Abstract
Objectives
Cerebrospinal fluid (CSF) visinin-like protein 1 (VILIP-1) has been suggested as a biomarker for neuron injury, which has been shown to have a important diagnostic value in symptomatic Alzheimer’s disease (AD). The study purpose is investigating potential effects of apolipoprotein E (APOE) ε4 on CSF VILIP-1 levels among the preclinical AD.
Methods
A total of 110 subjects (including 43 APOE ε4 carriers and 67 ε4 non-carriers) were obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) in the present study.
Results
The results showed that VILIP-1 concentrations in the CSF were statistically significantly increased in APOE ε4 carriers in comparison with non-carriers. Increased CSF VILIP-1 level was positively associated with the concentrations of both CSF-tau and P-tau levels.
Conclusions
Our findings suggested that APOE ε4 might affect CSF VILIP-1 level in preclinical AD, indicating an important role of APOE ε4 in neuron injury leading to AD.
Keywords: APOE ε4, VILIP-1, Alzheimer’s disease, cerebrospinal fluid
Introduction
As we have known, Alzheimer’s Disease (AD) is the most globally popular neurodegenerative disease. The apolipoprotein E (APOE) ε4 allelic variant has a crucial dose-dependent association with AD risk,1,2 which can accelerate the age of symptom onset.3 Based on the type of pathophysiology of each measurement, a core “A/T/N” system for biomarkers has been proposed that classifies the seven most important AD biomarkers into three binary categories, “A” represents the value of Aβ biomarker (amyloid PET or CSF Aβ42), “T” refers to the value of tau biomarker (CSF p-tau or tau PET), and “N” is a biomarker for neurodegeneration or neuronal injury (18F-fluorodeoxyglucose-PET, structural MRI, or CSF total tau).4 However, the mechanism underlying the regulation of AD progression associated with APOE ε 4 remains unknown.
As a neuronal calcium-sensor protein,5,6 visinin-like protein 1 (VILIP-1) has been suggested as a biomarker of neuron injury.7 Previous studies have shown that cerebrospinal fluid (CSF) VILIP-1 was significantly associated with AD, indicating that VILIP-1 may be a potential biomarker for neurodegeneration.8–10 Although it is unclear whether low levels of APOE actually contribute to the pathological changes of AD, it is hypothesized that APOE is critical for Aβ clearance and aggregation.11–13 Increasing evidence suggested that APOE was a major carrier of cholesterol required for neuronal activity and injury repair in the brain.14,15 Therefore, the hypothesis that APOE ε4 deleteriously influences neuron injury, and contributes to elevated CSF VILIP-1 concentrations, which subsequently leads to cognitive degeneration in APOE ε4 carriers who are at risk of progressing from mild cognitive impairment (MCI) to AD.
So, the objective of the research is to explore the effects of APOE ε4 on CSF VILIP-1 concentrations among the elderly participants from the Alzheimer’s Disease Neuroimaging Initiative (ADNI).
Methods
ADNI Study
ADNI database (adni.loni.usc.edu) provided detailed data for the research. During the experiment, data collectors have no access to participant information. The ADNI was founded in 2003 as a public–private partnership with the leading of Principal Investigator Michael W. Weiner, MD. The principle aim of ADNI is to examine if serial magnetic resonance imaging (MRI), positron emission tomography (PET), other biological markers, and clinical and neuropsychological evaluation could be used to assess the progression of MCI and early AD. For more details, please find www.adni-info.org. All participants or authorized representatives offered written informed consent. And each ADNI site received institutional review board (IRB) individually.
Participants
Demographic data were extracted from ADNI. Selection standard was discussed with details at http://www.adni-info.org. The participants involved in our analysis were aged from 55 to 90 years, with more than 6 years of schooling, and Spanish or English speaking. In addition, we excluded individuals having any other neurological disease other than AD. Totally, 110 individuals (including 43 APOE ε4 carriers and 67 non-carriers) were enrolled in our analysis.
Clinical Assessments
A certified cognitive evaluation containing the following listed contents was used to evaluate different domains of cognition in all participants: Mini-Mental State Examination (MMSE),16 Alzheimer’s Disease Assessment Scale-cognitive subscale 13 (ADAS-13),17 and Global Clinical Dementia Rating Scale (CDR-SB)18 were used to measure general cognitive function; The Rey Auditory Verbal Learning Test (RAVLT), including 5-min delayed recall (RAVLT-immediate recall), 30-min delayed recall (RAVLT-delayed recall), and yes-no recognition (RAVLT-recognition) were applied to measure memory;19 The Trail Making Test-A and B (TMT-A/B)20 was adopted to assess attention/executive function; Animal fluency and 30-item Boston Naming Task (BNT-30)21 was used to evaluate language; Clock Drawing Test (CDT) was applied to measure visuospatial;22 Functional Assessment Questionnaire (FAQ)23 and Neuropsychiatric Inventory (NPI)24 were used to assess psychosocial function.
Genotyping Analysis
APOE genotypes (gene map locus 19q13.2) were achieved from the ADNI database for all participants (adni.loni.usc.edu). Individuals involved were stratified into two groups: the ε2/ε4, ε3/ε4, or ε4/ε4 genotypes were defined as APOE ε4 carriers; the ε2/ε2, ε2/ε3, or ε3/ε3 genotypes were defined as APOE ε4 non-carriers.
CSF Measurements
A sandwich ELISA (together with the Erenna® immunoassay platform) was used to test VILIP-1 level in CSF.9 CSF Aβ42, total-tau, and P-tau levels were analyzed using a multiplex xMAP Luminex system (Luminex Corp, Austin, TX, USA) combining an INNOBIA AlzBio3 kit (Fujirebio, Ghent, Belgium), which has been described in previous publications.25–27 The unit for VILIP-1, Aβ42, total-tau and P-tau was pg/mL. More details of methodologies for the acquisition of ADNI and measurements as well as quality control process are located at www.adni-info.org.
Neuroimaging
The description of detailed information about ADNI neuroimaging standardized procedure can be found in a previous paper.28 ADNI MRI data were obtained from a 3-Tesla MRI scanner. FreeSurfer version 5.1 image analysis (http://surfer.nmr.mgh.harvard.edu/)29 was used to reflect cortical reconstruction and volumetric segmentation, as described in previous studies.30–33 In the current study, we also measured the hippocampus, entorhinal cortex (EC), fusiform and medial temporal-lobe atrophy (MTA) volumes. More description regarding the imaging protocol of ADNI is located at http://adni.loni.usc.edu/methods/documents/mri- protocols/.
Statistical Analysis
Student’s t-test for normally distributed continuous variables or Mann–Whitney test for skewed distributed variables was applied to tell demographic profile differences between APOE ε4 carriers and non-carriers in the elderly subjects. Chi-square test analysis was done to check the distribution of categorical parameters. Spearman’s correlation test was conducted to explore whether CSF VILIP-1 concentrations were linked to other core CSF biomarkers. In addition, linear regression models were adopted to examine if CSF VILIP-1 level is correlated to APOE ε4 genotype. SPSS software (version 23.0; IBM SPSS) was used for statistical analyses. A value of two-sided P < 0.05 was treated as the standard to show statistical significance in the paper. GraphPad Prism 6 was used to produce figures.
Results
Demographic Features for Participants, Stratified by APOE Alleles
Baseline demographic details of the subjects are shown in Table 1. We included 43 APOE ε4 carriers together with 67 APOE ε4 non-carriers in the current study. In brief, APOE ε4 carriers were younger than APOE ε4 non-carriers (P = 0.021). Gender (P = 0.796) and education levels (P = 0.284) did not appear to be different between the two groups. Furthermore, the scores of RAVLT-immediate recall (P = 0.003), RAVLT-delayed recall (P < 0.001), and RAVLT-recognition (P = 0.016) were lower among APOE ε4 carriers when comparing to APOE ε4 non-carriers. APOE ε4 carriers performed worse on MMSE (P = 0.003), ADAS13 (P < 0.001), CDR-SB (P < 0.001), and FAQ (P = 0.002) than APOE ε4 non-carriers. However, no significantly statistical differences existed in TMT-A, TMT-B, Animals fluency, BNT-30, CDT, or NPI (P = 0.693; P = 0.379; P = 0.437; P = 0.377; P = 0.534; P = 0.130) between APOE ε4 carriers and non-ε4 carriers. Finally, the CSF Aβ42, total tau, and P-tau levels appeared to be significantly different between two groups (P < 0.001; P < 0.001; and P < 0.001; respectively). Significantly smaller volumes of hippocampus and entorhinal cortex were found in APOE ε4 carriers in comparison to APOE ε4 non-carriers (P = 0.020; P < 0.001; respectively).
Table 1.
Demographic and Clinical Characteristics of Participants by APOE ε4 Zygosity
| Characteristics | ε4 Carriers (n = 43) | ε4 Non-Carriers (n = 67) | P-value |
|---|---|---|---|
| Age, years | 73.17 (6.09) | 75.82 (5.58) | 0.021 |
| Gender (female), % | 15 (34.88) | 25 (37.31) | 0.796 |
| Education, years | 16 (14–18) | 16 (14–18) | 0.284 |
| MMSE | 27 (26–29) | 29 (27–30) | 0.003 |
| ADAS-13 | 17.65 (7.04) | 12.10 (6.31) | <0.001 |
| CDR-SB | 1.5 (0.5–2.0) | 0 (0–1) | <0.001 |
| RAVLT-immediate recall | 4.35 (3.91) | 6.52 (3.52) | 0.003 |
| RAVLT-delayed recall | 1 (0–5) | 7 (3–9) | <0.001 |
| RAVLT-recognition | 10 (8–14) | 13 (11–14) | 0.016 |
| TMT-A | 34 (29–45) | 36 (29–45) | 0.693 |
| TMT-B | 92 (70–118) | 85 (67–106) | 0.379 |
| Animals fluency | 16.88 (4.38) | 17.61 (5.01) | 0.437 |
| BNT-30 | 28 (26–29) | 28 (25–30) | 0.377 |
| CDT | 5 (4–5) | 5 (4–5) | 0.534 |
| FAQ | 1 (0–5) | 0 (0–1) | 0.002 |
| NPI | 0 (0–0) | 0 (0–0) | 0.130 |
| CSF Aβ42 (pg/mL) | 576.8 (498.6–723.1) | 1148.0 (775.6–1643.0) | <0.001 |
| CSF-tau (pg/mL) | 333.29 (107.99) | 248.92 (85.90) | <0.001 |
| CSF P-tau (pg/mL) | 33.71 (12.69) | 23.15 (9.28) | <0.001 |
| CSF VILIP-1 (pg/mL) | 189.16 (58.90) | 148.25 (50.55) | <0.001 |
| Hippocampus (mm3) | 6385.54 (1051.64) | 6872.28 (1052.59) | 0.020 |
| Entorhinal (mm3) | 3177.65 (717.05) | 3762.28 (772.20) | <0.001 |
| Fusiform (mm3) | 17,168.63 (2260.15) | 16,819.05 (1932.13) | 0.388 |
| MTA (mm3) | 19,307.09 (2643.83) | 19,345.96 (2769.64) | 0.942 |
Notes: Data are presented as mean ± SD by using Student’s t test for normally distributed continuous variables, median (M) and the interquartile range (IQR) by Mann–Whitney test for skewed distribution variables. For gender, values are presented as number (%) by using Chi-square test.
Abbreviations: ADAS-13, Alzheimer’s disease assessment scale-cognitive subscale 13; BNT-30, boston naming task; CDR-SB, global clinical dementia rating scale; CDT, clock drawing Test; CSF, cerebrospinal fluid; FAQ, functional assessment questionnaire; MMSE, mini-mental state examination; MTA, mesial temporal atrophy; NPI, neuropsychiatric inventory; RAVLT, rey auditory verbal learning test; SD, standard deviation; TMT, the trail making test; VILIP-1, visinin-like protein-1.
Levels of CSF VILIP-1 in the Two Groups
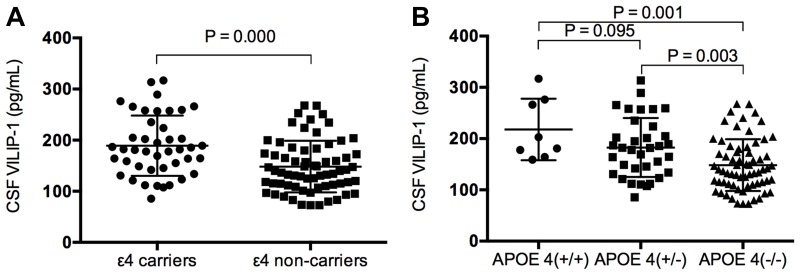
To further look into the association between APOE ε4 genotype and concentration of CSF VILIP-1, the concentrations of CSF VILIP-1 between APOE ε4 carriers and non-carriers were compared. We saw an obvious increased VILIP-1 level among the APOE ε4 carriers than the APOE ε4 non-carriers (mean, 189.16 vs. 148.25 pg/mL, P < 0.001, Table 1, Figure 1A). Furthermore, to evaluate the gene dose-effect of APOE ε4 on the level of CSF VILIP-1, the concentrations of CSF VILIP-1 among APOE ε4 (+/+), APOE ε4 (+/-) and APOE ε4 (-/-) subjects (APOE ε4 +/+, n = 8; APOE ε4 +/-, n =35; APOE ε4 -/-, n = 67) were compared. The results showed that CSF VILIP-1 concentrations were higher in APOE ε4 (+/+) compared to APOE ε4 (-/-) (P = 0.001), and CSF VILIP-1 levels were elevated in APOE ε4 (+/-) compared to APOE ε4 (-/-) subjects (P = 0.003) (Figure 1B).
Figure 1.
Comparison of CSF VILIP-1 concentrations in APOE ε4 carriers and APOE ε4 non-carriers in the elderly subjects. (A) CSF VILIP-1 levels were significantly elevated in APOE ε4 carriers compared with APOE ε4 non-carriers (P = 0.000). (B) The CSF VILIP-1 concentrations are elevated in a gene dose-dependent manner of APOE ε4. All data are shown as mean ± SD. P values tested by Student’s t-test.
Abbreviations: CSF, cerebrospinal fluid; SD, standard deviation; VILIP-1, visinin-like protein-1.
Correlations Between Aβ42, Tau, P-Tau and CSF VILIP-1
In order to evaluate if changes in CSF concentrations of VILIP-1 are associated with Aβ42, Tau and P-tau in the elderly, the associations between CSF VILIP-1 and other core CSF biomarkers in the whole sample (Table 2) were examined by conducting Spearman’s correlation analyses. The results demonstrated that CSF VILIP-1 concentration was positively related to Tau and P-tau (R = 0.857, P < 0.001; R = 0.815, P < 0.001). Nevertheless, no significant association between the levels of CSF VILIP-1 and Aβ42 (R = 0.000, P = 0.997) was found.
Table 2.
Correlations of CSF VILIP-1 Level with Aβ42, Tau and P-Tau
| Aβ42 | Tau | P-Tau | |
|---|---|---|---|
| CSF VILIP-1 | |||
| R | 0.000 | 0.857** | 0.815** |
| P | 0.997 | <0.001 | <0.001 |
Notes: Associations were measured by Spearman’s correlation analyses. **P < 0.01.
Abbreviations: CSF, cerebrospinal fluid; VILIP-1: visinin-like protein-1.
Relation Between CSF VILIP-1 Concentrations and APOE ε4 Levels
The linear regression analysis revealed the possible correlation of the presence of APOE ε4 allele and CSF VILIP-1 levels between the elderly subjects (Table 3). In the unadjusted model (Model 1), the CSF VILIP-1 concentration was statistically related with APOE ε4 (standardized β = 0.350, P < 0.001). In model 2 on the basis of fixed age, sex and education level, a significant association between concentrations of CSF VILIP-1 and APOE ε4 (standardized β = 0.344, P < 0.001) was witnessed. In the adjusted model 3 (which is model 2 plus MMSE, CDR-SB, RAVLT-immediate recall and RAVLT-delayed recall), the VILIP-1 level was still linked to APOE ε4 (standardized β = 0.298, P = 0.003). In model 4 (which is model 3 plus CSF Aβ42 and P-tau), the association between CSF VILIP-1 level and APOE ε4 (standardized β = 0.137, P = 0.050) continued to exist. In model 5 (model 4 plus volumes of hippocampus and entorhinal cortex), the concentration of CSF VILIP-1 was still linked with APOE ε4 (standardized β = 0.144, P = 0.049).
Table 3.
Linear Regression to Evaluate the Potential Association Between CSF VILIP-1 and APOE ε4 Status in the Elderly (Unadjusted and Adjusted)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Beta | P | Beta | P | Beta | P | Beta | P | Beta | P | |
| APOE ε4 (+) vs. (-) | 0.350 | <0.001 | 0.344 | <0.001 | 0.298 | 0.003 | 0.137 | 0.050 | 0.144 | 0.049 |
| Age | −0.080 | 0.390 | −0.061 | 0.526 | −0.038 | 0.515 | −0.044 | 0.484 | ||
| Gender | 0.208 | 0.033 | 0.211 | 0.035 | 0.027 | 0.659 | 0.032 | 0.633 | ||
| Education | 0.064 | 0.507 | 0.050 | 0.605 | −0.042 | 0.48 | −0.039 | 0.528 | ||
| MMSE | 0.069 | 0.537 | 0.042 | 0.539 | 0.045 | 0.518 | ||||
| CDR-SB | −0.010 | 0.929 | 0.010 | 0.889 | 0.006 | 0.936 | ||||
| RAVLT-immediate recall | 0.020 | 0.907 | 0.054 | 0.607 | 0.062 | 0.574 | ||||
| RAVLT-delayed recall | −0.215 | 0.218 | −0.101 | 0.346 | −0.107 | 0.325 | ||||
| CSF Aβ42 | 0.314 | <0.001 | 0.306 | <0.001 | ||||||
| CSF P-tau | 0.776 | <0.001 | 0.772 | <0.001 | ||||||
| Hippocampus | −0.033 | 0.691 | ||||||||
| Entorhinal | 0.042 | 0.584 | ||||||||
Notes: Model 1: unadjusted; Model 2: adjusted by age, gender, education; Model 3: adjusted by age, gender, education, MMSE, CDR-SB, RAVLT-immediate recall and RAVLT-delayed recall; Model 4: adjusted by age, gender, education, MMSE, CDR-SB, RAVLT-immediate recall, RAVLT-delayed recall, CSF Aβ42 and P-tau; Model 5: adjusted by age, gender, education, MMSE, CDR-SB, RAVLT-immediate recall, RAVLT-delayed recall, CSF Aβ42, P-tau, volumes of hippocampus and entorhinal cortex. Beta is standardized beta.
Abbreviations: CDR-SB, global clinical dementia rating scale; MMSE, mini-mental state examination; RAVLT, rey auditory verbal learning test.
Discussion
As a neuronal calcium-sensor protein,5,6 VILIP-1 has been suggested as a marker for neuron injury in brain injury models.7,34,35 Previous studies indicated that the level of CSF VILIP-1 was associated with the concentrations of CSF-tau and P-tau,6,8,9 supporting its utilization as a neurodegeneration marker. In addition, some studies revealed that CSF VILIP-1 could diagnostically discriminate AD from other dementias.36,37 Therefore, these numerous studies implied that CSF VILIP-1 might be a useful biomarker for AD pathophysiology.9,10,38-44 Although only one study found no significant difference in the longitudinal changes of CSF VILIP-1 levels in cognitively normal subjects and AD patients.45 Importantly, researchers also showed elevated levels of plasma VILIP-1 in AD patients compared to non-demented controls.9 Generally, the current VILIP-1 data suggest a possible role in the selection and prognosis of subjects (Table 4), but the results are different and require further investigation.
Table 4.
Studies to Assess the Role of CSF VILIP-1 as a Potential Biomarker
| Study | AD | MCI | Controls | Analysis Method | Results |
|---|---|---|---|---|---|
| Lee et al (2008)8 | 33 | / | 24 | ELISA | Significantly increased in AD compared to control subjects |
| Tarawneh et al (2011)9 | 98 | / | 211 | Microparticle based immunoassay (Erenna, Singulex, CA) | Significantly higher in AD compared to controls |
| Tarawneh et al (2012)10 | 60 | / | 211 | Microparticle based immunoassay (Erenna, Singulex, CA) | Significantly elevated in AD compared to controls |
| Luo et al (2013)37 | 61 | / | 40 | ELISA | Significantly higher in AD patients than control subjects |
| Kester et al (2015)45 | 65 | 61 | 37 | Microparticle based immunoassay (Erenna, Singulex, CA) | Baseline levels elevated in AD and MCI than controls but not significantly (P = 0.88); Baseline levels significantly increased in MCI progressed to AD than stable MCI; Longitudinal increased in MCI, but not in AD or cognitively normal individuals |
| Mroczko et al (2015)39 | 33 | 15 | 18 | ELISA | Significantly higher in AD patients compared with MCI and control individuals |
| Sutphen et al (2015)46 | 169 | Microparticle based immunoassay (Erenna, Singulex, CA) | Significantly increased in late middle-aged individuals compared with early and mid in APOE ε4 non-carriers | ||
| Tarawneh et al (2015)38 | 23 | / | 64 | Microparticle based immunoassay (Erenna, Singulex, CA) | Significantly elevated in AD compared with controls |
| Babic ´Leko et al (2016)36 | 109 | 43 | 9 | ELISA | Significantly higher in AD compared to MCI and control subjects |
| Tarawneh et al (2016)41 | 95 | / | 207 | Microparticle based immunoassay (Erenna, Singulex, CA) | Significantly elevated in AD compared with controls |
| Höglund et al (2017)47 | / | / | 129 | ELISA | No difference between high CSF Aβ and low CSF Aβ groups |
| Muszyn ´ski et al (2017)48 | 45 | 18 | 23 | ELISA | Significantly elevated only in AD group in comparison to control subjects |
| Sutphen et al (2018)42 | 16 | 76 | 56 | Microparticle based immunoassay (Erenna, Singulex, CA) | Baseline levels elevated in the MCI Aβ+ and AD Aβ+ groups compared with MCI Aβ- and controls Aβ- groups; Longitudinally decreased in AD Aβ+ groups |
| Zhang et al (2018)44 | 18 | 24 sMCI, 47 pMCI |
32 | Microparticle based immunoassay (Erenna, Singulex, CA) | Significantly elevated in AD and pMCI groups compared with control and sMCI groups |
Abbreviations: AD, Alzheimer’s disease; sMCI, stable mild cognitive impairment; pMCI, progressive mild cognitive impairment.
In our current study, we investigated the concentration of CSF VILIP-1 between APOE ε4 carriers and non-carriers in the elderly subjects. It was observed that CSF VILIP-1 level was statistically significantly elevated in APOE ε4 carriers than non-carriers. The concentration of CSF VILIP-1 was linked to CSF-tau and P-tau concentrations. What is more, CSF VILIP-1 level was substantially related to APOE ε4 genotype, regardless of age, gender, education, MMSE, CDR-SB, RAVLT-immediate recall, RAVLT-delayed recall, CSF Aβ42 and P-tau, volumes of hippocampus and entorhinal cortex. Notably, these findings are consistent with the previous follow-up study that in healthy individuals CSF VILIP-1 still has predictive value for future cognitive decline.9,46
APOE ε4 ranks top of genetic risk factors in the progression of sporadic AD.2 However, the precise underlying pathophysiologic mechanisms of APOE ε4 in the development of AD remain debated. The hypothesis that APOE ε4 carriers may play a role in neuron injury and has values in predicting rates of cognitive decline was supported by our findings. That CSF VILIP-1 level was elevated among the APOE ε4 allele carriers suggesting that APOE may influence VILIP-1 level. In this study, we found a notable association between CSF VILIP-1 and CSF-tau protein. As the cross-sectional design does not indicate causality, future prospective studies were warranted.
There were a few limitations to our study. Firstly, the evaluation of the prospective changes of VILIP-1 levels over time was not conducted due to the cross-sectional design applied in our study. Further longitudinal researches are in needed to confirm the conclusions. Secondly, when interpreting our results, the restricted sample inclusion in ADNI database should be considered. The relationship between APOE ε4 and CSF VILIP-1 will warrant further investigations in prospective study. In summary, APOE ε4 carriers had elevated CSF VILIP-1 levels in comparison with APOE ε4 non-carriers in preclinical AD.
Conclusion
Our findings suggested that APOE ε4 might affect CSF VILIP-1 level in preclinical AD, indicating an important role of APOE ε4 in neuron injury leading to AD.
Acknowledgments
Data collection and sharing for this project was funded by the Alzheimer’s Disease Neuroimaging Initiative (ADNI) (National Institutes of Health Grant U01 AG024904) and DOD ADNI (Department of Defense award number W81XWH-12-2-0012). ADNI is funded by the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and through generous contributions from the following: AbbVie, Alzheimer’s Association; Alzheimer’s Drug Discovery Foundation; Araclon Biotech; BioClinica, Inc.; Biogen; Bristol-Myers Squibb Company; CereSpir, Inc.; Cogstate; Eisai Inc.; Elan Pharmaceuticals, Inc.; Eli Lilly and Company; EuroImmun; F. Hoffmann-La Roche Ltd and its affiliated company Genentech, Inc.; Fujirebio; GE Healthcare; IXICO Ltd.; Janssen Alzheimer Immunotherapy Research & Development, LLC.; Johnson & Johnson Pharmaceutical Research & Development LLC.; Lumosity; Lundbeck; Merck & Co., Inc.; Meso Scale Diagnostics, LLC.; NeuroRx Research; Neurotrack Technologies; Novartis Pharmaceuticals Corporation; Pfizer Inc.; Piramal Imaging; Servier; Takeda Pharmaceutical Company; and Transition Therapeutics. The Canadian Institutes of Health Research is providing funds to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the National Institutes of Health (www.fnih.org). The grantee organization is the Northern California Institute for Research and Education, and the study is coordinated by the Alzheimer’s Therapeutic Research Institute at the University of Southern California. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of Southern California.
Funding Statement
This work was supported by grants from the National Key Research and Development Program (2016YFC1306505), the National Natural Science Foundation of China (81873778, 81501097), the Shanghai Municipal Education Commission-Gaofeng Clinical Medicine Grant (20152201).
Data Sharing Statement
Data used in preparation of this article were obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (adni.loni.usc.edu). As such, the investigators within the ADNI contributed to the design and implementation of ADNI and/or provided data but did not participate in the analysis or writing of this report. A complete listing of ADNI investigators can be found at: http://adni.loni.usc.edu/wp-content/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf.
Ethical Approval
This study was carried out in accordance with the recommendations of each ADNI site. The protocol was approved by the ADNI. All subjects gave written informed consent in accordance with the Declaration of Helsinki.
Disclosure
All authors claim that there are no conflicts of interest in this work.
References
- 1.Verghese PB, Castellano JM, Holtzman DM. Apolipoprotein E in Alzheimer’s disease and other neurological disorders. Lancet Neurol. 2011;10(3):241–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Corder EH, Saunders A, Strittmatter W, et al. Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. Science. 1993;261(5123):921–923. doi: 10.1126/science.8346443 [DOI] [PubMed] [Google Scholar]
- 3.Khachaturian AS, Corcoran CD, Mayer LS, Zandi PP, Breitner JC Apolipoprotein E epsilon4 count affects age at onset of Alzheimer disease, but not lifetime susceptibility: the Cache County Study. Arch Gen Psychiatry. 2004;61(5):518–524. doi: 10.1001/archpsyc.61.5.518 [DOI] [PubMed] [Google Scholar]
- 4.Jack CR Jr., Bennett DA, Blennow K, et al. A/T/N: an unbiased descriptive classification scheme for Alzheimer disease biomarkers. Neurology. 2016;87(5):539–547. doi: 10.1212/WNL.0000000000002923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Braunewell KH, Klein-Szanto AJK. Visinin-like proteins (VSNLs): interaction partners and emerging functions in signal transduction of a subfamily of neuronal Ca2+ -sensor proteins. Cell Tissue Res. 2009;335(2):301–316. doi: 10.1007/s00441-008-0716-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Groblewska M, Muszyński P, Wojtulewska-Supron A, et al. The role of visinin-like protein-1 in the pathophysiology of Alzheimer’s disease. J Alzheimers Dis. 2015;47(1):17–32. doi: 10.3233/JAD-150060 [DOI] [PubMed] [Google Scholar]
- 7.Laterza OF, Modur VR, Crimmins DL, et al. Identification of novel brain biomarkers. Clin Chem. 2006;52(9):1713–1721. doi: 10.1373/clinchem.2006.070912 [DOI] [PubMed] [Google Scholar]
- 8.Lee J-M, Blennow K, Andreasen N, et al. The brain injury biomarker VLP-1 is increased in the cerebrospinal fluid of Alzheimer disease patients. Clin Chem. 2008;54(10):1617–1623. doi: 10.1373/clinchem.2008.104497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tarawneh R, D’Angelo G, Macy E, et al. Visinin-like protein-1: diagnostic and prognostic biomarker in Alzheimer disease. Ann Neurol. 2011;70(2):274–285. doi: 10.1002/ana.22448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tarawneh R, Lee J-M, Ladenson JH, et al. CSF VILIP-1 predicts rates of cognitive decline in early Alzheimer disease. Neurology. 2012;78(10):709–719. doi: 10.1212/WNL.0b013e318248e568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Riddell DR, Zhou H, Atchison K, et al. Impact of apolipoprotein E (ApoE) polymorphism on brain ApoE levels. J Neurosci. 2008;28(45):11445–11453. doi: 10.1523/JNEUROSCI.1972-08.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim J, Jiang H, Park S, et al. Haploinsufficiency of human APOE reduces amyloid deposition in a mouse model of amyloid-beta amyloidosis. J Neurosci. 2011;31(49):18007–18012. doi: 10.1523/JNEUROSCI.3773-11.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liao F, Hori Y, Hudry E, et al. Anti-ApoE antibody given after plaque onset decreases Abeta accumulation and improves brain function in a mouse model of Abeta Amyloidosis. J Neurosci. 2014;34(21):7281–7292. doi: 10.1523/JNEUROSCI.0646-14.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mahley RW, Huang Y. Apolipoprotein e sets the stage: response to injury triggers neuropathology. Neuron. 2012;76(5):871–885. doi: 10.1016/j.neuron.2012.11.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhao N, Liu -C-C, Qiao W, et al. Apolipoprotein E, receptors, and modulation of Alzheimer’s disease. Biol Psychiatry. 2018;83(4):347–357. doi: 10.1016/j.biopsych.2017.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- 17.Mohs RC, Knopman D, Petersen RC, et al. Development of cognitive instruments for use in clinical trials of antidementia drugs: additions to the Alzheimer’s Disease Assessment Scale that broaden its scope. The Alzheimer’s Disease Cooperative Study. Alzheimer Dis Assoc Disord. 1997;11(Suppl 2):S13–21. doi: 10.1097/00002093-199700112-00003 [DOI] [PubMed] [Google Scholar]
- 18.Morris JC. The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology. 1993;43(11):2412–2414. doi: 10.1212/WNL.43.11.2412-a [DOI] [PubMed] [Google Scholar]
- 19.Estevez-Gonzalez A, Kulisevsky J, Boltes A, et al. Rey verbal learning test is a useful tool for differential diagnosis in the preclinical phase of Alzheimer’s disease: comparison with mild cognitive impairment and normal aging. Int J Geriatr Psychiatry. 2003;18(11):1021–1028. doi: 10.1002/gps.1010 [DOI] [PubMed] [Google Scholar]
- 20.Reitan RM. The relation of the trail making test to organic brain damage. J Consult Psychol. 1955;19(5):393–394. doi: 10.1037/h0044509 [DOI] [PubMed] [Google Scholar]
- 21.Domoto-Reilly K, Sapolsky D, Brickhouse M, et al. Naming impairment in Alzheimer’s disease is associated with left anterior temporal lobe atrophy. Neuroimage. 2012;63(1):348–355. doi: 10.1016/j.neuroimage.2012.06.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brodaty H, Moore CM. The clock drawing test for dementia of the Alzheimer’s type: a comparison of three scoring methods in a memory disorders clinic. Int J Geriatr Psychiatry. 1997;12(6):619–627. doi: [DOI] [PubMed] [Google Scholar]
- 23.Pfeffer RI, Kurosaki TT, Harrah CH, et al. Measurement of functional activities in older adults in the community. J Gerontol. 1982;37(3):323–329. doi: 10.1093/geronj/37.3.323 [DOI] [PubMed] [Google Scholar]
- 24.Cummings JL, Mega M, Gray K, et al. The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology. 1994;44(12):2308. doi: 10.1212/WNL.44.12.2308 [DOI] [PubMed] [Google Scholar]
- 25.Shaw LM, Vanderstichele H, Knapik-Czajka M, et al. Cerebrospinal fluid biomarker signature in Alzheimer’s disease neuroimaging initiative subjects. Ann Neurol. 2009;65(4):403–413. doi: 10.1002/ana.21610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Olsson A, Vanderstichele H, Andreasen N, et al. Simultaneous measurement of beta-amyloid(1-42), total tau, and phosphorylated tau (Thr181) in cerebrospinal fluid by the xMAP technology. Clin Chem. 2005;51(2):336–345. doi: 10.1373/clinchem.2004.039347 [DOI] [PubMed] [Google Scholar]
- 27.Shaw LM, Vanderstichele H, Knapik-Czajka M, et al. Qualification of the analytical and clinical performance of CSF biomarker analyses in ADNI. Acta Neuropathol. 2011;121(5):597–609. doi: 10.1007/s00401-011-0808-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jack CR Jr., Bernstein MA, Fox NC, et al. The Alzheimer’s disease neuroimaging initiative (ADNI): MRI methods. J Magn Reson Imaging. 2008;27(4):685–691. doi: 10.1002/jmri.21049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McDonald CR, McEvoy LK, Gharapetian L, et al. Regional rates of neocortical atrophy from normal aging to early Alzheimer disease. Neurology. 2009;73(6):457–465. doi: 10.1212/WNL.0b013e3181b16431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fischl B, Liu A, Dale AM. Automated manifold surgery: constructing geometrically accurate and topologically correct models of the human cerebral cortex. IEEE Trans Med Imaging. 2001;20(1):70–80. doi: 10.1109/42.906426 [DOI] [PubMed] [Google Scholar]
- 31.Fischl B, Salat DH, Busa E, et al. Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron. 2002;33(3):341–355. doi: 10.1016/S0896-6273(02)00569-X [DOI] [PubMed] [Google Scholar]
- 32.Fleisher A, Grundman M, CR Jack, et al. Sex, Apolipoprotein E epsilon 4 status, and hippocampal volume in mild cognitive impairment. Arch Neurol. 2005;62(6):953–957. doi: 10.1001/archneur.62.6.953 [DOI] [PubMed] [Google Scholar]
- 33.Han X, Jovicich J, Salat D, et al. Reliability of MRI-derived measurements of human cerebral cortical thickness: the effects of field strength, scanner upgrade and manufacturer. Neuroimage. 2006;32(1):180–194. doi: 10.1016/j.neuroimage.2006.02.051 [DOI] [PubMed] [Google Scholar]
- 34.Molinuevo JL, et al. Current state of Alzheimer’s fluid biomarkers. Acta Neuropathol. 2018;136(6):821–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dhiman K, Blennow K, Zetterberg H, et al. Cerebrospinal fluid biomarkers for understanding multiple aspects of Alzheimer’s disease pathogenesis. Cell Mol Life Sci. 2019;76(10):1833–1863. doi: 10.1007/s00018-019-03040-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Babic Leko M, Borovečki F, Dejanović N, et al. Predictive value of cerebrospinal fluid visinin-like protein-1 levels for Alzheimer’s disease early detection and differential diagnosis in patients with mild cognitive impairment. J Alzheimers Dis. 2016;50(3):765–778. doi: 10.3233/JAD-150705 [DOI] [PubMed] [Google Scholar]
- 37.Luo X, Hou L, Shi H, et al. CSF levels of the neuronal injury biomarker visinin-like protein-1 in Alzheimer’s disease and dementia with Lewy bodies. J Neurochem. 2013;127(5):681–690. doi: 10.1111/jnc.12331 [DOI] [PubMed] [Google Scholar]
- 38.Tarawneh R, Head D, Allison S, et al. Cerebrospinal fluid markers of neurodegeneration and rates of brain atrophy in early Alzheimer disease. JAMA Neurol. 2015;72(6):656–665. doi: 10.1001/jamaneurol.2015.0202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mroczko B, Groblewska M, Zboch M, et al. Evaluation of visinin-like protein 1 concentrations in the cerebrospinal fluid of patients with mild cognitive impairment as a dynamic biomarker of Alzheimer’s disease. J Alzheimers Dis. 2015;43(3):1031–1037. doi: 10.3233/JAD-141050 [DOI] [PubMed] [Google Scholar]
- 40.Braunewell KH. The visinin-like proteins VILIP-1 and VILIP-3 in Alzheimer’s disease-old wine in new bottles. Front Mol Neurosci. 2012;5:20. doi: 10.3389/fnmol.2012.00020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tarawneh R, D’Angelo G, Crimmins D, et al. Diagnostic and prognostic utility of the synaptic marker neurogranin in Alzheimer disease. JAMA Neurol. 2016;73(5):561–571. doi: 10.1001/jamaneurol.2016.0086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sutphen CL, McCue L, Herries EM, et al. Longitudinal decreases in multiple cerebrospinal fluid biomarkers of neuronal injury in symptomatic late onset Alzheimer’s disease. Alzheimers Dement. 2018;14(7):869–879. doi: 10.1016/j.jalz.2018.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Olsson B, Lautner R, Andreasson U, et al. CSF and blood biomarkers for the diagnosis of Alzheimer’s disease: a systematic review and meta-analysis. Lancet Neurol. 2016;15(7):673–684. doi: 10.1016/S1474-4422(16)00070-3 [DOI] [PubMed] [Google Scholar]
- 44.Zhang H, Ng KP, Therriault J, et al. Cerebrospinal fluid phosphorylated tau, visinin-like protein-1, and chitinase-3-like protein 1 in mild cognitive impairment and Alzheimer’s disease. Transl Neurodegener. 2018;7(1):23. doi: 10.1186/s40035-018-0127-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kester MI, Teunissen CE, Sutphen C, et al. Cerebrospinal fluid VILIP-1 and YKL-40, candidate biomarkers to diagnose, predict and monitor Alzheimer’s disease in a memory clinic cohort. Alzheimers Res Ther. 2015;7(1):59. doi: 10.1186/s13195-015-0142-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sutphen CL, Jasielec MS, Shah AR, et al. Longitudinal cerebrospinal fluid biomarker changes in preclinical alzheimer disease during middle age. JAMA Neurol. 2015;72(9):1029–1042. doi: 10.1001/jamaneurol.2015.1285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hoglund K, Kern S, Zettergren A, et al. Preclinical amyloid pathology biomarker positivity: effects on tau pathology and neurodegeneration. Transl Psychiatry. 2017;7(1):e995. doi: 10.1038/tp.2016.252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Muszynski P, Kulczyńska-Przybik A, Borawska R, et al. The relationship between markers of inflammation and degeneration in the central nervous system and the blood-brain barrier impairment in Alzheimer’s disease. J Alzheimers Dis. 2017;59(3):903–912. doi: 10.3233/JAD-170220 [DOI] [PubMed] [Google Scholar]