Abstract
Children with autism spectrum disorder (ASD) exhibit significant difficulties with emotion regulation. Respiratory sinus arrhythmia (RSA) is a biomarker for processes related to emotion regulation, with higher baseline rates linked to beneficial outcomes. Although reduction in RSA in response to challenge can index adaptive processes in community samples, excessive withdrawal may suggest loss of regulatory control among children with clinical concerns. Psychophysiological risk for problems may be protected against or exacerbated by parenting environments more or less supportive of the development of children’s regulatory competence. RSA was examined in 61 children with ASD ages 6 to 10 years in relation to externalizing behavior, and parenting was considered as a moderator. RSA was obtained during laboratory tasks and positive parenting, negative parenting, and children’s externalizing behaviors were each indexed through multiple methods. RSA reactivity interacted with negative, but not positive parenting. Higher RSA reactivity was associated with more externalizing behavior under conditions of higher negative parenting, but with lower externalizing behavior at lower levels of negative parenting. Similarly, negative parenting was only associated with externalizing behaviors in the context of high child RSA reactivity. Implications for our understanding of emotion regulation in children with ASD, and for related interventions are discussed.
Keywords: autism spectrum disorder (ASD), respiratory sinus arrhythmia (RSA), externalizing behavior problems, parenting, psychophysiology, emotion regulation
Autism spectrum disorder (ASD) is a neurodevelopmental condition characterized by deficits in social communication and the presence of restricted and/or repetitive behaviors (American Psychiatric Association, 2013). Although externalizing behaviors (e.g., non-compliance, aggression, disruptiveness) are not included in the diagnostic criteria for ASD, these challenges are common in children with ASD (McClintock, Hall, & Oliver 2003) and cause significant distress for both the children and the adults supporting them (Caplan, Feldman, Eisenhower, & Blacher, 2016; Lecavalier, Leone, & Wiltz, 2006; Shawler & Sullivan, 2017). Externalizing problems can interfere with learning opportunities, impair functioning, and lead to more restrictive educational environments for children with ASD (Koegel, Koegel, & Surratt, 1992; Lauderdale-Littin, Howell, & Blacher, 2013).
Although many factors can contribute to the development of externalizing problems, these behaviors in children with ASD are often thought to be related to underlying challenges with emotion regulation (Mazefsky, Pelphrey, & Dahl, 2012; Samson, Hardan, Lee, Phillips, & Gross, 2015). Indeed, children with ASD exhibit more behaviors reflective of emotion dysregulation, fewer strategies considered beneficial for regulation, and diminished effects of regulatory efforts compared to children without ASD (Jahromi, Meek, & Ober-Reynolds, 2012; Mazefsky & White, 2014; Samson et al., 2015).
Respiratory Sinus Arrhythmia (RSA)
Autonomic nervous system activity is one route to better understanding the biological underpinnings of reactivity and regulation in children with ASD (see Benevides & Lane, 2015). This system is comprised of the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). SNS activity is often referred to as the “flight or fight” response, which involves an increase in arousal related to risk assessment, reward motivation, and/or inhibitory efforts (Beauchaine, 2001). The PNS is the arousal “brake,” slowing heart rate and reducing arousal through increased output of the vagus nerve (Beauchaine, 2015a; Benevides & Lane, 2015). In this way, PNS activity is a substrate and psychophysiological index of emotion regulation (Beauchaine, 2015b). PNS activity is typically measured through respiratory sinus arrhythmia (RSA), as indexed by high-frequency heart-rate variability related to respiratory patterns.
RSA is commonly measured as a baseline level or through reduction in RSA in response to a challenge (RSA reactivity). Higher baseline RSA is thought to index better emotion regulation abilities and is associated with a host of desirable child outcomes, whereas lower baseline RSA is observed across several forms of psychopathology (Beauchaine, 2015b). RSA reactivity is more complicated in its interpretation, and may depend upon the population studied and the nature of the challenge (Beauchaine, 2015a; Beauchaine et al., 2019; Graziano & Derefinko, 2013; Obradović, Bush, & Boyce, 2011). RSA reactivity (i.e., reduction in RSA) in response to a challenge is often considered beneficial in community samples, in that this process allows for an efficient and incremental increase in arousal to address the demands of the situation, as well as greater SNS activation when needed (Graziano & Derefinko, 2013). Alternatively, higher RSA reactivity (higher withdrawal) in response to challenge may reflect a loss of regulatory control, particularly for children with clinical concerns, resulting in behavior more heavily driven by the SNS (Beauchaine, 2015a; Beauchaine et al., 2019).
Although the evidence is somewhat mixed, several studies have found lower baseline RSA as a function of ASD status (Benevides & Lane, 2015). In one of the few studies to examine RSA reactivity in ASD, Vaughn Van Hecke et al. (2009) found higher RSA reactivity to a video of an unfamiliar person in children with ASD relative to peers without ASD. The few studies that have examined RSA and individual differences among children with ASD have linked higher RSA baseline to better social skills (Bal et al., 2010; Guy, Souders, Bradtreet, DeLussey, & Herrington, 2014).
RSA and Externalizing Behavior
Several studies have linked lower baseline RSA with externalizing behavior in children without ASD (see Beauchaine, Gatzke-Kopp, & Mead, 2007; Beauchaine, 2015b). The only identified study to date that has examined RSA in relation to externalizing behavior in children with ASD was conducted by Neuhaus, Bernier, and Beauchaine (2014). However, the association between baseline RSA and externalizing behavior, which was low and not statistically significant, was presented only for the entire sample, which included children without ASD. Moreover, in a regression involving the full sample in which social skills were controlled, externalizing behaviors exhibited an unexpected positive relation to baseline RSA.
The current study examined RSA in children with ASD between the ages of 6 and 10 years. This age range represents an important period for parental influence on emotion regulation in children both with ASD (Fenning, Baker, & Moffitt, 2018) and without ASD (Morris, Silk, Steinberg, Myers, & Robinson, 2007), and falls within the ages included in previous examinations of the effects of physiology on externalizing behavior in this population (e.g., Baker et al., 2018a; Neuhaus et al., 2014; Vaughn Van Hecke et al., 2009). Based upon the literature, it was hypothesized that higher baseline RSA would be associated with lower externalizing behavior, and that higher RSA reactivity would be associated with higher externalizing behavior. To the extent that children with ASD experience challenges with regulation and may have relatively low baseline RSA, higher RSA reactivity (i.e., reduction in RSA) could yield very low levels of RSA that reflect loss of regulatory control among these children.
RSA × Parenting Interactions
Several theories propose person-by-environment processes wherein certain developmental outcomes are a function of interactions between child characteristics and parenting. The dual-risk perspective, also known historically as the diathesis-stress perspective, proposes that some children are more vulnerable to poor environments than others based upon biological risk factors (Heim & Nemeroff, 1999; Roisman et al., 2012). Differential-susceptibility theory similarly suggests that certain children have biological profiles that sensitize them to poor environments, but also argues that these same profiles allow children to take advantage of supportive environments (Belsky, Bakermans-Kranenburg, & van IJzendoorn, 2007; Roisman et al., 2012). Boyce & Ellis (2005) proposed the biological-sensitivity-to-context model, which is consistent with the differential susceptibility hypothesis, but more specifically identifies psychophysiological reactivity as a key index and mechanism of sensitivity to both adverse and advantageous environmental conditions.
Consistent with person-by-environment models, interactions between SNS reactivity and parenting have predicted child externalizing behavior in several studies of children with ASD (Baker et al., 2018a; Baker, Fenning, Howland, & Huynh, 2018b) and without ASD (Erath, El-Sheikh, Hinnant, & Cummings, 2011; Kochanska et al., 2015). RSA reactivity and parenting have also interacted in research on children with neurotypical development. Dyer, Blocker, Day, and Bean (2016) found that, among boys, the highest rates of externalizing problems were observed when high RSA reactivity was combined with more authoritarian maternal parenting styles. Similarly, Obradović et al. (2011) found that high RSA reactivity to a cognitively-based stressor appeared to strengthen the relation between exposure to marital conflict and children’s externalizing problems. No published studies have tested interactions between RSA reactivity and parenting in children with ASD.
The Current Study
The current study tested interactions between RSA reactivity and both positive and negative aspects of parenting in children with ASD. We hypothesized that higher RSA reactivity would be less positively related to externalizing behavior in the context of more optimal parental support (i.e., higher positive and lower negative parenting) and, likewise, that stronger associations between parenting and externalizing behavior would be found for children with higher RSA reactivity. Including positive and negative environmental conditions allowed a more complete comparison of dual-risk and biological-sensitivity-to-context models than most prior studies that included only measures of adverse environmental conditions.
In examining RSA reactivity, it is important to be attentive to the nature of the stressor (Beauchaine, 2015b; Beauchaine et al., 2019). In a learning context, high reactivity to frustration when attempting to complete a requested task may elicit disruptive behaviors in children with ASD (Mohammadzaheri, Koegel, Rezael, & Bakhshi, 2015). As such, we measured RSA reactivity during a task that specifically involved asking the child to engage in a frustrating activity—in this case, tracing a star using only a mirror image as a guide (El-Sheikh, 2005).
The current study was also concerned with robust, multi-method assessment of the variables of interest. We included multiple indices of positive parenting, each of which involved careful coding. Parental co-regulatory scaffolding has proven to be a powerful factor in the development of children with developmental disabilities (e.g., Baker, Fenning, Crnic, Baker, & Blacher, 2007; Fenning & Baker, 2012), and has been identified as a moderator for links between SNS risk and externalizing behavior in children with ASD (Baker et al., 2018a). Parental warm attitudes, as coded through a parent speech sample, are negatively associated with externalizing problems in children (Baker et al., 2018b) and adults with ASD (Woodman, Mailick, & Greenberg, 2016). Similarly, we utilized both coding and questionnaire data in our composite of negative parenting. Critical parent attitudes, as coded during the aforementioned speech sample, have been established as a fairly reliable correlate of externalizing behavior in children with ASD (Baker et al., 2018b), with evidence for a causal pathway from criticism to behavior problems (rather than vice-versa) in adolescents and adults with ASD (Greenberg, Seltzer, Hong, & Orsmond, 2006). Harsh parenting, as measured by questionnaire, has been examined in numerous studies of psychophysiology and externalizing problems in samples without ASD (e.g., Erath et al., 2011). Finally, consistent with the only other previous study examining RSA in relation to externalizing behavior in ASD (Neuhaus et al., 2014), we utilized parent-report on a child behavior checklist for our main outcome measure, and this measurement was augmented with a symptom count from a structured diagnostic interview for clinical symptoms of oppositional defiant disorder, which co-occurs with ASD at rates as high as 37% (Kaat & Lecavalier, 2013).
Method
Participants
An initial sample of 77 children with ASD ages 6 to 10 years and their primary caregivers participated in a laboratory visit that included child assessment, psychophysiological data collection, structured parent-child tasks, parent interview, and parent completion of questionnaires. Children with an existing ASD diagnosis provided by a physician or psychologist were recruited from the community and from local service providers via flyers. Exclusionary criteria for the child included the presence of a genetic disorder of known etiology and significant motor impairment that would prevent task engagement.
Of the original 77 children, 11 refused the electrodes for measurement of RSA, and RSA data were determined to be artifactual for 5 additional children (e.g., noise or loss of signal due to pulling on electrode wires). Missing data analyses revealed no significant differences between the 16 children without usable RSA data and those included in the study except that missing data occurred more frequently for males (25% missing) as compared to females (0%), χ2 = 4.89, p =.03, and for children with higher ASD symptom scores, t = 2.43, p = .02, d = .63. Missing data were not significantly related to estimated IQ, t = −1.59 p = .18, d = .41.
The remaining sample of 61 children (74% male) was diverse with regard to intellectual ability and ASD symptom levels (see Table 1), with estimated IQ ranging from 47 to 121. The majority of the families identified their children as Hispanic (47%), 33% were Caucasian, non-Hispanic, 5% were Asian American, 5% were African American, 3% identified as “other,” and 8% identified their children as “multi-ethnic/racial.” The median annual family income was between US$50,000 and 70,000. The majority of primary caregivers were married (71%) and 3% of the primary caregivers were fathers. Nineteen (31%) of the children were taking medication, most commonly for attention problems/hyperactivity (13%), asthma (8%), allergies (7%) or seizures (5%). No children were reported to be taking SSRIs, which are sometimes related to RSA measurements (Beauchaine et al., 2019).
Table 1.
Descriptive Statistics and Correlations among Variables of Interest (n=61).
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | M (SD) | |
|---|---|---|---|---|---|---|---|---|
| 1. Age in Years | -- | 7.95 (1.48) | ||||||
| 2. IQ | −.23+ | -- | 80.02 (20.68) | |||||
| 3. ASD Symptom Level | −.06 | −.11 | -- | 7.21 (2.06) | ||||
| 4. RSA Baseline | .36** | −.25+ | .04 | -- | 5.96 (1.17) | |||
| 5. RSA Reactivity | −.02 | −.00 | .06 | .00 | -- | 0.00a (0.73) | ||
| 6. Positive Parenting | .01 | −.02 | −.15 | .01 | −.07 | -- | 0.01b (0.62) | |
| 7. Negative Parenting | −.09 | .08 | −.04 | −.19 | .14 | −.05 | -- | −0.01b (0.80) |
| 8. Externalizing Composite | −.26* | .26* | −.08 | .03 | .03 | −.10 | .17 | 0.01b (0.91) |
Note: ASD = Autism spectrum disorder; RSA = Respiratory sinus arrhythmia
Scores represent residuals from a regression.
Composites were generated by averaging standardized scores.
p<.10,
p<.05,
p<.01
Procedures
All procedures were approved by our institutional review board. Parents consented for themselves and for their children, and assent was obtained from children.
RSA data collection.
Following consent, the children were seated at a table that faced a small television on a stand in front of them. A wall was to the children’s left and a temporary partition was placed to the children’s right, behind which the parent eventually was seated. The electrodes were placed on the child by a female research assistant with the help of the parent. Electrodes were placed on the lower ribs and on the right clavicle. A short adjustment period occurred during which the data acquisition systems were checked for appropriate signal and then a three-minute baseline procedure was performed. This baseline involved viewing a series of nature slides on the television that included scenes of trees, water, mountains, etc. (Erath, Bub, & Tu, 2016). Parents were asked beforehand if they felt that their children had any particular interests in, or fears of, these types of stimuli and none were reported. A video camera mounted high above the television recorded the child for later data assurance and allowed the parent to view the child from behind the partition. The child then engaged in the three-minute challenging task. As in previous studies that utilized this task to elicit physiological arousal related to negative emotion (e.g., El-Sheikh, 2005), the children were given a pencil and a structure was placed in front of them that allowed them to attempt to trace a star with only an indirect view of their hand and the paper by way of a mirror. This process reverses the directionality of the image, making the task difficult to perform. Despite the large range of cognitive functioning present in our sample, every child was judged to have understood the request for basic tracing, and each child demonstrated sufficient motor skills to engage with the task.
Scaffolding task.
Following the RSA data collection, the parents and children were asked to engage in a series of interactive tasks, including one from which the measure of parental scaffolding was obtained. In this task, which has been used several times by our laboratory and others with children with ASD and related disabilities (Baker et al., 2007; 2018a), the dyad was provided with colorful block tiles and a photo of a completed puzzle. The child was instructed to make the structure depicted in the photo. The parent was asked to let the child try it on his or her own, and then to provide any help that the parent deemed necessary. The experimenter returned after five minutes.
Parent speech sample.
A five-minute speech sample was completed with the parent in a separate room from the child (Daley & Benson, 2008). The experimenter asked the parent to speak uninterrupted for five minutes about the child and his or her relationship with the child. The speech was audiotaped and coded for warmth and criticism.
Parent interview and forms.
Parents reported on their children’s externalizing behavior problems using a child behavior checklist, and were also interviewed individually about their children’s symptoms of oppositional defiant disorder using a module from a structured diagnostic interview.
Measures
Diagnostic confirmation and ASD symptom level.
Diagnostic confirmation was primarily based upon the existence of an ASD diagnosis by a community physician or psychologist, and evidence that the child met the criterion for an autism spectrum classification on our laboratory administration of the Autism Diagnostic Observation Schedule-2 (ADOS-2; Lord et al., 2012). The ADOS-2 is a semi-structured assessment that facilitates observation and recording of child behaviors related to language, social communication, play, repetitive behaviors, and restricted interests and was performed by assessors certified as research reliable in the system. Most children (66%) received Module 3, 26% were tested with Module 2, and 8% received Module 1. The ADOS-2 comparison score was used to characterize the sample according to overall ASD symptom severity and to provide a robust measure of ASD symptom levels for consideration as a covariate. The comparison score allows for examination of symptom levels across different modules, with 1 indicative of minimal to no evidence of ASD-related symptoms, and 10 reflecting a high level of symptoms.
Five children did not meet the ADOS-2 criterion for an ASD classification, but were retained in the current sample following completion of an in-depth, multi-method clinical best estimate by a licensed clinical psychologist with research reliability in the ADOS-2 and significant expertise in ASD assessment. All five children met clinical criteria on the Social Responsiveness Scale-2 (SRS-2; Constantino & Gruber, 2012), a widely-used parent report measure of ASD symptoms, and all but one also met criteria on the Social Communication Questionnaire, Lifetime Version (SCQ; Rutter, Bailey, & Lord, 2003), a screening instrument based on the Autism Diagnostic Interview-Revised (ADI-R; Rutter, LeCouteur, & Lord, 2003).
Child IQ.
An estimate of child IQ was obtained using the Stanford-Binet 5 ABIQ (Roid, 2003). The ABIQ is comprised of two subscales with high loading on g: a Matrix Reasoning task that assesses non-verbal fluid reasoning and a Vocabulary task that evaluates expressive word knowledge. The Stanford-Binet 5 has sound psychometric properties and has been used previously for children with ASD (Matthews et al., 2015; Roid, 2003).
Respiratory sinus arrhythmia (RSA).
RSA was measured with a MindWare data acquisition system (MindWare Technologies, Inc., Gahanna, OH). Electrocardiography data were collected through disposable Ag-AgCl electrodes placed on participants’ right clavicle and lower left and right ribs. Data were sampled at 500 Hz, and RSA scores were quantified using spectral analysis (Berntson et al., 1997) with MindWare HRV analysis software (version 3.0.22) as the natural log of the variance in heart period within age-adjusted respiratory frequency bands (e.g., .27 – .50 Hz for 9-year-old children, .25 – .50 Hz for 10-year-old children; see Shader et al., 2018, for additional ranges). RSA was expressed in units of ln(ms2). Possible artifacts were flagged by an algorithm that detects improbable interbeat intervals, allowing visual inspection and editing when necessary; relatively few artifacts were detected and these were corrected manually (Berntson et al., 1997). RSA reactivity (RSA-R) was calculated as the residual of the regression of RSA during the star-tracing period on RSA during the baseline period (Burt & Obradović, 2013). Residualized change scores were multiplied by −1 so that higher RSA-R scores indicated greater reductions in RSA (i.e., greater withdrawal) from the baseline to the star-tracing period.1
Warmth and criticism.
Parental warmth and critical comments were each coded in accordance with the guidelines from the Autism Five-Minute Speech Sample (Daley & Benson, 2008). Warmth was indexed by the intensity of the feeling expressed by the parent about the child as represented by a positive and enthusiastic tone, spontaneous expressions of affection, love, appreciation, etc., and signs of concern and empathy, and was coded 1 (low), 2 (moderate) or 3 (high). Critical comments were measured through a frequency count of statements that criticize or find fault with the child. These comments include a present-tense negative description of the child’s personality or an account of problematic behavior delivered with a harsh tone or an indication of strong dislike or dissatisfaction. Psychometric support for this system has been provided in the form of high test-retest and inter-rater reliability, and associations with relevant child and family factors (Baker et al., 2018b; Benson, Daley, Karlof, & Robison, 2011). Reliability for the current sample, based upon 47% of cases, was ICC (absolute agreement) = .82 for critical comments, and kappa = .85 for warmth.
Scaffolding.
Parental support was coded from videotapes of the dyadic problem-solving task using the Parental Scaffolding Observation System (Hoffman, Crnic, & Baker, 2006). This system considers parents’ ability to provide motivational, emotional, and technical support to their children during a challenging activity. Motivational scaffolding includes the ability of the parent to recruit the child’s attention to the task, foster enthusiasm for the task, and to refocus the child should he or she become distracted. Emotional scaffolding scores reflect a parent’s ability to provide co-regulatory emotional support to the child and to contribute to the child’s feelings of accomplishment. Technical scaffolding evaluates the parent’s ability to provide structure and support for the child with regard to the task through instruction, guidance, prompting, and/or modification of the task or goal. Each of these subscales is rated from 1 (very low or absent support) to 5 (characteristically high support). These subscales are highly positively correlated and the measure is most commonly used as an average overall score (Baker et al., 2007). Inter-rater reliability based on 25% of cases was ICC = .73.
Harsh discipline.
Harsh discipline was measured with items from the Alabama Parenting Questionnaire (Frick, 1991). Our harsh discipline scale included two of the three items from the Corporal Punishment scale, with the item asking about hitting with a “belt, switch, or other object” omitted given its potential overlap with physical maltreatment, which we did not wish to capture. This item was replaced with the item reflecting harsh verbal discipline (“You yell or scream at your child when he/she has done something wrong.”), in order to provide a more complete measure of harsh discipline. The alpha for this scale was .60.
Externalizing behavior.
Externalizing behavior was partially indexed by parent report using the standardized Externalizing Scale T-score from the age-appropriate version of the Child Behavior Checklist (Achenbach, 2009), a widely-used measure with demonstrated validity in children with ASD (e.g., Pandolfi, Magyar, & Dill, 2012). Parents were also interviewed using the oppositional defiant disorder subscale of the Diagnostic Interview Schedule for Children (DISC; Costello, Edelbrock, & Costello, 1985; Shaffer et al., 2000), a structured, computer-facilitated diagnostic interview based upon criteria from the Diagnostic and Statistical Manual (American Psychiatric Association, 2013). The DISC has been used in previous studies to assess comorbid behavior disorders in children with neurodevelopmental disabilities (B. Baker, Neece, Fenning, Crnic, & Blacher, 2010). The current study considered the total number of ODD symptoms endorsed. Only the ODD module was administered due to meta-analytic findings suggesting fairly low rates of conduct disorder among children with ASD (e.g., 4%) as opposed to ODD (about 30% to 37%; Kaat & Lecavalier, 2013; Simonoff et al., 2008).
Data Analysis Plan
Composites for positive parenting, negative parenting, and child externalizing behavior were constructed on a theoretical basis regardless of the association between the relevant variables. Additional post-hoc analyses were performed for any individual component variables that were not significantly related in the predicted direction. Bivariate correlations were then considered, followed by two hierarchical regressions used to test study hypotheses. The first regression tested hypothesized main effects of RSA baseline and reactivity, and whether RSA reactivity interacted with positive parenting. The second regression tested the interaction between RSA reactivity and negative parenting. Significant interactions were followed up with estimates of the relevant simple slopes at the mean of the moderator, as well as 1 SD below and 1 SD above the mean. Regions of significance (RoS) analyses were conducted to consider the degree to which the interactions suggested dual-risk or biological-sensitivity-to-context models (Roisman et al., 2012).
Results
Consistent with previous studies (Baker et al., 2018b; Benson et al., 2011), most parents were rated moderate (63%) or high (30%) on warmth on the AFMSS. Similarly, average scaffolding was in the moderate to moderately high range (M = 3.56, SD = 0.82), and parents were relatively low on critical comments (M = 2.28, SD = 2.36) and harsh discipline (M =1.49, SD = 0.51). Consistent with meta-analytical findings for negative emotion induction tasks (Beauchaine et al., 2019), children demonstrated significant RSA withdrawal as a group when moving from the baseline (M = 5.96, SD == 1.17) to challenge task (M = 5.65, SD = 1.19), t = 3.17, p < .002, d = .41. The current sample mean for externalizing behavior on the CBCL fell at the threshold for “borderline” clinical problems (M = 59.62, SD = 9.44), with almost a third (30%) falling within the clinical range. Similarly, and consistent with previous reports (Kaat & Lecavalier, 2013; Simonoff et al., 2008), 34% of the sample met criteria for ODD on the DISC (M = 2.49, SD = 2.71).
Parental critical comments and harsh discipline scores each exhibited some skew and were normalized through square-root transformation. These variables were positively correlated, r = .33, p = .015, and were standardized and averaged to generate the negative parenting composite. The association between parental warmth and scaffolding suggested an unexpected inverse association, r = −.23, p = .08. Subsequently, analyses were performed for the overall positive parenting variable, but also for warmth and scaffolding separately.2 Scores for the children on the CBCL and the DISC ODD symptom scales were highly positively correlated, r = .70, p < .001, and were standardized and averaged for the externalizing behavior composite.
Lower child age and higher estimated IQ were each significantly related to higher externalizing behavior and were controlled in subsequent analyses (see Table 1). Medication use to treat inattention/hyperactivity was related to higher baseline RSA, t = −2.62, p = .011, d = .68; however, this variable was not related to any other variable of interest and did not alter results when controlled or when RSA scores were adjusted prior to analysis. No other demographic variable or aspect of medication status was related to either RSA measures or the outcome variable. All variables were mean-centered for inclusion in the regressions. Child age and estimated IQ were entered on the first step of the first regression, along with RSA baseline, RSA reactivity and positive parenting (Table 2). The interaction between the latter two variables was added on the second step. Neither RSA baseline nor reactivity was significantly related to externalizing behavior, nor was the interaction between RSA reactivity and positive parenting. Analyses treating each of the positive parenting variables separately were similarly not significant for either warmth, ß = −.27, p = .055, or scaffolding, ß = .16, p = .386.
Table 2.
Hierarchical Linear Regressions Predicting from RSA Reactivity and Parenting to Externalizing Composite
| Positive Parenting to Externalizing Composite | Negative Parenting to Externalizing Composite | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | ß | t | p | R2 | B | SE | ß | t | p | R2 | |
| Step 1 | ||||||||||||
| Age | −.17 | .08 | −.29 | −2.01* | .049 | .150 | −.16 | .08 | −.27+ | −1.99+ | .051 | .168 |
| IQ | .01 | .01 | .24+ | 1.88+ | .066 | .01 | .01 | .24+ | 1.88+ | .066 | ||
| RSA baseline | .15 | .11 | .19 | 1.40 | .167 | .17 | .11 | .22 | 1.61 | .112 | ||
| RSA reactivity | .04 | .16 | .03 | 0.27 | .792 | .02 | .15 | .02 | 0.13 | .898 | ||
| Parenting | −.14 | .18 | −.10 | −0.78 | .436 | .20 | .15 | .17 | 1.36 | .179 | ||
| Step 2 | ||||||||||||
| Age | −.16 | .08 | −.26+ | −1.93+ | .059 | .153 | −.17 | .08 | −.28* | −2.20* | .032 | .257 |
| IQ | .01 | .01 | .24+ | 1.78+ | .080 | .01 | .01 | .24+ | 1.93+ | .059 | ||
| RSA baseline | .15 | .11 | .20 | 1.44 | .156 | .17 | .10 | .21 | 1.65 | .105 | ||
| RSA reactivity | .07 | .16 | .05 | 0.40 | .691 | −.05 | .15 | −.04 | −0.31 | .759 | ||
| Parenting | −.14 | .19 | −.09 | −0.73 | .468 | .10 | .14 | .09 | 0.71 | .478 | ||
| RSA reactivity × Parenting | −.14 | .28 | −.07 | −0.49 | .624 | .64 | .25 | .32* | 2.55* | .014 | ||
Note: ASD = Autism spectrum disorder; RSA = Respiratory sinus arrhythmia. Confidence interval for the significant interaction was 0.14 to 1.15.
p<.10,
p<.05
In the second regression, negative parenting replaced positive parenting. RSA reactivity interacted with negative parenting in the prediction of the externalizing composite (Table 2). Follow up analyses revealed that higher RSA-R predicted more externalizing behavior in the context of high negative parenting, t = 2.04, p = .045, d = .53, did not predict at medium levels, t = −0.36, p = .717, d = .09, and was associated with fewer externalizing behaviors at lower levels of negative parenting, t = −2.07, p = .043, d = .53 (Figure 1). RoS analyses suggested that the interaction was significant at levels of negative parenting higher than .075 and lower than −0.73 (each well within the observed range of scores). Considering RSA-R as a moderator of parenting, negative parenting was only related to higher externalizing behavior in the context of high RSAR, t = 2.84, p = .006, d = .73, but not at medium, t = 0.72, p = .474, d = .19, or low levels of RSA-R, t = −1.42, p = .161, d = .37 (Figure 2). RoS analyses indicated that negative parenting related to externalizing behaviors at levels of RSA-R higher than 0.28 (within the range of observed scores).
Figure 1.
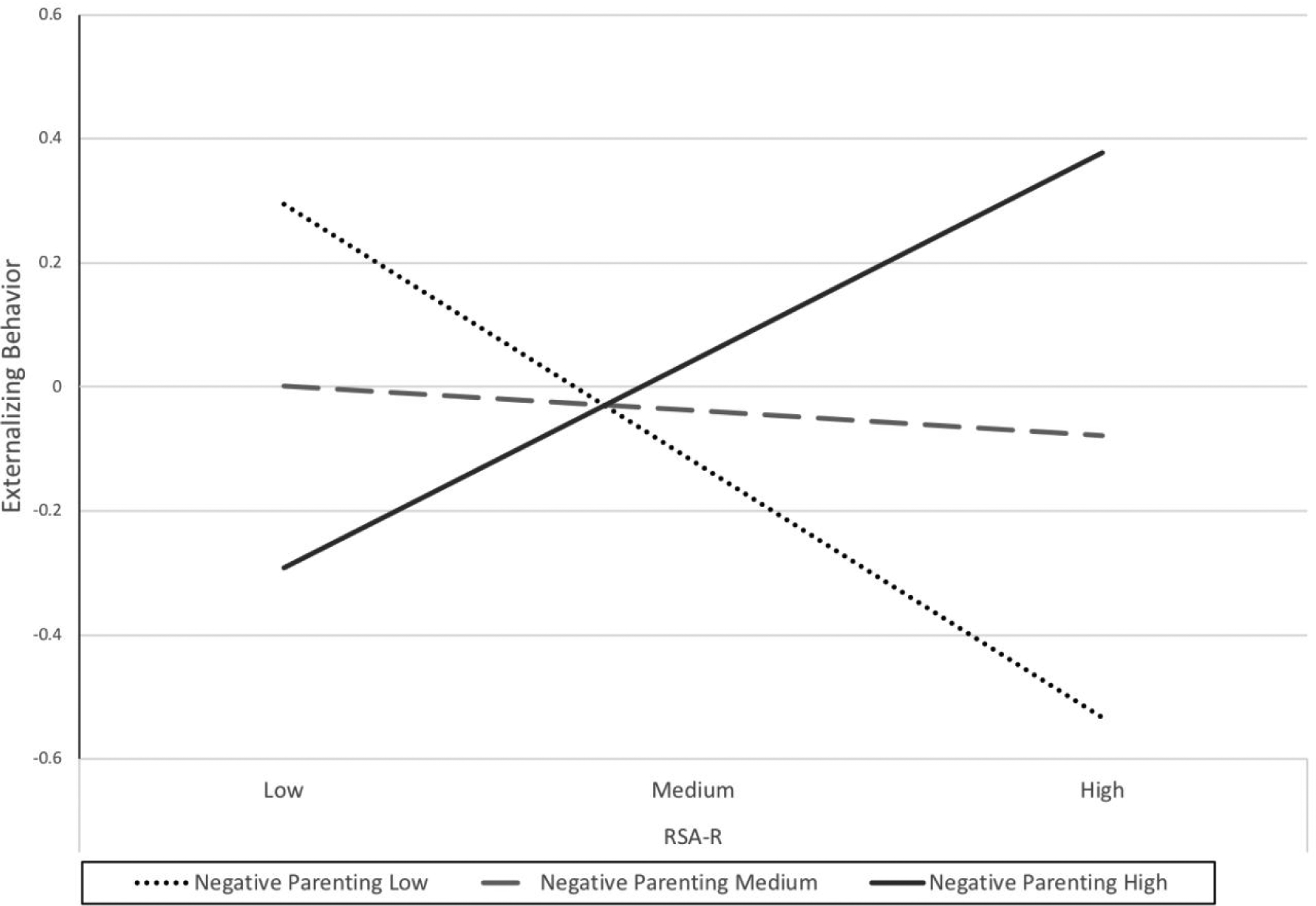
Negative parenting moderating the association between respiratory sinus arrhythmia reactivi1ty (RSA-R) and externalizing behavior.
Figure 2.
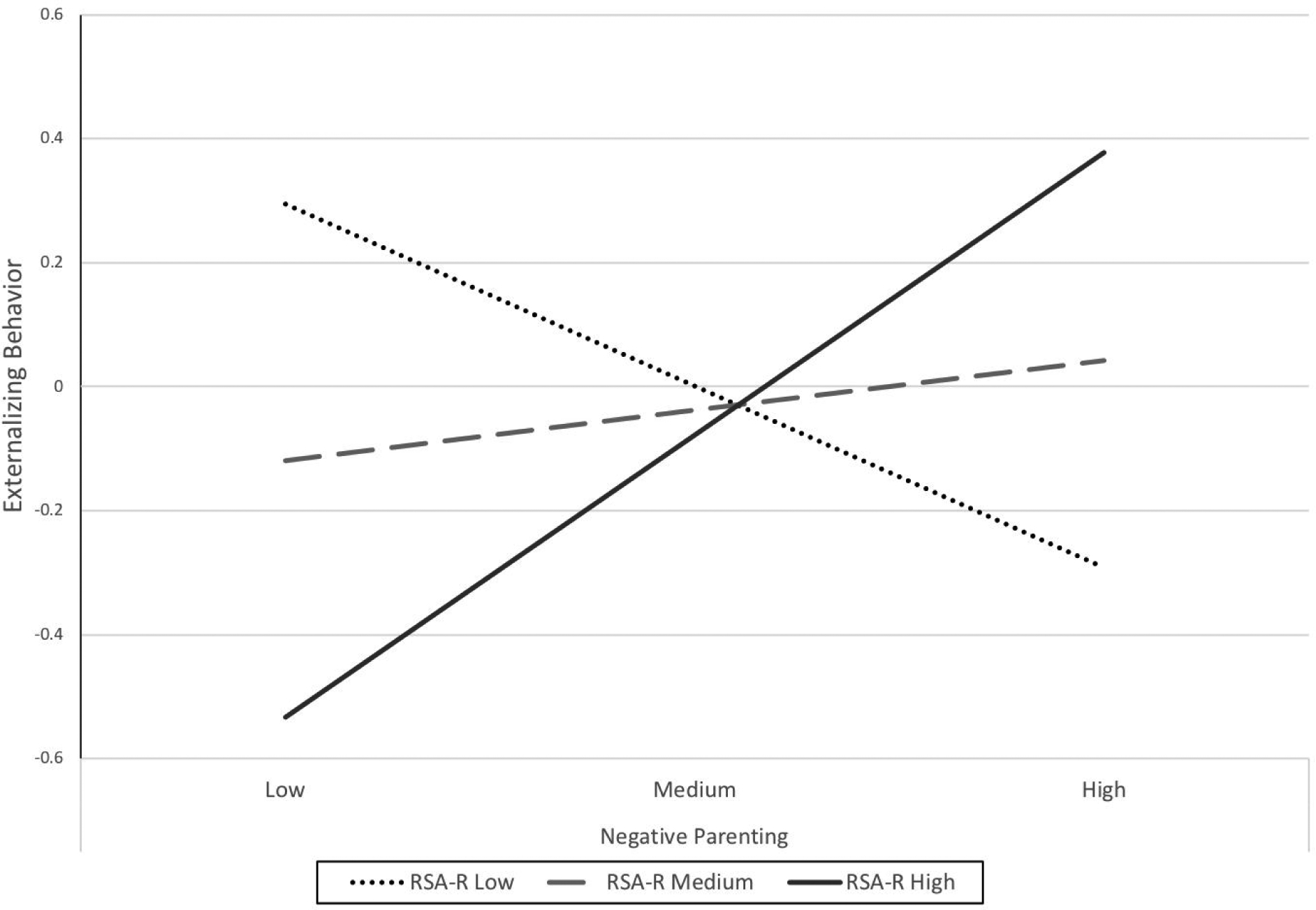
Respiratory sinus arrhythmia reactivity (RSA-R) moderating the association between negative parenting and externalizing behavior.
Discussion
The current study examined relations between measures of respiratory sinus arrhythmia (RSA) and externalizing behavior in children with ASD, and the potential for parenting to buffer or strengthen these associations. RSA reactivity to challenge interacted with negative parenting, but not positive parenting, in the prediction of child externalizing behavior. The significant interaction finding suggests slightly different interpretations depending upon which predictor is considered the moderator.
Follow-up analyses that considered parenting as the moderator suggested that variation in negative parenting alters the association between higher RSA reactivity and externalizing behavior. Lower levels of negative parenting may allow the increased child arousal reflected in RSA withdrawal to be channeled into task engagement, whereas higher levels of parental negativity in the context of higher child RSA reactivity may promote dysregulation, perhaps through further escalation of arousal or engagement in coercive exchanges (Beauchaine & Zalewski, 2016).
When RSA reactivity was considered as the moderator of environmental effects, there was some support for a biological-sensitivity-to-context/differential-susceptibility model. Variation in negative parenting was associated with externalizing behavior only for children exhibiting higher RSA reactivity. Moreover, while higher RSA reactivity was associated with higher externalizing behavior in the context of high levels of negative parenting, higher RSA reactivity actually predicted significantly lower externalizing behavior at the low end of negative parenting as well. Effects of RSA reactivity at both high and low negative parenting suggest that high RSA reactivity may represent an increased sensitivity to environmental effects, for better and for worse (Belsky et al., 2007; Roisman et al., 2016). Of course, the lack of any significant interactions between RSA reactivity and positive parenting limit the evidence for biological sensitivity to variations in negative parenting only. Physiological sensitivity to the effects of negative parenting are consistent with recent findings that children with ASD who exhibited higher SNS reactivity appeared more susceptible to the effects of parental criticism than those with lower SNS reactivity; however, those findings suggested a dual-risk rather than a differential susceptibility process (Baker et al., 2018b).
It is important to recognize that no significant association between parenting and children’s externalizing behavior was present for children with lower levels of RSA reactivity. These findings, along with the elevated externalizing scores for the sample as a whole, may validate the experience of parents of some children with ASD whose behavior problems persist despite the delivery of what is generally considered to be beneficial parenting.
The lack of a direct main effect of baseline RSA on child behavior in the current study could partially be due to challenges in obtaining a true baseline for children with ASD. Although we utilized a relatively common protocol, the proper paradigm for establishing baseline for psychophysiology among children with clinical difficulties is debated (see Beauchaine, 2015a; Beauchaine et al., 2019). For children with ASD in particular, a new and potentially intimidating laboratory setting may have already activated the psychophysiological processes of interest. It is therefore possible that the current baseline represented a “snapshot” of an already dynamic process.
The observed absence of a positive association between parental warmth and scaffolding was unexpected. It is possible, however, that parents’ warm attitudes towards their children with ASD may be distinct from their scaffolding, which taps motivating, co-regulating, and teaching the child (Grusec & Davidov, 2010; Gottman, Katz, & Hooven, 1996). Positive parenting also did not moderate associations between RSA measures and externalizing behavior. A previous study found that higher quality scaffolding appeared to buffer the effects of SNS risk on externalizing problems in children with ASD (Baker et al., 2018a). RSA may be more sensitive to parental socialization (Beauchaine et al., 2007; Bell, Shader, Webster-Stratton, Reid, & Beauchaine, 2018), thus it is possible that this type of external co-regulatory support may serve as more of a contributor to the development of RSA than as a moderator of its effects.
Although the current sample is relatively large for investigations involving psychophysiology in ASD, replication would strengthen conclusions. As is the case for many studies of RSA in children with ASD (e.g., Neuhaus et al., 2014; Vaughn Van Hecke et al., 2009) and without ASD (e.g., Liew et al., 2011), we did not control for children’s height, weight, or BMI, which have been linked to RSA baseline (but not reactivity) in some community samples (e.g., El-Sheikh, 2005). However, these variables may be related to RSA measurement primarily at extreme levels (Fraley, Birchem, Senkottaiyan, & Alpert, 2005), and many studies have not found them to be related to RSA measurements (Calkins, Graziano, & Keane, 2007; Gentzler, Rottenberg, Kovacs, George, & Morey, 2012; Scarpa, Haden & Tanaka, 2010). Similarly, we did not measure children’s motor skills, which could have contributed to variation in children’s responses to the challenge task; however, children with significant motor impairments were not included in the study, and it appears unlikely that motor skills were associated with our variables of interest in a manner that would confound the observed interaction findings.
Our sample exhibited significant ethnic diversity, but was not large enough to examine the degree to which the processes under consideration varied by ethnic group. Historically, investigations involving psychophysiology in ASD have excluded children with lower levels of intellectual functioning (see Lydon et al., 2015 for a review). Lower child estimated IQ did not appear to significantly compromise measurement in the current study, which we hope will encourage researchers to be more inclusive in extending psychophysiological measurement to a broader population of individuals with ASD.
Among children with ASD, who are characterized by regulation challenges, higher RSA reactivity was associated with higher levels of externalizing behavior under conditions of high negative parenting, but lower externalizing behavior in the context of lower parental negativity. These results suggest the utility of considering interactions between child psychophysiology and parenting when investigating how the environment can support children with ASD. Findings from the current study combined with previous studies of children with ASD (Baker et al., 2018a) and without ASD (see Beauchaine et al., 2015) suggest the potential for tailoring parenting interventions based upon regulatory profiles. For example, previous work from our lab with a separate sample of children suggested that parent co-regulation may be particularly important for reducing behavior problems in children with low SNS arousal tendencies (Baker et al., 2018a), while reduction in parental criticism might benefit those with high SNS reactivity (Baker et al., 2018b). The present study suggests that children high in RSA reactivity may uniquely benefit from less negative parental attitudes and reductions in harsh discipline. Further clarity will be gained through investigations that consider both SNS and RSA tendencies simultaneously.
Acknowledgements:
This project was funded by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R15HD087877) awarded to the first two authors. We thank Mariann Howland, Meghan Orr, David Huynh, Caitlyn Kelleher, Kerensa Jorgenson, Brandon Lacey, Marison Lee, Arielle Garcia, Alex Gant, Shivani Patel, Karrie Tran, Jasmine Gonzalez, Kyra Da Silva Colaco, Lauren Richardson, and the staff and families of the Autism Emotion and the Family Project. Jacquelyn Moffitt is now at the University of Miami and Alyssa Bailey is now at Auburn University.
Footnotes
Although the use of residual scores to calculate physiological reactivity is common, some researchers have utilized a difference score obtained by subtracting mean RSA in baseline from RSA during the challenge task (or vice-versa; Beauchaine et al., 2019). Each approach has its strengths and weaknesses and one is not clearly superior to the other for the current purpose (Burt & Obradović, 2013). Utilizing difference scores resulted in RSA-R scores that were very highly correlated with those from the residual-derived method used here, r = .95, p < .001.
Although the three-level ordinal scale for warmth was retained for combination with scaffolding (which produced a continuous variable), warmth was treated dichotomously (low/moderate = 0, high = 1) in the individual follow-up regression given the ordinal nature of the variable, the non-normal distribution, and low rate of “low” scores.
Contributor Information
Jason K. Baker, California State University, Fullerton;
Rachel M. Fenning, California State University, Fullerton;
Stephen A. Erath, Auburn University;
Brian R. Baucom, University of Utah;
Daniel S. Messinger, University of Miami;
Jacquelyn Moffitt, California State University, Fullerton;.
Alexander Kaeppler, Auburn University,.
Alyssa Bailey, California State University, Fullerton;.
References
- Achenbach T (2009). The Achenbach System of Empirically Based Assessment (ASEBA): Development, Findings, Theory, and Applications. Burlington, VT: University of Vermont Research Center for Children, Youth, & Families. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Baker B, Neece C, Fenning R, Crnic K, & Blacher J (2010a). Mental disorders in five-year-old children with or without developmental delay: Focus on ADHD. Journal of Clinical Child and Adolescent Psychology, 39, 492–505. doi: 10.1080/15374416.2010.486321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker JK, Fenning RM, Crnic KA, Baker B, & Blacher J (2007). Prediction of social skills in 6-year-old children with and without developmental delays: Contributions of early regulation and maternal scaffolding. American Journal on Mental Retardation, 112, 375–391. doi: 10.1352/0895-8017(2007)112[0375:POSSIY]2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- Baker JK, Fenning RM, Erath SA, Baucom BR, Moffitt JM, & Howland MA (2018a). Sympathetic under-arousal and externalizing behavior problems in children with autism spectrum disorder. Journal of Abnormal Child Psychology, 46, 895–906. doi: 10.1007/s10802-017-0332-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker JK, Fenning RM, Howland MA, & Huynh D (2018b). Parental criticism and behavior problems in children with autism spectrum disorder. Autism. 10.1177/1362361318804190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bal E, Harden E, Lamb D, Vaughan Van Hecke A, Denver J, & Porges S (2010). Emotion recognition in children with autism spectrum disorders: Relations to eye gaze and autonomic state. Journal of Autism and Developmental Disorders, 40, 358–370. Doi: 10.1007/s10803-009-0884-3 [DOI] [PubMed] [Google Scholar]
- Beauchaine TP (2001). Vagal tone, development, and Gray’s motivational theory: Toward an integrated model of autonomic nervous system functioning in psychopathology. Development and Psychopathology, 13, 183–214. doi: 10.1017/s0954579401002012 [DOI] [PubMed] [Google Scholar]
- Beauchaine TP (2015a). Future directions in emotion dysregulation and youth psychopathology. Journal of Clinical Child & Adolescent Psychology, 44, 875–896. Doi: 10.1080/15374416.2015.1038827 [DOI] [PubMed] [Google Scholar]
- Beauchaine TP (2015b). Respiratory sinus arrhythmia: A transdiagnostic biomarker of emotion dysregulation and psychopathology. Current Opinions in Psychology, 3, 43–73. Doi: 10.1016/j.copsyc2015.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP, Bell Z, Knapton E, McDonough-Caplan H, Shader T, & Zisner A (2019). Respiratory sinus arrhythmia reactivity across empirically based structural dimensions of psychopathology: A meta-analysis. Psychophysiology. 10.1111/psyp.13329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP, Gatzke-Kopp L, & Mead HK (2007). Polyvagal theory and developmental psychopathology: Emotion dysregulation and conduct problems from preschool to adolescence. Biological Psychology, 74, 174–184. doi:10.1016=j.biopsycho.2005.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP, Neuhaus E, Gatzke-Kopp LM, Reid MJ, Chipman J, Brekke A, et al. (2015). Electrodermal responding predicts responses to, and may be altered by, preschool intervention for ADHD. Journal of Consulting and Clinical Psychology, 83, 293–303. doi: 10.1037/a0038405 [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, & Zalewski M (2016). Physiological and developmental mechanisms of emotional lability in coercive relationships In Dishion TJ & Snyder JJ (Eds.), Oxford handbook of coercive relationship dynamics. New York, NY: Oxford University Press. [Google Scholar]
- Bell Z, Shader T, Webster-Stratton C, Reid MJ, Beauchaine TP (2018). Improvements in negative parenting mediate changes in children’s autonomic responding following a preschool intervention for ADHD. Clinical Psychological Science, 6, 134–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belsky J, Bakermans-Kranenburg M, & van IJzendoorn M (2007). For better and for worse: Differential susceptibility to environmental influences. Current Directions in Psychological Science, 16, 300–304. [Google Scholar]
- Benevides T, & Lane S (2015). A review of cardiac autonomic measures: Considerations for examination of physiological response in children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 45, 560–575. Doi: 10.1007/s10803-013-1971-z [DOI] [PubMed] [Google Scholar]
- Benson PR, Daley D, Karlof KL, & Robison D (2011). Assessing expressed emotion in mothers of children with autism: The Autism-Specific Five Minute Speech Sample. Autism, 15, 65–82. doi: 10.1177/1362361309352777 [DOI] [PubMed] [Google Scholar]
- Berntson G, Bigger J, Eckberg D, Grossman P, Kaufmann P Malik M, … van der Molen M (1997). Heart rate variability: Origins, methods, and interpretive caveats. Psychophysiology, 34, 623–648. Doi: 10.1111/j.1469.8986.1997.tb02140.x [DOI] [PubMed] [Google Scholar]
- Boyce W, & Ellis B (2005). Biological sensitivity to context I: An evolutionary-developmental theory of origins and functions of stress reactivity. Development and Psychopathology, 17, 271–301. Doi: 10.1017/S09545794050145 [DOI] [PubMed] [Google Scholar]
- Burt KB, & Obradović J (2013).The construct of psychophysiological reactivity: Statistical And psychometric issues. Developmental Review, 33, 29–57. doi: 10.1037/t05570-000 [DOI] [Google Scholar]
- Calkins S, Graziano P, & Keane S (2007). Cardiac vagal regulation differentiates among children at risk for behavior problems. Biological Psychology, 74, 144–153. doi: 10.1016/j.biopsycho.2006.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caplan B, Feldman M, Eisenhower A, & Blacher J (2016). Student-teacher relationships for young children with autism spectrum disorder: Risk and protective factors. Journal of Autism and Developmental Disorders, 46, 3653–3666. DOI 10.1007/s10803-016-2915-1 [DOI] [PubMed] [Google Scholar]
- Constantino JN & Gruber CP (2012). Social Responsiveness Scale, Second Edition (SRS-2) Manual. Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Costello EJ, Edelbrock CS, & Costello AJ (1985). Validity of the NIMH Diagnostic Interview Schedule for Children: A comparison between psychiatric and pediatric referrals. Journal of Abnormal and Child Psychology, 13, 579–595. doi: 0091-0627/85/1200-0579504.50/0 [DOI] [PubMed] [Google Scholar]
- Daley D, & Benson PR (2008). Manual for coding expressed emotion in parents of children with autism spectrum disorders: The autism-specific five minute speech sample. Boston: Center for Social Development and Education, University of Massachusetts Boston. [Google Scholar]
- Dyer W, Blocker D, Day R, & Bean R (2016). Parenting style and adolescent externalizing behaviors: The moderating role of respiratory sinus arrhythmia. Journal of Marriage and Family, 78, 1149–1165. Doi: 10.1111/jomf.12316 [DOI] [Google Scholar]
- El-Sheikh M (2005). Stability of respiratory sinus arrhythmia in children and young adolescents: A longitudinal examination. Developmental Psychobiology, 46, 66–74. Doi: 10.1002/dev.20036 [DOI] [PubMed] [Google Scholar]
- Erath SA, Bub K, & Tu K (2016). Responses to peer stress predict academic outcomes across the transition to middle school. Journal of Early Adolescence, 36, 5–28. Doi: 10.1177/0272431614556350 [DOI] [Google Scholar]
- Erath SA, El-Sheikh M, Hinnant J, & Cummings M (2011). Skin conductance level reactivity moderates the association between harsh parenting and growth in child externalizing behavior. Developmental Psychology, 47, 693–706. doi: 10.1037/a0021909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenning RM, & Baker JK (2012). Mother-child interaction and resilience in children with early developmental risk. Journal of Family Psychology, 26, 411–420. doi: 10.1037/a0028287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenning RM, Baker JK, & Moffitt J (2018). Intrinsic and extrinsic predictors of emotion regulation in children with autism spectrum disorder. Journal of Autism and Developmental Disorders. 10.1007/s10803-018-3647-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraley MA, Birchem JA, Senkottaiyan N, & Alpert MA (2005). Obesity and the electrocardiogram. Obesity reviews, 6, 275–281. 10.1111/j.1467-789X.2005.00199.x [DOI] [PubMed] [Google Scholar]
- Frick PJ (1991). The Alabama Parenting Questionnaire. Unpublished, University of Alabama. [Google Scholar]
- Gentzler A, Rottenberg J, Kovacs M, George C, & Morey J (2012). Atypical development of resting respiratory sinus arrhythmia in children at high risk for depression. Developmental Psychology, 54, 556–567. doi: 10.1002/dev.20614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottman JM, Katz LF, & Hooven C (1996). Parental meta-emotion philosophy and the emotional life of families: Theoretical models and preliminary data. Journal of Family Psychology, 10, 243–268. Doi: 10.1037/0893-3200.10.3.243 [DOI] [Google Scholar]
- Graziano P, & Derefinko K (2013). Cardiac vagal control and children’s adaptive functioning: A meta-analysis. Biological Psychology, 94, 22–37. Doi: / 10.1016/j.biopsycho.2013.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg JS, Seltzer MM, Hong J, & Orsmond G (2006). Bidirectional effects of expressed emotion and behavior problems and symptoms in adolescents and adults with autism. American Journal on Mental Retardation, 111, 229–249. doi: 10.1352/0895-8017(2006)111[229:BEOEEA]2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- Grusec J, & Davidov M (2010). Integrating different perspectives on socialization theory and research: A domain-specific approach. Child Development, 81, 687–709. Doi: 10.111/j.1467-8624.2010.0146.x [DOI] [PubMed] [Google Scholar]
- Guy L, Souders M, Bradstreet L, DeLussey C, & Herrington J (2014). Emotion regulation and respiratory sinus arrhythmia in autism spectrum disorder. Journal of Autism and Developmental Disorders, 44, 2614–2620. Doi: 10.1007/s10803-014-2124-8 [DOI] [PubMed] [Google Scholar]
- Heim C, & Nemeroff CB (1999). The impact of early adverse experiences on brain systems involved in the pathophysiology of anxiety and affective disorders. Biological Psychiatry, 46, 1509–1522. [DOI] [PubMed] [Google Scholar]
- Hinnant J, & El-Sheikh M (2009). Children’s externalizing and internalizing symptoms over time: The role of individual differences in patterns of RSA responding. Journal of Abnormal Child Psychology, 37, 1049–1061. Doi: 10.1007/sl0802-009-0341-1 [DOI] [PubMed] [Google Scholar]
- Hoffman C, Crnic K & Baker JK (2006). Maternal depression and parenting: Implications for children’s emergent emotion regulation and behavioral functioning. Parenting: Science and Practice, 6, 271–295. doi: / 10.1207/s15327922par0604_1 [DOI] [Google Scholar]
- Jahromi L, Meek S, & Ober-Reynolds S (2012). Emotion regulation in the context of frustration in children with high functioning autism and their typical peers. Journal of Child Psychology and Psychiatry, 53, 1250–1258. doi: 10.1002/aur.1366 [DOI] [PubMed] [Google Scholar]
- Kaat AJ, & Lecavalier L (2013). Disruptive behavior disorders in children and adolescents with autism spectrum disorders: a review of the prevalence, presentation, and treatment. Research in Autism Spectrum Disorders, 7, 1579–1594. [Google Scholar]
- Kochanska G, Brock RL, Chen KH, Aksan N, & Anderson SW (2015). Paths from mother–child and father–child relationships to externalizing behavior problems in children differing in electrodermal reactivity: A longitudinal study from infancy to age 10. Journal of Abnormal Child Psychology, 43, 721–734. doi 10.1007/s10802-014-9938-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koegel RL, Koegel LK, & Surratt A (1992). Language intervention and disruptive behavior in preschool children with autism. Journal of Autism and Developmental Disorders, 22, 141–153. [DOI] [PubMed] [Google Scholar]
- Lauderdale-Littin S, Howell E, & Blacher J (2013). Educational placement for children with autism spectrum disorders in public and non-public school settings: The impact of social skills and behavior problems. Education and Training in Autism and Developmental Disabilities, 48, 469–478. [Google Scholar]
- Lecavalier L, Leone S, & Wiltz J (2006). The impact of behavior problems on caregiver stress in young people with autism spectrum disorder. Journal of Intellectual Disability Research, 50, 172–183. doi: 10.1111/j.1365-2788.2005.00732.x [DOI] [PubMed] [Google Scholar]
- Liew J, Eisenberg N, Spinrad T, Eggum N, Haugen R, Kupfer A, …, Baham M (2011). Physiological regulation and fearfulness as predictors of young children’s empathy-related reactions. Social Development, 20, 111–134. doi: 10.1111/j.1467-9507.2010.00575.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore P, Risi R, Gotham K, & Bishop S (2012). Autism Diagnostic Observation Schedule, Second Edition (ADOS-2) Manual. Torrance, CA: WPS. [Google Scholar]
- Lydon S, Healy O, Reed P, Mulhern T, Hughes BM, & Goodwin MS (2015). A systematic review of physiological reactivity to stimuli in autism. Developmental Neurorehabilitation, 19, 1–21. doi: 10.3109/17518423.2014.971975 [DOI] [PubMed] [Google Scholar]
- Matthews NL, Pollard E, Ober-Reynolds S, Kirwan J, Malligo A, & Smith C (2015). Revisiting cognitive and adaptive functioning in children and adolescents with autism spectrum disorder. Journal of Autism and Developmental Disabilities, 45, 138–156. doi: 10.1007/s10803-014-2200-0 [DOI] [PubMed] [Google Scholar]
- Mazefsky C, Pelphrey K, & Dahl R (2012). The need for a broader approach to emotion regulation research in autism. Child Development Perspectives, 6, 92–97. doi: 10.1111/j.1750-8606.2011.00229.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazefsky C, & White S (2014). Emotion regulation concepts & practice in autism spectrum disorder. Child and Adolescent Psychiatric Clinics of North America, 23, 15–24. doi: 10.1016/j.chc.2013.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClintock K, Hall S, & Oliver C (2003). Risk markers associated with challenging behaviours in people with intellectual disabilities: A meta analytic study. Journal of Intellectual Disability Research, 47, 405–416. doi: 10.1046/j.1365-2788.2003.00517.x [DOI] [PubMed] [Google Scholar]
- Mohammadzaheri F, Koegel LK, Rezael M, & Bakhshi E (2015). A randomized clinical trial comparison between pivotal response treatment (PRT) and adult-driven applied behavior analysis (ABA) intervention on disruptive behaviors in public school children with autism. Journal of Autism and Developmental Disorders, 45, 2899–2907. doi: 10.1007/s10803-015-2451-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris AS, Silk J, Steinberg L, Myers S, & Robinson LR (2007). The role of family context in the development of emotion regulation. Social Development, 16, 361–388. doi: 10.1111/j.1467-9507.2007.00389.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuhaus E, Bernier R, & Beauchaine TP (2014). Brief report: Social skills, internalizing and externalizing symptoms, and respiratory sinus arrhythmia in autism. Journal of Autism and Developmental Disorders, 44, 730–737. DOI 10.1007/s10803-013-1923-7 [DOI] [PubMed] [Google Scholar]
- Obradović J, Bush N, & Boyce W (2011). The interactive effect of marital conflict and stress reactivity on externalizing and internalizing symptoms: The role of laboratory stressors. Development and Psychopathology, 23, 101–114. Doi: 10.1017/S094579410000672 [DOI] [PubMed] [Google Scholar]
- Pandolfi V, Magyar CI, & Dill CA (2012). An initial psychometric evaluation of the CBCL 6 – 18 in a sample of youth with autism spectrum disorders. Research in Autism Spectrum Disorders, 6, 96–108. doi: 10.1016/j.rasd.2011.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roid GH (2003). Stanford-Binet Intelligence Scales, Fifth Edition Itasca, IL: Riverside. [DOI] [PubMed] [Google Scholar]
- Roisman GI, Newman DA, Fraley RC, Haltigan JD, Groh AM, & Haydon KC(2012). Distinguishing differential susceptibility from diathesis-stress: Recommendations for evaluating interaction effects. Development and Psychopathology, 24, 389–409. doi: 10.1017/S0954579412000065 [DOI] [PubMed] [Google Scholar]
- Rutter M, Bailey A, & Lord C (2003). The social communication questionnaire Manual. Torrance, CA: Western Psychological Services. [Google Scholar]
- Rutter M, LeCouteur A, & Lord C (2003). The autism diagnostic interview-revised (ADI-R). Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Samson AC, Hardan AY, Lee IA, Phillips JM, & Gross JJ (2015). Maladaptive behavior in autism spectrum disorder: The role of emotion experience and emotion regulation. Journal of Autism and Developmental Disorders, 45, 3424–3432. [DOI] [PubMed] [Google Scholar]
- Scarpa A, Haden SC, & Tanaka A (2010). Being hot tempered: Autonomic, emotional and behavioral distinctions between childhood reactive and proactive aggression. Biological Psychology, 84, 488–496. doi: 10.1016/j.biopsycho.2009.11.006 [DOI] [PubMed] [Google Scholar]
- Shader T, Gatzke-Kopp L, Crowell S, Jamila Reid M, Thayer JF, Vasey M, … Beauchaine TP (2018). Quantifying respiratory sinus arrhythmia: Effects of misspecifying breathing frequencies across development. Development and Psychopathology, 30, 351–366. doi: 10.1017/S0954579417000669 [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas C, Dulcan M, & Schwab-Stone M (2000). NIHM Diagnostic Interview Schedule for Children Version IV: Description, differences from previous versions, and reliability of some common diagnoses. JAMA Psychiatry, 39, 28–38. [DOI] [PubMed] [Google Scholar]
- Shawler P, & Sullivan M (2017). Parental stress, discipline strategies, and child behavior problems in families of young children with autism spectrum disorders. Focus on Autism and Other Developmental Disorders, 32, 142–151. Doi: 10.1177/1088357615610114 [DOI] [Google Scholar]
- Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, & Baird G (2008). Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child and Adolescent Psychiatry, 47, 921–929. [DOI] [PubMed] [Google Scholar]
- Vaughan Van Hecke A, Lebow J, Bal E, Lamb D, Harden E, … Porges S (2009). Electroencephalogram and heart rate regulation to familiar and unfamiliar people in children with autism spectrum disorder. Child Development, 80, 1118–113. [DOI] [PubMed] [Google Scholar]
- Woodman AC, Mailick MR, & Greenberg JS (2016). Trajectories of internalizing and externalizing symptoms among adults with autism spectrum disorders. Development and Psychopathology, 28, 565–581. doi: 10.1017/S095457941500108X [DOI] [PMC free article] [PubMed] [Google Scholar]


