Abstract
The health of people ever incarcerated in New York City (NYC) jails during 2001 to 2005 was characterized by matching jail, shelter, mortality, sexually transmitted infection, HIV, and tuberculosis (TB) data from the NYC Departments of Health and Mental Hygiene, Correction, and Homeless Services. Compared with nonincarcerated people and those living in the lowest income NYC neighborhoods, those ever incarcerated had higher HIV prevalence and HIV case rates. Ever-incarcerated females also had higher rates of gonorrhea and syphilis than nonincarcerated females. Ever-incarcerated people who used the single adult homeless shelter system had higher HIV, gonorrhea, and TB case rates and all-cause mortality rates than ever-incarcerated people without shelter use, when adjusting for other variables. People ever incarcerated in NYC jails are at risk for conditions of public health importance. Sex-specific jail- and community-based interventions are needed.
Keywords: jail, sexually transmitted infection, tuberculosis, HIV, mortality, homeless people
Introduction
In the United States, ever-incarcerated people have higher rates of HIV, sexually transmitted infections (STIs), tuberculosis (TB), and all-cause mortality compared with the general population (Baillargeon & Bradshaw, 2003; Binswanger et al., 2007; Hammett, Harmon, & Rhodes, 2002; Massoglia, 2008; Mertz, Voigt, Hutchins, Levine, & the Jail STD Prevalence Monitoring Group, 2002; National Commission on Correctional Health Care, 2002; White et al., 2001). Ever-incarcerated individuals often report behaviors associated with increased morbidity and mortality, such as having multiple sex partners and unprotected sex, intravenous drug use, and being homeless (Begier et al., 2010; Franklin, Kaytal, Mahajan, & Parvez, 2012; Parvez, Kaytal, Alper, Leibowitz, Venters, 2013). Risk taking behaviors upon release from incarceration may contribute to disease transmission during the community reentry period (Morrow, Eldridge, Nealey-Moore, Grinstead, & The Project START Study Group, transmission during the community reentry period (Morrow, Eldridge, Nealey-Moore, Grinstead, & The Project START Study Group, Rosen, Schoenbach, & Wohl, 2008). Additionally, many of the communities from which incarcerated individuals come, and to which they are released, are low-income neighborhoods with high rates of morbidity and all-cause mortality, thus contributing to the cyclical nature of incarceration and illness (Karpati, Bassett, & McCord, 2006; Myers et al., 2010, 2011)
In New York City (NYC), nearly 245,000 people (540,078 incarcerations) passed through the jail system from 2001 through 2005, representing 4% of the NYC population aged 16 to 89 years. Understanding the unique health issues facing individuals who have been incarcerated in NYC is vital to developing targeted interventions to reduce risks for this population and their community contacts. While studies generally show increased health risks among people who have been incarcerated and among people from low-income neighborhoods, understanding the role of incarceration, separate from poverty, in NYC is still needed. Similarly, while studies show high morbidity among people who have been homeless (Hwang, 2001; Kerker et al., 2005), it is critical to characterize the health risks among people who have been both incarcerated and homeless in NYC (Greenberg & Rosenheck, 2008) to identify appropriate interventions. We quantified morbidity and mortality among people who were ever incarcerated in NYC jails during 2001 to 2005 using data registries from the NYC Department of Correction (DOC), NYC Department of Health and Mental Hygiene (DOHMH), and NYC Department of Homeless Services (DHS). To assess the health risk of incarceration separately from poverty and homelessness, we compared morbidity and mortality of the ever-incarcerated population with that of the three lowest income neighborhoods of the city and of people who had experienced both incarceration and homelessness in NYC. These data can be used to guide NYC jail policy and programming as well as community-based programs serving ever-incarcerated individuals.
Method
Population in the Study
The study population included individuals aged 16 to 89 years who were incarcerated at least once in an NYC jail during 2001 to 2005 (ever incarcerated). This included detainees who were incarcerated in jail facilities on Rikers Island and in borough houses of detention in Brooklyn (until June 6, 2003, when it closed), Manhattan, and the Bronx during the study period. Ever-incarcerated people were compared with the NYC general population, excluding those who were incarcerated in NYC jails during the study period (nonincarcerated) and with the subset of nonincarcerated residents living in the lowest income NYC neighborhoods. The number of nonincarcerated people was calculated by subtracting the number of ever-incarcerated people from the total number of people in NYC or in the lowest income NYC neighborhoods according to the 2000 census. Within the ever-incarcerated population, people who had also been in NYC homeless shelters during the study period were compared to those who had not.
NYC jail facilities are operated by DOC. During this study period, the DOHMH oversaw chronic, urgent, and emergency medical and mental health services for the incarcerated. Newly incarcerated people receive a comprehensive medical history and physical examination within 24 hours of admission, including routine screening for TB and voluntary screening for HIV and STI. Gonorrhea and chlamydia screening is universally offered to females and, as of 2005, to all males aged ≤ 35 years. Syphilis screening is offered to everyone regardless of age. Treatment is provided as indicated. Case management is provided to people diagnosed with HIV infection or TB disease.
Data Sources
A cross-agency match was performed using data from DOHMH, DOC, and DHS (see Appendix). The DOC ever-incarcerated population data set was matched to DOHMH’s death, STI, HIV, and TB registries. All deaths occurring in NYC, as well as new diagnoses of STI, HIV, and suspected or confirmed cases of TB, are reported to DOHMH. We included reported cases of chlamydia, gonorrhea, and syphilis (all stages) and limited the analysis to 2001 through 2003, the years before routine chlamydia and gonorrhea screening was implemented in NYC jails for males, in order to avoid reporting increases in STI due to detection bias (Franklin et al., 2012). We included all reported HIV cases, including patients seen by an NYC provider even if the patient lived elsewhere. From 2001 through 2005, 8% of people in the NYC HIV registry were living outside of NYC or had an unknown residence (DOHMH, 2017). In addition, we included confirmed active TB cases either diagnosed in NYC or among NYC residents diagnosed elsewhere during 2001 to 2005. The match also included the registry of adults who used the DHS single adult shelter system during 2001 to 2005.
Variables
DOC provided demographic information, including race/ethnicity, sex, nativity, and zip code of residence (Lim et al., 2012). Age at the midpoint of the study period was used to allow for comparability across multiple data sources. Incarceration was described by frequency (1, 2–3, and ≥ 4 incarcerations) and total incarceration time (“length of stay” [LOS], which indicates cumulative days incarcerated during the study period: < 4 days and ≥ 4 days). Three types of criminal charges were analyzed for their association with health outcomes: violent crimes (including hazing, murder, assault, resisting arrest, and harassment), drug-related crimes (e.g., including possession and drug sales), and prostitution. Zip codes were categorized into 42 NYC neighborhoods (United Hospital Fund Staff, 2002). Lowest income neighborhoods were defined using the percentage of neighborhood residents who according to the U.S. Census 2000 were living below 200% of the federal poverty level. The three lowest income neighborhoods were all in the Bronx and included Crotona–Tremont, High Bridge–Morrisania, and Hunts Point–Mott Haven, where on average 42% of the population lived in poverty (Lim et al., 2012).
Statistical Analyses
We conducted descriptive analyses of our study population. We then examined overall and cause-specific mortality, STI case rates, HIV prevalence and newly diagnosed case rates, TB case rates, and homelessness rates, as well as incarceration characteristics (see Appendix). All measures of mortality and morbidity were age-adjusted using the direct standardization method based on U.S. Census 2000 data (Klein & Schoenborn, 2001). Pearson’s χ2 was used for comparisons of categorical variables. Nonoverlapping confidence intervals were used to determine whether rates were different between groups such as ever incarcerated versus nonincarcerated or males versus females. When two confidence intervals did overlap, significance was tested with a Z statistic. Differences between and within males and females were analyzed because rates and patterns of morbidity and mortality sometimes vary by sex. Multivariate regression analyses assessed whether, among ever-incarcerated people, mortality and morbidity were independently associated with demographic and incarceration characteristics as well as single adult homeless shelter use. Rate ratios (RRs) and prevalence ratios (PR) were estimated using a log-linear Poisson regression model, and 95% confidence intervals (95% CI) were calculated using the generalized estimation equation, which is generally robust to model misspecification. Statistical significance was tested at two-sided a <.05. Analyses were conducted using SAS® 9.2 software (SAS Institute, Inc., Cary, NC).
Results
During 2001 to 2005, 244,298 individuals aged 16 to 89 years were incarcerated at least once in NYC jails. Among ever-incarcerated people, the majority (63%) were aged 25 to 49 years. Fifty-one percent of the nonincarcerated NYC population and 52% of people in the lowest income neighborhoods were in this age range (Table 1). Most ever-incarcerated people (89%) were male; slightly less than half of the nonincarcerated (47%) and lowest income neighborhood (44%) populations were male. More than one quarter (29%) of ever-incarcerated people were jailed 2 to 3 times and 16% were jailed ≥ 4 times during the study period. The jail cumulative LOS was ≤ 1 month for 62% of the study population; nearly one quarter (22%) had an LOS of 31 to 90 days.
Table 1.
Demographic Characteristics of Ever-Incarcerated People, NYC 2001 to 2005.
| Number of Incarcerated (Column %)a | Number of New Yorkers (Column %)b | Number of New Yorkers in Lowest Income Neighborhoods (Column %)c | ||
|---|---|---|---|---|
| Total | 244,298 | 6,231,402 | 349,120 | |
| Age | 16–18 | 20,152 (8.3) | 311,453 (5.0) | 26,301 (7.5) |
| 19–24 | 52,129 (21.3) | 698,201 (11.2) | 48,839 (14.0) | |
| 25–34 | 68,432 (28.0) | 1,368,021 (22.0) | 78,448 (22.5) | |
| 35–49 | 86,143 (35.3) | 1,794,398 (28.8) | 103,434 (29.6) | |
| 50–89 | 17,442 (7.1) | 2,059,329 (33.1) | 92,098 (26.4) | |
| Sex | Male | 214,644 (89.3) | 2,898,672 (46.5) | 154,793 (44.3) |
| Female | 25,680 (10.7) | 3,332,730 (53.5) | 194,327 (55.7) | |
| Race/ethnicity | Non-Hispanic White | 23,156 (9.6) | 2,364,340 (37.9) | 6,024 (1.7) |
| Non-Hispanic Black | 125,245 (52.0) | 1,448,587 (23.3) | 114,989 (32.9) | |
| Hispanic | 84,798 (35.2) | 1,564,069 (25.1) | 216,463 (62.0) | |
| Asian | 2,222 (0.9) | 631,192 (10.1) | 4,035 (1.2) | |
| Other | 5,410 (2.3) | 223,214 (3.6) | 7,609 (2.2) | |
| Nativityd | U.S.-born (including Puerto Rico) | 189,737 (78.7) | 3,540,454 (56.7) | — |
| Foreign-born | 51,511 (21.4) | 2,703,739 (43.3) | — |
Note. NYC = New York City.
Column percentages do not include missing data.
Age, sex, and race/ethnicity data for the estimates of New Yorkers are from the U.S. Census Bureau. Nativity data for the estimates of New Yorkers are from Census 2000, Public Use Microdata Sample, United States, prepared by the U.S. Census Bureau (2003).
The “lowest income neighborhoods” include people living in three neighborhoods in the South Bronx (Crotona–Tremont, High Bridge–Morrisania, and Hunts Point–Mott Haven), which have the highest percentage of residents with income below 200% of the federal poverty level according to the U.S. Census 2000.
Nativity data were not available by zip code and therefore could not be analyzed for people living in the lowest income neighborhoods, which were defined by zip code.
Among the ever-incarcerated population, 27,441 (11%) had also used the single adult homeless shelter system, compared with 0.2% among the nonincarcerated population. Ever-incarcerated people who had used a shelter were more likely to have had multiple incarcerations during the study period than the ever incarcerated who had not used a shelter; 28% of shelter users had been incarcerated ≥ 4 times, versus 15% of nonshelter users (p < .05).
Mortality
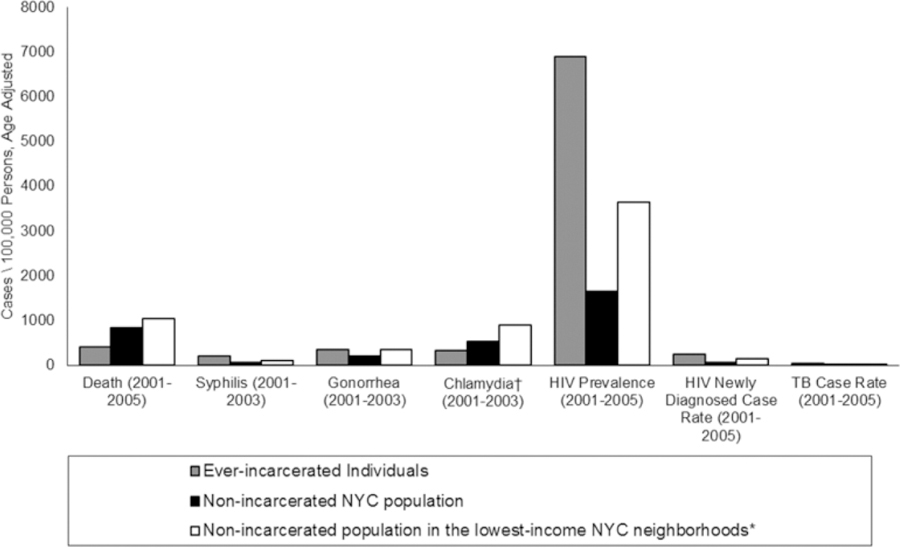
During the study period, there were 1,680 deaths among 244,298 ever incarcerated people. Their age-adjusted all-cause death rate was lower than the rates among the nonincarcerated (417 per 100,000, 95% CI [390, 446] vs. 841 per 100,000, 95% CI [838, 845]) and lowest income neighborhood (1,032 per 100,000, 95% CI [1015, 1049]) populations (Figure 1). There were no statistically significant sex differences in the overall death rates in the ever-incarcerated population, unlike in the nonincarcerated and lowest income neighborhood populations, in which males had higher death rates than females (Table 2). Among ever-incarcerated people, the most common cause of death was drug related (n = 335), followed by HIV (n = 332) and homicide (n = 279). Among the ever-incarcerated population, a higher proportion of females than males died due to HIV (31% vs. 18%, p < .0001) and a higher percentage of males than females died due to homicide (19% vs. 4%, p < .001). Seven percent of deaths occurred in jail.
Figure 1.
Morbidity and mortality among people incarcerated for at least 1 day in a New York City (NYC) jail, the nonincarcerated NYC population, and people in the lowest income neighborhoods* of NYC. *The “lowest income neighborhoods” include Crotona–Tremont, High Bridge–Morrisania, and Hunts Point–Mott Haven, which have the highest percentage of residents with income below 200% of the federal poverty level according to the U.S. Census 2000. †Rates of chlamydia are much higher among females than males in NYC (Bureau of Sexually Transmitted Disease Control Quarterly Report, 2005). Differences between the ever-incarcerated population, the nonincarcerated population, and people in the lowest income neighborhoods are affected by the fact that ever-incarcerated people were predominantly male, while people with chlamydia were predominantly female. Ever-incarcerated females had a higher rate of chlamydia (1,522, 95% CI [1,229, 1,880]) as compared to the general population of females (815, 95% CI [798, 832]). They were not statistically different from females in the lowest income neighborhoods (1,287, 95% CI [1,208, 1,369]).
Table 2.
Sex-Specific Morbidity and Mortality Among People Who Had Been Incarcerated for at Least 1 Day in an NYC Jail and in NYC Nonincarcerated Populations, 2001 to 2005.
| Ever-Incarcerated People |
Nonincarcerated NYC Residents |
Nonincarcerated NYC Residents From Lowest Income Neighborhoodsa |
|||||
|---|---|---|---|---|---|---|---|
| N | Rate per 100,000 [95% CI] | N | Rate per 100,000 [95% CI] | N | Rate per 100,000 [95% CI] | ||
| Deathb (2001 to 2005) | Female | 238 | 472.4 [383.1, 579.1] | 119,007 | 716.2 [712.1, 720.3] | 6,679 | 834.4 [814.4, 854.7] |
| Male | 1,440 | 415.3 [386.2, 446.3] | 125,442 | 1,004.2 [998.6, 1,009.8] | 7,329 | 1,320.7 [1,290.3, 1,351.6] | |
| Syphilis case ratec (2001 to 2003) | Female | 306 | 465.4 [265.4, 756.0] | 3,360 | 34.2 [30.8, 37.8] | 415 | 74.2 [54.1, 98.1] |
| Male | 664 | 176.5 [123.8, 241.7] | 6,353 | 76.5 [70.9, 82.3] | 556 | 140.6 [107.2, 179.4] | |
| Gonorrhea case ratec (2001 to 2003) | Female | 705 | 968.8 [743.0, 1,259.6] | 19,459 | 196.2 [188.0, 204.7] | 2,306 | 331.9 [292.3, 374.6] |
| Male | 1,901 | 281.1 [238.4, 330.6] | 17,960 | 201.7 [192.8, 210.7] | 1,891 | 392.5 [340.5, 449.2] | |
| Chlamydia case ratec (2001 to 2003) | Female | 1,082 | 1,522.1 [1,229.0, 1,880.0] | 81,034 | 814.7 [797.9, 831.8] | 9,047 | 1,287.0 [1,208.4, 1,368.8] |
| Male | 1,430 | 199.7 [165.8, 240.2] | 16,998 | 190.1 [181.6, 198.9] | 1,939 | 387.9 [337.3, 443.0] | |
| HIV prevalenced (2001 to 2005) | Female | 2,694 | 11,638.3 [10,947.6, 12,373.0] | 30,018 | 935.7 [925.1, 946.4] | 4,785 | 2,588.2 [2,514.6, 2,663.6] |
| Male | 9,280 | 6,361.3 [6,179.0, 6,548.5] | 66,284 | 2,530.1 [2,510.8, 2,549.5] | 6,189 | 5,202.2 [5072.1, 5,335.0] | |
| HIV new case ratee (2001 to 2005) | Female | 587 | 541.5 [474.0, 619.1] | 6,566 | 40.2 [39.2, 41.2] | 1,124 | 117.1 [110.3, 124.3] |
| Male | 1,908 | 218.7 [204.6, 233.8] | 13,517 | 94.6 [93.0, 96.3] | 1,432 | 202.9 [192.2, 214.0] | |
| TB case ratef (2001 to 2005) | Female | 60 | 47.7 [1.1, 205.3] | 2,270 | 13.7 [11.0, 16.7] | 187 | 19.8 [8.1, 37.3] |
| Male | 294 | 43.8 [15.7, 88.4] | 3,520 | 26.5 [22.3, 31.2] | 246 | 40.1 [18.8, 70.2] | |
Note. NYC = New York City; TB = tuberculosis.
The “lowest income neighborhoods” include Crotona–Tremont, High Bridge–Morrisania, and Hunts Point–Mott Haven, which have the highest percentage of residents with income below 200% of the federal poverty level according to the U.S. Census 2000.
Sex was unknown for 2 ever-incarcerated people who died.
N is the number of cases, not people.
Sex was unknown for 57 ever-incarcerated people in the HIV prevalence category.
Sex was unknown for 16 ever-incarcerated people in the HIV incidence category.
Sex was unknown for 2 ever-incarcerated people who had TB.
STIs
During 2001 to 2003, there were 306 cases of syphilis (all stages), 705 cases of gonorrhea, and 1,082 cases of chlamydia reported among ever-incarcerated females and 664, 1,901, and 1,430 cases of syphilis, gonorrhea, and chlamydia, respectively, among males. The case rates of syphilis, gonorrhea, and chlamydia were higher among ever-incarcerated females than among nonincarcerated females in NYC (Table 2). While syphilis and gonorrhea rates were higher among ever-incarcerated females than among females in the lowest income neighborhoods, the chlamydia case rate was not statistically different between the two populations.
Ever-incarcerated males had higher syphilis and gonorrhea rates than did nonincarcerated males (Table 2), but chlamydia rates were not statistically different. Syphilis rates were not statistically different among ever-incarcerated males versus males in the lowest income neighborhoods; in contrast, rates of gonorrhea and chlamydia were lower among ever-incarcerated males than among males in the lowest income neighborhoods. There was a higher syphilis rate among males compared to females in the nonincarcerated population; however, the ever-incarcerated syphilis rate was higher among females than males.
HIV Prevalence and Newly Diagnosed Case Rates
During 2001 to 2005, among the ever incarcerated, there were 9,280 males, 2,694 females, and 57 people with missing sex data who had HIV infection (Table 2). HIV prevalence was 4 times as high among ever-incarcerated people (6,888 per 100,000, 95% CI [6711, 7068]) as among nonincarcerated New Yorkers (1,652 per 100,000, 95% CI [1641, 1662]) and nearly twice as high as among people living in the lowest income neighborhoods (3,635 per 100,000, 95% CI [3566, 3704]; Figure 1). Ever-incarcerated females had a nearly twice as high HIV prevalence as males, in contrast to higher male HIV prevalence among the nonincarcerated and lowest income neighborhood populations (Table 2). The female ever-incarcerated HIV prevalence was 12 times that among nonincarcerated females and 4.5 times as high as the lowest income neighborhood female population prevalence. The male ever-incarcerated HIV prevalence was 2.5 times the male nonincarcerated prevalence and slightly higher than the lowest income population prevalence.
Among ever-incarcerated individuals, 1,908 males, 587 females, and 16 people with missing sex data were newly diagnosed with HIV during the study period. The newly diagnosed HIV case rate was nearly 4 times as high among ever-incarcerated people (250 per 100,000, 95% CI [236, 265]) as among the nonincarcerated (65 per 100,000, 95% CI [65, 66]) and nearly twice that among people in the lowest income neighborhoods (153 per 100,000, 95% CI [147, 160]; Figure 1). Among the ever incarcerated, the HIV case rate was 2.5 times as high as among females than among males, in contrast to community rates where male HIV incidence rates were higher (Table 2). The HIV case rate among ever-incarcerated females was 13.5 times as high as among nonincarcerated females and nearly 5 times that among females from the lowest income neighborhoods. Ever-incarcerated males had twice as high of an HIV case rate as nonincarcerated males.
TB
Among ever-incarcerated people, there were 294 males, 60 females, and 2 people with missing sex data with confirmed active TB during 2001 to 2005. The active TB case rate among ever-incarcerated people was 44 per 100,000 (95% CI [18, 86]), which was not statistically different from the rates among the nonincarcerated (19, 95% CI [17, 22]) and lowest income neighborhood populations (28, 95% CI [16, 43]; Figure 1). No statistically different sex differences in TB rates were seen among the ever-incarcerated or the lowest income neighborhoods; among the nonincarcerated, males had nearly twice the TB rate as females (Table 2). There were no statistically significant differences among females who had been incarcerated compared to nonincarcerated females or females in the lowest income neighborhoods. There were also no significant differences among males across the three groups.
Incarceration Characteristics
After adjusting for demographic and incarceration characteristics as well as single adult homeless shelter use, HIV, all three STI, and TB rates were higher among people with multiple incarcerations than among those with only one incarceration during the study period (Table 3). Among ever-incarcerated people charged with prostitution (n = 3,287, 1%), HIV prevalence and case rates of HIV, all three STI, and TB were higher than those among persons not charged with prostitution. People who were incarcerated at least once due to a violent crime charge had lower HIV prevalence and newly diagnosed case rates than those not charged with a violent crime. People charged with drug crimes had higher HIV prevalence and new case rates, and higher case rates of syphilis and gonorrhea than those not charged with drug crimes.
Table 3.
RRs and HIV PR; (95% Confidence Interval)a of Morbidity and Mortality by Incarceration Patterns Among People Who Had Been Incarcerated for at Least 1 Day in NYC.
| Mortality (2001 to 2005) |
Syphilis Case Rate (2001 to 2003) |
Gonorrhea Case Rate (2001 to 2003) |
Chlamydia Case Rate (2001 to 2003) |
HIV Prevalence (2001 to 2005) |
HIV New Case Rate (2001 to 2005) |
TB Case Rate (2001 to 2005) |
|
|---|---|---|---|---|---|---|---|
| RRadj [95% CI]b | RRadj [95% CI]b | RRadj [95% CI]b | RRadj [95% CI]b | PRadj [95% CI]b | RRadj [95% CI]b | RRadj [95% CI]b | |
| Frequency of incarceration during study period | |||||||
| 1 | — | — | — | — | — | — | — |
| 2–3 | 0.9 [0.8, 1.1] | 1.3 [1.1, 1.6] | 1.7 [1.5, 1.9] | 1.8 [1.6, 2.0] | 1.5 [1.4, 1.5] | 1.3 [1.2, 1.5] | 1.5 [1.2, 2.0] |
| ≥4 | 0.7 [0.6, 0.9] | 2.7 [2.3, 3.3] | 2.7 [2.4, 3.1] | 2.6 [2.2, 2.9] | 2.0 [1.9, 2.1] | 2.2 [1.9, 2.5] | 1.6 [1.2, 2.3] |
| Duration of incarceration | |||||||
| < 4 days | — | — | — | — | — | — | — |
| ≥4 days | 1.0 [0.9, 1.2] | 4.5 [3.1, 6.5] | 1.2 [1.0, 1.4] | 1.1 [1.0, 1.3] | 1.4 [1.3, 1.5] | 1.3 [1.2, 1.5] | 1.0 [0.8, 1.4] |
| Chargesc | |||||||
| Violence vs. any other type of charge (not charged with violence) | 1.1 [1.0, 1.2] | 0.9 [0.8, 1.0] | 1.2 [1.1, 1.3] | 1.1 [1.0, 1.2] | 0.8 [0.8, 0.9] | 0.9 [0.8, 1.0]d | 0.9 [0.7, 1.2] |
| Drug vs. any other type of charge (not charged with drug) | 1.3 [1.1, 1.4] | 1.4 [1.2, 1.7] | 1.2 [1.1, 1.3] | 1.0 [1.0, 1.2] | 1.5 [1.4, 1.5] | 1.3 [1.2, 1.4] | 1.2 [1.0, 1.5] |
| Prostitution vs. any other type of charge (not charged with prostitution) | 1.2 [0.8, 1.8] | 2.5 [1.9, 3.2] | 2.0 [1.7, 2.4] | 1.6 [1.4, 1.9] | 1.8 [1.7, 2.0] | 2.9 [2.4, 3.5] | 2.7 [1.5, 4.9] |
| Admitted to single adult homeless shelters in 2001 to 2005 | |||||||
| Yes vs. no | 2.2 [2.0, 2.5] | 1.1 [0.9, 1.3] | 1.3 [1.2, 1.5] | 1.0 [0.9, 1.2] | 1.0 [1.0, 1.1] | 1.5[1.4, 1.7] | 1.5 [1.2, 2.0] |
Note. NYC = New York City; TB = tuberculosis; RR = rate ratios; PR = prevalence ratio.
RRs and PR were estimated using a log-linear Poisson regression model, and 95% confidence intervals for RR and PR were calculated using the generalized estimation equation.
Models adjusted for age, race/ethnicity, and sex.
People may have been charged with multiple crimes, and therefore, the three categories of charges are not mutually exclusive.
The upper bound of the CI is 0.9987 and therefore considered significant.
The rate of drug-related death was positively associated with drug-related criminal charges (RR = 1.48, 95% CI [1.16, 1.90]). The rate of HIV-related death was also positively associated with drug-related criminal charges (RR = 1.59, 95% CI [1.24, 2.05]) and negatively associated with violence-related charges (RR = 0.67, 95% CI [0.50, 0.90]).
Homelessness
Ever-incarcerated people who had used single adult shelters during the study period had higher case rates of HIV (393, 95% CI [352, 440] vs. 229, 95% CI [214, 245]) and gonorrhea (532, 95% CI [377, 729] vs. 320, 95% CI [275, 373]), than those without shelter use; HIV prevalence and syphilis and chlamydia case rates did not statistically differ between the groups when controlling for age, race/ ethnicity, and sex (Table 3). Although the case rate of active TB among ever-incarcerated people who had used shelters was not statistically different from those who had not used shelters (73, 95% CI [7, 226] vs. 39, 95% CI [13,82], when adjusting for the variables in Table 3, the TB case rate was 1.5 times as high among those who had been in shelters. The overall death rate was twice as high among ever-incarcerated people who had used shelters than among those who had not. Leading causes of death among ever-incarcerated individuals who had been in single adult homeless shelters were drug related (27%), HIV (19%), and heart disease (11%). For those without shelter use, leading causes of death were homicide (21%), HIV (20%), and drug related (17%).
Discussion
Our study represents the first match of incarcerations, health, and homeless shelter registries conducted to characterize the health status of ever-incarcerated populations in NYC. We found substantial morbidity among people ever incarcerated in NYC jails during 2001 to 2005, suggesting that people experiencing incarceration have greater health risks than both the nonincarcerated and the subset of nonincarcerated living in the lowest income neighborhoods.
We found disproportionately high HIV prevalence rates, HIV newly diagnosed case rates, and STI case rates among the ever-incarcerated versus nonincarcerated population. Ever-incarcerated people also had higher HIV prevalence and newly diagnosed case rates than the lowest income neighborhood populations. Published reports have shown that ever-incarcerated populations are at high risk for HIV and other STI due to risky behaviors such as having multiple sex partners, engaging in condomless sex, and/or engaging in community sex work (Begier et al., 2010; Franklin et al., 2012; Human Rights Watch, 2012; Parvez et al., 2013). Risky sexual behavior is especially prevalent both shortly before and after incarceration (MacGowan et al., 2003; Morrow et al., 2007; Stephenson et al., 2006). Our results support continued jail-based HIV and STI screening and treatment for incarcerated populations.
An alternative explanation about higher HIV and STI rates among ever-incarcerated individuals than nonincarcerated ones is ascertainment bias due to differences in accessing HIV and STI screening in jail versus in the community. Evidence suggests that ever-incarcerated people do not routinely seek health care in the community (Conklin, Lincoln, & Tuthill, 2000; Kulkarni, Baldwin, Light-stone, Gelberg, & Diamant, 2010; Lee, Vlahov, & Freudenberg, 2006; Wang et al., 2008), whereas those incarcerated are offered screening at jail entry.
We found that ever-incarcerated females were a particularly vulnerable group with high morbidity and mortality rates. They had higher HIV and syphilis rates than ever-incarcerated males and disproportionately higher HIV and STI rates than nonincarcerated and lowest income neighborhood females, suggesting that they have additional health risks relative to ever-incarcerated males. The higher HIV prevalence among incarcerated females versus males was also documented in a DOHMH HIV serosurvey of jail entrants (Begier et al., 2010). Ever-incarcerated females, particularly those engaging in sex work, have reported substance use, exchanging sex for other needs, having multiple sex partners and unprotected sex, being homeless, and experiencing intimate partner violence or childhood abuse, all of which can adversely impact their mental and physical health (Human Rights Watch, 2012; Kim, Johnson, Goswami, & Puisis, 2011; Meyer et al., 2014; Parvez et al., 2013). Incarcerated females leaving jail often have greater comorbidities, including mental health and substance use issues, and worse HIV treatment outcomes in the community than males (Meyer et al., 2014). DOHMH has worked with community partners to identify gender-specific strategies to address the unique social services and health care needs of ever-incarcerated females (Meyer et al., 2014; Parvez et al., 2013).
We also found that people experiencing both incarceration and homelessness were at higher risk of morbidity and mortality than those only experiencing incarceration. They had significantly higher rates of HIV incidence, gonorrhea, TB, and mortality than those without shelter use, when adjusting for other variables. Homelessness has been associated with numerous HIV and STI risk factors, including past child abuse, current mental illness or substance use disorders, unprotected sex or multiple sex partners, and trading sex for other needs (Caton et al., 2013; Jenness et al., 2011). The association between homelessness and TB has been documented elsewhere (Kerker et al., 2005) and may be related to inadequate health care access, substance use, and living in crowded conditions (Haddad, Wilson, Ijaz, Marks, & Moore, 2005; Samuel et al., 2012; Tan de Bibiana et al., 2011). The mortality risk among the homeless has been attributed to substance use and injury, among other causes (Barrow, Herman, Córdova, & Struening, 1999; Hibbs et al., 1994). DOHMH and DHS have identified interventions to mitigate health risks and mortality among homeless populations (Gambatese et al., 2013; Kerker et al., 2005); further strategies targeted toward the ever incarcerated and homeless are needed.
Our finding of a lower all-cause death rate among ever-incarcerated people has been found by others (Spaulding et al., 2011) and may reflect a decreased likelihood of violence, drug overdose, or traffic accidents during incarceration. This finding could also reflect greater access to health care during incarceration than when living in the community. A DOHMH report on health disparities revealed limited access to health care among the poorest New Yorkers compared with the wealthiest (Karpati et al., 2004). In contrast, NYC jails provide comprehensive medical and mental health services to all incarcerated people. Some studies have found excess mortality after release from jail (Binswanger et al., 2007; Lim et al., 2012; Rosen et al., 2008). Lim et al. (2012) found that people formerly incarcerated in NYC jails were at increased risk of drug-and homicide-related deaths postincarceration. Further studies exploring mortality risk among the ever incarcerated, including those with extended postincarceration follow-up periods, are warranted.
Limitations
This study has limitations. First, our data may have been undermatched by 10% to 20% (see Appendix), and calculated rates may be underestimated due to incomplete data matching. Second, data from those who used single adult shelters are not generalizable to the general homeless population in NYC (i.e., homeless adults in families, with or without minor children, adults who are persistently unsheltered, or adults or families residing in alternative shelter systems1). Third, these data were limited in the potential confounders or explanatory variables that could be included in analyses. Fourth, this analysis does not indicate whether disease transmission occurred during incarceration. Fifth, the average daily inmate population in NYC jails declined from 13,576 in fiscal year (FY) 2005 to 10,240 in FY 2015 (NYC Mayor’s Office of Operations, 2009, 2015), and the characteristics of the shrinking population may have changed to an extent that an analysis of more recent data could yield different conclusions. However, a study of the NYC jail population incarcerated in 2011 showed a very similar sex and race/ethnicity composition to the population described in this article, and the percentage of inmates in NYC jails who had HIV was higher than in NYC overall (Jordan et al., 2013). Other data are not available for this study to compare the characteristics of people incarcerated from 2001 through 2005 to more recent years. Finally, our study follow-up period of 5 years may be insufficient to detect certain health events such as TB or mortality; thus, our article is limited to health issues that developed proximal to incarceration. Nevertheless, this article has strengths in the breadth of health indicators assessed over multiple years using DOHMH registries and large sample sizes, providing concrete measures of the burden of morbidity and mortality among people who were ever incarcerated in NYC jails from 2001 through 2005.
Conclusions
Ever-incarcerated individuals in NYC are at increased risk for conditions of public health importance, when compared with nonincarcerated populations. Although incarcerated people often come from low-income neighborhoods with high morbidity rates, those experiencing incarceration have added risk for poor health. Ever-incarcerated females and those experiencing homelessness are particularly vulnerable. Our study supports continued jail-based public health screening, treatment, and case management (Jordan et al., 2013; Mellow et al., 2008). In addition, sex-specific jail-and community-based interventions need to be continued to prevent or mitigate the high morbidity experienced by ever-incarcerated people. Furthermore, continued surveillance of health outcomes among the ever-incarcerated population is needed. Finally, interventions aimed at people who have been both incarcerated and homeless, such as supportive housing, which have been found to improve lives (Aidala, McAllisterm, Yomogida, & Shubert, 2014), should be expanded in NYC.
Acknowledgments
We are grateful for preparation of data sets, data linkage, interpretation of results, and/or review of the draft manuscript by the NYC Department of Correction, the NYC Department of Homeless Services, and numerous people within the NYC Department of Health and Mental Hygiene, including those in the Commissioner’s Office, Division of Epidemiology, and Bureaus of HIV/AIDS Prevention and Control, STD Prevention and Control, TB Control, Vital Statistics, Public Health Informatics and Data Services, and Correctional Health Services.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Appendix
Methodology Supplement
Matching process.
The data set of people ever incarcerated in NYC jails from 2001 through 2005 was deduplicated to identify unique individuals. Through QualityStage software (IBM Corporation, Armonk, NY), a matching algorithm was implemented using first name, last name, date of birth, sex, and Social Security number. Each record in a matched set had a weight based on reliability and availability of the matching fields. NYC DOHMH staff reviewed samples of the matched sets and determined a weight cut point at which all potential matched records were considered to be actual matches (Lim et al., 2012). To estimate reliability, the match outcomes were compared with the surveillance data from each disease registry that originated from NYC jails during 2001 to 2005. The percentages of registry lab and provider reports originating from NYC jails that also matched to a person in the DOC data set were 89%, 85%, and 81% for STI, HIV, and TB, respectively, suggesting that the match algorithm undermatched by 10% to 20%. Overmatching was likely to be low because subject matter experts minimized the probability of false matches when setting cut points.
Rate calculations.
To calculate death rates, the number of deaths or new diagnoses during 2001 to 2005 was used as the numerator. Person-years in the denominator accounted for time at risk, as these were events that could occur only once in a lifetime. For mortality rates among ever-incarcerated people, person-years were the number of years between the first incarceration during the study period and the end of the study period or death. For people who had not been incarcerated in NYC jails during 2001 to 2005 (nonincarcerated), we divided the number of deaths by 5 times the NYC 2000 Census counts as a proxy of person-years in the reference population. We removed the number of ever-incarcerated individuals from both the numerator and denominator of NYC rates.
Annualized case rates of syphilis, gonorrhea, and chlamydia diagnosed in NYC were limited to 2001 to 2003 because a jail-based STI screening program was piloted in late December 2003 and implemented in all jails in 2005 among males aged ≤ 35 years (Franklin et al., 2012). This jail-based screening greatly increased the rate of male chlamydia and gonorrhea cases reported by jails (Pathela et al., 2009). To avoid making population comparisons when disease detection rates could have differed due to screening opportunities, the STI analysis was limited to the years before the jail STI screening policy changed. Because STI could occur multiple times, we divided the STI cases among ever-incarcerated people by the total number of ever-incarcerated people during 2001 to 2003. We annualized this case rate by dividing STI rates by 3. Similar computations were used to calculate STI rates among nonincarcerated people.
HIV prevalence was based on individuals diagnosed with HIV during 2001 to 2005 or who were diagnosed before 2001 and were presumed through death registry matching to be alive as of January 1, 2001. We calculated HIV prevalence among ever-incarcerated people by dividing the number of ever-incarcerated people diagnosed with HIV on December 31, 2005 or earlier by the total number of ever-incarcerated people during the study period. To obtain HIV prevalence among nonincarcerated people, we divided the number of nonincarcerated NYC residents living with HIV during 2001 to 2005 by NYC population counts from the 2000 U.S. Census (excluding the total number of ever-incarcerated people).
The HIV newly diagnosed case rates represent people newly diagnosed with HIV during 2001 to 2005. To calculate rates of new HIV diagnosis, the number of new diagnoses during 2001 to 2005 was used as the numerator. Person-years in the denominator accounted for time at risk, as these were events that could occur only once in a lifetime. For HIV newly diagnosed case rates among ever-incarcerated people, the denominator was limited to people who did not have an HIV diagnosis prior to 2001; person-years were calculated as the time difference between the beginning of the study (January 1, 2001) and the first HIV diagnosis or the end of the study (December 31, 2005) for people who were not HIV infected. For nonincarcerated NYC residents, we divided new HIV diagnoses and the number of deaths by 5 times the NYC 2000 Census counts as a proxy of person-years in the reference population. Since incarcerated individuals were a subset of NYC residents, we removed their contributions from both the numerator and denominator of NYC rates.
Because TB theoretically could occur more than once, we divided the TB cases among ever-incarcerated people by the total number of ever-incarcerated people during 2001 to 2005. We annualized this case rate by dividing TB rates by 5. Similar computations were used to calculate TB rates among nonincarcerated people.
The percentage of ever-incarcerated people who had been in a single adult homeless shelter for at least 1 day during 2001 to 2005 was calculated by dividing the number of people who had been both incarcerated and in a shelter by the number of ever-incarcerated people. Single adult shelters can be used by people aged ≥ 18 years. Although NYC jails can admit inmates as young as 16 years, because we did not calculate the age at any given incarceration, we included all jail inmates in the homeless shelter analysis regardless of age. The percentage of people who had been in a single adult shelter among the nonincarcerated NYC population was calculated by dividing the number of people who had been in a shelter but not incarcerated by 5 times the difference between the number of people in NYC aged 18 to 89 years and the total number of ever-incarcerated people.
Footnotes
Declaration of Conflicting Interests
The authors disclosed no conflicts of interest with respect to the research, authorship, or publication of this article. For information about JCHC’s disclosure policy, please see the Self-Study Program.
Alternative shelter systems include those serving people with advanced HIV/AIDS, victims of domestic violence, and individuals facing housing emergencies, such as fire or flood.
References
- Aidala AA, McAllister W, Yomogida M, & Shubert V (2014). Frequent users service enhancement ‘FUSE’ initiative. New York City FUSE II evaluation report. New York, NY: Columbia University, Mailman School of Public Health; Retrieved from http://www.csh.org/wp-content/uploads/2014/01/FUSE-Eval-Report-Final_Linked.pdf [Google Scholar]
- Baillargeon J, & Bradshaw P (2003). The association of infectious disease diagnoses with incarceration-related factors among prison inmates. Journal of Correctional Health Care, 10, 15–33. doi: 10.1177/107834580301000103 [DOI] [Google Scholar]
- Barrow SM, Herman DB, Córdova P, & Struening EL (1999). Mortality among homeless shelter residents in New York City. American Journal of Public Health, 89, 529–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begier EM, Bennani Y, Forgione L, Punsalang A, Hanna DB, Herrera J, … Parvez F (2010). Undiagnosed HIV infection among New York City jail entrants, 2006: Results of a blinded serosurvey. Journal of Acquired Immune Deficiency Syndromes, 54, 93–101. doi: 10.1097/QAI.0b013e3181c98fa8 [DOI] [PubMed] [Google Scholar]
- Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, Elmore JG, & Koepsell TD (2007). Release from prison—A high risk of death for former inmates. New England Journal of Medicine, 356, 157–165. doi: 10.1056/NEJMsa064115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caton CLM, El-Bassel N, Gelman A, Barrow S, Herman D, Hsu E, … Felix A (2013). Rates and correlates of HIV and STI infection among homeless women. AIDS and Behavior, 17, 856–864. doi: 10.1007/s10461-012-0198-x [DOI] [PubMed] [Google Scholar]
- Conklin TJ, Lincoln T, & Tuthill RW (2000). Self-reported health and prior health behaviors of newly admitted correctional inmates. American Journal of Public Health, 90, 1939–1941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklin WB, Katyal M, Mahajan R, & Parvez FM (2012). Chlamydia and gonorrhea screening using urine-based nucleic acid amplification testing among males entering New York City jails: A pilot study. Journal of Correctional Health Care, 18, 120–130. doi: 10.1177/1078345811435767 [DOI] [PubMed] [Google Scholar]
- Gambatese M, Marder D, Begier E, Gutkovich A, Mos R, Griffin A, … Madsen A (2013). Programmatic impact of 5 years of mortality surveillance of New York City homeless populations. American Journal of Public Health, 103, S193–S198. doi: 10.2105/AJPH.2012.301196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg GA, & Rosenheck RA (2008). Jail incarceration, homelessness, and mental health: A national study. Psychiatric Services, 59, 170–177. doi: 10.1176/appi.ps.59.2.170 [DOI] [PubMed] [Google Scholar]
- Haddad MB, Wilson TW, Ijaz K, Marks SM, & Moore M (2005). Tuberculosis and homelessness in the United States, 1994–2003. Journal of the American Medical Association, 293, 2762–2766. doi: 10.1001/jama.293.22.2762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammett TM, Harmon MP, & Rhodes W (2002). The burden of infectious disease among inmates of and releasees from US correctional facilities, 1997. American Journal of Public Health, 92, 1789–1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbs JR, Benner L, Klugman L, Spencer R, Macchia I, Mellinger AK, & Fife D (1994). Mortality in a cohort of homeless adults in Philadelphia. New England Journal of Medicine, 331, 304–309. doi: 10.1056/NEJM199408043310506 [DOI] [PubMed] [Google Scholar]
- Human Rights Watch. (2012). Sex workers at risk. Condoms as evidence of prostitution in four US cities. Retrieved from http://www.hrw.org/sites/default/files/reports/us0712ForUpload_1.pdf
- Hwang SW (2001). Homelessness and health. Canadian Medical Association Journal, 164, 229–233. [PMC free article] [PubMed] [Google Scholar]
- Jenness SM, Begier EM, Neaigus A, Murrill CS, Wendel T, & Hagan H (2011). Unprotected anal intercourse and sexually transmitted diseases in high-risk heterosexual women. American Journal of Public Health, 101, 745–750. doi: 10.2105/AJPH.2009.181883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan AO, Cohen LR, Harriman G, Teixeira PA, Cruzado-Quinones J, & Venters H (2013). Transitional care coordination in New York City jails: Facilitating linkages to care for people with HIV returning home from Rikers Island. AIDS and Behavior, 17, S212–S219. doi: 10.1007/s10461-012-0352-5 [DOI] [PubMed] [Google Scholar]
- Karpati AM, Bassett MT, & McCord C (2006). Neighbourhood mortality inequalities in New York City,1989–1991 and 1991–2001. Journal of Epidemiology and Community Health, 60, 1060–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karpati AM, Kerker B, Mostashari F, Singh T, Hajat A, Thorpe L, … Frieden T (2004). Health disparities in New York City. New York: New York City Department of Health and Mental Hygiene; Retrieved from http://www.commonwealthfund.org/*/media/files/publications/other/2004/jul/health-disparities-in-new-york-city/karpati_disparities-pdf.pdf [Google Scholar]
- Kerker B, Bainbridge J, Li W, Kennedy J, Bennani Y, Agerton T, … Gutkovich A (2005). The health of homeless adults in New York City: A report from the New York City Departments of Health and Mental Hygiene and Homeless Services. Retrieved from https://www1.nyc.gov/assets/doh/downloads/pdf/epi/epi-homeless-200512.pdf
- Kim S, Johnson TP, Goswami S, & Puisis M (2011). Risk factors for homelessness and sex trade among incarcerated women: A structural equation model. Journal of International Women’s Studies, 12, 128–148. [PMC free article] [PubMed] [Google Scholar]
- Klein RJ, & Schoenborn CA (2001). Age adjustment using the 2000 projected U.S. population. Healthy People 2010 Statistical Notes, no.20. Hyattsville, MD: National Center for Health Statistics; Retrieved from http://www.cdc.gov/nchs/data/statnt/statnt20.pdf [PubMed] [Google Scholar]
- Kulkarni SP, Baldwin S, Lightstone AS, Gelberg L, & Diamant AL (2010). Is incarceration a contributor to health disparities? Access to care of formerly incarcerated adults. Journal of Community Health, 35, 268–274. doi: 10.1007/s10900-010-9234-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J, Vlahov D, & Freudenberg N (2006). Primary care and health insurance among women released from New York City jails. Journal of Health Care for the Poor and Underserved, 17, 200–217. doi: 10.1353/hpu.2006.0028 [DOI] [PubMed] [Google Scholar]
- Lim S, Levanon Seligson A, Parvez FM, Luther CW, Mavinkurve MP, Binswanger IA, & Kerker BD (2012). Risks of drug-related death, suicide, and homicide during the immediate post-release period among people released from New York City jails, 2001–2005. American Journal of Epidemiology, 175, 519–526. doi: 10.1093/aje/kwr327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacGowan RJ, Margolis A, Gaiter J, Morrow K, Zack B, & Askew J, … The Project START Study Group. (2003). Predictors of risky sex of young men after release from prison. International Journal of STD & AIDS, 14, 519–523. [DOI] [PubMed] [Google Scholar]
- Massoglia M (2008). Incarceration as exposure: The prison, infectious disease, and other stress-related illnesses. Journal of Health and Social Behavior, 49, 56–71. [DOI] [PubMed] [Google Scholar]
- Mellow J, Hoge SK, Lee JD, Natarajan M, Yu SV, Greifinger RB, & Belkin G (2008). Mapping the innovation in correctional health care service delivery in New York City. Retrieved from http://johnjay.jjay.cuny.edu/files/NYCMappingHeathCare.pdf
- Mertz KJ, Voigt RA, Hutchins K, & Levine WC, & The Jail STD Prevalence Monitoring Group. (2002). Findings from STD screening of adolescents and adults entering corrections facilities: Implications for STD control strategies. Sexually Transmitted Diseases, 29, 834–839. [DOI] [PubMed] [Google Scholar]
- Meyer JP, Zelenev A, Wickersham JA, Williams CT, Teixeira PA, & Altice FL (2014). Gender disparities in HIV treatment outcomes following release from jail: Results from a multicenter study. American Journal of Public Health, 104, 434–441. doi: 10.2105/AJPH.2013.301553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrow KM, Eldridge G, Nealey-Moore J, & Grinstead O, & The Project START Study Group. (2007). HIV, STD, and hepatitis risk in the week following release from prison: An event-level analysis. Journal of Correctional Health Care, 13, 27–38. doi: 10.1177/1078345807299457 [DOI] [Google Scholar]
- Myers C, Hakenewerth A, Olson C, Kerker B, Krauskopf M, Tavares A, … Farley T (2011). Health disparities in New York City: Disparities in breast, colorectal, and cervical cancers in New York City. New York: New York City Department of Health and Mental Hygiene; Retrieved from https://www1.nyc.gov/assets/doh/downloads/pdf/episrv/disparitiestwo.pdf [Google Scholar]
- Myers C, Olson C, Kerker B, Thorpe L, Greene C, & Farley T (2010). Health disparities in New York City: Health disparities in life expectancy and death. New York: New York City Department of Health and Mental Hygiene; Retrieved from https://www1.nyc.gov/assets/doh/downloads/pdf/episrv/disparitiesone.pdf [Google Scholar]
- National Commission on Correctional Health Care. (2002). The health status of soon-to-be-released inmates: A report to Congress (Vol. 1). Retrieved from https://www.ncjrs.gov/pdffiles1/nij/grants/189735.pdf [Google Scholar]
- New York City Department of Health and Mental Hygiene. (2017). New York City HIV/AIDS annual surveillance statistics. Retrieved from https://www1.nyc.gov/site/doh/data/data-sets/hiv-aids-annual-surveillance-statistics.page
- NYC Mayor’s Office of Operations. (2009, 2015). Mayor’s management reports. Retrieved from http://www1.nyc.gov/site/operations/performance/archives.page
- Parvez F, Katyal M, Alper H, Leibowitz R, & Venters H (2013). Female sex workers incarcerated in New York City jails: Prevalence of sexually transmitted infections and associated risk behaviors. Sexually Transmitted Infections, 89, 280–284. doi: 10.1136/sextrans-2012-050977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pathela P, Hennessy RR, Blank S, Parvez F, Franklin W, & Schillinger JA (2009) The contribution of a urine-based jail screening program to citywide male chlamydia and gonorrhea case rates in New York City. Sexually Transmitted Diseases, 36, S58–S61. [DOI] [PubMed] [Google Scholar]
- Rosen DL, Schoenbach VJ, & Wohl DA (2008). All-cause and cause-specific mortality among men released from state prison, 1980–2005. American Journal of Public Health, 98, 2278–2284. doi: 10.2105/AJPH.2007.121855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samuel V, Benjamin C, Renwick O, Hilliard A, Arnwine S, Spike D, … Dantes R (2012). Notes from the field: Tuberculosis cluster associated with homelessness—Duval County, Florida, 2004–2012. Morbidity and Mortality Weekly Report, 61, 539–540. [PubMed] [Google Scholar]
- Spaulding AC, Seals RM, McCallum VA, Perez SD, Brzozowski AK, & Steenland NK (2011). Prisoner survival inside and outside of the institution: Implications for health-care planning. American Journal of Epidemiology, 173, 479–487. doi: 10.1093/aje/kwq422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson BL, Wohl DA, McKaig R, Golin CE, Shain L, Adamian M, … Kaplan AH (2006). Sexual behaviours of HIV-seropositive men and women following release from prison. International Journal of STD & AIDS, 17, 103–108. doi: 10.1258/095646206775455775 [DOI] [PubMed] [Google Scholar]
- Tan de Bibiana J, Rossi C, Rivest P, Zwerling A, Thibert L, McIntosh F, … Schwartzman K (2011). Tuberculosis and homelessness in Montreal: A retrospective cohort study. BMC Public Health, 11, 833. doi: 10.1186/1471-2458-11-833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The New York City Department of Health and Mental Hygiene Bureau of Sexually Transmitted Disease Control Quarterly Report Vol 3, no.4, December 2005. Accessed August 21, 2017 from: https://www1.nyc.gov/assets/doh/downloads/pdf/std/std-quarterlyreport2005-4.pdf [Google Scholar]
- United Hospital Fund Staff. (2002). New York City Community Health Atlas, 2002. United Hospital Fund; Retrieved from http://www.uhfnyc.org/publications/99007 [Google Scholar]
- United States Census 2000 Summary File 3. (2000). Washington, DC: U.S. Census Bureau; Retrieved from http://www.census.gov/census2000/sumfile3.html. [Google Scholar]
- U.S. Census Bureau, 2000 Census of Population and Housing, Public Use Microdata Sample, United States: Technical Documentation, 2003. [Google Scholar]
- Wang EA, White MC, Jamison R, Goldenson J, Estes M, & Tulsky JP (2008). Discharge planning and continuity of health care: Findings from the San Francisco County Jail. American Journal of Public Health, 98, 2182–2184. doi: 10.2105/AJPH.2007.119669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White MC, Tulsky JP, Portillo CJ, Menendez E, Cruz E, & Goldenson J (2001). Tuberculosis prevalence in an urban jail: 1994 and 1998. International Journal of Tuberculosis and Lung Disease, 5, 400–404. [PubMed] [Google Scholar]