literature from 1966 until 2001. For this update, we searched the following sources (from 2001 to December 2007) without any language restrictions (the electronic database searches were conducted on 21 December 2007). A further updated search was conducted (17 March 2009) to capture publications between 2007 and March, week 1, 2009; and to incorporate the newer optimally sensitive search strategies to identify reports of RCTs in MEDLINE that were first published by The Cochrane Collaboration in March 2008 (Lefebvre 2008). This search was last updated (on 13 December 2010) to capture publications between 2009 and 2010. 1. The Cochrane Musculoskeletal Review Group Specialised Register 2. Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library) 3. MEDLINE (Ovid) 4. EMBASE (Ovid) 5. CINAHL (Ovid) (until 2007); CINAHL (EBSCOhost) (for 2009 and 2010 searches) 6. ISI Web of Science 7. Reference lists in review articles and trials retrieved 8. Personal communication with experts in the field
For the database searches, we combined search terms describing lateral elbow pain and terms describing surgery with the optimally sensitive search strategies to identify reports of RCTs in MEDLINE (Lefebvre 2008). We modified the MEDLINE search as appropriate for the CENTRAL, EMBASE, CINAHL and Web of Science databases. The search strategies for all the electronic databases are outlined in Appendix 1; Appendix 2; Appendix 3; Appendix 4; Appendix 5.
Data collection and analysis
Selection of studies
For this updated review, we generated the electronic searches in MEDLINE, EMBASE, CINAHL and CENTRAL and downloaded the citations into Endnote 10. We independently reviewed the information to identify trials that could potentially meet the inclusion criteria. Full articles describing these trials were obtained and two authors (RB, RJ) independently applied the selection criteria to the studies. There was complete consensus concerning the final inclusion of trials.
Data extraction and management
Two review authors (RJ, RB), who were not masked to trial identifiers, independently extracted study characteristics including source of funding, study population and the selection criteria used to define it, intervention, analyses and outcomes using standardised data extraction forms. For trials that presented outcomes at multiple follow‐up times, we made an ad hoc decision to extract outcomes at the last time point only. We contacted the authors of recent original studies to obtain more information when needed. We recorded such contact in the notes section of the table 'Characteristics of included studies'.
Assessment of bias in included studies
Two authors (RB, RJ) independently assessed the risk of bias of each included study against key criteria: random sequence generation; allocation concealment; blinding of participants, intervention provider and outcome assessors; incomplete outcome data; selective outcome reporting; and other sources of bias. Studies that failed to meet these criteria were considered to have a high risk of bias. Also, we assessed the overall grading of the evidence related to each of the main outcomes using the GRADE approach (Schünemann 2008b). These methods have been updated since the publication of the protocol for this review to reflect revised guidance from The Cochrane Collaboration. We resolved disagreements by consensus.
Measures of treatment effect
In order to assess efficacy, raw data for outcomes of interest (means and standard deviations for continuous outcomes and number of events for dichotomous outcomes) as well as number of participants were extracted if available from the published reports. If reported data were converted or imputed, this was recorded in the notes section of the table 'Characteristics of included studies'. The results of each RCT were plotted as point estimates with 95% confidence intervals. Point estimates were measured as relative risk for dichotomous outcomes, and mean difference and standard deviation for continuous outcomes.
Data synthesis
The studies were first assessed for clinical homogeneity with respect to the duration of the disorder, control group and outcomes. As all included studies were clinically heterogeneous with different interventions and comparators, we described them separately and did not combine outcomes in a meta‐analysis. For clinically homogeneous studies, we planned to test statistical heterogeneity using the Q test (Chi2) and I2 statistic. We planned to pool clinically and statistically homogeneous studies using the fixed‐effect model, and clinically homogeneous and statistically heterogeneous studies using the random‐effects model. A sensitivity analysis was planned to assess any bias attributable to allocation concealment. However there were insufficient data for meta‐analysis or sensitivity analysis.
We presented the main outcomes (pain, disability or function and adverse events) of the review in 'Summary of findings' tables which include an overall grading of the evidence using the GRADE approach (Schünemann 2008b) and a summary of the available data on the main outcomes, as recommended by The Cochrane Collaboration (Schünemann 2008a). We also planned to calculate the number needed to treat (NNT), absolute change and relative difference for continuous outcomes (pain, disability or function) and dichotomous outcomes (adverse events), but the included trials did not report adverse events. Thus, for continuous outcomes the NNT to benefit (NNTB) was calculated using the Wells calculator software, available from the Cochrane Musculoskeletal Group editorial office (www.cochranemsk.org), which requires a minimal clinically important difference for input into the calculator. For disability measured using the DASH score, we assumed a 10 point difference in the mean Orthopaedic Surgeons' Disabilities of the Arm, Shoulder and Hand (DASH) score as a minimal clinically important change (Gummesson 2003). Absolute change (benefit) was calculated from the mean difference and expressed both as a per cent and in the original units, and relative difference in the change from baseline was calculated as the absolute benefit divided by the baseline mean of the control group.
Results
Description of studies
Results of the search
The updated search strategies yielded 632 references for the 2007 search; 220 extra references in the March 2009 update; and 337 references in December 2010. Of the 632 references yielded in the December 2007 search, we identified seven potentially eligible trials and found that three met inclusion criteria (Dunkow 2004; Keizer 2002; Leppilahti 2001). In the March 2009 search update, we identified a further three potentially eligible studies and found two that met inclusion criteria (Meknas 2008; Radwan 2008). We identified one potentially eligible study in the December 2010 search update (Yan 2009), which was awaiting translation and classification at the time of submission of this review for publication.
Included studies
Details of the five included trials are provided in the table, 'Characteristics of included studies'. The included trials were all published in English, and were performed in the UK (Dunkow 2004), the Netherlands (Keizer 2002), Finland (Leppilahti 2001), Norway (Meknas 2008) and Egypt (Radwan 2008). The number of participants in each trial were 45 (47 elbows) (Dunkow 2004), 40 (Keizer 2002), 26 (Leppilahti 2001), 24 (Meknas 2008) and 56 (Radwan 2008).
Study participants
Inclusion criteria varied slightly across studies (see table 'Characteristics of included studies'). Participants in all studies had conservative treatment prior to surgery, including physiotherapy and corticosteroid injections, for a time period of 12 months or more in Dunkow 2004 and Meknas 2008, longer than six months in Keizer 2002 and Radwan 2008, and in an unspecified time frame in Leppilahti 2001. Although all studies included participants with 'tennis elbow' or 'lateral epicondylitis', the diagnostic criteria used to describe the condition differed between studies. Dunkow 2004 included participants with resisted extension of the middle finger and pinch grip with the wrist in extension causing pain over the common extensor region. Keizer 2002 included participants with lateral elbow pain, pain at the lateral epicondyle during resisted dorsiflexion of the wrist with the elbow extended; and Meknas 2008 described similar inclusion criteria of pain and tenderness in the lateral epicondylar area with exacerbation of pain with resisted extension in the wrist and digits. Leppilahti 2001 used a broader definition and included participants with pain on the lateral aspect of the elbow on activity, and local tenderness, although more than two‐thirds had pain provoked by resisted finger extension. Radwan 2008 included participants with pain induced by two or more diagnostic tests (palpation of the lateral epicondyle; Thomsen test ‐ resisted wrist extension; chair test ‐ patient attempts to lift a 3.5 kg chair with shoulder flexed to 60 ° and elbow extended).
The age of participants was similar across studies (mean age in the fifth decade). The mean duration of symptoms was 11 (range 6 to 48) months in Keizer 2002; 23 (range 5 to 60) months in Leppilahti 2001; 28 months in one group and 22 months in the other group (range 12 to 60 months) in Meknas 2008; 18 (range 6 to 60) months in Radwan 2008; and not reported in Dunkow 2004.
Interventions
Dunkow 2004, Leppilahti 2001 and Meknas 2008 compared two surgical techniques. Dunkow 2004 compared open surgical release (removal of damaged portion) of the tendon of the extensor carpi radialis brevis (ECRB) muscle with percutaneous tenotomy (creation of a gap at the origin of the tendon). Leppilahti 2001 performed lengthening of the ECRB tendon, using an open surgical technique to access the tendon of the ECRB, and compared this to open surgery to decompress (dissect a space around the nerve by making an incision thought the muscle surrounding the nerve) the posterior interosseous nerve (PIN). Meknas 2008 compared open surgical release and repair of the ECRB tendon with radiofrequency tenotomy.
Radwan 2008 compared percutaneous tenotomy with extracorporeal shock wave therapy (ESWT). Keizer 2002 compared a modified Hohmann surgical release (also an open technique) of the tendon of the ECRB muscle with botulinum toxin injection.
Timing of follow up
All of the included trials measured outcomes at different time points following the intervention. Dunkow 2004 reported outcomes at an average of 12 months (range 12 to 14 and 11 to 13 in the percutaneous and open groups respectively); Keizer 2002 reported outcomes at 3, 6, 12 and 24 months; Meknas 2008 reported outcomes at 3, 6, 12 weeks and 10 to 18 months; Radwan 2008 reported outcomes at 3, 6 and 12 months; while Leppilahti 2001 reported outcomes at an average of 31 (range 22 to 48) months following the intervention.
Outcome assessment
No trial reported all pre‐specified primary outcomes. Trials did not all report the same outcomes, and also reported different measures of the same outcome often in a form not suitable for extraction in a meta‐analysis. This is described below and outlined in the table 'Characteristics of included studies'.
Pain, a pre‐specified primary outcome of the review, was not reported uniformly across studies. Dunkow 2004 did not report pain. Keizer 2002, Meknas 2008 and Radwan 2008 measured pain on a visual analogue scale (VAS); however Meknas 2008 did not report standard deviations in their published report (but provided data for this review). Keizer 2002 did not report means and standard deviations of the VAS scores but rather categorized the decrease in pain on a four point ordinal scale: 100% decrease in pain, 80% to 100% decrease, 50% to 80% decrease, < 50% decrease; thus we could not extract pain data for this trial. Leppilahti 2001 reported a subjective measure of pain relief on a four point ordinal scale, ranging from excellent to poor, and also reported the proportion with lateral elbow pain on activity and the proportion with pain on palpation.
Only two studies measured function using a validated scale. Dunkow 2004 used the American Academy of Orthopaedic Surgeons' Disabilities of the Arm, Shoulder and Hand (DASH) score, a 30‐item questionnaire which gives a score ranging from 0 to 100 points (0 = minimum disability and 100 = maximum disability). Meknas 2008 used the Mayo Elbow Performance Score (MEPS).
Two studies did not report if they measured adverse events (Dunkow 2004; Keizer 2002), while Radwan 2008 reported adverse events for one intervention group only.
Keizer 2002, Leppilahti 2001, Meknas 2008 and Radwan 2008 measured grip strength. Keizer 2002 using a dynamometer to obtain an objective measurement and also included a self‐assessment of loss of grip strength on a four point scale (ranging from no loss to severe loss). Meknas 2008 used a dynamometer but did not report standard deviations in their published report (but provided data for this review). Leppilahti 2001 and Radwan 2008 did not specify what instrument was used but Radwan 2008 reported grip strength compared with the normal side using a four point categorical scale (equal strength on both sides; up to 25% reduction; up to 50% reduction; up to 75% reduction).
Keizer 2002 also measured range of motion but, rather than report mean and standard deviation, the authors reported only the proportion of participants who had normal or limited range of motion.
Two trials used three‐point ordinal scales to measure participant reported success of the outcome: Dunkow 2004 used an ordinal scale with three possible responses: very pleased, satisfied or not satisfied with the result, while Keizer 2002 used the three response options of satisfied, moderately satisfied or not satisfied. Keizer 2002 also reported an outcome assessor rating of treatment outcome using a modified, Verhaar Scoring system (Verhaar 1993), which consists of a combination of pain scores and patient satisfaction to measure the outcome in a four‐point ordinal scale ('Excellent, Good, Fair, Poor'). Radwan 2008 measured participant reported residual pain at the end of follow‐up using a four point scale: excellent, good, acceptable or poor; and reported success as an excellent or good score. Leppilahti 2001 did not include a patient assessment of treatment success.
Three trials measured time to return to work (Dunkow 2004; Leppilahti 2001; Meknas 2008) and one trial measured proportion of participants in work at follow up (Keizer 2002).
Excluded studies
Six studies in total were excluded from this review: five identified in the 2007 and 2009 searches performed for this review update (Bartels 2005a; Bartels 2005b; Biggs 2006; Huang 2005; St Pierre 2008) plus a sixth study (Albrecht 1997) that was identified and excluded in the original review. Two studies were excluded as they were not randomised trials of surgery (Albrecht 1997; St Pierre 2008) while the remaining four were excluded as they did not include participants with lateral elbow pain (see the 'Characteristics of excluded studies' table).
Risk of bias in included studies
All of the five included trials failed to meet some of the risk of bias domains and thus the results of all trials may be biased.
Only one study (Meknas 2008) adequately described the sequence generation and concealment of allocation to treatment (personal communication with author), thus selection bias was minimised in this study. The results of the other four studies may have been subject to selection bias. No trial adequately reported if they blinded care‐givers, participants or outcome assessors. Due to the nature of the interventions, we judged that surgeons and most likely participants were not blinded. Outcome assessors could have been blinded more easily, at least for the trials comparing one type of surgery to another, but none of the trials reported if outcome assessors were blinded. As all the trials compared two active interventions, it is not known whether the lack of blinding would have favoured one treatment over the other.
Three trials reported outcome data for all randomised participants (Dunkow 2004; Leppilahti 2001; Meknas 2008) and one reported small losses balanced across treatment groups (Radwan 2008); thus the results of these trials were unlikely to be subject to attrition bias. Keizer 2002 did not address missing outcome data consistently across treatment groups and thus the results may be subject to bias. Four of the five trials selectively reported outcomes, mainly due to incomplete reporting of data. For example, the continuous outcomes pain and range of motion were reported in ordinal or dichotomized scales (Keizer 2002), and time to return to work was measured but reported only as a P value at one time point (Leppilahti 2001). It is uncertain if this would bias outcomes in one of the active treatment groups over the other.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
for the main comparison.
| Open extensor carpi radialis brevis release versus percutaneous extensor carpi radialis brevis tenotomy for chronic (>12 months) lateral elbow pain | ||||||
|
Patient or population: patients with chronic (>12 months) lateral elbow pain Settings: hospital Intervention: Open extensor carpi radialis brevis release versus percutaneous extensor carpi radialis brevis tenotomy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Open extensor carpi radialis brevis release versus percutaneous extensor carpi radialis brevis tenotomy | |||||
| Pain ‐ not measured | See comment | See comment | Not estimable | ‐ | See comment | Not measured |
| Disability DASH scale. Scale from: 0 to 100. (follow‐up: mean 12 months) | The mean disability in the control groups was 53 | The mean Disability in the intervention groups was 4 lower (7 to 1 lower) | 47 (1) | ⊕⊕⊝⊝ low1 | NNT= 4 (2 to 16) Absolute risk difference = 4% (1% to 7%) Relative percent change = 6% (1% to 10%) | |
| Adverse events ‐ not measured | See comment | See comment | Not estimable | ‐ | See comment | Not measured |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidance High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Lack of allocation concealment, unclear if outcome assessors blinded, and evidence from one small trial only
2.
| Radiofrequency tenotomy compared to open extensor carpi radialis brevis release for lateral elbow pain | ||||||
|
Patient or population: patients with lateral elbow pain Settings: hospital Intervention: Radiofrequency tenotomy Comparison: open extensor carpi radialis brevis release | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| open extensor carpi radialis brevis release | Radiofrequency tenotomy | |||||
| Pain‐ short term VAS scale. Scale from: 0 to 10. (follow‐up: 3 weeks) | The mean pain‐ short term in the control groups was 6.5 points | The mean Pain‐ short term in the intervention groups was 2.80 lower (5.07 to 0.53 lower) | 24 (1) | ⊕⊕⊕⊝ moderate1 | NNT= 3 (2 to 34) Absolute risk difference = ‐28% (‐50% to ‐5.3%) Relative percent change = ‐43% (‐78% to ‐1%) | |
| Pain‐ long term VAS. Scale from: 0 to 10. (follow‐up: 10‐18 months) | The mean pain‐ long term in the control groups was 6.5 points | The mean Pain‐ long term in the intervention groups was 0.2 higher (1.53 lower to 1.93 higher) | 24 (1) | ⊕⊕⊝⊝ low1,2 | Not statistically different | |
| Disability Mayo Elbow Performance. Scale from: 0 to 100. (follow‐up: 12 weeks) | The mean disability in the control groups was 60 points | The mean Disability in the intervention groups was 5.10 higher (9.52 lower to 19.72 higher) | 24 (1) | ⊕⊕⊝⊝ low1,3 | Not statistically different | |
| Adverse events ‐ not reported | See comment | See comment | Not estimable | ‐ | See comment | None reported for both treatment groups |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidance High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Unclear if outcome assessors blinded, and evidence from one small trial only
2 95% confidence interval includes no effect and the lower confidence limit crosses the minimal important difference (‐1.5 points on 10 point scale) for pain
3 95% confidence interval includes no effect
3.
| Open extensor carpi radialis brevis lengthening versus posterior interosseous nerve decompression for chronic (mean 23 months) lateral elbow pain | ||||||
|
Patient or population: patients with chronic (mean 23 months) lateral elbow pain Settings: Intervention: Open extensor carpi radialis brevis lengthening versus posterior interosseous nerve decompression | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Open extensor carpi radialis brevis lengthening versus posterior interosseous nerve decompression | |||||
| Pain ‐ not reported | See comment | See comment | Not estimable | ‐ | See comment | Pain available from single trial only, but measured using a short ordinal scale, therefore not extracted in review |
| Disability ‐ not measured | See comment | See comment | Not estimable | ‐ | See comment | |
| Adverse events ‐ not measured | See comment | See comment | Not estimable | ‐ | See comment | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidance High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
4.
| Percutaneous tenotomy versus extracorporal shock wave therapy for chronic (>6 months) lateral elbow pain | ||||||
|
Patient or population: patients with chronic (>6 months) lateral elbow pain Settings: Intervention: Percutaneous tenotomy versus extracorporal shock wave therapy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Percutaneous tenotomy versus extracorporal shock wave therapy | |||||
| Pain ‐ not reported | See comment | See comment | Not estimable | ‐ | See comment | Pain measured in single trial, but no overall pain score reported. |
| Disabilty ‐ not measured | See comment | See comment | Not estimable | ‐ | See comment | |
| Adverse events ‐ not measured | See comment | See comment | Not estimable | ‐ | See comment | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidance High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
We could not perform meta‐analysis of any outcome due to differing comparator arms, a lack of uniform measures of the same outcomes across trials, and failure to report outcomes in a form that could be extracted for meta‐analysis (for example pain measured in a continuous scale but only reported in the trial as ordinal groups). Therefore we present the results separately for each trial.
Open surgical release of ECRB versus percutaneous tenotomy
Data from one trial (47 participants) indicated that more participants in the percutaneous group were very pleased with the result compared with being either satisfied or not satisfied with the result (19, 9, 0) in comparison to those in the open group (6, 16, 2) (P = 0.012). The trial authors also reported that the percutaneous technique resulted in better function (improved median DASH scores) and faster return to work compared with the open surgical technique (Dunkow 2004). Similarly, assuming that the median approximates the mean, and calculating SD from the interquartile range, we found that the mean DASH score improved more in the percutaneous group compared with the open group 12 months following surgery: as measured by the DASH basic score mean difference (MD) ‐4 points (95% confidence interval (CI) ‐6.84 to ‐1.16) (Analysis 1.1). However, making the same assumptions for the change from baseline DASH score, we found no statistical difference in change scores between the two groups (MD ‐3.00 points, 95% CI ‐6.37 to 0.37). We found the DASH sport score improved more in the percutaneous group compared with the open group (MD ‐6.00 points, 95% CI ‐9.73 to ‐2.27) (Analysis 1.2) but the difference in the DASH high performance work score was not statistically significant between the two groups (MD ‐3.00 points, 95% CI ‐6.64 to 0.64) (Analysis 1.3). Participants who had percutaneous surgery returned to work sooner than those who had open surgery (MD ‐3.00 weeks, 95% CI ‐3.66 to ‐2.34) (Analysis 1.4).
1.1. Analysis.
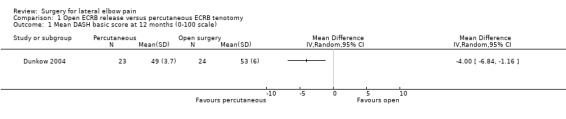
Comparison 1 Open ECRB release versus percutaneous ECRB tenotomy, Outcome 1 Mean DASH basic score at 12 months (0‐100 scale).
1.2. Analysis.
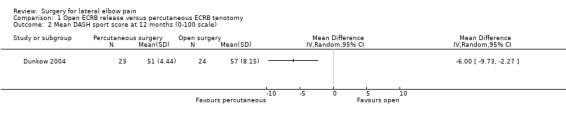
Comparison 1 Open ECRB release versus percutaneous ECRB tenotomy, Outcome 2 Mean DASH sport score at 12 months (0‐100 scale).
1.3. Analysis.
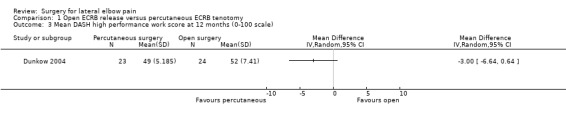
Comparison 1 Open ECRB release versus percutaneous ECRB tenotomy, Outcome 3 Mean DASH high performance work score at 12 months (0‐100 scale).
1.4. Analysis.
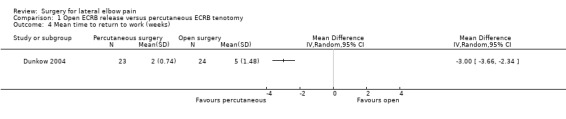
Comparison 1 Open ECRB release versus percutaneous ECRB tenotomy, Outcome 4 Mean time to return to work (weeks).
Open surgical release of ECRB versus radiofrequency microtenotomy
Data from one trial (24 participants) reported that pain was significantly improved from baseline in both the ECRB release and microtenotomy groups at all follow‐up times (Meknas 2008). The mean pain score in the microtenotomy group as measured by a 10 point VAS scale was 7.1 (SD 1.63) at baseline; reduced to 3.6 (SD 3.47) at 3 weeks; 3.2 (SD 2.64) at 6 weeks; 2.0 (SD 2.11) at 12 weeks; and 2.0 (SD 2.17) at 10 to 18 months follow up. The mean pain score in the ECRB release group was 6.5 (SD 1.58) at baseline; 6.4 (SD 2.13) at 3 weeks; 4.0 (SD 1.60) at 6 weeks; 3.1 (SD 2.40) at 12 weeks; and 1.8 (SD 2.14) at 10 to 18 months follow up. Meknas 2008 reported no significant differences in pain scores between the two groups at any time point. However reanalysis by the review authors found a significant difference in improvement in pain at three weeks favouring the microtenotomy group (MD ‐2.80 points on 10 point scale, 95% CI ‐5.07 to ‐0.53) (Analysis 2.1).
2.1. Analysis.
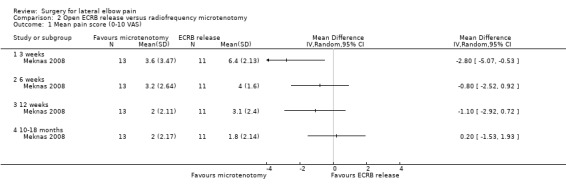
Comparison 2 Open ECRB release versus radiofrequency microtenotomy, Outcome 1 Mean pain score (0‐10 VAS).
The trial authors reported that function improved at 12 weeks follow up compared with baseline in both groups but the degree of improvement did not differ between groups (MD ‐5.10 points on a 100 point scale, 95% CI ‐19.72 to 9.52) (Analysis 2.2). Meknas 2008 reported that grip strength improved significantly from baseline in the microtenotomy group but not the release group, at 12 weeks; however the differences between groups were not significant (MD 3.50 kg, 95% CI ‐8.98 to 15.98) (Analysis 2.3).
2.2. Analysis.
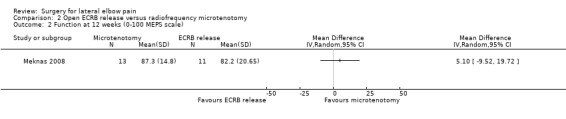
Comparison 2 Open ECRB release versus radiofrequency microtenotomy, Outcome 2 Function at 12 weeks (0‐100 MEPS scale).
2.3. Analysis.
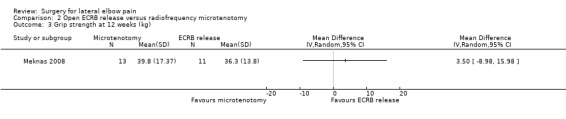
Comparison 2 Open ECRB release versus radiofrequency microtenotomy, Outcome 3 Grip strength at 12 weeks (kg).
There were no reported differences between groups with respect to time to return to work: ‐ 8/11 (73%) in the release group returned to work after a mean (SD) 11.5 (6.3) weeks while 11/13 (85%) in the microtenotomy group returned to work after a mean (SD) 10.7 (2.5) weeks. The other five participants did not return to work due to unrelated reasons. Skin temperature changes measured by dynamic infrared thermography prior to surgery were resolved in both groups following surgery (data not shown). There were no adverse effects from surgery in either group.
Open ECRB lengthening versus posterior interosseous nerve (PIN) decompression
Data from one trial (28 participants) indicated no differences between the two surgical techniques in the proportion of participants with lateral elbow pain on activity (Analysis 3.1), tenderness on palpation of the lateral epicondyle (Analysis 3.2) and tenderness on palpation over the posterior interosseous nerve (Analysis 3.3) at an average of 31 months following surgery. We could not extract any other outcomes from the trial. The trial authors reported no differences in the success of surgery or subjective assessment of pain between treatment groups (Leppilahti 2001).
3.1. Analysis.
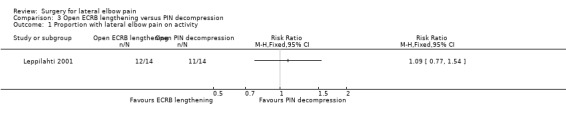
Comparison 3 Open ECRB lengthening versus PIN decompression, Outcome 1 Proportion with lateral elbow pain on activity.
3.2. Analysis.
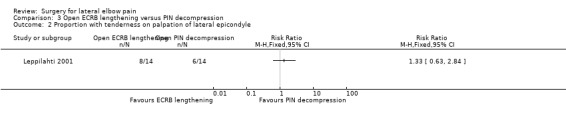
Comparison 3 Open ECRB lengthening versus PIN decompression, Outcome 2 Proportion with tenderness on palpation of lateral epicondyle.
3.3. Analysis.
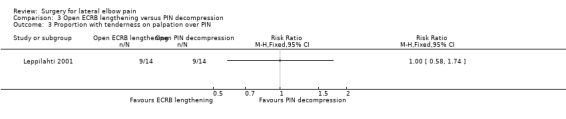
Comparison 3 Open ECRB lengthening versus PIN decompression, Outcome 3 Proportion with tenderness on palpation over PIN.
Open surgical release of ECRB versus botulinum toxin
One trial (40 participants) reported no difference in overall results of treatment as assessed by the investigators at two years follow up between participants undergoing surgery and those receiving botulinum toxin injection (Keizer 2002). We could not extract any data for analysis in RevMan.
Percutaneous tenotomy versus extracorporeal shock wave therapy (ESWT)
Data from one trial (56 participants) indicated that pain at night was improved significantly more in those receiving ESWT compared with those undergoing tenotomy at 12 months (MD 5 points on 100 point VAS, 95% CI 1.12 to 8.88) (Analysis 4.1). The trial authors (Radwan 2008) reported no difference in pain outcomes at any time point; which we confirmed at 12 months follow up for pain at rest (Analysis 4.2), pain on pressure (Analysis 4.3), pain on Thomsen test (Analysis 4.4) and pain on chair test (Analysis 4.5). We also found no difference between treatment groups in the proportion of participants with treatment success at 12 months follow up (Analysis 4.6).
4.1. Analysis.
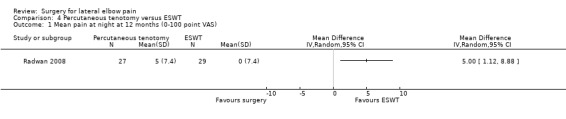
Comparison 4 Percutaneous tenotomy versus ESWT, Outcome 1 Mean pain at night at 12 months (0‐100 point VAS).
4.2. Analysis.
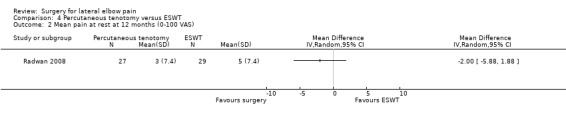
Comparison 4 Percutaneous tenotomy versus ESWT, Outcome 2 Mean pain at rest at 12 months (0‐100 VAS).
4.3. Analysis.
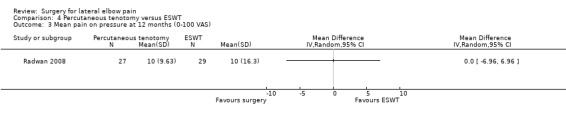
Comparison 4 Percutaneous tenotomy versus ESWT, Outcome 3 Mean pain on pressure at 12 months (0‐100 VAS).
4.4. Analysis.
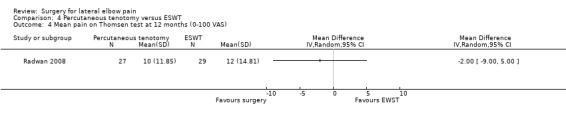
Comparison 4 Percutaneous tenotomy versus ESWT, Outcome 4 Mean pain on Thomsen test at 12 months (0‐100 VAS).
4.5. Analysis.
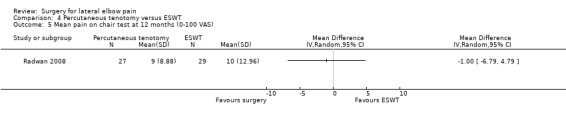
Comparison 4 Percutaneous tenotomy versus ESWT, Outcome 5 Mean pain on chair test at 12 months (0‐100 VAS).
4.6. Analysis.
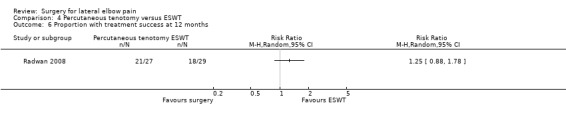
Comparison 4 Percutaneous tenotomy versus ESWT, Outcome 6 Proportion with treatment success at 12 months.
Discussion
Summary of main results
For this updated review, we identified five trials that fulfilled inclusion criteria. However, they were all small trials considered to be at risk of bias and used different interventions and outcome measures. This precluded meta‐analysis.
Open release with or without repair of the open extensor carpi radialis brevis (ECRB) tendon was studied in four trials and compared to percutaneous release of the ECRB tendon (Dunkow 2004), radiofrequency tenotomy (Meknas 2008), decompression of the PIN (Leppilahti 2001) or botulinum injection (Keizer 2002); while percutaneous release of the ECRB tendon was compared with ESWT in one trial (Radwan 2008).
Function, measured by the DASH, was reported to be significantly better following percutaneous tenotomy compared with open release of the ECRB tendon in one trial (Dunkow 2004), with a number needed to treat to benefit (NNTB) of 4 (Table 1). As there is some variation in the agreed minimally important clinical difference (MCID) in DASH score, we also calculated the NNTB using a MCID of 12.7 (personal communication, D Beaton) rather than 10 (Gummesson 2003) and found this changed the NNTB from 4 to 5. However, we are not confident of the results and further studies could change the direction of the effect. While pain outcomes were not reported in this trial, participants who had percutaneous surgery also returned to work sooner than those who had open surgery.
There was evidence from a single trial that radiofrequency microtenotomy resulted in quicker improvement in pain compared with open release of the ECRB tendon, with significant differences in pain seen at three weeks but not at later time points of 10 to 18 months (Meknas 2008; Table 2). Function, assessed by the Mayo Elbow Performance Score (MEPS), was found to be similar at 12 weeks in those who received open release of ECRB tendon compared to radiofrequency microtenotomy but data for other time points were not reported. There were no differences between groups reported for grip strength or time to return to work.
Data from single trials indicated that open release of the ECRB tendon was no different to botulinum toxin injection in terms of investigator assessment of success (Keizer 2002); open lengthening of the ECRB tendon did not differ from decompression of the PIN in terms of proportion of patients with pain (Leppilahti 2001); and pain at night was improved significantly more in those receiving extracorporeal shock wave therapy (ESWT) compared with those undergoing tenotomy, but there were no differences in other measures of pain (pain at rest, pain on pressure, pain on Thomsen test, and pain on chair test) (Radwan 2008).
No adverse events were reported in any of the trials.
Overall completeness and applicability of evidence
In the absence of placebo‐controlled trials there is insufficient evidence to be able to draw conclusions about the benefits and safety of release with or without repair of the ECRB tendon for persisting lateral elbow pain. There is a suggestion that percutaneous release of the ECRB tendon may result in better function and earlier return to work compared with open techniques but this is based upon a single trial at high risk of bias. Also based upon a single trial at high risk of bias, radiofrequency microtenotomy may confer earlier pain relief than open release but longer term outcomes appear similar. Based upon the results of three trials included in this review, we cannot be confident that one type of operation provides more benefit and less harm than another operative procedure. Based upon two single trials, open or percutaneous release of the ECRB tendon may result in similar outcomes to non‐operative treatment with botulinum injection or ESWT.
While operative interventions may benefit patients with persisting lateral elbow pain who have failed conservative treatment, surgical intervention remains an unproven treatment modality at this time.
Quality of the evidence
Overall, the trials were highly susceptible to bias as none met all key criteria for minimising bias, for example adequate allocation concealment, blinding of participants and outcome assessors. We suspect that the small number of trials identified is likely to be indicative of a lack of high quality research in the area rather than publication bias.
Potential biases in the review process
We are confident that the broad literature search used in this review has captured relevant literature and minimised the likelihood that we missed any relevant trials. Trial selection and data extraction, including risk of bias assessment, were done independently by two authors to minimise bias. However, the assumptions we made in transforming median and interquartile range to mean and SD in one trial may not be robust. The end of treatment scores revealed a significant benefit for those undergoing percutaneous surgery compared with open surgery in terms of function but there was no difference in function when change scores were used in the calculations.
The conclusions we can draw in our systematic review are limited by the quality of included trials. Trials were susceptible to bias and hampered by inadequate reporting and small sample size.
Agreements and disagreements with other studies or reviews
Our review is consistent with the conclusions of a recent review performed by Lo et al (Lo 2007). Their primary goal was to determine whether there was clear evidence to distinguish between open, percutaneous and arthroscopic operative approaches. While there are advantages and disadvantages to each approach, they concluded that based upon the current evidence, no technique was superior by any measure and they recommended deferring to expert surgical opinion for individual patients.
Authors' conclusions
Implications for practice.
There is a paucity of high quality evidence to either support or discourage the use of surgical interventions for lateral elbow pain. Patients undergoing surgical procedures for lateral elbow pain should do so in the knowledge that it is still an unproven treatment modality in this condition.
Implications for research.
Randomised controlled trials comparing surgical procedures to placebo, no treatment and non‐operative treatments are needed before any conclusions can be made about the role of surgery for lateral elbow pain. Planned trials should define lateral elbow pain with respect to chronicity and assess outcomes in terms of pain, function and adverse effect. The CONSORT statement should be used as a guide for both designing and reporting trials (Boutron 2008). Trial reporting should include the method of randomisation and treatment allocation concealment, follow up of all participants who entered the trial, and complete reporting of outcomes. Sample sizes should be reported and have adequate power to answer the research question; ideally trials should assess both the benefits and risks of surgery. To enable comparison and pooling of the results of RCTs, we suggest that future trials report means with standard deviations for continuous measures or number of events and total numbers analysed for dichotomous measures. Furthermore, development of a standard set of outcome measures for lateral elbow pain would enhance these research endeavours.
What's new
| Date | Event | Description |
|---|---|---|
| 15 December 2010 | New citation required but conclusions have not changed | In the original review no studies were identified that met inclusion criteria. In this review update, we included five trials. |
| 13 December 2010 | New search has been performed | New searches conducted 21 December 2008; 17 March 2009; 13 December 2010. Studies included or excluded: 15 December 2010 |
History
Protocol first published: Issue 3, 1999 Review first published: Issue 1, 2002
| Date | Event | Description |
|---|---|---|
| 10 June 2008 | Amended | CMSG ID C082‐R |
| 10 June 2008 | Amended | Converted to new review format. |
Acknowledgements
The first version of this review was supported by a fellowship granted to the second author by the Department of Health and Human Services, Victorian State Government, Victoria, Australia; and a one week's visiting fellowship to the Australasian Cochrane Centre granted by The Cochrane Collaboration. The authors would also like to thank former and current members of the Cochrane Musculoskeletal Group (CMSG) Editorial Team, Arne Gam, Bill Gillespie and Vivian Robinson for their helpful comments and suggestions for the original review, and the CMSG Trial Search Coordinator, Louise Falzon, for updating the search strategy and performing the searches for the updated review. The authors also thank Margaret Staples of the Monash Department of Clinical Epidemiology at Cabrini Hospital for providing statistical advice for the updated review, and Dr Khaled Meknas for providing unpublished trial data and descriptions of methodology for the Meknas 2008 study.
Appendices
Appendix 1. MEDLINE search strategy
exp Tennis Elbow/
exp Tendinopathy/
exp Tendon Injuries/
exp Elbow Joint/
exp Pain/
4 and 5
tennis elbow.tw.
(Tendinitis or Tendinosis or Tendonitis).tw.
(pain$ and lateral elbow).tw.
epicondylitis.tw.
common extensor origin.tw.
epicondylalgia.tw.
or/1‐3,6‐12
exp Surgery/
su.fs. (464870)
(surgery$ or surgeries or surgical or operat$).tw.
or/14‐16
clinical trial.pt.
randomized.ab
placebo.ab.
dt.fs.
clinical trials/
randomly.ab.
trial.ti.
groups.ab.
or/18‐23
animals/
humans/
27 and 28
27 not 29
26 not 30
and/13,17,31
Revised search 2007 to March Week 1, 2009
exp Tennis Elbow/
exp Tendinopathy/
exp Tendon Injuries/
exp Elbow Joint/
exp Pain/
4 and 5
tennis elbow.tw.
(Tendinitis or Tendinosis or Tendonitis).tw.
(pain$ and lateral elbow).tw.
epicondylitis.tw.
common extensor origin.tw.
epicondylalgia.tw.
or/1‐3,6‐12
exp Surgery/
su.fs.
(surgery$ or surgeries or surgical or operat$).tw.
or/14‐16
randomized controlled trial.pt.
controlled clinical trial.pt.
randomized.ab.
placebo.ab.
drug therapy.fs.
randomly.ab.
trial.ab.
groups.ab.
or/18‐25
(animals not (humans and animals)).sh.
26 not 27
and/13,17,28
Appendix 2. CENTRAL search strategy
MeSH descriptor Tennis Elbow explode all trees
MeSH descriptor Tendinopathy explode all trees
MeSH descriptor Tendon Injuries explode all trees
MeSH descriptor Elbow Joint explode all trees
MeSH descriptor Pain explode all trees
(#4 AND #5)
"tennis elbow":ti,ab
(Tendinitis or Tendinosis or Tendonitis):ti,ab
(pain* and "lateral elbow"):ti,ab
epicondylitis:ti,ab
"common extensor origin":ti,ab
epicondylalgia:ti,ab
(#1 OR #2 OR #3 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12)
MeSH descriptor Surgery explode all trees
Any MeSH descriptor with qualifier: SU
(surgery* or surgeries or surgical or operat*):ti,ab
(#14 OR #15 OR #16)
(#13 AND #17)
Appendix 3. EMBASE search strategy
exp Tennis Elbow/
exp Tendinitis/
exp Tendon Injury
exp Elbow/
exp PAIN/
4 and 5
tennis elbow.tw. (240)
(Tendinitis or Tendinosis or Tendonitis).tw.
(pain$ and lateral elbow).tw.
epicondylitis.tw.
common extensor origin.tw.
epicondylalgia.tw.
or/1‐3,6‐12
exp SURGERY/
su.fs
(surgery$ or surgeries or surgical or operat$).tw.
or/14‐16
13 and 17
random$.ti,ab.
factorial$.ti,ab.
(crossover$ or cross over$ or cross‐over$).ti,ab.
placebo$.ti,ab.
(doubl$ adj blind$).ti,ab.
(singl$ adj blind$).ti,ab.
assign$.ti,ab.
allocat$.ti,ab.
volunteer$.ti,ab.
crossover procedure.sh.
double blind procedure.sh.
randomized controlled trial.sh.
single blind procedure.sh.
or/19‐31
exp animal/ or nonhuman/ or exp animal experiment/
exp human/
33 and 34
33 not 35
32 not 36
18 and 37
Appendix 4. CINAHL search strategy
exp Tennis Elbow/
exp Tendinitis/
exp Tendon Injuries/
exp Elbow Joint/
exp PAIN/
4 and 5
tennis elbow.tw.
(Tendinitis or Tendinosis or Tendonitis).tw.
(pain$ and lateral elbow).tw.
epicondylitis.tw.
common extensor origin.tw.
epicondylalgia.tw.
or/1‐3,6‐12
exp Surgery, Operative/
su.fs.
(surgery$ or surgeries or surgical or operat$).tw.
or/14‐16
13 and 17
exp Clinical Trials/
clinical trial.pt.
(clinic$ adj trial$1).tw.
((singl$ or doubl$ or trebl$ or tripl$) adj (blind$3 or mask$3)).tw.
Randomi?ed control$ trial$.tw.
Random assignment/
Random$ allocat$.tw.
Placebo$.tw.
Placebos/
Quantitative studies/
Allocat$ random$.tw.
or/19‐29
18 and 30
Revised search March 2009, via EBSCOhost
S1 (MH "Tennis Elbow")
S2 (MH "Tendinitis+")
S3 (MH "Tendon Injuries+")
S4 ( ti pain* or ab pain* ) and ( ti lateral elbow or ab lateral elbow )
S5 ti epicondylitis or ab epicondylitis
S6 TI common extensor origin or AB common extensor origin
S7 ti epicondylalgia or ab epicondylalgia
S8 (MH "Elbow Joint")
S9 (MH "Pain+")
S10 S8 and S9
S11 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S10
S12 (MH "Surgery, Operative+")
S13 TI ( surgery* or surgeries or surgical or operat* ) or AB ( surgery* or surgeries or surgical or operat* )
S14 S12 or S13
S15 S11 and S14
S16 S11 and S14 Limiters ‐ Published Date from: 200712‐200903
Appendix 5. Web of Science search strategy
tennis elbow or tendinitis or tendonitis tendinosis or (elbow* and pain*) or epicondylitis or common extensor origin or epicondylalgia
surgery* or surgeries or surgical or operat*
#1 AND #2
trial* or random* or placebo* or control* or double or treble or triple or blind* or mask* or allocat* or prospective* or volunteer*or comparative or evaluation or follow‐up or followup
#3 AND #4
Data and analyses
Comparison 1. Open ECRB release versus percutaneous ECRB tenotomy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean DASH basic score at 12 months (0‐100 scale) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 Mean DASH sport score at 12 months (0‐100 scale) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3 Mean DASH high performance work score at 12 months (0‐100 scale) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4 Mean time to return to work (weeks) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 2. Open ECRB release versus radiofrequency microtenotomy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean pain score (0‐10 VAS) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 3 weeks | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 6 weeks | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 12 weeks | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 10‐18 months | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Function at 12 weeks (0‐100 MEPS scale) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3 Grip strength at 12 weeks (kg) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 3. Open ECRB lengthening versus PIN decompression.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Proportion with lateral elbow pain on activity | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Proportion with tenderness on palpation of lateral epicondyle | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Proportion with tenderness on palpation over PIN | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 4. Percutaneous tenotomy versus ESWT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean pain at night at 12 months (0‐100 point VAS) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 Mean pain at rest at 12 months (0‐100 VAS) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3 Mean pain on pressure at 12 months (0‐100 VAS) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4 Mean pain on Thomsen test at 12 months (0‐100 VAS) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5 Mean pain on chair test at 12 months (0‐100 VAS) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6 Proportion with treatment success at 12 months | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Dunkow 2004.
| Methods | Randomised controlled trial. Pre‐specified sample size calculation not reported. Overall validity of results: high risk of bias. |
|
| Participants | 45 participants (47 elbows); 24 elbows in the open group, with mean age of 43 years (range 30 to 58), and 23 elbows in the percutaneous group, mean age of participants was 46 years (range 32 to 58). Inclusion criteria: previous conservative treatment for 12 months (2 injections of 80mg hydrocortisone into the common extensor origin, and modification of activity); diagnosis of lateral epicondylitis‐ resisted extension of the middle finger and pinch grip with the wrist in extension provoking pain over the common extensor region. Exclusion criteria: none reported. | |
| Interventions | Group 1 (24 elbows), 'Open group': open surgical procedure consisting of 7cm incision over the common extensor origin, reflection of the extensor carpi radialis longus (ECRL) to expose the origin of the extensor carpi radialis brevis (ECRB), removal of the damaged portion of the tendon, and 3 drill holes in the lateral epicondyle. Group 2 (23 elbows), 'Percutaneous group': percutaneous surgical technique involving a 1cm incision over the mid‐point of the lateral epicondyle to expose the common extensor origin, which was divided, and a 1cm gap created at the common extensor origin with the wrist flexed. In both treatment groups, operations performed under tourniquet control, elbows wrapped in a wool and crepe bandage for 7 days; then bandage removed to begin post‐operative physiotherapy regime which was identical for both groups and supervised by the same physiotherapist. | |
| Outcomes | Assessed 12 months post‐operatively (range 12 to 14 months and 11 to 13 months in the percutaneous and open groups respectively. 1) American Academy of Orthopaedic Surgeons Disability of Arm, Shoulder and Hand (DASH) score: 100 point scale, 100 = maximum disability, 0 = minimum disability; assessed pre‐operatively and post‐operatively, and change in score from pre‐ to post‐operatively. 2) DASH score ‐ sports function section, and high‐performance work score (0 to 100 point scale, 100 = maximum disability) were also reported separately. 2) Participant satisfaction: self‐assessment of outcome rated as very pleased, satisfied or not satisfied with result 3) Median time to return to work. | |
| Sources of funding | Authors state, 'No benefits in any form have been received, or will be received from a commercial party related directly or indirectly to this article'. | |
| Notes | Co‐morbidity at baseline was reported to be 2 (range 1 to 3) and 2 (range 0.25 to 2) in the percutaneous and open groups although it is not clear what this was a measure of and whether the score reported is a mean or median. Post‐operative physiotherapy regime not described.
The trial authors reported median and interquartile ranges DASH scores and time to return to work; for the purposes of data extraction into RevMan, we assumed the median approximates the mean, and calculated the standard deviation assuming the width of the interquartile range will be approximately 1.35 standard deviations. We did not extract the participant satisfaction data, as the trial authors used a 3 point categorical scale that could not be logically dichotomized. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Comment: sequence generation not described |
| Allocation concealment? | Unclear risk | Quote: 'Patients were randomised to one of two groups using sealed envelopes'. Comment: unclear if envelopes were sequentially numbered and opaque, and unclear who opened the envelopes |
| Blinding? All outcomes | Unclear risk | Comment: unclear for participants and outcome assessor, surgeon unblinded (single surgeon performed all procedures) |
| Incomplete outcome data addressed? All outcomes | Low risk | Comment: no missing outcome data, and appears no participants crossed over to the other treatment |
| Free of selective reporting? | Unclear risk | Comment: pain not reported (may not have been measured); adverse events not reported, unclear if these were measured |
| Free of other bias? | Unclear risk | Comment: the trial does not report the number of participants (if any) screened and excluded prior to randomisation |
Keizer 2002.
| Methods | Randomised controlled trial. Pre‐specified sample size calculation not reported. Overall validity of results: high risk of bias. |
|
| Participants | 40 participants, 19 male and 21 female, mean age 42.8 years (range 25 to 72 years), mean duration of symptoms 10.5 months (range 6 to 48 months). Inclusion criteria: lateral elbow pain, pain at the lateral epicondyle on resisted dorsiflexion of the wrist with elbow extended, pain for at least 6 months, and failure of conservative treatment. Exclusion criteria: previous surgery; nerve entrapment; pregnancy; systemic neuromuscular disorders such as myasthenia gravis, neuropathy of the elbow (diagnosed by electromyography). | |
| Interventions | Group 1 (20 participants), 'Surgery group': surgical wrist extensor release (Hohmann operation), under Biers block anaesthesia, as an outpatient; 4cm curved incision over tip of lateral epicondyle and distal over the extensor carpi radius brevis to expose the extensor origin, the origin of the ECRB was incised transversely, just ventral of the lateral epicondyle, and the release continued to the synovium of the radiohumeral joint, the synovium was incised and the joint inspected for intraarticular lesions, then the wound closed, and covered with a compression bandage and sling for 2 weeks, then the sutures removed; following surgery participants were instructed to extend the elbow 3 times daily. Group 2 (20 participants), 'Botulinum toxin group': 30 to 40 units of botulinum toxin were injected into the ECRB; if insufficient paresis of the third and fourth fingers by 6 week follow up, a second injection was given. | |
| Outcomes | Assessed at 6 weeks, 3 months, 6 months, 1 year and 2 years.
1) Pain: participant subjective self‐assessment of presence of pain 4 point scale; no, occasional, regular, always. 2) Subjective loss of grip strength: participant subjective self‐assessment of loss of grip strength on 4 point scale; no, slight, moderate, severe. 3) Decrease in pain on VAS scale: 4 categories; 100%, 80‐100%, 50‐80%, <50%. 4) Satisfaction: participant subjective self‐assessment on 3 point scale; satisfied, moderately satisfied, not satisfied. 5) Sick leave on 3 point ordinal scale; full‐time, part‐time, unable to work. 6) Overall result: outcome assessor rated as 'Excellent, Good, Fair, Poor' using the modified Verhaar Scoring system (combination of pain and patient satisfaction, e.g., for 'Excellent': patient had no pain on lateral epicondyle, 100% decrease on VAS pain score, no pain on palpation, no pain on resisted extension of middle finger, and was satisfied; 'Good': occasional pain on lateral epicondyle, 80% to 100% decrease on VAS, slight palpation pain, slight pain provoked by resisted extension of middle finger, patient satisfied; 'Fair': moderate pain on lateral epicondyle, 50% to 80% decrease in VAS, moderate palpation pain, moderate pain provoked by resisted extension of middle finger, patient moderately satisfied; 'Poor': patient had pain on the lateral epicondyle, <50% decrease on VAS, severe palpation pain, severe pain on resisted extension of middle finger, patient dissatisfied). 7) Physical examination: includes range of motion, dichotomized as normal or limited (>5º); mean grip strength (with a dynamometer, elbow fully extended); local tenderness, resisted extension of wrist and resisted extension of middle finger categorised on 4 point scale (no, slight, moderate, severe). |
|
| Sources of funding | Not reported | |
| Notes | VAS, visual analogue scale The review authors made an ad hoc decision not to extract any outcomes, as data were not in a form easily amenable to meta‐analysis in RevMan (e.g., 4 point ordinal scales used for 'Overall result', and 3 point scale used to measure patient satisfaction not able to be dichotomized without losing information; mean but no variance reported for grip strength, range of motion only reported as dichotomized data); and it is unlikely that other (future) studies will use the same outcome measures (e.g., overall result categorised in the same way). Acknowledgements: JPH Reulen, Department of Clinical Neurophysiology, University Hospital, Maastricht, the Netherlands, for statistical advice. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Comment: sequence generation not described |
| Allocation concealment? | Unclear risk | Comment: not reported |
| Blinding? All outcomes | High risk | Comment: not reported, but the intervention‐providers and participants were most likely unblinded due to the nature of the interventions |
| Incomplete outcome data addressed? All outcomes | High risk | Comment: At 12 months 2/20 missing from the surgery group (refused assessment due to poor outcome); the authors did not impute data from these 2 lost participants; at 24 months, 1/20 from the botulinum toxin group was lost to follow up, the authors used 'last outcome carried forward', LOCF (from 12 month assessment for the 24 months evaluation of overall result (scored 'excellent'). This is likely to overestimate the treatment effect for the botulinum toxin group. Sick leave: numbers missing vary across time points, no reasons given |
| Free of selective reporting? | High risk | Comment: The trial authors measured pain on a continuous VAS scale, but report data only as decrease in pain on a 4 point ordinal scale; adverse events not reported (unclear if measured); range of motion, although measured on a continuous scale is only reported as a proportion of participants with normal or limited range |
| Free of other bias? | Low risk | |
Leppilahti 2001.
| Methods | Randomised controlled trial. Pre‐specified sample size calculation not reported. Overall validity of results: high risk of bias. | |
| Participants | 26 participants (28 elbows); mean duration of symptoms was 23 months (range 5 to 60 months). Decompression of posterior interosseous nerve (PIN group): 13 participants, 6 men and 7 women (14 elbows), mean age 42 years (range 33 to 50 years), 12 participants were manual workers who performed repetitive activities with their upper extremities. Lengthening of the extensor carpi radialis brevis (ECRB group): 14 participants, 7 men and 7 women (14 elbows), mean age 41 years (range 30 to 52 years), 11 participants were manual workers. Inclusion criteria: pain on activity on the lateral aspect of the elbow and local tenderness, previous conservative treatment (including physiotherapy, corticosteroid injections, splint or forearm support band) that did not result in continuous pain relief. Exclusion criteria: none reported. | |
| Interventions | Group 1, 'PIN group' (14 elbows): anterolateral longitudinal incision to expose the radial nerve in the groove between the brachioradial and brachial muscles, PIN exposed by distal dissection and decompressed at the arcade of Frohse by a 1‐2cm incision through the supinator muscle, then all sites of decompression along the PIN were released Group 2, 'ECRB group' (14 elbows): 4cm incision over the dorsilateral aspect of the forearm, proximal to where the thumb extensors obliquely cross the radius, Z‐shaped tenotomy dissection of the tendon of the ECRB muscle, and insertion of a suture to hold the ends loosely together. In both groups, surgery was performed under tourniquet control. | |
| Outcomes | Assessed at 22 to 48 months (mean 31 months) following surgery: 1) function: mean (and range) postoperative grip strength in both hands; 2) pain relief: 4 point ordinal scale as 'excellent'‐ upper limb completely relieved of the pre‐operative symptoms; 'good'‐ slight periodic pain; 'fair'‐ pain provoked by activity (but better than pre‐surgery); 'poor'‐ no improvement in pain or activity tolerance; 3) proportion of participants with lateral elbow pain on activity; 4) proportion of participants with tenderness on palpation at the lateral epicondyle of the humerus, and palpation over the PIN on the volar side of the elbow; 5) rate of re‐operation; 6) post‐operative complications; 7) time to return to work. | |
| Sources of funding | Not reported | |
| Notes | We did not extract pain relief data as the data presented were not easily amenable to meta‐analysis (short ordinal scale with no logical dichotomization point); we also did not extract mean grip strength, or time to return to work from the trial, as only range was provided as a measure of variance, and thus we could not estimate standard deviation in a robust way; the only data we could extract was the proportion of participants with lateral elbow pain on activity or with palpation. The authors report that there were no adverse events in their study. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Comment: not described |
| Allocation concealment? | Unclear risk | Comment: not reported |
| Blinding? All outcomes | High risk | Comment: unlikely; surgeon unblinded (single surgeon performed all procedures); unclear if lack of blinding of outcome assessor would bias toward one intervention |
| Incomplete outcome data addressed? All outcomes | Low risk | Comment: all randomised participants provided outcome data |
| Free of selective reporting? | High risk | Comment: the trial authors measured time to return to work, but did not report the mean (and SD), only a P value at one time point |
| Free of other bias? | Low risk | |
Meknas 2008.
| Methods | Randomised controlled trial; pre‐specified sample size calculation not reported. Overall validity of results: high risk of bias. | |
| Participants | 24 patients, 11 women and 13 men; mean age 49.2 years (range 36‐62 years) in the release group, and 46.7 years (range 30‐64 years) in the microtenotomy group; mean symptom duration in the release group was 27.6 months (range 12‐60 months), and 22 months (range 12‐50 months) in the microtenotomy group. Inclusion criteria: pain and tenderness in the lateral epicondylar area with exacerbation of pain with resisted extension in the wrist and digits, minimum symptom duration 12 months, and all participants failed conservative treatment which consisted of at least 3 injections with corticosteroid drugs that had a short‐term effect, NSAIDs for several weeks without clear improvement and physical therapy in primary health care institutes over a period of at least 3 months. Exclusion criteria: patients with cancer, severe systemic diseases, seriously reduced general health status, or with an unclear diagnosis with diffuse pain. |
|
| Interventions | All operations were performed by a single orthopaedic surgeon as outpatient procedures using local anaesthesia and sedation. Group 1, extensor tendon release and repair ('release group') (11 people): 3 to 4 cm incision centred slightly distal to the lateral epicondyle, and the origin of the common extensor was exposed by dissection, the interval between the extensor carpi radialis longus (ECRL) and extensor digitorum communis (EDC) was widened by a small incision in line with the fibres, exposing the extensor carpi radialis brevis (ECRB). The proximal origin of ECRB was released from its attachment, the damaged portion of the tendon was removed, and the epicondyle decorticated. Median length of the operation was 30 minutes (range 22‐40 minutes). Group 2, microtenotomy group (13 people): 3cm incision over epicondyle to expose the extensor tendon, radiofrequency (RF) energy delivered via a Topaz electrode perpendicular to the tendon surface in a grid‐like pattern of 3 to 6 micro ablations; tendon penetrated 3 to 5mm deep to perform micro ablation. Median length of the operation was 18 minutes (range 10‐23 minutes). |
|
| Outcomes | Outcomes measured at baseline, 3, 6 and 12 weeks post‐operatively. Pain also assessed at 10 to 18 months via telephone interview. 1) Pain: measured using a 0 to 10 point visual analogue (VAS) scale; 0 = no pain. 2) Grip strength: measured using a dynamometer in kg. 3) Function: measured by the Mayo Elbow Performance Score (MEPS). This is a multidimensional 100 point scale that includes 4 domains (pain ‐ maximum score of 45 points, function ‐ maximum score of 25 points, motion ‐ maximum score of 20 points, and stability ‐ maximum score of 10 points). A higher score reflects a better outcome. 4) Time to return to work. 5) Presence of lateral epicondylitis as indicated by 'hot spot' with dynamic infrared thermography (DIRT). 6) Adverse effects. |
|
| Sources of funding | Not reported. The authors report no conflict of interests. | |
| Notes | No standard deviations (SD) were reported for pain, grip strength and function in the published trial, however the authors provided them upon request. The trial authors reported that there was a lack of difference between treatments for all outcomes at all time points. We were able to perform a re‐analysis for the outcome of pain and we found that there was a significant difference between groups at 3 weeks favouring microtenotomy (MD ‐2.80 (‐5.07, ‐0.5), but no difference between groups at other time points for this outcome. We presented pain outcomes in RevMan at all time points, but at the last time point only for other outcomes (12 weeks for function; 12 weeks for strength). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Participants assigned to treatment group on day of operation by 'drawing lots' |
| Allocation concealment? | Low risk | Not reported in trial but personal correspondence with author (K Meknas) indicates 24 sealed envelopes, half indicating ECRB release, and half microtenotomy were available in the operating theatre; the participants were allocated treatment by drawing lots |
| Blinding? All outcomes | High risk | Patients informed of operation they would be receiving once they entered the operating theatre (personal communication, K Meknas); unclear if outcome assessors were aware of treatment, but participants could have informed them |
| Incomplete outcome data addressed? All outcomes | Low risk | Outcomes appeared to be included for all enrolled participants although not stated explicitly |
| Free of selective reporting? | High risk | All outcomes that were prespecified in the methods are included in the results however the results for all time points are not reported and some results are . Only the results for pain are presented for baseline, 3,6, 12 weeks and between 10 and 18 months. MEPS and grip strength are only reported for baseline and 12 weeks Trial authors did not report SD in the published report, but provided SDs upon request |
| Free of other bias? | Low risk | |
Radwan 2008.
| Methods | Randomised controlled trial. Pre‐specified sample size calculation reported. Overall validity of results: high risk of bias. | |
| Participants | 56 participants. Surgery group: n=27, 18 males, 16 with right side involved, 17 with dominant side involved, mean age 40 years (range 22 to 59 years), duration of symptoms 18 months (range 6 to 60 months). Extracorporal shock wave therapy (ESWT) group: n=29, 15 males, 18 with right elbow involved, 19 with dominant side involved, mean age 40 years (range 23 to 60 years), mean duration of symptoms 17 months (range 6 to 48 months). Inclusion criteria: lateral epicondylitis diagnosed by pain induced by 2 or more diagnostic tests (palpation of the lateral epicondyle; Thomsen test‐ resisted wrist extension; chair test‐ patient attempts to lift a 3.5 kg chair with shoulder flexed to 60 degrees and elbow extended); and failure of at least 6 months of conservative treatment including NSAIDs, corticosteroid injections, physical therapy, exercise program and elbow brace. Exclusion criteria: younger than 18 years; pregnant; local infection; malignancy; elbow arthritis; generalised polyarthritis; ipsilateral shoulder dysfunction; neurological abnormalities; radial nerve entrapment; cardiac arrhythmia or pacemaker; received corticosteroid injection in the previous 6 weeks. | |
| Interventions | Group 1, 'Operative group' (27 participants): percutaneous tenotomy, release of the common extensor origin performed through a transverse incision of 1‐2cm just distal to the lateral epicondyle, under general anaesthesia and tourniquet control; the common extensor origin was divided leaving a 1cm gap. The incision was left open to drain; bulky dressing and posterior plaster splint applied for one week. Group 2, 'ESWT Group' (29 participants): ESWT given under conscious sedation anaesthesia, repetitive high energy shock waves delivered by the electro hydraulic method; each patient received 100 graded shocks (14‐18 kV; 0.12‐0.22 J/mm2) initially to assess the effectiveness of anaesthesia, then 1400 shocks at 18 kV (0.22 mJ/m2) for a total of 1500 shocks at 4 shocks/s, and total energy delivered of 324.25J. |
|
| Outcomes | 1) Pain VAS 0 (no pain) to 100 (maximum pain) at baseline, 3, 6, 12 and 52 weeks:
2) Grip strength compared with normal side, on 4 point categorical scale at baseline, 3, 6, 12 and 52 weeks: 1 (equal strength on both sides), 2 (up to 25% reduction), 3 (up to 50% reduction), 4 (up to 75% reduction). 3) Participant assessment of residual pain compared with baseline using Roles and Maudsley criteria at 52 weeks: Excellent ‐ no pain, full movement, full activity; Good ‐ occasional discomfort, full movement, full activity; Acceptable‐ some discomfort after prolonged activities; Poor ‐ pain limiting activity. 4) Proportion of participants with treatment success at 52 weeks: defined as 'excellent' or 'good score' based on Roles and Maudsley criteria (in 3, above). |
|
| Sources of funding | None reported | |
| Notes | The trial authors reported median and interquartile ranges for continuous outcomes measured using 100mm VAS scale (night pain, rest pain, pain on pressure, Thomsen test, Chair test). For the purposes of data extraction into RevMan, we assumed the median approximates the mean, and calculated the standard deviation assuming the width of the interquartile range is approximately 1.35 standard deviations. We made an ad hoc decision to present outcomes in RevMan at the last time point only (12 months), due to lack of differences between treatments at all time points. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: 'Patients were randomised into two groups' Comment: method used to generate the allocation sequence not reported |
| Allocation concealment? | Unclear risk | Quote: 'Closed envelope technique' Comment: insufficient information reported to determine whether envelopes were sequentially numbered and opaque |
| Blinding? All outcomes | Unclear risk | Comment: blinding not reported, but unlikely, as it is not possible to blind participants and study personnel to treatment. It is also unlikely that outcome assessors were blinded to treatment; but it is uncertain if this would bias one treatment over the other |
| Incomplete outcome data addressed? All outcomes | Low risk | Comment 6/56 participants (3 in each group) did not complete the 12 month follow‐up; these losses were unlikely to bias outcomes |
| Free of selective reporting? | High risk | Adverse events reported for ESWT group; not reported for surgery group |
| Free of other bias? | Low risk | |
ECRL: extensor carpi radialis longus ECRB: extensor carpi radialis brevis DASH score: American Academy of Orthopedic Surgeons Disability of Arm, Shoulder and Hand score PIN: posterior interosseous nerve ECRB: extensor carpi radialis brevis NSAIDs: non‐steroidal anti‐inflammatory drugs
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Albrecht 1997 | Not clear if RCT, actual surgical intervention not randomised |
| Bartels 2005a | Participants did not have lateral elbow pain |
| Bartels 2005b | Participants did not have lateral elbow pain |
| Biggs 2006 | Participants did not have lateral elbow pain |
| Huang 2005 | Participants did not have lateral elbow pain |
| St Pierre 2008 | Not an RCT |
Characteristics of studies awaiting assessment [ordered by study ID]
Yan 2009.
| Methods | Randomised controlled trial, parallel arms |
| Participants | 26 patients (28 elbows) with recalcitrant lateral epicondylitis. The mean duration of conservative care was 23. 0 months (4 ‐ 60 months). The mean follow‐up was 17.4 months (4 ‐ 32 months) |
| Interventions | n=13 elbows treated with an open Nirschl procedure n=15 with an arthroscopic Nirschl procedure |
| Outcomes | Baseline and follow‐up: Pain: using VAS (visual analog scale) scores; Function: Mayo 12 points elbow scores; Time of return to work or sports; Participant satisfaction with procedure |
| Notes | Authors state in abstract that participants treated with the open surgical technique had 'better function in the return‐to work and sports' than the arthroscopic group |
Differences between protocol and review
In this review update, the methods for assessing risk of bias and the search strategy to identify randomised controlled trials were updated, and summary of findings tables were added to reflect current recommendations of The Cochrane Collaboration. To create 'Summary of findings' tables, we decided that pain, function, and adverse events were to be the main outcomes. All other outcomes were secondary outcomes and not displayed in the 'Summary of findings' tables.
Contributions of authors
RB was responsible for writing the manuscript, extracting and analysing the data and interpretation of results for the original and updated reviews. SG was responsible for performing the search, extracting and analysing the data and interpretation of results for the original review, and contributed to writing the manuscript for the original review. SB contributed surgical expertise and contributed to writing the manuscript for the original review. LB contributed data extraction in the original review. NS and WA contributed methodological expertise, and contributed to writing the original and updated reviews. RJ was responsible for selecting studies, extracting and analysing data, and for drafting the manuscript for the updated review.
Sources of support
Internal sources
Department of Epidemiology and Preventive Medicine, Monash University, Melbourne, Australia.
External sources
No sources of support supplied
Declarations of interest
None known
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Dunkow 2004 {published data only}
- Dunkow PD, Jatti M, Muddu BN. A comparison of open and percutaneous techniques in the surgical treatment of tennis elbow. The Journal of Bone and Joint Surgery. British volume 2004;86(5):701‐4. [DOI] [PubMed] [Google Scholar]
Keizer 2002 {published data only}
- Keizer SB, Rutten HP, Pilot P, Morre HHE, v Os JJ, Verburg AD. Botulinum toxin injection versus surgical treatment for tennis elbow: a randomized pilot study. Clinical Orthopaedics and Related Research 2002;401:125‐31. [DOI] [PubMed] [Google Scholar]
Leppilahti 2001 {published data only}
- Leppilahti J, Raatikainen T, Pienimaki T, Hanninen A, Jalovaara P. Surgical treatment of resistant tennis elbow. A prospective, randomised study comparing decompression of the posterior interosseous nerve and lengthening of the tendon of the extensor carpi radialis brevis muscle. Archives of Orthopaedic and Traumatic Surgery 2001;121(6):329‐32. [DOI] [PubMed] [Google Scholar]
Meknas 2008 {published data only}
- Meknas K, Odden‐Miland A, Mercer JB, Castillejo M, Johansen O. Radiofrequency microtenotomy: a promising method for treatment of recalcitrant lateral epicondylitis. American Journal of Sports Medicine 2008;36(10):1960‐5. [DOI] [PubMed] [Google Scholar]
Radwan 2008 {published data only}
- Radwan YA, ElSobhi G, Badawy WS, Reda A, Khalid S. Resistant tennis elbow: shock‐wave therapy versus percutaneous tenotomy. International Orthopaedics 2008;32:671‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Albrecht 1997 {published data only}
- Albrecht S, Kleihues H, Cordis R, Noack W. Diagnostic and treatment strategies for the operative treatment of radiohumeral epicondylopathy. Archives of Orthopaedic and Traumatic Surgery 1997;116:164‐72. [DOI] [PubMed] [Google Scholar]
Bartels 2005a {published data only}
- Bartels RHMA, Termeer EH, Wilt GJ, Rossum LGM, Meulstee J, Verhagen WIM, Grotenhuis JA. Simple decompression or anterior subcutaneous transposition for ulnar neuropathy at the elbow: A cost‐minimization analysis ‐ Part 2. Neurosurgery 2005;56(3):531‐5. [MEDLINE: ; 0148‐396X] [DOI] [PubMed] [Google Scholar]
Bartels 2005b {published data only}
- Bartels RHMA, Verhagen WIM, Wilt GJ, Meulstee J, Rossum LGM, Grotenhuis JA. Prospective randomized controlled study comparing simple decompression versus anterior subcutaneous transposition for idiopathic neuropathy of the ulnar nerve at the elbow: Part 1. Neurosurgery 2005;56(3):522‐9. [MEDLINE: ; 0148‐396X] [DOI] [PubMed] [Google Scholar]
Biggs 2006 {published data only}
- Biggs M, Curtis JA. Randomized, prospective study comparing ulnar neurolysis in situ with submuscular transposition. Neurosurgery 2006;58(2):296‐303. [MEDLINE: ; 0148‐396X] [DOI] [PubMed] [Google Scholar]
Huang 2005 {published data only}
- Huang JH, Zager EL, Tozer K, Kliot M, Kim DH, Murovic JA, Kline DG. Prospective randomized controlled study comparing simple decompression versus anterior subcutaneous transposition for idiopathic neuropathy of the ulnar nerve at the elbow: Part 1 ‐ Commentary. Neurosurgery 2005;56(3):529‐30. [MEDLINE: ; 0148‐396X] [DOI] [PubMed] [Google Scholar]
St Pierre 2008 {published data only}
- Pierre P, Nirschl RP. Mini‐open surgical management of tennis elbow pathology. Techniques in Orthopaedics 2008;23:158‐67. [Google Scholar]
References to studies awaiting assessment
Yan 2009 {published data only}
- Yan H, Cui GQ, Liu YL, Xiao J, Yang YP, Ao YF. [A randomized comparison of open and arthroscopic Nirschl debridement for refractory lateral epicondylitis]. Chung‐Hua Wai Ko Tsa Chih [Chinese Journal of Surgery] 2009;47(12):888‐91. [PubMed] [Google Scholar]
Additional references
Allander 1974
- Allander E. Prevalence, incidence and remission rates of some common rheumatic diseases and syndromes. Scandinavian Journal of Rheumatology 1974;3:145‐53. [DOI] [PubMed] [Google Scholar]
Assendelft 1996
- Assendelft WJJ, Hay EM, Adshead R, Bouter LM. Cortiosteroid injections for lateral epicondylitis: a systematic overview. The British Journal of General Practice 1996;46:209‐16. [PMC free article] [PubMed] [Google Scholar]
Bisset 2005
- Bisset L, Paungmali A, Vicenzino B, Beller E. A systematic review and meta‐analysis of clinical trials on physical interventions for lateral epicondylalgia. British Journal of Sports Medicine 2005;39(7):411‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bisset 2006
- Bisset L, Beller E, Jull G, Brooks P, Darnell R, Vicenzino B. Mobilisation with movement and exercise, corticosteroid injection, or wait and see for tennis elbow: randomised trial. BMJ 2006;333(7575):939. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bjordal 2008
- Bjordal JM, Lopes‐Martins RA, Joensen J, Couppe C, Ljunggren AE, Stergioulas A, Johnson MI. A systematic review with procedural assessments and meta‐analysis of low level laser therapy in lateral elbow tendinopathy (tennis elbow). BMC Musculoskeletal Disorders 2008;9:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Borkholder 2004
- Borkholder CD, Hill VA, Fess EE. The efficacy of splinting for lateral epicondylitis: a systematic review. Journal of Hand Therapy 2004;17(2):181‐99. [DOI] [PubMed] [Google Scholar]
Bosworth 1955
- Bosworth DM. The role of the orbicular ligament in tennis elbow. The Journal of Bone and Joint Surgery 1955;37A:527‐33. [PubMed] [Google Scholar]
Bosworth 1965
- Bosworth DM. Surgical treatment of tennis elbow. A follow‐up study. The Journal of Bone and Joint Surgery 1965;47A(8):1533‐6. [PubMed] [Google Scholar]
Boutron 2008
- Boutron I, Moher D, Altman DG, Schulz K, Ravaud P, for the CONSORT group. Methods and processes of the CONSORT Group: Example of an extension for trials assessing nonpharmacologic treatments. Annals of Internal Medicine 2008;148:295‐309. [DOI] [PubMed] [Google Scholar]
Boyd 1973
- Boyd HB, McLeod Jr HC. Tennis elbow. Journal of Bone and Joint Surgery 1973;55A:1183‐7. [PubMed] [Google Scholar]
Boyer 1999
- Boyer MI, Hastings H. Lateral tennis elbow: "Is there any science out there?". Journal of Shoulder and Elbow Surgery 1999;8:481‐91. [DOI] [PubMed] [Google Scholar]
Brosseau 2002
- Brosseau L, Casimiro L, Milne S, Welch V, Shea B, Tugwell P, Wells GA. Deep transverse friction massage for treating tendinitis. Cochrane Database of Systematic Reviews 2002, Issue 4. [Art. No.: CD003528. DOI: 10.1002/14651858.CD003528] [DOI] [PubMed] [Google Scholar]
Buchbinder 2002
- Buchbinder R, Green S, Bell S, Barnsley L, Smidt N, Assendelft WJJ. Surgery for lateral elbow pain in adults: a systematic review. Cochrane Database of Systematic Reviews 2002, Issue 1. [Art. No.: CD003525. DOI: 10.1002/14651858.CD003525] [DOI] [PubMed] [Google Scholar]
Buchbinder 2005
- Buchbinder R, Green SE, Youd JM, Assendelft WJ, Barnsley L, Smidt N. Shock wave therapy for lateral elbow pain. Cochrane Database of Systematic Reviews 2005, Issue 4. [Art. No.: CD003524. DOI: 10.1002/14651858.CD003524.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Calvert 1985
- Calvert PT, Macpherson IS, Allum RL, Bentley G. Simple lateral release in treatment of tennis elbow. Journal of the Royal Society of Medicine 1985;78:912‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Coonrad 1973
- Coonrad RW, Hooper WR. Tennis elbow: its course, natural history, conservative and surgical management. The Journal of Bone and Joint Surgery 1973;55A:1177‐82. [PubMed] [Google Scholar]
Cyriax 1936
- Cyriax MB. The pathology and treatment of tennis elbow. The Journal of Bone and Joint Surgery 1936;18:921. [PubMed] [Google Scholar]
Friden 1994
- Friden J, Lieber R. Physiological consequences of surgical lengthening of extensor carpi radialis brevis muscle‐tendon junction for tennis elbow. Journal of Hand Surgery 1994;19A:269‐74. [DOI] [PubMed] [Google Scholar]
Friedlander 1967
- Friedlander HL, Reid RL, Cape RF. Tennis elbow. Clinical Orthopaedics and Related Research 1967;51:109‐16. [PubMed] [Google Scholar]
Gardner 1970
- Gardner RS. Tennis elbow. The Journal of Bone and Joint Surgery 1970;72:248‐53. [Google Scholar]
Goldberg 1987
- Goldberg EJ, Abraham E, Siegel I. The surgical treatment of chronic lateral humeral epicondylitis by common extensor release. Clinical Orthopaedics and Related Research 1988;233:208‐12. [PubMed] [Google Scholar]
Green 2001
- Green S, Buchbinder R, Barnsley L, Hall S, White M, Smidt N, Assendelft WJJ. Nonsteroidal anti‐inflammatory drugs (NSAIDs) for treating lateral elbow pain in adults. Cochrane Database of Systematic Reviews 2001, Issue 4. [Art. No.: CD003686. DOI: 10.1002/14651858.CD003686] [DOI] [PubMed] [Google Scholar]
Green 2002
- Green S, Buchbinder R, Barnsley L, Hall S, White M, Smidt N, Assendelft W. Acupuncture for lateral elbow pain. Cochrane Database of Systematic Reviews 2002, Issue 1. [Art. No.: CD003527. DOI: 10.1002/14651858.CD003527] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gummesson 2003
- Gummesson C, Atroshi I, Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self‐rated health change after surgery. BMC Musculoskeletal Disorders 2003;4(11):Available from: http://www.biomedcentral.com/1471‐2474/4/11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Herd 2008
- Herd CR, Meserve BB. A systematic review of the effectiveness of manipulative therapy in treating lateral epicondylalgia. Journal of Manual and Manipulative Therapy 2008;16(4):225‐37. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hudak 1996
- Hudak P, Cole D, Haines A. Understanding prognosis to improve rehabilitation: The example of lateral elbow pain. Archives of Physical Medicine and Rehabilitation 1996;77:586‐92. [DOI] [PubMed] [Google Scholar]
Kaplan 1959
- Kaplan EB. Treatment of tennis elbow (epicondylitis) by denervation. The Journal of Bone and Joint Surgery 1959;41‐A:147‐51. [PubMed] [Google Scholar]
Kohia 2008
- Kohia M, Brackle J, Byrd K, Jennings A, Murray W, Wilfong E. Effectiveness of physical therapy treatments on lateral epicondylitis. Journal of Sport Rehabilitation 2008;17(2):119‐36. [DOI] [PubMed] [Google Scholar]
La Freniere 1979
- Freniere JG. Tennis elbow ‐ Evaluation, treatment and prevention. Physical Therapy 1979;59:742. [DOI] [PubMed] [Google Scholar]
Lefebvre 2008
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0 (updated February 2008). The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org (accessed 18 June 2008).
Lo 2007
- Lo MY, Safran MR. Surgical treatment of lateral epicondylitis: a systematic review. Clinical Orthopaedics and Related Research 2007;463:98‐106. [DOI] [PubMed] [Google Scholar]
Murtagh 1988
- Murtagh JE. Tennis elbow. Australian Family Physician 1988;17(90):94‐5. [PubMed] [Google Scholar]
Newey 1994
- Newey ML, Patterson MH. Pain relief following tennis elbow release. Journal of the Royal College of Surgeons of Edinburgh 1994;39:60‐1. [PubMed] [Google Scholar]
Nirschl 1979
- Nirschl RP, Pettrone FA. The surgical treatment of lateral epicondylitis. The Journal of Bone and Joint Surgery 1979;61A(6):832‐9. [PubMed] [Google Scholar]
Osgood 1922
- Osgood R. Radiohumeral bursitis, epicondylitis eoicondylalgia (tennis elbow). Archives of Surgery 1922;4:420. [Google Scholar]
Posch 1978
- Posch JN, Goldberg VM, Larrey R. Extensor fasciotomy for tennis elbow: a long term follow‐up study. Clinical Orthopaedics and Related Research 1978;135:179‐82. [PubMed] [Google Scholar]
Schünemann 2008a
- Schünemann HJ, Oxman AD, Higgins JPT, Vist GE, Glasziou P, Guyatt GH. Chapter 11: Presenting results and ‘Summary of findings' tables. In: Higgins JPT, Green S, editors, Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 (updated September 2008). The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org.
Schünemann 2008b
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, Guyatt GH. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S, editors, Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 (updated September 2008). The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org.
Smidt 2002a
- Smidt N, Windt DA, Assendelft WJ, Deville WL, Korthals‐De Bos IB, Bouter LM. Corticosteroid injections, physiotherapy, or a wait‐and‐see policy for lateral epicondylitis: a randomised controlled trial. Lancet 2002;359:657‐62. [DOI] [PubMed] [Google Scholar]
Smidt 2002b
- Smidt N, Assendelft WJJ, Windt DAWM, Hay EM, Buchbinder R, Bouter LM. Corticosteroid injections for lateral epicondylitis: a systematic review. Pain 2002;96:23‐40. [DOI] [PubMed] [Google Scholar]
Smidt 2003
- Smidt N, Assendelft W J, Arola H, Malmivaara A, Green S, Buchbinder R, Windt D, Bouter LM. Effectiveness of physiotherapy for lateral epicondylitis: a systematic review. Annals of Medicine 2003;35(1):51‐62. [DOI] [PubMed] [Google Scholar]
Spencer 1953
- Spencer G, Herndon C. Surgical treatment of epicondylitis. The Journal of Bone and Joint Surgery: American volume 1953;35‐A:421‐4. [PubMed] [Google Scholar]
Struijs 2002
- Struijs PAA, Smidt N, Arola H, Dijk CN van, Buchbinder R, Assendelft WJJ. Orthotic devices for tennis elbow. Cochrane Database of Systematic Reviews 2002, Issue 1. [Art. No.: CD001821. DOI: 10.1002/14651858.CD001821] [DOI] [PMC free article] [PubMed] [Google Scholar]
Trethowan 1929
- Trethowan WH. Tennis elbow. British Medical Journal 1929;2:1218. [Google Scholar]
Verhaar 1993
- Verhaar J, Walenkamp G, Kester A, Mameren H, Linden T. Lateral extensor release for tennis elbow. A prospective long‐term follow‐up study. The Journal of Bone and Joint Surgery. American volume 1993;75‐A(7):1034‐43. [DOI] [PubMed] [Google Scholar]
Wilhelm 1996
- Wilhelm A. Tennis elbow: treatment of resistant cases by denervation. Journal of Hand Surgery. British volume 1996;21‐B:523‐33. [DOI] [PubMed] [Google Scholar]
Wittenberg 1992
- Wittenberg RH, Schaal S, Muhr G. Surgical treatment of persistent elbow epicondylitis. Clinical Orthopaedics and Related Research 1992;278:73‐80. [PubMed] [Google Scholar]
Yerger 1985
- Yerger B, Turner T. Percutaneous extensor tenotomy for chronic tennis elbow. Orthopedics 1985;8:1261‐3. [DOI] [PubMed] [Google Scholar]


