Abstract
Purpose
To report, with the aid of original imaging, an unusual differential diagnosis of an iris tumor.
Observations
A 60-year-old Caucasian man visited our clinic with a large amelanotic iris mass in the left eye in the absence of concomitant extraocular inflammation or neoplastic evidence. The patient reported an ocular trauma caused by a wire 5 years prior to his visit, which resolved after a short course of antibiotic eye drops. Orbital magnetic resonance imaging with contrast enhancement was consistent with an iris tumor; ultrasound biomicroscopy indicated a semi-solid, mid-stromal iris formation continuous with the lens. Surgical inspection was performed. Surgery showed the presence of a hypermature cataract with a fine break in the anterior capsule of the lens covered by the iris surface. The liquefied cortex infiltrated the iris without diffusing into the aqueous humor.
Conclusions and Importance
A so-called morgagnian cataract developed, likely following a penetrating ocular wound. The progressive, slow infiltration of the iris stroma by the crystalline matrix mimicked the appearance of an amelanotic iris tumor.
Keywords: Cataract, Iris tumor, Ultrasound biomicroscopy
1. Introduction
An amelanotic or slightly pigmented iris mass is an uncommon finding, but usually indicates a benign or malignant tumor. In adult/elderly patients, differential diagnosis chiefly involves an iris melanoma versus rarer forms such as: secondary cysts (which may result from anterior segment surgery, prolonged use of miotics, metastasis, or parasites); leiomyoma, a benign smooth muscle tumor often located in the pupillary margin; inflammatory granulomas.1, 2, 3 Iris melanoma is a slow-growing tumor that typically presents during the fifth decade of life. Regarding pigmentation, amelanotic forms have been widely reported, although some residual pigmentation is usually present.4
A so-called morgagnian cataract, named after the Italian anatomist Giovanni B. Morgagni, is a form of hypermature cataract in which the brown sclerosed nucleus is present in a capsular bag filled by milky white, liquefied cortex. Quite common in the past, it is presently exceptionally rare in developed countries. We report a case of morgagnian cataract that involved clinical and instrumental differentiation from the abovementioned iris lesions.
2. Case report
A 60-year-old Caucasian male was referred to the eye clinic of the University Hospital of Parma for bilateral painless worsening of his vision that lasted for several months. The patient denied any systemic symptoms or disorders in his ocular history. He reported a wound in the left eye (LE) caused by a wire, which occurred 5 years prior and resolved with a short course of local therapy. At the first examination, the best-corrected visual acuity (BCVA) was 20/63 in the right eye (RE) and counting fingers at 50 cm in the LE; the intraocular pressures were 13 and 20 mmHg, respectively. The anterior segment of the RE was regular with slight lens cataract. A fundus examination showed an atrophic scar of the macular pigment epithelium, while optical coherence tomography (OCT), fluorescein, and indocyanine green angiography were suggestive of chronic central serous chorioretinopathy. This evidence, paired with the presence of an initial lens sclerosis, justified the limited BCVA in the RE.
Fig. 1 shows a slit-lamp image of the LE (different angles), which had two ovoid structures affecting about 180° of the inferior iris circumference. This mass pushed the iris surface forward to the corneal endothelium. Using ultrasound with 20- and 50-MHz probes, the lesion appeared to dissect the iris stroma with a mild/high echogenic outer layer, a fine “vacuolation” in the central part, and a hyporeflective inner layer (Fig. 2A and B). The iris root and the ciliary body were not significantly altered, and the lens showed a heterogeneous content but did not manifest capsule breaks. The anterior segment OCT allowed the visualization only of the cornea and of the anterior wall of the dilated iris structure, which stopped any further penetration of the examining infrared emission. The fundus was not directly observable. Magnetic resonance imaging (MRI) confirmed the presence of an iris deformation in the LE, with a size of 9 mm in width × 7 mm in height × 3 mm in depth, characterized by mild contrast enhancement (Fig. 3). Complementary blood tests and organ examinations to investigate possible inflammatory or infectious etiologies (chiefly sarcoidosis, syphilis, or tuberculosis), or to disclose possible systemic malignancies (i.e., chest computed tomography and abdominal B-ultrasound) were negative. Although the MRI was compatible with a nodular mass in the iris, the ultrasound indicated a mixed solid and liquid content. We suspected a morgagnian cataract as a potential diagnosis and planned surgical inspection/treatment with possible withdrawal for histological/cytological examination. Surgery confirmed the presence of a hypermature cataract with a fine anterior capsule break under the iris surface; the liquefied cortex infiltrated the iris without extending to the anterior chamber.
Fig. 1.
Slit-lamp appearance of the affected eye. In the left part of the image the whole mass in front view; in the right part the lateral view showing the contact between iris and cornea.
Fig. 2.
Ultrasound biomicroscopy with longitudinal positioning of the probe at seven o'clock: 50-MHz scan (A) and 20-MHz scan (B). In both scans: the yellow arrow marks the limbal border of the lesion; the green asterisk indicates the anterior wall of the iris mass; the cyan asterisk indicates the core of the lesion. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
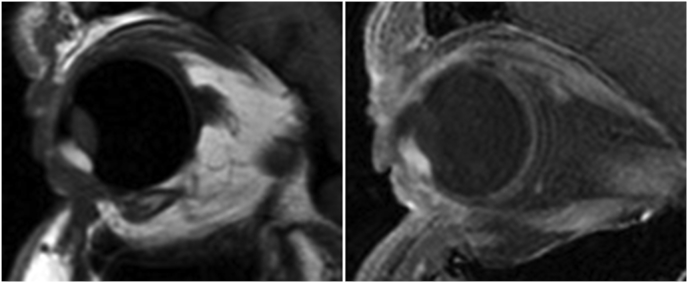
Fig. 3.
Magnetic resonance imaging (MRI) of the orbit in sagittal view. In the left part the T1-weighted imaging before contrast enhancement; in the right part after contrast-enhancement by a circumscribed area of the anterior chamber of the eye.
3. Discussion
Morgagnian cataracts were seen frequently in past centuries, whereas today patients require surgery at much earlier stages. However, this condition is still common in less-developed countries, where surgical treatment is not available and cataract represents a primary cause of blindness. In the present case, it is conceivable that the affected eye (i.e. the LE) experienced a prior decrease in visual acuity due to serous maculopathy. The ocular trauma was probably a pericorneal, self-sealing penetrating wound (actually, no leucomas were observable on the overall corneal surface) without residual intraocular foreign bodies. This event could have however damaged the lens capsule and triggered cataract progression. Only when noticeable visual loss was experienced also in the RE, the patient would have become aware of the symptoms. Surprisingly, the cataract grew directly into the iris stroma, thus distorting the appearance of the anterior segment but not leading to the classical complications of a morgagnian cataract, involving late evidence of a phacomorphic or phacolytic glaucoma and uveitis.5 The confounding clinical presentation, paired with its MRI appearance, compatible with that of an iris tumor, was challenging for diagnosis.6 To the best of our knowledge, a morgagnian cataract has never been included in the differential diagnosis of an iris mass.1,7,8 The usefulness of this case also addresses the confirmation of the role of ultrasound biomicroscopy (UBM) for the characterization of some anterior segment lesions and masses, mostly those developing into and behind the iris. In such cases optical coherence tomography of the anterior segment is often not fully informative.
Patient consent
The patient gave his written consent for the processing of personal data and images.
Declaration of competing interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Acknowledgments and Disclosures
The English in this document has been checked by at least two professional editors, both native speakers of English. For a certificate, please see: http://www.textcheck.com/certificate/UUV3uU.
References
- 1.Shields J.A., Sanborn G.E., Augsburger J.J. The differential diagnosis of malignant melanoma of the iris. A clinical study of 200 patients. Ophthalmology. 1983;90:716–720. doi: 10.1016/s0161-6420(83)34500-0. [DOI] [PubMed] [Google Scholar]
- 2.Georgalas I., Petrou P., Papaconstantinou D. Iris cysts: a comprehensive review on diagnosis and treatment. Surv Ophthalmol. 2018;63:347–364. doi: 10.1016/j.survophthal.2017.08.009. [DOI] [PubMed] [Google Scholar]
- 3.Rouberol F., Duquesne N., Kodjikian L. Sarcoid granuloma simulating amelanotic melanoma of the iris: a case report. J Fr Ophtalmol. 2002;25:831–834. [French] [PubMed] [Google Scholar]
- 4.Pick Z.S., Wilson G.A. Tapioca melanoma of the iris. Clin Exp Optom. 2009;92:154–156. doi: 10.1111/j.1444-0938.2008.00344.x. [DOI] [PubMed] [Google Scholar]
- 5.Lezrek O., Belhadj O., Jaja Z. Post-traumatic morgagnian cataract. J Fr Ophtalmol. 2016;39:322–323. doi: 10.1016/j.jfo.2015.09.014. [French] [DOI] [PubMed] [Google Scholar]
- 6.Shields C.L., Di Nicola M., Bekerman V.P. Iris melanoma outcomes based on the American joint committee on cancer classification (eighth edition) in 432 patients. Ophthalmology. 2018;125:913–923. doi: 10.1016/j.ophtha.2017.11.040. [DOI] [PubMed] [Google Scholar]
- 7.Jongebloed W.L., Kalicharan D., Los L.I. The Morgagnian and Brunescens cataract morphology studied with with SEM and TEM. Eur J Morphol. 1993;31:97–102. [PubMed] [Google Scholar]
- 8.Deshmukh S., Bhattacharjee H., Gupta K. Triangle sign" in Morgagnian cataract. Indian J Ophthalmol. 2019;67:137. doi: 10.4103/ijo.IJO_940_18. [DOI] [PMC free article] [PubMed] [Google Scholar]