Abstract
Vaping, the use of electronic cigarettes, involves different mechanics than conventional combustion cigarettes. Consumers who vape tend to overinhale and then forcefully exhale to eliminate the vapor, which is usually produced in much greater quantity than generated by a regular cigarette. Effectively, they are performing an exaggerated Valsalva maneuver. This can increase their risk for developing potential spontaneous pneumomediastinum. Here we present a case of spontaneous pneumomediastinum secondary to electronic cigarette use.
Keywords: Crepitus, pneumomediastinum, subcutaneous emphysema, vaping
Pneumomediastinum, also known as mediastinal emphysema, is a rare condition in which free air is present within the mediastinum. First described by Laennec in 1819 as a consequence of traumatic injury, the disorder was later reported to also occur spontaneously by Hamman in 1939.1 There are many causes of pneumomediastinum, but the condition is classified into two subtypes, spontaneous/primary or secondary/provoked. Spontaneous pneumomediastinum is due to alveolar rupture caused by an increase in intrathoracic pressure, much like the Valsalva maneuver. Secondary pneumomediastinum is associated with blunt force trauma, penetrating chest trauma, endobronchial/esophageal/chest wall procedures, lung disease, or mechanical ventilation. Pneumomediastinum by itself rarely leads to significant complications and is usually self-limiting; in rare cases, it is a marker for a more serious underlying condition. This report reviews a case of pneumomediastinum from vaping.
CASE DESCRIPTION
A 25-year-old man with no significant past medical history presented to the emergency department with 3 days of unrelenting substernal chest pain and neck stiffness. The pain was nonradiating and described as a heavy pressure, as if something were sitting on his chest. The patient also noticed that his voice sounded nasal or congested, and his neck felt swollen. The symptoms gradually worsened throughout the morning before he decided to come to the hospital. He denied any other constitutional symptoms.
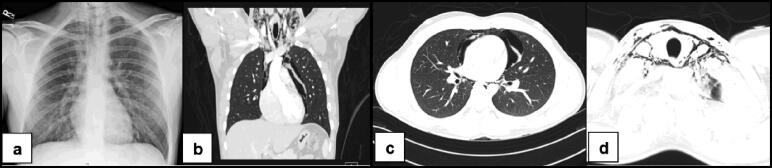
Initial evaluation showed normal vital signs and no leukocytosis. A chest x-ray revealed significant subcutaneous cervical and mediastinal air, which displaced the pericardium peripherally, particularly along the left aspect of the heart (Figure 1a). No pleural effusions or pneumothoraces were identified. A computed tomography scan of the chest revealed marked pneumomediastinum extending superiorly into the neck but without any concerning pleural effusions or fluid collections to suggest esophageal perforation (Figure 1b, c, d).
Figure 1.
Imaging studies showing (a) cervical emphysema and pneumomediastinum without pneumothorax; (b) marked pneumomediastinum extending superiorly; (c) pneumomediastinum surrounding the pericardium; and (d) cervical pneumomediastinum with extensive dissection.
The patient was admitted for observation, withholding food and fluids by mouth. Physical exam showed crepitus along the supraclavicular region, extending to the anterior chest and neck. This slowly improved over the next 2 days. Additional imaging with a soluble contrast esophagram showed no esophageal perforation. Upon further questioning, the patient stated he had begun vaping with NJOY Ace Pods 6 weeks earlier in an attempt to quit smoking. He had smoked approximately 1 pack of cigarettes per week for the past 6 to 7 years without any acute complications. The night before admission, however, at a social gathering he utilized his e-cigarette in much greater frequency than normal. After careful observation for 48 h, the patient was discharged home without operative intervention. Strong recommendations to stop utilizing e-cigarettes were given as well as smoking cessation advice and counseling.
DISCUSSION
The incidence of electronic cigarette use is increasing, especially among minors and teenagers. A new wave of previously unseen complications is being seen as a result of its use, including collapsed lungs2 and pneumomediastinum.1 Individuals who use electronic cigarettes are more likely to significantly increase their intrathoracic volume in an attempt to obtain a large amount of inhaled aerosol from the device to then be able to puff it out in a large cloud. During this active overinhalation, the body’s natural response is to forcefully expire in an attempt to decompress the lungs. If the lungs recoil to decrease the intrathoracic pressure against a closed glottis, this can produce a rapid increase in intrathoracic pressure, causing air to escape out of the alveoli and conducting airways into the mediastinum by way of peribronchial vascular sheaths, causing pneumomediastinum, the so-called Mecklin effect.3
Electronic cigarettes like Juul, NJOY, and others have been advertised as healthier alternatives to tobacco-containing cigarettes, yet these products contain numerous irritants, including toxins such as aldehydes and acetyl pyrazine. Many studies are under way to better understand the deleterious effects and true toxicity of electronic cigarettes. For now, consumers should refrain from using such products as much as possible, and health care providers should be aware of their potentially severe side effects and actively query patients about their use.
References
- 1.Marasco RD, Loizzi D, Ardò NP, Fatone FN, Sollitto F. Spontaneous pneumomediastinum after electronic cigarette use. Annals Thorac Surg. 2018;105(6):e269–e271. [DOI] [PubMed] [Google Scholar]
- 2.Dinerstein C. JUUL blamed for collapsed lung. News [American Council on Science and Health], August 14, 2019. https://www.acsh.org/news/2019/08/14/juul-blamed-collapsed-lung-14222.
- 3.Carolan LP, McColley AS, Sharma DG. Pneumomediastinum: Overview. https://emedicine.medscape.com/article/1003409-overview. Accessed February 26, 2019.