Highlights
-
•
COVID-19 is spreading fast with an increasing number of infected patients worldwide.
-
•
This review summarizes the epidemiology, clinical characteristics, diagnosis, treatment and prevention of COVID-19.
-
•
The specific mechanism of the virus remains unknown, and specific drugs for the virus have not been developed to date.
Keywords: SARS-CoV-2, COVID-19, Coronavirus, Pneumonia, Respiratory infection
Abstract
COVID-19, the disease caused by SARS-CoV-2, is a highly contagious disease. The World Health Organization has declared the ongoing outbreak to be a global public health emergency. Currently, the research on SARS-CoV-2 is in its primary stages. Based on current published evidence, this review systematically summarizes the epidemiology, clinical characteristics, diagnosis, treatment and prevention of COVID-19. It is hoped that this review will help the public to recognize and deal with SARS-CoV-2, and provide a reference for future studies.
1. Background
In late December 2019, a case of unidentified pneumonia was reported in Wuhan, Hubei Province, People's Republic of China (PRC). Its clinical characteristics were very similar to those of viral pneumonia. After analysis of respiratory samples, the experts at the PRC Centers for Disease Control declared that the pneumonia, later known as novel coronavirus pneumonia (NCP), was caused by a novel coronavirus [1]. The World Health Organization (WHO) officially named the disease ‘COVID-19’. The International Committee on Taxonomy of Viruses named the virus ‘severe acute respiratory syndrome coronavirus 2’ (SARS-CoV-2). Designation of a formal name for the novel coronavirus and the disease it caused is conducive to communication in clinical and scientific research. This virus belongs to the β-coronavirus family, a large class of viruses that are prevalent in nature. Similar to other viruses, SARS-CoV-2 has many potential natural hosts, intermediate hosts and final hosts. This poses major challenges for the prevention and treatment of viral infection. Compared with severe acute respiratory syndrome and Middle East respiratory syndrome coronaviruses (SARS-CoV and MERS-CoV, respectively), SARS-CoV-2 has high transmissibility and infectivity, and a low mortality rate [2]. Genome analysis of SARS-CoV-2 sequences revealed that the complete genome sequence recognition rates of SARS-CoV and bat SARS coronavirus (SARSr-CoV-RaTG13) were 79.5% and 96%, respectively [3]. This implies that SARS-CoV-2 might originate from bats. On 29 February 2020, data published by WHO showed that since 12 December 2019 when the first case was reported, there had been 79 394 confirmed cases of SARS-CoV-2 infection and 2838 deaths [4]. In the meantime, 6009 cases had been confirmed and 86 patients had died in 53 countries and regions outside China (Fig. 1 ) [4]. COVID-19 poses a major threat to global public health. This article reviews the genetic structure, source of infection, route of transmission, pathogenesis, clinical characteristics, and treatment and prevention of SARS-CoV-2 in order to help follow-up research, prevention and treatment, and to provide readers with the latest understanding of this new infectious disease.
Fig. 1.
Geographical distribution of 85 403 confirmed cases of COVID-19 novel coronavirus pneumonia. The depth of colour represents the number of confirmed cases of COVID-19 infection.
Source:https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200229-sitrep-40-covid-19 (data as reported at 10AM CET on 29 February 2020).
2. Genetic structure and pathogenic mechanism of SARS-CoV-2
Coronaviruses are single-stranded RNA viruses with a diameter of 80–120 nm. There are four types: α-coronavirus, β-coronavirus, δ-coronavirus and γ- coronavirus [5]. Prior to SARS-CoV-2, six coronaviruses were known to cause disease in humans, including SARS-CoV and MERS-CoV [6]. SARS-CoV-2, like SARS-CoV and MERS-CoV, is a β-coronavirus. The genome sequence homology of SARS-CoV-2 and SARS is approximately 79%; SARS-CoV-2 is closer to the SARS-like bat coronaviruses (MG772933) than SARS-CoV [7], which descended from SARS-like bat coronaviruses. Interestingly, several analyses have shown that SARS-CoV-2 uses angiotension-converting enzyme 2 (ACE2) as its receptor, in common with SARS-CoV [8]. Coronaviruses mainly recognize their corresponding receptors on target cells through S proteins on their surface; entry to the cells results in infection. A structure model analysis shows that SARS-CoV-2 binds to ACE2 with more than 10-fold higher affinity than SARS-CoV, at a level above the threshold required for virus infection [9]. The detailed mechanism by which SARS-CoV-2 infects humans via binding of S-protein to ACE2, the strength of the interaction for risk of human transmission, and how SARS-CoV-2 causes organ damage remain unknown, and more studies are needed. These results explain the faster transmission capability of SARS-CoV-2 in humans compared with SARS-CoV, and the higher number of confirmed cases of COVID-19 compared with SARS-CoV infection. Considering the higher affinity of SARS-CoV-2 binding to ACE2, soluble ACE2 may be a potential candidate for the treatment of COVID-19.
3. Prevalence of SARS-CoV-2
The basic reproduction number (R0) represents the average number of secondary infections that patients may cause in a completely susceptible population without intervention [10]. Estimation of R0 varies between research teams and is updated as more information becomes available. Using the SEIR model, Wu et al. estimated the R0 of SARS-CoV-2 to be 2.47–2.86 [11]. Majumder et al. used the IDEA model and reported R0 of 2.0–3.3 [12]. The estimated R0 values of other β-coronaviruses, such as SARS-CoV, are 2.2–3.6 [13]. The estimated R0 value of MERS-CoV is 2.0–6.7 [14]. These results indicate that SARS-CoV-2 has relatively high transmissibility. Large studies from China reported that the median age of cases was 47 years (interquartile range 35–58 years), 87% of cases were aged 30–79 years and 3% were aged ≥80 years, and the number of female patients was 41.9% [15,16]. Most cases were diagnosed in Hubei Province, China (75%). Eighty-one percent of cases were classified as mild, 14% were classified as severe and 5% were classified as critical. The overall case-fatality rate (CFR) was 2.3%; however, among cases aged 70–79 years and ≥80 years, the CFR was 8.0% and 14.8%, respectively [16]. This indicates that elderly males are more susceptible to SARS-CoV-2 compared with other groups, and this virus is more likely to affect elderly males with chronic underlying diseases (e.g. diabetes, hypertension, heart disease, etc.) [17]. In summary, the prevalence of COVID-19 is high, the population is generally susceptible to SARS-CoV-2, and COVID-19 spread rapidly from a single city (Wuhan) to the entire country in just 30 days. Prompt measures are clearly needed to control the spread of the disease.
4. Transmission of SARS-CoV-2
Previous epidemiological studies have shown that there are three factors involved in viral spreading: source of infection, route of transmission and susceptibility [18]. This is the case for SARS-CoV-2.
4.1. Source of infection
Bats are considered to be the natural hosts of SARS-CoV-2, and pangolins and snakes are thought to be intermediate hosts. A study from Peking University suggested that SARS-CoV-2 infection is probably caused by snakes [19], but a later study found no evidence that snakes are the hosts of SARS-CoV-2 [20]. A study from Wuhan Institute of Virology showed 96.2% similarity in the gene sequence between SARS-CoV-2 and bat coronavirus using sequencing technology [21]. This implied that bats are the potential source of SARS-CoV-2. Using macrogenomic sequencing, molecular biological detection and electron microscopic analysis, Xu et al. [22] showed 99% similarity between SARS-CoV-2 isolated from pangolins and the virus strains currently infecting humans. This group also observed SARS-CoV-2 granules and revealed that pangolins are the potential intermediate host of SARS-CoV-2. Although no studies to date have fully elucidated the potential natural host and intermediate host of SARS-CoV-2, adequate evidence shows that this virus might be sourced from wild animals. At present, it is considered that the main source of infection of SARS-CoV-2 is patients with COVID-19. However, debate remains regarding whether these patients are infectious during the incubation period.
4.2. Route of transmission
Droplets and close contact are the most common routes of transmission of SARS-CoV-2, and aerosol transmission may be another route. In addition, researchers have detected SARS-CoV-2 in samples of stool, gastrointestinal tract, saliva and urine. Based on bioinformatics, evidence has indicated that the digestive tract may be a route of SARS-CoV-2 infection [23]. SARS-CoV-2 RNA has been detected consistently in gastrointestinal tissue from patients with COVID-19 [24]. Moreover, SARS-CoV-2 was detected in the tears and conjunctival secretions of patients with COVID-19 [25]. A retrospective study of nine pregnant women with COVID-19 indicated that the possibility of intrauterine vertical transmission between mothers and infants during late pregnancy was temporarily excluded [26]. However, available data on pregnant women infected with SARS-CoV-2 are inadequate; further studies are required to verify the possibility of vertical transmission of SARS-CoV-2 in pregnant women.
4.3. Susceptible population and viral latenc
An epidemiological investigation report reported that elderly people are most susceptible to SARS-CoV-2 (median age at death 75 years), and most of the patients who died had comorbidities or a history of surgery before admission [27]. Zhong et al. found that, based on the clinical features of 1099 patients with COVID-19, the median incubation period was 3 days (range 0–24 days), and the median time from symptom onset to death was 14 days [15,27]. For SARS-CoV infection, the median latency was 4 days, the average interval from symptom onset to hospital admission was 3.8 days, and the average interval from hospital admission to death was 17.4 days [28]. The median latency of MERS-CoV infection was 7 days [29]. The median incubation period for COVID-19 is shorter than that for SARS and MERS. However, the maximum latency of SARS-CoV-2 currently observed is as high as 24 days, which may increase the risk of virus transmission. Moreover, people aged ≥70 years had a shorter median interval (11.5 days) from symptom onset to death compared with patients aged <70 years (20 days), demonstrating that disease progression is more rapid in elderly people compared with younger people [27]. As such, our focus should be on elderly people who might be more vulnerable to SARS-CoV-2.
5. Clinical characteristics of SARS-CoV-2 infection
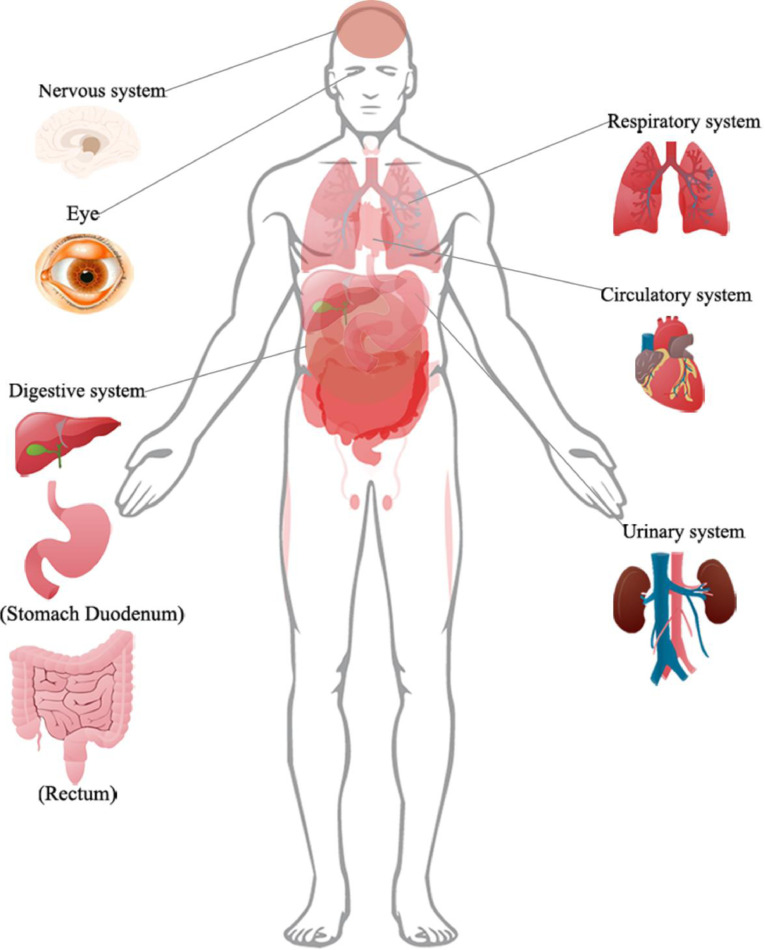
SARS-CoV-2 produces an acute viral infection in humans with a median incubation period of 3 days [15]; this is similar to SARS-CoV with an incubation period of 2–10 days [30]. The presenting features of COVID-19 in adults are pronounced. The most common symptoms of COVID-19 are fever (87.9%), cough (67.7%) and fatigue (38.1%); diarrhoea (3.7%) and vomiting (5.0%) are rare [15,31], similar to other coronavirus infections. Most patients had some degree of dyspnoea at presentation; the interval from symptom onset to the development of acute respiratory distress syndrome was only 9 days among the initial cases [1]. Moreover, severe cases are prone to a variety of complications, including acute respiratory distress syndrome, acute heart injury and secondary infection [17]. There is already some evidence that COVID-19 can cause damage to tissues and organs other than the lungs. In a study of 214 patients with COVID-19, 78 (36.4%) patients had neurological manifestations [32]. In addition, there is evidence of ocular surface infection in patients with COVID-19, and SARS-CoV-2 RNA was detected in eye secretions of patients [33]. Some patients with COVID-19 have had arrhythmia, acute heart injury, impaired renal function and abnormal liver function (50.7%) at admission [1,34,35]. A case report of the pathological manifestations of a patient with pneumonia showed moderate microvesicular steatosis in liver tissue [36]. Tissue samples of stomach, duodenum and rectal mucosa have tested positive for SARS-CoV-2 RNA [37] (Fig. 2 ).
Fig. 2.
Organ involvement confirmed by clinical features or biopsy in patients with COVID-19.
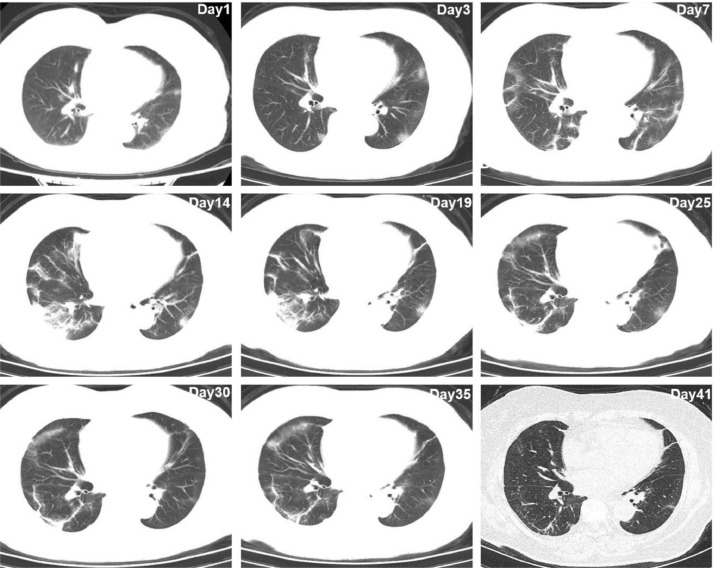
In general, the radiographic features of coronaviruses are similar to those found in community-acquired pneumonia caused by other organisms [38]. Chest computed tomography (CT) scan is an important tool to diagnose this pneumonia. Several typical imaging features are frequently observed in COVID-19 pneumonia, including predominant ground-glass opacity (65%), consolidations (50%), smooth or irregular interlobular septal thickening (35%), air bronchogram (47%), and thickening of the adjacent pleura (32%), with predominantly peripheral and lower lobe involvement [39] (Fig. 3 ). A recent study reported that most patients (90%) had bilateral chest CT findings, and the sensitivity of chest CT to suggest COVID-19 was 97% [33]. Combining chest CT imaging features with clinical symptom and laboratory tests could facilitate early diagnosis of COVID-19 pneumonia.
Fig. 3.
Serial chest computer tomography scan of a 64-year-old female infected with SARS-CoV-2 in 2020. Several areas of ground-glass opacities, consolidations, air bronchogram and intralobular interstitial thickening, with prominent involvement of the lower lobes of both lungs, were observed.
Laboratory examination revealed that 82.1% of patients were lymphopenic and 36.2% of patients were thrombocytopenic. Most patients had normal leukocytes, but leukopenia was observed in 33.7% of patients. In addition, most patients demonstrated elevated levels of C-reactive protein, lactate dehydrogenase and creatinine kinase, but a minority of patients had elevated transaminase, abnormal myocardial enzyme spectrum or elevated serum creatinine [1,15]. In comparison with bacterial pneumonia, patients with COVID-19 had a lower oxygenation index. Cytokine release syndrome is a vital factor that aggravates disease progression. Higher levels of interleukin (IL)-6 and IL-10, and lower levels of CD4+T and CD8+T have been observed in patients with COVID-19, correlated with the severity of disease [40].
6. Diagnosis of SARS-CoV-2
The detection of viral nucleic acid is the standard for non-invasive diagnosis of COVID-19. However, the detection of SARS-CoV-2 nucleic acid has high specificity and low sensitivity, so there may be false-negative results and the testing time could be relatively long. The Novel Coronavirus Pneumonia Diagnosis and Treatment Plan (5th trial version) took ‘suspected cases with pneumonia imaging features’ as the clinical diagnostic criteria in Hubei Province [41]. The Novel Coronavirus Pneumonia Diagnosis and Treatment Plan (6th trial version) eliminated the distinction between Hubei Province and other provinces [42]. The likely reason is that the number of people infected with COVID-19 outside Hubei province is increasing as population mobility increases. Furthermore, Zhang developed a test for rapid detection (1 h) of SARS-CoV-2 using SHERLOCK technology. Although clinical verification has not been undertaken to date, this technology, once proved, may be conducive to rapid diagnosis of the disease [43]. A research group at Peking University claimed to have developed a new method for rapid construction of the transcriptome sequencing library of SHERRY, which is helpful for rapid sequencing of SARS-CoV-2 [44].
7. Treatment of SARS-CoV-2
7.1. Antiviral Western medical treatment
At present, the treatment of patients with COVID-19 is mainly symptomatic. Remdesivir has been reported as a promising antiviral drug against a wide array of RNA viruses. Holshue et al. reported that treatment of a patient with COVID-19 with remdesivir achieved good results [45]. Xiao et al. found that remdesivir was effective in the control of COVID-19 in vitro. Meanwhile, chloroquine has been found to have immunomodulatory activity and could effectively inhibit SARS-CoV-2 in vitro [46]. Clinical controlled trials have shown that chloroquine was effective in the treatment of patients with COVID-19 [47]. Remdesivir is undergoing a large number of clinical trials in several hospitals; the efficacy of the drug is uncertain at present. Arbidol, a small indole derivative molecule, was found to block viral fusion of influenza A and B viruses and hepatitis C viruses [48], and to have an antiviral effect on SARS-CoV in cell experiments [49]; as such, it may be a possibility for treatment of patients with COVID-19. A randomized controlled study on the treatment of COVID-19 with Arbidol and Kaletra showed that Arbidol had a better therapeutic effect than Kaletra and could significantly reduce the incidence of severe cases. In addition, lopinavir/ritonavir, nucleoside analogues, neuraminidase inhibitors, remdesivir and peptide EK1 could also be possibilities for the treatment of COVID-19 [50].
7.2. Chinese medical treatment
Chinese medicine has also played an important role in the treatment of COVID-19. Local governments and medical institutions have published a number of traditional Chinese medicine prescriptions. The Novel Coronavirus Pneumonia Diagnosis and Treatment Plan (6th trial version) suggested the use of a lung clearing and detoxification decoction [42]. A joint study by the Shanghai Institute of Materia Medica and Wuhan Institute of Virology, Chinese Academy of Sciences found that Shuanghuanglian oral liquid could inhibit SARS-CoV-2. Previous studies have shown that baicalin, chlorogenic acid and forsythin in Shuanghuanglian oral liquid have certain inhibitory effects on various viruses and bacteria [51,52]. The mechanism might be that these components play a therapeutic role by effectively reducing the inflammatory response of the body caused by viruses and bacteria [53]. Lianhuaqingwen capsule has been shown to have a wide-spectrum effect on a series of influenza viruses, including H7N9, and could regulate the immune response of the virus, reducing the level of inflammatory factors in the early stage of infection [54].
7.3. Immunoenhancement therapy
One of the pathogenesis of SARS-CoV is caused by a disproportionate immune response. Boosting the body's immunity is a potential candidate protocol for treating SARS patients. Interferons can inhibit viral infection by inducing both innate and adaptive immune response. Synthetic recombinant interferon α has been shown to be effective for the treatment of patients with SARS in clinical trials, the interferon alfacon-1 plus corticosteroids treatment had a shorter time to 50% resolution of lung radiographic abnormalities compared with corticosteroids treatment alone and was associated with reduced disease-associated impaired oxygen saturation [55]. Interferon was also found to be an effective inhibitor of MERS-CoV replication [56]. These findings suggest that interferon could be used in the treatment of COVID-19. Intravenous immunoglobulin might be the safest immunomodulator for long-term use in all age groups, and could help to inhibit the production of pro-inflammatory cytokines and increase the production of anti-inflammatory mediators [57]. Moreover, thymosin alpha-1 (Ta1) can be an immune booster for patients with SARS, effectively controlling the spread of disease [58]. Intravenous immunoglobulin and Ta1 may also be considered for treatment of COVID-19.
7.4. Convalescent plasma therapy
When there are no sufficient vaccines or specific drugs, convalescent plasma therapy could be an effective way to alleviate the course of disease for severely infected patients [59]. In a retrospective analysis, convalescent plasma therapy is more effective than severe doses of hormonal shock in patients with severe SARS, reducing mortality and shortening hospital stays [60]. A prospective cohort study by Hung et al. showed that for patients with pandemic H1N1 influenza virus infection in 2009, the relative risk of death was significantly lower in patients treated with convalescent plasma [61]. Moreover, from the perspective of immunology, most patients who recover from COVID-19 will produce specific antibodies against the SARS-CoV-2, and their serum could be used to prevent re-infection. At the same time, antibodies can limit viral reproduction in the acute phase of infection and help clear the virus, which is conducive to rapid recovery from the disease [62]. Theoretically, viraemia peaks during the first week of most viral infections, and it should be more effective to give convalescent plasma early in the disease course [63]. Therefore, the plasma of patients who have recovered from COVID-19 could be collected to prepare plasma globulin specific to SARS-CoV-2. However, the safety of plasma globulin products specific to SARS-CoV-2 deserves further consideration.
7.5. Auxiliary blood purification treatment
At present, extracorporeal blood purification technology is used in the treatment of patients with severe NCP [42]. According to the latest study, ACE2, the key receptor of SARS-CoV-2, is highly expressed in human kidney (nearly 100 times higher than in lung). Kidney might be the main target of attack for SARS-CoV-2. Early continuous blood purification treatment could reduce renal workload and help to promote the recovery of renal function [64]. The most severe cases of COVID-19 may suffer from a cytokine storm. The imbalance of pro-inflammatory factors and anti-inflammatory factors may cause immune damage. Therefore, blood purification technology could be used to remove inflammatory factors, eliminate cytokine storms, correct electrolyte imbalances and maintain acid–base balance to control patients’ capacity load in an effective manner [65]. In this way, patient symptoms could be improved and blood oxygen saturation could be increased.
In summary, there are four possibilities for drug treatment of COVID-19: antiviral Western medicine, Chinese medicine, immunoenhancement therapy and viral-specific plasma globulin. Machines could be used as auxiliary therapy. However, randomized double-blinded clinical trials with large sample sizes should be used as the standard to determine whether antiviral drugs could be used in clinical practice.
8. Prevention of COVID-19
To date, there are no specific antiviral treatments or vaccines for SARS-CoV-2, and the clinical treatment of COVID-19 has been limited to support and palliative care until now. Therefore, there is an urgent need to develop a safe and stable COVID-19 vaccine. Dr. Tedros, Director-General of WHO, said that it was expected that a vaccine for SARS-CoV-2 would be available in 18 months. SARS-CoV-2 is an RNA virus, so RNA-virus-related vaccines, including measles, polio, encephalitis B virus and influenza virus, could be the most promising alternatives. Interpersonal transmission of the virus could be prevented by immunizing healthcare workers and the non-infected population [66].
Prevention of infectious diseases by traditional Chinese medicine has been recorded for a long time in Chinese history, and a study has been published on the prevention of SARS by traditional Chinese medicine [67]. The present principles on prevention of COVID-19 are to tonify body energy to protect the outside body, dispel wind, dissipate heat and dissipate dampness with an aromatic agent. The six most commonly used Chinese herbal medicines are astragalus, liquorice, fangfeng, baizhu and honeysuckle. However, the decoction is not suitable for long-term use; the best period of use is 1 week [68]. Studies have shown that vitamin C may prevent the susceptibility of lower respiratory tract infection under certain conditions [69], while COVID-19 may cause lower respiratory tract infection. Therefore, a moderate amount of vitamin C supplementation may be a way to prevent COVID-19. In addition, a decrease in vitamin D and vitamin E levels in cattle could lead to bovine coronavirus infection [70]. This suggests that proper supplementation of vitamin D and vitamin E may enhance resistance to SARS-CoV-2. Patients with primary basic diseases, especially those with chronic diseases such as hypertension, diabetes, coronary heart disease and cancer, are more susceptible to SARS-CoV-2, and their risk of a poor prognosis will increase significantly after infection because they will have low systemic immunity as a result of the disease itself and treatment [71]. Therefore, it is particularly important to enhance self-resistance. The main way to boost personal immunity is to maintain personal hygiene, a healthy lifestyle and adequate nutritional intake [72,73]. For individuals, taking protective measures can effectively prevent SARS-CoV-2 infection, including improving personal hygiene, wearing medical masks, adequate rest and good ventilation [15].
In conclusion, COVID-19 is a serious infectious disease caused by the novel coronavirus, SARS-CoV-2. Its main initial symptoms – fever, cough and fatigue – are similar to those of SARS. The most likely source of SARS-CoV-2 is bats. This virus is highly infectious and can be transmitted through droplets and close contact. Some cases are life-threatening; as such, COVID-19 poses a great threat to global health and safety. Controlling the spread of the epidemic and reducing mortality as soon as possible is the burning issue. The specific mechanism of the virus remains unknown, and no specific antiviral drugs have been developed. At present, it is important to control the source of infection, cut off the route of transmission, and use existing drugs and means to control progress of the disease proactively. We should also strive to develop specific drugs, promote the research and development of vaccines, and reduce morbidity and mortality of COVID-19 in order to protect the safety of the population.
Acknowledgments
Declarations
Funding: This study was supported by a grant from the National Natural Science Foundation of PRC (No. 81800609).
Competing Interests: None declared.
Ethical approval: Not required.
Editor: Jean-Marc Rolain
References
- 1.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu Y., Gayle A.A., Wilder-Smith A., Rocklov J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J Travel Med. 2020;27(2):taaa021. doi: 10.1093/jtm/taaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization . WHO; Geneva: 2020. Coronavirus disease 2019 (COVID-19) Situation Report 40. [PubMed] [Google Scholar]
- 5.Chan J.F., To K.K., Tse H., Jin D.Y., Yuen K.Y. Interspecies transmission and emergence of novel viruses: lessons from bats and birds. Trends Microbiol. 2013;21:544–555. doi: 10.1016/j.tim.2013.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu A., Peng Y., Huang B., Ding X., Wang X., Niu P. Genome composition and divergence of the novel coronavirus (2019-nCoV) originating in China. Cell Host Microbe. 2020;27(3):325–328. doi: 10.1016/j.chom.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoffmann M., Kleine-Weber H., Krüger N., Müller M., Drosten C., Pöhlmann S. The novel coronavirus 2019 (2019-nCoV) uses the SARS-coronavirus receptor ACE2 and the cellular protease TMPRSS2 for entry into target cells. bioRxiv. 2020 2020.01.31.929042. [Google Scholar]
- 9.Wrapp D., Wang N., Corbett K.S., Goldsmith J.A., Hsieh C.L., Abiona O. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science (New York, NY) 2020;367(6483):1260–1263. doi: 10.1126/science.abb2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Remais J. Modelling environmentally-mediated infectious diseases of humans: transmission dynamics of schistosomiasis in China. Adv Exp Med Biol. 2010;673:79–98. doi: 10.1007/978-1-4419-6064-1_6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu J.T., Leung K., Leung G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395(10225):689–697. doi: 10.1016/S0140-6736(20)30260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Majumder M.A.M., Kenneth D. Early transmissibility assessment of a novel coronavirus in Wuhan, China. SSRN. 2020 doi: 10.2139/ssrn.3524675. [DOI] [Google Scholar]
- 13.Lipsitch M., Cohen T., Cooper B., Robins J.M., Ma S., James L. Transmission dynamics and control of severe acute respiratory syndrome. Science (New York, NY) 2003;300:1966–1970. doi: 10.1126/science.1086616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Majumder M.S., Rivers C., Lofgren E., Fisman D. Estimation of MERS-coronavirus reproductive number and case fatality rate for the Spring 2014 Saudi Arabia outbreak: insights from publicly available data. PLoS Curr. 2014;6 doi: 10.1371/currents.outbreaks.98d2f8f3382d84f390736cd5f5fe133c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guan W-J, Ni Z-Y, Hu Y, Liang W-H, Ou C-Q, He J-X. Clinical characteristics of 2019 novel coronavirus infection in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [Google Scholar]
- 16.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 17.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barreto M.L., Teixeira M.G., Carmo E.H. Infectious diseases epidemiology. J Epidemiol Community Health. 2006;60:192–195. doi: 10.1136/jech.2003.011593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ji W., Wang W., Zhao X., Zai J., Li X. Homologous recombination within the spike glycoprotein of the newly identified coronavirus may boost cross-species transmission from snake to human. J Med Virol. 2020;92 doi: 10.1002/jmv.25682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang C., Zheng W., Huang X., Bell E.W., Zhou X. Zhang Y.Protein structure and sequence re-analysis of 2019-nCoV genome does not indicate snakes as its intermediate host or the unique similarity between its spike protein insertions and HIV-1. J Proteome Res. 2020;19(4):1351–1360. doi: 10.1021/acs.jproteome.0c00129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xu X., Chen P., Wang J., Feng J., Zhou H., Li X. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci China Life Sci. 2020;63(3):457–460. doi: 10.1007/s11427-020-1637-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang J., Zhao S., Liu M., Zhao Z., Xu Y., Wang P. ACE2 expression by colonic epithelial cells is associated with viral infection, immunity and energy metabolism. medRxiv. 2020;2020 2020.02.05.20020545. [Google Scholar]
- 24.Xiao F., Tang M., Zheng X., Li C., He J., Hong Z. Evidence for gastrointestinal infection of SARS-CoV-2. medRxiv. 2020 doi: 10.1053/j.gastro.2020.02.055. 2020.02.17.20023721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xia J., Tong J., Liu M., Shen Y., Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. 2020 doi: 10.1002/jmv.25725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen H., Guo J., Wang C., Luo F., Yu X., Zhang W. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395(10226):809–815. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang W., Tang J., Wei F. Updated understanding of the outbreak of 2019 novel coronavirus (2019-nCoV) in Wuhan, China. J Med Virol. 2020;92:441–447. doi: 10.1002/jmv.25689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lessler J., Reich N.G., Brookmeyer R., Perl T.M., Nelson K.E., Cummings D.A. Incubation periods of acute respiratory viral infections: a systematic review. Lancet Infect Dis. 2009;9:291–300. doi: 10.1016/S1473-3099(09)70069-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cho S.Y., Kang J.M., Ha Y.E., Park G.E., Lee J.Y., Ko J.H. MERS-CoV outbreak following a single patient exposure in an emergency room in South Korea: an epidemiological outbreak study. Lancet. 2016;388:994–1001. doi: 10.1016/S0140-6736(16)30623-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chan P.K., Tang J.W., Hui D.S. SARS: clinical presentation, transmission, pathogenesis and treatment options. Clin Sci. 2006;110:193–204. doi: 10.1042/CS20050188. [DOI] [PubMed] [Google Scholar]
- 31.Yang Y., Lu Q., Liu M., Wang Y., Zhang A., Jalali N. Epidemiological and clinical features of the 2019 novel coronavirus outbreak in China. medRxiv. 2020;2020 2020.02.10.20021675. [Google Scholar]
- 32.Mao L., Wang M., Chen S., He Q., Chang J., Hong C. Neurological manifestations of hospitalized patients with COVID-19 in Wuhan: China: a retrospective case series study. medRxiv. 2020 2020.02.22.20026500. [Google Scholar]
- 33.Ai T., Yang Z., Hou H., Zhan C., Chen C., Lv W. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020 doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li Z., Wu M., Guo J., Yao J., Liao X., Song S. Caution on kidney dysfunctions of 2019-nCoV patients. medRxiv. 2020;2020 2020.02.08.20021212. [Google Scholar]
- 35.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xiao F., Tang M., Zheng X., Li C., He J., Hong Z., et al. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology doi: 10.1053/j.gastro.2020.02.055. [DOI] [PMC free article] [PubMed]
- 38.Wong K.T., Antonio G.E., Hui D.S., Lee N., Yuen E.H., Wu A. Severe acute respiratory syndrome: radiographic appearances and pattern of progression in 138 patients. Radiology. 2003;228:401–406. doi: 10.1148/radiol.2282030593. [DOI] [PubMed] [Google Scholar]
- 39.Shi H., Han X., Jiang N., Cao Y., Alwalid O., Gu J. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wan S., Yi Q., Fan S., Lv J., Zhang X., Guo L. Characteristics of lymphocyte subsets and cytokines in peripheral blood of 123 hospitalized patients with 2019 novel coronavirus pneumonia (NCP) medRxiv. 2020 2020.02.10.20021832. [Google Scholar]
- 41.China National health commission. The novel coronavirus pneumonia diagnosis and treatment plan (5th trial version). 2020.
- 42.China National health commission. The novel coronavirus pneumonia diagnosis and treatment plan (6th trial version). 2020.
- 43.Zhang F., OmarAbudayyeh O., Gootenberg J.S. https://www.broadinstitute.org/files/publications/special/COVID-19%20detection%20(updated).pdf
- 44.Di L., Fu Y., Sun Y., Li J., Liu L., Yao J. RNA sequencing by direct tagmentation of RNA/DNA hybrids. Proc Natl Acad Sci USA. 2020;117:2886–2893. doi: 10.1073/pnas.1919800117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Holshue M.L., DeBolt C., Lindquist S., Lofy K.H., Wiesman J., Bruce H. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang M., Cao R., Zhang L., Yang X., Liu J., Xu M. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30(3):269–271. doi: 10.1038/s41422-020-0282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gao J., Tian Z., Yang X. Breakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. Biosci Trends. 2020;14(1):72–73. doi: 10.5582/bst.2020.01047. [DOI] [PubMed] [Google Scholar]
- 48.Boriskin Y.S., Leneva I.A., Pecheur E.I., Polyak S.J. Arbidol: a broad-spectrum antiviral compound that blocks viral fusion. Curr Med Chem. 2008;15:997–1005. doi: 10.2174/092986708784049658. [DOI] [PubMed] [Google Scholar]
- 49.Khamitov R.A., Loginova S., Shchukina V.N., Borisevich S.V., Maksimov V.A., Shuster A.M. [Antiviral activity of arbidol and its derivatives against the pathogen of severe acute respiratory syndrome in the cell cultures] Vopr Virusol. 2008;53:9–13. [PubMed] [Google Scholar]
- 50.Lu H. Drug treatment options for the 2019-new coronavirus (2019-nCoV) Biosci Trends. 2020;14(1):69–71. doi: 10.5582/bst.2020.01020. [DOI] [PubMed] [Google Scholar]
- 51.Li W. [The curative effect observation of shuanghuanglian and penicillin on acute tonsillitis] Lin Chuang Er Bi Yan Hou Ke Za Zhi. 2002;16:475–476. [PubMed] [Google Scholar]
- 52.Lu H.T., Yang J.C., Yuan Z.C., Sheng W.H., Yan W.H. [Effect of combined treatment of Shuanghuanglian and recombinant interferon alpha 2a on coxsackievirus B3 replication in vitro] Zhongguo Zhong Yao Za Zhi. 2000;25:682–684. [PubMed] [Google Scholar]
- 53.Chen X., Howard O.M., Yang X., Wang L., Oppenheim J.J., Krakauer T. Effects of Shuanghuanglian and Qingkailing, two multi-components of traditional Chinese medicinal preparations, on human leukocyte function. Life Sci. 2002;70:2897–2913. doi: 10.1016/s0024-3205(02)01541-2. [DOI] [PubMed] [Google Scholar]
- 54.Ding Y., Zeng L., Li R., Chen Q., Zhou B., Chen Q. The Chinese prescription lianhuaqingwen capsule exerts anti-influenza activity through the inhibition of viral propagation and impacts immune function. BMC Complement Altern Med. 2017;17:130. doi: 10.1186/s12906-017-1585-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Loutfy M.R., Blatt L.M., Siminovitch K.A., Ward S., Wolff B., Lho H. Interferon alfacon-1 plus corticosteroids in severe acute respiratory syndrome: a preliminary study. JAMA. 2003;290:3222–3228. doi: 10.1001/jama.290.24.3222. [DOI] [PubMed] [Google Scholar]
- 56.Mustafa S., Balkhy H., Gabere M.N. Current treatment options and the role of peptides as potential therapeutic components for Middle East respiratory syndrome (MERS): a review. J Infect Public Health. 2018;11:9–17. doi: 10.1016/j.jiph.2017.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gilardin L., Bayry J., Kaveri S.V. Intravenous immunoglobulin as clinical immune-modulating therapy. CMAJ. 2015;187:257–264. doi: 10.1503/cmaj.130375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kumar V., Jung Y.S., Liang P.H. Anti-SARS coronavirus agents: a patent review (2008– present) Expert Opin Ther Pat. 2013;23:1337–1348. doi: 10.1517/13543776.2013.823159. [DOI] [PubMed] [Google Scholar]
- 59.Mair-Jenkins J., Saavedra-Campos M., Baillie J.K., Cleary P., Khaw F.M., Lim W.S. The effectiveness of convalescent plasma and hyperimmune immunoglobulin for the treatment of severe acute respiratory infections of viral etiology: a systematic review and exploratory meta-analysis. J Infect Dis. 2015;211:80–90. doi: 10.1093/infdis/jiu396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Soo Y.O., Cheng Y., Wong R., Hui D.S., Lee C.K., Tsang K.K. Retrospective comparison of convalescent plasma with continuing high-dose methylprednisolone treatment in SARS patients. Clin Microbiol Infect. 2004;10:676–678. doi: 10.1111/j.1469-0691.2004.00956.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hung I.F., To K.K., Lee C.K., Lee K.L., Chan K., Yan W.W. Convalescent plasma treatment reduced mortality in patients with severe pandemic influenza A (H1N1) 2009 virus infection. Clin Infect Dis. 2011;52:447–456. doi: 10.1093/cid/ciq106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Baron S., editor. Medical microbiology. 4th edition. University of Texas Medical Branch; Galveston, TX: 1996. [PubMed] [Google Scholar]
- 63.Cheng Y., Wong R., Soo Y.O., Wong W.S., Lee C.K., Ng M.H. Use of convalescent plasma therapy in SARS patients in Hong Kong. Eur J Clin Microbiol Infect Dis. 2005;24:44–46. doi: 10.1007/s10096-004-1271-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zarbock A., Kellum J.A., Schmidt C., Van Aken H., Wempe C., Pavenstadt H. Effect of early vs delayed initiation of renal replacement therapy on mortality in critically ill patients with acute kidney injury: the ELAIN randomized clinical trial. JAMA. 2016;315:2190–2199. doi: 10.1001/jama.2016.5828. [DOI] [PubMed] [Google Scholar]
- 65.Lim C.C., Tan C.S., Kaushik M., Tan H.K. Initiating acute dialysis at earlier Acute Kidney Injury Network stage in critically ill patients without traditional indications does not improve outcome: a prospective cohort study. Nephrology. 2015;20:148–154. doi: 10.1111/nep.12364. [DOI] [PubMed] [Google Scholar]
- 66.Zhang L., Liu Y. Potential interventions for novel coronavirus in China: a systematic review. J Med Virol. 2020;92(5):479–490. doi: 10.1002/jmv.25707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lau J.T., Leung P.C., Wong E.L., Fong C., Cheng K.F., Zhang S.C. The use of an herbal formula by hospital care workers during the severe acute respiratory syndrome epidemic in Hong Kong to prevent severe acute respiratory syndrome transmission, relieve influenza-related symptoms, and improve quality of life: a prospective cohort study. J Altern Complement Med. 2005;11:49–55. doi: 10.1089/acm.2005.11.49. [DOI] [PubMed] [Google Scholar]
- 68.Luo H., Tang Q.L., Shang Y.X., Liang S.B., Yang M., Robinson N. Can Chinese medicine be used for prevention of corona virus disease 2019 (COVID-19)? A review of historical classics, research evidence and current prevention programs. Chin J Integr Med. 2020;26(4):243–250. doi: 10.1007/s11655-020-3192-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hemila H. Vitamin C intake and susceptibility to pneumonia. Pediatr Infect Dis J. 1997;16:836–837. doi: 10.1097/00006454-199709000-00003. [DOI] [PubMed] [Google Scholar]
- 70.Nonnecke B.J., McGill J.L., Ridpath J.F., Sacco R.E., Lippolis J.D., Reinhardt T.A. Acute phase response elicited by experimental bovine diarrhea virus (BVDV) infection is associated with decreased vitamin D and E status of vitamin-replete preruminant calves. J Dairy Sci. 2014;97:5566–5579. doi: 10.3168/jds.2014-8293. [DOI] [PubMed] [Google Scholar]
- 71.Liang W., Guan W., Chen R., Wang W., Li J., Xu K. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.High K.P. Nutritional strategies to boost immunity and prevent infection in elderly individuals. Clin Infect Dis. 2001;33:1892–1900. doi: 10.1086/324509. [DOI] [PubMed] [Google Scholar]
- 73.Simpson R.J., Kunz H., Agha N., Graff R. Exercise and the regulation of immune functions. Prog Mol Biol Transl Sci. 2015;135:355–380. doi: 10.1016/bs.pmbts.2015.08.001. [DOI] [PubMed] [Google Scholar]