Abstract
Aims
To estimate trends in the prevalence of cannabis use and risk perceptions of cannabis use from 2005–2017 among United States (U.S.) persons with and without depression.
Design
Linear time trends of the prevalence of any, daily, and non-daily past-30-day cannabis use and perceived great risk associated with regular cannabis use (outcome variables) among persons with and without past-year depression were assessed using logistic regression with survey year as the predictor. All analyses were adjusted for gender, age, race/ethnicity, and income; models assessing time trends of cannabis use prevalence were also adjusted for perceived risk.
Setting
The United States: National Survey on Drug Use and Health, an annual cross-sectional survey, 2005–2017 public use data files.
Participants
728,691 persons age ≥12 years.
Measurements
Self-report of any, daily, and non-daily past-30-day cannabis use and perceived great risk associated with regular cannabis use.
Findings
The prevalence of any, daily, and non-daily cannabis use in the past month was higher among those with depression versus those without (e.g., 2017 for any use: 18.94% vs. 8.67%; adjusted odds ratio (aOR)=2.17 (95% confidence interval (CI)=1.92, 2.45)). Any, daily, and non-daily cannabis use increased among persons with and without depression from 2005–2017, yet the increase in any (aORs=1.06 vs. 1.05; p=0.008) and daily (aORs=1.10 vs. 1.07; p=0.021) cannabis use adjusted for sociodemographic characteristics was more rapid among those with depression. Perception of great risk associated with regular cannabis use was significantly lower among those with depression (p<0.001) and decreased significantly more rapidly over the study period among persons with depression, compared with those without (aORs=0.89 vs. 0.92; p<0.001).
Conclusions
The prevalence of cannabis use in the U.S. increased from 2005 to 2017 among persons with and without depression and was approximately twice as common among those with depression. Persons with depression experienced a more rapid decrease in perception of risk, which may be related to the more rapid increase in any and daily past-month cannabis use in this group.
Keywords: cannabis, marijuana, depression, major depressive episode, epidemiology, NSDUH
INTRODUCTION
Cannabis is the most commonly used psychoactive substance in the United States (U.S.) and globally [1]. Heavy cannabis use is associated with psychiatric and substance use comorbidities, disability, and psychosocial and health problems [2–6]. The prevalence of cannabis use, including daily cannabis use, has increased significantly in recent years among youth and adults in the U.S. general population [7–9]. This increase has coincided with—and may be at least partially driven by—rapid legalization of cannabis for medicinal and recreational use in the U.S. and other countries, and the seemingly parallel decline in perception of risks associated with cannabis use [7, 8]. Accumulating data suggest that daily/heavy cannabis use is both more common and has potentially more negative outcomes for persons with common mental health problems (e.g., depression), compared with those without mental health problems [10–14].
Major depression is the most common mental health condition in the U.S., with lifetime prevalence of approximately 17% [15, 16] and past-year prevalence of approximately 6–10% [17–19]. Recent data suggest that the prevalence of depression is also on the rise in the U.S., especially among young persons [20]. Historically, both clinical and epidemiologic studies have found that cannabis use is consistently more prevalent among persons with depression than among those without depression [21–24]. Meta-analyses indicate that there is evidence for cannabis use—and heavy use, in particular—being causally related to the onset of affective disorders, including depression [21, 25]. Although the literature on the potential impact of cannabis use among persons with depression remains relatively scarce—and no randomized controlled trials on the use of cannabis among persons with depression have been conducted—cannabis use has been associated with harmful impact on the course of depression, especially among adolescent-onset users [26]. Additionally, cannabis use appears to promote the progression of depressive symptoms [27, 28], and heavy cannabis use has been associated with less successful depression treatment [27] and increased dysphoria in response to tetrahydrocannabidol (THC) administration among persons with depression [29, 30]. Cannabis use among young persons has also been linked to increased likelihood of suicidal ideation and attempts [12, 31]. Increased depressive symptomatology has been noted among heavy cannabis users [23, 32]. Given the increasing normalization of cannabis use within the U.S., it is conceivable that the relationship between depression and cannabis use, or the disparity in cannabis use by depression status, may be changing (i.e., the strength of the relationship may be weakening as cannabis use becomes more mainstream). It is also not known whether cannabis use may be increasing more rapidly among those with depression, or whether heavier or regular use, which have historically been more common among those with depression [12], may be increasing disproportionately among those with depression. Estimating whether cannabis use—especially at higher frequencies—has increased disproportionately among persons with depression is needed to understand whether and to what degree changes in use may be concentrated in certain vulnerable segments of the population.
There are numerous possible explanations that have been put forward as to why cannabis use may be more common among persons with depression than among those without depression. These include self-medication of depression symptoms, cannabis use increasing the risk of depression, and common risk factors for both (e.g., tobacco use) leading to the co-occurrence of depression and cannabis use [12, 21, 22, 33]. Yet, these reasons would not explain why there may be a disproportionate increase in cannabis use among persons with depression versus those without in the U.S. at this time. One potential factor that could explain this disparity is a difference in risk-taking and risk perceptions. Indeed, greater risk-taking behavior has consistently been reported among persons with mental health problems [22]. There is also an inverse relationship between cannabis use and perceptions of its harmfulness [7, 34, 35]. Moreover, declining perceptions of risk associated with cannabis use have been documented in the literature among the general population [7, 8]. It is not known, however, whether perception of risk associated with cannabis use differs between persons with and without mental health conditions. If so, this systematic difference in perception could reflect one potential factor that may contribute to a differential rate of increase in cannabis use by depression status. Perception of risk is a modifiable factor that could be addressed through education and intervention.
The present study sought to begin to fill these gaps in the literature. First, the study estimated the prevalence of current (i.e., any past-30-day) cannabis use in 2017 among those with past-year depression compared to those without past-year depression in the U.S. overall and stratified by sociodemographic characteristics. Second, the study estimated trends in the prevalence of any past-30-day cannabis use, daily, and non-daily cannabis use among persons with and without past-year depression from 2005 to 2017. Third, the study examined perceived risk associated with regular cannabis use among those with and without depression, and estimated trends in the perception of risk associated with cannabis use among those with and without depression from 2005 to 2017.
METHODS
Design and participants
Data were obtained from the 2005–2017 National Survey on Drug Use and Health (NSDUH) public use data files, for a combined total sample size of 728,691 individuals. The NSDUH is sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA) and is designed to provide estimates of the prevalence of extra-medical use (i.e., use of drugs that are obtained outside of the formal medical system and/or drugs used in ways not directed by a medical professional) of legal and illegal drugs in the household population of the U.S., age 12 and older. The survey employs a 50-state design with an independent multistage area probability sample for each of the 50 states and the District of Columbia. Informed consent was obtained before the start of every interview. Participants were given a description of the study, read a statement describing the legislation that assures the confidentiality of any information they provide, and assured that participation in the study was voluntary. Surveys were administered by computer-assisted personal interviewing (CAPI) conducted by an interviewer and audio computer-assisted self-interviewing (ACASI). Respondents were offered a U.S. $30 incentive payment for participation. The present analyses are based on de-identified data that is exempt from Institutional Review Board review.
Sampling weights for the NSDUH were computed to control for unit-level and individual-level non-response and were adjusted to ensure consistency with population estimates obtained from the U.S. Census Bureau. In order to use data from the 13 years of combined data, a new weight was created upon aggregating the 13 datasets by dividing the original weight by the number of data sets combined. Further descriptions of the NSDUH are found elsewhere [36].
Measures
Sociodemographic variables
Sociodemographic variables included gender (male, female), race/ethnicity (White, Black, Hispanic, Other (i.e., Native American/Alaska Native; Native Hawaiian/Other Pacific Islander; Asian; more than 1 race)), age (12–17, 18–25, 26+), marital status (married, widowed/divorced/separated, never married), and total annual family income (<$20,000, $20,000-$74,999, $75,000+).
Cannabis use variables
Participants indicating past-year cannabis use reported the number of days they used cannabis in the past 30 days. Participants who reported using cannabis on 25 days or greater were classified as “daily cannabis users,” while those reporting use on <25 days were classified as “non-daily cannabis users,” which was reflected in a dichotomous variable. Individuals reporting 0 days of cannabis use within the past 30 days were classified as non-users (i.e., non-past-month users). This cannabis use status classification scheme has been used in prior research [7, 9, 37].
Perceived risk associated with regular cannabis use
All participants were asked about the level of risk they perceived being associated with regular cannabis use (i.e., smoking cannabis once or twice a week): “How much do people risk harming themselves physically and in other ways when they smoke [cannabis] once or twice a week?” Response options included “no risk”, “slight risk”, “moderate risk”, and “great risk”. As in prior analyses [7, 8, 38], perceived risk was dichotomized as “perceived great risk” versus “other perceived risk”.
Depression
Depression status was defined as experiencing at least five out of nine Diagnostic and Statistical Manual of Mental Disorders, 4th. Edition (DSM-IV) clinical features [39] for a Major Depressive Episode, where at least one criterion is depressed mood or loss of interest or pleasure in daily activities. The questions specifically referred to “the worst or most recent period of time when (the respondent) experienced symptoms.” Individuals who reported having these symptoms within the past 12 months—for a period of two weeks or longer—were considered to have had past-year depression.
Statistical analysis
Data were weighted to reflect the complex design of the NSDUH sample and were analyzed with Stata SE, version 13.0 software. These findings did not derive from pre-registered analyses and the analyses should be considered exploratory. We used Taylor series estimation methods (Stata “svy” commands) to obtain proper standard error estimates for the cross-tabulations. First, we examined the combined prevalence of any past-30-day cannabis use by depression status in survey year 2017 by sociodemographic characteristics and perceived risk of regular cannabis use. Next, we examined the prevalence of perceived great risk associated with regular cannabis use, as well as the prevalence of any, daily, and non-daily cannabis use among persons with and without past-year depression across time, from 2005 to 2017.
Linear time trends of daily and non-daily cannabis use were assessed using logistic regression models with continuous year as the predictor. Multivariable logistic regression was then used to adjust for sociodemographic variables (i.e., gender, age, race/ethnicity, income) and perceived risk associated with regular cannabis use. Within these analyses, odds ratios indicate the slope of the increase/decrease (i.e., rapidity of change) in daily and non-daily cannabis use between 2005 and 2017. Furthermore, models with year-by-depression status interaction terms, and F-tests to test the significance of these interactions, were used to assess differential time trends (i.e., differences in the rapidity of change between persons with depression versus without depression). An alpha level of 0.05 was used for all analyses.
RESULTS
Current cannabis use among persons with and without past-year depression, overall and by sociodemographic characteristics
In 2017, the prevalence of current (past-30-day) cannabis use was more than twice as common among participants with past-year depression than among those without past-year depression (18.94% vs. 8.67%; p<0.001). Among sociodemographic subgroups, the highest prevalences of cannabis use were found for men with depression (22.61%), persons age 18–25 with depression (29.71%), Black persons with depression (22.91%), never married persons with depression (22.77%), and respondents who reported no perceived risk associated with regular cannabis use (no depression, 29.90%; with depression 38.61%; Table 1). After adjusting for all sociodemographic characteristics, past-year depression remained associated with more than a two-fold increase in the likelihood of being a current cannabis user (adjusted odds ratio (aOR)=2.17, 95% confidence interval (CI)=1.92, 2.45; Table 1).
Table 1.
The association between past-30-day cannabis use with past-year and no past-year depression, by sociodemographic characteristics, National Survey on Drug Use and Health 2017
| Unadjusted prevalence of cannabis use | ||||||
|---|---|---|---|---|---|---|
| No past-year MDE | Past-year MDE | Past-year MDE vs. no past-year MDE | Past-year MDE vs. no past-year MDE | |||
| Characteristic | wt% (SE) | wt% (SE) | OR (95% CI) | pinta | aORb (95% CI) | pinta |
| Total sample | 8.67 (0.20) | 18.94 (0.78) | 2.46 (2.12, 2.77) | <0.001 | 2.17 (1.92, 2.45) | <0.001 |
| Gender | ||||||
| Male | 11.09 (0.33) | 22.61 (1.69) | 2.34 (1.92, 2.86) | Ref | 1.81 (1.45, 2.22) | Ref |
| Female | 6.28 (0.25) | 16.98 (0.79) | 3.05 (2.65, 3.51) | 0.028 | 2.42 (2.10, 2.79) | 0.008 |
| Age | ||||||
| 12–17 | 5.69 (0.29) | 12.27 (0.96) | 2.32 (1.88, 2.86) | Ref | 2.38 (1.90, 2.99) | Ref |
| 18–25 | 20.33 (0.44) | 29.71 (1.45) | 1.66 (1.42, 1.93) | 0.009 | 1.70 (1.45, 2.00) | 0.001 |
| 26+ | 7.26 (0.22) | 16.92 (1.01) | 2.60 (2.23, 3.04) | 0.352 | 2.31 (1.94, 2.74) | 0.132 |
| Race/Ethnicity | ||||||
| White | 8.96 (0.23) | 18.84 (0.99) | 2.36 (2.07, 2.68) | Ref | 2.04 (1.77, 2.34) | Ref |
| Black | 10.38 (0.44) | 22.91 (2.42) | 2.56 (1.92, 3.43) | 0.618 | 2.68 (2.00, 3.61) | 0.210 |
| Hispanic | 7.44 (0.38) | 16.72 (2.01) | 2.50 (1.81, 3.45) | 0.729 | 2.22 (1.60, 3.09) | 0.289 |
| Other | 6.54 (0.53) | 19.28 (2.99) | 3.41 (2.33, 5.00) | 0.069 | 2.54 (1.68, 3.84) | 0.152 |
| Marital status | ||||||
| Married | 4.96 (0.23) | 10.86 (1.32) | 2.33 (1.71, 3.18) | Ref | 2.46 (1.81, 3.34) | Ref |
| Widowed/divorced/separated | 6.65 (0.48) | 19.47 (2.39) | 3.40 (2.45, 4.70) | 0.107 | 3.45 (2.49, 4.77) | 0.188 |
| Never married | 15.12 (0.38) | 22.77 (1.03) | 1.65 (1.43, 1.91) | 0.046 | 1.84 (1.59, 2.13) | 0.102 |
| Income | ||||||
| <$20,000 | 12.30 (0.70) | 24.52 (1.93) | 2.32 (1.78, 3.01) | Ref | 2.23 (1.73, 2.87) | Ref |
| $20–74,999 | 8.67 (0.29) | 18.53 (0.99) | 2.39 (2.06, 2.79) | 0.809 | 2.21 (1.87, 2.60) | 0.968 |
| $75,000+ | 7.27 (0.29) | 15.52 (1.22) | 2.34 (1.91, 2.88) | 0.948 | 2.07 (1.65, 2. 60) | 0.495 |
| Perceived risk of twice weekly cannabis use | ||||||
| No risk | 29.90 (0.66) | 38.61 (1.67) | 1.47 (1.26, 1.72) | Ref | 1.45 (1.24, 1.71) | Ref |
| Slight risk | 10.43 (0.51) | 20.04 (1.45) | 2.15 (1.73, 2.68) | 0.009 | 1.97 (1.55, 2.51) | 0.044 |
| Moderate risk | 2.41 (0.21) | 5.32 (1.01) | 2.28 (1.45, 3.59) | 0.058 | 2.06 (1.29, 3.27) | 0.143 |
| Great risk | 0.68 (0.01) | 1.61 (0.54) | 2.38 (1.09, 5.20) | 0.224 | 2.00 (0.89, 4.49) | 0.332 |
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; MDE, Major Depressive Episode; OR, odds ratio; SE, standard error; wt%, weighted percentage
pint = p-value from t-test for product term beta=0; test for multiplicative interaction
Adjusted for all other variables listed in the table (except for risk perceptions), and calendar year (categorical)
In adjusted models, the strength of the relationship between depression and cannabis use in 2017 differed significantly by gender, age, and risk perceptions. The association between past-year depression and past-month cannabis use was stronger among women (aOR=2.42, 95% CI=2.10, 2.79) versus men (aOR=1.81, 95% CI=1.45, 2.22); interaction term aOR=1.37, 95% CI=1.09, 1.74). Associations between depression and cannabis use were stronger among individuals age 12–17 (aOR=2.38, 95% CI=1.90, 2.99) than among persons age 18–25 (aOR=1.70, 95% CI=1.45, 2.00; interaction term aOR=0.64, 95% CI=0.49, 0.82). Last, the association between depression and cannabis use was stronger among persons perceiving slight risk associated with regular cannabis use (aOR=1.97, 95% CI=1.55, 2.51) as compared to those who perceived no risk associated with use (aOR=1.45, 95% CI=1.24, 1.71; interaction term aOR=1.35, 95% CI=1.01, 1.80).
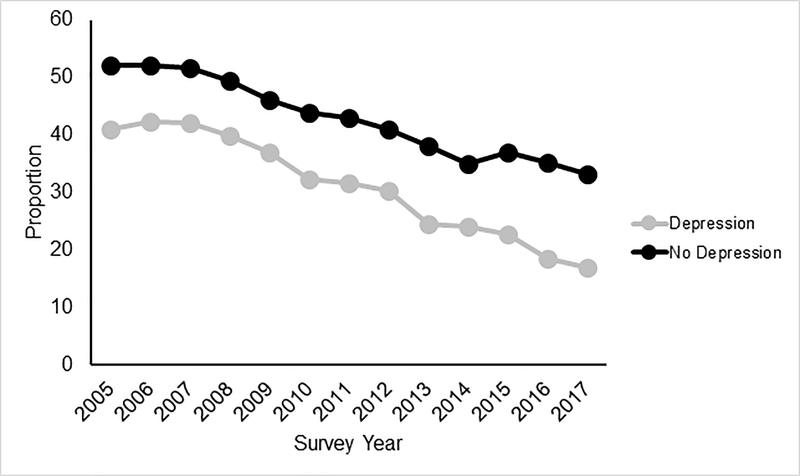
Perceived risk associated with regular cannabis use among persons with and without depression from 2005–2017
In 2017, the prevalence of perceived great risk of regular cannabis use was significantly lower among persons with versus without depression (17.07% vs. 33.13%; p<0.001; Supplemental Table 1). Between survey years 2005 and 2017, the prevalence of perceived great risk declined significantly among both persons with and without depression (p’s<0.001). The rate of change in the prevalence of perceived great risk associated with regular cannabis use was more rapid among persons with depression in unadjusted analyses (ORs=0.90 vs. 0.93; F(1, 110)=68.43; p<0.001) and after adjusting for sociodemographic characteristics (aORs=0.89 vs. 0.92; F(1, 110)=59.28; p<0.001).
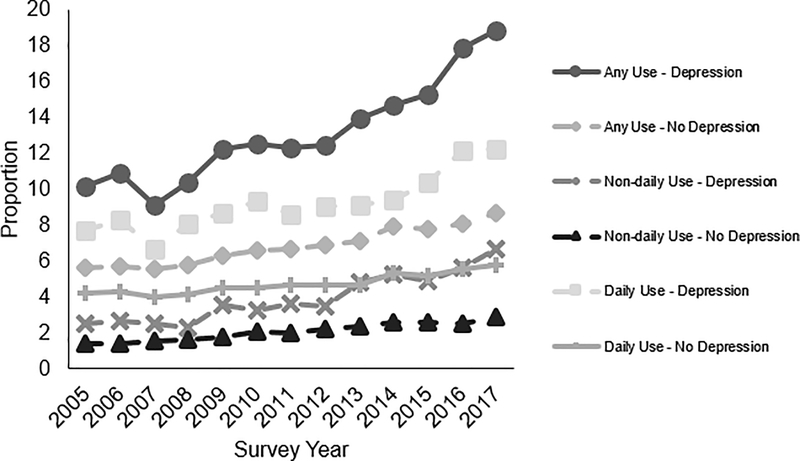
Any cannabis use among persons with and without depression from 2005–2017
In every year of the study period including 2017, past-30-day cannabis use was more common among persons with depression versus those without (2017: 18.84% vs. 8.67%; p<0.001; Supplemental Table 2a). Between 2005 and 2017, the prevalence of cannabis use increased significantly among persons with (10.19% vs. 18.84%; p<0.001) and without past-year depression (5.65% vs. 8.67%; p<0.001). The rate of increase in prevalence of cannabis use was significantly more rapid among persons with depression than among persons without depression when adjusting for sociodemographic characteristics (aOR=1.06 vs. 1.05; F(1, 110)=7.21; p=0.008) and perceived great risk associated with cannabis use (aORs=1.03 vs. 1.01; F(1, 110)=9.23; p=0.003).
Daily cannabis use among persons with and without depression from 2005–2017
In every year of the study period including 2017, past-30-day daily cannabis use was more common among persons with depression as compared to those without depression (2017: 6.66% vs. 2.87%; p<0.001; Supplemental Table 2b). From 2005 to 2017, the prevalence of past-year daily cannabis use increased significantly among both persons with (2.50% vs. 6.66%; p<0.001) and without (1.42% vs. 2.87%; p<0.001) past-year depression. The rate of increase in prevalence of daily cannabis use was significantly more rapid among persons with depression than persons without depression in the unadjusted model (ORs=1.10 vs. 1.06; F(1, 110)=8.90; p=0.004), when adjusting for sociodemographic characteristics (aORs=1.10 vs. 1.07; F(1,110)=5.50; p=0.021), and when adjusting for perceived great risk (aORs=1.06 vs. 1.03; F(1, 110)=7.35; p=0.008).
Non-daily cannabis use among persons with and without depression from 2005–2017
Similar to daily cannabis use, the prevalence of past-30-day non-daily cannabis use was greater among persons with depression versus those without depression for every year of the study period including the most recent year (2017: 12.27% vs. 5.80%; p<0.001; Supplemental Table 2c). Non-daily cannabis use increased between 2005 and 2017 among those with depression (7.69% vs. 12.27%; p<0.001) and among those without depression (4.23% vs. 5.80%; p<0.001). The rate of increase in prevalence of non-daily cannabis use was significantly more rapid among those with depression versus those without in the unadjusted model (ORs=1.05 vs. 1.03; F(1,110)=5.09; p=0.026), but not in either of the adjusted models.
DISCUSSION
The present study examined trends over a 13-year period in the prevalence of cannabis use among persons with and without past-year depression in the U.S. The prevalence of any past-month cannabis use, as well as both daily and non-daily cannabis use, increased over time between 2005 and 2017 among those with and without depression. The increase in the prevalence of any past-30-day and daily cannabis use was significantly more rapid among persons with depression; this has not previously been reported. Given recent findings suggesting that heavy cannabis use may be especially harmful among persons with mental health vulnerabilities [40], these findings potentially reflect newly emerging trends that warrant tracking.
Disparities in the prevalence of cannabis use by depression status were notable: both daily and non-daily cannabis use remained approximately twice as prevalent among those with depression relative to those without depression in all survey years. In 2017, the prevalence of current (i.e., past-30-day) cannabis use was approximately twice as high among persons with past-year depression than among those without depression; this difference was fairly consistent across sociodemographic groups. However, the magnitude of disparities in cannabis use should also be noted. For instance, much of the current cannabis use appears to occur among persons age 18–25: one-fifth (20.33%) of those in this age group without depression and nearly one-third (29.71%) of those with depression report current cannabis use. Cannabis use among young people is concerning for a number of reasons, including potential impact on brain development, which is ongoing into young adulthood [41]. Additionally, more than one-fifth (22.61%) of males with past-year depression report current cannabis use. These findings are roughly consistent with those indicating higher prevalence of cannabis use among younger and male persons [8, 42]. Collectively, our findings may be relevant in terms of intervention development and implementation, particularly when attempting to identify and target subgroups that may be at greatest risk for cannabis use.
This study also examined 13-year trends in the perceptions of risk related to cannabis use among persons with and without past-year depression. A novel finding here was that perception of great risk associated with regular cannabis use was significantly lower among those with depression versus those without depression. In addition, the perception of risk declined more rapidly among those with depression. These findings provide some new clues to a potential modifiable factor that may be contributing to the disproportionate use of cannabis and speed of increase in cannabis use among those with depression over the past decade [43, 44]. Lower perception of risk associated with cannabis use is associated with higher cannabis use incidence and prevalence [45, 46], and there is a reciprocal relationship between risk perceptions associated with cannabis use and cannabis use among youth [47, 48]. It may be beneficial to target cannabis-related risk perceptions among persons with depression—potentially via messaging and educational campaigns—in order to reduce the prevalence of cannabis use among this high-risk group, especially among young people. While it is not possible to discern these pathways in this study, it is conceivable that the potential risks associated with cannabis use may be minimized by someone suffering from depression; for example, a) higher risk taking has been noted among persons with depression and other mental health problems generally [49–51]; b) if they perceive that cannabis will help relieve depression, this may lead to minimization of risk along the lines of delay discounting and/or feelings that even if there is risk, it will be worth it to obtain relief; c) for persons with depression, perceived risks may be weighed against those perceived to be associated with taking prescribed antidepressants or other medicines, and this calculation could result in perception of lower risk in this context. Future research should examine whether targeting risk perceptions has a consequential positive impact on cannabis use and whether this benefit is differentially experienced by persons with depression.
Limitations of the present study should be noted. First, data were collected via self-report, which is subject to recall and social desirability biases. The NSDUH utilizes ACASI to mitigate the likelihood of social desirability bias; ACASI was designed to provide respondents with a private and confidential means of responding to questions and to increase honest reporting of illegal drug use and other sensitive behaviors [52]. Additionally, neither route of administration of cannabis, potency and/or type of cannabis strains used, nor reasons for using cannabis are fully detailed. In future work, understanding whether the associations between depression and cannabis use are related to other aspects of cannabis use such as the route of administration of cannabis (e.g., smoked versus vaporized versus edible) or reasons for cannabis use (e.g., medicinal versus recreational) would be helpful in terms of understanding the mechanisms underlying this relationship. Moreover, the present analysis was not able to control for state-level cannabis legalization/medicalization, which is likely to be associated with cannabis use patterns and risk perceptions.
Additionally, given the repeated cross-sectional nature of the NSDUH, we are unable to explore changes within the same individuals over time. Relatedly, we are unable to comment on the directionality of the relationship between cannabis use and depression in the present sample. Longitudinal data would be needed to allow the observation of potentially important trends in depression and cannabis use over time at the population level. Given that NSDUH does not assess motivations for cannabis use, we are unable to determine whether increases in cannabis use may be at least partially explained by attempts to self-medicate depressive symptoms [33, 53, 54]—or, alternately, whether increase in cannabis use are contributing to increases in depressive symptoms. Moreover, this study was conducted in the U.S., potentially limiting the conclusions that can be drawn regarding these associations in an international context.
Conclusions
Our findings provide new evidence suggesting that the prevalence of any past-30-day cannabis use and past-30-day daily cannabis use is increasing more rapidly among U.S. individuals with depression compared with those without depression and that the absolute prevalence of cannabis use is twice as high among persons with depression than among individuals without depression. In addition, our findings highlight several particularly vulnerable subgroups among whom interventions may be most needed (e.g., persons age 18–25 and men) based on their relatively disproportionate high prevalence of cannabis use, particularly among those with depression. Our findings also shed new light on one potential modifiable factor, risk perceptions, which is related to the prevalence of cannabis use. The greater prevalence of cannabis use among those with past-year depression, as well as the growing populations of persons with past-year depression who use cannabis in the U.S. [7–9], point to the need for greater understanding of the subgroups who are disproportionally using cannabis to develop appropriate interventions and make clinical and public health recommendations.
Supplementary Material
Figure 1.
Prevalence of perceived great risk of regular cannabis use, stratified by past-year depression
Figure 2.
Prevalence of past-30-day any, daily, and non-daily cannabis use, stratified by past-year depression
Acknowledgements
Work on this study was supported by grants from the National Institute on Drug Abuse (NIDA) K01DA043413 (LRP) and R01DA02892 (RDG). The funders had no role in study design, data analysis, interpretation of data, or in the writing of the manuscript or the decision to submit the article for publication. All authors were and are independent from funders.
Footnotes
Declaration of competing interest: None.
References
- 1.World Health Organization. The health and social effects of nonmedical cannabis use [Internet]. 2019. [Available from: https://www.who.int/substance_abuse/publications/cannabis_report/en/index5.html.
- 2.Fergusson DM, Boden JM Cannabis use and later life outcomes. Addiction 2008; 103: 969–76; discussion 77–78. [DOI] [PubMed] [Google Scholar]
- 3.Guttmannova K, Kosterman R, White HR, Bailey JA, Lee JO, Epstein M et al. The association between regular marijuana use and adult mental health outcomes. Drug Alcohol Depend 2017; 179: 109–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Suerken CK, Reboussin BA, Egan KL, Sutfin EL, Wagoner KG, Spangler J et al. Marijuana use trajectories and academic outcomes among college students. Drug Alcohol Depend 2016; 162: 137–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Volkow ND, Compton WM, Weiss SRB Adverse health effects of marijuana use. New Engl J Med 2014; 371: 879. [DOI] [PubMed] [Google Scholar]
- 6.Hasin DS, Kerridge BT, Saha TD, Huang B, Pickering R, Smith SM et al. Prevalence and correlates of DSM-5 cannabis use disorder, 2012–2013: findings from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Am J Psychiatry 2016; 173: 588–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pacek LR, Mauro PM, Martins SS Perceived risk of regular cannabis use in the United States from 2002 to 2012: differences by sex, age, and race/ethnicity. Drug Alcohol Depend 2015; 149: 232–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Compton WM, Han B, Jones CM, Blanco C, Hughes A Marijuana use and use disorders in adults in the USA, 2002–14: analysis of annual cross-sectional surveys. Lancet Psychiatry 2016; 3: 954–64. [DOI] [PubMed] [Google Scholar]
- 9.Goodwin RD, Pacek LR, Copeland J, Moeller SJ, Dierker L, Weinberger A et al. Trends in daily cannabis use among cigarette smokers: United States, 2002–2014. Am J Public Health 2018; 108: 137–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weinberger AH, Pacek LR, Sheffer CE, Budney AJ, Lee J, Goodwin RD Serious psychological distress and daily cannabis use, 2008 to 2016: potential implications for mental health? Drug Alcohol Depend 2019; 197: 134–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gobbi G, Atkin T, Zytynski T, Wang S, Askari S, Boruff J et al. Association of cannabis use in adolescence and risk of depression, anxiety, and suicidality in young adulthood: a systematic review and meta-analysis. JAMA Psychiatry 2019; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Silins E, Horwood LJ, Patton GC, Fergusson DM, Olsson CA, Hutchinson DM et al. Young adult sequelae of adolescent cannabis use: an integrative analysis. Lancet Psychiatry 2014; 1: 286–93. [DOI] [PubMed] [Google Scholar]
- 13.Fergusson DM, Boden JM, Horwood LJ Psychosocial sequelae of cannabis use and implications for policy: findings from the Christchurch Health and Development Study. Soc Psychiatry Psychiatr Epidemiol 2015; 50: 1317–26. [DOI] [PubMed] [Google Scholar]
- 14.Borodovsky JT, Budney AJ Cannabis regulatory science: risk-benefit considerations for mental disorders. Int Rev Psychiatry 2018; 30: 183–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kessler RC, Bromet EJ The epidemiology of depression across cultures. Annu Rev Public Health 2013; 34: 119–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005; 62: 593–602. [DOI] [PubMed] [Google Scholar]
- 17.Mojtabai R, Olfson M, Han B National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics 2016; 138: e20161878–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weinberger AH, Gbedemah M, Martinez AM, Nash D, Galea S, Goodwin RD Trends in depression prevalence in the USA from 2005 to 2015: widening disparities in vulnerable groups. Psychol Med 2018; 48: 1308–15. [DOI] [PubMed] [Google Scholar]
- 19.Weinberger AH, Bandiera FC, Leventhal AM, Dierker LC, Gbedemah M, Tidey JW et al. Socioeconomic disparities in smoking among U.S. adults with depression, 2005–2014. Am J Prev Med 2018; 54: 765–75. [DOI] [PubMed] [Google Scholar]
- 20.Goodwin RD, Wall MM, Garey L, Zvolensky MJ, Dierker L, Galea S et al. Depression among current, former, and never smokers from 2005 to 2013: the hidden role of disparities in depression in the ongoing tobacco epidemic. Drug Alcohol Depend 2017; 173: 191–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lev-Ran S, Roerecke M, Le Foll B, George TP, McKenzie K, Rehm J The association between cannabis use and depression: a systematic review and meta-analysis of longitudinal studies. Psychol Med 2014; 44: 797–810. [DOI] [PubMed] [Google Scholar]
- 22.Lucatch AM, Coles AS, Hill KP, George TP Cannabis and mood disorders. Curr Addict Rep 2018; 5: 336–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Degenhardt L, Hall W, Lynskey M Exploring the association between cannabis use and depression. Addiction 2003; 98: 1493–504. [DOI] [PubMed] [Google Scholar]
- 24.Horwood LJ, Fergusson DM, Coffey C, Patton GC, Tait R, Smart D et al. Cannabis and depression: an integrative data analysis of four Australasian cohorts. Drug Alcohol Depend 2012; 126: 369–78. [DOI] [PubMed] [Google Scholar]
- 25.Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, Burke M et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet 2007; 370: 319–28. [DOI] [PubMed] [Google Scholar]
- 26.Lowe DJE, Sasiadek JD, Coles AS, George TP Cannabis and mental illness: a review. Eur Arch Psychiatry Clin Neurosci 2019; 269: 107–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bahorik AL, Leibowitz A, Sterling SA, Travis A, Weisner C, Satre DD Patterns of marijuana use among psychiatry patients with depression and its impact on recovery. J Affect Disord 2017; 213: 168–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moitra E, Anderson BJ, Stein MD Reductions in cannabis use are associated with mood improvement in female emerging adults. Depress Anxiety 2016; 33: 332–8. [DOI] [PubMed] [Google Scholar]
- 29.Mathew RJ, Wilson WH, Tant SR Acute changes in cerebral blood flow associated with marijuana smoking. Acta Psychiatr Scand 1989; 79: 118–28. [DOI] [PubMed] [Google Scholar]
- 30.Ablon SL, Goodwin FK High frequency of dysphoric reactions to tetrahydrocannabinol among depressed patients. Am J Psychiatry 1974; 131: 448–53. [PubMed] [Google Scholar]
- 31.Pedersen W Does cannabis use lead to depression and suicidal behaviours? A population-based longitudinal study. Acta Psychiatr Scand 2008; 118: 395–403. [DOI] [PubMed] [Google Scholar]
- 32.Feingold D, Rehm J, Lev-Ran S Cannabis use and the course and outcome of major depressive disorder: a population based longitudinal study. Psychiatry Res 2017; 251: 225–34. [DOI] [PubMed] [Google Scholar]
- 33.Bolton JM, Robinson J, Sareen J Self-medication of mood disorders with alcohol and drugs in the National Epidemiologic Survey on Alcohol and Related Conditions. J Affect Disord 2009; 115: 367–75. [DOI] [PubMed] [Google Scholar]
- 34.Compton WM, Thomas YF, Conway KP, Colliver JD Developments in the epidemiology of drug use and drug use disorders. Am J Psychiatry 2005; 162: 1494–502. [DOI] [PubMed] [Google Scholar]
- 35.Okaneku J, Vearrier D, McKeever RG, LaSala GS, Greenberg MI Change in perceived risk associated with marijuana use in the United States from 2002 to 2012. Clin Toxicol (Phila) 2015; 53: 151–5. [DOI] [PubMed] [Google Scholar]
- 36.Center for Behavioral Health Statistics and Quality. Behavioral health trends in the United States: results from the 2014 National Survey on Drug Use and Health. 2015. Report No.: SMA 15–4927. [Google Scholar]
- 37.Budney AJ, Moore BA, Vandrey RG, Hughes JR The time course and significance of cannabis withdrawal. J Abnorm Psychol 2003; 112: 393–402. [DOI] [PubMed] [Google Scholar]
- 38.Pacek LR, Towe SL, Hobkirk AL, Nash D, Goodwin RD Frequency of cannabis use and medical cannabis use among persons living with HIV in the United States: findings from a nationally representative sample. AIDS Educ Prev 2018; 30: 169–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th text revision ed Washington, D.C.: American Psychiatric Association; 2000. [Google Scholar]
- 40.Ksir C, Hart CL Cannabis and psychosis: a critical overview of the relationship. Curr Psychiatry Rep 2016; 18: 12. [DOI] [PubMed] [Google Scholar]
- 41.Lubman DI, Cheetham A, Yücel M Cannabis and adolescent brain development. Pharmacol Ther 2015; 148: 1–16. [DOI] [PubMed] [Google Scholar]
- 42.Hasin DS, Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H et al. Prevalence of marijuana use disorders in the United States between 2001–2002 and 2012–2013. JAMA Psychiatry 2015; 72: 1235–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McCambridge J, Strang J The efficacy of single-session motivational interviewing in reducing drug consumption and perceptions of drug-related risk and harm among young people: results from a multi-site cluster randomized trial. Addiction 2004; 99: 39–52. [DOI] [PubMed] [Google Scholar]
- 44.McCambridge J, Strang J Deterioration over time in effect of Motivational Interviewing in reducing drug consumption and related risk among young people. Addiction 2005; 100: 470–8. [DOI] [PubMed] [Google Scholar]
- 45.Parker MA, Anthony JC A prospective study of newly incident cannabis use and cannabis risk perceptions: results from the United States Monitoring the Future study, 1976–2013. Drug Alcohol Depend 2018; 187: 351–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Parker MA, Anthony JC Population-level predictions from cannabis risk perceptions to active cannabis use prevalence in the United States, 1991–2014. Addict Behav 2018; 82: 101–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Grevenstein D, Nagy E, Kroeninger-Jungaberle H Development of risk perception and substance use of tobacco, alcohol and cannabis among adolescents and emerging adults: evidence of directional influences. Subst Use Misuse 2015; 50: 376–86. [DOI] [PubMed] [Google Scholar]
- 48.Salloum NC, Krauss MJ, Agrawal A, Bierut LJ, Grucza RA A reciprocal effects analysis of cannabis use and perceptions of risk. Addiction 2018; 113: 1077–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Testa CR, Steinberg L Depressive symptoms and health-related risk-taking in adolescence. Suicide Life Threat Behav 2010; 40: 298–305. [DOI] [PubMed] [Google Scholar]
- 50.Soleimani MA, Pahlevan Sharif S, Bahrami N, Yaghoobzadeh A, Allen KA, Mohammadi S The relationship between anxiety, depression and risk behaviors in adolescents. Int J Adolesc Med Health 2017; 31. [DOI] [PubMed] [Google Scholar]
- 51.Verger P, Lions C, Ventelou B Is depression associated with health risk-related behaviour clusters in adults? Eur J Public Health 2009; 19: 618–24. [DOI] [PubMed] [Google Scholar]
- 52.Macalino GE, Celentano DD, Latkin C, Strathdee SA, Vlahov D Risk behaviors by audio computer-assisted self-interviews among HIV-seropositive and HIV-seronegative injection drug users. AIDS Educ Prev 2002; 14: 367–78. [DOI] [PubMed] [Google Scholar]
- 53.Haney M, Gunderson EW, Rabkin J, Hart CL, Vosburg SK, Comer SD et al. Dronabinol and marijuana in HIV-positive marijuana smokers. Caloric intake, mood, and sleep. J Acquir Immune Defic Syndr 2007; 45: 545–54. [DOI] [PubMed] [Google Scholar]
- 54.Prentiss D, Power R, Balmas G, Tzuang G, Israelski DM Patterns of marijuana use among patients with HIV/AIDS followed in a public health care setting. J Acquir Immune Defic Syndr 2004; 35: 38–45. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.