Summary
The purpose of this study was to determine the effects of teaching stress-coping strategies and group cognitive-behavioral therapy on stress and burnout among nurses. Stress and burnout have always been a significant problem in nursing, which can have a direct or indirect negative impact on the individual and his/her social life. A semi-experimental study was conducted on 60 nurses by means of a pre-test and post-test design. Nurses meeting the inclusion criteria were assigned to two groups, a control group and an intervention group, by the block randomization method. The nurses in the intervention group received group cognitive-behavioral therapy. They completed the Maslach Burnout Inventory (MBI) before, immediately after and one month post intervention. There was a significant negative correlation only between burnout and work experience (r = -0.35 and p = 0.01). After intervention, burnout (p = 0.002) significantly decreased. The effectiveness of the intervention was also maintained after a month. The results showed that stress-coping strategies and group cognitive-behavioral therapy can be effective in reducing burnout. This method can be used to provide counseling services for nurses in health centres.
Keywords: cognitive behavioral therapy, coping, occupational stress, burnout, nursing
Abstract
Le but de cette étude était d’évaluer les effets d’un apprentissage de gestion du stress (AGS) et de thérapie cognitivocomportementales de groupe (TCCG) sur le stress et le burn- out des infirmièr(e)s, reconnus comme des problèmes récurrents chez eux (elles), avec des impacts sur leur vie. Une étude semi- expérimentale pré et post- test a été conduite chez 60 infirmièr(e) s, réparti(e)s en 2 groupes (intervention I qui bénéficiait TCCG et témoin T, randomisation en blocs), après vérification des critères d’inclusion. Ils (elles) complétaient l’inventaire de burn- out de Maslach avant, juste après et 1 mois après la TCCG. On notait une corrélation inverse entre expérience et burn- out (r=-0,35 ; p= 0,01). Le burn- out décroissait significativement (p = 0,002) après intervention, effet persistant à 1 mois. Cette étude montre que AGS et TCCG semblent efficaces sur le burn- out. Elle pourrait faire partie d’une proposition de services dans les CTB.
Introduction
Humans and their environment constantly interact with each other. The existence of environmental stimuli, if not beyond human ability, is harmless for the survival of life1 and causes reactions that are necessary for evolution and for maintaining a balance between humans and the environment. One of the most important stressful environmental stimuli that can cause chronic psychological stress is the type of occupation a person is engaged in. If stress is caused by overwork, it can do physical and psychological harm to the individual, endanger his/her health, threaten organizational goals, and reduce the quality of the person’s performance.
Employed people who are engaged in stressful environments, such as health workers in intensive care and burn units, and are under pressure at work, often experience burnout. The term burnout is used to describe a syndrome that includes physical exhaustion leading to emotional exhaustion and job abandonment.2 This phenomenon has physical and psychological symptoms.3 Physical symptoms are energy loss, chronic fatigue, weakness, increased vulnerability to diseases, chronic headaches, muscle tension, back pain, multiple physical complaints and sleep disorders, while psychological symptoms include helplessness, disappointment, increased stress and conflict, increased neurodegenerative conditions such as restlessness, anger and irritability, negative attitudes towards oneself, one’s occupation and life, and ultimately withdrawal behaviors such as absenteeism and escape from work.4,5 The term “burnout” was defined for the first time in the late 1960s by Freudeberger when he observed fatigue symptoms in his staff. He called this phenomenon a syndrome of physical and mental exhaustion that occurs in people working in assisted care professions.6 Burnout is a psychological syndrome and one of the major inevitable consequences of occupational stress, which continues to persist until stress is eliminated.7 This phenomenon has the three dimensions of emotional exhaustion, depersonalization, and a reduction in sense of personal competence.8-10
Emotional exhaustion is the pressure associated with tension, anxiety, physical exhaustion and insomnia. Depersonalization (cynicism) of the person is a negative and cynical response to people who are usually recipients of the service from the individual, and refers to the individual’s perception of his or her client. A decrease in a person’s sense of adequacy is a reduction in sense of accomplishment in personal performance and a negative self-assessment of work.6 Burnout is more likely to occur in people doing occupations where they spend a lot of hours in close contact with other people. Hospital staff are directly in contact with all segments of a community and at the same time are closely involved in people’s problems.11 Among the healthcare occupations, nursing involves spending many hours with patients and being continually exposed to several stressors. Having a relationship with patients leads to a depletion of the nurses’ emotional resources. Therefore the phenomenon is more common in nurses, to such an extent that, according to some studies, in the United States burnout is four times higher among nurses than among any other service providers.7 In recent years, the burnout phenomenon has attracted the attention of many researchers and practitioners. A lot of research on burnout has examined its association with various individual and environmental variables. 12,13
Weigl et al. showed that high workload and lack of responsible support from authorities had an impact on increasing emotional exhaustion and depression in nurses.14 Undoubtedly, these factors will in the long term lead to adverse physical and psychological effects, and a degradation in professional activity and nursing care. Therefore it is essential to identify the causes of occupational stress and adopt suitable coping strategies as well as continuing education for therapeutic practitioners, especially nurses. To prevent and reduce stress and burnout, various interventions such as cognitive-behavioral training, physical and mental relaxation, and organizational interventions including changing work conditions, organized support, modified care, increasing communication skills and changing work plans, alone or in combination, have been exploited.15 Mohammadzadeh and colleagues examined the relation between psychological empowerment, quality of work life and burnout among health workers, and showed that the higher employee psychological empowerment, the lower the burnout.16 A clinical trial conducted by Stenlund in Sweden showed that both cognitive-behavioral rehabilitation and Qigong (physical mental exercise originating from traditional Chinese medicine) techniques were able to decrease burnout, fatigue, depression, anxiety and obsessive-compulsive symptoms in patients who had long-term burnout and had abandoned work.17 In the study by Sandahl, individual and group cognitive therapy was effective in reducing the symptoms of depression caused by working, but comparing the two methods did not show a significant relationship.18 In some studies that emphasized the effects of cognitive-behavioral training and physical-mental relaxation, as well as changes to the work plan, on reducing stress, the quality of study was low and the samples studied were not big enough. Therefore, the present study aimed to investigate the effect of stress-coping strategies and group cognitive-behavioral therapy on burnout among nurses.
Methods
Design and study protocol
This is a semi-experimental interventional study on 60 nurses working in Hazrat Fatima Hospital in Tehran in 2014. The study was conducted after being approved by the Ethics Committee of Iran University of Medical Sciences, and registered on the Iranian clinical trials website to obtain a license (Irct ID: IRCT201604178177N14). Consent forms were signed by the nurses in the sample before participating in the research. The inclusion criteria included nurses of both sexes, undergraduate and postgraduate education, age groups without restrictions, more than one year of clinical work, and working in different wards. Exclusion criteria were having a chronic physical and psychological illness, taking drugs that affected the mental system, and loss of a first-degree relative (father, mother, spouse or child) less than six months beforehand. It was also announced that one of the admission requirements was the principle of confinement to educational materials and issues raised by the group members in each session.
Participants in the study included all nurses, head nurses and supervisors who met the inclusion criteria. They were assigned by the block randomization method to two groups of 30 subjects. The intervention group participated in 10 group cognitive therapy sessions of 1.5 to 2 hours, once a week for 2 and a half months. Meanwhile, no psychological intervention was performed on the control group. A group cognitive therapy book19 was chosen to educate the participants, and the researcher developed the protocol for each group psychotherapy session with a cognitive approach based on this book. At the beginning of each session, the objectives of the meeting were discussed, followed by a summing up of the previous meeting. A few minutes were then allocated to examining the homework from the previous meeting. The total therapeutic goals of the sessions were as follows:
Session One provides participants with the information that physiological, cognitive and behavioral processes interact with each other, that emotions have cognitive, physiological and behavioral components, and that all or most emotional responses have cognitive components;
Session Two empowers participants to receive the preliminary thoughts between the event and the emotional response and to write them in three columns, (I) the activating event, (II) beliefs or thoughts, and (III) emotional outcomes;
In Session Three participants recognize the most important aspects of the cognitive theories of depression, anxiety and anger, become familiar with the characteristics of happy thoughts and how they can be reached, identify important cognitive distortions and discover their ability to recognize them in their thoughts. Finally, they must recognize their potential resistance to cognitive therapy, and learn strategies to deal with this resistance;
In Session Four participants become acquainted with the point that their thoughts, just like emotional outcomes, have behavioral consequences, and that also their behavioral consequences may be ineffective;
Session Five focuses on the nature of schemas (central beliefs, thoughts, inefficient attitudes), and the relationship between schemas and happy thoughts, as well as on downward arrows for identifying schemas;
In Session Six participants accept the principle that beliefs are volatile. Dominant cultural beliefs change throughout human history, and individuals also change their beliefs over time;
Session Seven focuses on the understanding that beliefs can be evaluated based on a number of criteria, that beliefs can have different degrees of efficiency, and that individuals use a set of beliefs to organize their behaviors that are, to some extent, consistent and compatible with other beliefs held by others. Consistency with other beliefs and the beliefs of other people has an implicit implication on the correctness of that belief.
In Session Eight participants can apply a logical analysis to their beliefs. Logical analysis is the strongest technique for challenging people’s beliefs. An important aspect of logical analysis is that it has multiple ways of challenging beliefs in itself. Therefore, in this way, through the challenge to their beliefs participants tend to conclude that their beliefs are true or false.
In Session Nine participants can “oppose” their negative beliefs, and in Session Ten they can create a practical application for themselves that will encourage them to continue practicing techniques and approaches they have learned throughout the program, and provide a program for continuity and sustainability of alteration. In order to achieve the proposed therapeutic goals, cognitive-behavioral methods are taught to them.
The training was conducted by a clinical psychiatrist with a Master degree. The topics of the training sessions were cognitive stress and negative thinking, stress-coping strategies including relaxation, recognition of personality types and effective communication methods. The training was conducted using group discussion and group member participation, whiteboard, Power Point and role model. Nurses were present in the classroom during working hours. The nurses’ attendance was coordinated by the hospital’s nursing director with a written invitation. In order to motivate employees in the classroom, hours were calculated as part of their in-service training hours and their points were included in their annual evaluation.
Outcome measures
A demographic questionnaire was used to collect personal, social and occupational data including age, sex, marital status, educational level, work experience, overtime worked per month, work area, work shift, number of children and economic status. Burnout in all participants in the study was determined by the Maslach Burnout Questionnaire.
Maslach Burnout Questionnaire (MBQ). The Maslach Burnout Questionnaire has 22 items which measure burnout in the three dimensions of emotional exhaustion (9 questions), personality depersonalization (5 questions), and individual performance (8 questions). In order to determine the total burnout score, questions 1, 2, 3, 5, 6, 9, 10, 12, 13, 14, 15, 19, 21 and 22 are considered (+) and questions 4, 7, 8, 11, 16, 17, 18 and 20 (-), and then aggregated. Results for burnout frequency will be 35 to 84 (high), -15 to 34 (average), -16 to -66 (low) and for burnout severity 40 to 98 (high), -18 to 39 (average) and -19 to -77 (low). The validity of the questionnaire was verified by Maslach and Jackson and its reliability was calculated through Cronbach’s alpha, which was reported between -0.60 and 0.08. In Sedghi’s research, the reliability was determined to be 0.78.20 The Cronbach’s alpha was reported as 0.8 in the present study.
Data collection. In the second stage, the nurses in the intervention group received group cognitive therapy. In the third stage, immediately after and one month after training completion, the burnout level of all participants in the study was determined and evaluated by the Maslach burnout inventory.
Data analysis. Data were extracted and analyzed by SPSS.V18 software. Quantitative data are reported as mean and standard deviation (SD) and qualitative data as percentage. For analytical analysis, repeated measures, variance analysis (ANOVA) and chi-square were used.
Results
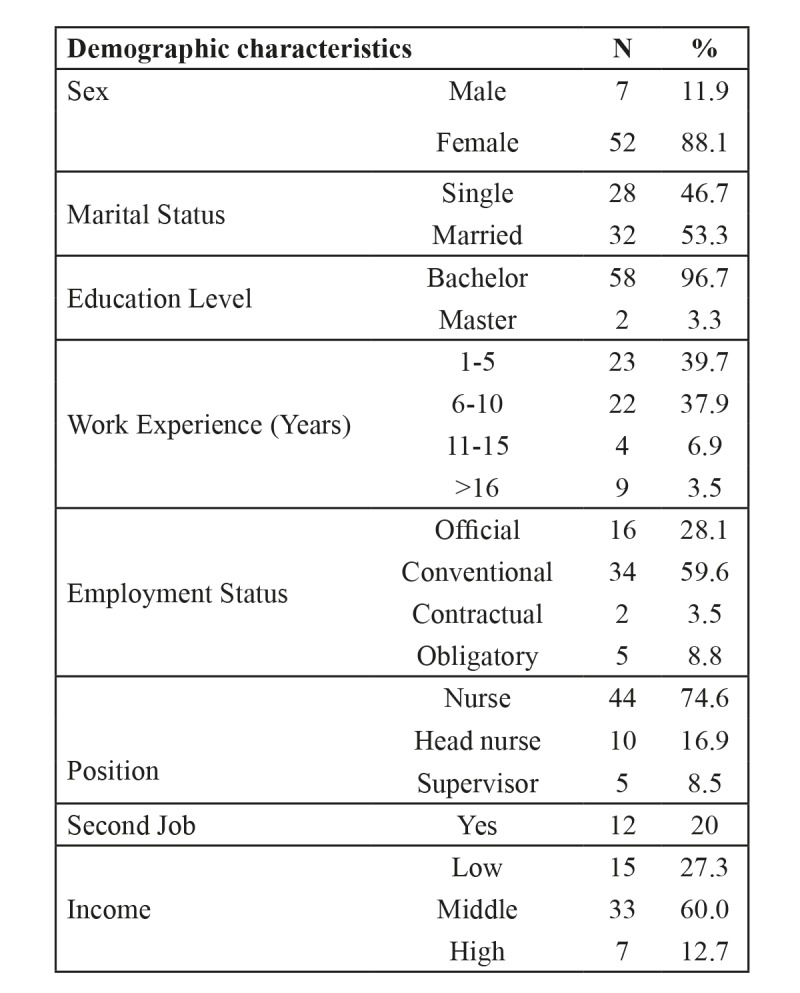
Sixty nurses were divided into two groups. The mean age was 33.21 ± 7.04 years and the difference between the two groups was not significant. Most of the participants were women (88.1%) and married (53.3%). Among them, 74.6% were nurses, 16.9% and 8.5% were head nurses and supervisors, respectively. Their level of education was mostly Bachelor Degree and 39.7% participants had 1-5 years’ work experience. The employment status of most of the participants was contractual, 20% had a second job and 60% had an income of 1,500,000-1,000,000 Touman (Table I).
Table I.
Among the demographic variables, only work experience and burnout had a negative and significant relationship, which means that as work experience increased, the degree of burnout decreased. There was no significant relationship between any of the other variables with burnout.
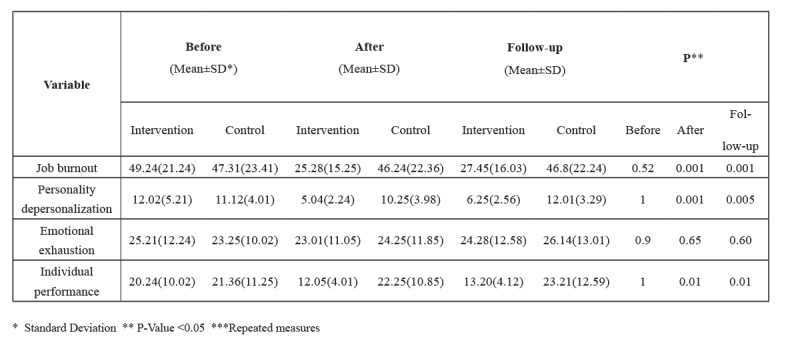
The pre-intervention evaluation showed that the mean burnout group score was 54.21 ± 17.25 and 52.89 ± 16.05 in the intervention and control group, respectively. This indicated that the burnout rate in the two groups was high. As indicated in the table, the variable burnout and its subscales before intervention were not significantly different in the two groups. The rate of burnout decreased immediately (P = 0.001, P = 0.002), and also significantly one month after the intervention (P = 0.001 and P = 0.005). In the study of burnout subscales, depersonalization and accomplishment decreased significantly immediately (P = 0.001, P = 0.01) and one month later (P = 0.005 and P = 0.01), but the emotional fatigue subscale in both stages of evaluation did not show a significant decrease (P = 0.65 and P = 0.66) (Table II).
Table II. Comparison of job burnout and its subscales including personality depersonalization, emotional exhaustion and individual performance before and after intervention and at follow-up.
Discussion
Burnout has always been a significant problem in nursing, which can have a direct or indirect negative impact on the individual and his/her social life. The aim of this study was to determine the effect of teaching stress-coping strategies and group cognitive-behavioral therapy on burnout among nurses. The results of this study indicated that there was a significant negative relationship between demographic characteristics of work experience and burnout. This means that the greater the work experience of nurses, the lower the burnout, which is probably due to more experience and more adaptability in the workplace. However, there was no relationship between age, marital status and the employment of nurses with burnout. The results of Sedghi Goyaghaj et al.,20 Abdi21 and Sahebzadeh22 proved that nurses with less work experience had higher burnout rates. In a study by Xie and colleagues on Chinese nurses, burnout was more common in younger nurses. Therefore the results of the Chinese study can be compared with the present study, because younger nurses often have less work experience. In the study by Gomez, levels of personality deprivation and emotional exhaustion were higher among the subscales of burnout in younger nurses.24 However, in a study by Ebdo on doctors and nurses working in the emergency department, most participants showed a moderate level of burnout, and age, sex, frequency of exposure to work-related violence, work experience and workload were significant predictors of burnout among the participants. The results ofthis study were consistent with our study in relation to reverse work experience and burnout.25
Another study showed that coping-strategy training can significantly reduce burnout in nurses. The results of the meta-analysis performed by Lee26 and also Bahranian’s study27 on the effectiveness of training in reducing burnout were similar to the present study. Also Orly, who examined the cognitive-behavioral intervention and its effect on the psychological health of nurses, showed that cognitive-behavioral education could increase sense of coherence and mood status in nurses and reduce job stress and fatigue. The results of the study confirmed the positive effect of cognitive-behavioral intervention on emotional and cognitive stressors, and were consistent with the results of the present study.12 Although our study showed that teaching coping strategies and group cognitive-behavioral therapy were effective in subscales of personality depersonalization and individual performance, they were not so in emotional exhaustion. The results of the Sedghi Goyaghaj et al. study20 were consistent with the first two components but inconsistent with the subscale of emotional fatigue, which can be explained by the difference in the research environment.
Recent research has shown that the effectiveness of education can be maintained over time, so that despite a decrease in effectiveness after a month, there was still a significant difference in the results before and after the intervention. The results of Lee et al.26 were also consistent with the current study, and found that efficacy was maintained from 6 months to one year.
Conclusion
The results of this study showed that teaching stress-coping strategies and group cognitive-behavioral therapy can be effective in reducing nurse burnout. Therefore, this method can be used to provide counseling services to nurses in health centres.
Acknowledgments
Acknowledgments.The Iran University of Medical Sciences funded this study. The authors would like to thank the nurses of Hazrat Fateme Hospital.
Clinical trial registration.This study was recorded in the Iran Registry of Clinical Trials with the number Irct ID: IRCT201604178177N14 on 2016-06-09.
References
- 1.Akbarbegloo M, Valizadeh L. Occupational tension and coping strategies in nurses in psychological ward - Razi hospital, Tabriz. Mod Care J. 2011;8(1):45–51. [Google Scholar]
- 2.Andolhe R, Barbosa RL, Oliveira EMd, Costa ALS, Padilha KG. Stress, coping and burnout among Intensive Care Unit nursing staff: associated factors. Revista da Escola de Enfermagem da USP. 2015;49(SPE):58–64. doi: 10.1590/S0080-623420150000700009. [DOI] [PubMed] [Google Scholar]
- 3.Manzano-García G, Ayala J-C. Insufficiently studied factors related to burnout in nursing: results from an e-Delphi study. PloS one. 2017;12(4):e0175352. doi: 10.1371/journal.pone.0175352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mooghali A, Habibi H, Ahmadi M, Habibi F. Relationship between job satisfaction and burnout among nurses in public and private hositals in Shiraz City in 2012. Hospital. 2015;14(3):119–126. [Google Scholar]
- 5.Mohammadzadeh A, Maleki S. Investigating the relationship between psychological empowerment and quality of work life with job burnout among health experts of Health Deputy Ilam Province in 2014. SJIMU. 2017;24(6):54–65. [Google Scholar]
- 6.Aghajani MJ. The professional burnout of nurses in different wards. J Res Dev Nurs Midwifery. 2013;9(2):97–104. [Google Scholar]
- 7.Hosseininejad SM, Aminiahidashti H, Montazer SH, Elyasi F. Job burnout among the emergency department nurses of medical training centers affiliated to Mazandaran University of Medical Sciences. Iranian Journal of Emergency Medicine. 2016;3(4):125–131. [Google Scholar]
- 8.Geuens N, Van Bogaert P, Franck E. Vulnerability to burnout within the nursing workforce - the role of personality and interpersonal behaviour. J Clin Nurs. 2017;26(23-24):4622–4633. doi: 10.1111/jocn.13808. [DOI] [PubMed] [Google Scholar]
- 9.Oosterholt BG, Van der Linden D, Maes JH, Verbraak MJ, Kompier MA. Burned out cognition - cognitive functioning of burnout patients before and after a period with psychological treatment. Scand J Work Environ Health. 2012;38(4):358–369. doi: 10.5271/sjweh.3256. [DOI] [PubMed] [Google Scholar]
- 10.Ríos-Risquez MI, García-Izquierdo M. Patient satisfaction, stress and burnout in nursing personnel in emergency departments: a cross-sectional study. Int J Nurs Stud. 2016;59:60–67. doi: 10.1016/j.ijnurstu.2016.02.008. [DOI] [PubMed] [Google Scholar]
- 11.Pourreza A, Monazam MR, Abassinia M, Asghari M. Relationship between job burnout and mental health of nurses working in province of Qom. J Hosp. 2012;11(2):45–54. [Google Scholar]
- 12.Orly S, Rivka B, Rivka E, Dorit S-E. Are cognitive-behavioral interventions effective in reducing occupational stress among nurses? Appl Nurs Res. 2012;25(3):152–157. doi: 10.1016/j.apnr.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 13.Rahmani F, Behshid M, Zamanzadeh V, Rahmani F. Relationship between general health, occupational stress and burnout in critical care nurses of Tabriz teaching hospitals. Iran J Nurs. 2010;23(66):54–63. [Google Scholar]
- 14.Weigl M, Stab N, Herms I, Angerer P. The associations of supervisor support and work overload with burnout and depression: a cross-sectional study in two nursing settings. JAN. 2016;72(8):1774–1788. doi: 10.1111/jan.12948. [DOI] [PubMed] [Google Scholar]
- 15.Ruotsalainen JH, Verbeek JH, Mariné A, Serra C. Preventing occupational stress in healthcare workers. The Cochrane Library. 2015 doi: 10.1002/14651858.CD002892.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mohammadzadeh A, Maleki S. Investigating the relationship between psychological empowerment and quality of work life with job burnout among health experts of Health Deputy Ilam Province in 2014. SJIMU, 2017;24(6):54–65. [Google Scholar]
- 17.Stenlund T, Ahlgren C, Lindahl B, Burell G. Cognitively oriented behavioral rehabilitation in combination with Qigong for patients on long-term sick leave because of burnout: REST - a randomized clinical trial. Int J Behav Med. 2009;16(3):294. doi: 10.1007/s12529-008-9011-7. [DOI] [PubMed] [Google Scholar]
- 18.Sandahl C, Lundberg U, Lindgren A. Two forms of group therapy and individual treatment of work-related depression: a one-year follow-up study. Int J Group Psychother. 2011;61(4):538–555. doi: 10.1521/ijgp.2011.61.4.538. [DOI] [PubMed] [Google Scholar]
- 19.Free ML. Cognitive therapy in groups: guidelines and resources for practice. John Wiley & Sons. 2007 [Google Scholar]
- 20.Sedghi Goyaghaj N, Rostami M, Khosrozadeh M, Hosseini M. Effect of positive thinking skills training on nurse’s job burnout. J Nurs Educ. 2016;3(4):38–47. [Google Scholar]
- 21.Abdi F, Khaghanizade M, Sirati M. Determination of the amount burnout in Nursing Staff. J Behav Sci. 2008;2(1):51–59. [Google Scholar]
- 22.Sahebzadeh M, Karimi S, Hosseini SM, Akhtar DG, Hosseini S. Job burnout of nursing administrators and chief executive officers in University Hospitals and its relation to their demographic features. Health Inf Manag J. 2011;7:637–648. [Google Scholar]
- 23.Xie Z, Wang A, Chen B. Nurse burnout and its association with occupational stress in a cross-sectional study in Shanghai. JAN. 2011;67(7):1537–1546. doi: 10.1111/j.1365-2648.2010.05576.x. [DOI] [PubMed] [Google Scholar]
- 24.Gómez-Urquiza JL, Vargas C, De la Fuente EI, Fernández-Castillo R, Cañadas-De la Fuente GA. Age as a risk factor for burnout syndrome in nursing professionals: a meta-analytic study. Res Nurs Health. 2017;40(2):99–110. doi: 10.1002/nur.21774. [DOI] [PubMed] [Google Scholar]
- 25.Abdo S, El-Sallamy R, El-Sherbiny A, Kabbash I. Burnout among physicians and nursing staff working in the emergency hospital of Tanta University, Egypt. E Mediterr Health J. 2015;21(12):906. doi: 10.26719/2015.21.12.906. [DOI] [PubMed] [Google Scholar]
- 26.Lee H-F, Kuo C-C, Chien T-W, Wang Y-R. A meta-analysis of the effects of coping strategies on reducing nurse burnout. Appl Nurs Res. 2016;31:100–110. doi: 10.1016/j.apnr.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 27.Bahrainian A, Khanjani S, Masjedi AA. The eficacy of group acceptance and commitment therapy (act)-based training on burnout in nurses. Police Medicine. 2016;5(2):143–152. [Google Scholar]


