Since December 2019, an increasing number of cases of the 2019 novel coronavirus disease (COVID-19) infected by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) have been identified in Wuhan, a large city of 11 million people in central China[1], [2]. By February 19, 2020, the rapid spread of the virus had caused 74,280 cases and 2,009 deaths in China. Most cases were identified in Hubei Province, followed by bordering provinces, such as Guangdong Province, Henan Province, Hunan Province, and Anhui Province. In addition, cases have been reported in 24 other countries and regions, including the USA, Japan, and Spain. Meanwhile, the National Health Commission of the People's Republic of China (NHCPRC) released the latest diagnosis and treatment strategy (Sixth Edition), which defines suspected cases by the following two criteria: patients with epidemic history and two clinical manifestations (fever and/or symptoms of lower respiratory illness with imaging characteristics of pneumonia, normal or decreased white blood cells at early onset, or decreased lymphocyte count); patients with no epidemic history and three clinical manifestations; and confirmed cases (suspected patient with positive etiologic evidence). While fighting the epidemic, hospitals reduced the clinical admissions to most other departments, including oncology departments. As a result, some cancer patients’ benefits were compromised due to delays in treatment plans. Radiation therapy is one of the main treatment modalities for cancer, and more than half of all people with cancer receive radiation therapy as part of their cancer treatment. The staff at most radiation therapy centers have been off of work since January 24, 2020, the beginning of the Chinese Spring Festival. This has led to a prolonged interval of the radiation treatment plans of some cancer patients, which may reduce the biological effects of radiotherapy. To address this dilemma, we need to tailor cancer treatment plans to provide radiotherapy to the patients in greatest need and develop effective protective measures to prevent the spread of COVID-19 during the radiation implementation procedure. Therefore, on February 17, 2020, 24 days after Wuhan lockdown, we investigated the recent situations of radiation therapy centers in Guangdong Province, Hunan Province, Anhui Province, Zhejiang Province and Jiangxi Province, as well as analyzed their responses and suggestions. We propose our preliminary strategies here regarding the tailoring of cancer treatments in this special period.
On February 17, 2020, we used Wenjuanxing (an online questionnaire platform powered by www. wjx.cn) to conduct a survey of the radiotherapy implementation status during the endemic period in 74 hospitals, all of which are located in endemic areas, including Guangdong Province, Anhui Province, Hunan Province, Zhejiang Province and Jiangxi Province. Half of the investigated hospitals were officially designated institutions for COVID-19, 86% of which had confirmed cases. Among unofficially designated hospitals, 29% had confirmed cases. There are 160 linear accelerators in these 74 hospitals (2.16 per hospital), 60 of which were off of work during the Chinese Spring Festival, which started on January 24, 2020. The average off-work period in the 60 hospitals was 5.28 days, meaning patients admitted to these hospitals had to wait for nearly one full work week. By February 17, 72 hospitals had returned to work to provide radiation therapy. Of the other two hospitals, one plans to resume radiotherapy on February 29, while the other had not finalized the specific date.
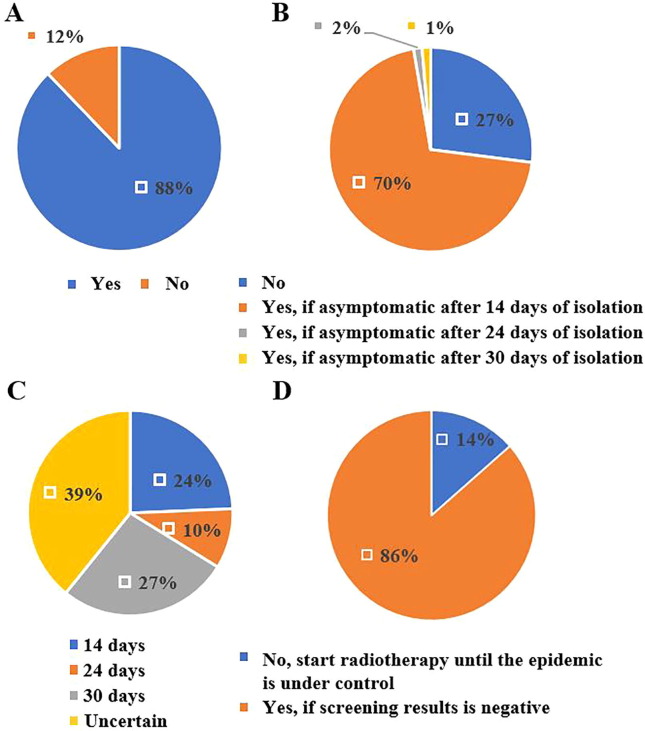
Based on survey results from all hospitals, 88% of them said that they would provide radiation treatment for patients with negative screening results, while others said they would not (Fig. 1 A). Opinions varied with regard to the length of the necessary isolation period before the delivery of radiation therapy to asymptomatic patients with an epidemic travel history. 70% of hospitals believed that asymptomatic patients could be treated after 14 days of isolation, 2% suggested that 24 days were necessary, 1% demanded 30 days, while the other 27% said they would not provide radiation treatment for these patients for the time being (Fig. 1B). For confirmed COVID-19 patients who had been cured, all hospitals showed a more cautious attitude. Up to 39% of hospitals indicated that they would not provide radiation treatment for them, and the proportion of hospitals that believed that they could start radiotherapy after isolation for 14, 24 or 30 days was 24%, 10%, or 27%, respectively (Fig. 1C). For newly diagnosed cancer patients with negative COVID-19 screening results, hospitals had a relatively mild attitude. 86% of the investigated hospitals were willing to provide radiotherapy to this group of patients (Fig. 1D). Our data showed that most hospitals were very cautious about delivering radiotherapy to cancer patients during epidemic outbreaks, which was necessary to curb the spread of the virus. However, the long isolation period of medical observation may compromise the benefits to cancer patients, some of whom would not start timely treatment and others of whom would not experience the optimal biological effects of radiation therapy due to delays in treatment. Further studies are warranted to determine the optimal isolation period so that clinicians can provide timely and continuous treatment for cancer patients without risking the spread of COVID-19.
Fig. 1.
Reports on the COVID-19 screening status of cancer patients receiving radiation therapy during the endemic period. A. Surveys on whether patients with negative screening results could receive radiation therapy. *Negative screening results: no fever or nonproductive cough, no endemic area travel history, negative throat swab nucleic acid test, and no typical viral pneumonia presentation on chest CT. All of the test results mentioned above were met. B. Surveys on whether asymptomatic patients with endemic area travel history could receive radiation therapy. C. Surveys on the necessary interval period of cancer patients who were diagnosed with COVID-19 and cured. D. Surveys on whether newly diagnosed cancer patients could receive radiation therapy during the COVID-19 endemic period.
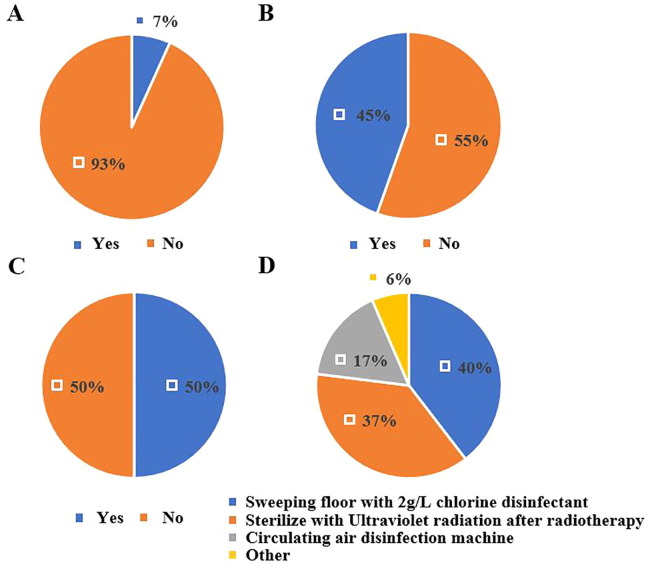
In terms of protective measures, these hospitals had different strategies in the implementation process of radiation therapy. 93% percent of radiotherapy centers have designed exclusive areas for patients receiving radiation treatment (Fig. 2 A). 55% percent of hospitals did not encourage patients to take the stairs instead of using the elevator, which suggested that they should place more emphasis on the disinfection of hospital elevators on a regular basis. Hospitals recommended that patients take the stairs, cleaners sterilize frequently contacted areas, such as staircase handrails, should not be neglected (Fig. 2B). 50% of radiotherapy centers would wipe and disinfect the treatment bed and surrounding accessories during the treatment interval (Fig. 2C), which may reduce the risk of infection but may also require more manpower and time. All hospitals had relatively high awareness of the importance of sterilization of the radiation treatment room (Fig. 2D).
Fig. 2.
Issues concerning protective measures during radiotherapy implementation. A. Surveys on whether it is necessary to design an exclusive path to the treatment room. B. Surveys on whether patients should take the stairs instead of using the elevator. C. Surveys on whether it is necessary to disinfect the treatment room during treatment intervals. D. Surveys on the disinfection methods for the treatment room.
To ensure the safety of cancer patients and medical staff, we formulated a preliminary strategy to manage patients who require radiation treatment during the COVID-19 outbreak. (1) Before the delivery of radiation therapy, we should screen all patients, as recommended by the NHCPRC, and classify them into confirmed cases, suspected cases, cases that require medical isolation, and cases with negative screening results. For patients with negative screening, if they are early-stage cancer patients or if radiation therapy intervention is urgently needed, they can choose the nearest radiotherapy center as appropriate; for patients with locally advanced tumors, we recommend a neoadjuvant chemotherapy regimen at first and an appropriate delay of radiation therapy. For patients who are already receiving radiotherapy, treatment should be continued as appropriate and radiotherapy doses should be adjusted based on biological effects. (2) The radiation treatment room and nearby areas should be thoroughly disinfected during treatment intervals. (3) Reasonable protective measures should be provided to patients and radiotherapy technicians. (4) Patients are encouraged to use online platforms for medical consultation and receive treatment in the nearest hospital to reduce exposure to crowds.
The epidemic has posed major challenges for both oncologists and cancer patients. Because of the influx of COVID-19 patients, most hospitals have had to decrease the number of beds available for other patients, including cancer patients, while this also increases the risk of exposing patients to SARS-CoV-2 infection. Although the epidemic has been controlled gradually via emergent regulations nationwide, it is still necessary to put more thought into such public health emergencies. The epidemic puts cancer patients in an even worse situation. It is important that oncologists discern whether their patients are at risk of COVID-19 exposure, but it is more challenging to balance the relationship between treating tumors and preventing viruses. In this report, we investigated the response of radiotherapy centers in face of epidemic situation, provided scientific and reasonable references for cancer patients with the appropriate plan of radiotherapy without compromising the Interests.
Conflict of interest
We declare no competing interests. We admire the efforts of all medical staff to fight against the COVID-19 crisis during this period. We are also particularly grateful to the radiation oncology professional committee of the Anhui Cancer Association and the Guangzhou Cancer Association for their help in completing the questionnaire.
Author contribution statement
Study design: Z.G.L. and W.J.
Data collection: H.J., W.P.C., S.S.G. and Y.L.Z.
Formal analysis: W.W., W.P.C. and S.S.G.
Investigation: W.W., Y.L.Z., S.S.G. and G.H.Z.
Supervision: H.J., H.L.Z., S.Y.W. and H.Y.Z.
Writing—review and editing: W.P.C., Y.L.Z., W.W., G.H.Z., W.J. and Z.G.L.
Footnotes
The Editors of the Journal, the Publisher and the European Society for Radiotherapy and Oncology (ESTRO) cannot take responsibility for the statements or opinions expressed by the authors of these articles. Practitioners and researchers must always rely on their own experience and knowledge in evaluating and using any information, methods, compounds or experiments described herein. Because of rapid advances in the medical sciences, in particular, independent verification of diagnoses and drug dosages should be made. For more information see the editorial “Radiotherapy & Oncology during the COVID-19 pandemic”, Vol. 146, 2020.
References
- 1.Wu J.T., Leung K., Leung G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020 doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. New Engl J Med. 2020 doi: 10.1016/s0140-6736(20)30260-9). [DOI] [PMC free article] [PubMed] [Google Scholar]