Abstract
Cardiac conduction abnormalities, including left bundle branch block (LBBB), are common following transcatheter aortic valve replacement (TAVR). This study assessed the incidence and outcomes of new or widening persistent LBBB following TAVR. Data regarding 550 consecutive patients undergoing TAVR between 2012 and 2016 at our institution were retrospectively reviewed. Both 30-day and 1-year outcomes of patients with isolated new or worsening LBBB following TAVR were reviewed. Fifty-two patients (9.5%) developed new or worsening LBBB. Six of the 52 (11.5%) patients received a permanent pacemaker (PPM) for LBBB prior to discharge. For patients discharged home following TAVR without a PPM, the 1-year PPM requirement was 15.2% in patients with new or worsening LBBB compared to 4.5% in patients without new or worsening LBBB (P = 0.01). One-year mortality rates for patients who did not have a new PPM placed before discharge were 15.2% in patients with new or worsening LBBB, 13.9% in patients without new or worsening LBBB, and 11.9% in patients with preoperative PPMs (P = 0.81). Patients with new or worsening persistent LBBB discharged without a PPM experience a higher requirement for PPM implantation in the year following TAVR compared to patients without new or worsening persistent LBBB.
Keywords: Left bundle branch block, permanent pacemaker, transcatheter aortic valve replacement
Cardiac conduction abnormalities are one of the most common adverse events following transcatheter aortic valve replacement (TAVR), and the incidence of new left bundle branch block (LBBB) ranges from 5% to 65%.1 LBBB is an issue because anatomically, the left bundle branch is near the site of valve deployment and can be disrupted by the native calcium or by the valve prosthesis.2,3 Newer-generation valves with sealing skirts and higher radial strength may create more conduction anomalies than earlier generation valves.4 Deployment can cause temporary or permanent damage that results in the development of LBBB. Recommendations for patients with new LBBB after TAVR include a 30-day mobile cardiac outpatient telemetry device or an implantable loop recorder, although, at the time this study was completed, there were no commonly regarded strategies.5,6 There was also no definitive consensus on the effect of new LBBB after TAVR on mortality. In this study, we investigated the incidence and clinical outcomes of patients with new or worsening LBBB following TAVR at a single site.
METHODS
Institutional review board approval for a retrospective review of all TAVR patients at our institution between January 2012 and March 2016 was obtained in order to evaluate the incidence and outcomes of patients with new or worsening LBBB following TAVR. Patients with a preoperative permanent pacemaker (PPM) were separated into their own cohort.
Three electrocardiograms were reviewed per patient. The pre-TAVR, immediate postprocedure, and predischarge electrocardiograms were evaluated for the presence of new or worsening LBBB. New LBBB was defined as a QRS interval >120 msec that was present in the postprocedure electrocardiogram and persisted on the predischarge electrocardiogram. Worsening LBBB was defined as an increase of at least 10% from baseline LBBB on postprocedure electrocardiogram that persisted on the predischarge electrocardiogram. Each electrocardiogram was reviewed by two separate physicians following this protocol.
Patient charts, the Society of Thoracic Surgery National Database, the Society of Thoracic Surgery/American College of Cardiology Transcatheter Valve Therapy Registry, and our local TAVR database were reviewed to obtain baseline patient demographics, intraoperative and postoperative characteristics, and 30-day and 1-year outcomes. Continuous variables are presented as mean ± standard deviation and categorical variables are presented as percentages. Standard clinical indications for PPM insertion were applied to all patients following TAVR.7,8
Data were compared between three groups: patients who had preoperative PPMs, patients who developed new or worsening LBBB, and patients who did not develop new or worsening LBBB following TAVR. Chi-square analyses were performed between the groups.
RESULTS
A total of 550 patients underwent TAVR during the 4-year study period. Of these, 126 (22.9%) had preoperative PPMs. The baseline and intraoperative characteristics were similar between the three cohorts (Tables 1 and 2). Following TAVR, 52 (12.3%) patients without preoperative PPM were diagnosed with new or worsening persistent LBBB. Of these patients, in six (11.5%), the likelihood of progression was deemed so high on initial evaluation by the electrophysiologist due to associated AV block or progressive QRS widening that discharge without a PPM was considered dangerous. The remaining 372 patients did not develop new or worsening LBBB, and 84 (22.6%) met clinical indications for PPM. In-hospital mortality was similar between the three groups at 0% for preoperative PPM, 2.4% for patients without new or worsening LBBB, and 1.9% for patients with new or worsening LBBB (P = 0.21).
Table 1.
Baseline characteristics for patients undergoing transcatheter aortic valve replacement
| Variable |
Preop PPM (n = 126) |
New or worsening LBBB |
P value | |
|---|---|---|---|---|
| No (n = 372) | Yes (n = 52) | |||
| Age (years) | 83 ± 7.0 | 81 ± 8.6 | 82 ± 7.3 | 0.12 |
| STS score (%) | 8 ± 4.1 | 7.2 ± 3.7 | 7.56 ± 4.12 | 0.06 |
| Men | 73 (57.9%) | 196 (52.7%) | 22 (42.3%) | 0.16 |
| Frail | 49 (38.9%) | 110 (29.5%) | 16 (30.8%) | 0.15 |
| White | 116 (92.1%) | 339 (91.1%) | 48 (92.3%) | 0.92 |
| Diabetes mellitus | 59 (46.8%) | 166 (44.6%) | 26 (50.0%) | 0.73 |
| Dyslipidemia | 113 (89.7%) | 340 (91.4%) | 25 (48.1%) | <0.001 |
| Hypertension | 119 (94.4%) | 348 (93.5%) | 51 (98.1%) | 0.42 |
| Dialysis | 2 (1.6%) | 4 (1.1%) | 1 (1.9%) | 0.82 |
| Smoker | 38 (30.2%) | 136 (36.6%) | 14 (26.9%) | 0.22 |
| Lung disease: moderate/severe | 36 (28.6%) | 82 (22.0%) | 13 (25.0%) | 0.32 |
| Liver disease | 5 (4.0%) | 34 (9.1%) | 1 (1.9%) | 0.05 |
| Mediastinal radiation | 6 (4.8%) | 14 (3.8%) | 0 | 0.29 |
| Peripheral vascular disease | 55 (43.7%) | 162 (43.5%) | 20 (38.5%) | 0.78 |
| Cerebrovascular disease | 48 (38.1%) | 130 (34.9%) | 17 (32.7%) | 0.74 |
| Prior procedures | ||||
| PCI | 62 (49.2%) | 173 (46.5%) | 23 (44.2%) | 0.8 |
| Coronary bypass | 54 (42.9%) | 104 (28.0%) | 18 (34.6%) | 0.008 |
| Surgical AVR | 6 (4.8%) | 14 (3.8%) | 0 | 0.30 |
| TAVR | 0 | 2 (0.5%) | 0 | 0.62 |
| Balloon aortic valvuloplasty | 22 (17.5%) | 44 (11.8%) | 14 (26.9%) | 0.009 |
| Previous MI | 32 (25.4%) | 92 (24.7%) | 6 (11.5%) | 0.10 |
| NYHA class III/IV | 101 (80.2%) | 305 (82.0%) | 43 (83.0%) | 0.88 |
| Body mass index (kg/m2) | 27.0 ± 5.4 | 27.5 ± 6.6 | 28.59 ± 6.01 | 0.30 |
| Ejection fraction (%) | 52.7 ± 12.7 | 54.3 ± 13.1 | 56.78 ± 9.18 | 0.13 |
| Creatinine (µmol/L) | 1.5 ± 1.1 | 1.3 ± 0.7 | 1.51 ± 1.38 | 0.15 |
AVR indicates aortic valve replacement; LBBB, left bundle branch block; MI, myocardial infarction; NYHA, New York Heart Association; PCI, percutaneous coronary intervention; PPM, permanent pacemaker; STS, Society of Thoracic Surgeons; TAVR, transcatheter aortic valve replacement.
Table 2.
Perioperative characteristics for patients undergoing transcatheter aortic valve replacement
| Variable |
Preop PPM (n = 126) |
New or worsening LBBB |
P value | |
|---|---|---|---|---|
| No (n = 372) | Yes (n = 52) | |||
| Elective procedure | 121 (96.0%) | 366 (98.4%) | 51 (98.1%) | 0.29 |
| Procedure indication | ||||
| Aortic stenosis | 119 (94.4%) | 354 (95.2%) | 51 (98.1%) | 0.57 |
| Valve-in-valve | 6 (4.8%) | 16 (4.3%) | 0 (0.0%) | 0.30 |
| Aortic insufficiency | 1 (0.8%) | 2 (0.5%) | 1 (1.9%) | 0.54 |
| Cardiopulmonary bypass | 2 (1.6%) | 8 (2.2%) | 1 (1.9%) | 0.93 |
| General anesthesia | 121 (96.0%) | 333 (89.5%) | 46 (88.5%) | 0.07 |
| Inotropes (preop) | 2 (1.6%) | 2 (0.5%) | 1 (1.9%) | 0.40 |
| Access | ||||
| Transfemoral | 106 (84.1%) | 310 (83.3%) | 49 (94.2%) | 0.12 |
| Transapical | 18 (14.3%) | 51 (13.7%) | 1 (1.9%) | 0.05 |
| Transaortic | 2 (1.6%) | 11 (3.0%) | 2 (3.9%) | 0.63 |
| Valve type | ||||
| Sapien | 24 (19.0%) | 68 (18.3%) | 4 (7.7%) | 0.15 |
| Sapien XT | 49 (38.9%) | 123 (33.1%) | 10 (19.2%) | 0.04 |
| Sapien 3 | 35 (27.8%) | 132 (35.5%) | 33 (63.5%) | <0.001 |
| CoreValve | 17 (13.5%) | 33 (8.9%) | 4 (7.7%) | 0.28 |
| Evolut | 1 (0.8%) | 16 (4.3%) | 1 (1.9%) | 0.14 |
| PPM predischarge | N/A | 84 (22.6%) | 6 (11.5%) | 0.10 |
| Hospital mortality | 0 (0.0%) | 9 (2.4%) | 1 (1.9%) | 0.21 |
| Length of stay (days) | 4.4 ± 5.4 | 4.6 ± 5.5 | 4 ± 3.0 | 0.79 |
| Vascular complications | 19 (15.1%) | 57 (15.3%) | 11 (21.2%) | 0.54 |
| Reoperation | 3 (2.4%) | 13 (3.5%) | 0 (0.0%) | 0.34 |
| Cardiac arrest | 3 (2.4%) | 11 (3.0%) | 0 (0.0%) | 0.44 |
| Atrial fibrillation | 14 (11.1%) | 66 (17.7%) | 7 (13.5%) | 0.19 |
LBBB indicates left bundle branch block; PPM, permanent pacemaker.
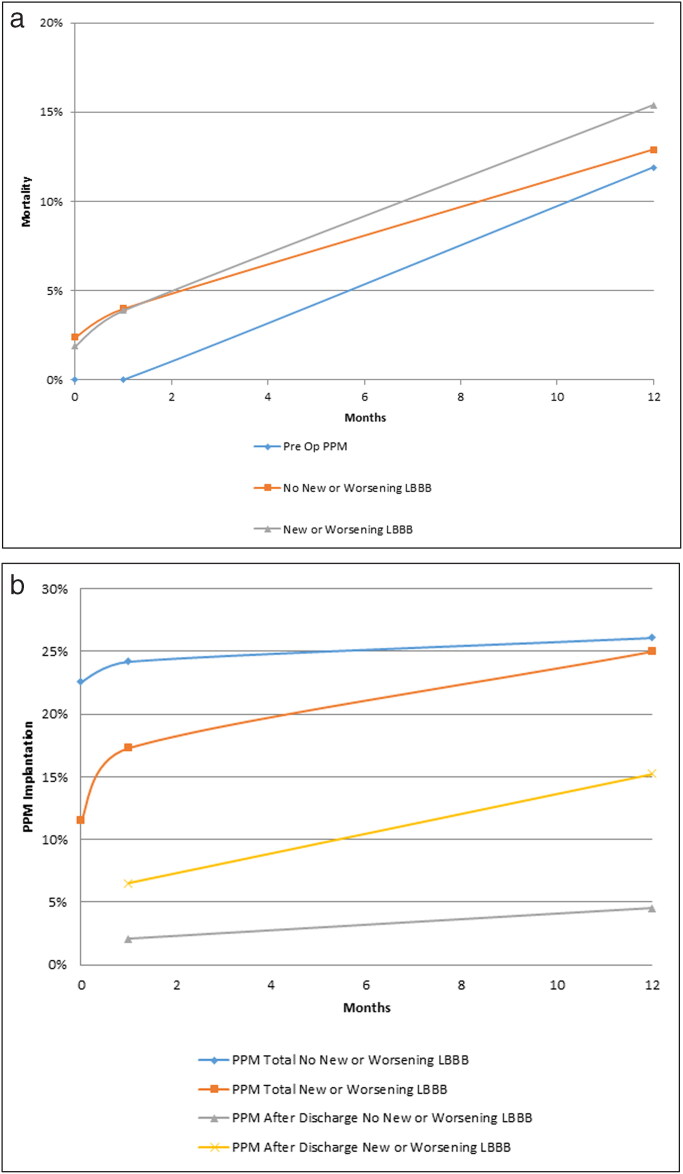
At 30 days, the PPM rate following TAVR was 24.2% in patients without new or worsening LBBB and 17.3% in patients with new or worsening LBBB (P = 0.36). Following hospital discharge, the rate of PPM placement was 2.1% in patients without new or worsening LBBB and 6.5% in patients with new or worsening LBBB (P = 0.21; Figure 1a). Of postdischarge PPM placements in patients with new or worsening LBBB, 4% were emergent. The 30-day mortality was 0% for the patients with prior PPMs, 4.0% in patients with no new or worsening LBBB, and 3.9% in patients with new or worsening LBBB (P = 0.07). The postdischarge 30-day mortality was 0% in patients with prior PPMs, 1.7% in patients with no new or worsening LBBB, and 2.0% in patients with new or worsening LBBB (P = 0.67). In patients discharged home without a new PPM, 30-day mortality was 0% in patients with preoperative PPM, 2.1% in patients with no new or worsening LBBB, and 2.2% in patients with new or worsening LBBB (P = 0.25). In patients with new or worsening LBBB, the 30-day readmission rate was 19.2%, compared to 10.3% in patients with prior PPMs and 10.2% in patients with no new or worsening LBBB (P = 0.15). The new or worsening LBBB had resolved in 13.5% of patients at 30-day follow-up (Table 3).
Figure 1.
Outcomes after transcatheter aortic valve replacement. (a) Permanent pacemaker implantation, total and after discharge, based on experience of new or worsening left bundle branch block. (b) Mortality rates for patients with preoperative pacemaker, no preoperative pacemaker without new or worsening left bundle branch block, and no preoperative pacemaker with left bundle branch block.
Table 3.
Outcomes at 30 days and 1 year after transcatheter aortic valve replacement
| Variable |
Preop PPM (n = 126) |
New or worsening LBBB |
P value | |
|---|---|---|---|---|
| No (n = 372) | Yes (n = 52) | |||
| 30 days | ||||
| PPM total | N/A | 90 (24.2%) | 9 (17.3%) | 0.36 |
| PPM discharge to 30 days | N/A | 6/288 (2.1%) | 3/46 (6.5%) | 0.21 |
| LBBB resolved | N/A | N/A | 7 (13.5%) | N/A |
| Mortality | 0 (0.0%) | 15 (4.0%) | 2 (3.9%) | 0.07 |
| Mortality discharge to 30 days | 0 (0.0%) | 6/363 (1.7%) | 1/51 (2.0%) | 0.67 |
| Mortality discharged without PPM to 30 days | 0 (0.0%) | 6/281 (2.1%) | 1/46 (2.2%) | 0.25 |
| Readmission | 13 (10.3%) | 38 (10.2%) | 10 (19.2%) | 0.15 |
| Stroke/transient ischemic attack | 1 (0.8%) | 8 (2.2%) | 0 (0.0%) | 0.36 |
| 1 year | ||||
| PPM total | N/A | 97 (26.1%) | 13 (25.0%) | 1 |
| PPM discharge to 1 year | N/A | 13/288 (4.5%) | 7/46 (15.2%) | 0.01 |
| LBBB resolved | N/A | N/A | 13 (25.0%) | N/A |
| Mortality | 15 (11.9%) | 48 (12.9%) | 8 (15.4%) | 0.82 |
| Mortality discharge to 1 year | 15/126 (11.9%) | 39/363 (10.7%) | 7/51 (13.7%) | 0.79 |
| Mortality discharged without PPM to 1 year | 15/126 (11.9%) | 39/281 (13.9%) | 7/46 (15.2%) | 0.81 |
LBBB indicates left bundle branch block; PPM, permanent pacemaker.
For those patients who were discharged home without a PPM, at 1 year, PPMs were required in 15.2% of patients with new or worsening LBBB compared to 4.5% in patients without new or worsening LBBB due to associated AV block or progressive QRS widening (P = 0.01). Of the postdischarge PPM placements in patients with new or worsening LBBB, 12% were emergent. The 1-year mortality was 11.9% for the patients with prior PPMs, 12.9% in patients with no new or worsening LBBB, and 15.4% in patients with new or worsening LBBB (P = 0.82; Figure 1b). The postdischarge 1-year mortality was 11.9% in patients with prior PPMs, 10.7% in patients with no new or worsening LBBB, and 13.7% in patients with new or worsening LBBB (P = 0.79). In patients discharged home without a new PPM, 1-year mortality was 11.9% in patients with a preoperative PPM, 13.9% in patients with no new or worsening LBBB, and 15.2% in patients with new or worsening LBBB (P = 0.81; Table 3). The 1-year mortality rate among patients with new or worsening LBBB was 4% in those with a PPM and 11% in those without a PPM (P = 0.18). The causes of death were multifactorial in those patients with new or worsening LBBB at 1 year, and the contribution of arrhythmia to the cause of death was difficult to determine. Final causes of death included sepsis in two patients, pulseless electrical activity arrest following an emergency room visit for arrhythmias in one patient, cardiogenic shock in one patient, congestive heart failure in one patient, Alzheimer’s disease in one patient, complications following an amputation in one patient, and complications of mesenteric ischemia at the time of TAVR in one patient. The new or worsening LBBB had resolved in 25% of patients at 1-year follow-up.
DISCUSSION
The present study demonstrated that new or worsening persistent LBBB was common following TAVR at 9.5% of the total cohort, or 12.3% of those without a pre-TAVR PPM, and resolved in one-quarter of patients at 1-year follow-up. Most importantly, among patients who were discharged without a PPM, those with new or worsening persistent LBBB required PPM implantation more frequently than those without LBBB (15.2% vs 4.5%, P = 0.01), often receiving the PPM weeks to months after the TAVR procedure. At 1 year, overall mortality in patients with and without persistent LBBB was comparable (13.7% vs 10.7%, P = NS).
Conduction issues are the most common complication from TAVR. Published rates of LBBB following TAVR vary widely in the literature from 5% to 65%.1,6,9 Such wide variation is likely due to the fact that LBBB is very common in the moments immediately after valve deployment and can be transient, disappearing within minutes to hours and leading to reporting discrepancies. Persistence of LBBB to hospital discharge or, from a long-term perspective, persistence of LBBB out to 1 year cannot be predicted for an individual patient. In general, half of the cases of postimplant LBBB resolve prior to hospital discharge, and half of the cases of persistent LBBB at discharge resolve in 1-year follow-up, a figure that was modestly higher than what we found.10–14 Regardless of persistence, the mechanism of TAVR-related LBBB has been postulated to be compression on the interventricular membranous septum and the contiguous atrioventricular node and left bundle, causing inflammation, edema, ischemia, and scarring.15–17
Predictors of the need for PPM after TAVR are generally anatomical/mechanical and parallel the pathophysiology of TAVR-related LBBB. Factors that predispose patients to TAVR-related PPM include right bundle branch block or left anterior fascicular block at baseline, smaller left ventricular outflow tract diameter, valve oversizing, a higher ratio of annulus diameter to left ventricular outflow tract diameter, depth of the prosthesis in the left ventricular outflow tract, severe mitral annular calcification, and calcification of either the left ventricular outflow tract or left or right coronary cusp.5,13,18–22 Although both LBBB and the need for PPM have been reported at higher rates with self-expanding valves compared to balloon-expandable valves,11,18,23 the gap in post-TAVR PPM is narrowing with the newest generation of commercially available balloon-expandable and self-expanding valves.22
In our study, new onset of persistent LBBB or worsening of LBBB was not associated with mortality at 1 year, with event rates too low to draw statistical conclusions. It is not entirely clear whether TAVR-related LBBB is associated with late mortality. No prospective trials exist that look specifically at TAVR-related LBBB and mortality. Several retrospective trials reported no effect on long-term mortality for new-onset LBBB after TAVR,5,9,19,20,24 while others suggested that LBBB after TAVR is a marker for late mortality.11,23,25,26 A meta-analysis of eight studies showed that TAVR-related LBBB was a marker of cardiac death at 1 year (relative risk 1.39, 95% confidence interval 1.04–1.86), but did not meet clinical significance for all-cause mortality (relative risk 1.21, 95% confidence interval 0.98–1.50).27
The management of LBBB after TAVR is currently not defined by international societies, resulting in individual centers developing their own management strategies. In our study, the subset of patients with new or worsening LBBB who did not require PPM prior to discharge had a significantly increased requirement for PPM at 1 year. Furthermore, over half of these patients received their pacemaker implant more than 30 days following the TAVR procedure, suggesting progressive dysfunction of the atrioventricular node induced by the TAVR valve. In various retrospective trials, approximately 80% of patients with new-onset LBBB following TAVR, who ultimately required PPM, had advanced atrioventricular block as the indication, with one large study reporting 5 months as the median time for PPM implantation after TAVR.27,28 Presently, most TAVR centers are either doing no postdischarge monitoring or 30-day mobile continuous outpatient telemetry for new TAVR-related LBBB. Due to the delay in the progression of atrioventricular block after TAVR, that strategy may miss a substantial subset of individuals who could benefit from PPM implantation.
It is too premature to determine if longer-term monitoring would have a favorable impact on hospitalization, syncope, or death. The recently published Ambulatory Electrocardiographic Monitoring for the Detection of High-Degree AtrioVentricular Block in Patients With New-Onset Persistent Left Bundle Branch Block After Transcatheter Aortic Valve Implantation study monitored 103 patients after TAVR using implantable ambulatory electrocardiographic monitoring for 12 months.29 Significant conduction abnormalities were reported in approximately 20% of patients, with nearly half of those requiring a permanent implantable rhythm altering device for correction. Using the results of this study along with combined expertise, an expert consensus scientific panel recently proposed a management algorithm for new-onset LBBB after TAVR in which a temporary pacemaker is suggested for 24 h. Then recommendations for PPM or the need for further evaluation/observation (including additional temporary pacing, continuous electrocardiographic monitoring, or invasive electrophysiological studies to aid decision for PPM) are made based on specific changes in electrocardiograms.30 Further studies are now being suggested to define key factors that may predispose patients for significant conduction abnormalities requiring treatment-altering care.
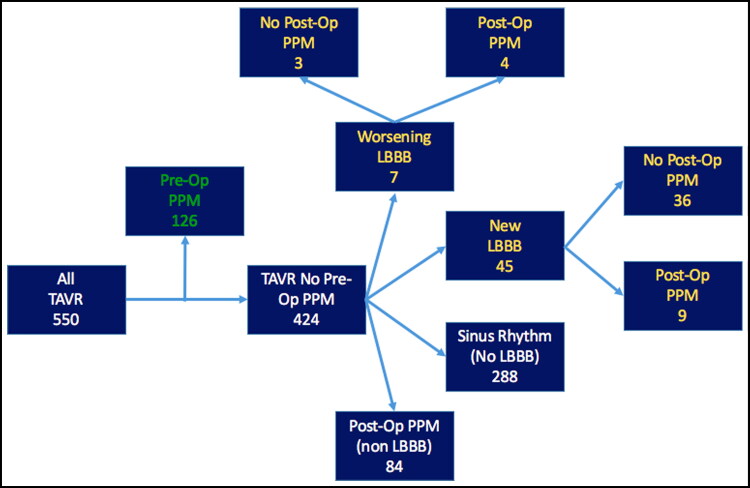
One weakness of this study is its retrospective design. We accounted for reporting bias by having all electrocardiograms blinded and reviewed by two independent cardiologists. Additionally, our study is also limited by the potential for patients to receive urgent PPMs at outside medical facilities. Given that we have 100% 1-year follow-up of all TAVRs completed at our institution, we can accurately report complications and mortality in our patient population (Figure 2). It is also important to note that 87% of patients received balloon-expandable valves, and late outcomes for self-expanding valves could be different. Outcomes could also be subject to implantation technique; while it is clear that deep or low implantations should be avoided, varying techniques between centers or individual operators may influence the risk of LBBB or late high-degree atrioventricular block.
Figure 2.
CONSORT diagram of patient population with PPM outcomes to 1 year.
In conclusion, PPM implantation in patients with new or worsening LBBB who are discharged home after TAVR without a PPM is common. The increased need for PPM often presents >30 days after TAVR, which is an argument for the need to implement new policies for long-term monitoring in these patients. Prospective, randomized controlled trials are needed to determine optimal treatment of patients who develop persistent or worsening LBBB following TAVR.
References
- 1.Massoullié G, Bordachar P, Ellenbogen KA, et al. New-onset left bundle branch block induced by transcutaneous aortic valve implantation. Am J Cardiol. 2016;117(5):867–873. doi: 10.1016/j.amjcard.2015.12.009. [DOI] [PubMed] [Google Scholar]
- 2.Kawashima T, Sato F. Visualizing anatomical evidences on atrioventricular conduction system for TAVI. Int J Cardiol. 2014;174(1):1–6. doi: 10.1016/j.ijcard.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 3.Steinberg BA, Harrison JK, Frazier-Mills C, Hughes GC, Piccini JP. Cardiac conduction system disease after transcatheter aortic valve replacement. Am Heart J. 2012;164(5):664–671. doi: 10.1016/j.ahj.2012.07.028. [DOI] [PubMed] [Google Scholar]
- 4.De Torres-Alba F, Kaleschke G, Diller GP, et al. Changes in the pacemaker rate after transition from Edwards SAPIEN XT to SAPIEN 3 transcatheter aortic valve implantation: the critical role of valve implantation height. JACC Cardiovasc Interv. 2016;9(8):805–813. doi: 10.1016/j.jcin.2015.12.023. [DOI] [PubMed] [Google Scholar]
- 5.Testa L, Latib A, De Marco F, et al. Clinical impact of persistent left bundle-branch block after transcatheter aortic valve implantation with CoreValve Revalving System. Circulation. 2013;127(12):1300–1307. doi: 10.1161/CIRCULATIONAHA.112.001099. [DOI] [PubMed] [Google Scholar]
- 6.Egger F, Nürnberg M, Rohla M, et al. High-degree atrioventricular block in patients with preexisting bundle branch block or bundle branch block occurring during transcatheter aortic valve implantation. Heart Rhythm. 2014;11(12):2176–2182. doi: 10.1016/j.hrthm.2014.07.014. [DOI] [PubMed] [Google Scholar]
- 7.Epstein AE, Dimarco JP, Ellenbogen KA, et al. American College of Cardiology; American Heart Association Task Force on Practice Guidelines; American Association for Thoracic Surgery; Society of Thoracic Surgeons. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities. Heart Rhythm. 2008;5(6):e1–e62. doi: 10.1016/j.hrthm.2008.04.014. [DOI] [Google Scholar]
- 8.Epstein AE, DiMarco JP, Ellenbogen KA, et al. Heart Rhythm Society. 2012 ACCF/AHA/HRS focused update incorporated into the ACCF/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2013;61(3):e6–e75. doi: 10.1016/j.jacc.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 9.Franzoni I, Latib A, Maisano F, et al. Comparison of incidence and predictors of left bundle branch block after transcatheter aortic valve implantation using the CoreValve versus the Edwards valve. Am J Cardiol. 2013;112(4):554–559. doi: 10.1016/j.amjcard.2013.04.026. [DOI] [PubMed] [Google Scholar]
- 10.Boerlage-Van Dijk K, Kooiman KM, Yong ZY, et al. Predictors and permanency of cardiac conduction disorders and necessity of pacing after transcatheter aortic valve implantation. Pacing Clin Electrophysiol. 2014;37(11):1520–1529. doi: 10.1111/pace.12460. [DOI] [PubMed] [Google Scholar]
- 11.Houthuizen P, van der Boon RM, Urena M, et al. Occurrence, fate and consequences of ventricular conduction abnormalities after transcatheter aortic valve implantation. EuroIntervention. 2014;9(10):1142–1150. doi: 10.4244/EIJV9I10A194. [DOI] [PubMed] [Google Scholar]
- 12.Roten L, Wenaweser P, Delacrétaz E, et al. Incidence and predictors of atrioventricular conduction impairment after transcatheter aortic valve implantation. Am J Cardiol. 2010;106(10):1473–1480. doi: 10.1016/j.amjcard.2010.07.012. [DOI] [PubMed] [Google Scholar]
- 13.van der Boon RM, Van Mieghem NM, Theuns DA, et al. Pacemaker dependency after transcatheter aortic valve implantation with the self-expanding Medtronic CoreValve System. Int J Cardiol. 2013;168(2):1269–1273. doi: 10.1016/j.ijcard.2012.11.115. [DOI] [PubMed] [Google Scholar]
- 14.Piazza N, Onuma Y, Jesserun E, et al. Early and persistent intraventricular conduction abnormalities and requirements for pacemaking after percutaneous replacement of the aortic valve. JACC Cardiovasc Interv. 2008;1(3):310–316. doi: 10.1016/j.jcin.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 15.Erkapic D, De Rosa S, Kelava A, Lehmann R, Fichtlscherer S, Hohnloser SH. Risk for permanent pacemaker after transcatheter aortic valve implantation: a comprehensive analysis of the literature. J Cardiovasc Electrophysiol. 2012;23(4):391–397. doi: 10.1111/j.1540-8167.2011.02211.x. [DOI] [PubMed] [Google Scholar]
- 16.Piazza N, Nuis RJ, Tzikas A, et al. Persistent conduction abnormalities and requirements for pacemaking six months after transcatheter aortic valve implantation. EuroIntervention. 2010;6(4):475–484. doi: 10.4244/EIJ30V6I4A80. [DOI] [PubMed] [Google Scholar]
- 17.Moreno R, Dobarro D, López de Sá E, et al. Cause of complete atrioventricular block after percutaneous aortic valve implantation: insights from a necropsy study. Circulation. 2009;120(5):e29–e30. doi: 10.1161/CIRCULATIONAHA.109.849281. [DOI] [PubMed] [Google Scholar]
- 18.van der Boon RM, Houthuizen P, Urena M, et al. Trends in the occurrence of new conduction abnormalities after transcatheter aortic valve implantation. Catheter Cardiovasc Intervent. 2015;85(5):E144–E152. doi: 10.1002/ccd.25765. [DOI] [PubMed] [Google Scholar]
- 19.Urena M, Mok M, Serra V, et al. Predictive factors and long-term clinical consequences of persistent left bundle branch block following transcatheter aortic valve implantation with a balloon-expandable valve. J Am Coll Cardiol. 2012;60(18):1743–1752. doi: 10.1016/j.jacc.2012.07.035. [DOI] [PubMed] [Google Scholar]
- 20.Nazif TM, Dizon JM, Hahn RT, et al; PARTNER Publications Office.. Predictors and clinical outcomes of permanent pacemaker implantation after transcatheter aortic valve replacement: the PARTNER (Placement of AoRtic TraNscathetER Valves) trial and registry. JACC Cardiovasc Interv. 2015;8(1):60–69. doi: 10.1016/j.jcin.2014.07.022. [DOI] [PubMed] [Google Scholar]
- 21.Abramowitz Y, Kazuno Y, Chakravarty T, et al. Concomitant mitral annular calcification and severe aortic stenosis: prevalence, characteristics and outcome following transcatheter aortic valve replacement. Eur Heart J. 2017;38(16):1194–1203. doi: 10.1093/eurheartj/ehw594. [DOI] [PubMed] [Google Scholar]
- 22.Mauri V, Reimann A, Stern D, et al. Predictors of permanent pacemaker implantation after transcatheter aortic valve replacement with the SAPIEN 3. JACC Cardiovasc Interv. 2016;9(21):2200–2209. doi: 10.1016/j.jcin.2016.08.034. [DOI] [PubMed] [Google Scholar]
- 23.Schymik G, Tzamalis P, Bramlage P, et al. Clinical impact of a new left bundle branch block following TAVI implantation: 1-year results of the TAVIK cohort. Clin Res Cardiol. 2015;104(4):351–362. doi: 10.1007/s00392-014-0791-2. [DOI] [PubMed] [Google Scholar]
- 24.Carrabba N, Valenti R, Migliorini A, et al. Impact on left ventricular function and remodeling and on 1-year outcome in patients with left bundle branch block after transcatheter aortic valve implantation. Am J Cardiol. 2015;116(1):125–131. doi: 10.1016/j.amjcard.2015.03.054. [DOI] [PubMed] [Google Scholar]
- 25.Urena M, Webb JG, Eltchaninoff H, et al. Late cardiac death in patients undergoing transcatheter aortic valve replacement: incidence and predictors of advanced heart failure and sudden cardiac death. J Am Coll Cardiol. 2015;65(5):437–448. doi: 10.1016/j.jacc.2014.11.027. [DOI] [PubMed] [Google Scholar]
- 26.Houthuizen P, Van Garsse LA, Poels TT, et al. Left bundle-branch block induced by transcatheter aortic valve implantation increases risk of death. Circulation. 2012;126(6):720–728. doi: 10.1161/CIRCULATIONAHA.112.101055. [DOI] [PubMed] [Google Scholar]
- 27.Regueiro A, Abdul-Jawad Altisent O, Del Trigo M, et al. Impact of new-onset left bundle branch block and periprocedural permanent pacemaker implantation on clinical outcomes in patients undergoing transcatheter aortic valve replacement: a systematic review and meta-analysis. Circ Cardiovasc Interv. 2016;9(5):e003635. doi: 10.1161/CIRCINTERVENTIONS.115.003635. [DOI] [PubMed] [Google Scholar]
- 28.Urena M, Webb JG, Cheema A, et al. Impact of new-onset persistent left bundle branch block on late clinical outcomes in patients undergoing transcatheter aortic valve implantation with a balloon-expandable valve. JACC Cardiovasc Interv. 2014;7(2):128–136. doi: 10.1016/j.jcin.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 29.Rodés-Cabau J, Urena M, Nombela-Franco L, et al. Ambulatory electrocardiographic monitoring for the detection of high degree atrio-ventricular block in patients with new-onset persistent left bundle branch block after transcatheter aortic valve implantation. The “MARE” study. JACC Cardiovasc Interv. 2018;11(15):1495–1505. doi: 10.1016/j.jcin.2018.04.016. [DOI] [PubMed] [Google Scholar]
- 30.Rodés-Cabau J, Ellenbogen KA, Krahn AD, et al. Management of conduction disturbances associated with transcatheter aortic valve replacement: JACC Scientific Expert Panel. J Am Coll Cardiol. 2019;74(8):1086–1106. doi: 10.1016/j.jacc.2019.07.014. [DOI] [PubMed] [Google Scholar]