To the Editor,
The World Health Organization declared the outbreak of coronavirus disease (COVID)-19 a pandemic on 12 March 2020, with Italy being considered the new “epicentre” of the crisis, which originated in China. As of 15 March 2020, 22,512 cases have been reported in Italy, 2,026 (9%) of which are healthcare workers.1 Unfortunately, rates for intensive care unit admission with the need for tracheal intubation and mechanical ventilation are approximately 5% in patients with COVID-19.2 Given the rapid growth of this outbreak and the need to minimize morbidity in healthcare workers, it is paramount that healthcare professionals be familiar with both the definition of a high-risk exposure and the correct donning and doffing procedures for the protective personal equipment (PPE) needed during the care of these patients.
A high-risk exposure has been defined as “prolonged close contact with COVID-19 patients who are not wearing a face mask while the healthcare practitioner’s nose and mouth are exposed to material potentially infected with the virus”.3 When healthcare providers’ eyes, nose, or mouth are unprotected during the conduct of aerosol-generating medical procedures on patients with COVID-19 (e.g., intubation, extubation, cardiopulmonary resuscitation, bronchoscopy, and nebulizer therapy), there is a high risk of contamination.3 When used correctly, PPE protects from this contamination, but it is imperative that PPE is properly donned and doffed.
We have run a number of donning/doffing PPE training simulations with anesthesiologists in our institution. These simulations have revealed critical aspects of the process that, if done improperly, may lead to breaches in biosafety and potential contamination with the virus, causing COVID-19.
Potential donning biosafety breaches
Mask: An N95 respirator is recommended. Qualitative mask-fit testing should ideally be performed in advance, as correct face mask and size are needed to ensure a proper seal. Facial hair at the face-mask interface promotes seal leakage and may decrease protection.4 We strongly recommend shaving facial hair.
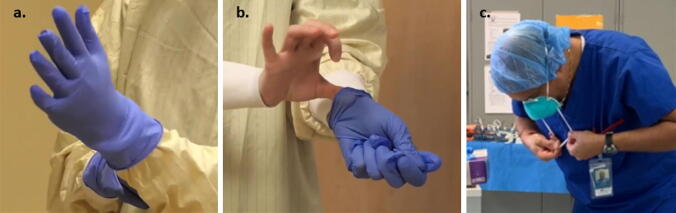
- Gloving: Although not needed to be sterile, always use extended-cuff gloves. Ensuring that the most distal part of the gown’s sleeve is covered snugly by the glove is paramount to preventing hand and forearm contamination (Figure A).
Figure.
Doffing of personal protective equipment. A) The sleeve fits snugly below the extended cuff of the glove. B) Minimal contact possible between the un-gloved hand/ fingers with the sleeve of the gloved hand when removing the second glove. C) Maintaining tension in the inferior strap is useful for preventing snapping of the face mask while removing. Hand hygiene with an alcohol-based hand sanitizer between each of the doffing steps is recommended Time management: PPE should be donned properly; this should be done carefully and never be rushed. This might mean a delay in giving care in code blue/airway management response times.
Potential doffing biosafety breaches
-
4.
Degloving: Gloves are considered the most contaminated part of PPE after performing a high-risk exposure medical procedure. Removal of the first glove is usually easier than the second one. When removing the second glove, ensure that there is as minimal contact as possible between the sleeve of the gloved hand and the un-gloved hand/ fingers (Figure B). Avoid snapping of gloves.
-
5.
Removing gown: The gown is the second most contaminated PPE element. Ensure that bare hands do not touch the front of the gown when removing (e.g., reaching back to untie a reusable gown). A surgical gown that can be pulled off without having to untie it may confer additional safety.
-
6.
Removing mask: Always avoid touching the front of the mask (and/or face shield) with the hands when removing. Maintaining tension on the inferior strap is useful for preventing snapping while removing (Figure C).
-
7.
We recommend hand hygiene with alcohol-based sanitizers be performed for 15–20 sec after each article of PPE is doffed to ensure complete removal of virus contamination from hands.
The correct use of PPE is necessary to decrease the number of infected healthcare workers caring for patients with COVID-19. We hope that highlighting some of these critical aspects of donning/doffing of PPE will lower the probability of encountering biosafety breaches, ultimately translating into a lesser illness-burden among healthcare workers caring for COVID-19 patients.
Acknowledgments
Conflicts of interest
None.
Funding statement
None.
Editorial responsibility
This submission was handled by Dr. Hilary P. Grocott, Editor-in-Chief, Canadian Journal of Anesthesia.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Livingston E, Bucher K. Coronavirus disease 2019 (COVID-19) in Italy. JAMA. 2020 doi: 10.1001/jama.2020.4344. [DOI] [PubMed] [Google Scholar]
- 2.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Interim U.S. Guidance for Risk Assessment and Public Health Management of Healthcare Personnel with Potential Exposure in a Healthcare Setting to Patients with Coronavirus Disease (COVID-19). Available from URL: https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-risk-assesment-hcp.html (accessed March 2020).
- 4.Floyd EL, Henry JB, Johnson DL. Influence of facial hair length, coarseness, and areal density on seal leakage of a tight-fitting half-face respirator. J Occup Environ Hyg. 2018;15:334–340. doi: 10.1080/15459624.2017.1416388. [DOI] [PubMed] [Google Scholar]