Abstract
Background
Hip or knee replacement is a major surgical procedure that can be physically and psychologically stressful for patients. It is hypothesised that education before surgery reduces anxiety and enhances clinically important postoperative outcomes.
Objectives
To determine whether preoperative education in people undergoing total hip replacement or total knee replacement improves postoperative outcomes with respect to pain, function, health‐related quality of life, anxiety, length of hospital stay and the incidence of adverse events (e.g. deep vein thrombosis).
Search methods
We searched the Cochrane Central Register of Controlled Trials (2013, Issue 5), MEDLINE (1966 to May 2013), EMBASE (1980 to May 2013), CINAHL (1982 to May 2013), PsycINFO (1872 to May 2013) and PEDro to July 2010. We handsearched the Australian Journal of Physiotherapy (1954 to 2009) and reviewed the reference lists of included trials and other relevant reviews.
Selection criteria
Randomised or quasi‐randomised trials of preoperative education (verbal, written or audiovisual) delivered by a health professional within six weeks of surgery to people undergoing hip or knee replacement compared with usual care.
Data collection and analysis
Two review authors independently assessed trial quality and extracted data. We analysed dichotomous outcomes using risk ratios. We combined continuous outcomes using mean differences (MD) or standardised mean differences (SMD) with 95% confidence intervals (CI). Where possible, we pooled data using a random‐effects meta‐analysis.
Main results
We included 18 trials (1463 participants) in the review. Thirteen trials involved people undergoing hip replacement, three involved people undergoing knee replacement and two included both people with hip and knee replacements. Only six trials reported using an adequate method of allocation concealment, and only two trials blinded participants. Few trials reported sufficient data to analyse the major outcomes of the review (pain, function, health‐related quality of life, global assessment, postoperative anxiety, total adverse events and re‐operation rate). There did not appear to be an effect of time on any outcome, so we chose to include only the latest time point available per outcome in the review.
In people undergoing hip replacement, preoperative education may not offer additional benefits over usual care. The mean postoperative anxiety score at six weeks with usual care was 32.16 on a 60‐point scale (lower score represents less anxiety) and was 2.28 points lower with preoperative education (95% confidence interval (CI) ‐5.68 to 1.12; 3 RCTs, 264 participants, low‐quality evidence), an absolute risk difference of ‐4% (95% CI ‐10% to 2%). The mean pain score up to three months postoperatively with usual care was 3.1 on a 10‐point scale (lower score represents less pain) and was 0.34 points lower with preoperative education (95% CI ‐0.94 to 0.26; 3 RCTs, 227 participants; low‐quality evidence), an absolute risk difference of ‐3% (95% CI ‐9% to 3%). The mean function score at 3 to 24 months postoperatively with usual care was 18.4 on a 68‐point scale (lower score represents better function) and was 4.84 points lower with preoperative education (95% CI ‐10.23 to 0.66; 4 RCTs, 177 participants; low‐quality evidence), an absolute risk difference of ‐7% (95% CI ‐15% to 1%). The number of people reporting adverse events, such as infection and deep vein thrombosis, did not differ between groups, but the effect estimates are uncertain due to very low quality evidence (23% (17/75) reported events with usual care versus 18% (14/75) with preoperative education; risk ratio (RR) 0.79; 95% CI 0.19 to 3.21; 2 RCTs, 150 participants). Health‐related quality of life, global assessment of treatment success and re‐operation rates were not reported.
In people undergoing knee replacement, preoperative education may not offer additional benefits over usual care. The mean pain score at 12 months postoperatively with usual care was 80 on a 100‐point scale (lower score represents less pain) and was 2 points lower with preoperative education (95% CI ‐3.45 to 7.45; 1 RCT, 109 participants), an absolute risk difference of ‐2% (95% CI ‐4% to 8%). The mean function score at 12 months postoperatively with usual care was 77 on a 100‐point scale (lower score represents better function) and was no different with preoperative education (0; 95% CI ‐5.63 to 5.63; 1 RCT, 109 participants), an absolute risk difference of 0% (95% CI ‐6% to 6%). The mean health‐related quality of life score at 12 months postoperatively with usual care was 41 on a 100‐point scale (lower score represents worse quality of life) and was 3 points lower with preoperative education (95% CI ‐6.38 to 0.38; 1 RCT, 109 participants), an absolute risk difference of ‐3% (95% CI ‐6% to 1%). The number of people reporting adverse events, such as infection and deep vein thrombosis, did not differ between groups (18% (11/60) reported events with usual care versus 13% (7/55) with preoperative education; RR 0.69; 95% CI 0.29 to 1.66; 1 RCT, 115 participants), an absolute risk difference of ‐6% (‐19% to 8%). Global assessment of treatment success, postoperative anxiety and re‐operation rates were not reported.
Authors' conclusions
Although preoperative education is embedded in the consent process, we are unsure if it offers benefits over usual care in terms of reducing anxiety, or in surgical outcomes, such as pain, function and adverse events. Preoperative education may represent a useful adjunct, with low risk of undesirable effects, particularly in certain patients, for example people with depression, anxiety or unrealistic expectations, who may respond well to preoperative education that is stratified according to their physical, psychological and social need.
Keywords: Humans; Length of Stay; Patient Education as Topic; Anxiety; Anxiety/prevention & control; Arthroplasty, Replacement, Hip; Arthroplasty, Replacement, Hip/adverse effects; Arthroplasty, Replacement, Hip/psychology; Arthroplasty, Replacement, Knee; Arthroplasty, Replacement, Knee/adverse effects; Arthroplasty, Replacement, Knee/psychology; Early Ambulation; Postoperative Complications; Postoperative Complications/psychology; Preoperative Care; Preoperative Care/methods; Randomized Controlled Trials as Topic
Plain language summary
Preoperative education for hip or knee replacement
Background ‐ what is preoperative education?
Preoperative education refers to any educational intervention delivered before surgery that aims to improve people's knowledge, health behaviours and health outcomes. The content of preoperative education varies across settings, but frequently comprises discussion of presurgical procedures, the actual steps in the surgical procedure, postoperative care, potential stressful scenarios associated with surgery, potential surgical and non‐surgical complications, postoperative pain management and movements to avoid post‐surgery. Education is often provided by physiotherapists, nurses or members of multidisciplinary teams, including psychologists. The format of education ranges from one‐to‐one verbal communication, patient group sessions, or video or booklet with no verbal communication.
Study characteristics
This summary of a Cochrane review presents what we know from research on whether preoperative education improves outcomes (e.g. pain, function) compared with usual care in people receiving hip or knee replacement. After searching for all relevant studies to May 2013, we included nine new studies since the last review, giving a total of 18 studies (1463 participants); 13 trials included 1074 people (73% of the total) undergoing hip replacement, three involved people undergoing knee replacement and two included both people with hip and knee replacements. Most participants were women (59%) and the mean age of participants was within the range of 58 to 73 years
Key results ‐ what happens to people who have preoperative education compared with people who have usual care for hip replacement
Postoperative anxiety (lower scores mean less anxiety):
People with hip replacement who had preoperative education had postoperative anxiety at six weeks that was 2.28 points lower (ranging from 5.68 points lower to 1.12 points higher) (4% absolute improvement, ranging from 10% improvement to 2% worsening). ‐ People who had usual care for hip replacement rated their postoperative anxiety score as 32.16 points on a scale of 20 to 80 points.
Pain (lower scores mean less pain):
People with hip replacement who had preoperative education had pain at up to three months that was 0.34 points lower (ranging from 0.94 points lower to 0.26 points higher) (3% absolute improvement, ranging from 9% improvement to 3% worsening). ‐ People who had usual care for hip replacement rated their pain score as 3.1 points on a scale of 0 to 10 points.
Function (lower scores mean better function or less disability):
People with hip replacement who had preoperative education had function at 3 to 24 months that was 4.84 points lower (ranging from 10.23 points lower to 0.66 points higher) (7% absolute improvement, ranging from 15% improvement to 1% worsening). ‐ People who had usual care for hip replacement rated their function score as 18.4 points on a scale of 0 to 68 points.
Side effects:
About 5 fewer people out of 100 had adverse events (such as infection or deep vein thrombosis) with preoperative education compared with usual care but this estimate is uncertain. ‐ 18 out of 100 people reported adverse events with preoperative education for hip replacement. ‐ 23 out of 100 people reported adverse events with usual care for hip replacement.
Quality of the evidence
This review shows that in people receiving hip or knee replacement who are provided with preoperative education:
There is low‐quality evidence suggesting that preoperative education may not improve pain, function, health‐related quality of life and postoperative anxiety any more than usual care. Further research is very likely to have an important impact on our confidence in these estimates and is likely to change the estimates.
Health‐related quality of life, global assessment of treatment success and re‐operation rates were not reported.
We are uncertain whether preoperative education results in any fewer adverse events, such as infection or deep vein thrombosis, compared with usual care, due to the very low quality evidence.
Summary of findings
Summary of findings for the main comparison. Preoperative education versus usual care for hip replacement.
| Preoperative education versus usual care for hip replacement | ||||||
| Patient or population: hip replacement Settings: inpatient and outpatient Intervention: preoperative education versus usual care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Preoperative education versus usual care | |||||
| Pain Visual analogue scale. Scale from: 0 to 10 (lower scores indicate less pain). Follow‐up: up to 3 months | The mean pain in the control groups was 3.11 | The mean pain in the intervention groups was 0.34 lower (0.94 lower to 0.26 higher)2 | ‐ | 227 (3 studies) | ⊕⊝⊝⊝ low3,4 | Absolute risk difference ‐3% (95% CI ‐9% to 3%); relative per cent change ‐11% (95% CI ‐30% to 8%). NNTB NA SMD ‐0.17 (95% CI ‐0.47 to 0.13) |
| Function WOMAC function (Likert scale version). Scale from: 0 to 68 (lower scores indicate better function). Follow‐up: from 3 to 24 months | The mean function in the control groups was 18.45 | The mean function in the intervention groups was 4.84 lower (10.23 lower to 0.66 higher)6 | ‐ | 177 (4 studies) | ⊕⊝⊝⊝ low3,4 | Absolute risk difference ‐7% (95% CI ‐15% to 1%); relative per cent change ‐26% (95% CI ‐56% to 4%). NNTB NA SMD ‐0.44 (95% CI ‐0.93 to 0.06). |
| Health‐related quality of life | See comment | See comment | Not estimable | ‐ | See comment | 2 trials reported measuring health‐related quality of life using the Nottingham Health Profile, but neither reported data suitable for analysis. |
| Global assessment of treatment success | See comment | See comment | Not estimable | ‐ | See comment | No trial reported measuring global assessment of treatment success. |
| Postoperative anxiety Spielberger State‐Trait Anxiety Index. Scale from: 20 to 80 (lower scores indicated less anxiety). Follow‐up: mean 6 weeks | The mean postoperative anxiety in the control groups was 32.167 | The mean postoperative anxiety in the intervention groups was 2.28 lower (5.68 lower to 1.12 higher) | ‐ | 264 (3 studies) | ⊕⊕⊝⊝ low4,8 | Absolute risk difference ‐4% (95% CI ‐10% to 2%); relative per cent change ‐7% (95% CI ‐18% to 4%). |
| Total number of serious adverse events (infection, thrombosis, other serious adverse events) | Study population | RR 0.79 (95% CI 0.19 to 3.21) | 150 (2 studies) | ⊕⊝⊝⊝ very low3,4,9 | Absolute risk difference ‐10% fewer adverse events with preoperative education (‐46% fewer to 27% more); relative per cent change ‐21% (95% CI ‐81% to 221%). | |
| 227 per 1000 | 179 per 1000 (43 to 728) | |||||
| Re‐operation rate | See comment | See comment | Not estimable | ‐ | See comment | No trial reported measuring re‐operation rate. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; NA: not available; NNTB: number needed to treat for an additional beneficial outcome; RR: risk ratio; SMD: standardised mean difference; WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Mean visual analogue scale (VAS) (0‐10) pain score at 3 months in the usual care group reported in McGregor 2004 was used as the assumed control group risk.
2 To convert SMD to mean difference (MD), the pooled baseline standard deviation (SD) in McGregor 2004 (SD = 2) was multiplied by the SMDs and 95% CIs to convert values to a 0‐ to 10‐point VAS.
3 In all but 1 randomised controlled trial, allocation concealment was unclear, and no trial blinded participants. 4 95% CIs of the MD are wide. 5 Mean WOMAC function score at 3 months in the usual care group reported in McGregor 2004 was used as the assumed control group risk.
6 To convert SMD to MD, the pooled baseline SD in McGregor 2004 (SD = 11) was multiplied by the SMDs and 95% CIs to convert values to the 0‐ to 68‐point WOMAC function (Likert scale version) score.
7 Control group mean calculated as the mean of Butler 1996 and Doering 2000 (which both reported end of treatment values; Giraudet 2003 was excluded from this estimation as only change scores were reported).
8 Only 1 of the 3 included RCTs had unclear allocation concealment (the remaining 2 RCTs had clear allocation concealment), though no RCT blinded participants.
9 Heterogeneity was very high (I2 = 85%).
Summary of findings 2. Preoperative education versus usual care for knee replacement.
| Preoperative education versus usual care for knee replacement | ||||||
| Patient or population: people with knee replacement Settings: inpatient and outpatient Intervention: preoperative education versus usual care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Preoperative education versus usual care | |||||
| Pain WOMAC pain. Scale from: 0 to 100 (lower scores indicate less pain). Follow‐up: mean 12 months | The mean pain in the control groups was 80 | The mean pain in the intervention groups was 2 higher (3.45 lower to 7.45 higher) | ‐ | 109 (1 study) | ⊕⊕⊝⊝ low1,2 | Absolute risk difference 2% (95% CI ‐4% to 8%); relative per cent change 2.5% (95% CI ‐4% to 9%). |
| Function WOMAC function. Scale from: 0 to 100 (lower scores indicate better function). Follow‐up: mean 12 months | The mean function in the control groups was 77 | The mean function in the intervention groups was 0 higher (5.63 lower to 5.63 higher) | ‐ | 109 (1 study) | ⊕⊕⊝⊝ low1,2 | Absolute risk difference 0% (95% CI ‐6% to 6%); relative per cent change 0% (95% CI ‐7% to 7%). |
| Health‐related quality of life SF‐36 Physical Component Score. Scale from: 0 to 100 (higher scores indicate better quality of life). Follow‐up: mean 12 months | The mean health‐related quality of life in the control groups was 41 | The mean health‐related quality of life in the intervention groups was 3 lower (6.38 lower to 0.38 higher) | ‐ | 109 (1 study) | ⊕⊕⊝⊝ low1,2 | Absolute risk difference ‐3% (95% CI ‐6% to 1%); relative per cent change ‐7% (95% CI ‐16% to 1%). |
| Global assessment of treatment success | See comment | See comment | Not estimable | ‐ | See comment | No trial reported measuring global assessment of treatment success. |
| Postoperative anxiety | See comment | See comment | Not estimable | ‐ | See comment | No trial reported measuring postoperative anxiety. |
| Total number of serious adverse events (infection, thrombosis, other serious adverse events | Study population | RR 0.69 (0.29 to 1.66) | 115 (1 study) | ⊕⊕⊕⊝ low1,2 | Absolute risk difference ‐6% (95% CI ‐19% to 8%); relative per cent change ‐31% (95% CI ‐71% to 66%). | |
| 183 per 1000 | 127 per 1000 (53 to 304) | |||||
| Re‐operation rate | See comment | See comment | Not estimable | ‐ | See comment | No trial reported measuring re‐operation rate. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; SF‐36: 36‐item Short Form; WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Participants were not blind to treatment. 2 95% CIs are wide and include the null value.
Background
Hip replacement and knee replacement are commonly performed surgical procedures. Although global data are not readily available, in the US alone, over 230,000 hip and 540,000 knee replacements were carried out in 2006, up from 124,000 and 209,000, respectively, in 1994 (DeFrances 2008). Other developed economies have witnessed similar increases. In England and Wales, for example, over 89,000 hip and over 93,000 knee procedures were carried out in 2012 (NJR 2013). This trend is likely to continue as populations age and surgical techniques become more commonplace.
Description of the condition
The main indicators for hip or knee replacement are persistent pain or limitation of function (or both) that cannot be managed by conservative treatment alone (Brady 2000). The leading cause of such pain is osteoarthritis but may also include rheumatoid arthritis, trauma, congenital abnormalities, dysplasia and osteochondritic disease. In the absence of treatments that provide a cure for conditions such as osteoarthritis, management is directed primarily towards relieving pain and reducing functional limitation. Joint replacement is one surgical option when medical treatment provides inadequate symptom relief (Creamer 1998).
Description of the intervention
Preoperative education refers to any educational intervention delivered before surgery that aims to improve patients' knowledge, perspectives, health behaviours and health outcomes (Hathaway 1986; Oshodi 2007a; Oshodi 2007b; Shuldham 1999). The content of preoperative education varies across settings, but often comprises discussion of presurgical procedures, the surgical procedure, postoperative care, potential stressful scenarios associated with surgery, potential complications, pain management and movements to avoid post‐surgery (Louw 2013). Education is often provided by physiotherapists, nurses or members of multidisciplinary teams, including psychologists (Johansson 2005; Louw 2013). The format of education ranges from one‐to‐one verbal communication, group sessions, or video or booklet with no verbal communication (Hathaway 1986; Louw 2013; Shuldham 1999).
How the intervention might work
Hip or knee replacement is a major surgical procedure that requires inpatient physiotherapy and outpatient rehabilitation following a stay in hospital (Palmer 1999). These surgical procedures can be stressful, affecting the person both physically and psychologically (Gammon 1996b). Perception of pain and anxiety is often heightened when people feel a lack of control over their situation, and is very common around surgery (Bastian 2002). If a person is unduly anxious, physical recovery and well‐being may be affected, prolonging hospital stay and increasing the cost of care. By ensuring full understanding of the operation and postoperative routines, and promoting physical recovery and psychological well‐being through preparatory information, it is hypothesised that people will be less anxious, have a shorter hospital stay and be better able to cope with postoperative pain (biopsychosocial approach) (Louw 2013; Shuldham 1999). In addition, educating people about postoperative care routines may reduce the incidence of postoperative complications, the most serious of which is pulmonary embolism resulting from deep vein thrombosis (Brady 2000). A key component of preoperative education is to provide the person with a greater understanding of potential complications, such as dislocation in hip replacement, and recognition of complications, such as deep vein thrombosis. It is also important to emphasise the most common post‐surgical side effects (e.g. swelling after knee replacement around the knee and in the ankle).
Why it is important to do this review
Following the publication of the original version of this review (McDonald 2004), plus another systematic review published shortly afterwards (Johansson 2005), the evidence base for preoperative education has grown. The most recent systematic review of preoperative education for hip or knee replacement by Louw 2013 included trials published up to February 2011. The review authors chose not to synthesise the results in a meta‐analysis, though reported that of the 13 included trials, only one had a positive effect on postoperative pain while the remaining trials identified no significant difference between groups on this outcome. Postoperative pain was the only outcome of interest in the Louw 2013 systematic review. Therefore, an up‐to‐date systematic review of the efficacy and safety of preoperative education on other outcomes (e.g. function, health‐related quality of life, adverse events) is necessary.
Objectives
To determine whether preoperative education in people undergoing total hip replacement or total knee replacement improves postoperative outcomes with respect to pain, function, health‐related quality of life, anxiety, length of hospital stay and the incidence of adverse events (e.g. deep vein thrombosis).
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCT) or quasi‐randomised trials comparing educational interventions given preoperatively to people undergoing total hip or total knee replacement surgery.
Types of participants
People undergoing planned total hip or total knee replacement. We originally planned to include only trials of people undergoing surgery for osteoarthritis or rheumatoid arthritis (or where such people accounted for at least 90% of the entire trial population) to avoid clinical heterogeneity. However, few trials reported these data so we included all trials of people undergoing planned hip or knee replacement surgery.
Types of interventions
Any preoperative education regarding the surgery and its postoperative course delivered by a health professional within six weeks of surgery. Education could be given verbally or in any written or audiovisual form, and could include preoperative instruction of postoperative exercise routines.
All comparators were considered, although we excluded trials comparing various methods of delivery of preoperative education in the absence of a control group receiving standard or routine care. We also excluded trials that incorporated some form of postoperative intervention (e.g. use of reminder systems to perform exercises).
Types of outcome measures
Major outcomes
The major outcomes were:
pain measured by visual analogue scales (VAS), numerical or categorical rating scales; and
function. Where trialists reported outcome data for more than one function scale, we extracted data on the scale that was highest on the following list: 1. Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) function; 2. Harris Hip Score; 3. Oxford Hip/Knee Score; 4. 36‐item Short Form (SF‐36) Physical Component Score; 5. Health Assessment Questionnaire; 6. any other function scale;
health‐related quality of life measured using the SF‐36 or Nottingham Health Profile;
global assessment of treatment success as defined by the trialists (e.g. proportion of participants with significant overall improvement);
postoperative anxiety measured using the State‐Trait Anxiety Inventory or Hospital Anxiety and Depression Scale;
number of participants experiencing any serious adverse events (e.g. infection, deep vein thrombosis, other serious adverse events);
re‐operation rate.
Minor outcomes
Other outcomes were:
preoperative anxiety measured using the State‐Trait Anxiety Inventory or Hospital Anxiety and Depression Scale;
length of hospital stay;
mobility (number of days to stand or walk);
range of motion.
Time points
For this update of the review, we did not pre‐specify a primary time point. We extracted data from all time points and performed separate analyses (forest plots not shown) to include all available studies per outcome per time point. There did not appear to be an effect of time on any outcome, so we chose to include only the latest time point available per outcome.
Search methods for identification of studies
Electronic searches
We searched the following electronic databases, unrestricted by date or language, up to 31 May 2013:
Cochrane Central Register of Controlled Trials (Issue 5, 2013);
MEDLINE (Ovid);
EMBASE (Ovid);
CINAHL (EBSCO);
PsycINFO (Ovid).
We also searched the Physiotherapy Evidence Database (PEDro) in July 2010.
We used specific subject headings and additional text words describing the intervention and participants to identify relevant trials. The complete search strategy for the MEDLINE database is provided in Appendix 1. This strategy was adapted for the other electronic databases as appropriate (Appendix 2; Appendix 3; Appendix 4; Appendix 5).
We searched for ongoing randomised trials and protocols of published trials in the clinical trials register maintained by the US National Institute of Health (www.clinicaltrials.gov) and the Clinical Trial Register at the International Clinical Trials Registry Platform of the World Health Organization (www.who.int/ictrp/en/).
Searching other resources
We handsearched the Australian Journal of Physiotherapy (1954 to 2009) and screened the reference lists of retrieved review articles and reports of trials to identify potentially relevant trials.
Data collection and analysis
The description below relates to the methods for data collection and analysis applied during the update of this review in 2013. The previous version of this review (published in 2003) followed methods recommended at that time.
Selection of studies
Two review authors (SM, KB) independently selected the trials to be included in the review. We retrieved all articles selected by at least one of the review authors for closer examination. We resolved disagreements through discussion or by consulting a third review author (JW).
Data extraction and management
Two review authors (SM, KB) independently extracted the following data from the included trials and entered the data in Review Manager 5 (RevMan 2012). The third and fourth review authors (JW, MP) checked the data.
Design, size and location of the trial.
Characteristics of the trial population including age, gender, reason for undergoing surgery and any reported exclusion criteria.
Description of the intervention including the content and format of the preoperative education, the timing and duration of its delivery, and the type of personnel involved.
Methodological characteristics as outlined below in the Assessment of risk of bias in included studies section.
Outcome measures ‐ number of events for dichotomous outcomes, and means and standard deviations for continuous outcomes.
Multiplicity of outcome data is common in RCTs (Page 2013). We used the following a priori decision rules to select which data to extract:
where trialists reported both final values and change from baseline values for the same outcome, we extracted final values;
where trialists reported both unadjusted and adjusted values for the same outcome, we extracted unadjusted values; and
where trialists reported data analysed based on the intention‐to‐treat (ITT) sample and another sample (e.g. per‐protocol, as‐treated), we extracted ITT‐analysed data.
Assessment of risk of bias in included studies
The same two review authors (SM, KB) independently assessed the risk of bias of each included trial and resolved any disagreement through discussion or consultation with the third and fourth review authors (JW, MP). We assessed the following methodological domains, as recommended by The Cochrane Collaboration (Higgins 2011):
sequence generation;
allocation concealment;
blinding of participants, personnel and outcome assessors;
incomplete outcome data;
selective outcome reporting;
other potential threats to validity.
Each of these criteria were explicitly judged as: low risk of bias, high risk of bias or unclear risk of bias (either lack of information or uncertainty over the potential for bias). As part of the updating process, we completed the risk of bias assessment for the nine original included trials.
Measures of treatment effect
As far as possible, the analyses were based on ITT data (outcome data provided for every randomised participant) from the individual trials. For each trial, we present continuous outcome data as point estimates with 95% confidence intervals (CI). We presented the results for continuous outcomes as mean differences (MD) if outcomes included in a meta‐analysis were measured using the same scale. If outcomes were measured using different scales, we pooled data using standardised mean differences (SMD). We presented the results of dichotomous outcomes as risk ratios (RR).
Unit of analysis issues
The unit of analysis was the participant. None of the trials were cluster trials and we did not identify any trials in which participants underwent double knee or double hip replacements.
Dealing with missing data
We requested additional trial details and data from trial authors when the data reported were incomplete.
Assessment of heterogeneity
We assessed clinical heterogeneity by determining whether participants, interventions, comparators, outcome measures and timing of outcome assessment were similar across the included trials. We quantified statistical heterogeneity across trials using the I2 statistic. We interpreted the I2 statistic using the following as an approximate guide: 0% to 40% might not be important heterogeneity; 30% to 60% may represent moderate heterogeneity; 50% to 90% may represent substantial heterogeneity; 75% to 100% may represent considerable heterogeneity (Deeks 2011).
Assessment of reporting biases
To assess publication bias, we would have generated funnel plots if at least 10 trials examining the same treatment comparison were included in a meta‐analysis (Sterne 2011); however, we identified too few trials to undertake this analysis. To assess outcome reporting bias, we planned to compare the outcomes specified in trial protocols with the outcomes reported in the corresponding trial publications. If trial protocols were unavailable, we compared the outcomes reported in the methods and results sections of the trial publications (Dwan 2011). We generated an Outcome Reporting Bias In Trials (ORBIT) Matrix (ctrc.liv.ac.uk/orbit/) using the ORBIT classification system (Kirkham 2010).
Data synthesis
We anticipated substantial clinical heterogeneity between trials, so we used a random‐effects model for all meta‐analyses.
'Summary of findings' table
We collated the main results of the review into 'Summary of findings' tables, which provide key information concerning the quality of evidence and the magnitude and precision of the effect of the interventions (Schünemann 2011a). We included the following outcomes in the 'Summary of findings' tables: pain, function, health‐related quality of life, global assessment of treatment success, postoperative anxiety, total adverse events (infection, thrombosis, other serious adverse events) and re‐operation rate. For all outcomes, data for the latest time point available were included. Outcomes pooled using SMDs were re‐expressed as MDs by multiplying the SMD by a representative control group baseline standard deviation from a trial, using a familiar instrument. The 'Summary of findings' table includes an overall grading of the evidence related to each of the main outcomes, using the GRADE approach (considers study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of a body of evidence for each outcome (Schünemann 2011b).
In addition to the absolute and relative magnitude of effect provided in the 'Summary of findings' table, we have reported the absolute per cent difference, the relative per cent change from baseline, and the number needed‐to‐treat (NNT) for an additional beneficial outcome (NNTB) or for an additional harmful outcome (NNTH) (the NNT was only provided for outcomes that shows a statistically significant difference).
For dichotomous outcomes, we calculated the absolute risk difference using the risk difference statistic in Review Manager 5 (RevMan 2012) and the result expressed as a percentage; the relative percentage change was calculated as the RR ‐ 1 and was expressed as a percentage; and the NNT from the control group event rate and the RR were determined using the Visual Rx NNT calculator (Cates 2008).
For continuous outcomes, we calculated the absolute risk difference as the MD between intervention and control groups in the original measurement units (divided by the scale), expressed as a percentage; the relative difference was calculated as the absolute change (or MD) divided by the baseline mean of the control group from a representative trial. We used the Wells calculator to obtain the NNTB for continuous measures (available at the Cochrane Musculoskeletal Group (CMSG) Editorial office; musculoskeletal.cochrane.org/). The minimal clinically important difference (MCID) for each outcome was determined for input into the calculator. We assumed an MCID of 1.5 points on a 10‐point pain scale (15 points on 100‐point scale), and 10 points on a 100‐point scale for function or disability (Gummesson 2003) for input into the calculator.
Subgroup analysis and investigation of heterogeneity
We did not plan or undertake any subgroup analyses.
Sensitivity analysis
We performed a sensitivity analysis to investigate the robustness of the treatment effect for postoperative pain and postoperative function to allocation concealment by removing the trials that reported inadequate or unclear allocation concealment from the meta‐analysis to see if this changed the overall treatment effect.
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of studies awaiting classification; Characteristics of ongoing studies.
Results of the search
The database searches were revised and re‐run in both June 2012 and May 2013 to cover the period from 2003 to 2013. Following the process of automatic deduplication, the updated search identified 1309 records. From screening the titles and abstracts of the 1309 records, we excluded 1287 records that were clearly not relevant. Of the 22 potentially eligible full‐text reports assessed, we identified nine trials that met our inclusion criteria (see flow chart in Figure 1). Nine excluded trials are listed in the Characteristics of excluded studies table. Three trials are awaiting assessment (Eschalier 2012; Huang 2012; Wilson 2012), and one trial is ongoing (Riddle 2012). The nine new included trials (Beaupre 2004; Giraudet 2003; Gocen 2004; Johansson 2007; McDonald 2004; McGregor 2004; Siggeirsdottir 2005; Sjöling 2003; Vukomanović 2008) were added to the existing nine trials from the previous version (Butler 1996; Clode‐Baker 1997; Cooil 1997; Crowe 2003; Daltroy 1998; Doering 2000; Lilja 1998; Santavirta 1994; Wijgman 1994). The earliest trials were published in 1994 and the most recent in 2008. All trials were published in English with the exception of Wijgman 1994, which was published in Dutch.
1.
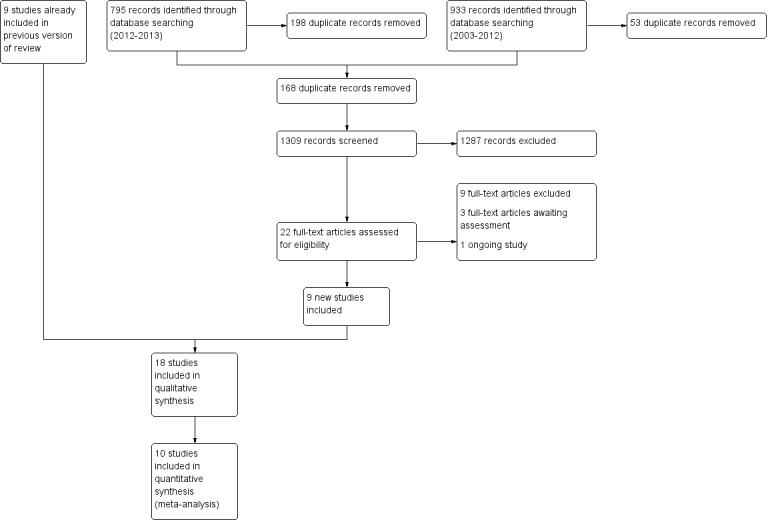
Trial flow diagram for the review update (literature searches from 2003 to 2013).
Included studies
See Characteristics of included studies table.
Design
Seventeen of the included trials were randomised and one was quasi‐randomised (Sjöling 2003). Sixteen were two‐arm trials, one was a three‐arm trial (McDonald 2004), and one was a four‐arm trial (Daltroy 1998). One trial used stratification to produce balanced groups according to age (Daltroy 1998), and another used gender, age and socioeconomic status (Cooil 1997).
Setting
Trials were set in hospitals and were conducted in North America or Europe; five each in Scandinavia and continental Europe, three each in Canada and the UK, and two in the USA. With the exception of Siggeirsdottir 2005, trials were conducted at a single site.
Participants
Thirteen trials involved people undergoing hip replacement (Butler 1996; Clode‐Baker 1997; Cooil 1997; Doering 2000; Giraudet 2003; Gocen 2004; Johansson 2007; Lilja 1998; McGregor 2004; Santavirta 1994; Siggeirsdottir 2005; Vukomanović 2008; Wijgman 1994); three involved people undergoing knee replacement (Beaupre 2004; McDonald 2004; Sjöling 2003); and two included people with both hip and knee replacements (Crowe 2003; Daltroy 1998). Overall, the 18 included trials involved 1463 participants (range 26 to 222). The number of people undergoing hip replacement was 1074 (73% of the total). Most participants were women (59%) and the mean age of participants was within the range of 58 to 73 years, with the exception of Gocen 2004.
The inclusion and exclusion criteria varied considerably between the trials. Half of the trials reported age as an inclusion criterion, with none of these explicitly excluding older people. The most commonly stated exclusion criteria were previous hip or knee replacement surgery and difficulties in communicating (reading, writing and language). The patient profile differed most markedly in Crowe 2003 since the inclusion criteria deliberately targeted people with poor functioning, limited social support and existing co‐morbidities.
Interventions
The nature, content and timing of the preoperative education varied considerably between trials. In four trials, participants received written information in addition to one or more education sessions before admission to hospital (Giraudet 2003; Johansson 2007; McGregor 2004; Siggeirsdottir 2005). Written information alone was provided before admission in one trial (Butler 1996). Santavirta 1994 combined the provision of pre‐admission written information with a teaching session on admission that was planned according to the needs of each participant. Sjöling 2003 also provided a teaching session on admission, though in this trial the written information was distributed at the time of the education session rather than before.
Five trials included an audiovisual component. Clode‐Baker 1997 sent written information, a video and plastic model bones to participants before admission; Crowe 2003 combined a video presentation with an individually tailored programme of education before admission; McDonald 2004 showed either one of two films to participants in two of the intervention groups after the standard preoperative class; Daltroy 1998 and Doering 2000 showed participants a video after admission in the presence of the investigator. In six trials, information was provided in teaching sessions delivered by physiotherapists or nurses; three of these took place before admission (Beaupre 2004; Gocen 2004; Vukomanović 2008), and three after admission (Cooil 1997; Lilja 1998; Wijgman 1994).
All trials provided some form of standardised information for participants, consisting mainly of printed materials, thus ensuring all participants (including people in the control group) received some information before surgery. Detailed descriptions of the content and methods used to deliver the education interventions are given in Table 3.
1. Description of the education intervention.
| Trial ID | Content |
| Beaupre 2004 | Participants in the treatment group underwent a 4‐week exercise/education programme before surgery. The education programme consisted of instruction regarding crutch walking, bed mobility and the postoperative range of motion routine. The exercise programme was designed to improve knee mobility and strength using simple exercises with progressive resistance. The subjects were asked to attend the treatment programme three times a week for four weeks. |
| Butler 1996 | An 18‐page teaching booklet 'Total hip replacement: a patient guide' was sent to participants at home. The booklet was developed by a multidisciplinary team and contained: information on the anatomy of a normal and diseased hip; total hip prosthesis; exercises to practice before admission; what to expect in hospital; precautions following surgery and planning for discharge. The booklet had a readability age of Grade 6 to 7 with 22 drawings and photographs. |
| Clode‐Baker 1997 | A 20‐minute video, booklet and set of plastic models were sent to participants at home. The video followed the progress of a person undergoing hip replacement surgery, from difficulties encountered at home through to the hospital stay, postoperative recovery and exercises. The booklet addressed similar issues and included advice from previous participants. The booklet described arthritis and backed up information presented in the video. The life‐size plastic model bones demonstrated changes of the total hip replacement by comparison with a normal hip joint, osteoarthritis and an implanted total hip replacement prosthesis. |
| Cooil 1997 | An information sheet that was already in clinical use was made available at the participants' bedside. The sheet contained instructions on the postoperative protocol, exercises and advice on beneficial and harmful postoperative activities. In addition, a verbal explanation of the sheet's contents was given, and the exercises and activities were taught through demonstration and practiced under supervision. |
| Crowe 2003 | A preoperative education package consisting of a 50‐minute video and a booklet giving information on length of hospital stay, discharge criteria, respite care and diet was provided to participants the first time they visited the clinic following randomisation. The video focused on the participant's responsibility during the postoperative phase and use of equipment. Some participants were given a tour of the hospital unit, demonstration of equipment, dietician counselling and social work input. All participants received extensive individualised counselling from an occupational therapist on all aspects of optimising function and independence postoperatively, including home assessments, and were provided with a telephone contact for additional information. A physical conditioning programme was available to participants to improve strength and endurance and facilitate postoperative mobility. Participants also received the same standard preoperative clinic visit as the control participants. |
| Daltroy 1998 | A 12‐minute audiotape slide programme was presented by a research assistant at the bedside the day before surgery. The audiotape oriented the participant to the hospital, staff, surgery and rehabilitation. Participants were told of various stressful aspects of their hospital stay, and reassured that these were normal. The tape complemented the standard preoperative information. The comparison group received relaxation training consisting of oral and written instructions and an 18‐minute audiotape. |
| Doering 2000 | A 12‐minute video shown in hospital preoperatively in the presence of the investigator. The video followed a person with osteoarthritis undergoing hip replacement. Filmed from the person's perspective, the video showed what to expect from hospital, the procedure, the recovery and rehabilitation. It included original dialogue, a narrator giving procedural information and interviews with the person. |
| Giraudet 2003 | Participants in the multidisciplinary collective information group (trial group) received verbal information and a standard information leaflet. They also attended an education session 2 to 6 weeks before surgery, where a multidisciplinary team including a surgeon and an anaesthetist presented a standardised education programme. The team discussed the intervention and answered the questions of patients and their significant others. The control group received only the usual verbal information from the surgeon and the anaesthetist and the standard information leaflet. |
| Gocen 2004 | Participants in the trial group received preoperative physiotherapy to strengthen and improve range of motion of the hip, beginning from eight weeks before the operation. These participants also received an educational programme that included advice on movements that should be avoided, use of assistance devices, posture, lifting and carrying, washing and bathing. The control group received no preoperative physiotherapy or educational programme. |
| Johansson 2007 | Standard written education materials plus education using the concept map method. The education was delivered by two specially trained nurses two weeks before admission and lasted approximately 30 to 60 minutes. The concept map method involved counselling in relation to biophysiological, functional, experiential, ethical, social and financial issues about pre and postoperative care. |
| Lilja 1998 | In addition to being informed by ward nurses about preoperative routines and what to expect before and after the operation, participants spent 30 minutes with an anaesthetic nurse. The information provided by the nurse covered the importance of preoperative preparation and patient participation in recovery, the operating theatre and mobilisation following surgery. |
| McDonald 2004 | Participants were randomly assigned to one of three groups. In the preoperative period, the communication group (treatment group) viewed a 4‐minute pain communication film as well as a 10‐minute pain management film. Comparison group 1 viewed only the pain management film, and comparison group 2 received standard care only. Handouts reinforcing the main content of both films were distributed to the communication group. Comparison group 1 received only the pain management handout. |
| McGregor 2004 | Participants in the treatment group received a preoperative hip class 2 to 4 weeks before surgery and an information booklet. The information booklet documented information on the surgery, rehabilitation stages including exercise regimens, and answers to commonly asked questions. The preoperative class enforced the booklet and ensured that all participants could do the exercises, understood how to use walking aids postoperatively, and could adapt their homes for the recovery period. The control group received the standard preoperative treatment, which included a description of the surgery and its risks and approximations on length of hospital stay. |
| Santavirta 1994 | Before admission, participants received an 18‐page guide on hip replacement surgery and postoperative rehabilitation. They also received a 20‐ to 60‐minute teaching session by the investigator, which was planned according to each participant's situation. Elements covered included safe walking, active exercises, wound care, temperature taking, rehabilitation and discharge planning. |
| Siggeirsdottir 2005 | Participants in the trial group participated in a preoperative education and training programme, given by a physiotherapist or an occupational therapist (or both), about one month before the planned operation. The programme covered postoperative rehabilitation, exercises and postoperative assistive devices. Participants also received an illustrated brochure containing information on how to move and exercise postoperatively. When a trial group participant was discharged, a physiotherapist or occupational therapist could accompany the person home and return for follow‐up home visits if this was considered necessary. Control group participants were treated according to the clinical procedures already in use and were discharged when rehabilitated, or could be transferred to another rehabilitation facility. |
| Sjöling 2003 | Participants received specific information (verbally and in a leaflet) which emphasised the person's own role in pain management by trying to improve knowledge in areas important for their well‐being. The specific information covered issues such as people taking an active role in their treatment; postoperative pain and pain management; and the importance of physiotherapy. |
| Vukomanović 2008 | Participants received short‐term intensive preoperative preparation consisting of education and elements of physiotherapy. They were informed about the operation, caution measures and rehabilitation following the operation through conversation with the clinician and a brochure. They were instructed by a physiotherapist to perform exercises and basic activities. |
| Wijgman 1994 | Participants received preoperative instructions for 30 minutes in groups of 4 to 6 delivered by two physiotherapists. They also received preoperative exercise therapy including muscle setting exercises. |
The nature of the intervention and the patient profile differed most markedly in Crowe 2003. In this trial, various interventions tailored to individual needs were offered to participants in addition to educational material. In contrast to all other trials, the inclusion criteria deliberately targeted people with poor functioning, limited social support and existing co‐morbidities. Only one other trial incorporated tailoring the intervention (a teaching session) to each participant's specific situation (Santavirta 1994).
Outcomes
The outcomes measured varied considerably (see Table 4), though many trials only partially reported results (e.g. reported the difference between groups as being non‐significant, though did not report the summary statistics required for meta‐analysis). Of the primary outcomes, 11 trials reported measuring pain, but only five trials reported data in a format suitable for analysis (Beaupre 2004; Doering 2000; Giraudet 2003; McDonald 2004; McGregor 2004), whereas five trials measured and fully reported data for function (Beaupre 2004; Gocen 2004; McGregor 2004; Siggeirsdottir 2005; Vukomanović 2008), and five trials measured adverse events, of which three fully reported outcome data (Beaupre 2004; Giraudet 2003; Siggeirsdottir 2005). The most common fully reported outcomes were length of hospital stay (eight trials: Beaupre 2004; Butler 1996; Crowe 2003; Doering 2000; Giraudet 2003; Siggeirsdottir 2005; Vukomanović 2008; Wijgman 1994), and mobility (days to stand or walk) (six trials: Crowe 2003; Doering 2000; Giraudet 2003; Gocen 2004; Vukomanović 2008; Wijgman 1994).
2. Outcome Reporting Bias In Trials (ORBIT) outcome matrix.
| Study ID | Major outcomes | Minor outcomes | Other outcomes | |||||||||
| Pain | Function | HRQoL | Global assessment | Postop anxiety | Adverse events | Re‐operation rate | Preop anxiety | LOS | Mobility | ROM | Knowledge (recall) | |
| Beaupre 2004 | Full | Full | Full | Unclear | Unclear | Full | Unclear | Unclear | Full | Unclear | Full | Unclear |
| Butler 1996 | Unclear | Unclear | Unclear | Unclear | Full | Unclear | Unclear | Full | Full | Unclear | Unclear | Unclear |
| Clode‐Baker 1997 | Partial | Unclear | Partial | Unclear | Partial | Unclear | Unclear | Unclear | Partial | Partial | Unclear | Unclear |
| Cooil 1997 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Partial |
| Crowe 2003 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Full | Full | Full | Unclear | Unclear |
| Daltroy 1998 | Partial | Unclear | Unclear | Unclear | Partial | Unclear | Unclear | Unclear | Partial | Unclear | Unclear | Unclear |
| Doering 2000 | Full | Unclear | Unclear | Unclear | Full | Unclear | Unclear | Full | Full | Full | Unclear | Unclear |
| Giraudet 2003 | Full | Unclear | Unclear | Unclear | Full | Full | Unclear | Full | Full | Full | Unclear | Unclear |
| Gocen 2004 | Partial | Full | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Partial | Full | Full | Unclear |
| Johansson 2007 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Partial | Unclear | Unclear | Partial |
| Lilja 1998 | Partial | Unclear | Unclear | Unclear | Partial | Unclear | Unclear | Partial | Unclear | Unclear | Unclear | Unclear |
| McDonald 2004 | Full | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| McGregor 2004 | Full | Full | Unclear | Unclear | Unclear | Partial | Unclear | Unclear | Partial | Unclear | Unclear | Unclear |
| Santavirta 1994 | Unclear | Unclear | Unclear | Unclear | Unclear | Partial | Unclear | Unclear | Unclear | Unclear | Unclear | Partial |
| Siggeirsdottir 2005 | Unclear | Full | Partial | Unclear | Unclear | Full | Unclear | Unclear | Full | Unclear | Unclear | Unclear |
| Sjöling 2003 | Partial | Unclear | Unclear | Unclear | Partial | Unclear | Unclear | Unclear | Partial | Unclear | Unclear | Unclear |
| Vukomanović 2008 | Partial | Full | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Full | Full | Full | Unclear |
| Wijgman 1994 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Full | Full | Unclear | Unclear |
HRQoL: health‐related quality of life; LOS: length of hospital stay; preop: preoperative; postop: postoperative; ROM: range of motion.
'Full' = sufficient data for inclusion in a meta‐analysis were reported (e.g. mean, standard deviation, and sample size per group for continuous outcomes).
'Partial' = insufficient data for inclusion in a meta‐analysis were reported (e.g. means only, with no measures of variation).
'Unclear' = unclear whether the outcome was measured or not (as a trial protocol was unavailable).
Excluded studies
We excluded trials for the following reasons: information was not specific to hip or knee surgery (Bondy 1999; Mikulaninec 1987); trial was not randomised (Hough 1991; Roach 1995); participants received a combined pre‐ and postoperative intervention (Gammon 1996a; Pour 2007; Ródenas‐Martínez 2008; Wong 1985); trial investigated the effect of preoperative depression on postoperative recovery and was not a randomised trial of preoperative education (Brull 2002); and the trial did not investigate postoperative outcomes (Haslam 2001) (see Characteristics of excluded studies table).
Risk of bias in included studies
See Characteristics of included studies table. The results of the risk of bias assessment are also presented graphically in Figure 2 and Figure 3.
2.
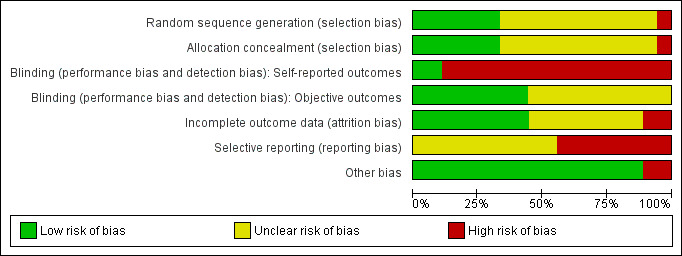
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included trials.
3.
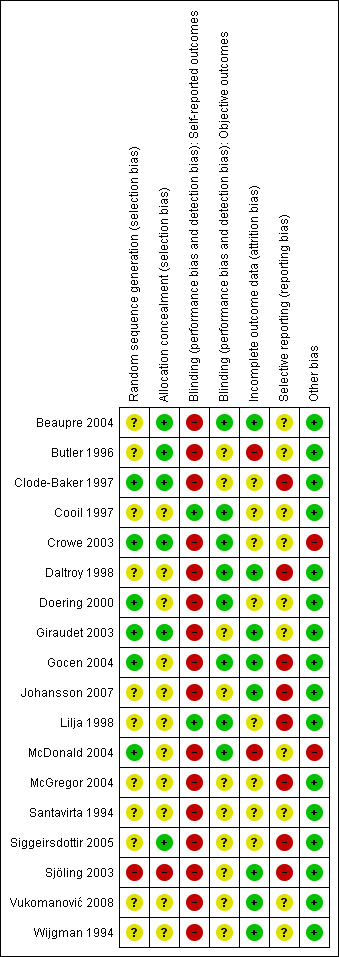
Allocation
We assessed three trials as low risk of selection bias having both adequate random sequence generation and allocation concealment (Clode‐Baker 1997; Crowe 2003; Giraudet 2003). We assessed three other trials as low risk of selection bias on the basis of adequate allocation concealment even though the method of random sequence generation was not specified (Beaupre 2004; Butler 1996; Siggeirsdottir 2005). We assessed risk of selection bias as unclear in eight trials reported to be randomised since neither the methods of random sequence generation nor treatment allocation were specified (Cooil 1997; Daltroy 1998; Johansson 2007; Lilja 1998; McGregor 2004; Santavirta 1994; Vukomanović 2008; Wijgman 1994). We assessed a further three trials as unclear risk of selection bias despite reporting an adequate method for the random sequence generation because the method of treatment allocation was either not specified (Doering 2000; McDonald 2004), or unclear (Gocen 2004). We assessed one trial as high risk of selection bias as participants were allocated to groups on an alternate basis (Sjöling 2003).
Blinding
Blinding was considered by type of outcome (self reported and objective). For self reported outcomes, two trials attempted to blind participants by not informing them of the aim and design of the trial (Lilja 1998), and by obscuring the purpose of the trial during the explanation to participants (Cooil 1997). We rated the remaining 16 trials at high risk of bias because blinding of participants was either not attempted or not described (but since blinding is difficult to achieve with an educational intervention, it was likely not to have been attempted).
Blinding of outcome assessors for the objective outcomes was attempted in eight trials (Beaupre 2004; Cooil 1997; Crowe 2003; Daltroy 1998; Doering 2000; Gocen 2004; Lilja 1998; McDonald 2004), though measures of success of blinding were not provided. It is feasible that participants may have accidentally unblinded assessors by describing a facet of their preoperative care. The remaining 10 trials did not provide any details about the blinding of objective outcomes so we rated them as having unclear risk of bias on this domain.
Incomplete outcome data
Incomplete outcome data were not particularly well accounted for. We assessed eight trials as low risk of bias (Beaupre 2004; Daltroy 1998; Giraudet 2003; Gocen 2004; Johansson 2007; Sjöling 2003; Vukomanović 2008; Wijgman 1994). Of these, Beaupre 2004 explained the distribution of, and reasons for, incomplete data and used statistical strategies to compensate for missing values. The remaining seven trials described drop‐outs adequately without correcting statistically for missing values. However, we considered the drop‐outs were unlikely to have affected the results because the missing values were small and the outcomes were continuous. We rated eight trials as unclear in their reporting of incomplete data either because the amount or reasons for missing data were not explained (Clode‐Baker 1997; Cooil 1997; Crowe 2003; Doering 2000; Lilja 1998; McGregor 2004; Santavirta 1994; Siggeirsdottir 2005). We assessed two trials as high risk of bias: Butler 1996 had unexplained missing values in all data (ranging from 2 to 12 participants missing); and McDonald 2004 removed some data post‐hoc due to author interpretation.
Selective reporting
We rated eight trials at high risk of selective reporting bias because the data necessary to include the trial in a meta‐analysis of at least one outcome (e.g. standard deviations) were not reported (Clode‐Baker 1997; Daltroy 1998; Gocen 2004; Johansson 2007; Lilja 1998; McGregor 2004; Siggeirsdottir 2005; Sjöling 2003). We rated all remaining trials as unclear risk of bias because trial protocols were unavailable, making it impossible to determine whether additional outcomes were measured but not reported based on the results.
Other potential sources of bias
We rated two trials at high risk of other bias. The control group in Crowe 2003 had worse function at baseline, and this baseline imbalance may have biased the results to favour the intervention group. McDonald 2004 reported changing the protocol in order to minimise confounding, but this was done after the initial data analysis (i.e. result‐driven modification).
Effects of interventions
Eleven trials presented data in a format suitable for analysis (i.e. number of participants with events or means and standard deviations) (Beaupre 2004; Butler 1996; Crowe 2003; Doering 2000; Giraudet 2003; Gocen 2004; McDonald 2004; McGregor 2004; Siggeirsdottir 2005; Vukomanović 2008; Wijgman 1994). The data from three other trials were reported as medians and ranges and are reported in an additional table (Clode‐Baker 1997; Johansson 2007; Sjöling 2003) (Table 5). The remaining four trials either did not measure any outcomes of interest to the review or partially reported outcome data (Cooil 1997; Daltroy 1998; Lilja 1998; Santavirta 1994). Despite attempts to contact all authors, we were only able to secure additional data for three trials (Butler 1996; Crowe 2003; Doering 2000). Although the trials differed somewhat in the participant characteristics and intervention components, we judged that there was sufficient clinical homogeneity to pool the results using random‐effects meta‐analyses.
3. Results of included studies with data not appropriate for meta‐analysis.
| Trial ID | Outcome | Results |
| Clode‐Baker 1997 | Preoperative anxiety (Hospital Anxiety and Depression Scale 0 to 21) | Intervention: median 6 (range 1 to 17). Control: median 8 (range 2 to 21). No statistically significant difference between the 2 groups. |
| Clode‐Baker 1997 | Postoperative anxiety (Hospital Anxiety and Depression Scale 0 to 21) | Intervention: median 5 (range 1 to 15). Control: median 5 (range 1 to 15). No statistically significant difference between the 2 groups. |
| Clode‐Baker 1997 | Nottingham Health Profile (postoperative) (0 to 38) | Intervention: median 10 (range 1 to 29). Control: median 9 (range 0 to 19). No statistically significant difference between the 2 groups. |
| Clode‐Baker 1997 | Days to mobilisation | Intervention: median 2 (range 1 to 6). Control: median 2 (range 2 to 3). No statistically significant difference between the 2 groups. |
| Clode‐Baker 1997 | Length of hospital stay | Intervention: median 12 (range 7 to 21). Control: median 12 (range 7 to 23). No statistically significant difference between the 2 groups. |
| Johansson 2007 | Length of hospital stay | Intervention: mean 6.78. Control: mean 8.18. Not statistically significant. |
| Sjöling 2003 | VAS pain postoperative day 1 | Intervention: median 4 (IQR 3.3 to 5.7; range 2 to 9.3). Control: median 4.3 (IQR 2.2 to 6; range 0 to 8.3). No statistically significant difference between the 2 groups. |
| Sjöling 2003 | VAS pain postoperative day 2 | Intervention: median 3.8 (IQR 2.6 to 5.1; range 1 to 9.3). Control: median 4.0 (IQR 3.3 to 5; range 0 to 7.3). No statistically significant difference between the 2 groups. |
| Sjöling 2003 | VAS pain postoperative day 3 | Intervention: median 3.0 (IQR 1.7 to 3.7; range 0 to 7.7). Control: median 2.3 (IQR 1.7 to 4.2; range 0 to 8.3). No statistically significant difference between the 2 groups. |
| Vukomanović 2008 | VAS pain at discharge | Intervention: mean 3.95, SD 13.08, median 0 (range 0 to 58). Control: mean 6.2, SD 14.95, median 0 (range 0 to 50). No statistically significant difference between the 2 groups. |
IQR: interquartile range; VAS: visual analogue scale.
Preoperative education for hip replacement versus usual care
See Table 1.
Pain
See Analysis 1.1. Three trials measured useable outcome data for postoperative pain using a visual analogue scale (VAS) at at least one time point (Doering 2000; Giraudet 2003; McGregor 2004). At up to three months postoperatively, pain was lower in participants receiving preoperative education, though the difference was not statistically significant (3 trials, 227 participants, SMD ‐0.17; 95% CI ‐0.47 to 0.13; I2 = 20%; this is equivalent to a MD of ‐0.34 points (95% CI ‐0.94 to 0.26) on a 10‐point scale). Clode‐Baker 1997 measured pain using a 6‐point ordinal scale and only reported that there was no statistically significant difference between groups on this outcome at the end of the first postoperative week. Daltroy 1998 only reported that pain measured on a 1 to 5 scale was not statistically significantly different between groups four days postoperatively. Gocen 2004 reported measuring pain but reported no results in the publication. Lilja 1998 only reported mean scores for VAS pain and identified no statistically significant difference between groups on day one, two and three postoperatively. Sjöling 2003 reported median (interquartile range (IQR)) data for VAS pain and identified no statistically significant difference between groups on postoperative day one, two and three (see Table 5). Vukomanović 2008 reported skewed data for VAS pain and identified no statistically significant difference between groups at hospital discharge (see Table 5).
1.1. Analysis.
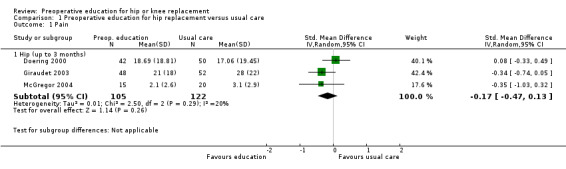
Comparison 1 Preoperative education for hip replacement versus usual care, Outcome 1 Pain.
Function
See Analysis 1.2. Four trials measured postoperative function using either the WOMAC function, Oxford Hip Score, or Harris Hip Score (Gocen 2004; McGregor 2004; Siggeirsdottir 2005; Vukomanović 2008). Participants receiving preoperative education had better function scores compared with people receiving usual care at 3 to 24 months postoperatively (4 trials, 177 participants, SMD ‐0.44; 95% CI ‐0.93 to 0.06; I2 = 61%; this is equivalent to a MD of ‐4.84 points (95% CI ‐10.23 to 0.66) on the WOMAC Likert (0 to 68) scale). However, participants were not blind to treatment in any of these trials, so self reported function may have been overestimated by participants receiving preoperative education. No other hip replacement trials reported measuring function.
1.2. Analysis.
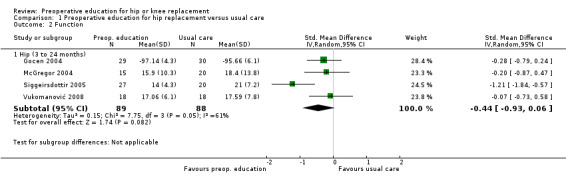
Comparison 1 Preoperative education for hip replacement versus usual care, Outcome 2 Function.
Health‐related quality of life
Two trials reported measuring health‐related quality of life (Clode‐Baker 1997; Siggeirsdottir 2005), but neither presented outcome data in a format suitable for inclusion in a meta‐analysis. Clode‐Baker 1997 reported median (IQR) data for the Nottingham Health Profile and identified no statistically significant difference between groups on this outcome (see Table 5). Siggeirsdottir 2005 also used the Nottingham Health Profile and reported that the usual care group had lower scores on this outcome, but did not report the statistical significance of the difference.
Global assessment of treatment success
Global assessment of treatment success was not assessed in any of the trials included in the review.
Postoperative anxiety
See Analysis 1.3. Three trials measured postoperative anxiety using the Spielberger State‐Trait Anxiety Index at different time periods (Butler 1996; Doering 2000; Giraudet 2003). Anxiety was 2.28 points lower (on the 60‐point scale) at up to six weeks postoperatively in participants receiving preoperative education, though this difference was not statistically significant (3 trials, 264 participants, MD ‐2.28; 95% CI ‐5.68 to 1.12; I2 = 22%). Clode‐Baker 1997 reported median (IQR) data for the Hospital Anxiety and Depression Scale postoperatively and identified no statistically significant difference between groups on this outcome (see Table 5). Daltroy 1998 only reported that anxiety measured on a 1 to 4 scale was not statistically significantly different between groups four days postoperatively. Lilja 1998 only reported mean scores for the Hospital Anxiety and Depression Scale and identified no statistically significant difference between groups on day one, two and three postoperatively.
1.3. Analysis.
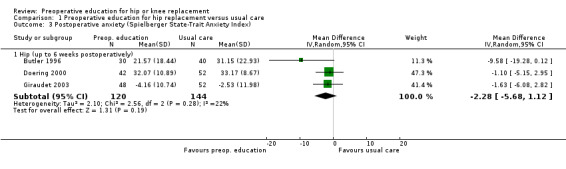
Comparison 1 Preoperative education for hip replacement versus usual care, Outcome 3 Postoperative anxiety (Spielberger State‐Trait Anxiety Index).
Adverse events
See Analysis 1.4. Four trials reported measuring adverse events (Giraudet 2003; McGregor 2004; Santavirta 1994; Siggeirsdottir 2005), but only two reported sufficient data to include in a meta‐analysis (Giraudet 2003; Siggeirsdottir 2005). The risk of experiencing any serious postoperative complication was reduced by 21% in participants receiving preoperative education, though this effect was not statistically significant (2 trials, 31 participants, RR 0.79; 95% CI 0.19 to 3.21; I2 = 78%). McGregor 2004 reported that some participants reported minor postoperative complications and that these were similar in number between groups, and Santavirta 1994 reported that there was no statistical difference in the number of early complications. No trial referred specifically to incidence of infection or deep vein thrombosis.
1.4. Analysis.
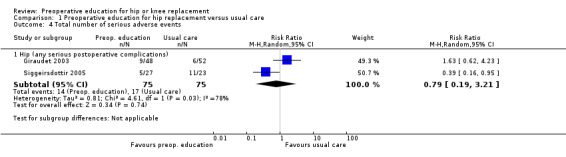
Comparison 1 Preoperative education for hip replacement versus usual care, Outcome 4 Total number of serious adverse events.
Re‐operation rate
Re‐operation rate was not assessed in any of the trials included in the review.
Preoperative anxiety
See Analysis 1.5. Four trials measured preoperative anxiety using the Spielberger State‐Trait Anxiety Index (range of scores 20 to 80) (Butler 1996; Crowe 2003; Doering 2000; Giraudet 2003). Preoperative education resulted in preoperative anxiety that was 5.1 points lower (on the 60‐point scale) compared with usual care (4 trials, 333 participants, MD ‐5.10; 95% CI ‐7.17 to ‐3.03; I2 = 4%). However, participants were not blind to treatment in any of these trials, so self reported anxiety may have been overestimated by participants receiving preoperative education. Clode‐Baker 1997 reported median (IQR) data for the Hospital Anxiety and Depression Scale preoperatively and identified no statistically significant difference between groups on this outcome (see Table 5). Lilja 1998 only reported mean scores for the Hospital Anxiety and Depression Scale and identified no statistically significant difference between groups preoperatively. Sjöling 2003 only reported that there was no statistically significant difference between groups in state or trait anxiety preoperatively.
1.5. Analysis.
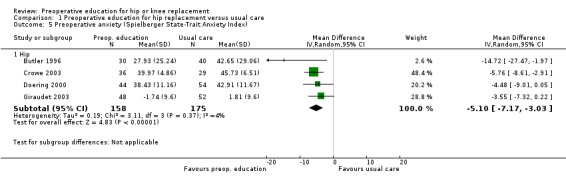
Comparison 1 Preoperative education for hip replacement versus usual care, Outcome 5 Preoperative anxiety (Spielberger State‐Trait Anxiety Index).
Length of hospital stay
See Analysis 1.6. Seven trials measured length of hospital stay (days) (Butler 1996; Crowe 2003; Doering 2000; Giraudet 2003; Siggeirsdottir 2005; Vukomanović 2008; Wijgman 1994). Preoperative education resulted in a non‐statistically significant reduction in length of hospital stay by less than one day (7 trials, 487 participants, MD ‐0.79; 95% CI ‐1.96 to 0.37; I2 = 82%). Note that the high statistical heterogeneity suggests that this result should be interpreted with caution. Clode‐Baker 1997 reported median (IQR) data and Johansson 2007 reported mean values only, and both identified no statistically significant difference between groups on this outcome (see Table 5). Daltroy 1998; Gocen 2004; and Sjöling 2003 only reported that there were no statistically significant differences between groups in length of hospital stay.
1.6. Analysis.
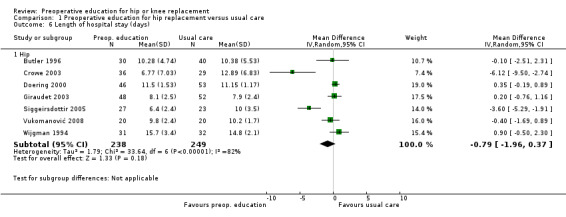
Comparison 1 Preoperative education for hip replacement versus usual care, Outcome 6 Length of hospital stay (days).
Mobility
See Analysis 1.7. Six trials reported data on mobility (Crowe 2003; Doering 2000; Giraudet 2003; Gocen 2004; Vukomanović 2008; Wijgman 1994). Preoperative education did not result in a statistically significant reduction in days to stand or walk (6 trials, 417 participants, MD ‐0.12; 95% CI ‐0.30 to 0.07; I2 = 47%). Clode‐Baker 1997 reported median (IQR) data and identified no difference between groups on this outcome (see Table 5).
1.7. Analysis.
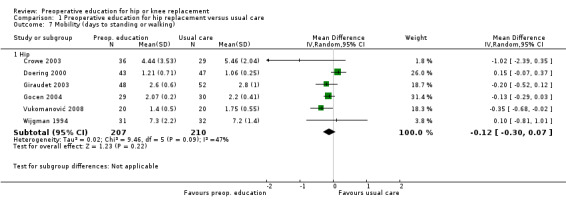
Comparison 1 Preoperative education for hip replacement versus usual care, Outcome 7 Mobility (days to standing or walking).
Range of motion
See Analysis 1.8. Two trials assessed various measures of hip range of motion (degrees) at up to six weeks postoperatively (Gocen 2004; Vukomanović 2008). None of the differences between groups on any measure of range of motion were clinically or statistically significant (hip abduction: 2 trials, 95 participants, MD ‐1.09; 95% CI ‐5.35 to 3.17; I2 = 0%; flexion of the hip with flexed knee: 1 trial, 36 participants, MD 0.75; 95% CI ‐7.67 to 9.17; flexion of the hip with extended knee: 1 trial, 36 participants, MD ‐0.25; 95% CI ‐9.17 to 8.67).
1.8. Analysis.
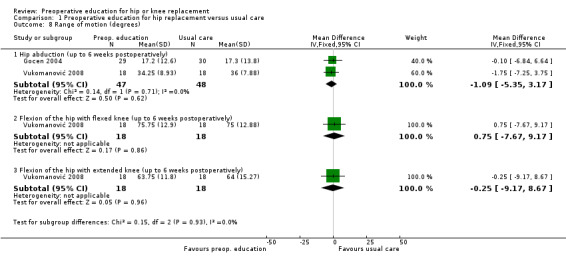
Comparison 1 Preoperative education for hip replacement versus usual care, Outcome 8 Range of motion (degrees).
Sensitivity analyses
See Analysis 1.9 and Analysis 1.10. For the outcome of pain, after removing trials with inadequate or unclear allocation concealment, only one of the trials remained (Giraudet 2003). Similar to the main analysis, there were no statistically significant differences in pain at up to six weeks postoperatively (1 trial, 100 participants, MD ‐7.00; 95% CI ‐14.85 to 0.85). For the outcome of function, one of four trials with adequate allocation concealment remained (Siggeirsdottir 2005). This trial found that function was 7 points lower on the Oxford Hip Scale (0‐60 scale) in the group receiving preoperative education at six months postoperatively (1 trial, 47 participants, MD ‐7.00; 95% CI ‐10.55 to ‐3.45); however, non‐blinded participants receiving preoperative education may have overestimated their self reported function.
1.9. Analysis.
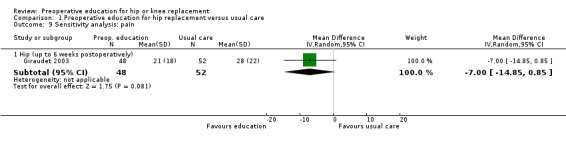
Comparison 1 Preoperative education for hip replacement versus usual care, Outcome 9 Sensitivity analysis: pain.
1.10. Analysis.
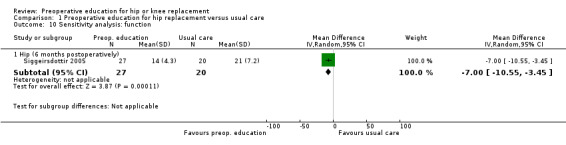
Comparison 1 Preoperative education for hip replacement versus usual care, Outcome 10 Sensitivity analysis: function.
Preoperative education for knee replacement versus usual care
See Table 2.
Pain
See Analysis 2.1. Two trials measured postoperative pain using a VAS at at least one time point (Beaupre 2004; McDonald 2004). Differences between groups on a 100‐point scale were small and not statistically significant at two days postoperatively (1 trial, 26 participants, MD ‐12.20; 95% CI ‐29.77 to 5.37) or 12 months postoperatively (1 trial, 109 participants, MD 2.00; 95% CI ‐3.45 to 7.45). We chose not to combine these RCTs in a meta‐analysis given the considerable heterogeneity in time points.
2.1. Analysis.
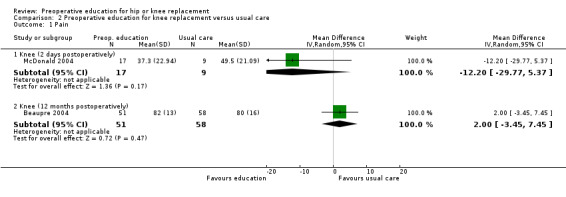
Comparison 2 Preoperative education for knee replacement versus usual care, Outcome 1 Pain.
Function
See Analysis 2.2. One trial measured postoperative function using the WOMAC function (Beaupre 2004). Participants receiving preoperative education had function scores that were not statistically significantly different from people receiving usual care at 12 months postoperatively on a 100‐point scale (1 trial, 109 participants, MD 0; 95% CI ‐5.63 to 5.63).
2.2. Analysis.
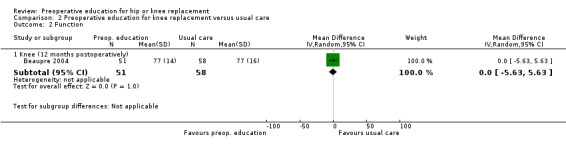
Comparison 2 Preoperative education for knee replacement versus usual care, Outcome 2 Function.
Health‐related quality of life
See Analysis 2.3. One trial measured health‐related quality of life using the SF‐36 (Beaupre 2004). At 12 months postoperatively, scores were lower (worse) for the preoperative education group on the Physical Component Score (1 trial, 109 participants, MD ‐3.00; 95% CI ‐6.38 to 0.38) and Mental Component Score (1 trial, 109 participants, MD ‐2.00; 95% CI ‐5.06 to 1.06), but these differences were not statistically significant.
2.3. Analysis.
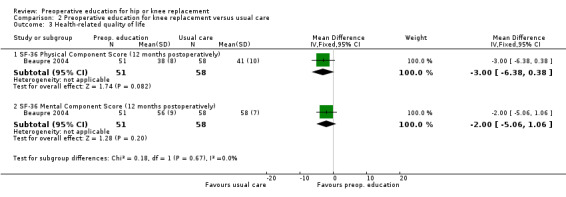
Comparison 2 Preoperative education for knee replacement versus usual care, Outcome 3 Health‐related quality of life.
Global assessment of treatment success
Global assessment of treatment success was not assessed in any of the trials included in the review.
Postoperative anxiety
Postoperative anxiety was not assessed in any of the trials included in the review.
Adverse events
See Analysis 2.4. One trial measured adverse events (Beaupre 2004). The risk of experiencing any serious postoperative complication was reduced by 31% in participants receiving preoperative education, though this effect was not statistically significant (1 trial, 115 participants, RR 0.69; 95% CI 0.29 to 1.66). Risk ratios for each type of postoperative complication were as follows: deep vein thrombosis (1 trial, 115 participants, RR 0.55; 95% CI 0.14 to 2.08); pulmonary emboli (1 trial, 115 participants, RR 1.09; 95% CI 0.16 to 7.48); and infection (1 trial, 115 participants, RR 0.73; 95% CI 0.13 to 4.19).
2.4. Analysis.
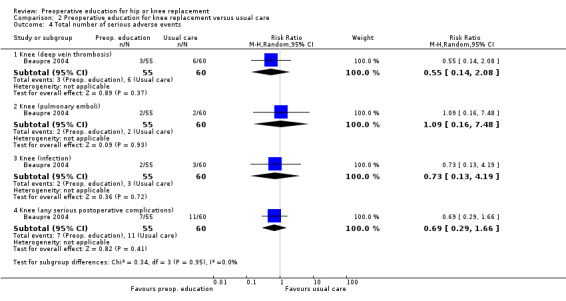
Comparison 2 Preoperative education for knee replacement versus usual care, Outcome 4 Total number of serious adverse events.
Re‐operation rate
Re‐operation rate was not assessed in any of the trials included in the review.
Preoperative anxiety
See Analysis 2.5. One trial measured preoperative anxiety using the Spielberger State‐Trait Anxiety Index (range of scores 20 to 80) (Crowe 2003). Preoperative education resulted in preoperative anxiety that was 5.5 points lower in participants undergoing knee replacement, though participants were not blind to treatment, so the preoperative education group may have overestimated their self reported anxiety (1 trial, 68 participants, MD ‐5.52; 95% CI ‐8.34 to ‐2.70).
2.5. Analysis.
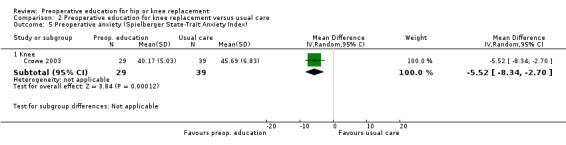
Comparison 2 Preoperative education for knee replacement versus usual care, Outcome 5 Preoperative anxiety (Spielberger State‐Trait Anxiety Index).
Length of hospital stay
See Analysis 2.6. Two trials measured length of hospital stay (days) (Beaupre 2004; Crowe 2003). Preoperative education reduced length of stay for participants with knee replacement by 1.86 days (2 trials, 183 participants, MD ‐1.86; 95% CI ‐3.40 to ‐0.32; I2 = 0%). Both trials were at low risk of selection and detection bias.
2.6. Analysis.
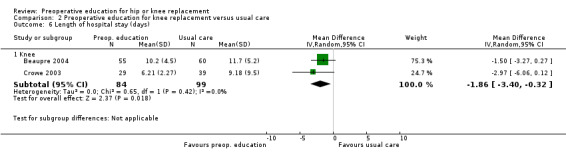
Comparison 2 Preoperative education for knee replacement versus usual care, Outcome 6 Length of hospital stay (days).
Mobility
See Analysis 2.7. One trial reported data on mobility (Crowe 2003). Preoperative education resulted in a reduction in days to stand or walk that was not statistically significant (1 trial, 68 participants, MD ‐1.13; 95% CI ‐2.82 to 0.56).
2.7. Analysis.
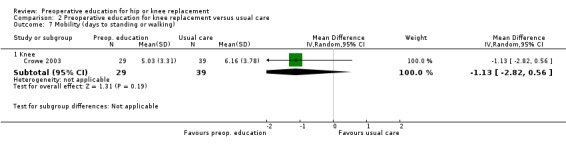
Comparison 2 Preoperative education for knee replacement versus usual care, Outcome 7 Mobility (days to standing or walking).
Range of motion
See Analysis 2.8. One trial assessed knee flexion and extension (i.e. total range of sagittal knee motion in degrees) (Beaupre 2004). The difference between groups at 12 months postoperatively favoured the preoperative education group but was not statistically significant (1 trial, 109 participants, MD ‐4.00; 95% CI ‐10.02 to 2.02).
2.8. Analysis.
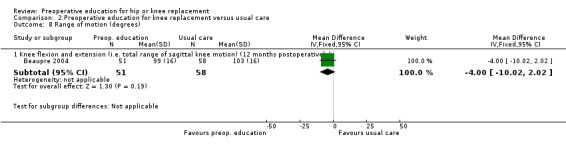
Comparison 2 Preoperative education for knee replacement versus usual care, Outcome 8 Range of motion (degrees).
Sensitivity analyses
See Analysis 2.9 and Analysis 2.10. For the outcomes postoperative pain and postoperative function, after removing trials with inadequate or unclear allocation concealment, only one trial remained (Beaupre 2004). WOMAC pain scores (0‐100 scale) were 2 points higher in the preoperative education group at 12 months postoperatively (1 trial, 109 participants, MD 2.00; 95% CI ‐3.45 to 7.45), and WOMAC function scores (0‐100 scale) were not different between groups at 12 months postoperatively (1 trial, 109 participants, MD 0; 95% CI ‐5.63 to 5.63). Neither of these differences were statistically significant.
2.9. Analysis.
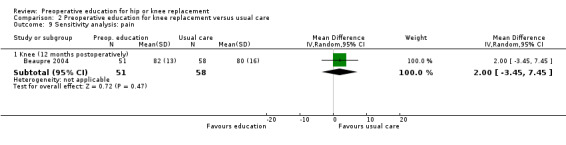
Comparison 2 Preoperative education for knee replacement versus usual care, Outcome 9 Sensitivity analysis: pain.
2.10. Analysis.
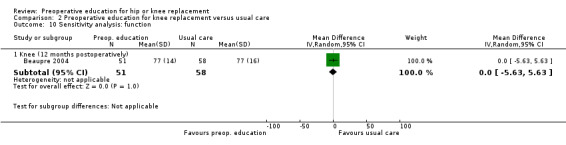
Comparison 2 Preoperative education for knee replacement versus usual care, Outcome 10 Sensitivity analysis: function.
Discussion
Summary of main results
The results of the 18 trials (1463 participants) suggest that preoperative education may be no better or worse than usual care for several participant‐reported outcome measures, including pain, function, health‐related quality of life and postoperative anxiety.
Preoperative education was found to reduce preoperative anxiety in people undergoing hip replacement. This is potentially of clinical importance because anxiety is not only an uncomfortable psychological state, but it also interacts with pain and coping, which are thought to influence functional outcomes. Being very anxious before surgery does not necessarily mean a person will have worse outcomes, or find it harder to recover from the procedure, but it may have an effect on a person's ability to understand and retain important information (Bastian 2002; Wallace 1986). However, the results of the meta‐analysis of preoperative anxiety should be treated with caution as the effect was small and participants were not blind to treatment.
Length of hospital stay was statistically significantly reduced by almost two days in participants receiving preoperative education for knee replacement, but the corresponding reduction for people receiving education for hip replacement was smaller and non‐significant. Along with preoperative education, enhanced recovery or 'fast track' programmes have also been introduced into clinical practice over a similar period (Savaridas 2013). These programmes aim to enhance each component part of the patient pathway, from preoperative education to postoperative rehabilitation. Enhanced recovery programmes represent a biopsychosocial model that aims to address the physical, psychological and social need of the patient. Reduction in length of stay is widespread with such programmes, and is almost certainly related to multiple pathway changes, rather than simply one component. In many of the larger centres, hip and knee replacements are treated by different groups of surgeons, which has led to the development of joint specific pathways, introduced at different times. Traditionally, greater focus has been upon knee replacements, due to the worse patient‐reported outcomes, which may explain the differences in length of stay between hip and knee replacement.
For length of stay, established ward routines may also determine when people are mobilised and discharged, and the pressure on need for hospital beds means that people are returning home at the earliest safe opportunity (Clode‐Baker 1997). Therefore, it is not surprising that the length of hospital stay is largely unaffected by preoperative education. A person's level of anxiety and knowledge may determine how much time staff spend with them but may not prevent hospital staff mobilising the person on the prescribed day. Differences between the trials regarding length of hospital stay and days to standing or walking may be more of a reflection of when and where these trials were conducted, and the guidelines and protocols in place at the time.
Adverse events such as infection and deep vein thrombosis were lower in participants receiving preoperative education for hip or knee replacement compared with usual care, though differences were not statistically significant (trials would likely have been underpowered to detect differences between groups in adverse events).
Overall completeness and applicability of evidence
The findings of this review need to be interpreted after consideration of several factors. Only a small number of trials contributed data to the pooled analyses. The small sample size of many of the trials means that rare but potentially important postoperative complications were less likely to be detected. Only five trials included people undergoing total knee replacement, and thus the results should be applied cautiously to this group of people. Few trials reported suitable data on our patient‐important outcomes of interest (particularly pain, function, health‐related quality of life, global assessment of treatment success and re‐operation rate, the latter two were not reported as an outcome in any of the trials). The included trials more commonly measured surrogate outcomes such length of hospital stay and days to stand or walk.
Quality of the evidence
The overall quality of the evidence was low according to the GRADE approach (see Table 1; Table 2). We limited the presentation of pain and function to evidence from trials with adequate allocation concealment. For most outcomes, the main reasons for downgrading of evidence were serious concerns about risk of bias due to lack of blinding (and unclear allocation concealment for some trials reporting outcomes other than pain and function), and the imprecision of the effect estimates (reflected in wide 95% CIs that crossed the null value). The lack of participant blinding in the majority of trials is concerning given that many outcomes were self reported, and empirical evidence indicates that unblinded trials with self reported outcomes show exaggerated treatment effects (Savović 2012). An additional concern is that eight trials were rated at high risk of selective reporting bias because the data necessary to include the trial in a meta‐analysis of at least one outcome (e.g. standard deviations) were not reported (Clode‐Baker 1997; Daltroy 1998; Gocen 2004; Johansson 2007; Lilja 1998; McGregor 2004; Siggeirsdottir 2005; Sjöling 2003). This is concerning given the results of one study that suggests that selective outcome reporting of 'positive' or statistically significant trial results can bias the results and conclusions of systematic reviews (Kirkham 2010).
Potential biases in the review process
While our described methods attempted to minimise bias in the selection of trials, collection of published data and analysis for the review, our searches were limited to electronic databases, and, as a result, we have only included published trials. In future updates of this review, we will attempt to identify grey literature, given that empirical evidence suggests that published trials tend to have exaggerated treatment effects compared with unpublished trials (Song 2010). It was also difficult to obtain relevant unpublished data from the authors of included trials. Further, it was difficult to assess selective outcome reporting as we identified no protocols or trial registry entries for the included trials.
Agreements and disagreements with other studies or reviews
The results of the current review agree with several other recently published reviews. Louw 2013 included the trials by Beaupre 2004; Clode‐Baker 1997; Daltroy 1998; Doering 2000; Giraudet 2003; Gocen 2004; Lilja 1998; McDonald 2004; McGregor 2004; Sjöling 2003; and Vukomanović 2008, and, in agreement with our review, concluded that preoperative education for hip or knee replacement has no statistically significant effect on postoperative pain (which was the only outcome investigated). One systematic review by Wallis 2011 examined the effect of a range of preoperative interventions for hip or knee replacement (exercise and education, exercise alone, manual therapy, cognitive therapy, braces, orthotics, acupuncture); however, trials of education alone were not eligible. Only three trials in the Wallis 2011 review were included in the current review (Beaupre 2004; Gocen 2004; Vukomanović 2008). In one meta‐analysis of 'days to stand or walk', which pooled data from Gocen 2004 and Vukomanović 2008, Wallis 2011 concluded that preoperative exercise and education for hip replacement was superior to usual care. However, we reached a more cautious conclusion regarding this outcome because we combined data from these two trials with data from an additional four "education only" trials (Crowe 2003; Doering 2000; Giraudet 2003; Wijgman 1994). Wallis 2011 also included the trial conducted by Ferrara 2008, which was excluded from the current review as the education component of the "exercise plus education" intervention was delivered postoperatively. Finally, one review of randomised trials and non‐randomised studies published from 2004 to 2010 and investigating the effect of preoperative education for a range of surgical procedures (e.g. hip replacement, thoracic surgery, cardiac artery by‐pass graft surgery) concluded that knowledge about the surgical procedure was the only beneficial outcome of education (Ronco 2012).
Authors' conclusions
Implications for practice.
Our review was unable to establish if preoperative education reduces anxiety or leads to improved surgical outcomes such as improvements in pain and function, or reduced adverse events over and above usual care. However, educating and informing people preoperatively has become such an essential part of patient care that it would be unethical to exclude this from current practice. Indeed, preoperative education is now so embedded within practice around the world that it can be seen as integral to the consent process. Despite the excellent results experienced by a large proportion of people having hip and knee replacements, many people experience ongoing pain, dysfunction and disability. Improving patient outcomes is thus a high priority that increasingly relies on non‐surgical factors. Preoperative education may represent a useful adjunct, with low risk of undesirable effects, particularly in certain people (e.g. people with depression, anxiety or unrealistic expectations) who may respond well to preoperative education that is stratified according to their physical, psychological and social need. The review did provide low‐quality evidence that preoperative education may have a small beneficial effect on preoperative anxiety.
Implications for research.
Preoperative education in its current form may not be sufficient to improve postoperative outcomes. One possible reason for the lack of demonstrable benefit is that the preoperative education evaluated is not targeted at the individual person, and is thus not adapted to the person's psychosocial factors. Future research should investigate how a stratified biopsychosocial approach could be used to assess individual patient requirements (e.g. physical, psychological and social need) and tailor preoperative education accordingly. Further research could also assess which method, or combination of methods, is best for delivering patient‐stratified education, and how preoperative education can be reinforced by postoperative care.
What's new
| Date | Event | Description |
|---|---|---|
| 14 September 2015 | Amended | New citation ‐ author amendment |
History
Protocol first published: Issue 1, 2002 Review first published: Issue 1, 2004
| Date | Event | Description |
|---|---|---|
| 4 February 2014 | New citation required but conclusions have not changed | A substantial amount of new information has been added to the updated review including: the addition of nine new studies; important changes to the methodology (risk of bias and summary of findings tables were added to review); and extensive re‐writing (not affecting the conclusions) in the reporting of the methods and results to align with the standards recommended by the Cochrane Collaboration's Methodological Expectations of Cochrane Intervention Reviews (MECIR) project. |
| 31 May 2013 | New search has been performed | A new search was conducted on 31st May 2013. Nine new studies were included (Beaupre 2004; Giraudet 2003; Gocen 2004; Johansson 2007; McDonald 2004; McGregor 2004; Siggeirsdottir 2005; Sjöling 2003; Vukomanović 2008) in the update, in addition to the nine trials included in the previous version. |
| 10 May 2008 | Amended | Converted to new review format. CMSG ID: A017‐R |
Notes
For Doering 2000, we are waiting for translation of the report published in Zeitschrift Fuer Psychosomatische Medizin Und Psychotherapie in 2001 that presents three‐month follow‐up data on mobility.
Acknowledgements
We thank Amrita Williams for assistance in drafting the background section; Cristel Dunshea for help with extracting data from Wijgman 1994; and Gordon Butler, Stephan Doering and Jean Crowe for providing additional trial data.
Appendices
Appendix 1. MEDLINE search strategy
| 1. exp Arthroplasty, Replacement/ 2. exp Joint Prosthesis/ 3. ((hip$ or knee$) adj5 (arthroplast$ or prosthe$ or replac$)).tw. 4. or/1‐3 5. exp Preoperative Care/ 6. exp Patient Education/ 7. exp Postoperative Period/ 8. (information or instruct$ or educat$ or advice or support$).mp. 9. (video$ or tape$ or audio$ or leaflet$ or pamphlet$ or booklet$).mp. 10. or/5‐9 11. clinical trial.pt. 12. randomized.ab. 13. placebo.ab. 14. dt.fs. 15. clinical trials/ 16. randomly.ab. 17. trial.ti. 18. group.ab. 19. or/11‐16 20. animals/ 21. humans/ 22. 20 and 21 23. 20 not 22 24. 19 not 23 25. and/4,10,24 |
Appendix 2. EMBASE search strategy
| 1. exp Arthroplasty, Replacement/ 2. exp Joint Prosthesis/ 3. ((hip$ or knee$) adj5 (arthroplast$ or prosthe$ or replac$)).tw. 4. or/1‐3 5. exp Preoperative Care/ 6. exp Patient Education/ 7. exp Postoperative Period/ 8. (information or instruct$ or educat$ or advice or support$).mp. 9. (video$ or tape$ or audio$ or leaflet$ or pamphlet$ or booklet$).mp. 10. or/5‐9 11. (random$ or placebo$).ti,ab. 12. ((single$ or double$ or triple$ or treble$) and (blind$ or mask$)).ti,ab. 13. controlled clinical trial$.ti,ab. 14. RETRACTED ARTICLE/ 15. or/11‐14 16. (animal$ not human$).sh,hw. 17. 15 not 16 18. and/4,10,17 |
Appendix 3. CENTRAL search strategy
1. ARTHROPLASTY REPLACEMENT explode all trees (MeSH) 2. JOINT PROSTHESIS explode all trees (MeSH) 3. ((hip* near replac*) or (hip* near prosthe*) or (hip* near arthroplast*)) 4. ((knee* near replac*) or (knee* near prosthe*) or (knee* near arthroplast*)) 5. PATIENT EDUCATION as Topic explode all trees (MeSH) 6. PREOPERATIVE CARE explode all trees (MeSH) 7. (information or instruct* or educat* or advice* or support*) 8. (preoperativ* or pre‐operativ*) 9. (#1 or #2 or #3 or #4) 10. (#5 or #6 or #7 or #8) 11. (#9 and #10)
Appendix 4. CINAHL search strategy
| S1 (MH "Arthroplasty, Replacement+") S2 (MH "Orthopedic Prosthesis+") S3 TI hip* N5 replace* or TI hip* N5 arthroplast* or TI hip* N5 prosthe* or TI knee* N5 replace* or TI knee* N5 arthroplast* or TI knee* prosthe* or AB hip* N5 replace* or AB hip* N5 arthroplast* or AB hip* N5 prosthe* or AB knee* N5 replace* or AB knee* N5 arthroplast* or AB knee* N5 prosthe* S4 S1 or S2 or S3 S5 (MH "Patient Education+") S6 (MH "Preoperative Education") S7 TI ( information or instruct* or educat* or advice or support* ) or AB ( information or instruct* or educat* or advice or support* ) S8 TI ( video* or tape* or audio* or leaflet* or pamphlet* or booklet* ) or AB ( video* or tape* or audio* or leaflet* or pamphlet* or booklet* ) S9 S5 or S6 or S7 or S8 S10 S4 and S9 S11 (MH "Clinical Trials+") S12 TI "clinical trial*" or AB "clinical trial*" S13 PT clinical trial S14 TI singl* blind* or TI singl* mask* or TI doubl* blind* or TI doubl* mask* or TI trebl* blind* or TI trebl* mask* or TI tripl* blind* or TI tripl* mask* S15 AB singl* blind* or AB singl* mask* or AB doubl* blind* or AB doubl* mask* or AB trebl* blind* or AB trebl* mask* or AB tripl* blind* or AB tripl* mask* S16 TI Randomi?ed control* trial* or AB Randomi?ed control* trial* S17 (MH "Random Assignment") S18 TI Random* allocat* or AB Random* allocat* S19 TI Placebo* or AB Placebo* S20 (MH "Placebos") S21 (MH "Quantitative trials") S22 TI Allocat* random* or AB Allocat* random* S23 S11 or S12 or S13 or S14 or S15 or S16 or S17 or S18 or S19 or S20 or S21 or S22 S24 S10 and S23 |
Appendix 5. PsycINFO search strategy
| 1. ((hip$ or knee$) adj5 (replac$ or arthroplast$ or prosthe$)).mp. 2. exp Client Education/ 3. (information or instruct$ or educat$ or advice or support$).mp. 4. (video$ or tape$ or audio$ or leaflet$ or pamphlet$ or booklet$).mp. 5. or/2‐4 6. 1 and 5 |
Data and analyses
Comparison 1. Preoperative education for hip replacement versus usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Hip (up to 3 months) | 3 | 227 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.47, 0.13] |
| 2 Function | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Hip (3 to 24 months) | 4 | 177 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐0.93, 0.06] |
| 3 Postoperative anxiety (Spielberger State‐Trait Anxiety Index) | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Hip (up to 6 weeks postoperatively) | 3 | 264 | Mean Difference (IV, Random, 95% CI) | ‐2.28 [‐5.68, 1.12] |
| 4 Total number of serious adverse events | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 Hip (any serious postoperative complications) | 2 | 150 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.19, 3.21] |
| 5 Preoperative anxiety (Spielberger State‐Trait Anxiety Index) | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Hip | 4 | 333 | Mean Difference (IV, Random, 95% CI) | ‐5.10 [‐7.17, ‐3.03] |
| 6 Length of hospital stay (days) | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 Hip | 7 | 487 | Mean Difference (IV, Random, 95% CI) | ‐0.79 [‐1.96, 0.37] |
| 7 Mobility (days to standing or walking) | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Hip | 6 | 417 | Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.30, 0.07] |
| 8 Range of motion (degrees) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Hip abduction (up to 6 weeks postoperatively) | 2 | 95 | Mean Difference (IV, Fixed, 95% CI) | ‐1.09 [‐5.35, 3.17] |
| 8.2 Flexion of the hip with flexed knee (up to 6 weeks postoperatively) | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | 0.75 [‐7.67, 9.17] |
| 8.3 Flexion of the hip with extended knee (up to 6 weeks postoperatively) | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | ‐0.25 [‐9.17, 8.67] |
| 9 Sensitivity analysis: pain | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1 Hip (up to 6 weeks postoperatively) | 1 | 100 | Mean Difference (IV, Random, 95% CI) | ‐7.0 [‐14.85, 0.85] |
| 10 Sensitivity analysis: function | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 10.1 Hip (6 months postoperatively) | 1 | 47 | Mean Difference (IV, Random, 95% CI) | ‐7.0 [‐10.55, ‐3.45] |
Comparison 2. Preoperative education for knee replacement versus usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Knee (2 days postoperatively) | 1 | 26 | Mean Difference (IV, Random, 95% CI) | ‐12.20 [‐29.77, 5.37] |
| 1.2 Knee (12 months postoperatively) | 1 | 109 | Mean Difference (IV, Random, 95% CI) | 2.0 [‐3.45, 7.45] |
| 2 Function | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Knee (12 months postoperatively) | 1 | 109 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐5.63, 5.63] |
| 3 Health‐related quality of life | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 SF‐36 Physical Component Score (12 months postoperatively) | 1 | 109 | Mean Difference (IV, Fixed, 95% CI) | ‐3.0 [‐6.38, 0.38] |
| 3.2 SF‐36 Mental Component Score (12 months postoperatively) | 1 | 109 | Mean Difference (IV, Fixed, 95% CI) | ‐2.0 [‐5.06, 1.06] |
| 4 Total number of serious adverse events | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 Knee (deep vein thrombosis) | 1 | 115 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.14, 2.08] |
| 4.2 Knee (pulmonary emboli) | 1 | 115 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.16, 7.48] |
| 4.3 Knee (infection) | 1 | 115 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.13, 4.19] |
| 4.4 Knee (any serious postoperative complications) | 1 | 115 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.29, 1.66] |
| 5 Preoperative anxiety (Spielberger State‐Trait Anxiety Index) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Knee | 1 | 68 | Mean Difference (IV, Random, 95% CI) | ‐5.52 [‐8.34, ‐2.70] |
| 6 Length of hospital stay (days) | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 Knee | 2 | 183 | Mean Difference (IV, Random, 95% CI) | ‐1.86 [‐3.40, ‐0.32] |
| 7 Mobility (days to standing or walking) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Knee | 1 | 68 | Mean Difference (IV, Random, 95% CI) | ‐1.13 [‐2.82, 0.56] |
| 8 Range of motion (degrees) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Knee flexion and extension (i.e. total range of sagittal knee motion) (12 months postoperatively) | 1 | 109 | Mean Difference (IV, Fixed, 95% CI) | ‐4.0 [‐10.02, 2.02] |
| 9 Sensitivity analysis: pain | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1 Knee (12 months postoperatively) | 1 | 109 | Mean Difference (IV, Random, 95% CI) | 2.0 [‐3.45, 7.45] |
| 10 Sensitivity analysis: function | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 10.1 Knee (12 months postoperatively) | 1 | 109 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐5.63, 5.63] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Beaupre 2004.
| Methods | Randomised parallel group trial. | |
| Participants | 131 participants undergoing total knee replacement. Intervention group: 39 women, 26 men (mean age 67 years, SD 7); control group: 33 women, 33 men (mean age 67 years, SD 6). Inclusion criteria: diagnosis of non‐inflammatory arthritis; aged 40‐75 years; ability to understand English, or use a translator. Exclusion criteria: none stated. Location: Canada. |
|
| Interventions | Intervention group (n = 65) received an education programme consisting of instructions on crutch walking, bed mobility and transfers, and postoperative range of motion routine. Plus an exercise programme designed to improve knee mobility and strength, similar to the post‐surgical exercise routine. Participants attended 3 sessions/week for 4 weeks (12 treatment sessions in total) within 6 weeks of surgery. Control group (n = 66) continued with regular activities until surgery. |
|
| Outcomes | Pain, stiffness and function (WOMAC 100‐mm VAS (0‐100 points) higher score represented less pain, stiffness and dysfunction); overall health status (SF‐36 (0‐100 points) higher score represented better health status); active knee range of motion; health service utilisation (re‐admission, further surgery, etc.); healthcare costs; length of hospital stay; complications. Participants were assessed pre‐ and post‐intervention and 3, 6 and 12 months postoperatively. | |
| Notes | WOMAC scores were transformed to a range from 0 to 100 points, where high scores indicated less pain and dysfunction. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomized, in blocks of 20 patients, ..." Comment: no description of how the sequence within each block was generated but probably adequate. |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization was performed using consecutively numbered opaque envelopes." |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Quote: patients had to be "willing to undertake the intervention and attend follow‐up visits..." Comment: patients were aware of the intervention and which group they were allocated to, making blinding of self‐reported outcomes not feasible. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Quote: "... a randomized clinical trial with blinded assessment of outcomes by a physical therapist not involved with the intervention." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: the number, reasons and distribution of exclusions between the 2 groups was adequately described. At least 80% of follow‐up assessments were completed. Missing data from the 3‐month and 6‐month assessments were imputed using the 'cold‐decking' strategy, which was robust when checked in a sensitivity analysis. |
| Selective reporting (reporting bias) | Unclear risk | Comment: all outcomes listed in the methods were reported in the results, but without the trial protocol, it is unclear whether any other outcomes were measured but not reported based on the results. |
| Other bias | Low risk | Comment: no other sources of bias identified. |
Butler 1996.
| Methods | Randomised parallel group trial. | |
| Participants | 80 participants aged 17‐85 years (mean 63, SD 13) undergoing total hip replacement. Intervention group: 18 women, 14 men (mean age 64 years, SD 13); control group: 22 women, 26 men (mean age 62 years, SD 13). Inclusion criteria: ability to read English. Exclusion criteria: previous hip replacement. Location: Canada. |
|
| Interventions | Intervention group (n = 32) posted an 18‐page teaching booklet as part of the pre‐admission package 4‐6 weeks before surgery. Control group (n = 48) posted pre‐admission package only (containing information of a general nature). |
|
| Outcomes | Anxiety (Spielberger State‐Trait Anxiety Inventory (20‐80 points) higher score represented greater anxiety); length of hospital stay; practising of pre‐hospital preparatory exercises; attendance at physiotherapy and occupational therapy sessions; participant satisfaction. Participants were assessed pre‐ and post‐intervention. | |
| Notes | On admission, both groups were treated identically. Patient satisfaction ratings were only taken just before discharge, by which time both groups had received the same information. An overall satisfaction rating was not obtained. Instead, ratings were given for each of six questions. The data entered in the review for patient satisfaction relate to the question "How satisfied were you with the amount of information you received about your hip joint and what a total hip replacement is?". | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: sequence generation not described. |
| Allocation concealment (selection bias) | Low risk | Quote: "A patient guide booklet was randomly added to half of the preadmission packages mailed out to THR [total hip replacement] patients." Comment: random allocation of the patient guide booklet was done by a clerk in the Admissions Department (and was concealed from the trial investigators) ‐ personal communication with author. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Comment: patients were not aware of the trial when booklets were randomly added to half the packages mailed out. Only at admission were patients informed of the purpose of the trial, gave their consent and then completed the anxiety inventory. Knowledge of the intervention could have influenced responses, especially those relating to anxiety and satisfaction with information. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Comment: unclear if trial personnel were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Eight additional patients were excluded because they were discharged before their predischarge data could be collected." Comment: not clear if these 8 participants were undergoing hip replacement for the first time (and thus would have been included in the analysis). There were missing data for all outcomes (in addition to the 8 participants mentioned above) ranging from 2 to 12 participants (length of stay). The reasons for drop‐outs are not stated. |
| Selective reporting (reporting bias) | Unclear risk | Comment: outcomes stated in the methods were reported in the results. Outcome data for satisfaction were not reported in sufficient detail in the paper but were provided by the study author on request. Without the trial protocol, it is unclear whether any other outcomes were measured but not reported based on the results. |
| Other bias | Low risk | Comment: no other sources of bias identified. |
Clode‐Baker 1997.
| Methods | Randomised parallel group trial. | |
| Participants | 78 participants undergoing total hip replacement (52 women, 26 men; aged ≤ 65 years (25 participants), aged 66‐74 years (27 participants), aged ≥ 75 years (27 participants)). Inclusion criteria: none stated. Exclusion criteria: none stated. Location: Leicester, UK. |
|
| Interventions | Intervention group (n = 41) was posted information (video and booklet) about the procedure and postoperative recovery about 4 weeks before surgery. On admission, offered the chance to see life‐size plastic model bones. Control group (n = 37) received no preadmission video or booklet but were seen routinely on admission by nursing staff who provided information about the hospital stay. |
|
| Outcomes | Pain (descriptive ordinal scale); general health state (Nottingham Health Profile); stress (Stress Arousal Checklist); anxiety and depression (Hamilton Anxiety and Depression Scale); days to mobilisation; length of hospital stay; sleep disturbance; satisfaction with information received. Participants were assessed pre‐intervention, 1 week postoperatively and 1 week post‐discharge. | |
| Notes | 25% of participants were undergoing their second primary total hip replacement and "nearly all" of these participants were in the intervention group. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Those who agreed to participate were randomized by an independent statistician..." Comment: very likely that the sequence was randomly generated if done by an independent statistician. |
| Allocation concealment (selection bias) | Low risk | Quote: "...were randomized by an independent statistician..." Comment: likely to be adequate since allocation was independent of the trial personnel. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Comment: no description of any attempt to blind patients and blinding is unlikely to have been possible. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Quote: "Nursing staff was not told to which group patients had been allocated." Comment: unlikely to have much impact on the results as most outcomes were participant reported. Participants could easily inadvertently disclose their group allocation to nursing staff. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: reasons for initial exclusions (cancelled or postponed operations) adequately described. Data on several participants were missing for various outcomes without any explanation, though the impact of missing data is unlikely to seriously affect the continuous outcomes. |
| Selective reporting (reporting bias) | High risk | Comment: all outcomes listed in the methods were reported in the results, but without the trial protocol, it is unclear whether any other outcomes were measured but not reported based on the results. Outcome data were only reported as medians and IQRs, so data were unable to be included in meta‐analyses. |
| Other bias | Low risk | Comment: no other sources of bias identified. |
Cooil 1997.
| Methods | Randomised parallel group trial with randomisation within matched pairs based on age, gender and socioeconomic status. | |
| Participants | 42 participants (30 women, 12 men) undergoing total hip replacement. Intervention group: mean age 69 years (SD 8, range 54 to 84); control group: mean age 69 years (SD 8, range 56 to 84). Inclusion criteria: unilateral total hip replacement. Exclusion criteria: previous hip replacement surgery, unable to read or hear. Location: Essex, UK. |
|
| Interventions | Intervention group (n = 21) given an information sheet containing instructions for the postoperative protocol, a list of exercises plus advice on harmful and beneficial postoperative activities. Participants received verbal explanation of the content and were taught exercises and activities through demonstration and practice by a 'physiotherapy helper'. Control group (n = 21) given the same information sheet, asked to read and follow instructions but received no further contact with demonstrator. |
|
| Outcomes | Participant co‐operation and understanding (recall of exercises and advice on first postoperative day); participant satisfaction with content and delivery of information. Participants were assessed 1 and 2 days postoperatively. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The first subject in each matched pair was randomly assigned to one of the two groups..." Comment: sequence generation not stated. |
| Allocation concealment (selection bias) | Unclear risk | Comment: allocation concealment not described. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | Low risk | Quote: patients were "told that the aim of the trial was to evaluate the physiotherapy service." Comment: likely the patients were not fully aware of the differences between the 2 groups. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Quote: "...patients were tested by an independent assessor, who had no previous contact with the patients and who was blind to the subject grouping." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: data for 3 participants were missing for the recall scores but this is not explicitly reported or explained. Unlikely that this would adversely affect the overall results. |
| Selective reporting (reporting bias) | Unclear risk | Comment: all outcomes listed in the methods were reported in the results, but without the trial protocol, it is unclear whether any other outcomes were measured but not reported based on the results. |
| Other bias | Low risk | Comment: no other sources of bias identified. |
Crowe 2003.
| Methods | Randomised parallel group trial. | |
| Participants | 133 participants undergoing total hip replacement (65 participants) or total knee replacement (68 participants). Intervention group: 51 women, 14 men (mean age 67 years, SD 12); control group: 55 women, 13 men (mean age 71 years, SD 11). Inclusion criteria: participants who were not functioning well; had limited social support or co‐existing medical conditions, or both. Exclusion criteria: participants who were functioning well despite their joint dysfunction, who were managing activities of daily living and had good carer support. General exclusions included people with limited English and who were undergoing a revision or second joint replacement within 2 years. Location: Ontario, Canada. |
|
| Interventions | Intervention group (n = 65) received a preoperative education package (video, booklet plus information on length of stay, discharge criteria, respite care and diet). Some participants given tour of the hospital unit, demonstration of equipment, dietician counselling and social work input. All received individualised counselling from an occupational therapist. Control group (n = 68) received 1 standard preoperative clinic visit (lasting about 7 hours) 1‐2 weeks before surgery. Participants were informed about the hospital stay and the immediate postoperative phase. |
|
| Outcomes | Days to eligibility for discharge; preoperative anxiety (Spielberger State‐Trait Anxiety Inventory (20‐80 points) higher score represented greater anxiety); length of hospital stay; days to mobilisation (out of bed, walking and climbing stairs). | |
| Notes | Randomisation resulted in uneven numbers of hip and knee replacements in each group. Data for hip and knee replacement groups were obtained from the study author. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Subjects were allocated to one of the two groups by means of a random number table and using a system of sealed envelopes." |
| Allocation concealment (selection bias) | Low risk | Quote: "Subjects were allocated to one of the two groups by means of a random number table and using a system of sealed envelopes." |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Quote:"[Participants] were telephoned by the research coordinator who explained the trial. Oral assent was obtained, and the client signed an informed consent at his/her initial trial visit." Comment: participants were unlikely to be blinded and this may impact self reported outcomes like anxiety. It was not possible to blind the in‐hospital PT and OT staff as participants often choose to discuss previous rehabilitation with staff. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Quote: "Outcomes were measured in‐hospital by an investigator who was blinded to group allocation." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: incomplete outcome data not reported. It is unclear if there were missing data and if so, how this was handled. Results tables report continuous measures but omit the denominator. |
| Selective reporting (reporting bias) | Unclear risk | Comment: all outcomes listed in the methods were reported in the results, but without the trial protocol, it is unclear whether any other outcomes were measured but not reported based on the results. |
| Other bias | High risk | The control group had significantly poorer overall function prior to surgery (i.e. a pre‐existing difference that favoured the treatment group). |
Daltroy 1998.
| Methods | Randomised 4‐arm trial using a 2 x 2 factorial design stratified by joint and age (18‐70 years, > 70 years). | |
| Participants | 222 participants undergoing total hip replacement (n = 104) or total knee replacement (n = 118) (146 women, 76 men; mean age 64 years, SD 12). Inclusion criteria: participants scheduled for knee or hip replacement. Exclusion criteria: previous hip or knee surgery, inability to speak English or fill out questionnaires. Location: Boston, USA. |
|
| Interventions | Information group (n = 58) received a 12‐minute audio‐tape slide programme from a research assistant the day before surgery on the postoperative in‐hospital rehabilitation experience. A pamphlet was also left at the bedside. Relaxation group (n = 58) received training in Benson's Relaxation Response with a bedside audiotape the day before surgery. Information plus relaxation group (n = 52) received the information intervention followed by relaxation training. Control group (n = 54) received neither intervention. |
|
| Outcomes | Length of hospital stay; anxiety on day 4 (Spielberger State‐Trait Anxiety Inventory (20‐80 points) higher score represented greater anxiety); pain (1‐5 ordinal scale, where 1 represented least pain and 5 most pain; and charted pain medication used during the first 4 days after surgery); mental status on day 4 (Mini‐Mental State Examination (0‐30 points) higher score represented normal cognition); use of continuous passive motion machine; usefulness of intervention materials. | |
| Notes | Data from the Information plus relaxation group were excluded from the analyses because our inclusion criteria specified that the education/information intervention should be the sole component of the intervention. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...were assigned randomly to one of the treatment groups." Comment: sequence generation not described. |
| Allocation concealment (selection bias) | Unclear risk | Comment: allocation concealment not described. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Comment: baseline data were collected before randomisation, so these data are unaffected by group allocation. No description of any attempt to blind patients and blinding is unlikely to have been possible. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Quote: "In order to conceal the patient's group assignment from nurses, rehabilitation staff, and surgeons, all questionnaires and the intervention itself were administered by either of two research assistants." Comment: staff providing postoperative care were blinded but the research assistants administering the intervention and the outcome questionnaires were not blind. The trial authors reported that staff responses at patient discharge indicated that blinding was successfully implemented among the staff. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Five patients had incomplete followup questionnaire data and were excluded from all followup analyses except length of stay..." Comment: exclusions pre‐randomisation were described. Post‐randomisation, 1 participant was excluded because of postoperative complications unrelated to the surgery, and 5 had incomplete follow‐up questionnaire data. Neither the reasons for incomplete data nor the distribution between groups were given; however, the impact was likely to be minimal because of the relatively small number of missing participants (less than 3%), plus the outcomes were continuous measures. |
| Selective reporting (reporting bias) | High risk | Comment: results of all outcomes were partially reported. Trialists only reported means and SDs for both groups combined, and presented mean values of each group, with no measures of variation, in figure format. Trialists also reported that for all outcomes, the differences between groups was not statistically significant. Attempts to retrieve missing data from trialists were unsuccessful. All outcomes listed in the methods were reported in the results, but without the trial protocol, it is unclear whether any other outcomes were measured but not reported based on the results. |
| Other bias | Low risk | Comment: no other sources of bias identified. |
Doering 2000.
| Methods | Randomised parallel group trial. | |
| Participants | 100 participants undergoing total hip replacement. Intervention group: 21 women, 25 men (mean age 59 years, SD 11); control group: 17 women, 37 men (mean age 60 years, SD 9). Inclusion criteria: aged ≥ 18 years, osteoarthritis of the hip. Exclusion criteria: previous hip surgery, co‐morbidity associated with severe pain, scheduled elective hip replacement, co‐morbidity that might alter cortisol and catecholamine excretion, psychiatric co‐morbidity. Location: Innsbruck, Austria. |
|
| Interventions | Intervention group (n = 46) shown a 12‐minute video in the presence of an investigator the night before surgery; film contained procedural information (pre‐ and postoperative), behavioural instructions and information about a participant's likely sensory experiences. Control group (n = 54) received preoperative information delivered by a surgeon and anaesthetist, and routine information sheets. |
|
| Outcomes | Anxiety (Spielberger State‐Trait Anxiety Inventory (20‐80 points) higher score represented greater anxiety); depression (von Zerssen Depression Scale; scoring system not reported); days to mobilisation (standing and climbing stairs); length of hospital stay; pain (100‐mm VAS, and postoperative analgesics); blood pressure; cortisol excretion. Participants were assessed preoperatively and 2 days postoperatively. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients... were randomly assigned to the preparation or control group." Comment: randomisation was performed by means of chance numbers (personal communication) |
| Allocation concealment (selection bias) | Unclear risk | Comment: allocation concealment not described. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Comment: No description of any attempt to blind participants; participants likely to be aware of group allocation and this may have influenced participants' responses to the anxiety questionnaire. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Quote: "Physicians of the Departments of Orthopedics and Anesthesia were blind to the assignment of patients to groups." Comment: for measures of mobility and use of analgesics outcome assessment was blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: there does not appear to be any withdrawals (e.g. cortisol data were complete) but missing values are not explicitly reported. |
| Selective reporting (reporting bias) | Unclear risk | Comment: data for all continuous outcomes were presented as mean values without measures of variation in figure format; however, trialists provided means and SDs on request. All outcomes listed in the methods were reported in the results, but without the trial protocol, it is unclear whether any other outcomes were measured but not reported based on the results. |
| Other bias | Low risk | Comment: no other sources of bias identified. |
Giraudet 2003.
| Methods | Randomised parallel group trial. | |
| Participants | 100 participants undergoing total hip replacement. Intervention group: 24 women, 24 men (mean age 63 years, SD 9); control group: 32 women, 20 men (mean age 64 years, SD 10). Inclusion criteria: first elective total hip replacement for primary hip osteoarthritis. Exclusion criteria: secondary osteoarthritis or another disease of the hip, age > 80 years, American Society of Anesthesiologists physical status score > 2, Montgomery and Asberg Depression Rating scale > 30, inability to speak French, sight impairment, living far from Paris. Location: Paris, France. |
|
| Interventions | Intervention group (n = 48) attended a half‐day, small‐group (3‐6 per group) multidisciplinary information session 2 to 6 weeks before surgery. The multidisciplinary team consisted of a rheumatologist, surgeon, anaesthetist, physiotherapist and psychiatrist. The programme was standardised but the multidisciplinary team varied. Participants also received the usual verbal information and standard information leaflet. Control group (n = 52) received usual verbal information from the surgeon and anaesthetist (based on the participant's personality, psychology, expectations and needs) plus the standard information leaflet that contained practical information, advice and warnings on hospitalisation and rehabilitation. |
|
| Outcomes | Anxiety pre‐ and postoperatively (Spielberger State‐Trait Anxiety Inventory (20‐80 points) higher score represented greater anxiety); pain (VAS (0‐100 points) a higher score represented worse pain, and personal analgesic use diary); days to standing; length of hospital stay; rehabilitation; participant satisfaction (range 0‐100); complications. Participants were assessed preoperatively and 1 and 7 days postoperatively. | |
| Notes | All participants were permitted to stand on day 2, but the day participants were permitted to walk depended on the person's recovery. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The allocation sequence was generated by the random placement of thoroughly shuffled marked cards..." |
| Allocation concealment (selection bias) | Low risk | Quote: "... the random placement of thoroughly shuffled marked cards into sequentially numbered sealed, opaque envelopes by the outpatient clinic assistant..." |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Comment: no description of any attempt to blind participants and blinding is unlikely to have been possible. Knowledge of being in the intervention group may have influenced participants' use of analgesics and their anxiety levels. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Comment: blinding of outcome assessors not reported, though this could have been done. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All but one patient (control group) completed the trial. This patient withdrew... refusing to complete the State Anxiety Inventory after surgery." |
| Selective reporting (reporting bias) | Unclear risk | Comment: all outcomes listed in the methods were reported in the results, but without the trial protocol, it is unclear whether any other outcomes were measured but not reported based on the results. |
| Other bias | Low risk | Comment: no other sources of bias identified. |
Gocen 2004.
| Methods | Randomised parallel group trial. | |
| Participants | 59 participants undergoing total hip replacement. Intervention group: 13 women, 16 men (mean age 47 years, SD 11); control group: 8 women, 22 men (mean age 56 years, SD 14). Inclusion criteria: osteoarthritis of the hip joint, no previous physiotherapy for hip osteoarthritis. Exclusion criteria: other chronic diseases or arthritis in other joints necessitating treatment. Location: Izmir, Turkey. |
|
| Interventions | Intervention group (n = 29) were given stretching and strengthening exercises 3 times daily for 8 weeks before surgery, and an education programme that included advice on movements to avoid, use of devices and activities of daily living. Control group (n = 30) received neither the preoperative exercises nor the education programme. |
|
| Outcomes | Function* (Harris Hip Score (maximum 100 points) 90‐100: good function and excellent results, 80‐90: good, 70‐80: fair, < 70: poor results); range of motion; pain (VAS; units of the scale not reported); days to mobility (walking and climbing stairs); length of hospital stay. Participants were assessed preoperatively, at discharge, and 3 months and 2 years postoperatively. | |
| Notes | *Harris Hip Score data at 2 years included in Analysis 1.2. Both groups received the same postoperative and education programme beginning the day after surgery. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The patients were randomly divided into two groups using a table of random numbers of a computer programme (Excel 2000)." |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Even numbers were allocated to the control group and odd numbers to the trial group." Comment: it is not clear who was involved in the allocating the participants or what steps were taken to conceal the random sequence. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Comment: no description of any attempt to blind participants and blinding is unlikely to have been possible. Knowledge of being in the intervention group may have influenced participants' experience of pain. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Quote: "Postoperative treatment was performed by a physical therapist who was blinded to the patients' groups. ... All measurements were performed by a staff physical therapist who was blinded to the trial." Comment: it is possible that participants could disclose which group they were in during treatment or measurement by the physiotherapist. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: 1 participant assigned to the trial group was not operated on because of cardiovascular problems and was excluded from the analysis. Data for the 59 participants that underwent surgery were available at discharge and 1‐year follow‐up. No mean or SD given for length of hospital stay. |
| Selective reporting (reporting bias) | High risk | Comment: trialists reported measuring pain with VAS in the methods section, but no pain data were reported in the results section. Also, without the trial protocol, it is unclear whether any other outcomes were measured but not reported based on the results. |
| Other bias | Low risk | Comment: no other sources of bias identified. |
Johansson 2007.
| Methods | Randomised parallel group pre‐post test design. | |
| Participants | 123 participants undergoing total hip replacement. Intervention group: 32 women, 30 men (mean age 60 years); control group: 31 women, 30 men (mean age 65 years). Inclusion criteria: aged ≥ 18 years, able to complete questionnaires. Exclusion criteria: none stated. Location: Finland. |
|
| Interventions | Intervention group (n = 62) received standard written education materials plus education using the concept map method that was delivered by 2 specially trained nurses 2 weeks before admission lasting 30‐60 minutes. The concept map method involved counselling in biophysiological, functional, experiential, ethical, social and financial issues about care both pre‐ and postoperative. Control group (n = 61) received standard written education materials only. |
|
| Outcomes | Participant knowledge (Orthopaedic Patient Knowledge Questionnaire); participant empowerment (Modified Empowerment Questionnaire); length of hospital stay; length of discussion at admission; need for further care. Participants were assessed preoperatively and at discharge. | |
| Notes | Trialists only reported that "The length of hospital stay was shorter among group A patients than in group B (A: M = 6.78 days; B: M = 8.18 days)". Requests for the SDs of each group were unsuccessful. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "A randomized two‐group pre‐test post‐test design was used..." Comment: sequence generation not described. |
| Allocation concealment (selection bias) | Unclear risk | Comment: method of allocation not described. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Quote: "Patients were informed about the purpose of the trial". Comment: no description of any attempt to blind participants and blinding is unlikely to have been possible. Knowledge of being in the intervention group may have influenced how participants performed in the pre‐ and posttest questionnaires. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Quote: "The clinical outcomes... were gathered from patients' documents." Comment: unclear if the staff responsible for participant discharge were part of the trial personnel; however, the risk of bias is likely to be minor. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: the number of post‐randomisation drop‐outs per group (11% in the intervention group and 16% in the control) and the reasons for the drop‐outs were described. Continuous outcomes unlikely to be affected by the proportion of drop‐outs. |
| Selective reporting (reporting bias) | High risk | Comment: SDs for length of hospital stay were missing from the published report. All other outcomes listed in the methods were reported in the results, but without the trial protocol, it is unclear whether any other outcomes were measured but not reported based on the results. |
| Other bias | Low risk | Comment: no other sources of bias identified. |
Lilja 1998.
| Methods | Randomised parallel group trial. | |
| Participants | 55 participants (median age 65 years) undergoing total hip replacement. Intervention group: 9 women, 13 men; control group: 8 women, 20 men. Inclusion criteria: aged < 75 years. Exclusion criteria: none stated. Location: Angelholm, Sweden. |
|
| Interventions | Intervention group (n = 22) given extended formalised information concerning pre‐ and postoperative procedures by an anaesthetic nurse for 30 minutes the day before surgery. Control group (n = 28) informed about pre‐ and postoperative routines by a ward nurse. |
|
| Outcomes | Anxiety (Hospital Anxiety and Depression Scale (0‐21 points) higher score represented greater anxiety); pain (VAS, ranging from 0 (no pain) to 10 (worst imaginable pain)); serum cortisol (radioimmunoassay). Participants were assessed preoperatively and 1 and 3 days postoperatively. | |
| Notes | Aim of the trial was to evaluate effects of extended preoperative information on perioperative stress. 5 participants withdrew post‐randomisation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "... were randomized into two groups..." Comment: sequence generation not described. |
| Allocation concealment (selection bias) | Unclear risk | Comment: method of allocation not described. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | Low risk | Quote: "To avoid interventional bias, the patients were only informed that a trial was in progress, but were not informed about the aim and the design of the trial." |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Quote: "The randomized design of the trial was kept from all personnel who came into contact with the patients except for the anaesthetic nurses who participated in the extended information. These nurses did not participate in any way in the postoperative registrations of stress, anxiety and pain." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: reasons are given for the withdrawal of the 5 participants after randomisation and their distribution between the 2 groups; it is not clear whether some of these participants underwent surgery. The study authors stated there were no other exclusions but it was not clear if there were any missing data within each analysis because the sample size was not reported. |
| Selective reporting (reporting bias) | High risk | Comment: trialists only reported mean values of each group with no measures of variation for all outcomes (and noted that the differences between groups on all outcomes were not statistically significant. Attempts to retrieve this missing data from trialists were unsuccessful. In addition, all outcomes listed in the methods were reported in the results, but without the trial protocol, it is unclear whether any other outcomes were measured but not reported based on the results. |
| Other bias | Low risk | Comment: no other sources of bias identified. |
McDonald 2004.
| Methods | Randomised 3‐arm trial. | |
| Participants | 26 participants undergoing total knee replacement (mean age 72 years, SD 5, range 65 to 88). Intervention group: 8 women, 9 men (mean age 73 years, SD 6); control group: 7 women, 2 men (mean age 72 years, SD 7). Inclusion criteria: aged ≥ 65 years, experiencing only non‐malignant pain; able to communicate in English. Exclusion criteria: previous hip or knee replacement, delirium or dementia. Location: Connecticut, USA. |
|
| Interventions | Intervention group (n = 17) attended the standard preoperative class provided by the hospital and viewed a pain management and pain communication film. Control group (n = 9) attended the standard preoperative class only. |
|
| Outcomes | Pain (Short Form of the McGill Pain Questionnaire, including 100‐mm VAS for pain intensity and present pain intensity scale where a higher score represented worse pain). Patients were assessed 1 and 2 days postoperatively and 1 and 7 days post‐discharge. | |
| Notes | The purpose of the trial was to test the effects of teaching preoperative basic pain management and communication skills on postoperative pain. Data for the second comparison group (viewed pain management film only) were not included in the analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Random assignment to group was accomplished through use of a table of random numbers." |
| Allocation concealment (selection bias) | Unclear risk | Comment: method of allocation not stated. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Comment: no description of any attempt to blind participants and blinding is unlikely to have been possible. |
| Blinding (performance bias and detection bias) Objective outcomes | Low risk | Quote: "The second author, who was blind to the older adults' conditions, obtained the postoperative pain measures after screening for delirium." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: study authors were explicit in stating how participants and data were handled, but some participants were removed due to a change in the protocol, and other participants were removed due to author interpretation. For example, all participants receiving hip replacements were removed from the analysis. |
| Selective reporting (reporting bias) | Unclear risk | Comment: the study authors reported the reasons for the difference between outcome measures initially used, and outcomes included in the results. Without the trial protocol, it is unclear whether any other outcomes were measured but not reported based on the results. |
| Other bias | High risk | Comment: change in protocol described and justified on the basis of minimising confounds, but it was done after the initial data analysis. |
McGregor 2004.
| Methods | Randomised parallel group trial. | |
| Participants | 35 participants (25 women, 10 men; mean age 72 years, SD 9, range 51 to 92) undergoing total hip replacement. Intervention group: 19 participants (mean age 71 years, SD 9); control group: 20 participants (mean age 73 years, SD 10). Inclusion criteria: none stated. Exclusion criteria: revision or bilateral arthroplasty, previous hip joint surgery, co‐existing morbidity, mental confusion, inadequate comprehension of English. Location: London, UK. |
|
| Interventions | Intervention group (n = 19) attended a preoperative hip class 2‐4 weeks before surgery and received an information booklet containing information about the surgery, pre‐ and postoperative stages and rehabilitation, including exercises. The preoperative class reinforced the information in the booklet and covered adaptations participants could make to their homes in the immediate postoperative period. Control group (n = 20) received the standard preoperative management that included a description of the surgery and its risk. They did not receive an information booklet or attend a class. |
|
| Outcomes | Function (WOMAC, administered using the Likert Scale version, which ranges from 0 to 68 where a higher score represented more dysfunction*; Harris Hip Score (maximum 100 points) 90‐100: good function and excellent results, 80‐90: good, 70‐80: fair, < 70: poor results; and Barthel Activities of Daily Living Index (0‐20 points) higher score represented less dysfunction); pain (WOMAC Likert Scale version (0‐20 points) higher score represented worse pain; and a VAS (0‐10 points) higher score indicated worse pain**) and expectations of postoperative pain (VAS, units of measurement not reported); mood (Positive Affect Negative Affect Scale); fatigue (VAS, units of measurement not reported); satisfaction (VAS, units of measurement not reported); length of hospital stay; economic analysis (EuroQoL EQ‐5D); complications. Participants were assessed preoperatively, at discharge, and 3 months postoperatively. | |
| Notes | *WOMAC function scale data at 3 months included in Analysis 1.2. **Only the 0‐10 VAS was included in the analysis of 'pain'. Trialists only reported that "On average, patients in group A spent 15 days in the hospital for the surgical procedure, whereas patients in group B spent 18 days in the hospital". Requests for the SDs of each group were unsuccessful. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...patients were allocated randomly into either group A or group B." Comment: sequence generation not described. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "...patients were randomized by age and not functional status." Comment: how participants were stratified and whether allocation was concealed was not described. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Comment: no description of any attempt to blind participants and blinding is unlikely to have been possible. Knowledge of being in the intervention group may have influenced participants' preoperative expectations of postoperative pain, mood and pain. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Comment: not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "...4 patients [from the intervention group] were subsequently lost to review." Comment: reasons for loss to follow‐up not stated. Impact of incomplete data likely to be minimal because outcomes were all continuous measures. Not clear if the pre‐discharge results included the 4 participants subsequently lost to review. |
| Selective reporting (reporting bias) | High risk | Comment: SDs for length of hospital stay were missing from the published report. All other outcomes listed in the methods were reported in the results, but without the trial protocol, it is unclear whether any other outcomes were measured but not reported based on the results. |
| Other bias | Low risk | Comment: no other sources of bias identified. |
Santavirta 1994.
| Methods | Randomised parallel group trial. | |
| Participants | 60 participants undergoing total hip replacement. Intervention group: 19 women, 8 men (mean age 59 years, SD 6); control group: 19 women, 14 men (mean age 58 years, SD 5). Inclusion criteria: aged ≥ 18 years. Exclusion criteria: previous major orthopaedic surgery, severe disabilities. Location: Helsinki, Finland. |
|
| Interventions | Intervention group (n = 27) before admission received an 18‐page patient information booklet covering all aspects of total hip replacement surgery and postoperative rehabilitation. On admission, participants had a 20‐ to 60‐minute teaching session delivered by one of the investigators concerning total hip replacement surgery and rehabilitation that was individually planned according to each participant's specific situation. Control group (n = 33) received the 18‐page booklet only. |
|
| Outcomes | Patient knowledge (disease, treatment and rehabilitation); patient satisfaction with information provided; patient compliance (questionnaire); complications. Participants were assessed preoperatively and 2‐3 months postoperatively. | |
| Notes | Measurements taken on admission to hospital and 2‐3 months postoperatively. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "... patients were randomly divided into an experimental and to a control group." Comment: sequence generation not described. |
| Allocation concealment (selection bias) | Unclear risk | Comment: method of allocation not described. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Comment: no description of any attempt to blind participants and blinding is unlikely to have been possible. Knowledge of being in the intervention group may have resulted in participatns trying to retain information and influenced the way they felt about the information. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Quote: "Orthopaedic surgeons who took care of and operated on these patients were knowledgeable of the trial but informed and treated the patients in their usual way." Comment: unclear if the surgeons were aware of which participants had received the individualised teaching session. Since the focus of the trial was on measures of patient knowledge, satisfaction and compliance, this is not an important source of bias. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: no exclusions or withdrawals reported. Sample sizes are not reported in the results tables so not possible to verify if are no missing data. |
| Selective reporting (reporting bias) | Unclear risk | Comment: all outcomes listed in the methods were reported in the results, but without the trial protocol, it is unclear whether any other outcomes were measured but not reported based on the results. |
| Other bias | Low risk | Comment: no other sources of bias identified. |
Siggeirsdottir 2005.
| Methods | Multi‐site randomised trial. | |
| Participants | 50 participants (26 women, 24 men; mean age 68 years, range 28 to 86) undergoing total hip replacement. Intervention group: 14 women, 13 men (mean age 69 years, range 52 to 81); control group: 12 women, 11 men (mean age 66 years, range 28 to 86). Inclusion criteria: participants living in their own home diagnosed with osteoarthritis of the hip, rheumatoid arthritis, primary segmental collapse of the femoral head or sequelae after developmental diseases or hip trauma. Exclusion criteria: primary hip fracture, metastatic tumours, dementia. Location: Reykjavik and Akranes, Iceland. |
|
| Interventions | Intervention group (n = 27) received a preoperative education and training programme 1 month before surgery given by a physiotherapist or occupational therapist (or both). Participants were informed about rehabilitation, became familiar with exercises and the devices to be used postoperatively. Participants also received an illustrated brochure on how to exercise postoperatively. Following discharge, participants received regular home visits from an outpatient team. Control group (n = 23) was treated according to clinical procedures already in use. |
|
| Outcomes | Function* (Oxford Hip Score (12‐60 points) higher score represented more dysfunction; Harris Hip Score (maximum 100 points) 90‐100: good function and excellent results, 80‐90: good, 70‐80: fair, < 70: poor results; and Nottingham Health Profile (maximum 100 points) higher score represented more dysfunction); length of hospital stay; complications. Participants were assessed preoperatively and 2, 4 and 6 months postoperatively. | |
| Notes | *Only outcome data for the Oxford Hip Score was reported in the trial publication, so no outcome data for the Harris Hip Score and Nottingham Health Profile were included in the review. Oxford Hip Score data at 6 months included in Analysis 1.2. The original trial design was to carry out the trial at one hospital only. The decision to expand to a second site was made for financial reasons, and because of a high initial drop‐out. Treatment group was treated differently postoperatively, in that a physiotherapist or occupational therapist visited them at home after discharge. Only data up to discharge were used in the analyses. A cost analysis of the trial was published as a separate paper (Siggeirsdottir 2005). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: sequence generation not described. |
| Allocation concealment (selection bias) | Low risk | Quote: "...they were randomized into one of the two groups (SG [study group] or CG [control group]) by opening a sealed envelope containing a note indicating which group the patient was to be allocated." |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Comment: no description of any attempt to blind participants and blinding is unlikely to have been possible. Knowledge of being in the intervention group may have influenced participants' pain and function scores. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Comment: not described. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: 2 control group participants missing preoperative pain and function scores. Impact of incomplete data likely to be minimal because outcomes are continuous measures. |
| Selective reporting (reporting bias) | High risk | Comment: outcome data were not fully reported for the Harris Hip Score or Nottingham Health Profile (trialists only reported P values for the differences between groups rather than means and SDs). Also, without the trial protocol, it is unclear whether any other outcomes were measured but not reported based on the results. |
| Other bias | Low risk | Comment: no other sources of bias identified. |
Sjöling 2003.
| Methods | Randomised parallel group trial. | |
| Participants | 60 participants (36 women, 24 men; mean age 71 years, range 54 to 86) undergoing total knee replacement. Inclusion criteria: diagnosis of osteoarthritis, aged ≥ 50 years. Exclusion criteria: rheumatoid arthritis, postoperative state of confusion. Location: Sweden. |
|
| Interventions | Intervention (n = 30) and control (n = 30) groups had a 20‐ to 40‐minute private information session with one of the investigators within 4 days of surgery. Information of a procedural nature was given verbally and in a leaflet. Participants were informed of postoperative pain measurements and showed how to use the VAS. Intervention group received additional specific information (verbally and in a leaflet) that emphasised the participant's role in pain management and explained the benefits of well‐treated postoperative pain for improving recovery and reducing complications. |
|
| Outcomes | Pain (VAS with scores ranging from 0 to 10 where a higher score represented worse pain, postoperative analgesics); satisfaction with pain management and nursing care; state and trait anxiety (5‐point Likert scale where a higher score represented greater anxiety); length of hospital stay. Participants were assessed preoperatively and 1, 2 and 3 days postoperatively. | |
| Notes | Trialists reported that "The mean length of hospitalisation was 11 days and it was the same for both groups". Attempts to retrieve missing SDs were unsuccessful. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "... the first patient was randomised to the treatment group and each subsequent following patient was altered (sic) allocated to either group." Comment: alternation is not a random method of generating a sequence. |
| Allocation concealment (selection bias) | High risk | Comment: unlikely that allocation was concealed using alternation. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Comment: no description of any attempt to blind participants and blinding is unlikely to have been possible. Knowledge of being in the intervention group may have influenced participants' pain measurements and satisfaction with care. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Quote: staff were aware that patients were taking part in a trial but "They were not informed that the patients were divided into two groups and participating in an intervention trial." Comment: staff assessed pain by getting participants to indicate their pain on the VAS and so it is possible that staff could have discovered which group a participant was in. The impact on the objective outcomes of staff being aware of group allocation is likely to be minor. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All the patients with postoperative patient controlled analgesia (PCA), two in the treatment group and one in the control group, were excluded from the analysis of analgesic use postoperatively due to their markedly higher use of opioids, leading to disturbances in the data." Comment: the number of participants excluded from the analyses and the reasons why are described in full. |
| Selective reporting (reporting bias) | High risk | Comment: all outcomes listed in the methods were reported in the results, but without the trial protocol, it is unclear whether any other outcomes were measured but not reported based on the results. Outcome data were only reported as medians and IQRs, so data were unable to be included in meta‐analyses. |
| Other bias | Low risk | Comment: no other sources of bias identified. |
Vukomanović 2008.
| Methods | Randomised parallel group trial. | |
| Participants | 45 participants undergoing total hip replacement. Intervention group: 14 women, 9 men (mean age 60 years, SD 11, range 30 to 70); control group: 16 women, 6 men (mean age 56 years, SD 18, range 19 to 70). Inclusion criteria: primary or secondary osteoarthritis, aged ≤ 70 years, ability to walk and climb stairs unaided. Exclusion criteria: none stated (see Notes). Location: Serbia. |
|
| Interventions | Intervention group (n = 23) were given a brochure and received intensive preoperative preparation from a physician (1 appointment) and physiotherapist (2 practical classes). The education covered the surgery and rehabilitation, including instruction in performing exercises and activities from the postoperative rehabilitation programme (e.g. getting out of bed, walking with crutches, etc.). Control group (n = 22) did not receive preoperative education or physiotherapy. |
|
| Outcomes | Pain (VAS (0‐100 points) higher score represented worse pain); range of motion; functional status (Harris Hip Score (maximum 100 points) 90‐100: good function and excellent results, 80‐90: good, 70‐80: fair, < 70: poor results; hip score of the Japanese Orthopaedic Association (JOA) (0‐80 points) higher score represented less dysfunction; and Oxford Hip Score (12‐60 points) higher score represented more dysfunction*); ability to perform 9 activities of daily living; length of hospital stay; days to stand or walk. Participants were assessed preoperatively, at discharge and 15 months postoperatively (Oxford Hip Score). | |
| Notes | *Oxford Hip Score data at 15 months included in Analysis 1.2, as this was the latest time point available in the trial report. No pre‐trial exclusion criteria stated but reasons for exclusion during the trial included intraoperative fracture or postoperative complications that compromised or delayed start of physiotherapy. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients were randomly divided into two groups." Comment: sequence generation not described. |
| Allocation concealment (selection bias) | Unclear risk | Comment: allocation concealment not described. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Comment: no description of any attempt to blind participants and blinding is unlikely to have been possible. Staff assessed functional status and evaluated the participant's ability to perform 9 basic activities but there is no description of whether any of the trial personnel or staff were blinded. Knowledge of being in the intevention group may have influenced participants' assessments of pain and functional status. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Comment: no description of blinding of trial personnel; length of stay could have been influenced by awareness of a participant's assignment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: 5 participants were excluded postoperatively (3 from intervention group, 2 from control group) due to complications during or following surgery. 4 participants were lost to follow‐up at 15 months (2 in each group). Impact of incomplete data likely to be minimal because outcomes are all continuous measures. |
| Selective reporting (reporting bias) | Unclear risk | Comment: all outcomes listed in the methods were reported in the results, but without the trial protocol, it is unclear whether any other outcomes were measured but not reported based on the results. |
| Other bias | Low risk | Comment: no other sources of bias identified. |
Wijgman 1994.
| Methods | Randomised parallel group trial. | |
| Participants | 64 participants undergoing total hip replacement (48 women, 16 men; mean age 65 years, range 42 to 85). Inclusion criteria: primary coxarthrosis confirmed by X‐ray. Exclusion criteria: pathological malformations (other than hip problems) that could interfere with rehabilitation. Location: Maastricht, Netherlands. |
|
| Interventions | Intervention group (n = 31) received preoperative instructions (30 minutes) in groups of 4‐6 delivered by 2 physiotherapists as well as preoperative exercise therapy including muscle‐setting exercises. Control group (n = 33) not described. |
|
| Outcomes | Days to mobilisation (standing, walking and climbing stairs); length of hospital stay; pain (medication). Participants were assessed preoperatively and 7, 10 and 14 days postoperatively. | |
| Notes | Publication is written in Dutch and was translated into English. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients... were divided at random..." Comment: sequence generation not described. |
| Allocation concealment (selection bias) | Unclear risk | Comment: method of allocation not described. |
| Blinding (performance bias and detection bias) Self‐reported outcomes | High risk | Comment: no description of any attempt to blind participants and blinding is unlikely to have been possible. |
| Blinding (performance bias and detection bias) Objective outcomes | Unclear risk | Comment: no description of blinding of trial personnel; mobilisation and length of stay could have been influenced by awareness of a participant's assignment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Adequate description of withdrawals. |
| Selective reporting (reporting bias) | Unclear risk | Comment: outcome data were only presented as box plots, and attempts to retrieve means and SDs were successful. All outcomes listed in the methods were reported in the results, but without the trial protocol, it is unclear whether any other outcomes were measured but not reported based on the results. |
| Other bias | Low risk | Comment: no other sources of bias identified. |
IQR: interquartile range; SD: standard deviation; SF‐36: 36‐item Short Form; VAS: visual analogue scale; WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Berge 2004 | Examined the effects of a pain management programme that was administered > 6 weeks prior to surgery. |
| Bondy 1999 | Studied the effects of anaesthetic patient education on preoperative anxiety. Although the participants were undergoing total hip replacements, the information was not specific to hip or knee replacement surgery. |
| Brull 2002 | Not a trial of preoperative education. Anxiety and depression were measured in a randomly selected group of participants undergoing elective hip or knee replacement with the aim of measuring the effects of preoperative anxiety and depression on postoperative recovery. |
| Ferrara 2008 | The preoperative intervention included only physiotherapy exercises; advice was delivered postoperatively. No additional education was provided. |
| Gammon 1996a | In addition to receiving preoperative education, participants in the intervention group were also exposed to a postoperative teaching programme before discharge. The trial was excluded because it was not possible to isolate the effects of the preoperative education. |
| Gill 2009 | The trial compared two preoperative exercise‐based programmes without a specific educational component. As participants were awaiting surgery at the time of the trial, all outcomes were measured only preoperatively. |
| Haslam 2001 | A trial to detect differences between acupuncture and advice/exercise in the symptomatic treatment of osteoarthritis of the hip. Participants were on a waiting list for hip replacement but did not have surgery as part of the trial. Advice given was not related to surgery for hip replacement. |
| Hough 1991 | Not a randomised trial. |
| Mancuso 2008 | The trial measured changes in patients' expectations of postoperative recovery. No outcomes were measured of relevance to the inclusion criteria of this review. |
| Mikulaninec 1987 | Preoperative instruction was of a general nature and not specific to hip or knee replacement. It was designed for people undergoing a range of general surgical procedures including abdominal, thoracic, perineal and orthopaedic surgery. |
| Nuñez 2006 | The intervention was delivered to people on the waiting list for knee replacement surgery. No surgery occurred during the trial period, and all outcomes were measured preoperatively. |
| Pour 2007 | The intervention and control groups received different postoperative rehabilitation and analgesia. The effects of the preoperative counselling intervention could not be determined. |
| Roach 1995 | Not a randomised trial. |
| Ródenas‐Martínez 2008 | In addition to preoperative education, the intervention group received more frequent postoperative physiotherapy than the control group. From postoperative measurements, the effects of the preoperative education intervention could not be determined. |
| Wong 1985 | The intervention combined preoperative instruction of rehabilitation exercises with postoperative behavioural strategies (including an alarm clock reminder to do exercises and verbal reinforcement from nurses). |
| Yeh 2005 | A quasi‐experimental design was used whereby "all subjects were not randomly assigned". To begin with, 33 participants were recruited to the control group, then a further 33 participants were recruited to the experimental group. |
Characteristics of studies awaiting assessment [ordered by study ID]
Eschalier 2012.
| Methods | Randomised trial. |
| Participants | 44 participants undergoing total knee replacement. |
| Interventions | Education booklet (n = 22) versus usually delivered information (n = 22). |
| Outcomes | Patient knowledge and beliefs (scores at inclusion to the trial, day before surgery and 6 weeks after surgery). Satisfaction score at final evaluation. |
| Notes | Study conducted in France. Reported as conference abstract. |
Huang 2012.
| Methods | Randomised trial. |
| Participants | 243 participants undergoing total knee replacement. |
| Interventions | Preoperative rehabilitation education programme started 2‐4 weeks before admission (n = 126) versus standard rehabilitation programme (n = 117). |
| Outcomes | Functional recovery, pain tolerance, length of stay, medical cost and post‐surgery complications. |
| Notes | Study conducted in Taiwan. |
Wilson 2012.
| Methods | Randomised trial. |
| Participants | 143 participants undergoing total knee arthroplasty. |
| Interventions | Individually delivered preoperative educational intervention (n = 73) versus usual care (n = 70). |
| Outcomes | Primary: pain‐related interference with activity. Secondary: pain, nausea, expected postoperative activity, analgesic and antiemetic in early postoperative period. |
| Notes | Study conducted in Ontario, Canada. PhD thesis. |
Characteristics of ongoing studies [ordered by study ID]
Riddle 2012.
| Trial name or title | KASTPain Trial. |
| Methods | 3‐arm randomised trial. |
| Participants | People scheduled for total knee arthroplasty. |
| Interventions | Group 1: 8 x 1‐hour sessions of 1‐to‐1 instruction delivered over a 2‐month period beginning about 2 weeks before surgery. Group 2: arthritis education sessions. Group 3: usual care. |
| Outcomes | Primary: function‐related pain. Secondary: self reported function, pain, global rating, walk test and physical performance. Cost measures: employment status, healthcare visits, inpatient admissions. |
| Starting date | Unknown. |
| Contact information | Daniel L Riddle: dlriddle@vcu.edu. Departments of Physical Therapy and Orthopaedic Surgery, Virginia Commonwealth University, Richmond, VA, USA. |
| Notes | Study conducted in 4 sites in US (Virginia, Illinois and North Carolina). |
Differences between protocol and review
In the previous version of this review (McDonald 2004), types of outcome measures included in the review were as follows:
postoperative pain (short‐ and long‐term);
length of hospital stay;
compliance with postoperative exercise routine;
patient satisfaction;
occurrence of postoperative deep vein thrombosis;
range of motion;
preoperative anxiety;
postoperative anxiety;
postoperative mobility.
The outcomes reported in this review have been modified from the original review to make them as consistent as possible with other Cochrane reviews on hip and knee replacement. Assessment for study risk of bias has been performed using The Cochrane Collaboration's 'Risk of bias' tool in this update of the review. We have included a 'Summary of findings' table and an ORBIT outcome matrix.
Contributions of authors
SM ran the searches. SM and KB assessed trials for inclusion. SM, MJP, KB and JW assessed risk of bias and extracted data. SM and MJP drafted the text of the review, and all authors contributed to interpreting the results and writing the discussion. AS commented on the text of the review and helped draft the discussion and implications for practice/research sections. Two authors of the first published version of this review (Sally Green and Sarah Hetrick) were not involved in this update.
Sources of support
Internal sources
Australasian Cochrane Centre, Australia.
External sources
No sources of support supplied
Declarations of interest
None known.
Deceased
Edited (no change to conclusions)
References
References to studies included in this review
Beaupre 2004 {published data only}
- Beaupre LA, Lier D, Davies DM, Johnston DBC. The effect of a preoperative exercise and education program on functional recovery, health related quality of life, and health service utilization following primary total knee arthroplasty. Journal of Rheumatology 2004;31(6):1166‐73. [PubMed] [Google Scholar]
Butler 1996 {published and unpublished data}
- Butler GS, Hurley CA, Buchanan KL, Smith‐VanHorne J. Prehospital education: effectiveness with total hip replacement surgery patients. Patient Education & Counseling 1996;29(2):189‐97. [DOI] [PubMed] [Google Scholar]
Clode‐Baker 1997 {published data only}
- Clode‐Baker E, Draper E, Raymond N, Haslam C, Gregg P. Preparing patients for total hip replacement. A randomized controlled trial of a preoperative educational intervention. Journal of Health Psychology 1997;2(1):107‐14. [DOI] [PubMed] [Google Scholar]
Cooil 1997 {published data only}
- Cooil J, Bithell C. Pre‐operative education for patients undergoing total hip replacement: a comparison of two methods. Physiotherapy Theory & Practice 1997;13(2):163‐73. [Google Scholar]
Crowe 2003 {published and unpublished data}
- Crowe J, Henderson J. Pre‐arthroplasty rehabilitation is effective in reducing hospital stay. Canadian Journal of Occupational Therapy ‐ Revue Canadienne d'Ergotherapie 2003;70(2):88‐96. [DOI] [PubMed] [Google Scholar]
Daltroy 1998 {published data only}
- Daltroy LH, Morlino CI, Eaton HM, Poss R, Liang MH. Preoperative education for total hip and knee replacement patients. Arthritis Care & Research 1998;11(6):469‐78. [DOI] [PubMed] [Google Scholar]
Doering 2000 {published and unpublished data}
- Doering S, Behensky H, Rumpold G, Schatz DS, Rossler S, Hofstotter B, et al. Videotape preparation of patients before hip replacement surgery improves mobility after three months. Zeitschrift Fuer Psychosomatische Medizin Und Psychotherapie 2001;47(2):140‐52. [DOI] [PubMed] [Google Scholar]
- Doering S, Katzlberger F, Rumpold G, Roessler S, Hofstoetter B, Schatz DS, et al. Videotape preparation of patients before hip replacement surgery reduces stress. Psychosomatic Medicine 2000;62(3):365‐73. [DOI] [PubMed] [Google Scholar]
Giraudet 2003 {published data only}
- Giraudet‐Le Quintrec J‐S, Coste J, Vastel L, Pacault V, Jeanne L, Lamas J‐P, et al. Positive effect of patient education for hip surgery. Clinical Orthopaedics and Related Research 2003;414:112‐20. [DOI] [PubMed] [Google Scholar]
Gocen 2004 {published data only}
- Gocen Z, Sen A, Unver B, Karatosun V, Gunal I. The effect of preoperative physiotherapy and education on the outcome of total hip replacement: a prospective randomized controlled trial. Clinical Rehabilitation 2004;18:353‐8. [DOI] [PubMed] [Google Scholar]
Johansson 2007 {published data only}
- Johansson K, Salantera S, Katajisto J. Empowering orthopaedic patients through preadmission education: results from a clinical study. Patient Education and Counseling 2007;66:84‐91. [DOI] [PubMed] [Google Scholar]
Lilja 1998 {published data only}
- Lilja Y, Ryden S, Fridlund B. Effects of extended preoperative information on perioperative stress: an anaesthetic nurse intervention for patients with breast cancer and total hip replacement. Intensive & Critical Care Nursing 1998;14(6):276‐82. [DOI] [PubMed] [Google Scholar]
McDonald 2004 {published data only}
- McDonald DD, Molony SL. Postoperative pain communication skills for older adults. Western Journal of Nursing Research 2004;26(8):836‐52. [DOI] [PubMed] [Google Scholar]
McGregor 2004 {published data only}
- McGregor AH, Rylands, H, Owen A, Dore CJ, Hughes SPF. Does preoperative hip rehabilitation advice improve recovery and patient satisfaction?. Journal of Arthroplasty 2004;19(4):464‐8. [DOI] [PubMed] [Google Scholar]
Santavirta 1994 {published data only}
- Santavirta N, Lillqvist G, Sarvimaki A, Honkanen V, Konttinen YT, Santavirta S. Teaching of patients undergoing total hip replacement surgery. International Journal of Nursing Studies 1994;31(2):135‐42. [DOI] [PubMed] [Google Scholar]
Siggeirsdottir 2005 {published data only}
- Siggeirsdottir K, Olafsson O, Jonsson H, Iwarsson S, Gudnason V, Jonsson B. Short hospital stay augmented with education and home‐based rehabilitation improves function and quality of life after hip replacement. Acta Orthopaedica 2005;76(4):555‐62. [DOI] [PubMed] [Google Scholar]
- Sigurdsson E, Siggeirsdottir K, Jonsson H Jr, Gudnason V, Matthiasson T, Jonsson BY. Early discharge and home intervention reduces unit costs after total hip replacement: results of a cost analysis in a randomized study. International Journal of Health Care Finance and Economics 2008;8(3):181‐92. [DOI] [PubMed] [Google Scholar]
Sjöling 2003 {published data only}
- Sjöling M, Nordahl G, Olofsson N, Asplund K. The impact of preoperative information on state anxiety, postoperative pain and satisfaction with pain management. Patient Education and Counseling 2003;51:169‐76. [DOI] [PubMed] [Google Scholar]
Vukomanović 2008 {published data only}
- Vukomanović A, Popović Z, Durović A, Krstić L. The effects of short‐term preoperative physical therapy and education on early functional recovery of patients younger than 70 undergoing total hip arthroplasty [Efekti kratkotrajne preoperativne fizikalne terapije i edukacije na rani funkcijski oporavak bolesnike mladih od 70 godina sa totalnom artroplastikom kuka]. Vojnosanitetski Pregled 2008;65(4):291‐7. [DOI] [PubMed] [Google Scholar]
Wijgman 1994 {published data only}
- Wijgman AJ, Dekkers GH, Waltje E, Krekels T, Arens HJ. No positive effect of preoperative exercise therapy and teaching in patients to be subjected to hip arthroplasty. Nederlands Tijdschrift Voor Geneeskunde 1994;138(19):949‐52. [PubMed] [Google Scholar]
References to studies excluded from this review
Berge 2004 {published data only}
- Berge DJ, Dolin SJ, Williams AC, Harman R. Pre‐operative and post‐operative effect of a pain management programme prior to total hip replacement: a randomized controlled trial. Pain 2004;110(1‐2):33‐9. [DOI] [PubMed] [Google Scholar]
Bondy 1999 {published data only}
- Bondy LR, Sims N, Schroeder DR, Offord KP, Narr BJ. The effect of anesthetic patient education on preoperative patient anxiety. Regional Anesthesia & Pain Medicine 1999;24(2):158‐64. [DOI] [PubMed] [Google Scholar]
Brull 2002 {published data only}
- Brull R, McCartney CJL, Chan VWS. Do preoperative anxiety and depression affect the quality of recovery and the length of stay after hip or knee arthroplasty. Canadian Journal of Anesthesia 2002;49(1):109. [DOI] [PubMed] [Google Scholar]
Ferrara 2008 {published data only}
- Ferrara PE, Rabini A, Maggi L, Piazzini DB, Logroscino G, Magliocchetti G, et al. Effect of pre‐operative physiotherapy in patients with end‐stage osteoarthritis undergoing hip arthroplasty. Clinical Rehabilitation 2008;22(10‐11):977‐86. [DOI] [PubMed] [Google Scholar]
Gammon 1996a {published data only}
- Gammon J, Mulholland CW. Effect of preparatory information prior to elective total hip replacement on post‐operative physical coping outcomes. International Journal of Nursing Studies 1996;33(6):589‐604. [DOI] [PubMed] [Google Scholar]
- Gammon J, Mulholland CW. Effect of preparatory information prior to elective total hip replacement on psychological coping outcomes. Journal of Advanced Nursing 1996;24(2):303‐8. [DOI] [PubMed] [Google Scholar]
Gill 2009 {published data only}
- Gill SD, McBurney H, Schulz DL. Land‐based versus pool‐based exercise for people awaiting joint replacement surgery of the hip or knee: results of a randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2009;90(3):388‐94. [DOI] [PubMed] [Google Scholar]
Haslam 2001 {published data only}
- Haslam R. A comparison of acupuncture with advice and exercises on the symptomatic treatment of osteoarthritis of the hip: a randomised controlled trial. Acupuncture in Medicine 2001;19(1):19‐26. [DOI] [PubMed] [Google Scholar]
Hough 1991 {published data only}
- Hough D, Crosat S, Nye P. Patient education for total hip replacement. Nursing Management 1991;22(3):80I‐80P. [DOI] [PubMed] [Google Scholar]
Mancuso 2008 {published data only}
- Mancuso CA, Graziano S, Briskie LM, Peterson MG, Pellicci PM, Salvati EA, et al. Randomized trials to modify patients' preoperative expectations of hip and knee arthroplasties. Clinical Orthopaedics and Related Research 2008;466(2):424‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mikulaninec 1987 {published data only}
- Mikulaninec CE. Effects of mailed preoperative instructions on learning and anxiety. Patient Education and Counselling 1987;10(3):253‐65. [DOI] [PubMed] [Google Scholar]
Nuñez 2006 {published data only}
- Nuñez M, Nuñez E, Segur JM, Macule F, Quinto L, Hernandez MV, et al. The effect of an educational program to improve health‐related quality of life in patients with osteoarthritis on waiting list for total knee replacement: a randomized study. Osteoarthritis and Cartilage 2006;14(3):279‐85. [DOI] [PubMed] [Google Scholar]
Pour 2007 {published data only}
- Pour AE, Parvizi J, Sharkey PF, Hozack WJ, Rothman RH. Minimally invasive hip arthroplasty: what role does patient preconditioning play?. Journal of Bone and Joint Surgery. American Volume 2007;89(9):1920‐7. [DOI] [PubMed] [Google Scholar]
Roach 1995 {published data only}
- Roach JA, Tremblay LM, Bowers DL. A preoperative assessment and education program: implementation and outcomes. Patient Education & Counseling 1995;25(1):83‐8. [DOI] [PubMed] [Google Scholar]
Ródenas‐Martínez 2008 {published data only}
- Ródenas‐Martínez S, Santos‐Andrés JF, Abril‐Boren C, Usabiaga‐Bernal T, Abouh‐Lais S, Aguilar‐Naranjo JJ. Effectiveness of a pre‐surgery rehabilitation program in total knee arthroplasty [Eficacia de un programa de rehabilitación preoperatoria en prótesis total de rodilla]. Rehabilitación 2008;42(1):4‐12. [Google Scholar]
Wong 1985 {published data only}
- Wong J, Wong S. A randomized controlled trial of a new approach to preoperative teaching and patient compliance. International Journal of Nursing Studies 1985;22(2):105‐15. [DOI] [PubMed] [Google Scholar]
Yeh 2005 {published data only}
- Yeh ML, Chen HS, Liu PH. Effects of multimedia with printed nursing guide in education on self‐efficacy wand functional activity and hospitalization in patients with hip replacement. Patient Education and Counseling 2005;57:217‐24. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Eschalier 2012 {published data only}
- Eschalier B, Descamps S, Pereira B, Girard MG, Boisgard S, Coudeyre E. Evaluation of a pre operative education approach for patient undergoing total knee replacement. Annals of Physical and Rehabilitation Medicine 2012;55:e117‐e8+e20. [Google Scholar]
Huang 2012 {published data only}
- Huang SW, Chen PH, Chou YH. Effects of a preoperative simplified home rehabilitation education program on length of stay of total knee arthroplasty patients. Orthopaedics & Traumatology: Surgery & Research 2012;98(3):259‐64. [DOI] [PubMed] [Google Scholar]
Wilson 2012 {published data only}
- Wilson RA. A randomized controlled trial of an individualized preoperative education intervention for symptom management following total knee arthroplasty. Dissertation Abstracts International: Section B: The Sciences and Engineering 2012;73(4‐B):2123. [Google Scholar]
References to ongoing studies
Riddle 2012 {published data only}
- Riddle DL, Keefe FJ, Ang D, J K, Dumenci L, Jensen MP, et al. A phase III randomized three‐arm trial of physical therapist delivered pain coping skills training for patients with total knee arthroplasty: the KASTPain protocol. BMC Musculoskeletal Disorders 2012;13:149. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Bastian 2002
- Bastian H, Cochrane Collaboration Consumer Network. Reducing anxiety before surgery, 2002. www.wagnerdiasresende.med.br/ANXIETY_SURGERY.htm (accessed 25 April 2014).
Brady 2000
- Brady OH, Masri BA, Garbuz DS, Duncan CP. Rheumatology: 10. Joint replacement of the hip and knee: when to refer and what to expect. Canadian Medical Association Journal 2000;163(10):1285‐91. [PMC free article] [PubMed] [Google Scholar]
Cates 2008 [Computer program]
- Cates C. Visual Rx 2.0 NNT Calculator. www.nntonline.net, 2008.
Creamer 1998
- Creamer P, Flores R, Hochberg MC. Management of osteoarthritis in older adults. Clinics in Geriatric Medicine 1998;14(3):435‐54. [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG. Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
DeFrances 2008
- DeFrances CJ, Lucas CA, Buie VC, Golosinskiy A. 2006 National Hospital Discharge Survey. National Health Statistics Reports 2008, issue 5:1‐20. [PubMed]
Dwan 2011
- Dwan K, Altman DG, Cresswell L, Blundell M, Gamble CL, Williamson PR. Comparison of protocols and registry entries to published reports for randomised controlled trials. Cochrane Database of Systematic Reviews 2011, Issue 1. [DOI: 10.1002/14651858.MR000031.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gammon 1996b
- Gammon J, Mulholland CW. Effect of preparatory information prior to elective total hip replacement on post‐operative physical coping outcomes. International Journal of Nursing Studies 1996;33(6):589‐604. [DOI] [PubMed] [Google Scholar]
Gummesson 2003
- Gummesson C, Atroshi I, Ekdahl C. The Disabilities of the Arm, Shoulder and Hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self‐rated health change after surgery. BMC Musculoskeletal Disorders 2003;4:11. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hathaway 1986
- Hathaway D. Effect of pre‐operative instruction on post‐operative outcomes: a meta‐analysis. Nursing Research 1986;35(5):269‐75. [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Johansson 2005
- Johansson K, Nuutila L, Virtanen H, Katajisto J, Salanterä S. Preoperative education for orthopaedic patients: systematic review. Journal of Advanced Nursing 2005;50(2):212‐23. [DOI] [PubMed] [Google Scholar]
Kirkham 2010
- Kirkham JJ, Dwan KM, Altman DG, Gamble C, Dodd S, Smyth R, et al. The impact of outcome reporting bias in randomised controlled trials on a cohort of systematic reviews. BMJ 2010;340:c365. [DOI] [PubMed] [Google Scholar]
Louw 2013
- Louw A, Diener I, Butler DS, Puentedura EJ. Preoperative education addressing postoperative pain in total joint arthroplasty: review of content and educational delivery methods. Physiotherapy Theory and Practice 2013;29(3):175‐94. [PUBMED: 23035767] [DOI] [PubMed] [Google Scholar]
NJR 2013
- NJR StatsOnline, National Joint Registry. www.njrcentre.org.uk (accessed 25 April 2014).
Oshodi 2007a
- Oshodi TO. The impact of preoperative education on postoperative pain. Part 1. British Journal of Nursing 2007;16(12):706‐10. [DOI] [PubMed] [Google Scholar]
Oshodi 2007b
- Oshodi TO. The impact of preoperative education on postoperative pain. Part 2. British Journal of Nursing 2007;16(13):790‐7. [DOI] [PubMed] [Google Scholar]
Page 2013
- Page MJ, McKenzie JE, Forbes A. Many scenarios exist for selective inclusion and reporting of results in randomized trials and systematic reviews. Journal of Clinical Epidemiology 2013;66(5):524‐37. [DOI] [PubMed] [Google Scholar]
Palmer 1999
- Palmer LM. Management of the patient with a total joint replacement: the primary care practitioner's role. Lippincott's Primary Care Practice 1999;3(4):419‐27. [PubMed] [Google Scholar]
RevMan 2012 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.2. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2012.
Ronco 2012
- Ronco M, Iona L, Fabbro C, Bulfone G, Palese A. Patient education outcomes in surgery: a systematic review from 2004 to 2010. International journal of evidence‐based healthcare 2012;10(4):309‐23. [PUBMED: 23173656] [DOI] [PubMed] [Google Scholar]
Savaridas 2013
- Savaridas T, Serrano‐Pedraza I, Khan SK, Martin K, Malviya A, Reed MR. Reduced medium‐term mortality following primary total hip and knee arthroplasty with an enhanced recovery program. A study of 4,500 consecutive procedures. Acta Orthopaedica 2013;84(1):40‐3. [PUBMED: 23368747] [DOI] [PMC free article] [PubMed] [Google Scholar]
Savović 2012
- Savović J, Jones HE, Altman DG, Harris RJ, Jüni P, Pildal J, et al. Influence of reported study design characteristics on intervention effect estimates from randomized, controlled trials. Annals of Internal Medicine 2012;157(6):429‐38. [DOI] [PubMed] [Google Scholar]
Schünemann 2011a
- Schünemann HJ, Oxman AD, Higgins JPT, Vist GE, Glasziou P, Guyatt GH. Chapter 11: Presenting results and 'Summary of findings' tables. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Schünemann 2011b
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, Guyatt GH. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Shuldham 1999
- Shuldham C. A review of the impact of pre‐operative education on recovery from surgery. International Journal of Nursing Studies 1999;36:171‐7. [DOI] [PubMed] [Google Scholar]
Song 2010
- Song F, Parekh S, Hooper L, Loke YK, Ryder J, Sutton AJ, et al. Dissemination and publication of research findings: an updated review of related biases. HealthTechnology Assessment 2010;14(8):1‐193. [PUBMED: 20181324] [DOI] [PubMed] [Google Scholar]
Sterne 2011
- Sterne JAC, Egger M, Moher D. Chapter 10: Addressing reporting biases. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Wallace 1986
- Wallace LM. Pre‐operative state anxiety as a mediator of psychological adjustment to and recovery from surgery. British Journal of Medical Psychology 1986;59:253‐61. [DOI] [PubMed] [Google Scholar]
Wallis 2011
- Wallis JA, Taylor NF. Pre‐operative interventions (non‐surgical and non‐pharmacological) for patients with hip or knee osteoarthritis awaiting joint replacement surgery ‐ a systematic review and meta‐analysis. Osteoarthritis and Cartilage 2011;19(12):1381‐95. [PUBMED: 21959097] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
McDonald 2004
- McDonald S, Hetrick SE, Green S. Pre‐operative education for hip or knee replacement. Cochrane Database of Systematic Reviews 2004, Issue Issue 1. [DOI: 10.1002/14651858.CD003526.pub2] [DOI] [PubMed] [Google Scholar]


