Abstract
Chronic Kidney Disease (CKD) is known to be an important risk factor for accidental, low-energy falls especially among elder individuals. The high incidence of falls is a major cause of morbidity and mortality with a substantial annual cost. Patients suffering from CKD are more prone to fall and develop fractures than the general population. Multiple risk factors have been identified and analyzed in order to explain this fact, such as drug combination, diabetes mellitus, orthostatic hypotension, vitamin D deficiency, sarcopenia and anemia, all very common in CKD. In this mini review of published evidence, we tried to search and present a complete aspect of the problem called ‘Falls in Chronic Kidney Disease’, focusing especially on the risk factors, discussing each one separately and its association with low- energy falls. Concluding, we discuss potential therapies and treatment goals based on the pathophysiology of CKD and accidental falls and propose new fields of investigation.
Keywords: Chronic kidney disease, Accidental falls, End stage renal disease, Hemodialysis
Introduction
It is estimated that approximately one third of the general population beyond the age of 65 years suffers from at least one fall every year[1-3] whereas half of them falls repeatedly[3,4]. This percentage increases to 35% after the age of 75 years[4]. Falls and their complications are the fifth leading cause of death in the developed world[5] with substantial cost[6]. More specifically in the United States the total cost of the fall-related fractures exceeds $US10 billions[7]. Patients on hemodialysis are on greater risk of falling and fall- related complications[3,8]. Moreover, they have a three to four times greater risk for hip fractures compared to the general population[8,9]. The morbidity and mortality are higher in the hemodialysis population[6] and in peritoneal dialysis patients as well[10].
Definition of the fall
In order to evaluate the incidence and complications of a fall it is important to determine the exact definition of this term. There are differences between the definition of a fall given by health care providers and seniors. More specifically, seniors focus on the consequences of the fall and associate the loss of balance to the incidence, whereas health care providers talk about the fall event itself[11]. Both groups tend to include in the definition only injurious events with the risk of disregarding non-injurious falls. Thus, it is recommended that a definition of a fall is provided to patients when asked if they have fallen or not[11].
Fall-related injuries
According to a prospective cohort study that included hemodialysis patients, the proportion of falls that needed medical attention was 19%, with the majority of injuries being minor (bruises and lacerations). A 7% of the patients experienced head injuries, with loss of consciousness, a 4% sustained fractures and 4% died due to an injury produced by the fall[2]. Moreover, except physical injuries, falls and disequilibrium can lead to ‘fear of falling’ which further restricts every day activities[8,12], leads to depression[12] and reduces physical exercise such as walking[13].
Fall risk
The risk of falling is multifactorial. Although previously divided into two categories[8] - intrinsic and extrinsic risk factors- the most recent literature broadly classifies them into three categories: intrinsic, extrinsic and exposure to risk[14]. Table 1 shows the most important intrinsic risk factors. Women fall more frequently than men and Caucasians more than Afro-Carribeans[14]. The use of more than 4 medication categories and a variety of medical conditions such as CKD, diabetes and depression are common among fallers[14]. Moreover, impaired mobility, muscle atrophy and vitamin D deficiency are important risk factors for accidental falls[14].
Table 1.
Falls associated intrinsic risk factors. (Retrieved from Todd C. et al. 2004)[14].
| 1. | History of falls |
| 2. | Advanced Age |
| 3. | Gender (women>men) |
| 4. | Ethnicity |
| 5. | Medicines |
| 6. | Medical Conditions |
| 7. | Impaired Mobility |
| 8. | Sedentary behavior |
| 9. | Psychological Status |
| 10. | Nutritional Deficiency |
| 11. | Impaired Cognition |
| 12. | Visual Impairement |
| 13. | Foot Problems |
Extrinsic are the environmental factors that may have impact on the fall incidence. These include poor lighting, stares, slippery floor, inappropriate clothing and others[8,14]. Studies of risk exposure have revealed that either lack of activity or excessive physical activity can cause falls, fact that shows the complex relationship between falls and risk[14].
End- Stage Renal Disease patients form a special category that not only may have similar intrinsic and extrinsic risk factors for falls with the general population, but also usually have many comorbidities, as well as special skeletal, hematological and endocrine abnormalities that expose them to a greater risk of falls and fractures[12,15].
More specifically, vitamin D deficiency[8], post-hemodialysis postural hypotension[8], diabetic neuropathy, sarcopenia[16,17], polypharmacy[18,19] have been proved to be important risk factors for the increased fall incidence of the CKD and HD population. The most important causes of accidental falls in renal disease are revised in Table 2. Onwards, we will try to briefly analyze them according to the most recent studies and publications.
Table 2.
Etiology of most important CKD associated falls.
| 1. | Use of drugs |
| 2. | Dementia |
| 3. | Diabetes Mellitus |
| 4. | Postural Hypotension |
| 5. | Vitamin D Deficiency |
| 6. | Sarcopenia |
| 7. | Anemi |
Use of drugs
Polypharmacy is no longer considered an independent risk factor for falls in the elders, however the type of medication used may increase the risk of falling[19]. As a high number of drugs per person are prescribed, omissions could occur which cause higher proportion of hospitalization[19].
In a meta-analysis the impact of nine classes of medications was studied (antihypertensives, diuretics, β-blockers, sedatives/hypnotics, neuroleptics/antipsychotics, antidepressants, benzodiazepines, narcotic analgesics, NSAIDS) in elderly persons. The results revealed that elderly individuals were more prone to fall when prescribed antidepressants, benzodiazepines or sedatives and hypnotics[5].
A retrospective case- control study conducted in hospitalized, CKD patients, found that this population experienced more falls when treated with antidepressant or anticonvulsant drugs. Additionally, medications for dementia have been implicated as a risk factor for falls. It is shown that patients suffering from dementia have higher falling risk[19]. The association of CKD with cognitive impairment and dementia has been suggested in cross- sectional and longitudinal studies[20].
Another reason for the increased risk of falls in HD patients receiving many drugs is that hemodialysis itself, fluid balance disturbance and increased uremic toxins can change the pharmacokinetics of certain medications leading to interactions and side-effects[21].
Several criteria have been proposed in order to identify the Potentially Inappropriate Medications (PIMs) in elderly Hemodialysis Patients. A recently published study that used the STOPP criteria was able to identify a large number of PIMs in the hemodialysis population (the most prevalent being proton-pump inhibitors)[21].
This fact makes us think that we can always revise our patients’ medications so as to find and reduce those of them not appropriate.
Diabetes mellitus
Diabetes is the leading cause of chronic kidney disease and the prevalence of diabetic nephropathy is steadily increasing from 1988 through 2008[22].
Both high and low values of HbA1c can cause falls in diabetic patients[23,24]. It has been proved that achieving values of HbA1c≤6% with insulin treatment increases the risk of falls as a result of hypoglycemic episodes[23]. On the other hand, a significant relationship exists between poor glycemic control (values of HbA1c>7%) and risk of falls. This is due to complications of diabetes such as peripheral neuropathy and visual impairment[24].
Equally important is the special type of hypoglycemia that occurs in HD sessions affecting more often diabetic HD patients. This is the intradialytic hypoglycemia, which affects more often the diabetic renal patients, especially those who have achieved a better glycemic control[25].
Orthostatic hypotension (OH)
The relationship between orthostatic hypotension (decrease of 20 mmHg in systolic blood pressure or decrease of 10 mmHg in diastolic blood pressure from supine to standing position) and falls is not certain[26,27].
Various studies have managed to show that orthostatic hypotension is a risk factor for falls. More specifically, the results of a longitudinal cohort study indicated that sustained orthostatic hypotension was an independent risk factor for future, unexplained and injurious falls[27]. In a prospective study of 844 elderly nursing home residents, OH was an independent risk factor for recurrent falls[26].
Autonomic nervous system dysfunction has been also proved to lead to orthostatic and generalized hypotension[28].
Again hemodialysis patients are a population with special characteristics and more reasons to suffer from episodes of postural hypotension and consequently more falls.
Hemodialysis patients have increased prevalence for both orthostatic hypotension and autonomic nervous system dysfunction[28,29]. OH is usually caused by the nature of HD treatment itself[28] (rapid fluid exchange) or by a possible underestimation of hemodialysis dry weight[30]. Moreover, autonomic dysfunction due to uremia, diabetes and amyloidosis is also common in dialysis-dependent patients and a risk factor for falls[28,29].
A better dry weight calculation, as well as a better diabetes and uremia control could be of significance in minimizing hypotensive episodes in this patient group.
Vitamin D deficiency
Vitamin D is a fat-soluble secosteroid which plays a central role in calcium and phosphate metabolism. The effect of vitamin D on muscle strength, bone and falls has been studied in general population as well as in CKD patients and the results are discussed in this section.
Vitamin D deficiency is associated with muscle pain, myopathy[31] and reduction of the muscle strength[32]. Supplementation and correction of vitamin D deficiency can improve the strength of quadriceps muscle and thus reduce the incidence of the falls that are associated with mortality[33]. Moreover Vitamin D is essential for bone growth and higher bone density[34].
The effect of vitamin D on falls has been studied in a meta-analysis which came to the conclusion that the supplementation of vitamin D reduces the risk of falls among ambulatory or institutionalized older individuals by more than 20%[35]. The effect on muscles perhaps is due to de novo protein synthesis[35]. The combination with calcium may be of significance in reducing the risk of falls[33,35].
Figure 1 shows the changes in vitamin D in Chronic Kidney Disease.
Figure 1.
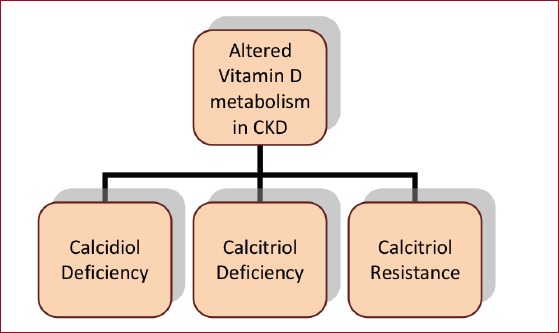
The changes in vitamin D in chronic kidney disease.
Chronic kidney disease can cause endocrine and mineral metabolism abnormalities even in early stages. Deficiency of 1,25 dihydroxyvitamin D [1,25(OH)2D3] due to hypohydroxylation of 25(OH)D3 by kidney 1 α- hydroxylase is one of them. 1, 25(OH)2D3 (calcitriol) leads to hyperparathyroidism (HPTH) and parathyroid gland hyperplasia in CKD and ESRD patients[36]. Low levels of active vitamin D lead to impaired binding in the vitamin D receptor (VDR). The loss of VDR in the parathyroid glands is causing resistance to the action of calcictriol[37].
CKD is also characterized by lower calcidiol, with reduced sun exposure, reduced skin production and loss of vitamin D binding protein (DBP) being the main reasons for these changes[37].
Vitamin D deficiency is defined as a serum 25(OH) D level <20 ng/ml and insufficiency as between 21-29 ng/ml[38]. The optimal range remains controversial[38]. Among other consequences, low levels of vitamin D in chronic kidney disease and ESRD cause high bone turnover[39], muscle weakness, higher risk of falls[40] and high mortality risk[41,42].
The KDOQI guidelines recommend the administration of ergocalciferol and cholecalciferol to patients with CKD stage 3 to 4 if calcidiol levels are below 30 ng/ml[43] but further investigation is needed in order to identify the optimal levels of vitamin D, the appropriate regimen, dose and route of administration[35].
Sarcopenia
The term sarcopenia was coined by Irwin Rosenberg[17]. Derives from Greek ‘sarx’ that means flesh and ‘penia’ that means poverty. Sarcopenia is a component of the frailty syndrome, recognized by increased vulnerability as a result of age decline and compromised function across multiple physiologic systems[36]. In its first definition sarcopenia was described as the muscle mass loss that occurs with advancing age[16]. Nowadays the definition has expanded to include muscle function and strength as well because in the elders the loss of muscle mass is only one reason for the loss of muscle strength among others, along with muscle atrophy and denervation of the muscle fibers[16].
A healthy adult is losing 1% of muscle mass every year while CKD patients begin to do so in an earlier age[44]. Predisposing factors for this difference have to do either with kidney disease itself (metabolic acidosis, uremic toxins, mitochondrial dysfunction, inflammation, malnutrition, insulin resistance, increased ubiquitination, vitamin D deficiency, higher PTH levels[38], physical inactivity[15,17], calcium-phosphate disorders and proteinuria[44]) or with the inflammatory process following HD (proinflammatory cytokines, oxidative stress)[38,44,45]. There is evidence that sarcopenia is associated with accidental falls: In a meta- analysis and systematic review of the health outcomes of sarcopenia it was shown that sarcopenic subjects were at a higher risk of accidental falls, fractures, hospitalization and longer hospital stay compared with non-sarcopenic subjects[16]. Moreover, loss of lean body mass weight is known to cause frequent falls and their complications[46]. It is therefore easy to understand that sarcopenia in CKD is of importance in CKD associated fall pathology but more research is needed focusing on this special population.
Anemia
The World Health Organization (WHO) defines anemia as a hemoglobin (Hb) <12 g/dl in females and <13 g/dl in males[40]. Anemia in chronic kidney disease patients was described 170 years ago by Richard Bright[41]. Now we know that anemia is a common feature of CKD and affects almost all patients with stage 5 CKD[42]. The development of anemia in CKD is multifactorial related to lower levels of erythropoietin, inhibition of erythropoiesis by uremic toxins, disordered iron homeostasis and erythrocyte survival[43].
The association between anemia and the risk of falls is ambiguous. There are studies that relate falls to anemia and others that do not come to this conclusion. For instance, two studies in older adults - hospitalized or in the community- managed to show an important link between anemia and accidental falls[47,48]. On the other hand, this independent association has not been always proved[49], which makes it a promising field for further investigation.
Discussion
In this mini review we tried to collect information about accidental, low-energy falls in chronic kidney disease population using published evidence. According to our investigation falling is a major clinical problem in elders, thus not only an important issue in every day clinical practice but also a big economic burden for the health system of a country. Chronic kidney disease and End Stage Renal Disease patients have a higher risk of falls, fall-related fractures, hospitalization and mortality.
These patients are prone to falls and their complications for many reasons. Kidney disease is associated with hormonal, bone and hematologic abnormalities. The excessive use of drugs in this patient category, especially that of antidepressants and hypnotics, as well as the higher incidence of diseases such as dementia are some of them. Moreover the complications of diabetes mellitus (i.e. diabetic neuropathy) are a major risk factor, keeping in mind that diabetes is the first cause of ESRD.
Accidental falls due to postural hypotension are common in HD, especially when dry- weight is underestimated.
Many studies concentrate on the importance of vitamin D and its relation with falls. The results of these studies conclude that vitamin D deficiency, - a very common complication of CKD- and secondary hyperparathyroidism can result in muscle weakness and injurious falls and that treatment of patients with CrCl <65 ml/min with alfacacidol can reduce the risk of falls and number of fallers[50].
It is also of great interest the investigation of anemia and sarcopenia of CKD and their possible relation with falls. More studies need to be done in order to have safe conclusions, but better control of the CKD abnormalities (such as metabolic acidosis, anemia) and muscle strength exercises seem to be reasonable solutions to this problem. Pharmacologic interventions that inhibit muscle wasting are in trials and research is needed in CKD population.
Moreover, progressive kidney disease is accompanied by an unhealthy lifestyle. It is estimated that for every month of hemodialysis the physical activity decreases by 3, 4%[51]. It has been shown that certain type of exercise on non- hemodialysis days is an interesting rehabilitation method for HD patients, providing a chance of better quality of life and lesser falls[52].
For some of the issues mentioned above, the evidence is controversial and further studies are needed in order to get to safe results and conclusions. Recognizing the most important risk factors for accidental falls is necessary in order to find the appropriate prevention measures and therapies.
One limitation of our research is that there is little evidence concerning chronic kidney disease patients Stages 1-4. The majority of researches on accidental falls are performed in HD population. This observation leads us to the conclusion that more studies should be done focusing on patients on less severe stages of CKD as well as renal transplant patients, so that we can have a better understanding of the problem.
Conclusion
Falls are extremely common among hemodialysis patients. Fall prevention has been found to be possible through review of the medications, orthostasis prevention, muscle strengthening, better glycemic control and vitamin D deficiency treatment. Further research is needed for the improvement of methods to prevent accidental falls as well as in order to include patients with less severe kidney disease.
Footnotes
Edited by: Yannis Dionyssiotis
References
- 1.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319(26):1701–7. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 2.Cook WL, Tomlinson G, Donaldson M, Markowitz SN, Naglie G, Sobolev B, Jassal SV. Falls and Fall-Related Injuries in Older Dialysis Patients. Clin J Am Soc Nephrol. 2006;1(6):1197–204. doi: 10.2215/CJN.01650506. [DOI] [PubMed] [Google Scholar]
- 3.Cook WL, Jassal SV. Prevalence of falls among seniors maintained on hemodialysis. Int Urol Nephrol. 2005;37(3):649–52. doi: 10.1007/s11255-005-0396-9. [DOI] [PubMed] [Google Scholar]
- 4.Tinetti ME, Speechley M. Prevention of falls among the elderly. N Engl J Med. 1989;320(16):1055–9. doi: 10.1056/NEJM198904203201606. [DOI] [PubMed] [Google Scholar]
- 5.Woolcott JC, Richardson KJ, Wiens MO, Patel B, Marin J, Khan KM, et al. Meta-analysis of the Impact of 9 Medication Classes on Falls in Elderly Persons. Arch Intern Med. 2009;169(21):1952–1960. doi: 10.1001/archinternmed.2009.357. [DOI] [PubMed] [Google Scholar]
- 6.Abdel-Rahman EM, Yan G, Turgut F, Balogun RA. Long-Term Morbidity and Mortality Related to Falls in Hemodialysis Patients:Role of Age and Gender - A Pilot Study. Nephron Clin Pract. 2011;118(3):c278–84. doi: 10.1159/000322275. [DOI] [PubMed] [Google Scholar]
- 7.Ray NF, Chan JK, Thamer M, Melton LJ. Medical Expenditures for the Treatment of Osteoporotic Fractures in the United States in 1995:Report from the National Osteoporosis Foundation. J Bone Miner Res. 1997;12(1):24–35. doi: 10.1359/jbmr.1997.12.1.24. [DOI] [PubMed] [Google Scholar]
- 8.John E. Morley. Falls in Elderly Patients With Kidney Disease. American Society of Nephrology, Geriatric Nephrology Curriculum. Available from:URL: https://www.asn-online.org/education/distancelearning/curricula/geriatrics/Chapter33.pdf .
- 9.Nickolas TL, McMahon DJ, Shane E. Relationship between Moderate to Severe Kidney Disease and Hip Fracture in the United States. J Am Soc Nephrol. 2006;17(11):3223–32. doi: 10.1681/ASN.2005111194. [DOI] [PubMed] [Google Scholar]
- 10.Farragher J, Chiu E, Ulutas O, Tomlinson G, Cook WL, Jassal SV. Accidental Falls and Risk of Mortality among Older Adults on Chronic Peritoneal Dialysis. Clin J Am Soc Nephrol. 2014;9(7):1248–53. doi: 10.2215/CJN.11001013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zecevic AA, Salmoni AW, Speechley M, Vandervoort AA. Defining a Fall and Reasons for Falling:Comparisons Among the Views of Seniors, Health Care Providers, and the Research Literature. Gerontologist. 2006;46(3):367–76. doi: 10.1093/geront/46.3.367. [DOI] [PubMed] [Google Scholar]
- 12.Boyd R, Stevens JA. Falls and fear of falling:burden, beliefs and behaviours. Age Ageing. 2009;38(4):423–8. doi: 10.1093/ageing/afp053. [DOI] [PubMed] [Google Scholar]
- 13.Jefferis BJ, Iliffe S, Kendrick D, Kerse N, Trost S, Lennon LT, et al. How are falls and fear of falling associated with objectively measured physical activity in a cohort of community-dwelling older men? BMC Geriatr. 2014;14:114. doi: 10.1186/1471-2318-14-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Todd C, Skelton D. What Are the Main Risk Factors for Falls among Older People and What Are the Most Effective Interventions to Prevent these Falls? Copenhagen, Denmark: World Health Organisation Health Evidence Network; 2004. [Google Scholar]
- 15.Avin KG, Moorthi RN. Bone is Not Alone:the Effects of Skeletal Muscle Dysfunction in Chronic Kidney Disease. Curr Osteoporos Rep. 2015;13(3):173–9. doi: 10.1007/s11914-015-0261-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beaudart C, Zaaria M, Pasleau F, Reginster JY, Bruyère O. Health Outcomes of Sarcopenia:A Systematic Review and Meta-Analysis. PLoS One. 2017;12(1):e0169548. doi: 10.1371/journal.pone.0169548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moorthi RN, Avin KG. Clinical relevance of sarcopenia in chronic kidney disease. Curr Opin Nephrol Hypertens. 2017;26(3):219–228. doi: 10.1097/MNH.0000000000000318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hammond T, Wilson A. Polypharmacy and Falls in the Elderly:A Literature Review. Nurs Midwifery Stud. 2013;2(2):171–175. doi: 10.5812/nms.10709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Angalakuditi MV, Gomes J, Coley KC. Impact of Drug Use and Comorbidities on In-Hospital Falls in Patients with Chronic Kidney Disease. Ann Pharmacother. 2007;41(10):1638–43. doi: 10.1345/aph.1H631. [DOI] [PubMed] [Google Scholar]
- 20.Etgen T. Kidney disease as a determinant of cognitive decline and dementia. Alzheimers Res Ther. 2015;7(1):29. doi: 10.1186/s13195-015-0115-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parker K, Aasebø W, Stavem K. Potentially Inappropriate Medications in Elderly Haemodialysis Patients Using the STOPP Criteria. Drugs Real World Outcomes. 2016;3(3):359–363. doi: 10.1007/s40801-016-0088-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Kidney Foundation:KDOQI Clinical Practice Guideline for Diabetes and CKD:2012 Update [published erratum appears in Am J Kidney Dis. 2013 Jun;61(6)1049] Am J Kidney Dis. 2012;60(5):850–86. doi: 10.1053/j.ajkd.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 23.Schwartz AV, Vittinghoff E, Sellmeyer DE, et al. Diabetes-Related Complications, Glycemic Control, and Falls in Older Adults Diabetes Care. 2008;31(3):391–396. doi: 10.2337/dc07-1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tilling LM, Darawil K, Britton M. Falls as a complication of diabetes mellitus in older people. J Diabetes Complications. 2006;20(3):158–62. doi: 10.1016/j.jdiacomp.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 25.Burmeister JE, Miltersteiner Dda R, Burmeister BO, Campos JF. Risk of hypoglycemia during hemodialysis in diabetic patients is related to lower pre-dialysis glycemia. Arch Endocrinol Metab. 2015;59(2):137–40. doi: 10.1590/2359-3997000000026. [DOI] [PubMed] [Google Scholar]
- 26.Ooi WL, Hossain M, Lipsitz LA. The Association between Orthostatic Hypotension and Recurrent Falls in Nursing Home Residents. Am J Med. 2000;108(2):106–11. doi: 10.1016/s0002-9343(99)00425-8. [DOI] [PubMed] [Google Scholar]
- 27.Finucane C, O'Connell MD, Donoghue O, Richardson K, Savva GM, Kenny RA. Impaired Orthostatic Blood Pressure Recovery Is Associated with Unexplained and Injurious Falls. J Am Geriatr Soc. 2017;65(3):474–482. doi: 10.1111/jgs.14563. [DOI] [PubMed] [Google Scholar]
- 28.Roberts RG, Kenny RA, Brierley EJ. Are elderly haemodialysis patients at risk of falls and postural hypotension? Int Urol Nephrol. 2003;35(3):415–21. doi: 10.1023/b:urol.0000022866.07751.4a. [DOI] [PubMed] [Google Scholar]
- 29.Jassal SV, Douglas JF, Stout RW. Prevalence of central autonomic neuropathy in elderly dialysis patients. Nephrol Dial Transplant. 1998;13(7):1702–8. doi: 10.1093/ndt/13.7.1702. [DOI] [PubMed] [Google Scholar]
- 30.Jaeger JQ, Mehta RL. Assessment of Dry Weight in Hemodialysis:An Overview. J Am Soc Nephrol. 1999;10(2):392–403. doi: 10.1681/ASN.V102392. [DOI] [PubMed] [Google Scholar]
- 31.Pérez-López FR. Vitamin D and its implications for musculoskeletal health in women:An update. Maturitas. 2007;58(2):117–37. doi: 10.1016/j.maturitas.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 32.Ward KA, Das G, Berry JL, Roberts SA, Rawer R, Adams JE, et al. Vitamin D Status and Muscle Function in Post-Menarchal Adolescent Girls. J Clin Endocrinol Metab. 2009;94(2):559–63. doi: 10.1210/jc.2008-1284. [DOI] [PubMed] [Google Scholar]
- 33.Murad MH, Elamin KB, Abu Elnour NO, Elamin MB, Alkatib AA, Fatourechi MM, et al. The Effect of Vitamin D on Falls:A Systematic Review and Meta-Analysis. J Clin Endocrinol Metab. 2011;96(10):2997–3006. doi: 10.1210/jc.2011-1193. [DOI] [PubMed] [Google Scholar]
- 34.Bruyère O, Cavalier E, Souberbielle JC, Bischoff-Ferrari HA, Beaudart C, Buckinx F, et al. Effects of vitamin D in the elderly population:current status and perspectives. Arch Public Health. 2014;72(1):32. doi: 10.1186/2049-3258-72-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, Staehelin HB, Bazemore MG, Zee RY, et al. Effect of Vitamin D on Falls A Meta-analysis. JAMA. 2004;291(16):1999–2006. doi: 10.1001/jama.291.16.1999. [DOI] [PubMed] [Google Scholar]
- 36.Xue QL. The Frailty Syndrome:Definition and Natural History. Clin Geriatr Med. 2011;27(1):1–15. doi: 10.1016/j.cger.2010.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Delgado C, Shieh S, Grimes B, Chertow GM, Dalrymple LS, Kaysen GA, et al. Association of self-reported frailty with falls and fractures among patients new to dialysis. Am J Nephrol. 2015;42(2):134–40. doi: 10.1159/000439000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Visser M, Deeg DJ, Lips P. Low Vitamin D and High Parathyroid Hormone Levels as Determinants of Loss of Muscle Strength and Muscle Mass (Sarcopenia):The Longitudinal Aging Study Amsterdam. J Clin Endocrinol Metab. 2003;88(12):5766–72. doi: 10.1210/jc.2003-030604. [DOI] [PubMed] [Google Scholar]
- 39.C Beaudart C, Dawson A, Shaw SC, et al. Nutrition and physical activity in the prevention and treatment of sarcopenia:systematic review. Osteoporos Int. 2017;28(6):1817–1833. doi: 10.1007/s00198-017-3980-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nutritional anaemias. Report of a WHO scientific group. World Health Organ Tech Rep Ser. 1968;405:5–37. [PubMed] [Google Scholar]
- 41.Bright R. Cases and observations:Illustrative of renal disease accompanied by the secretion of albuminous urine. Guys Hosp Rep. 1:338–1836. [Google Scholar]
- 42.National Kidney Foundation. KDOQI Clinical Practice Guidelines and Clinical Practice Recommendations for Anemia in Chronic Kidney Disease. Am J Kidney Dis. 2006;47(Suppl 3):S11–S145. doi: 10.1053/j.ajkd.2006.03.010. [DOI] [PubMed] [Google Scholar]
- 43.Babitt JL, Lin HY. Mechanisms of Anemia in CKD. J Am Soc Nephrol. 2012;23(10):1631–1634. doi: 10.1681/ASN.2011111078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Domański M, Ciechanowski K. Sarcopenia:a major challenge in elderly patients with end-stage renal disease. J Aging Res. 2012;2012:754739. doi: 10.1155/2012/754739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Honda H, Qureshi AR, Axelsson J, Heimburger O, Suliman ME, Barany P, et al. Obese sarcopenia in patients with end-stage renal disease is associated with inflammation and increased mortality. Am J Clin Nutr. 2007;86(3):633–8. doi: 10.1093/ajcn/86.3.633. [DOI] [PubMed] [Google Scholar]
- 46.Ohkawa S, Odamaki M, Ikegaya N, Hibi I, Miyaji K, Kumagai H. Association of age with muscle mass, fat mass and fat distribution in non-diabetic haemodialysis patients. Nephrol Dial Transplant. 2005;20(5):945–51. doi: 10.1093/ndt/gfh643. [DOI] [PubMed] [Google Scholar]
- 47.Dharmarajan TS, Norkus EP. Mild Anemia and the Risk of Falls in Older Adults From Nursing Homes and the Community. J Am Med Dir Assoc. 2004;5(6):395–400. doi: 10.1097/01.JAM.0000144734.84172.89. [DOI] [PubMed] [Google Scholar]
- 48.Dharmarajan TS, Avula S, Norkus EP. Anemia Increases Risk for Falls in Hospitalized Older Adults:An Evaluation of Falls in 362 Hospitalized, Ambulatory, Long-Term Care, and Community Patients. J Am Med Dir Assoc. 2007;8(3 Suppl 2):e9–e15. doi: 10.1016/j.jamda.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 49.Thaler-Kall K, Döring A, Peters A, Thorand B, Grill E, Koenig W, et al. Association between anemia and falls in community-dwelling older people:cross-sectional results from the KORA-Age study. BMC Geriatr. 2014;14:29. doi: 10.1186/1471-2318-14-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dukas L, Schacht E, Mazor Z, Stähelin HB. Treatment with alfacalcidol in elderly people significantly decreases the high risk of falls associated with a low creatinine clearance of <65 ml/min. Osteoporos Int. 2005;16(2):198–203. doi: 10.1007/s00198-004-1671-9. [DOI] [PubMed] [Google Scholar]
- 51.Johansen KL, Kaysen GA, Young BS, Hung AM, da Silva M, Chertow GM. Longitudinal study of nutritional status, body composition, and physical function in hemodialysis patient. Am J Clin Nutr. 2003;77(4):842–6. doi: 10.1093/ajcn/77.4.842. [DOI] [PubMed] [Google Scholar]
- 52.Dziubek W, Bulińska K, Kusztal M, et al. Evaluation of Exercise Tolerance in Dialysis Patients Performing Tai Chi Training:Preliminary Study. Evid Based Complement Alternat Med. 2016;2016:5672580. doi: 10.1155/2016/5672580. [DOI] [PMC free article] [PubMed] [Google Scholar]


