Abstract
Objectives:
This pilot study aimed to evaluate the effect of a sedentary behaviour (SB) reduction intervention (Stomp Out (Prolonged) Sitting (SOS)) in frail older adults.
Methods:
Participants (>65years) were recruited from sheltered housing complexes and randomized into 2 groups. On weeks 2, 6 and 10 both groups had face-to-face 40min motivational sessions, including feedback on physical function and SB. One group had the addition of real-time tactile feedback on sitting. Total sedentary time and patterns of SB were recorded by activPAL, along with validated measures of function: Timed Up and Go (TUG), Sit-to-Stand (STS) and balance tests. Outcomes were analyzed by intention-to-treat mixed model analysis.
Results:
Twenty-three participants started the SOS intervention. Health issues led to high attrition in this frail population. TUG (4 seconds faster) and STS (>2 rises more in 30 seconds) scores improved significantly in both groups. There were no significant changes in SB parameters.
Conclusion:
Motivational interviewing alongside functional test feedback, visual and real-time feedback on SB improved physical function over the study. This pilot study suggests that sit-to-stand transitions to break prolonged sitting time may help reduce frailty and functional decline in people who are often unable to engage in more intense exercise interventions.
Keywords: Sedentary Behavior, Sitting Time, Physical Function, Frailty, Older Adults
Introduction
The aim of health and social care policy in the UK is to support people to live healthier independent lives at home, which are, as far as possible, focused on prevention and early management[1,2]. In epidemiological studies, high levels of sitting time have been linked with frailty, falls and poor physical function and those older adults (OA) who break their sitting time more frequently have better physical function[3]. Frailer OA may potentially have more to gain from reducing sedentary time than younger, or more able adults, if there is the potential for functional gains without the higher energy expenditure of more formal exercise sessions, which are often considered unachievable in this group[4].
Sedentary behaviour (SB) is defined by both posture (sitting or reclining) and low energy expenditure (<1.5 Metabolic Equivalent of Task (METS)) during waking hours[5]. OA spend 65-80% of the waking day sedentary[6] which has a deleterious effect on metabolism, health and physical function[7,8]. Not all sitting is detrimental, therefore it is important to aim SB interventions at times in the day when SB is passive or non-purposeful and in the context of other tasks of the 24 hour day[9].
Interventions that are primarily aimed at changing sitting time, rather than combined with increasing physical activity, are thought to be the most successful at reducing sitting time[10]. Reducing SB, along with having its own benefits, may be an “entry level” intervention to engage OA in moving more often and towards their optimal physical activity potential by embedding small bouts of functional training within their daily routine. To date, interventions designed for OA aimed at reducing SB have asked the participants to set goals[11-15] or provided an information booklet with tips and tasks[16] over a period of 12 weeks or less. SB has been reported using objective measures (activPAL (AP)[12-14], ActiGraph[11] or Sense WearPro[15]) and self-report[15-16]. Results are mixed and only two studies observed functional outcomes.
Rosenberg et al. (2015) found a small positive effect on gait speed as a result of an 8 week programme to reduce SB in community dwelling older adults[13]. Barone Gibbs et al. (2017) found a small positive effect on Chair Sit-to-Stand Test (STS), but not on objectively measured SB[15]. Frail OA are underserved in SB intervention studies. Only Matei et al. (2015)[16] included older adults living in sheltered housing and this group was unable to positively change their sitting time, recorded by self-report.
It is recognised that interventions to change behaviour are complex and there is no clear approach to achieving behaviour change in OA[17]. Behavioural feedback is useful as it allow the participant to reflect on their behaviour. The activPAL-VTaP (VT) (PAL Technologies: www.paltechnologies.com) is an AP activity monitor unit with the additional facility of being able to provide real-time tactile feedback to the user on their sitting time by way of a vibration prompt. It was not known whether real-time feedback could have an effect on reducing SB in older adults. The aim of this randomized pilot trial was to examine the use of both real-time and retrospective SB feedback alongside functional feedback during motivational sessions and determine its effect on objectively measured SB and physical function in frailer older adults living in sheltered housing.
Materials and methods
Study design
The study was a two-arm randomized pilot study. Participants were recruited from Sheltered Housing Complexes in Glasgow (8 sites managed by 3 Sheltered Housing Associations and participants from Glasgow Caledonian University (GCU) Older Adults Database). Participants were randomized (random number table) before baseline assessments into either the AP or VT group. Data was collected between April 2013 and June 2014. The GCU School of Health and Life Sciences Ethical Committee gave approval (HLS12/59) and all participants gave written informed consent. Inclusion and exclusion criteria can be found in [Table 1]. The study is presented according to the Template for Intervention Description and Replication (TIDieR) guidelines (Appendix 1)[18]. A target of 25 participants was set as this was estimated to detect a 4% reduction in sitting time with (80%, alpha 0.05), to allow for attrition we aimed to recruit 35 participants.
Table 1.
Inclusion and exclusion criteria.
| Inclusion | Exclusion |
|---|---|
| 65+ years of age | Allergy to adhesive tape (for fixing the AP/VT to the thigh) |
| Medically Stable | Any acute or uninvestigated medical conditions. |
| Living in Sheltered Housing | |
| Independently Ambulatory (with or without a walking aid) | |
| Score <7 in the 6-CIT (Cognitive Impairment Test)‡ | |
| Able to achieve 100 degrees of hip flexion in both hips from a sitting and lying position (required to turn off VT equipment). | |
| Have intact vibro-tactile sensation on the thigh (assessed by neurothesiometer). |
Brooke P, Bullock R: Validation of a 6 item cognitive impairment test with a view to primary care usage. Int J Geriatr Psychiatry 1999; 14 (11): 936-40.
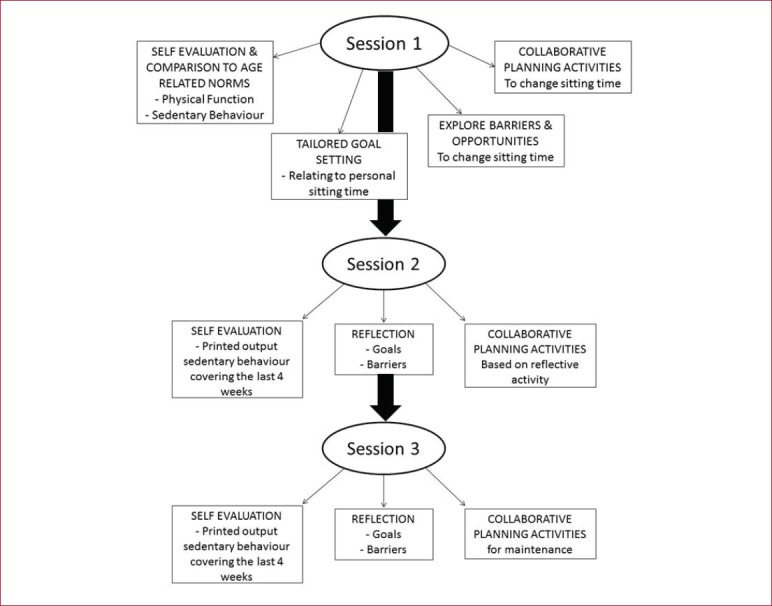
Intervention: Motivational session and retrospective feedback (AP)
During the study all participants received three 40 min face-to-face sessions with retrospective feedback every 4 weeks. The intervention was based on: the Transtheoretical Model[19]; previous intervention studies[11,20]; discussion with Sheltered Housing Support Officers; lifelogging contextual work and qualitative interviews with older adults[9,21]. A support pack was produced to ensure each participant received the same basic information and could refer to the pack between visits (Appendix 2).
Intervention: Addition of real-time feedback (VT)
The VT group, in addition to motivational sessions and retrospective feedback, received real-time feedback. VT parameters were set to meet each individual participants needs, relating to collaborative goals set during the intervention programme. Therefore, the time between the prompts (vibrations) differed from individual to individual along with the reset time. The reset time defines the time in upright activity required to restart the sitting timer. The participants could turn off the reminder at any time. It was also possible for the participants to choose to change prompt parameters.
Data collection
The study took place over a 14 week period including: baseline; 3 motivational sessions (Weeks 2, 6, 10); 4 weeks follow-up (Week 14), where the vibration was removed from the VT units. One researcher (an experienced Physiotherapist) provided the intervention and collected the data at the participant’s home. From week 1 of the study onwards, participants were asked to wear the AP/VT activity monitor 24 hours a day. The monitor was applied by the researcher on day one of the study. After 7 days the first set of data was retrieved and the second monitor was applied to the opposite leg. At baseline the participants completed the functional tests and questionnaires about their health, well-being, physical activity and SB[11,22]. These outcomes were repeated post study and at follow-up by the researcher un-blinded to the intervention group.
Functional performance testing
Validated functional tests were employed: Chair Sit-and-Reach for flexibility[23]; 30 secs STS for lower limb strength[24]; Timed Up and Go (TUG)[25] for mobility and falls risk; balance was assessed by a Balance Screening Tool[26]. All test are commonly used in Physiotherapy practice and have published ‘normal values’, this allowed the participants to compare their results to age related normal values during session 1. Where it was thought that the test was beyond the participant’s ability, or they declined to take part, that element of testing was omitted.
Sedentary behaviour measurement by activity monitoring
The AP inclinometer is a thigh mounted objective monitor shown to be a highly accurate method of measuring sitting posture in OA[27,28]. The AP/VT monitors were covered in medical grade waterproof packets. On the visits the monitors were applied to the mid–thigh using an adhesive pad (‘activPAL Stickie’), this was then covered with a hypoallergenic tape (Opsite Fexifix). The participants were instructed to remove the monitor and telephone the researcher if any adverse event occurred. The monitor also displayed the wording ‘activity monitor’ and a contact number in case the monitor was lost or the user was in a situation where they were unable to explain its purpose.
Data processing
The SB data was analyzed using the data from the activity monitors following the protocol of Chastin and Granat (2010)[29]. The variables analyzed were total sedentary time and patterns of SB. To avoid a daily participant burden of keeping a sleep diary over the study period, waking day SB was assessed by the following protocol: the start of the day was defined as the first stand/step after 06.30 hrs; the end of the day was defined by the step/stand before the first sit/lie after 22:00 hrs; if there was no sit/lie commencing between 22:00 hrs and 23:59 hrs the end of day will be defined at the point of the last stand/step before 22:00 hrs. To determine validity of this protocol this was compared to sleep diaries self-reported by the participants at the baseline week.
Statistical analysis
Data were analyzed using IBM SPSS 22 software. Total sitting time is expressed as a percentage of the waking day (SB Ratio). Fragmentation is a measure of patterns of sitting, where the number of bouts of sitting time per hour of the day is divided into total sitting time (b/hr). We analyzed the data as intention-to-treat (ITT) mixed model analysis (MMA) to assess the effectiveness of the intervention to: a) improve physical function and b) to change SB. All participants that started week one were included in the analysis. In each model there was a repeated measurement of the participants’ outcomes. The model takes into consideration the factor of the group and the covariant of time for each of the dependent variables (SB or functional outcomes). As others authors had reported a diminished intervention effect with time[11,13,16], we developed a MMA to examine the effect of day of the week i.e. day 1 being the first day following the intervention period, and so on, along with week of the month in order to understand the longitudinal effect.
Results
Recruitment & retention of participants
Recruitment was difficult and retention was low, reflecting the frailty of the older adults recruited in the study. As can be seen from [Figure 1], there were 2 phases of recruitment and the most common reason for withdrawal was participants’ health status.
Figure 1.
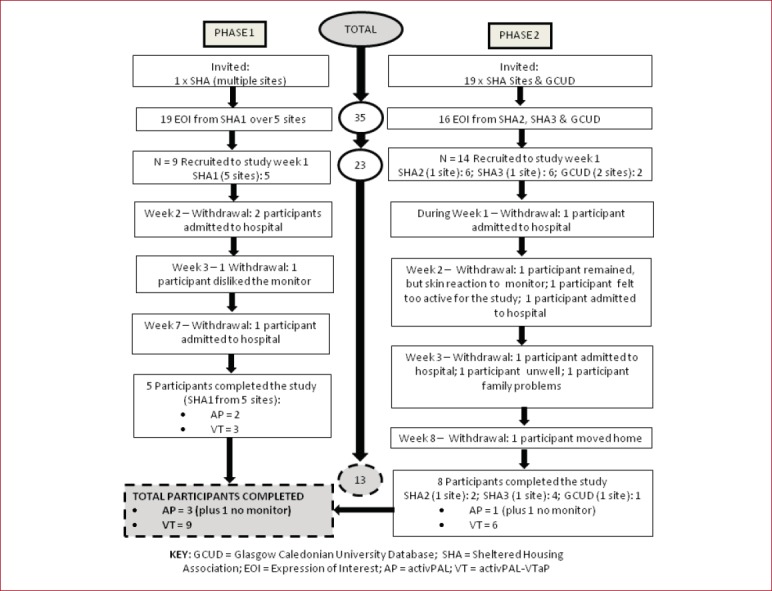
Consort Diagram for SOS Study.
Descriptive statistics
Twenty-three participants (17 female; mean age: 78.8±8.1; 12 VT group) were recruited and started week 1 (Figure 1). The majority of participants were female and despite randomization there were baseline differences in the groups (Table 2). The average waking day recording period was 14.0±0.2 hrs, this correlated well with the finding of the baseline sleep diaries (mean sleep reported=9.5±0.9 hrs, therefore 14.5 hrs remain as the waking period, N=15). Thirteen participants remained to the end of the study (one without AP monitor), representing 56.5% retention.
Table 2.
Descriptive statistics at baseline.
| Baseline Test | VT Group | N | AP Group | N |
|---|---|---|---|---|
| Sex (% female) | 67 | 12 | 67 | 11 |
| Age (years, Mean (SD)) | 74.0±6.1 | 12 | 83.2±7.7 | 11 |
| BMI (kg/m2, Mean (SD)) | 28.3±7.2 | 11 | 26.3±4.9 | 10 |
| No. of Medications | 5.3†† | 12 | 6.5†† | 11 |
| No. educated >HS | 3 | 12 | 0 | 11 |
| Timed Up & Go (sec, Mean (SD)) | 26.6±7.1†† | 11 | 29.8±16.1†† | 5 |
| Employed | 0 | 12 | 0 | 11 |
| EuroQoL(score/5)† | 1.6 | 12 | 1.5 | 11 |
| >1 Fall /last year (%) | 50†† | 12 | 63.6†† | 11 |
| Widow (%) | 16.7 | 12 | 54.5 | 11 |
| Single (%) | 16.7 | 12 | 36.4 | 11 |
| Divorced (%) | 33.3 | 12 | 0 | 11 |
| Married (%) | 33.3 | 12 | 9.1 | 11 |
= The European Quality of Life Questionnaire (EQ-5D-5L) average scores of self-reported: mobility, self-care, daily activities, pain, anxiety and depression collated;
= indication of frailty; BMI = Body Mass Index from self-reported height/weight; HS = High School.
Intention-to-treat
When the ITT MMA is applied to the physical function data (Figure 2), the VT groups had better physical function throughout the study. There were changes over time for both AP and VT groups. There was a significant effect of group and time for TUG test and a significant effect of time only was found in the STS test. The 1 leg stand test and 180° turn test had a significant group effect. As can be seen from [Figure 2], there was no significant effect found for group or time with SB ratio, SB fragmentation or flexibility.
Figure 2.
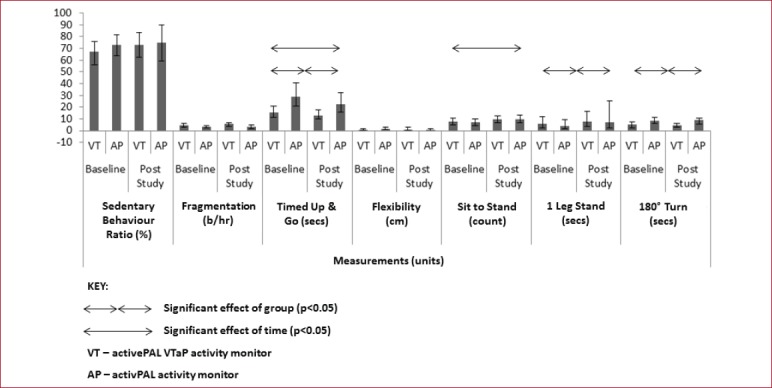
Marginal Mean (CI) of sedentary behaviour and function outcomes (N=23) as intention-to-treat mixed model analysis.
When the ITT MMA was applied to time periods, there was a significant effect of day (number of days after the intervention). As can be seen from [Figure 3], there is a pattern of sedentary accumulation where an initial post intervention drop is observed (after each motivation session) followed by increase, then a second smaller drop. There was no significant effect of group, week or day and week, with sedentary ratio data. When the MMA of fragmentation of SB was examined, the only significant effect was group with the VT group showing more fragmentation. There was no significant effect of day, week, or day and week on fragmentation.
Figure 3.
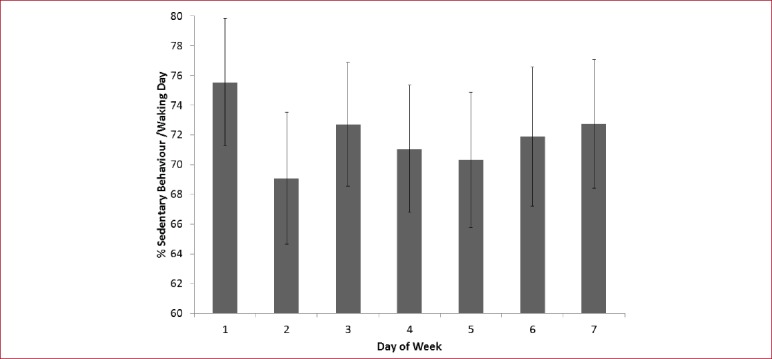
Marginal mean (CI) sedentary ratio by day (N=23). The figure examines the week after the motivational session has been delivered and combines each of the post-session days over the period of the study.
Adverse reactions
One participant (AP group) had a skin irritation under the area of the activity monitor and was unable to continue wearing the monitor from week 2, but remained in the study (minus activity monitor feedback).
Discussion
An intervention aimed at decreasing and breaking up long periods of SB, thus encouraging small bouts of functional training (i.e. rising from a chair) little, often, daily, maybe more risk averse and acceptable to frailer OA than formal exercise training. The older adults recruited for the SOS study were frail evidenced by the health-related drop-out, fall history, daily medication use and baseline TUG scores. Post study, both groups made favorable and clinically important gains in physical function suggesting the SOS intervention increased the participants’ ability to mobilize from a chair (TUG 4 secs faster and 2 more STS in 30 secs).
These findings are comparable to other studies of younger OA with better physical function at baseline where a small, but significant, positive effect was found in gait speed[13] and STS score[15]. Barone Gibbs et al.[15] study compared a “Sit Less” group to a “Get Active” group. Interestingly, the “Sit Less” group made functional gains that the “Get Active” group did not make despite a significant increase in their moderate to vigorous intensity physical activity (MVPA). The functional tests used have a ceiling effect, therefore, the frailer the start point, the more gain there is available to make. Regularly breaking up sitting is an activity intervention in itself, with the true effect of exercise by stealth through repeated sit-to-stands, rather than exercising only in ‘sessions’ and potentially sitting more in between.
Although there were no significant changes in sedentary time, fragmentation tended to improve for the VT group over time. It would seem that breaking up periods of prolonged sitting, more than total sedentary time, was easier for the older adults to gain and sustain change overtime, but only with the use of the vibrational prompts. There is also diminished effect as time progresses from the point of intervention. Both this study and Gardiner et al.[9] noted weekly behavioural patterns where OA appear to make positive changes in the first few post intervention days, followed by a negative change in the subsequent days, followed by a second, smaller, move towards positive change. This patterning may be due to fatigue or compensation and merits further investigation to both ensure the interventions are appropriate and sustainable[30].
The SOS study was a long-term intervention study with face-to-face monthly interventions, where individuals activity monitor and physical function feedback was discussed and appropriate collaborative goals were set. Other intervention studies aimed at reducing SB, tend to focus on the outcomes of SB and/or physical activity[11-16] and, to the authors knowledge, have not considered discussing participants own physical function as a motivational tool, this is therefore a novel component of the SOS study worth considering in future studies. Interestingly, a pilot study of the Functional Fitness MOT where functional normative data feedback and physical activity advice was given, found that OA expressed more interest in breaking up prolonged sitting, than in seeking out physical activity opportunities[31]. Frailer OA valued the face-to-face intervention of the SOS study[32] and it would appear that information booklets only are not sufficient to instigate self-reported sedentary change in those living in sheltered housing[16].
The SOS pilot study is limited by its small sample size, high attrition rates in this frail group, so was consequently underpowered to detect changes in SB. The study assessments were carried out by one researcher, not blinded to group allocation as the observations formed part of the intervention. A large RCT that addresses these limitations, with a longer follow up, is warranted.
For OA living in sheltered housing, it is appropriate to provide tailored advice to recommend reducing SB, as this will improve their sit-to-stand transfer and ability to mobilize. This study provided participants feedback on, and assessed, their physical function, along with their SB. It is recommended that future intervention studies should measure effects on function in this frail group and consider using functional feedback as a motivational tool. The novel use of the real-time feedback is also worth further investigation, although the SOS study did not unequivocally demonstrate its benefit across all outcomes.
In conclusion, it is hard to recruit and retain frailer OA to long-term RCT studies, but this vulnerable group may have the most to gain from reducing SB, thus is worth perseverance of the research and clinical communities to engage these individuals. Even in this frailer group, with a large health related drop-out, there was a significant improvement in functional ability, suggesting overall the SOS intervention had positive functional effects on frailer OA, despite no measurable change in SB.
Acknowledgements
With thanks to the residents and staff of the sheltered housing complexes that participated in this study.
Appendix 1.
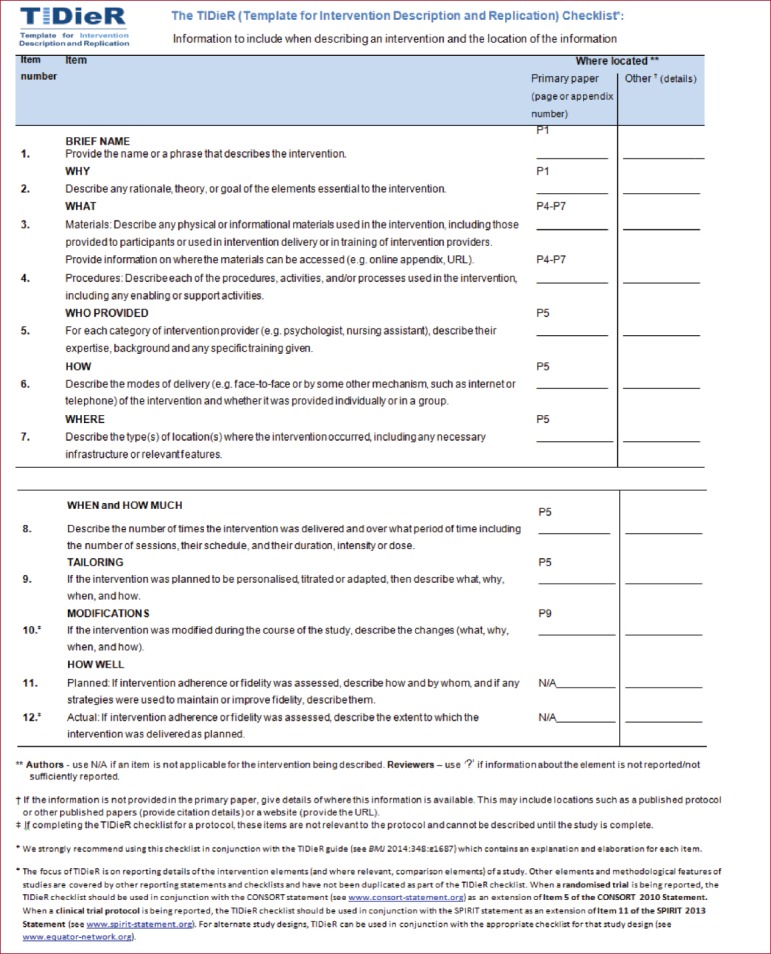
The TIDieR Checklist (page numbers relate to the originally submitted manuscript).
Appendix 2.
The support pack was personalized to each individual and included self-completing sections, thus allowing the participants to have a sense of responsibility and control over their behaviour (the intervention pack is available here: https://sedentaryblethering.files.wordpress.com/2017/07/sos-intervention-pack-juliet-harvey.pdf).
Footnotes
Edited by: Yannis Dionyssiotis
Ethical Approval
Glasgow Caledonian University Ethical Committee (Reference Number: HLS12/59).
Funding
This work was supported by Glasgow Caledonian University studentship and Scottish Innovation Voucher Scheme.
Contributors
All authors participated in the conception of this study, interpretation of the results and reviewed the manuscript. JH carried out recruitment, the intervention and data collection, analysis and writing of the manuscript.
References
- 1.Scottish Government 2017 Allied Health Professions Co-Creating Wellbeing with the People of Scotland The Active and Independent Living Programme in Scotland. [Accessed online (09/09/17)]. http://www.gov.scot/Publications/2017/06/1250 .
- 2.NHS England 2017 AHPs into Action:Using Allied Health Professionals to transform health, care and wellbeing. [Accessed online (09/09/17)]. https://www.england.nhs.uk/wp-content/uploads/2017/01/ahp-action-transform-hlth.pdf .
- 3.Sardinha LB, Santos DA, Silva AM, et al. Breaking-up Sedentary Time Is Associated With Physical Function in Older Adults. J Gerontol A Bio Sci Med Sci. 2015;70(1):119–124. doi: 10.1093/gerona/glu193. [DOI] [PubMed] [Google Scholar]
- 4.Manini T, Carr LJ, King AC, et al. Interventions to reduce sedentary behavior. Med Sci Sport Exerc. 2015;47(6):1306–1310. doi: 10.1249/MSS.0000000000000519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tremblay MS, Aubert S, Barnes JD, et al. Sedentary Behaviour Research Network (SBRN) Terminology Consensus Project process and outcome. Int J Nutr Phys Act. 2017;14:75. doi: 10.1186/s12966-017-0525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harvey JA, Chastin SFM, Skelton DA. How Sedentary are Older People:A Systematic Review of the Amount of Sedentary Behavior. J Aging Phys Act. 2015;23:471–87. doi: 10.1123/japa.2014-0164. [DOI] [PubMed] [Google Scholar]
- 7.de Rezende LFM, Rey-Lόpez JP, Matsudo VKR, et al. Sedentary behaviour and health outcomes among older adults:a systematic review. BMC Public Health. 2014;14:333. doi: 10.1186/1471-2458-14-333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reid N, Healy GN, Daly RM, et al. 12-year Television Viewing Time Trajectories and Physical Function in Older Adults. Med Sci Sport Exerc. 2017;49(7):1359–1365. doi: 10.1249/MSS.0000000000001243. [DOI] [PubMed] [Google Scholar]
- 9.Leask CF, Harvey JA, Skelton DA, et al. Exploring the context of sedentary behavior in older adults (what, where, why, when and with whom) Euro Rev Aging Phys Act. 2015;12:4. doi: 10.1186/s11556-015-0146-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martin A, Fitzsimons C, Jepson R, et al. Interventions with potential to reduce sedentary time in adults:systematic review and meta-analysis. Br J Sports Med. 2016;49(16):1056–1063. doi: 10.1136/bjsports-2014-094524. [DOI] [PubMed] [Google Scholar]
- 11.Gardiner PA, Eakin EG, Healy GN, et al. Feasibility of Reducing Older Adults'Sedentary Time. Am J Prev Med. 2011;41(2):174–177. doi: 10.1016/j.amepre.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 12.Fitzsimons CF, Alison K, Baker G, et al. Using individualised consultations and activPAL feedback to reduce sedentary time in older Scottish adults:Results of a feasibility and pilot study. Prev Med. 2013;57:718–720. doi: 10.1016/j.ypmed.2013.07.017. [DOI] [PubMed] [Google Scholar]
- 13.Rosenberg DE, Gell NM, Jones SMW, et al. The feasibility of reducing sitting time in overweight and obese older adults. Health Educ Behav. 2015;42(5):669–76. doi: 10.1177/1090198115577378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lewis LK, Rowlands AV, Gardiner PA, et al. Small Steps:Preliminary effectiveness and feasibility of an incremental goal-setting intervention to reduce sitting time in older adults. Maturitas. 2016;85:64–70. doi: 10.1016/j.maturitas.2015.12.014. [DOI] [PubMed] [Google Scholar]
- 15.Barone Gibbs B, Brach JS, Byard T, et al. Reducing Sedentary Behaviour Versus Moderate -to-Vigorous Intensity Physical Activity in Older Adults:A 12-week randomized clinical trial. J Aging Health. 2017;29(2):247–267. doi: 10.1177/0898264316635564. [DOI] [PubMed] [Google Scholar]
- 16.Matei R, Thune-Boyle I, Hamer M, et al. Acceptability of a theory-based sedentary behaviour reduction intervention for older adults ('On Your Feet to Earn Your Seat') Public Health. 2015;15:606. doi: 10.1186/s12889-015-1921-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Michie S, Richardson M, Johnston M, et al. The Behaviour Change Technique Taxonomy (V1) of 93 Hierarchically Clustered Techniques:Building an International Consensus for the Reporting of Behaviour Change Interventions. Ann Behav Med. 2013;46:89–95. doi: 10.1007/s12160-013-9486-6. [DOI] [PubMed] [Google Scholar]
- 18.Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions:Template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687. doi: 10.1136/bmj.g1687. [DOI] [PubMed] [Google Scholar]
- 19.Prochaska JO, DiClemente CC, Norcross JC. In Search of the Structure of Change;in Klar Y, Fisher J, Chinsky JM, Nadler:Self Change. Springer New York. 1992:87–114. [Google Scholar]
- 20.British Heart Foundation:National Centre for Physical Activity and Health 2014, The Functional Fitness MOT Programme Impact Assessment 2014. Accessed online (12/09/16) http://www.laterlifetraining.co.uk/wp-content/uploads/2012/04/MOT-impact-assessment.pdf .
- 21.Harvey JA, Chastin SFM, Skelton DA. Acceptability of novel lifelogging technology to determine context of sedentary behaviour in older adults. AIMS:Public Health. 2016;3(1):158–71. doi: 10.3934/publichealth.2016.1.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.EuroQoL:The European Quality of Life Questionnaire (EQ-5D-5L) EuroQoL Executive Office, Rotterdam, The Netherlands. [Accessed online (05/03/13)]. http://www.euroqol.org/about-eq-5d.html .
- 23.Jones CJ, Rikili RE, Max J, et al. The Reliability and Validity of a Chair Sit-and-Reach Test as a Measure of Hamstring Flexibility in Older Adults. Res Q Exerc Sport. 1998;69(4):338–343. doi: 10.1080/02701367.1998.10607708. [DOI] [PubMed] [Google Scholar]
- 24.Jones CJ, Rikli RE, Beam WC. A 30-s Chair-Stand Test as a Measure of Lower Body Strength in Community-Residing Older Adults. Res Q Exerc Sport. 1999;70(2):113–119. doi: 10.1080/02701367.1999.10608028. [DOI] [PubMed] [Google Scholar]
- 25.Podsiadlo D, Richardson S. The timed “Up &Go”:a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 26.Mackintosh S, Datson N, Frayer C. A balance screening tool for older people:Reliability and Validity. Int J Ther Rehabil. 2006;13(12):558–561. [Google Scholar]
- 27.Taraldsen K, Askim T, Sietvold U, et al. Evaluation of a body-worn sensor system to measure physical activity in older people with impaired function. Physical Therapy. 2011;91:277–285. doi: 10.2522/ptj.20100159. [DOI] [PubMed] [Google Scholar]
- 28.Lord S, Chastin S, McInnes L, et al. Exploring patterns of daily physical and sedentary behaviour in community dwelling older adults. Age Ageing. 2010;40:205–10. doi: 10.1093/ageing/afq166. [DOI] [PubMed] [Google Scholar]
- 29.Chastin SFM, Granat MH. Methods for objective measure, quantification and analysis of sedentary behaviour and inactivity. Gait Posture. 2010;31(1):82–86. doi: 10.1016/j.gaitpost.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 30.Murphy SL, Smith DM. Ecological Measurement of Fatigue and Fatigability in Older Adults with Osteoarthritis. J Gerontol A Bio Sci Med Sci. 2010;65A(2):184–189. doi: 10.1093/gerona/glp137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.de Jong LD, Peters A, Chalmers N, et al. Views of older adults and allied health professionals on the acceptability of the Functional Fitness MOT:a Mixed-Method Feasibility Study. In press PLOS One. 2017 [Google Scholar]
- 32.Harvey JA, Chastin SFM, Skelton DA. SOS Study:Stomp Out (prolonged) Sitting in Frailer Older Adults Pilot Intervention Study:Objective Effects and Perceived Strategies and Effects. J Aging Phys Act. 2016;(Suppl 24):S92. [Google Scholar]


