Abstract
Background:
Teach Back is a health communication strategy used to confirm patient understanding in a non-shaming way. Although Teach Back is widely recommended as a best practice strategy for improving patient outcomes and organizational health literacy, there is lack of consensus in the literature on the definition of Teach Back and the best methods for training health care workers (HCWs). Our experience suggests that if you teach specific, observable skills, these can be identified in practice and potentially measured in research.
Brief description of activity:
We created a training program, the 5Ts for Teach Back, based on a standardized operational definition of Teach Back and five specific, observable components. Participants use a Teach-Back Observation Tool to identify the 5Ts in practice and during peer evaluation. The program incorporates lecture, observation, practice, and videos with good and bad examples of Teach Back.
Implementation:
The training was offered to HCWs in a large academic health care system. Flexible training options ranged from a single 4-hour training to a more comprehensive program that included clinic-specific scenarios, peer coaching, and refresher activities over a 6-month period.
Results:
The 5Ts for Teach Back operationalizes the definition of Teach Back and provides a model for training HCWs in the use of Teach Back. The 5Ts for Teach Back can be used to train any HCW. A single training session does not guarantee proficiency in practice. Through coaching and refresher activities, competence in Teach Back increases.
Lessons learned:
Teaching entire clinical units may increase effectiveness, because Teach Back becomes embedded in the unit culture. The Observation Tool can be used for training, coaching, and evaluation. The standardized method and Observation Tool are potentially useful when evaluating Teach Back during outcomes and patient satisfaction research. [HLRP: Health Literacy Research and Practice. 2020;4(2):94–103.]
Plain Language Summary:
Health care workers may be clearer when giving information to patients if they use Teach Back. Studies do not show what methods are best for training health care workers how to do Teach Back. The 5Ts method breaks Teach Back into five skills that help health care workers do it well. The 5Ts can also confirm use and may be helpful for research.
Teach Back is a health communication strategy used to confirm patient understanding in a non-shaming way. Teach Back is among the most important skills health care workers (HCWs) need for effective communication with patients (Coleman, Hudson, & Pederson, 2017). The goal for this project was to train HCWs in the use of Teach Back, using a standardized operational definition, which transforms Teach Back into a set of skills that are easy to learn, verifiable in practice, and, potentially, measurable in research.
The setting for this project is the University of New Mexico Hospitals (UNMH), an academic medical center in the Southwest, which includes a 550-bed hospital and 29 outpatient primary care and specialty clinics. Built on Pueblo land, UNMH has a longstanding relationship with Native American communities, including a 1952 federal contract that allowed them to use the land on which the main hospital stands. All of the training is done by the two full-time employees of the hospital's Health Literacy Office. Since the program's inception, we have trained more than 1,300 HCWs, including nurses, physicians, nurse practitioners, physician assistants, appointment schedulers, clerks, medical assistants, social workers, interpreters, physical therapists, occupational therapists, technicians, hospital leadership, pharmacy students, and nursing students.
Background
In conversations with patients, HCWs tend to focus more on delivering information than checking for understanding. October, Dizon, and Roter (2018) found that HCWs dominate the conversation and that their speaking turns are denser, with more statements per turn, whereas patients have fewer statements per turn. When providers talk too much, neither provider nor patient can evaluate accurate reception of the information. HCWs often define their job as making sure they give the patient all the information they need. This may result in a “tendency toward long monologues, even if they offer the patient a chance to speak when they are finished” (Roter, 2011, p. 82). The use of Teach Back ensures that the opportunity for both delivery and reception occurs.
Definitions of Teach Back vary widely. Many are conceptual and do not provide the specificity necessary to identify the occurrence of Teach Back in practice or research. Teach Back is generally defined as a procedure during which the patients describe information they have been taught, using their own words, to confirm understanding of the information. Many authors have expanded the definition to include additional components considered central to performing this skill.
Included in many definitions is the concept that Teach Back is a measure of the HCW's ability to clearly communicate information (Institute for Healthcare Advancement, 2012; Kornburger, Gibson, Sadowski, Maletta, & Klingbeil, 2013; Morony et al., 2018). It is not a test of the patient's ability (Institute for Healthcare Advancement, 2012). Teach Back should be performed in a way that mitigates the possibility that patients feel ashamed for lack of understanding and encourages patients' participation in their care (Kornburger et al., 2013).
Several definitions of Teach Back explicitly indicate that if the patient is not able to accurately restate the information, the HCW should reteach the information (Institute for Healthcare Advancement, 2012; Bogue & Mohr, 2017; Griffey et al., 2015; Ha Dinh, Bonner, Clark, Ramsbotham, & Hines, 2016; Kornburger et al., 2013; Morony et al., 2018). After reteaching the information, the HCW should perform Teach Back again and continue the cycle until patient understanding is achieved (Ha Dinh et al., 2016; Kornberger et al., 2013). Kornberger et al. (2013) include two other components of Teach Back: the use of plain language and delivering a limited amount of information in an education session.
Is Teach Back Effective?
In a systematic review, Ha Dinh et al. (2016) found that there was little consistency among studies evaluating the effectiveness of use of specific communication skills (including Teach Back) to improve patient outcomes. Although not all studies achieved statistical significance in the outcome measure, overall, the use of Teach Back improved disease-specific knowledge, adherence, self-efficacy, and proper use of inhalers (Ha Dinh et al., 2016). Teach Back has been associated with increased recall and understanding of information, reduced hospital readmission, and decreased length of stay when readmission was necessary (Bravo et al., 2010; Griffey et al., 2015; Peter et al., 2015).
Methods for Training Health Care Professionals in Teach Back
No evidence exists favoring one method of teaching communication strategies, including Teach Back, over another (Coleman, 2011). Methods found in the literature for training communication skills include didactic teaching, workshops, small-group activities, peer role play, videos, standardized patient encounters, observation, modeling, feedback, service learning, and online trainings (Institute for Healthcare Advancement, 2012; Coleman, 2011). More research into training methods is needed (Coleman, 2011; Toronto & Weatherford, 2015).
A program that employs multiple teaching techniques is likely to be the most effective (Coleman, 2011). After a Teach-Back training that included viewing a poster, observing a video, guided practice, handouts, and follow-up, Kornburger et al. (2013) found that nurses' knowledge of Teach Back increased by 33%, measured at 4 weeks after training. In the same study, self-reported use of Teach Back increased by more than 40%; however, participants were still only using Teach Back in 45% of encounters. Mahramus et al. (2014) used a combination of demonstration and guided practice, followed by summative feedback, to train 150 registered nurses on an inpatient cardiac unit in the use of Teach Back when teaching self-care skills to patients with heart failure. Ninety-three percent of participants achieved competence in the use of Teach Back by the end of the training (measured by direct observation), and 96% reported using Teach Back in a 3-month follow-up survey (Mahramus et al., 2014). In a small qualitative study, a 2-hour training that combined video demonstration, handouts, role play, and peer learning was effective for Teach-Back training (Morony et al., 2018). Participants felt that follow-up with the trainers, providing cues in the workplace, and more peer interaction would have increased competence.
Tools for Measuring Teach Back
Few tools to measure the occurrence of Teach Back exist, and none are validated (Badaczewski et al., 2017). Badaczewski et al. (2017) proposed the Teach Back Loop Score, a scale grading the extent to which the educator attempts Teach Back, corrects misunderstanding, and repeats Teach Back on a 2-point scale. Mahramus et al. (2014) deemed that participants achieved Teach Back competence if they educated the patient, used Teach Back, and communicated the purpose of Teach Back to the patient. No tools were found that measured the specific components of Teach Back.
Description of the Program
The 5Ts for Teach Back
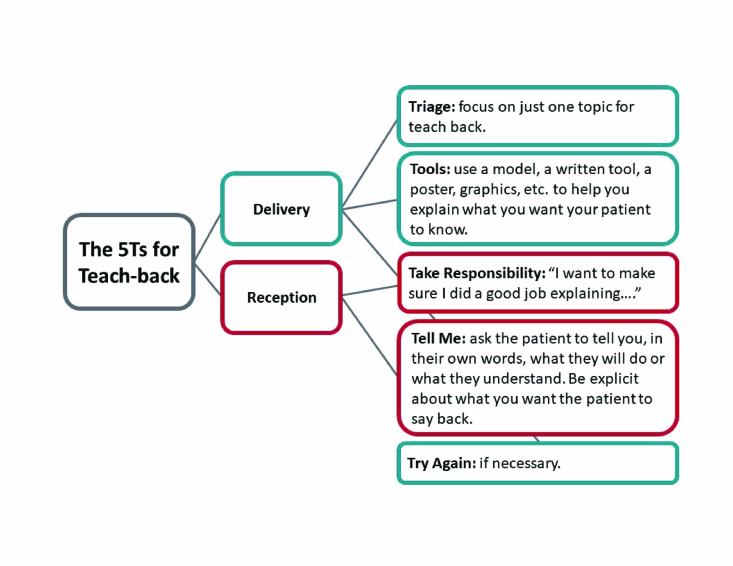
Teach Back is defined as asking patients, in a non-shaming way, to repeat, in their own words, specifically what they need to know or do. Based on this definition, the first author (K.A.) developed the 5Ts for Teach Back (5Ts), a training framework intended to make the process of Teach Back more concrete and easier to learn. The 5Ts is a standardized, operational definition of Teach Back containing five specific, observable steps: Triage, Tools, Take Responsibility, Tell Me, and Try Again. The Triage, Tools, and Try Again steps focus on effective information delivery, whereas the Take Responsibility and Tell Me steps serve to evaluate whether the patient received the information. We refer to the Take Responsibility and Tell Me steps as the “Teach Back lead-in.” Using all 5Ts encourages the inclusion of both delivery and reception (Figure 1).
Figure 1.
The 5Ts for Teach Back. Teach Back is about delivery and reception.
Triage. During the Triage step, the HCW determines which 1 to 3 topics are most important and will be the focus for education and Teach Back. Research has shown that the more information a clinician delivers, the less information the patient will remember correctly (Anderson, Dodman, Kopelman, & Fleming, 1979; Bravo et al., 2010). The Triage step is based on the concept of triage in a crowded emergency department, where HCWs must choose which patients to treat first based on their levels of acuteness. Similarly, a HCW who has several pieces of information to cover must triage the information by choosing Teach Back topics that are most important for the patient to remember or understand. This step is the key to Teach Back efficiency, discouraging the HCW from providing too much information. The HCW selects topics for Teach Back based on what are “can't miss” or frequently forgotten pieces of information.
When more than one topic is chosen for Teach Back, we encourage HCWs to use “chunk and check” (Brega et al., 2015). The HCW gives one topic, or “chunk,” of information at a time, each of which is followed by Teach Back. This process allows the HCW to deliver a larger amount of information in one teaching session, while making this amount of information manageable for the patient. By selecting the key points and stopping the delivery to perform Teach Back, HCWs are ensuring repetition and turn-taking, checking reception, and encouraging recall.
Tools. A tool is broadly defined as any aid that can assist the clinician with providing a clear explanation. Reader-friendly handouts, simple pen-and-paper drawings, models or diagrams, use of the HCW's own body (such as using the fist to represent the heart pumping), or even a relatable story are possible tools (Brega et al., 2015; Rubin, 2012). Tools should be accessible to patients with disabilities (e.g., braille, large print, read aloud, described) and professionally translated, if necessary (Brega et al., 2015).
Take responsibility. The Take Responsibility step is critical for the non-shaming aspect of the Teach-Back definition. This step happens once the HCW has delivered a chunk of information. The HCW may state, “That was a lot of information and it can be hard to remember all that at once, so I want to make sure I did a good job explaining it.”
The ideal Take Responsibility line contains two elements. The first is an acknowledgment of the quantity or complexity of the information given. This normalizes misunderstandings if they do occur, thereby reducing shame for the patient. The second is a statement implying that the HCW is the one being tested rather than the patient. This element also reduces the burden on the patient and reflects the impact of Teach Back on the HCW's communication skill development (Morony et al., 2018).
Tell me. During the Tell Me step, the HCW invites patients to state, in their own words, what they understood. The specificity of the Tell Me line impacts its effectiveness. Suppose an HCW spends 20 minutes explaining a new diagnosis of diabetes and then states, “Tell me what you learned about diabetes.” In this case, the patient may be overwhelmed by the quantity of information she is required to say back and therefore may not know where to start. Furthermore, the HCW will not be able to focus on the most important elements of the explanation. A more specific Tell Me line, such as, “How will you use your glucose meter when you go home?” allows the patient and the HCW to focus on one specific piece of information so they are both on the same page. An effective Triage step leads more naturally to specific Tell Me questions.
Try again. If the patient does not understand, the HCW must explain the information again, modifying the explanation to make it clearer. Depending on the magnitude of the error, another round of Teach Back may be needed. The HCW can assume responsibility for the error by returning to a Take Responsibility line, for example, “I'm sorry. I must not have explained that well enough.” Taking responsibility again may reduce the shame of an error for the patient.
Video
An extensive review of available Teach Back videos did not reveal a video demonstrating each of the 5Ts. We collaborated with our Information Technology department to produce a 15-minute video featuring a patient receiving discharge instructions from a physician and nurse. In the first part of the video, the HCWs do not perform Teach Back, and the patient demonstrates confusion about what she was taught. In the second part, the same discharge scenario is repeated, but with the HCWs demonstrating each of the 5Ts.
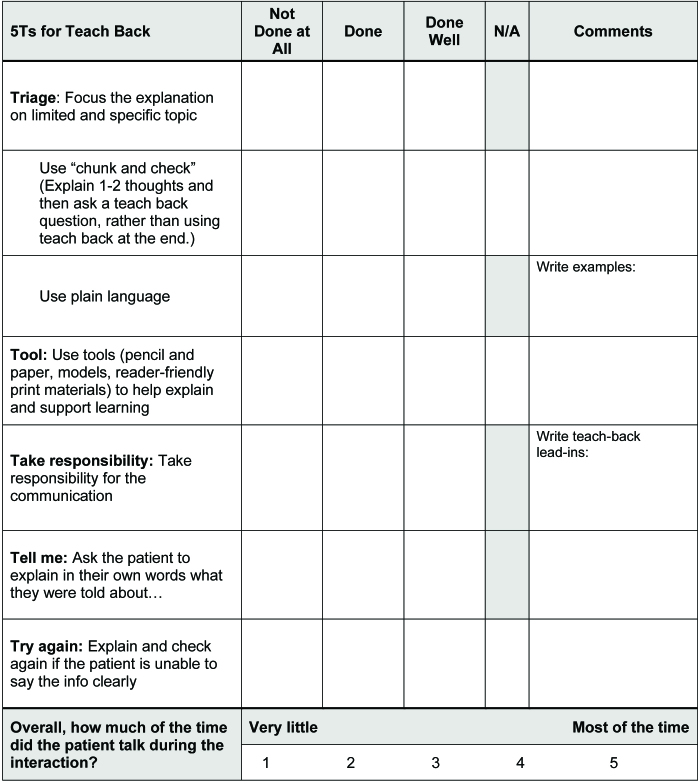
Observation Tool
The observation tool (Figure 2), based on the Always Use Teach Back! Toolkit model (Institute for Healthcare Advancement, 2012), lists each of the 5Ts, along with two additional “delivery” components. The tool is first used to rate the HCWs in the videos and again during practice sessions when participants observe their peers.
Figure 2.
Teach-Back Observation Tool. Sometimes, “chunking and checking,” using a “tool” or “trying again” is not appropriate. This is the reason for the “N/A” column.
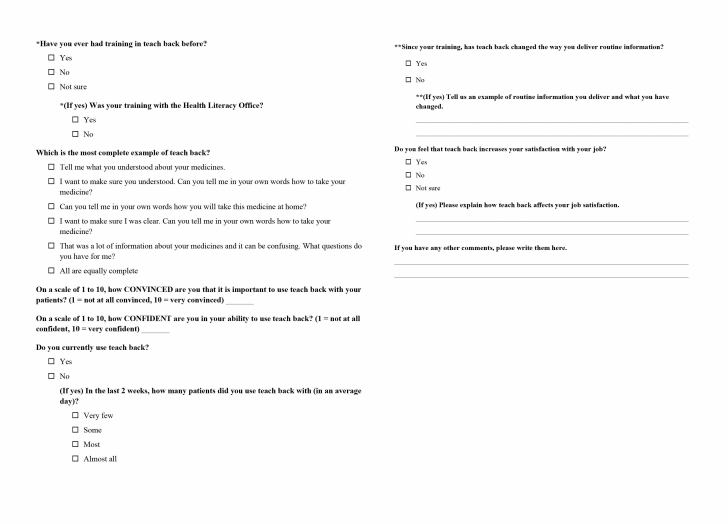
Pre- and Post-Training Surveys
We distribute an electronic pre-training survey about 1 week before the training date. We send a similar post-training survey 6 weeks after the training date (Figure 3).
Figure 3.
Pre- and post-training survey questions. *Only on the pre-training survey; **Only on the post-training survey.
Implementation
General Teach-Back Class
From 2014 to 2015, we developed an initial 4-hour class using the basic structure previously created by K.A. We obtained continuing nursing education credit for the class. Since 2016, we have been offering the training to HCWs in a large hospital. The class is listed on the hospital's centralized educational web page, offered regularly, and open to all hospital staff.
The training begins with a brief exercise in remembering a set of pill-taking instructions and a 1-hour didactic portion that encourages participants to think about why Teach Back is a useful tool. We talk about the complexity of the health care system, the overwhelming burden of detailed biomedical information that patients are given, and the fact that patients are seldom in an optimal condition for processing and retaining information.
We then introduce the 5Ts in an hour-long segment. We emphasize discussion of Triage and Take Responsibility. We also stress plain language and chunk-and-check as key concepts underlying effective delivery.
During the third hour of training, we show the two videos demonstrating patient education at the time of hospital discharge. In the first, the HCWs do not use Teach Back. In the second, the HCWs demonstrate all 5Ts. Using the Teach-Back Observation Tool, participants identify the 5Ts. The video observations provide a foundation for the final hour-long practice portion of the training. In the general training, because participants come from many different areas in the hospital system, we encourage participants to develop scenarios from their own experience. We also offer one or two simple, general topics. Participants work in groups of three: one acting as a patient, one acting as an HCW, and one acting as an observer. Before they start the practice, we encourage discussion of how to Triage the information and ask participants to write down the Take Responsibility and Tell Me lines they plan to use. Participants rotate roles, allowing each person to practice Teach Back as the HCW and to experience it as the patient and the observer.
Targeted Teach-Back Training
Later in 2016, in response to requests from units for trainings specific to their areas and appropriate to their schedules, we developed 1.5- to 2-hour targeted Teach-Back trainings. We also recognized that there might be advantages to training all staff from one unit as opposed to individuals. We hypothesized that this would be more effective for embedding the use of Teach Back in practice. HCWs could observe the strategy performed by their peers, learn from each other, and share their experiences. This process may serve as a continuation of the training and reinforce the expectation of its use. When we trained a specific unit, we worked in advance with unit leadership to tailor the practice session with scenarios and tools relevant to that unit, as well as to differing roles within the clinics or units.
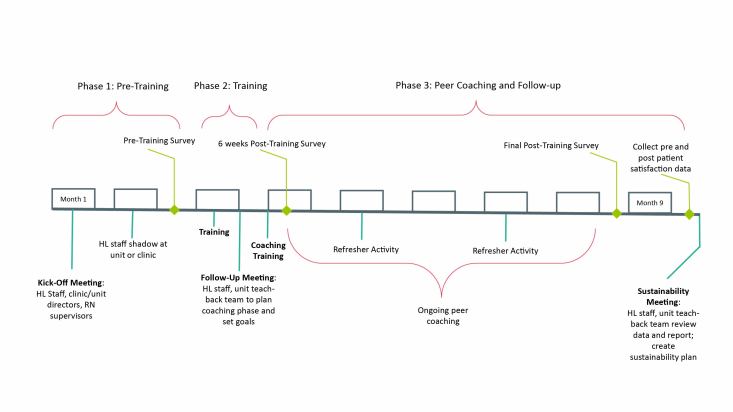
Midcourse Adjustments
By 2017, we saw clearly that one training did not ensure the use of the strategy in practice. We presented a proposal to ambulatory (outpatient/clinic) leadership for an extended version of the 5Ts training. The success of our proposal resulted from our growing reputation within the institution and our relationships with ambulatory management. We presented a clear outline and timeline (Figure 4) of the project and provided pre- and post-training survey data from the previous year of Teach-Back training. We proposed adding a 5-month follow-up period of peer coaching and skills validation, and two refresher activities to the targeted Teach-Back offering. Hospital leadership mandated the extended training, called Closing the Gap (CTG) With Teach Back, for all ambulatory clinics.
Figure 4.
Closing the gap with Teach Back timeline.
CTG consists of a 2-hour training, three meetings with leadership, and a Teach-Back team responsible for coaching and skills validation. We developed a detailed toolkit, which provides the framework and tools to guide clinics through the process. The toolkit contains instructions for the unit, a coaching guide, and sample refresher activities. We embedded as much flexibility into the program as possible, recognizing that much variability exists in the way clinics arrange their staff and clinic flow.
Before the training, the health literacy (HL) staff shadows staff at the clinic to observe conversations, note opportunities for Teach Back, and develop relevant scenarios for practice during training. The shadowing has the added benefit of introducing the HL staff to the unit and creating buy-in; staff have said that they feel the training is about them, not just another generic initiative (clinic leader, personal communication, January 19, 2018). After shadowing, the initial 2-hour training, which uses the same methods as the 4-hour class, is offered once or multiple times to ensure that all the staff were trained. Unit leadership identifies peer coaches, who receive an additional 1-hour training. These peer coaches observe HCWs using Teach Back and provide them with feedback for improvement. Two refresher activities are required during the course of the 5 months. Refresher activities could include game-based Teach-Back review sessions at staff meetings or visual reminders of the 5Ts on bulletin boards. The unit Teach-Back team decides on and creates the activities, with help from the HL Office as needed.
To provide an opportunity for continued skill building beyond the basic class, we developed three advanced Teach-Back classes. These trainings focus on (1) development and use of documents as tools for Teach Back, (2) listenability (Rubin, 2012), and (3) use of Teach Back during the discharge process. The addition of these three classes enables participants who have taken the first 4-hour training to keep working on their skills. It also allows units who participated in CTG to send newly hired staff for training and others for refreshers.
Results
We have successfully trained more than 1,300 HCWs to use the 5Ts when delivering any type of information to patients. We find that anyone who gives information to patients can benefit from a Teach-Back training. The flexibility of the 5Ts model and our training method allows us to tailor instruction to many different roles in the health care system.
The Take Responsibility step, although primarily aimed at creating a non-shaming environment for patients, may shift how HCWs approach information delivery and patient education. One nurse described Teach Back as “a different paradigm,” citing concepts introduced by the Take Responsibility step (nurse, personal communication, June 18, 2018). Perhaps it is because of this paradigm shift that Take Responsibility is the most often forgotten step in training practice. It is often a new habit to incorporate into practice and even a culture shift for a highly educated workforce that is taught to demonstrate confident expertise. One participant noted:
We are self-centered in the way that we deliver our education and Teach Back totally changed the way we look at it. It's our job to get the information through, and not the patients' to soak it up. They [the patients] are not from here [the hospital] so we can't expect that. I don't think we mean to expect that of the patients, but we do.
(nurse, personal communication, June 18, 2018)
The Take Responsibility step, therefore, not only lessens the patient's shame of not understanding, but can also change how health care staff view the education process itself.
We have anecdotal evidence that training participants do not correctly retain the operational definition of Teach Back (including the 5Ts) after a single training. For example, a year after he had taken a one-time training, an appointment scheduler defined the Tell Me step as asking the patient, “Did you understand what I just mentioned? Is there anything you'd like to go over once more? Does that make sense?” (appointment scheduler, personal communication, June 18, 2018). These questions suggest that a 2- to 4-hour training does not ensure retention of the 5Ts concept.
When discussing barriers to Teach Back, training participants often cite a lack of time. However, participants also seem to recognize that Teach Back saves time when looking at longer-term efficiency. For example, after completing the CTG program, a clinic leader stated that patients were more often prepared for their appointments because they had completed required pre-appointment laboratory assessments and tests (clinic leader, personal communication, January 19, 2018). Similarly, an appointment center scheduler noted that Teach Back improved efficiency of his call center because patients were not calling back with questions that could have been answered during the initial phone call. In the short term, however, staff often estimate that using Teach Back takes more time than patient encounters without Teach Back. Given time limitations, it is likely that HCWs may only use Teach Back with those whom they perceive to have trouble understanding (appointment scheduler, personal communication, June 18, 2018; Jager & Wynia, 2012). Therefore, Teach Back, when conceptualized strictly within short-term time constraints, seems to be less efficient. However, information included in our trainings about increased efficiency over time as the skill is practiced, as well as longer-term operational efficiency (e.g., fewer patient call-backs), can counter worries about time barriers.
Lessons Learned
Although we have not conducted a scientific research study, we have learned a great deal while conducting our Teach-Back trainings. During our classes, the observers in the practice sessions learn almost as much as the HCWs. Using the Observation Tool to recognize the 5Ts reinforces the skills. Follow up with some of our participants has shown that they do not retain knowledge of the 5Ts after a single Teach-Back training session. We expect post-training surveys to show that the follow-up component of our CTG with Teach-Back program will begin to rectify some of these misunderstandings.
Teach-Back training is becoming firmly entrenched in our institution. Units that adopted the universal use of Teach Back early have seen anecdotal successes, motivating other units to institute Teach Back. Support from all levels of leadership, through active participation in trainings and demonstration of its use, reinforced the value and importance of the strategy.
As entire units complete the CTG training, we are finding that Teach Back becomes embedded into the unit culture. Because the 5Ts are standardized and observable, managers can send new hires and HCWs needing review to our hospital-wide Teach-Back classes. Unit-based peer coaches use a modified version of the Teach-Back Observation Tool to evaluate and provide feedback on the effective use of Teach Back in practice.
We found that flexibility of the program is key to sustainability. Tailoring the program to an individual unit's staffing and schedule facilitates engagement. Shadowing on the unit ahead of the training also allows training scenarios to be tailored to the unit and increases the relevance for staff. Limiting the number of formal training sessions but supporting them with unit-based coaching allows for more frequent reinforcement of the 5Ts without significantly affecting unit workload.
Our organizational structure does not allow mandated Teach-Back training for physicians or other providers, who rarely participate in the trainings. Because providers deliver much of the patient education in our outpatient settings, increased provider participation is likely needed before we can measure whether Teach Back impacts Press Ganey patient satisfaction metrics for patient education. Anecdotally, providers feel there is not enough evidence to show the benefits of Teach Back outweigh the amount of time necessary to do Teach Back. As further research demonstrates the effectiveness of Teach Back, we hope that our providers will better appreciate the value of Teach Back.
While reviewing the literature, we noted that many researchers do not publish their operational definitions of Teach Back. The 5Ts could be useful in further research to determine the effect on patient outcomes when a standardized method of Teach-Back training is implemented.
The 5Ts model is a helpful tool when training HCWs in the use of Teach Back. The 5Ts model breaks Teach Back into individual observable skills, making it ideal for teaching the skill in small steps. Because all of the 5Ts steps are observable, they can be easily identified during training, coaching, and evaluation. Development of an institution-wide Teach-Back training program requires time and dedicated staff to complete. Obtaining high-level leadership support is critical to the success of the program.
As Coleman (2011) noted, there is a lack of data on the effectiveness of health literacy training methods and curricula. Our next steps would address this gap by validating the Teach-Back Observation Tool as well as the pre- and post-training surveys distributed to participants. Validating these tools will allow for their effective use in research. We will pursue mandatory 5Ts training for providers. We hypothesize that training both staff and providers will maximize the potential for improved patient satisfaction scores, lower read-mission rates, and better patient outcomes.
References
- Anderson J. L. Dodman S. Kopelman M. Fleming A. (1979). Patient information recall in a rheumatology clinic. Rheumatology and Rehabilitation, 18(1), 18–22 10.1093/rheumatology/18.1.18 PMID: [DOI] [PubMed] [Google Scholar]
- Badaczewski A. Bauman L. J. Blank A. E. Dreyer B. Abrams M. A. Stein R. E. K. Sharif I. (2017). Relationship between Teach Back and patient-centered communication in primary care pediatric encounters. Patient Education and Counseling, 100(7), 1345–1352 10.1016/j.pec.2017.02.022 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogue T. L. Mohr L. (2017). Putting the family back in the center: A Teach Back protocol to improve communication during rounds in a pediatric intensive care unit. Critical Care Nursing Clinics of North America, 29(2), 233–250 10.1016/j.cnc.2017.01.009 PMID: [DOI] [PubMed] [Google Scholar]
- Bravo B. N. Postigo J. M. Segura L. R. Selva J. P. Trives J. J. Córcoles M. J. López M. N. Hidalgo J. L. (2010). Effect of the evaluation of recall on the rate of information recalled by patients in primary care. Patient Education and Counseling, 81(2), 272–274 10.1016/j.pec.2010.01.022 PMID: [DOI] [PubMed] [Google Scholar]
- Brega A. G. Barnard J. Mabachi N. M. DeWalt D. A. Brach C. Cifuentes M. West D. R. (2015). AHRQ Health Literacy Precautions Toolkit (2nd ed). Agency for Healthcare Research and Quality. [Google Scholar]
- Coleman C. (2011). Teaching health care professionals about health literacy: A review of the literature. Nursing Outlook, 59, 70–78 10.1016/j.outlook.2010.12.004 PMID: [DOI] [PubMed] [Google Scholar]
- Coleman C. Hudson S. Pederson B. (2017). Prioritized health literacy and clear communication practices for health care professionals. HLRP: Health Literacy Research and Practice, 1(3), e91–e99 10.3928/24748307-20170503-01 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffey R. T. Shin N. Jones S. Aginam N. Gross M. Kinsella Y. Kaphingst K. A. (2015). The impact of Teach Back on comprehension of discharge instructions and satisfaction among emergency patients with limited health literacy: A randomized, controlled study. Journal of Communication in Healthcare, 8(1), 10–21 10.1179/1753807615Y.0000000001 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ha Dinh T. T. Bonner A. Clark R. Ramsbotham J. Hines S. (2016). The effectiveness of the Teach Back method on adherence and self-management in health education for people with chronic disease: A systematic review. JBI Database of Systematic Reviews and Implementation Reports, 14(1), 210–247 10.11124/jbisrir-2016-2296 PMID: [DOI] [PubMed] [Google Scholar]
- Institute for Healthcare Advancement. (2012). Always use Teach Back! Training toolkit. Retrieved from www.teachbacktraining.org
- Jager A. J. Wynia M. K. (2012). Who gets a Teach Back? Patient-reported incidence of experiencing a Teach Back. Journal of Health Communication, 17(Suppl. 3), 294–302 10.1080/10810730.2012.712624 PMID: [DOI] [PubMed] [Google Scholar]
- Kornburger C. Gibson C. Sadowski S. Maletta K. Klingbeil C. (2013). Using “Teach Back” to promote a safe transition from hospital to home: An evidence-based approach to improving the discharge process. Journal of Pediatric Nursing, 28(3), 282–291 10.1016/j.pedn.2012.10.007 PMID: [DOI] [PubMed] [Google Scholar]
- Mahramus T. Penoyer D. A. Frewin S. Chamberlain L. Wilson D. Sole M. L. (2014). Assessment of an educational intervention on nurses' knowledge and retention of heart failure self-care principles and the Teach Back method. Heart & Lung, 43(3), 204–212 10.1016/j.hrtlng.2013.11.012 PMID: [DOI] [PubMed] [Google Scholar]
- Morony S. Weir K. Duncan G. Biggs J. Nutbeam D. Mccaffery K. J. (2018). Enhancing communication skills for telehealth: Development and implementation of a Teach Back intervention for a national maternal and child health helpline in Australia. BMC Health Services Research, 18(1), 162 Advance online publication. 10.1186/s12913-018-2956-6 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- October T. W. Dizon Z. B. Roter D. L. (2018). Is it my turn to speak? An analysis of the dialogue in the family-physician intensive care unit conference. Patient Education and Counseling, 101(4), 647–652 10.1016/j.pec.2017.10.020 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peter D. Robinson P. Jordan M. Lawrence S. Casey K. Salas-Lopez D. (2015). Reducing readmissions using Teach Back: Enhancing patient and family education. The Journal of Nursing Administration, 45(1), 35–42 10.1097/NNA.0000000000000155 PMID: [DOI] [PubMed] [Google Scholar]
- Roter D. L. (2011). Oral literacy demand of health care communication: Challenges and solutions. Nursing Outlook, 59, 79–84 10.1016/j.outlook.2010.11.005 PMID: [DOI] [PubMed] [Google Scholar]
- Rubin D. L. (2012). Listenability as a tool for advancing health literacy. Journal of Health Communication, 17(Suppl. 3), 176–190 10.1080/10810730.2012.712622 PMID: [DOI] [PubMed] [Google Scholar]
- Toronto C. E. Weatherford B. (2015). Health literacy education in health professions schools: An integrative review. The Journal of Nursing Education, 54(12), 669–676 10.3928/01484834-20151110-02 PMID: [DOI] [PubMed] [Google Scholar]