Abstract
Aims
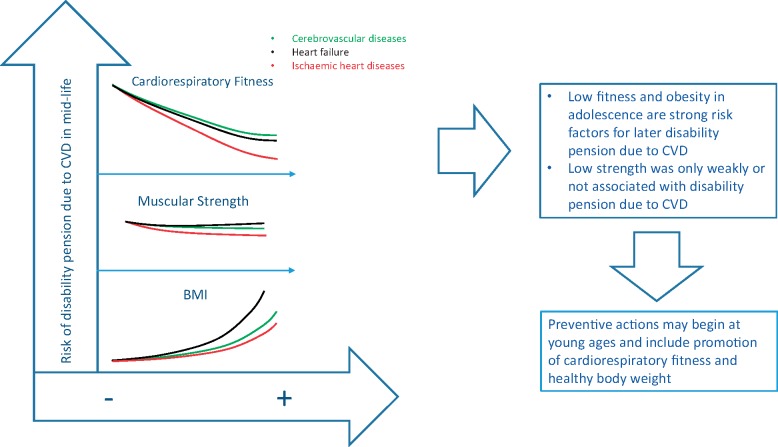
Cardiorespiratory fitness, muscular strength, and obesity in adulthood are risk factors for cardiovascular disease (CVD). However, little is known regarding the associations of these risk factors, already in adolescence, with later disability due to chronic CVD. Hence, we investigated associations of cardiorespiratory fitness, muscular strength, and body mass index (BMI) in adolescence with later chronic disability due to specific causes of CVD disability (i.e. cerebrovascular disease, ischaemic heart disease and heart failure).
Methods and results
This population-based cohort study included 1 078 685 male adolescents (16–19 years) from the Swedish military conscription register from 1972 to 1994. Cardiorespiratory fitness (bicycle ergometer test), muscular strength (knee extension strength), and BMI were measured during the conscription examination. Information about disability pension due to CVD was retrieved from the Social Insurance Agency during a mean follow-up of 28.4 years. Cardiorespiratory fitness was strongly and inversely associated with later risk of chronic CVD disability for all investigated causes. The association was particularly strong for ischaemic heart diseases (hazard ratio 0.11, 95% confidence interval 0.05–0.29 for highest vs. lowest fitness-quintiles). Furthermore, overweight/obesity were associated with CVD disability for all investigated causes. Conversely, associations of muscular strength with CVD disability were generally weak.
Conclusions
This study provides evidence for associations between low levels of cardiorespiratory fitness and obesity with later risk of chronic disability due to CVD. Preventive actions may begin at young ages and include promotion of cardiorespiratory fitness and healthy body weight.
Keywords: Cardiovascular disease, Cardiorespiratory fitness, Muscular strength, Obesity, Disability
See page 1511 for the editorial comment on this article (doi: 10.1093/eurheartj/ehz869)
Introduction
Cardiovascular (CV) disease (CVD) is a major cause of premature death and disability worldwide1 and therefore constitutes a major burden on societies. Identification of early preventable risk factors for later chronic disability due to CVD is therefore of great importance for prevention and early treatment.
Low levels of cardiorespiratory fitness and muscular strength are related to a higher risk of CVD.2–4 Importantly, cardiorespiratory fitness and muscular strength already in childhood are powerful predictors of CV health in youth and later in life.4–7 This is of great concern considering that low levels of physical activity, the major environmental determinant of cardiorespiratory fitness and muscular strength, have been reported in youth in high-income countries globally.8 We have previously examined cardiorespiratory fitness and muscular strength in adolescence in relation to later disability9,10 and found that low cardiorespiratory fitness, in particular, was a strong risk factor of later disability pension due to all causes and general categories, such as psychiatric disorders, musculoskeletal, injuries, nervous system, tumours, and circulatory causes. However, little is known regarding the associations of cardiorespiratory fitness and muscular strength in adolescence with later disability pension due to specific CVD diseases, such as cerebrovascular disease, ischaemic heart disease, and heart failure.
Furthermore, it is well-known that obesity11 established already in youth is related to early development of CVD. Obesity has also been associated with a higher risk of disability pension due to CVD,12 but it is unknown how obesity relates to the risk of later chronic disability due to specific causes of CVD. Moreover, it is of clinical and public health relevance whether cardiorespiratory fitness attenuates the association of obesity with later risk of disability pension due to specific causes of CVD. An objective and reliable way to study chronic disability due to CVD is to use data on disability pension, which is granted in many countries to individuals not being able to work full-time due to chronic disease. Clearly, disability pension in mid adulthood has a large impact on individuals and is also a great economic burden on societies.13
In this population-based study, we followed-up more than 1 million male participants from the Swedish Military Conscription Register to investigate the independent and combined associations of cardiorespiratory fitness, muscular strength, and body mass index (BMI), with later risk of disability pension due to cerebrovascular disease, ischaemic heart disease, and heart failure.
Methods
Study sample
The Swedish Multi-Generation Register was used to identify a population of males born in Sweden between 1951 and 1976 who performed conscription between 1972 and 1994. Linkage to the Swedish Military Conscription Register as well as other nation-wide registers was created by using the unique personal identification number which is assigned to all Swedish citizens at birth. The Cause of Death Register and the Registry of the Total Population was utilized to identify individuals who died or emigrated during follow-up. Conscription was mandatory by law for all young males in Sweden during the years covered by this study, and only 2–3% of adolescents (with severe chronic diseases) were exempted. Inclusion criteria in this study were age ≤19 years and availability of valid data on cardiorespiratory fitness, muscular strength, BMI, and confounders. Of the 1 125 739 adolescents who performed conscription, 42 178 had incomplete data on cardiorespiratory fitness and another 4433 males had missing data for muscular strength, BMI, and covariates or had extreme values for height, weight, and BMI, as described previously.12,14 Thus, the final sample consisted of 1 078 685 males. The study was approved by the Regional Ethics committee, Stockholm, Sweden and complies with the Declaration of Helsinki.
Baseline measurements
During the conscription examination, cardiorespiratory fitness was measured with a maximal workload test using a bicycle ergometer, as previously described.10 In short, each subject started with a warm-up, and the maximal workload (calculated as the highest power output in Watts) was thereafter measured by increasing the workload by 25 W per minute until exhaustion or when the prescribed pedalling rate could not be maintained. Muscular strength was also measured during conscription, using knee extension, handgrip, and elbow flexion strength, as previously described.9 In order to avoid presenting all the information in triplicate, the main analyses are shown for knee extension strength, which was generally the most powerful indicator of health-related muscular strength in our previous study.9 Briefly, knee extension strength was measured in Newtons, using an isometric dynamometer test performed at maximal contraction capacity, in a sitting position with 90° flexion over the main joint. Body mass index was calculated as weight (kg)/height squared (m2), using standardized height and weight measurements. Classification of BMI was performed according to World Health Organization (WHO) criteria (underweight <18.5 kg/m2, normal weight 18.5–24.9 kg/m2, overweight 25.0–29.9 kg/m2, obesity ≥30.0 kg/m2).
Disability pension
Date and cause of disability pension was retrieved from the Social Insurance Agency between the years of 1971–2012. During this time, men who were granted disability pension were assigned code for the cause of disability pension, which had to be confirmed by a physician, according to International Classification of Diseases (ICD) 8, 9, or 10. According to the Swedish law, a person may be granted disability pension if his/her working capacity is chronically reduced by at least 25% due to illness or injury. In the analysis, we used the primary ICD-code for the first disability pension event. Three major causes of disability pension due to CVD were studied: cerebrovascular disease, ischaemic heart disease, and heart failure. Supplementary material online, Table S1 shows the ICD codes for CVDs in this study.
Confounders
The following confounders were used in the study: childhood socioeconomic position based on parental occupation, age at conscription, conscription centre, and conscription year. Information about parental occupation was obtained from the Population and Housing Censuses from 1960 to 1990. Subsequently, childhood socioeconomic position was categorized into seven levels using the highest level of occupation of either parent.
Statistical analysis
Hazard ratios (HRs) and 95% confidence intervals (95% CIs) were estimated by means of Cox proportional hazards regression models. The men in the study were followed until they received disability pension, died, emigrated, or until the end of follow-up (31 December 2012). To investigate the associations of cardiorespiratory fitness and muscular strength with CVD disability, adolescents were classified into quintiles of cardiorespiratory fitness and muscular strength (cut-offs are shown in the footnotes of Table 1). In the combined analysis with cardiorespiratory fitness and BMI status (normal weight or obese), the lowest quintile of cardiorespiratory fitness was defined as unfit, whereas quintiles 2–5 were defined as fit according to previous studies.15 All models were adjusted for basic confounders, i.e. age, centre, year of conscription, childhood socioeconomic position, and BMI (when muscular strength and cardiorespiratory fitness were exposures). Subsequently, models were further adjusted for muscular strength and/or cardiorespiratory fitness. Adjustments for BMI, muscular strength, and cardiorespiratory fitness were conducted using continuous data. Proportional hazards assumption was verified with log–log plots and plots of Schoenfeld residuals. Statistical analyses were performed using SPSS Statistics 22 (IBM, Armonk, NY, USA) and Stata version 14.1 (Stata Corp, College Station, TX, USA).
Table 1.
Descriptive characteristics of the participants in the study (n = 1 078 685)
| Mean ± SD or % (n) | |
|---|---|
| Age at conscription | 18.32 ± 0.44 |
| Height (cm) | 179.3 ± 6.5 |
| Weight (kg) | 69.9 ± 10.3 |
| BMI (kg/m2) | 21.7 ± 2.8 |
| BMI categories | |
| Underweight (<18.5 kg/m2) | 8.1% (87 531) |
| Normal-weight (18.5–24.9 kg/m2) | 81.5% (879 045) |
| Overweight (25.0–29.9 kg/m2) | 8.7% (94 196) |
| Obesity (≥30.0 kg/m2) | 1.7% (17 913) |
| Cardiorespiratory fitnessa (W) | 275.2 ± 52.0 |
| Knee extension strengthb (N) | 573.7 ± 118.0 |
| Childhood SEP as indicated by highest occupation of parents | |
| Non-manual workers at higher level | 8.6% (92 332) |
| Non-manual workers at intermediate level | 21.2% (228 583) |
| Non-manual workers at lower level | 15.4% (166 231) |
| Self-employed or farmers | 7.4% (79 467) |
| Skilled workers | 32.7% (352 311) |
| Unskilled workers | 12.0% (129 334) |
| Others | 2.8% (30 427) |
BMI, body mass index; SEP, socioeconomic position.
Quintile 1 ≤ 229 W; Quintile 2 = 230–254 W; Quintile 3 255–284 W; Quintile 4 = 285–320 W; Quintile 5 ≥ 321 W.
Quintile 1 ≤ 470 N; Quintile 2 = 471–530 N; Quintile 3 = 531–590 N; Quintile 4 = 591–660 N; Quintile 5 ≥ 661 N.
Results
Characteristics of the 1 078 685 men in this study are presented in Table 1. Participants were followed for a maximum of 40.4 years (mean 28.4 ± 7.0 years, in total 30.6 million person-years) and during this time 2289 men were granted disability pension due to CVD. The most prevalent individual causes of CVD disability were cerebrovascular diseases (n = 1222) followed by ischaemic heart disease (n = 346) and heart failure (n = 147) (Supplementary material online, Table S1).
Cardiorespiratory fitness, muscular strength, and chronic cardiovascular disease disability
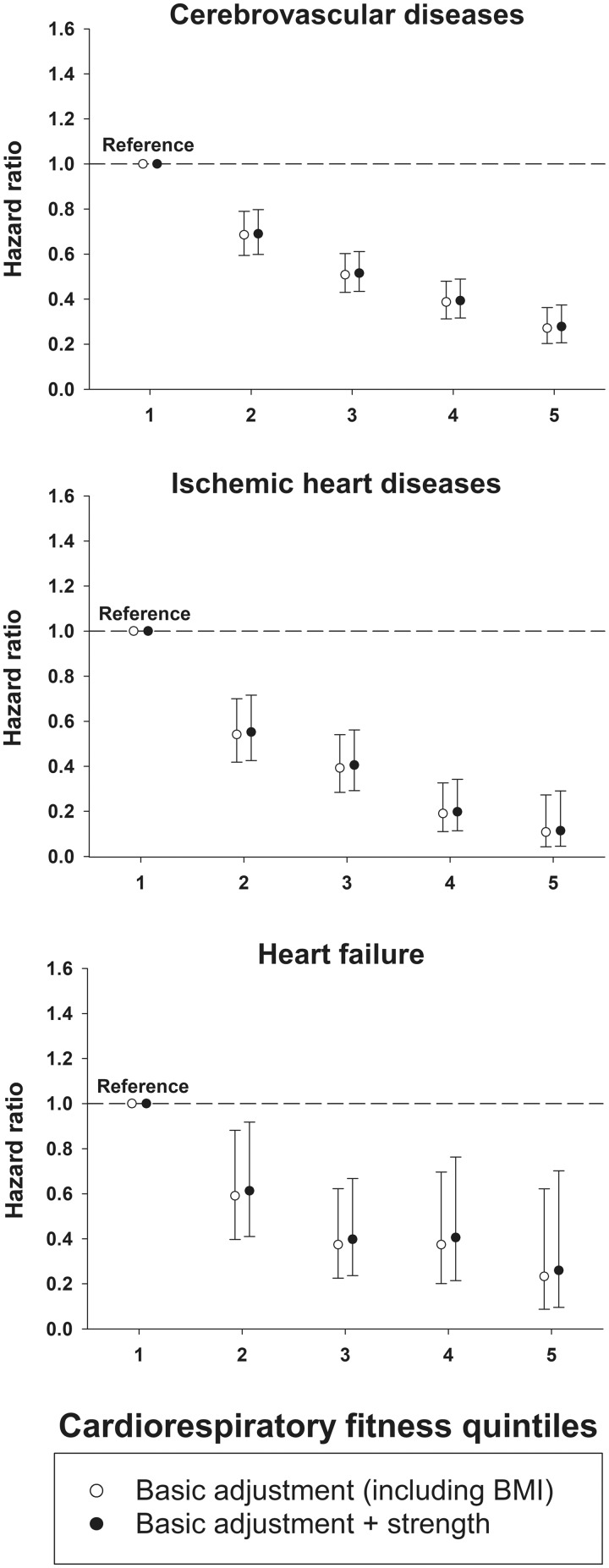
The associations of cardiorespiratory fitness at conscription with later chronic CVD disability are shown in Figure 1 (cumulative incidences in Supplementary material online, Figure S1). Higher cardiorespiratory fitness was associated with a lower risk of disability for all specific causes of CVD disability both in the basic models (including adjustment for BMI) and after additional adjustment for muscular strength. In the fully adjusted models, a higher cardiorespiratory fitness was associated with a lower risk of chronic disability due to cerebrovascular disease (HR 0.28; 95% CI 0.21–0.37 for highest vs. lowest cardiorespiratory fitness quintiles), ischaemic heart disease (HR 0.11; 95% CI 0.05–0.29), and heart failure (HR 0.26; 95% CI 0.10–0.70).
Figure 1.
Associations of cardiorespiratory fitness at conscription with later disability pension due to cardiovascular diseases (n = 1 078 685). Cox proportional hazards regression models were used to estimate hazard ratios with 95% confidence intervals. Basic adjustments in the analyses were age, centre, year of conscription, childhood socioeconomic position, and body mass index at conscription. Models were also further adjusted for muscular strength.
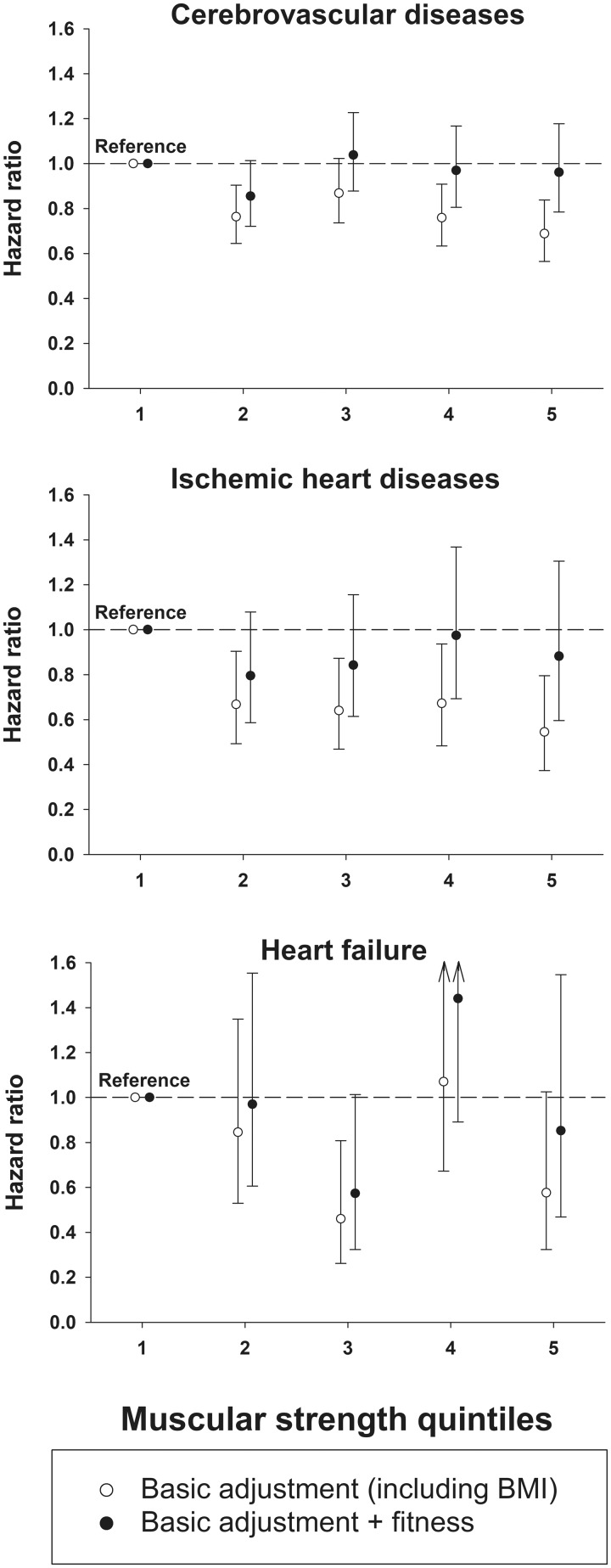
Figure 2 shows the corresponding associations of muscular strength at conscription with later chronic disability due to CVD (cumulative incidences in Supplementary material online, Figure S2). In the basic models, a higher muscular strength was associated with a lower risk of CVD disability, especially for cerebrovascular disease (HR 0.69; 95% CI 0.57–0.84 for highest vs. lowest muscular strength), and ischaemic heart disease (HR 0.55; 95% CI 0.37–0.80) for the highest vs. lowest quintile of muscular strength. However, the associations for muscular strength were generally weaker than for cardiorespiratory fitness (Figure 1) and did not reach statistical significance after further adjustment for cardiorespiratory fitness.
Figure 2.
Associations of muscular strength at conscription with disability pension due to cardiovascular diseases (n = 1 078 685). Cox proportional hazards regression models were used to estimate hazard ratios with 95% confidence intervals. Basic adjustments in the analyses were age, centre, year of conscription, childhood socioeconomic position, and body mass index at conscription. Models were also further adjusted for cardiorespiratory fitness.
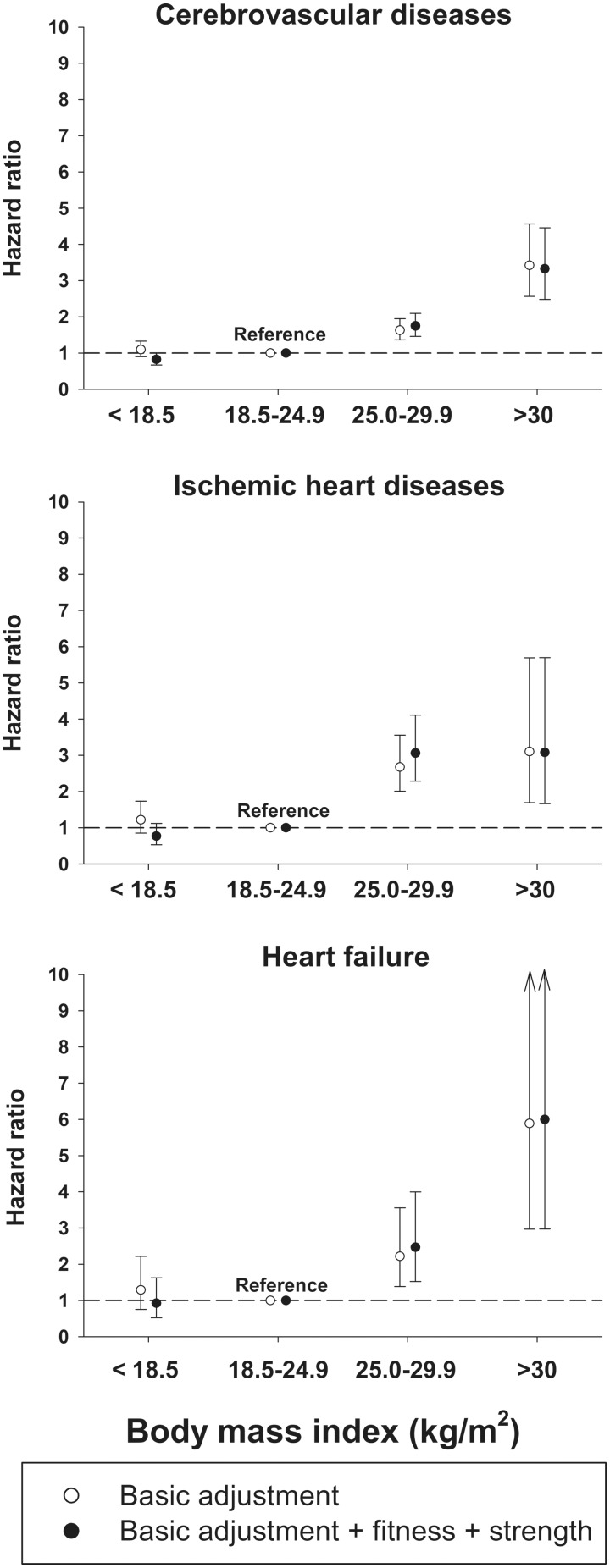
Body mass index and chronic cardiovascular disease disability
Associations of BMI at conscription with later chronic CVD disability are shown in Figure 3 (cumulative incidences in Supplementary material online, Figure S3). Obesity was associated with a greater risk of later CVD disability both in the basic models and after further adjustments for cardiorespiratory fitness and muscular strength. Thus, in the fully adjusted models, male adolescents with obesity were around 2.5 to 4 times more likely to be granted disability pension due to chronic cerebrovascular diseases and ischaemic heart disease (HRs between 2.47 and 4.35), and 6 times more likely due to heart failure (HR 6.00; 95% CI 2.97–12.11), compared to normal-weight adolescents.
Figure 3.
Associations of different body mass index categories at conscription with disability pension due to cardiovascular diseases (n = 1 078 685). Cox proportional hazards regression models were used to estimate hazard ratios with 95% confidence intervals. Basic adjustments in the analyses were age, centre, year of conscription, and childhood socioeconomic position. Models were also further adjusted for cardiorespiratory fitness and muscular strength.
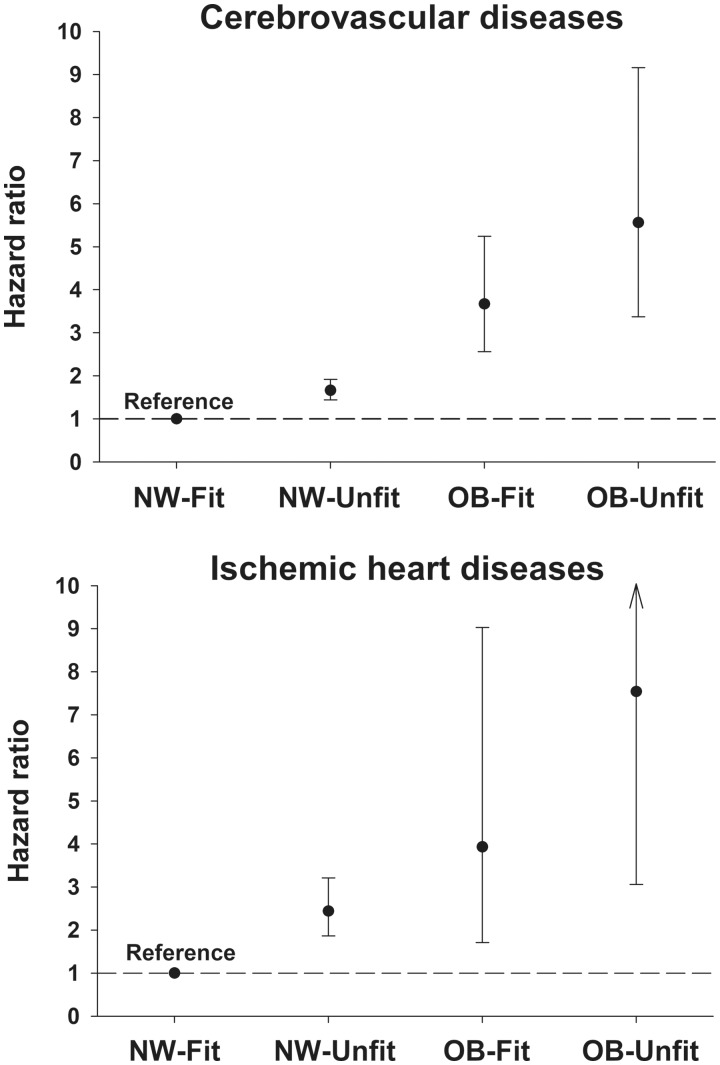
Combined associations of cardiorespiratory fitness and body mass index with chronic cardiovascular disease disability
The combined associations of cardiorespiratory fitness and BMI at conscription with later CVD disability due to cerebrovascular disease and ischaemic heart disease are presented in Figure 4 (combined analyses with heart failure had too few cases). There was a week, but statistically significant, correlation (r = 0.268, P < 0.001) between BMI (kg/m2) and cardiorespiratory fitness (W). A combination of a low cardiorespiratory fitness (i.e. first quintile) and obesity was strongly associated with a higher risk of chronic CVD disability for all investigated causes. The highest risk of disability pension was due to ischaemic heart disease for men who were both obese and unfit (HR 7.54; 95% CI 3.06–18.58). Being fit (cardiorespiratory fitness quintiles 2–5) attenuated the risk of chronic CVD disability for both normal weight and adolescents with obesity.
Figure 4.
Combined association of cardiorespiratory fitness and body mass index at conscription with disability pension due to cardiovascular diseases. NW, normal weight (n = 879 045); OB, obesity (n = 17 913). Adolescents with fitness in quintile 1 were considered as ‘Unfit’, while adolescents in quintiles 2–5 were considered ‘Fit’. Cox proportional hazards regression models were used to estimate hazard ratios with 95% confidence intervals. Models were adjusted for age, centre, year of conscription, childhood socioeconomic position, and muscular strength at conscription.
Sensitivity analyses
We conducted sensitivity analyses to assess the robustness of our findings. First, to further explore the shape of the associations with disability pension, we also used restricted cubic splines of cardiorespiratory fitness, muscular strength, and BMI, respectively (Supplementary material online, Figures S4–S6). Briefly, greater cardiorespiratory fitness and BMI were associated with lower risk of disability pension due to CVD, whereas associations for strength were considerably weaker. Second, in our analyses, we utilized the primary diagnosis for disability pension although some men (approximately 40%) also had a secondary ICD-code. Thus, we performed a sensitivity analysis in which we utilized both the first and secondary ICD-code, but conclusions were very similar to our main analyses. Third, we conducted stratified Cox regression models (based on 5-year-band on birth year), and results were very similar to our main results. Fourth, we conducted a sensitivity analysis in the individuals (n = 34 966) with data on smoking and alcohol consumption (these variables were only available in early years of the Swedish Conscription Registry, see Supplementary material online, Table S2). This analysis showed that low cardiorespiratory fitness (i.e. quartile 1) as compared to quartile 2–5 was a strong risk factors for disability pension due to cerebrovascular diseases and ischaemic heart disease even after adjustments for smoking and risky alcohol consumption at conscription. Finally, we assessed the robustness of the associations of cardiorespiratory fitness with disability pension by calculating E-values.16 As shown in Supplementary material online, Table S3, calculated E-values were generally high indicating robustness to residual confounding.
Discussion
Statement of principal findings
In this large population-based study, high cardiorespiratory fitness was strongly associated with lower risk of disability pension for all investigated specific causes of CVD disability, such as cerebrovascular disease, ischaemic heart disease, and heart failure and associations were robust to adjustments for BMI and muscular strength. Additionally, high muscular strength was also associated with a lower risk of chronic disability due to CVD, especially for cerebrovascular disease and ischaemic heart disease, but the associations were generally weaker than for cardiorespiratory fitness and did not persist after adjustment for cardiorespiratory fitness. Overweight, and particularly obesity, was associated with an increased risk of disability pension due to CVD for all investigated causes, even after adjustment for cardiorespiratory fitness and muscular strength. However, being fit appeared to attenuate the risk of disability pension for the investigated causes for both normal weight and adolescents with obesity.
Cardiorespiratory fitness, muscular strength, and chronic cardiovascular disease disability
There is substantial evidence supporting the impact of cardiorespiratory fitness for prevention17 treatment18 and as a predictor of later CVD.2,5,17–19 Previous studies, including our previous work,10 have reported that cardiorespiratory fitness in adolescence is associated with long-term risk of CVD events5 and disability pension due to all10,20 and circulatory causes.10 In the current study, we extend the existing literature by demonstrating that cardiorespiratory fitness is also predictive of later chronic disability due to specific causes of CVD, i.e. cerebrovascular disease, ischaemic heart disease, and heart failure. Furthermore, there is evidence for an inverse association between muscular strength and CVD later in life.7,21 Previous research and the result from this study indicate that the association of cardiorespiratory fitness with CVD may be stronger than for muscular strength.14,22 This could be due to the fact that cardiorespiratory fitness may represent a better indicator of the whole cardiovascular system than muscular strength and may be more strongly linked to CVD risk factors than muscle strength.23,24 In this study, muscular strength was measured at a single location (knee extension strength) and associations of muscular strength with health outcomes may be stronger in studies where muscle strength is assessed using multiple tests combining large muscle groups in the upper and lower body21 although further studies are needed. Comparison with previous studies are also complicated considering that this is, to the best of our knowledge, the first study to examine cardiorespiratory fitness and muscular strength in relation to disability pension due to specific causes of CVD.
It is not fully understood how cardiorespiratory fitness may be beneficial for CV health. However, high cardiorespiratory fitness has been associated with several CV adaptations which are favourable for healthy individuals, irrespective of age and sex.18 Cardiorespiratory fitness enhancing physical activity positively alters cardiac morphology, vasculature, and physiological performance; for example, increased end-diastolic diameter, increases in cardiac wall thickness, and less arterial stiffness.18 Moreover, higher intensities of physical activity from exercise training also attenuates declines in cardiac function associated with ageing.18
Body mass index and chronic cardiovascular disease disability: independent and combined associations with cardiorespiratory fitness
It is well-known that obesity in youth is related to CVD11,25 and also to the risk of disability pension.10,12,13 This study provides additional evidence of an association of overweight, and particularly obesity, with the risk of later chronic disability due to cerebrovascular diseases, ischaemic heart disease, and heart failure. In our study, a combination of low cardiorespiratory fitness and obesity jointly increased the risk of chronic CVD disability. This finding is in line with two studies which reported interactive effects of obesity and cardiorespiratory fitness on the risk of ischaemic heart disease19 and hypertension.14 Our findings expand the knowledge in the field to include combined associations of obesity and cardiorespiratory fitness on the risk of developing chronic CVD disability due to cerebrovascular diseases and ischaemic heart disease. Our findings also support the ‘fat but fit’ concept in relation to chronic CVD disability, since moderate to high levels of cardiorespiratory fitness (classified as fit) may attenuate the negative consequences of obesity on chronic CVD disability, supporting the evidence on the impact of cardiorespiratory fitness in obesity.15
Limitations and strengths
This study is based on military conscription data. Hence, one limitation is that we only have data for males in adolescence and their later risk of disability pension due to CVD. Thus, our results are relevant to men only and cannot be generalized to women. Furthermore, since ICD-codes from the Social Insurance Agency contained three-digit codes, we were only able to analyse relevant sub-chapters and diseases of the circulatory chapter of ICD rather than specific ICD-codes of four digits or more. Another important limitation is that we only had information regarding smoking and alcohol consumption during conscription for a sub-sample (n = 34 966) of adolescents in the study. However, our sensitivity analysis in this sample showed that low cardiorespiratory fitness remained associated with disability pension due to cerebrovascular diseases and ischaemic heart disease when adjusting for both smoking and risky alcohol consumption at conscription. Furthermore, our calculated E-values were generally high (≥6.35) indicating that a single unmeasured confounder would have to be associated with both cardiorespiratory fitness and disability pension by risk ratios of at least 6.35 to fully explain away the observed association.16 Although a single confounder of that magnitude is unlikely, future studies should consider the role of smoking, alcohol consumption, and other potential confounders, such as diet, in the association of cardiorespiratory fitness in youth with later CVD disability. Furthermore, it should be noted that the number of cases of CVD disability was relatively low since only chronic disabilities are granted disability pension and that the majority of the cohort were still relatively young at the end of follow-up (mean age: 47 years).
The main strengths of this study are the population-based study design and the large sample size allowing us to evaluate the risk of CVD disability for specific causes, in different BMI status categories and also to investigate the combined effect of cardiorespiratory fitness and BMI status on the risk of CVD disability. The population-based design also minimizes selection bias and non-response. Other strengths are that data on both cardiorespiratory fitness, muscular strength, and disability pension were objectively assessed and, therefore, the risk of bias as a result of self-reporting was avoided. Finally, cardiorespiratory fitness and muscular strength were measured in adolescence and CVD disability was assessed many years later. Since the prevalence of CVD is low in adolescence, this study design reduces the risk of reverse causation, i.e. reduced cardiorespiratory fitness and muscular strength due to CVD.
Clinical and public health implications
Cardiovascular disease remains a major cause of premature death and disability worldwide.1 The global burden of CVD (expressed as premature deaths, years of life lost, and years lived with disability) has continued to increase in the last decade even though age-standardized mortality has declined. Growth and ageing of the population contribute to this observed increase in burden of CVD.1,26 Consequently, disability pension due to CVD constitutes a major burden on societies, due to productivity losses,12,13 as well as on an individual level due to decreased quality of life.
Cardiovascular health is generally quite poor in contemporary youth.27,28 Since CVD risk factors track from childhood to adulthood,29 prevention of early risk factors is critical in order to achieve long-term CV health. The current study provides evidence for beneficial associations of cardiorespiratory fitness and risk of chronic CVD disability. A major concern is that only a small portion of contemporary youth meet the guideline recommendations of 60 min of moderate to vigorous physical activity per day.8 Although cardiorespiratory fitness has a fairly strong genetic component, low levels of physical activity is a major determinant of low cardiorespiratory fitness and may also explain increases in BMI over time.18,30 Therefore, increasing physical activity levels at young ages has the potential to have a large impact on long-term CV health. In this study, it can also be observed that adolescents with overweight and obesity had greater risk of chronic CVD disability later in life. Moreover, our results suggest that medium to high cardiorespiratory fitness may attenuate the increased risk of obesity on CVD disability, which points out the importance of high cardiorespiratory fitness levels also in individuals with obesity. Our results support the 2016 European Guidelines on CVD prevention in clinical practice which highlights the need to promote physical activity and healthy body weight already early in life for CVD prevention.31 There are cut points for youth to identify low levels of cardiorespiratory fitness to prevent CVD,32 and a recent American Heart Association statement claimed that measurement of cardiorespiratory fitness in clinical settings is both important and feasible.2 Hence, efforts to promote cardiorespiratory fitness and a healthy body weight may become a standard part of clinical encounters for early prevention of CVD (Take home figure).
Take home figure.
Association between risk factors at adolescence and disability pension due to cardiovascular disease in mid-life.
Conclusion
This large population-based study provides evidence for a strong association between low cardiorespiratory fitness in adolescence and later risk of chronic CVD disability due to cerebrovascular disease, ischaemic heart disease, and heart failure. Furthermore, overweight and particularly obesity was associated with an increased risk of chronic disability due to CVD for all investigated causes. Our study also supports that the increased risk of CVD disability observed in the presence of obesity can be at least partially attenuated by having a moderate to high cardiorespiratory fitness. Finally, although evidence of an association between muscular strength with CVD disability was found, this association was weaker than for cardiorespiratory fitness and BMI, and did not persist after adjustment for cardiorespiratory fitness. Altogether, our results suggest that preventive actions may begin at young ages and include promotion of cardiorespiratory fitness and healthy body weight, for long-term CV health and prevention of CVD disability.
Funding
This work was supported by the Karolinska Institutet to F.B.O (2018-02043). Furthermore, H.H. was supported by a grant from the Swedish Society of Medicine and the County Council of Östergötland, Sweden. P.H. was supported by grants from Henning and Johan Throne-Holst Foundation and the Strategic Research Area Health Care Science, Karolinska Institutet/Umeå University. F.B.O. was supported by a visiting grant from Henning and Johan Throne-Holst Foundation. Additional support was obtained from the European Union’s Horizon 2020 research and innovation programme under grant agreement No 667 302; the University of Granada Plan Propio de Investigación 2016-Excellence actions: Unit of Excellence on Exercise and Health (UCEES), and the Junta de Andalucía, Consejería de Conocimiento, Investigación y Universidades European Regional Development Fund (ERDF, SOMM17/6107/UGR); the SAMID III network, RETICS, funded by the PN I+D+I 2017-2021 (Spain), ISCIII-Sub-Directorate General for Research Assessment and Promotion (ERDF) (Ref. RD16/0022); and the EXERNET Research Network on Exercise and Health in Special Populations (DEP2005-00046/ACTI).
Conflict of interest: none declared.
Supplementary Material
References
- 1. Joseph P, Leong D, McKee M, Anand SS, Schwalm JD, Teo K, Mente A, Yusuf S.. Reducing the global burden of cardiovascular disease, Part 1: the epidemiology and risk factors. Circ Res 2017;121:677–694. [DOI] [PubMed] [Google Scholar]
- 2. Ross R, Blair SN, Arena R, Church TS, Després JP, Franklin BA, Haskell WL, Kaminsky LA, Levine BD, Lavie CJ, Myers J, Niebauer J, Sallis R, Sawada SS, Sui X, Wisløff U.. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation 2016;134:e653–e699. [DOI] [PubMed] [Google Scholar]
- 3. Smith JJ, Eather N, Morgan PJ, Plotnikoff RC, Faigenbaum AD, Lubans DR.. The health benefits of muscular fitness for children and adolescents: a systematic review and meta-analysis. Sports Med 2014;44:1209–1223. [DOI] [PubMed] [Google Scholar]
- 4. Ortega FB, Ruiz JR, Castillo MJ, Sjöström M.. Physical fitness in childhood and adolescence: a powerful marker of health. Int J Obes 2008;32:1–11. [DOI] [PubMed] [Google Scholar]
- 5. Hogstrom G, Nordstrom A, Nordstrom P.. Aerobic fitness in late adolescence and the risk of early death: a prospective cohort study of 1.3 million Swedish men. Int J Epidemiol 2016;45:1159–1168. [DOI] [PubMed] [Google Scholar]
- 6. Ruiz JR, Castro-Piñero J, Artero EG, Ortega FB, Sjöström M, Suni J, Castillo MJ.. Predictive validity of health-related fitness in youth: a systematic review. Br J Sports Med 2009;43:909.. [DOI] [PubMed] [Google Scholar]
- 7. Timpka S, Petersson IF, Zhou C, Englund M.. Muscle strength in adolescent men and risk of cardiovascular disease events and mortality in middle age: a prospective cohort study. BMC Med 2014;12:62.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Aubert S, Barnes JD, Abdeta C, Abi Nader P, Adeniyi AF, Aguilar-Farias N, Andrade Tenesaca DS, Bhawra J, Brazo-Sayavera J, Cardon G, Chang CK, Delisle Nyström C, Demetriou Y, Draper CE, Edwards L, Emeljanovas A, Gába A, Galaviz KI, González SA, Herrera-Cuenca M, Huang WY, Ibrahim IAE, Jürimäe J, Kämppi K, Katapally TR, Katewongsa P, Katzmarzyk PT, Khan A, Korcz A, Kim YS, Lambert E, Lee EY, Löf M, Loney T, López-Taylor J, Liu Y, Makaza D, Manyanga T, Mileva B, Morrison SA, Mota J, Nyawornota VK, Ocansey R, Reilly JJ, Roman-Viñas B, Silva DAS, Saonuam P, Scriven J, Seghers J, Schranz N, Skovgaard T, Smith M, Standage M, Starc G, Stratton G, Subedi N, Takken T, Tammelin T, Tanaka C, Thivel D, Tladi D, Tyler R, Uddin R, Williams A, Wong SHS, Wu CL, Zembura P, Tremblay MS.. Global matrix 3.0 physical activity report card grades for children and youth: results and analysis from 49 countries. J Phys Act Health 2018;15:S251–S273. [DOI] [PubMed] [Google Scholar]
- 9. Henriksson H, Henriksson P, Tynelius P, Ortega FB.. Muscular weakness in adolescence is associated with disability 30 years later: a population-based cohort study of 1.2 million men. Br J Sports Med 2018;53:1221–1230. [DOI] [PubMed] [Google Scholar]
- 10. Henriksson P, Henriksson H, Tynelius P, Berglind D, Löf M, Lee IM, Shiroma EJ, Ortega FB.. Fitness and body mass index during adolescence and disability later in life: a cohort study. Ann Intern Med 2019;170:230.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kelly AS, Barlow SE, Rao G, Inge TH, Hayman LL, Steinberger J, Urbina EM, Ewing LJ, Daniels SR.. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation 2013;128:1689–1712. [DOI] [PubMed] [Google Scholar]
- 12. Neovius M, Kark M, Rasmussen F.. Association between obesity status in young adulthood and disability pension. Int J Obes 2008;32:1319–1326. [DOI] [PubMed] [Google Scholar]
- 13. Neovius K, Johansson K, Rossner S, Neovius M.. Disability pension, employment and obesity status: a systematic review. Obes Rev 2008;9:572–581. [DOI] [PubMed] [Google Scholar]
- 14. Crump C, Sundquist J, Winkleby MA, Sundquist K.. Interactive effects of physical fitness and body mass index on the risk of hypertension. JAMA Intern Med 2016;176:210–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ortega FB, Lavie CJ, Blair SN.. Obesity and cardiovascular disease. Circ Res 2016;118:1752–1770. [DOI] [PubMed] [Google Scholar]
- 16. VanderWeele TJ, Ding P.. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med 2017;167:268–274. [DOI] [PubMed] [Google Scholar]
- 17. Swift DL, Lavie CJ, Johannsen NM, Arena R, Earnest CP, O'Keefe JH, Milani RV, Blair SN, Church TS.. Physical activity, cardiorespiratory fitness, and exercise training in primary and secondary coronary prevention. Circ J 2013;77:281–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lavie CJ, Arena R, Swift DL, Johannsen NM, Sui X, Lee D-C, Earnest CP, Church TS, O’Keefe JH, Milani RV, Blair SN.. Exercise and the cardiovascular system: clinical science and cardiovascular outcomes. Circ Res 2015;117:207–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Crump C, Sundquist J, Winkleby MA, Sundquist K.. Interactive effects of obesity and physical fitness on risk of ischemic heart disease. Int J Obes 2017;41:255–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rabiee R, Agardh E, Kjellberg K, Falkstedt D.. Low cardiorespiratory fitness in young adulthood and future risk of disability pension: a follow-up study until 59 years of age in Swedish men. J Epidemiol Community Health 2015;69:266–271. [DOI] [PubMed] [Google Scholar]
- 21. Ruiz JR, Sui X, Lobelo F, Morrow JR Jr, Jackson AW, Sjöström M, Blair SN.. Association between muscular strength and mortality in men: prospective cohort study. BMJ 2008;337:a439.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kim Y, White T, Wijndaele K, Westgate K, Sharp SJ, Helge JW, Wareham NJ, Brage S.. The combination of cardiorespiratory fitness and muscle strength, and mortality risk. Eur J Epidemiol 2018;33:953–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Steene-Johannessen J, Anderssen SA, Kolle E, Andersen LB.. Low muscle fitness is associated with metabolic risk in youth. Med Sci Sports Exerc 2009;41:1361–1367. [DOI] [PubMed] [Google Scholar]
- 24. Johannsen NM, Swift DL, Lavie CJ, Earnest CP, Blair SN, Church TS.. Combined aerobic and resistance training effects on glucose homeostasis, fitness, and other major health indices: a review of current guidelines. Sports Med 2016;46:1809–1818. [DOI] [PubMed] [Google Scholar]
- 25. Falkstedt D, Hemmingsson T, Rasmussen F, Lundberg I.. Body mass index in late adolescence and its association with coronary heart disease and stroke in middle age among Swedish men. Int J Obes 2007;31:777–783. [DOI] [PubMed] [Google Scholar]
- 26. Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, Moran AE, Sacco RL, Anderson L, Truelsen T, O'Donnell M, Venketasubramanian N, Barker-Collo S, Lawes CM, Wang W, Shinohara Y, Witt E, Ezzati M, Naghavi M, Murray C.. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet 2014;383:245–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shay CM, Gooding HS, Murillo R, Foraker R.. Understanding and improving cardiovascular health: an update on the American Heart Association's Concept of Cardiovascular Health. Prog Cardiovasc Dis 2015;58:41–49. [DOI] [PubMed] [Google Scholar]
- 28. Henriksson P, Henriksson H, Gracia-Marco L, Labayen I, Ortega FB, Huybrechts I, España-Romero V, Manios Y, Widhalm K, Dallongeville J, González-Gross M, Marcos A, Moreno LA, Castillo MJ, Ruiz JR.. Prevalence of ideal cardiovascular health in European adolescents: the HELENA study. Int J Cardiol 2017;240:428–432. [DOI] [PubMed] [Google Scholar]
- 29. Laitinen TT, Pahkala K, Magnussen CG, Viikari JS, Oikonen M, Taittonen L, Mikkilä V, Jokinen E, Hutri-Kähönen N, Laitinen T, Kähönen M, Lehtimäki T, Raitakari OT, Juonala M.. Ideal cardiovascular health in childhood and cardiometabolic outcomes in adulthood: the Cardiovascular Risk in Young Finns Study. Circulation 2012;125:1971–1978. [DOI] [PubMed] [Google Scholar]
- 30. Lavie CJ, Parto P, Archer E.. Obesity, fitness, hypertension, and prognosis: is physical activity the common denominator? JAMA Intern Med 2016;176:217–218. [DOI] [PubMed] [Google Scholar]
- 31. Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corrà U, Cosyns B, Deaton C, Graham I, Hall MS, Hobbs FDR, Løchen ML, Löllgen H, Marques-Vidal P, Perk J, Prescott E, Redon J, Richter DJ, Sattar N, Smulders Y, Tiberi M, van der Worp HB, van Dis I, Verschuren WMM, Binno S; ESC Scientific Document Group. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 2016;37:2315–2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ruiz JR, Cavero-Redondo I, Ortega FB, Welk GJ, Andersen LB, Martinez-Vizcaino V.. Cardiorespiratory fitness cut points to avoid cardiovascular disease risk in children and adolescents; what level of fitness should raise a red flag? A systematic review and meta-analysis. Br J Sports Med 2016;50:1451–1458. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.