Abstract
Borderline personality disorder and substance use disorder co-occur at a high rate. However, little is known about the mechanisms driving this association. This study examined substance use motives for three common substance use disorders among 193 individuals in substance use disorder treatment. We found that the coping motive consistently mediated the relationship between borderline personality and alcohol, cannabis, and prescription opioid use disorders. For this substance use disorder treatment sample, our findings support the self-medication model of substance use, and that interventions aimed at coping related substance use would be helpful among these patients.
Borderline personality disorder (BPD) and substance use disorders (SUD) co-occur at alarmingly high rates (Trull et al., 2018). The BPD and SUD relationship has been noted among adolescents (Stepp, Trull, & Sher, 2005) and adults (Carpenter, Wood, & Trull, 2015; Trull, Sher, Minks-Brown, Durbin, & Burr, 2000) as well as in research examining individuals in clinical populations (Sansone & Sansone, 2011) and the general public (Grant et al., 2008). Additionally, though this relationship has been well documented in the literature, little is known about why BPD and SUD are associated, what potential mechanisms may be underlying the association, and whether there are similarities/differences across substances. Therefore, in the present study, we examined substance use motives, or the reasons why individuals use substances, in a drug specific manner, as mediators of the relationship between BPD features and SUD symptomatology. Understanding how substance use motives may be involved in the BPD and SUD relationship could provide insight that may be relevant to prevention efforts and inform treatment interventions.
BPD is the most common personality disorder with numerous harmful consequences for both individuals and society (American Psychiatric Association [APA], 2013). BPD is characterized by impulsive actions, emotion dysregulation, problems with interpersonal relationships, increased risk for suicide, and disturbed identity (APA, 2013). BPD is most often presented in clinical settings in a categorical framework (either present or not present); however, a substantial evidence base suggests that a dimensional or trait-based approach may be more informative due to overwhelming empirical evidence that BPD exists on a continuum in nature, and due to BPD’s heterogeneous typology (Widiger & Trull, 2007). Although the general prevalence of BPD is quite low (Grant et al., 2008), BPD among individuals in treatment of substance use disorders occurs at troublingly high rates (Trull et al., 2018). Specifically, rates are approximately 2–3% (Trull, Jahng, Tomko, Wood, & Sher, 2010) among the general public, yet among individuals with current SUD the percentage of those with co-occurring BPD is 22.1% (Trull et al., 2018). Likewise, when patients in SUD treatment have co-occurring BPD they report poorer treatment outcomes (Tull & Gratz, 2012). Despite a great deal of research among mental health populations, surprisingly little research has been conducted on individuals in treatment for substance use disorders. This time point offers a unique snapshot into a clinically relevant period when individuals may have begun decreasing drug or alcohol use, and increasing awareness about changes necessary to improve their quality of life (Prochaska, Diclemente, & Norcross, 1993). This is important because this developmental period may provide insight into the disease progression of both BPD and SUD.
Substance use motives offer person-relevant reasoning or desires underlying drug or alcohol use (Cox & Klinger, 1988). Under the motivational framework, Cooper (1994), demonstrated that alcohol use is repeated to meet specific needs. The needs can be either internal or external in valance, and positive or negative (added or removed) in a behavioral context. Research has shown that the motivational framework is important for our understanding of drug specific pathways, both into and out of addiction. The alcohol use motives discovered by Cooper (1994) included coping (internal, negative), social (external, positive), conformity (external, negative), and enhancement (internal, positive). Further, research with cannabis motives, has uncovered a motive for expansion (Simons, Correia, Carey, & Borsari, 1998), and specific to prescription opioids, Jones, Spradlin, Robinson, and Tragesser (2014) found that a motive for physical pain was evident. In a comprehensive review on motives for alcohol, cannabis, and cigarette use, Cooper, Kuntsche, Levitt, Barber, & Wolf, (2016) reported that alcohol and cannabis motives appear to share some similarities, but suggest that future research avoid overgeneralizing across substances and consider the unique psychoactive and phenomenological properties of each drug.
Research specific to BPD and substance use motives has been rare, with only a handful of studies done previously. We found that four previous studies have examined BPD and substance use motives (Chabrol, Ducongé, Casas, Roura, & Carey, 2005; Salatino et al., 2018; Vest, Murphy, & Tragesser, 2018; Chugino et al., 2018). A study of cannabis motives performed among high school and college students in France found that expansion motives were strongly associated with BPD symptoms for boys and girls, coping and social motives were specific to boys, and that enhancement motives were specific to girls (Chabrol, Ducongé, Casas, Roura, & Carey, 2005). Salatino et al. (2018) found that BPD symptoms had a significant prospective relationship with coping and enhancement alcohol use motives among individuals that had been incarcerated in a county jail. Similarly, Chugino et al. (2018) found that coping motives were involved in an “affective pathway” while enhancement motives were involved in a “sensation-seeking pathway” in the relationship between BPD symptoms and alcohol problems in a sample of adolescent girls. Lastly, in a college student sample, Vest and colleagues (2018) found that BPD features were associated with alcohol and cannabis motives for coping and conformity in a similar pattern across gender and substance, but the relationship for all prescription opioid motives was specific to women only. What is clear from the research cited above is that coping appears to be the motive most consistently involved in the relationship between BPD and SUD across college, adolescent, and jail populations. What remains unclear is whether coping motives underlie the BPD and SUD relationship among other high-risk populations, including individuals in treatment for substance use disorder, and whether the pattern is consistent across substances.
In sum, BPD is consistently associated with substance use disorder across drugs and populations. Research has demonstrated that individuals with BPD are more likely to utilize emergency room services and incur negative consequences (Tomko, Trull, Wood, & Sher, 2014). Although there is substantial evidence to suggest that borderline personality is associated with alcohol, cannabis, prescription opioid use, few studies have examined potential mediators of this relationship. Thus, in the current project, we examined substance use motives as mediators of the relationship between borderline personality disorder features and cannabis, alcohol, and prescription opioid use disorder symptomatology among patients in treatment for substance use disorder. Based on previous findings, we predicted the coping motives would be the most consistent mediator across substances.
Methods
Participants and Procedure
Participants included 193 adult patients (Male = 122, Female = 71; MAge = 36.07, SD = 12.56, Range = 18–73) enrolled in SUD treatment in the outpatient level of care in two facilities located in eastern Washington state. Race and ethnic background were reported as 72.0% White (non-Hispanic), 18.7% Hispanic American, 3.6% African American, 3.1% Asian American, and 2.6% Native American. Educational attainment was reported as 56.0% a high school diploma and below, 30.5% some college courses taken with no degree, and 15.5% a college degree. Participants completed an informed consent detailing the voluntary nature of the study and were told that they could desist their involvement in the research project at any time without penalty. Participants were naive to the purpose of the study and were compensated with a $15 gift card. The only requirements for study enrollment were 1) outpatient treatment involvement, 2) age of 18 or greater, and 3) ability to read at the 8th grade level.
The research team conducted the data collection from August 2016 to June 2017. The pen and paper surveys were collected by a master’s level researcher in a recreation room at the treatment center. Participants were seated four feet apart and faculty at the treatment center were prohibited from entering the room while the survey was administered. The survey was generally completed in less than one hour and a researcher was available throughout to answer questions. No personally identifying information was collected as part of the study and the surveys were stored separately from the informed consent paperwork. Although it was a requirement of the study to be enrolled in treatment for a diagnosed substance use disorder, all of the information used in the present study was collected as part of the study and did not require access to patient medical records or treatment center chart notes. Surveys were stored in a locked cabinet in a locked office of the primary investigator.
The treatment center offered assessments, intakes, individual therapy sessions, and group therapy sessions at the outpatient level of care. The counseling consisted of a mixed approach which incorporated motivational interviewing, cognitive behavioral therapy, acceptance and commitment therapy, and other forms of evidence-based treatment practices. This was an abstinence-based program and patients were given random urinalysis tests to assist clinicians in assessing treatment progress. The milieu generally consisted of three-time weekly group sessions and monthly individual sessions. Treatment duration lasted anywhere from 90 days to 24 months depending on motivation, clinical progress, and judicial system involvement. The study design and procedures were approved by the Internal Review Board at Washington State University.
Measures
Borderline Personality Disorder Features
Borderline features were measured with the Personality Assessment Inventory for Borderlines (PIA-BOR; Morey, 1991). The PIA-BOR has been validated among clinical samples (Stein et al., 2007) and offers a reliable dimensional measure of borderline personality. The 24-item measure was scored on a 0 (false, not true at all) to 3 (very true) scale. For the current study, we summed all the items and used a total score. PIA-BOR scale reliability (α = .90) was excellent among our SUD sample. In the current sample, 34.4% (n = 66) scored above the clinical cut-off of 37.
Drinking Motives
Alcohol use motives were measured with the four-factor Drinking Motives Questionnaire-Revised (DMQ-R; Cooper, 1994). Reliability was excellent across all four subscales of coping (α = .93), enhancement (α = .90), social (α = .94), and conformity (α = .90). This DMQ-R is scored on a 1 (never) to 6 (almost always) scale and includes a total of 20 items (each subscale consists of 5 items). The enhancement subscale included items such as “drinking to celebrate a special occasion with friends”, coping included items such as “drinking to forget your problems, conformity included items such as “drinking to celebrate a special occasion with friends”, and social included items such as “drinking because it improves parties and celebrations”.
Cannabis Use Motives
Cannabis use motives were measured using the Marijuana Motives Measure (MMM; (Simons et al., 1998) on the same 0 (never) to 6 (almost always) scale. Although this measure was modeled after Cooper’s (1994) four-factor model, a significant difference is the addition of an expansion (of the mind) motive specific to cannabis use (e.g., using marijuana “because it helps me be more creative and original”). The expansion motive subscale is exclusive to this model and substance. Reliability scores for conformity (α = .92), coping (α = .93), enhancement (α = .93), social (α = .94) and perceptive and cognitive expansion (α = .92) for the present study were excellent.
Prescription Opioid Use Motives
Prescription opioid use motives were measured using the Opioid Prescription Medication Motives Questionnaire (OPMMQ; Jones et al., 2014). This 19-item measure of prescription opioid use motives employs the same 0 (never) to 6 (almost always) scale. This four-factor model measures how often persons use prescription opioids for coping, enhancement, social reasons, and a new motive—to relieve pain. The removal of the conformity and expansion (cannabis) motives for prescription opioids was based on previous research indicating low endorsement of the respective items (Jones et al. 2014). The pain motive was elucidated through confirmatory factor analysis (Jones et al. 2014). Thus, the items for pain (e.g., using prescription opioids “to relieve physical pain,” using prescription opioids “for headaches”) are exclusive to the motive scale for prescription opioids. Reliability scores for coping (α = .97), enhancement (α = .96), social (α = .96), and pain (α = .89) for the present study were also very good.
Substance Use Disorder Measures
We measured substance use disorder symptomatology for alcohol, cannabis, and prescription opioid use with a slightly modified version of the National Survey on Drug Use and Health (NSDUH; SAMSHA, 2010). The NSDUH is a 21-item measure answered in true and false (symptom present or not present) fashion. The 21-items were totaled for each substance separately to give an overall score for alcohol (α = .95), cannabis (α = .92), and prescription opioid use disorders (α = .97). Because the measure was from 2010, it was designed from DSM-IV terminology; consequently, we deleted the question regarding legal consequences and added the following question “In your lifetime, did using alcohol cause you to experience cravings or a strong desire to use alcohol?”. This was done to bring the NSDUH in line with current DSM-5 symptom wording for alcohol use disorder. We made similar adjustments in the cannabis and prescription opioid questionnaires as well.
Data Analyses
Demographics and the correlation table was computed using SPSS v.25 (IBM Corporation, 2017), all other analyses were completed with MPlus v.8.2 (Muthén & Muthén, 2017). Primary hypotheses were evaluated in MPlus using a path analysis that tested a parallel mediation model. In the model, BPD features were the X variable, the substance use motives subscales were the four mediator M variables, and substance use disorder symptom count was the Y outcome variable (Muthén, Muthén, and Asparouhov, 2017). In line with current methodological practices, 95% bias corrected bootstrap confidence intervals with 10,000 iterations were computed to measure the indirect effects. Indirect effects were significant if the bootstrap confidence interval did not contain zero. We wanted to see if the subscales of the substance use motives continued to mediate the BPD to SUD relationship while controlling for the influence of the other substance use motive subscales in a substance specific manner.
Due to the focus on motives for use, we selected only those participants who reported using each substance at least once. All 193 of the participants reported at least one time use of alcohol and cannabis, and 183 participants reported at least one time use of prescription opioids. Missing data were handled using the full information maximum likelihood estimator. Because the mediation models were “just identified”, we did not attend to global fit indices. Because of their historic influence on drug use outcome variables, we controlled for age and sex in all the mediation analyses. We also controlled for treatment location and whether the person was currently prescribed opioids for pain.
Results
Table 1 provides the descriptive statistics and Table 2 offers the bivariate correlations between the study variables. Nearly all study variables showed small to moderate correlations with each other. Coping, enhancement, and social motives for each substance (alcohol, cannabis, and prescription opioids) were, as expected, highly correlated with each other (r = .74 to .87).
Table 1.
All study variable means and standard deviations.
| Variable | Mean | SD | Min./Max. Score |
|---|---|---|---|
| BPD Features | 32.39 | 13.60 | 2.00 – 68.00 |
| Alcohol Motives | |||
| Coping | 3.88 | 1.71 | 1.00 – 6.00 |
| Enhancement | 4.09 | 1.55 | 1.00 – 6.00 |
| Conformity | 2.12 | 1.36 | 1.00 – 6.00 |
| Social | 4.30 | 1.48 | 1.00 – 6.00 |
| Cannabis Motives | |||
| Coping | 2.72 | 1.67 | 1.00 – 6.00 |
| Enhancement | 3.58 | 1.86 | 1.00 – 6.00 |
| Conformity | 1.78 | 1.24 | 1.00 – 6.00 |
| Social | 2.95 | 1.69 | 1.00 – 6.00 |
| Expansion | 2.23 | 1.54 | 1.00 – 6.00 |
| Prescription Opioid Motives | |||
| Coping | 2.40 | 1.82 | 1.00 – 6.00 |
| Enhancement | 2.77 | 1.90 | 1.00 – 6.00 |
| Social | 2.22 | 1.69 | 1.00 – 6.00 |
| Pain | 3.02 | 1.58 | 1.00 – 6.00 |
| SUD Symptomatology | |||
| Alcohol | 14.29 | 6.76 | 1.00 – 21.00 |
| Cannabis | 7.42 | 5.89 | 0.00 – 21.00 |
| Prescription Opioids1 | 7.74 | 7.61 | 0.00 – 21.00 |
Note. N = 193.
n = 183. BPD = borderline personality disorder; SUD = substance use disorder.
Table 2.
Bivariate correlations between variables.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 Age | -- | .17* | −.20** | −.09 | −.14 | −.24** | .04 | −.29** | −.35** | −.28** | −.04 | −.28** | −.14 | −.19* | −.14 | .05 | .09 | −.25** | −.05 |
| 2 Sex | -- | .19** | .16* | .07 | .08 | .14 | −.09 | −.12 | −.06 | .14 | −.06 | .18* | .13 | .16* | .22** | .03 | −.07 | .20** | |
| 3 Borderline Features | -- | .37** | .27** | .26** | .27** | .29** | .15* | .15* | .22** | .23** | .31** | .27** | .29* | .32** | .19** | .19** | .31** | ||
| 4 Alcohol Coping | -- | .79** | .75** | .50** | .26** | .21** | .22** | .25** | .22** | .30** | .34** | .33** | .32** | .71** | .18* | .25** | |||
| 5 Alcohol Enhancement | -- | .80** | .42** | .23** | .34** | .26** | .21** | .20* | .27** | .38** | .31** | .26** | .57** | .21** | .20** | ||||
| 6 Alcohol Social | -- | .42** | .22** | .25** | .28** | .20** | .21** | .28** | .35** | .32** | .22** | .48** | .17* | .19** | |||||
| 7 Alcohol Conformity | -- | .25** | .11 | .17* | .53** | .29** | .21** | .21** | .26** | .22** | .21** | .12 | .18* | ||||||
| 8 Cannabis Coping | -- | .74** | .83** | .43** | .71** | .29** | .34** | .34** | .20** | .14 | .71** | .24** | |||||||
| 9 Cannabis Enhancement | -- | .80** | .30** | .60** | .21** | .33** | .28** | .15* | .07 | .61** | .22** | ||||||||
| 10 Cannabis Social | -- | .41** | .68** | .26** | .31** | .34** | .12 | .10 | .67** | .23** | |||||||||
| 11 Cannabis Conformity | -- | .47** | .34** | .30** | .31** | .23** | .10 | .29** | .32** | ||||||||||
| 12 Cannabis Expansion | -- | .28** | .27** | .30** | .16* | .05 | .50** | .24** | |||||||||||
| 13 Rx Opioid Coping | -- | .85** | .87** | .51** | .07 | .20** | .80** | ||||||||||||
| 14 Rx Opioid Enhancement | -- | .86** | .53** | .15* | .25** | .73** | |||||||||||||
| 15 Rx Opioid Social | -- | .45** | .13 | .24** | .70** | ||||||||||||||
| 16 Rx Opioid Pain | -- | .22** | .16* | .51** | |||||||||||||||
| 17 Alcohol Use Disorder | -- | .18* | .07 | ||||||||||||||||
| 18 Cannabis Use Disorder | -- | .18* | |||||||||||||||||
| 19 Rx Opioid Use Disorder | -- | ||||||||||||||||||
Note. Rx = prescription. Substance use disorder variables are symptomotology count and not actual diagnosis of the disorder.
p < .05;
p < .01.
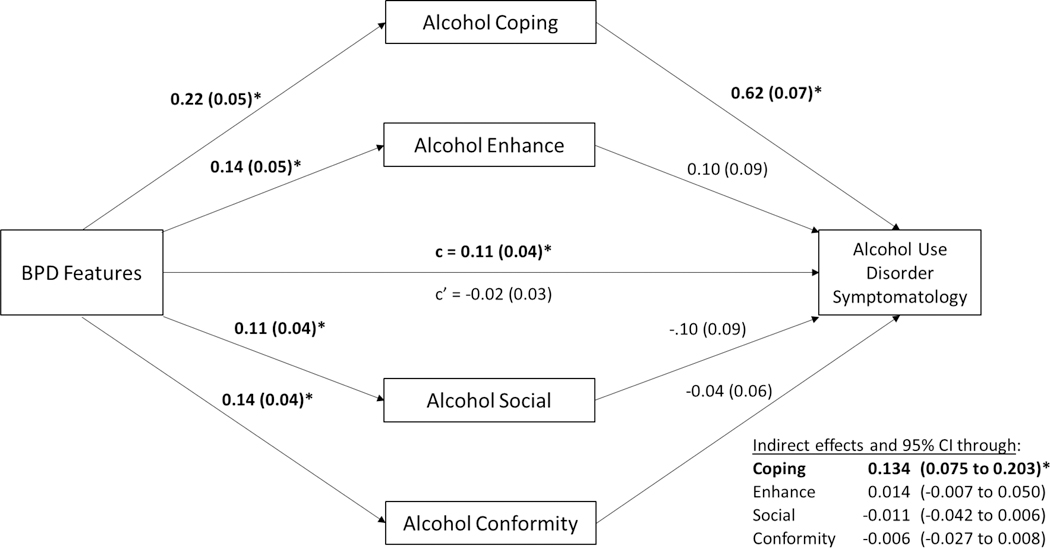
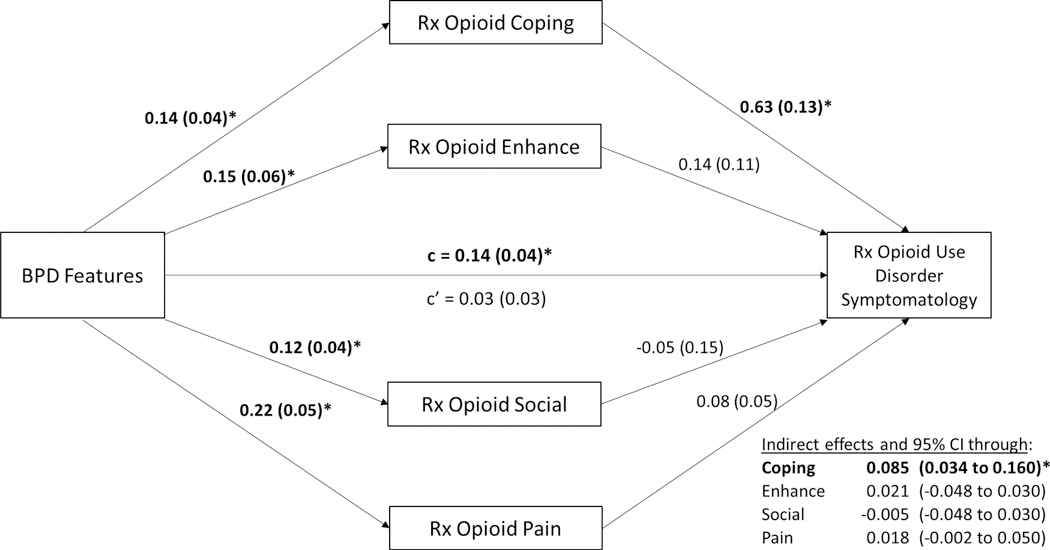
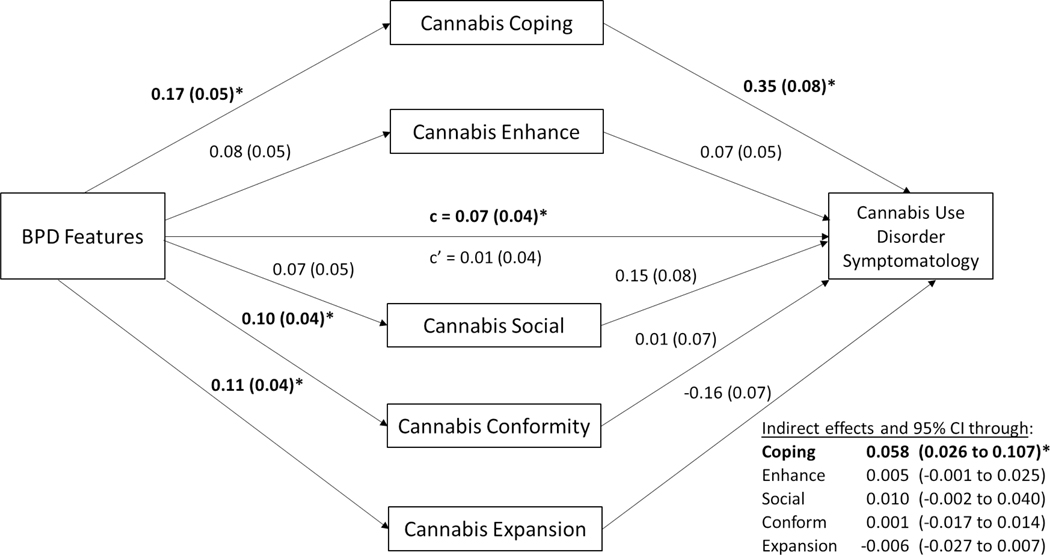
Figures 1–3 illustrate the direct and indirect results for each substance. First, across substances (Figures 1–3) the direct paths from BPD features to each of the motives were significant except for the enhancement and social cannabis motives. Second, for all substances, the direct path from coping to cannabis, alcohol, and prescription opioid use symptomatology, while controlling for BPD features were significant. All other direct paths from substance use motives to symptomatology count were not significant. Third, in parallel, BPD features had an indirect effect on alcohol, cannabis, and prescription opioid symptomatology via coping motives. In total, coping mediates the relationship between BPD and SUD across substances among individuals in outpatient treatment1.
Figure 1.
Estimated unstandardized direct and indirect paths for parallel mediation model. The relationship between BPD features and alcohol use disorder symptomatology are mediated by the motives for alcohol use subscales. BPD = borderline personality disorder. Bolded paths indicate significant relationships. Sex, age, location, and current opioid prescription were used as control variables.
*p < .05 and indirect effects that do not contain 0.
Figure 3.
Estimated unstandardized direct and indirect paths for parallel mediation model. The relationship between BPD features and prescription opioid use disorder symptomatology are mediated by the motives for prescription opioid use subscales. BPD = borderline personality disorder. Bolded paths indicate significant relationships. Sex, age, location, and current opioid prescription were used as control variables.
*p < .05 and indirect effects that do not contain 0.
Discussion
In this study, we were interested in the relationship between BPD features and SUD symptomatology. We provide preliminary support for the hypothesis that, among persons in SUD treatment, the relationship between BPD features and SUD symptomatology for cannabis, alcohol, and prescription opioids can be partially explained by a coping motive pathway. Our findings are consistent with a motivational model of substance use in which coping motives may help to explain why individuals with increased BPD features may be at risk for substance use disorders generally.
Although previous research has examined motives as mediators in the relationship between BPD and alcohol use (Salatino et al., 2018; Chugani et al., 2018), this study expands on previous research by examining motives across substances and in a high-risk SUD treatment population not examined before. Because drinking to cope includes the use of substances to avoid negative emotional states, this finding is novel and noteworthy in light of the substantial literature base suggesting that individuals with BPD experience frequent negative emotional states (American Psychiatric Association, 2013; Gratz, Rosenthal, Tull, Lejuez, & Gunderson, 2009; Linehan, 1993). Our findings on alcohol and cannabis motives also corroborate those of Cooper et al. (2016) who reported that these motives tend to share similarities across substances. Lastly, these findings suggest that there appears to be an “affective pathway” in the BPD/SUD relationship (Chugani et al., 2018), and that individuals with increased BPD features are more vulnerable to coping related substance use, regardless of the substance consumed (alcohol, cannabis, or prescription opioids).
One important finding was evidenced in the mediation model for prescription opioid use disorder. We found that the pain motive did not mediate the relationship between BPD and prescription opioid use disorder. This has important ramifications because it suggests that, among individuals with increased BPD features, despite the higher incidence of pain complaints, using prescription opioids to treat physical pain was not driving the relationship with prescription opioid use disorder. Likewise, it appears that, for prescription opioid use, the emotional or “affective pathway” seems to be driving the BPD/OUD relationship. However, it should be noted that the lack of indirect effect for the pain motive was not due to individuals with BPD reporting low motives for pain; rather, individuals with BPD tended to show high endorsement of pain motives, as indicated by the strong a-path between BPD and pain motives. Rather, the indirect effect was not significant due to the lower b-path from pain motives to prescription opioid use disorder, which may be in part due to covariance between motives, which is a common finding in motives research.
There are many clinical implications to be gleaned from our results. First, the current study adds to the clinical literature by examining the BPD and SUD relationship in a population that is underrepresented in the literature. Second, these results suggest that, for individuals with increased BPD features, substance use/misuse may be an effort to self-medicate (Khantzian, 2003) to avoid harmful emotional states that are a core feature of the disorder (Glenn & Klonsky, 2009). Third, the enhancement motive, which has been found to be a mediator among the Cluster B personality disorders (Tragesser, Trull, Sher, & Park, 2008) in a student population, was not found to be a significant mediator of the BPD/SUD relationship in our treatment sample. In our study, despite some associations between enhancement and BPD features, the motive that best explained the association with SUD symptoms was coping, across the board. Taken together, these findings can clearly inform clinical populations as individuals with increased BPD features may benefit from treatment for substance misuse that emphasizes strategies for adapting to or regulating negative emotional states. Clinical therapies such as mindfulness meditation, acceptance and commitment therapy, and dialectical behavioral therapy have shown promise in decreasing negative emotions and may be a valuable tool for treating this population (Baer, 2003; Bowen et al., 2006; Linehan, 1993; Powers, Zum Vörde Sive Vörding, & Emmelkamp, 2009; Witkiewitz, Bowen, Douglas, & Hsu, 2012). Additionally, interventions aimed at increasing participation in activities that may expand positive emotional states, that do not include harmful drug or alcohol use, may be vital in improving outcomes.
Our findings should be considered in the context of these noted limitations to our study. First, the research project was a cross-sectional design. Although the chronological ordering of our IV (BPD), mediator (motives), and DV (SUD) denote a design that is consistent in the literature, it could be possible that substance use is making BPD features worse. Future research will need to implement longitudinal designs to confirm the temporal ordering in the current study. Second, we only included three substances use outcomes in our models. This limitation is due to the current availability of motives for only these three substances. As additional valid measures of motives for other substances become available (i.e., cocaine, heroin, methamphetamine), the need to generalize these findings to other substance use disorders will be necessary. Third, we measured BPD features and symptomatology of SUD which limits the clinical utility of these findings. Future projects will need to incorporate DSM diagnostic criteria to complement our findings.
Strengths of our study include the large SUD treatment sample, the strong effect sizes across substances for coping, the use of the dimensional perspective of BPD, and the emphasis on an outpatient treatment sample that has largely been ignored in the BPD and SUD literature. The focus on this developmental period and population is crucial because these findings can be directly implemented into treatment interventions that will be beneficial across substances. This study lays the foundation for a clinical trial among outpatient treatment patients which can confirm these findings in a controlled longitudinal design.
In summary, results from this study suggest a strong pathway for negative emotion-initiated substance use (mediation) in the relationship between BPD and alcohol, cannabis, and prescription opioid use disorders among individuals who have been diagnosed with an SUD. Thus, our findings seem to support a self-medication model of substance use as it relates to BPD and SUD specifically (Khantzian, 2003). The motivational pathway through negative affect coping offers promise for the creation of clinical interventions aimed at treating individuals with co-occurring BPD and SUD.
Figure 2.
Estimated unstandardized direct and indirect paths for parallel mediation model. The relationship between BPD features and cannabis use disorder symptomatology are mediated by the motives for cannabis use subscales. BPD = borderline personality disorder. Bolded paths indicate significant relationships. Sex, age, location, and current opioid prescription were used as control variables.
*p < .05 and indirect effects that do not contain 0.
Acknowledgments
This project was funded by an internal grant from the Alcohol and Drug Abuse Research Program at Washington State University [2474-1362]; and the National Institute on Drug Abuse (T32 035165). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Although it was not a part of our primary analyses, in an exploratory examination we checked the model for invariance across gender for each substance. We held all of the direct paths equal to each other across gender and checked the modification indices (MI) for significant values (above 10). None of the modification indices were significant. Thus, we concluded that the models were invariant across gender for each substance. Of course, this finding should be tempered with extreme caution due to the small sample size for women.
The authors report no conflicts of interest.
References
- American Psychiatric Association. (2013a). Diagnostic and Statistical Manual of Mental Disorders: DSM-5. American Psychiatric Association, 991 10.1176/appi.books.9780890425596.744053 [DOI] [Google Scholar]
- American Psychiatric Association; (2013b). Diagnostic and statistical manual of mental disorders (5th ed.). In American Journal of Psychiatry. 10.1176/appi.books.9780890425596.744053 [DOI] [Google Scholar]
- Baer RA (2003). Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice, 10(2), 125–143. 10.1093/clipsy/bpg015 [DOI] [Google Scholar]
- Bowen S, Witkiewitz K, Dillworth TM, Chawla N, Simpson TL, Ostafin BD, … Marlatt GA (2006). Mindfulness meditation and substance use in an incarcerated population. Psychology of Addictive Behaviors, 20(3), 343–347. 10.1037/0893-164X.20.3.343 [DOI] [PubMed] [Google Scholar]
- Carpenter RW, Wood PK, & Trull TJ (2015). COMORBIDITY OF BORDERLINE PERSONALITY DISORDER AND LIFETIME SUBSTANCE USE DISORDERS IN A NATIONALLY REPRESENTATIVE SAMPLE. Journal of Personality Disorders, 29. [DOI] [PubMed] [Google Scholar]
- Chabrol H, Ducong?? E, Casas C, Roura C, & Carey KB (2005). Relations between cannabis use and dependence, motives for cannabis use and anxious, depressive and borderline symptomatology. Addictive Behaviors, 26(4), 829–840. 10.1016/j.addbeh.2004.08.027 [DOI] [PubMed] [Google Scholar]
- Cooper LM (1994). Motivations for Alcohol Use Among Adolescencts: Development and Validation of a Four-Factor Model. Psychological Assessment, 6(2), 117–128. [Google Scholar]
- Cooper LM, & Cooper ML (1994). Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment, 6(2), 117–128. 10.1037/1040-3590.6.2.117 [DOI] [Google Scholar]
- Cooper ML, Kuntsche E, Levitt A, Barber LL, & Wolf S (2016). Motivational models of substance use: A review of theory and research on motives for using alcohol, marijuana, and tobacco. In The Oxford Handbook of Substance Use and Substance Use Disorders: Volume 1. 10.1093/oxfordhb/9780199381678.013.017 [DOI] [Google Scholar]
- Cox WM, & Klinger E (1988). A motivational model of alcohol use. Journal of Abnormal Psychology, 97(2), 168–180. 10.1037/0021-843X.97.2.168 [DOI] [PubMed] [Google Scholar]
- Glenn CR, & Klonsky D (2009). Emotion Dysregulation as a Core Feature of Borderline Personality Disorder. Journal of Personality Disorders, 23(1), 20–28. 10.1159/000322806 [DOI] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, … Ruan WJ (2008). Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of Clinical Psychiatry, 69(4), 533–545. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/18426259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Rosenthal MZ, Tull MT, Lejuez CW, & Gunderson JG (2009). An experimental investigation of emotion dysregulation in borderline personality disorder. Personality Disorders: Theory, Research, and Treatment, S(1), 18–26. 10.1037/1949-2715.S.1.18 [DOI] [PubMed] [Google Scholar]
- Jones RE, Spradlin A, Robinson RJ, & Tragesser SL (2014). Development and validation of the opioid prescription medication motives questionnaire: a four-factor model of reasons for use. Psychology of Addictive Behaviors : Journal of the Society of Psychologists in Addictive Behaviors, 28(4), 1290–1296. 10.1037/a0037783 [DOI] [PubMed] [Google Scholar]
- Khantzian EJ (2003). The Self-Medication Hypothesis Revisited: The Dually Diagnosed Patient. Primary Psychiatry. 10.1016/S0140-6736(02)15879-X [DOI] [Google Scholar]
- Linehan MM (1993). Skills training manual for treating borderline personality disorder. In 1993 [Google Scholar]
- Powers MB, Zum Vörde Sive Vörding MB, & Emmelkamp PMG (2009). Acceptance and commitment therapy: A meta-analytic review. Psychotherapy and Psychosomatics. 10.1159/000190790 [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Diclemente CC, & Norcross JC (1993). In search of how people change: Applications to addictive behaviors. Journal of Addictions Nursing, 5(1), 2–16. 10.3109/10884609309149692 [DOI] [PubMed] [Google Scholar]
- Sansone RA, & Sansone LA (2011). Substance Use Disorders and Borderline Personality : Common Bedfellows OF SUBSTANCE USE DISORDERS. 8(9), 10–14. [PMC free article] [PubMed] [Google Scholar]
- Simons J, Correia CJ, Carey KB, & Borsari BE (1998). Validating a five-factor marijuana motives measure: Relations with use, problems, and alcohol motives. Journal of Counseling Psychology, 45(3), 265–273. 10.1037/0022-0167.45.3.265 [DOI] [Google Scholar]
- Stein MB, Pinsker-aspen JH, Hilsenroth MJ, Stein MB, Pinsker-aspen JH, & Hilsenroth MJ (2007). Borderline Pathology and the Personality Assessment Inventory ( PAI ): An Evaluation of Criterion and Concurrent Validity Borderline Pathology and the Personality Assessment Inventory ( PAI ): An Evaluation of Criterion and Concurrent Validity. 88(June 2015), 37–41. 10.1080/00223890709336838 [DOI] [PubMed] [Google Scholar]
- Stepp SD, Trull TJ, & Sher KJ (2005). Borderline personality features predict alcohol use problems. Journal of Personality Disorders, 19(6), 711–722. 10.1521/pedi.2005.19.6.711 [DOI] [PubMed] [Google Scholar]
- Tomko RL, Trull TJ, Wood PK, & Sher KJ (2014). Characteristics of Borderline Personality Disorder in a Community Sample: Comorbidity, Treatment Utilization, and General Functioning. Journal of Personality Disorders, 28(5), 734–750. 10.1521/pedi_2012_26_093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tragesser SL, Trull TJ, Sher KJ, & Park A (2008). Drinking Motives as Mediators in the Relation Between Personality Disorder Symptoms and Alcohol Use Disorder. Journal of Personality Disorders, 22(5), 525–537. 10.1521/pedi.2008.22.5.525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trull TJ , Sher KJ, Minks-Brown C, Durbin J, & Burr R(2000). Borderline personality disorder and substance use disorders: a review and integration. Clinical Psychology Review, 20(2), 235–253. 10.1016/S0272-7358(99)00028-8 [DOI] [PubMed] [Google Scholar]
- Trull Timothy J., Freeman LK, Vebares TJ, Choate AM, Helle AC, & Wycoff AM (2018). Borderline personality disorder and substance use disorders: an updated review. Borderline Personality Disorder and Emotion Dysregulation, 5(1), 15 10.1186/s40479-018-0093-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trull , Timothy J, Jahng S, Tomko RL, Wood PK, & Sher KJ (2010). Revised NESARC personality disorder diagnoses: gender, prevalence, and comorbidity with substance dependence disorders. Journal of Personality Disorders, 24(4), 412–426. 10.1521/pedi.2010.24.4.412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tull MT, & Gratz KL (2012). The impact of borderline personality disorder on residential substance abuse treatment dropout among men. Drug and Alcohol Dependence, 121(1–2), 97–102. 10.1016/j.drugalcdep.2011.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vest NA, Murphy KT, & Tragesser SL (2018). Borderline personality disorder features and drinking, cannabis, and prescription opioid motives: Differential associations across substance and sex. Addictive Behaviors, 87(December 2017), 46–54. 10.1016/j.addbeh.2018.06.015 [DOI] [PubMed] [Google Scholar]
- Widiger TA, & Trull TJ (2007). Plate tectonics in the classification of personality disorder: Shifting to a dimensional model. American Psychologist, 62(2), 71–83. 10.1037/0003-066X.62.2.71 [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Bowen S, Douglas H, & Hsu SH (2012). Mindfulness-based relapse prevention for substance craving. Addictive Behaviors. 10.1016/j.addbeh.2012.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]