Abstract
Adult patients with relapsed/refractory (R/R) B‐precursor acute lymphoblastic leukemia (ALL) have a poor prognosis. Blinatumomab is a bispecific T‐cell engager (BiTE) immuno‐oncology therapy with dual specificity for CD19 and CD3 that redirects patients’ CD3‐positive cytotoxic T cells to lyse malignant and normal B cells. We conducted an open‐label, phase 1b/2 study to determine the safety, pharmacokinetics, efficacy and recommended dose of blinatumomab in Japanese adults with R/R B‐precursor ALL. Patients received 9 μg/day blinatumomab during week 1 and 28 μg/day during weeks 2‐4, with a 2‐week treatment‐free interval (6‐week cycle); patients received 28 μg/day blinatumomab in subsequent cycles. Primary endpoints were the incidence of dose‐limiting toxicities (DLT) in phase 1b and complete remission (CR)/CR with partial hematologic recovery (CRh) within the first two cycles in phase 2. A total of 26 patients enrolled and 25 (96%) reported grade ≥3 adverse events (mostly cytopenias). There were no DLT. CR/CRh within two cycles was achieved by 4 of 5 patients (80%) in phase 1b and 8 of 21 patients (38%) in phase 2. Among patients with evaluable minimal residual disease, 4 (100%) in phase 1b and 3 (38%) in phase 2 had a complete MRD response. Median RFS for 8 patients who achieved CR/CRh in phase 2 was 5 (95% CI: 3.5‐6.4) months; median OS was not estimable. There were no significant associations between maximum cytokine levels or percentage of specific cell types during cycle 1 and response. Consistent with global studies, blinatumomab appeared to be safe and efficacious in Japanese adults with R/R ALL.
Keywords: acute lymphoblastic leukemia, blinatumomab, clinical study, Japan, phase 1b, refractory, relapsed
Flow of patients through the study. (A) Phase 1b part. (B) Phase 2 part.

1. INTRODUCTION
Adult patients with B‐precursor acute lymphoblastic leukemia (ALL) who relapse or who are refractory to treatment have a poor prognosis, with a 5‐year overall survival (OS) rate of approximately 10%.1, 2, 3, 4 Allogeneic hematopoietic stem cell transplantation (alloHSCT) can result in long‐term survival of patients with relapsed or refractory (R/R) ALL; however, only a small proportion can receive alloHSCT, largely due to resistant disease or complications from toxicities resulting from chemotherapy treatment.5, 6 The major goal of therapies given to qualify for alloHSCT is to achieve a complete remission (CR) with a duration that is long enough to prepare for alloHSCT.
A number of targeted immunotherapies have been developed to meet this urgent medical need for novel treatments for adults with R/R ALL, including bispecific T‐cell engager (BiTE) molecules, antibody‐drug conjugates and chimeric antigen receptor T cells (CART).7, 8 Blinatumomab is a BiTE immuno‐oncology therapy with dual specificity for CD19 and CD3.9, 10 CD19 is expressed in the majority (>90%) of tested B‐lineage ALL cells,11, 12 making it an ideal immunotherapy target for ALL. Blinatumomab simultaneously binds CD19+ B cells and CD3+ cytotoxic T cells and redirects T cells to lyse malignant and normal B cells.9, 10
Blinatumomab is approved globally to treat adults and children with B‐cell precursor ALL. In adults with R/R Philadelphia chromosome‐negative (Ph‐negative) B‐cell precursor ALL, single‐agent blinatumomab resulted in a CR or CR with partial hematologic recovery of peripheral blood counts (CR/CRh) rate of 43% within the first two cycles of treatment, median relapse‐free survival (RFS) of 5.9 months and median OS of 6.1 months.13 In a randomized study comparing blinatumomab with chemotherapy in adults with R/R ALL, blinatumomab significantly increased CR rates (34% vs 16%) and prolonged OS (7.7 months vs 4.0 months).14
Both pivotal blinatumomab studies were conducted in predominantly Caucasian patients. Here we report the results of an open‐label, multicenter, phase 1b/2 study to determine the safety, pharmacokinetics (PK), preliminary efficacy and recommended dose level of blinatumomab in Japanese adults with R/R B‐precursor ALL.
2. MATERIALS AND METHODS
2.1. Study design
This phase 1b/2 study included a 2‐week screening and prephase period. In the phase 1b dose‐finding part of the study, four cohorts of up to 6 patients each were planned; patients in the first cohort received the global recommended dose of induction blinatumomab for 4 weeks followed by a 2‐week treatment‐free interval (6‐week cycle). Dose de–escalation cohorts were planned in the event of dose‐limiting toxicities (DLT, defined in Doc S1). In cycle 1, blinatumomab was administered by continuous IV infusion as follows: week 1 at 9 μg/day and weeks 2‐4 at 28 μg/day. In subsequent cycles, patients received blinatumomab at 28 μg/day during weeks 1‐4. The infusion was interrupted if grade ≥3 cytokine release syndrome (CRS), clinically relevant neurologic events, tumor lysis syndrome or disseminated intravascular coagulation/coagulopathy related to blinatumomab occurred but could be restarted (after dexamethasone premedication) if the adverse event resolved to grade 1 or baseline within 1 week. After an interruption, blinatumomab was restarted at the lowest starting dose level (9 µg/day) for at least 7 days before increasing the dose (28 µg/day), except for grade ≥3 neurologic adverse events, where dose escalation was not allowed. Blinatumomab was discontinued for treatment interruptions longer than 2 weeks due to an adverse event or grade 4 event that was possibly related to blinatumomab, disease progression or hematological relapse, or if the patient would not benefit from continued treatment with blinatumomab or would benefit from a change of therapy, including alloHSCT.
No DLT were observed in the phase 1b part of the study; therefore, the phase 2 dose and dosing regimen remained the same as the phase 1b part.
Responders were defined as patients who achieved CR/CRh within two induction cycles. Responders received consolidation cycles of blinatumomab until they had disease progression, an intolerable adverse event, withdrew their consent or had received a maximum of five total induction/consolidation cycles.
Patients could receive an alloHSCT at any time following the first treatment cycle. There was a safety follow‐up visit 30 (±3) days after the last dose of blinatumomab, and patients were then followed at 3, 6, 9, 12, 18 and 24 months (±2 weeks) for disease and survival status.
The primary endpoint of the phase 1b part of the study was the incidence of DLT; the primary endpoint of the phase 2 part was CR/CRh within two cycles of treatment with blinatumomab.
Secondary endpoints included PK parameters and CR/CRh within the first two cycles of treatment for the phase 1b part and RFS and OS for the phase 2 part. Minimal residual disease (MRD) response was an exploratory endpoint.
The safety endpoints of both parts of the study were the incidence and severity of adverse events and the incidence of anti–blinatumomab antibody formation.
The study protocol was approved by the ethics committee or the institutional review board at each clinical site, and all patients provided signed informed consent before the start of any study‐related procedures. The study was conducted in accordance with the International Council for Harmonisation Good Clinical Practice Guideline and conforms to the provisions of the Declaration of Helsinki.
2.2. Patients
Eligible patients were ≥18 years old with Ph‐negative B‐precursor ALL and any of the following: R/R after first‐line therapy with first remission duration ≤12 months; or R/R after first salvage therapy; or R/R within 12 months of alloHSCT. Patients were also required to have >5% bone marrow blasts, adequate renal and liver function, and ECOG performance status of 0‐2.
Patients were excluded if they had Burkitt’s leukemia, a history of clinically relevant central nervous system pathology, autoimmune disease, any active acute graft‐versus‐host disease (GVHD), alloHSCT within 12 weeks before the start of blinatumomab, autologous HSCT within 6 weeks before the start of blinatumomab, chemotherapy or radiotherapy within 2 weeks before the start of blinatumomab, immunotherapy within 6 weeks before the start of blinatumomab, or previous anti–CD19 or blinatumomab therapy.
2.3. Dexamethasone premedication
Blinatumomab treatment is associated with adverse events of CRS and neurologic events.13, 14, 15 To reduce the incidence of CRS and neurologic events and to reduce the possibility of tumor lysis syndrome, patients with bone marrow blasts >50%, peripheral blood blast count ≥15 × 109/L, elevated lactate dehydrogenase or extramedullary high tumor load were treated with dexamethasone at ≤ 0 mg/m2 per day IV for up to 5 days during the prephase period; the dose could be increased to 24 mg/day if clinically indicated. Premedication with dexamethasone 20 mg IV was required within 1 h before treatment with blinatumomab in each cycle for the prevention of CRS.
2.4. Intrathecal prophylactic chemotherapy
Cerebrospinal fluid prophylaxis, consisting of an intrathecal regimen according to institutional or national guidelines (such as methotrexate, cytosine arabinoside or dexamethasone), was administered within 1 week (+3 days) before the start of blinatumomab and following each treatment cycle (after bone marrow aspiration on day 29). Intrathecal prophylactic chemotherapy during and after maintenance therapy was at the discretion of the investigator. This procedure could be omitted in the event of an anticipated safety risk to the patient.
2.5. Efficacy and safety assessments
Hematological response and MRD status were assessed using bone marrow aspirates and core biopsies taken at screening, at the end of infusion on day 29 of each cycle, at the safety follow‐up visit if a patient ended treatment for any reason other than relapse and during long‐term follow up if a patient had not relapsed by day 29 of their last treatment cycle.
Minimal residual disease was assessed at a central laboratory in Kiel, Germany and measured with the use of allele‐specific, real‐time quantitative PCR of clonal immunoglobulin heavy and light chain rearrangements and clonal T‐cell receptor beta, gamma and delta gene rearrangements. The assay sensitivity was at least 10−4, and the European Study Group on MRD detection in ALL (ESGMRD‐ALL) interpretation guidelines16 were used for MRD quantification. Responses were defined as: (a) CR: ≤5% bone marrow blasts, no evidence of disease, and full recovery of peripheral blood counts (platelets >100 000/μL and absolute neutrophil count (ANC) >1000/μL); (b) CRh: ≤5% bone marrow blasts, no evidence of disease and partial recovery of peripheral blood counts (platelets >50 000/μL and ANC >500/μL); (c) blast‐free hypoplastic or aplastic bone marrow: ≤5% bone marrow blasts, no evidence of disease and insufficient recovery of peripheral blood counts (platelets ≤ 50,000/μL and/or ANC ≤500/μL); (d) partial remission: >5% to <25% bone marrow blasts with a ≥50% reduction from baseline; (e) progressive disease: increase from baseline of ≥25% bone marrow blasts or an absolute increase of ≥5000 circulating leukemia cells/μL; (f) hematological relapse: >5% bone marrow blasts or blasts in peripheral blood after documented CR/CRh; (g) MRD response (measured by PCR): <10−4 leukemic cells; and (h) MRD complete response: no detectable leukemic cells.
Adverse events were recorded throughout the study, coded using the Medical Dictionary for Regulatory Activities (MedDRA) version 20.0, and graded according to the NCI Common Terminology Criteria for Adverse Events (CTCAE) version 4.03.
Cytokine release syndrome was diagnosed by the investigators and reported as “cytokine release syndrome” or “cytokine storm” according to CTCAE version 4.03. A list of clinically relevant neurologic events is provided in Doc S2. The DLT assessment window was the first 2 weeks of treatment. If the dose of blinatumomab was reduced, the DLT assessment window was the first 3 weeks of treatment.
2.6. Pharmacokinetic and pharmacodynamic analyses
Serum samples for PK analysis were collected during cycle 1 (day 1: before the infusion and 2, 6 and 10 hours after infusion; day 2: 24 hours after infusion start; day 8: before infusion start; day 15: any time during infusion; day 29: during infusion and 1, 2, 4 and 6 hours after the end of infusion) and days 8, 15 and 29 of all other cycles at any time during the infusion. Blood cytokine levels of IL‐2, IL‐4, IL‐6, IL‐10, TNF‐α and IFN‐γ were monitored by measuring the respective markers in serum using the FACS‐based BD Cytometric Bead Array Human Th1/Th2 Kit II (BD Biosciences), following the manufacturer’s instructions and as previously described by Nägele et al.17
Lymphocyte subsets were measured by flow cytometry in whole peripheral blood before treatment and at various time points after the blinatumomab infusion, as previously described.17
Levels of serum blinatumomab were quantified as described previously.18
2.7. Statistical analyses
The planned sample size was a maximum of 18 patients for the phase 1b part (a minimum of 2 and a maximum of 6 patients at each dose level). The planned sample size for the phase 2 part was a maximum of 21 patients and was based on the primary efficacy endpoint of hematological response (CR/CRh in the first two cycles). Simon’s mini‐max 2‐stage design19 was used with a sample size of 13 patients in the first stage and 21 evaluable patients in total, based on a 1‐sided type 1 error of 0.025 and a power of 90% to detect the effective response rate assumption of ≥40% over an ineffective treatment rate of ≤10%. An interim analysis was conducted after the first 13 patients enrolled into the phase 2 part had either discontinued treatment or completed their first two treatment cycles. If more than 1 patient achieved a CR/CRh within the first two cycles of treatment, additional patients could be enrolled up to the maximum of 21 patients. If 6 or more patients achieved a CR/CRh within two cycles of treatment, the study’s ineffective treatment assumption would be rejected.
Analyses of efficacy and safety included all patients who received any infusion of blinatumomab. The proportion of patients who achieved responses (CR, CRh, and MRD response) were summarized with exact 95% confidence intervals (CI). RFS and OS are described with Kaplan‐Meier estimates.
Pharmacokinetics parameters of blinatumomab were estimated by noncompartmental analysis and summarized by descriptive statistics.
Associations between cytokine levels or lymphocyte subsets and responses were characterized by logistic regression. Densities were transformed by log2 for statistical analysis, and the method of Benjamini‐Hochberg20 was used to estimate the false discovery rate for each association. Longitudinal data (cycle 1) for hematological subsets were modeled with linear mixed effects models containing an interaction between visit and response status.
3. RESULTS
3.1. Patient disposition and baseline characteristics
Five patients in the phase 1b part and 21 in the phase 2 part of the study were enrolled between 4 June 2015 and 24 August 2017. The flow of patients through the study is shown in Figure 1. All 5 patients enrolled in the phase 1b part of the study completed the first two cycles of blinatumomab, and all discontinued blinatumomab (due to death). Sixteen patients enrolled in the phase 2 part of the study completed the first two cycles of blinatumomab treatment, and all 21 patients discontinued blinatumomab, with 18 (85.7%) patients continuing the study and 3 (14%) patients discontinuing the study (2 had died and 1 had withdrawn consent). Patient characteristics are summarized in Table 1. Approximately half of all patients had received a prior HSCT, and most patients had received at least 1 prior salvage therapy.
Figure 1.
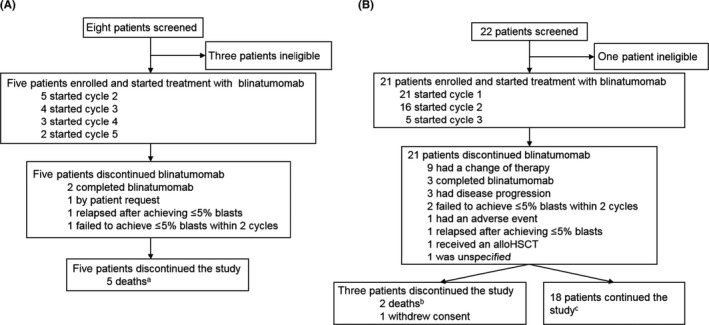
Flow of patients through the study. A, Phase 1b part. B, Phase 2 part. aDeaths in the phase 1b part of the study were due to liver failure (1 patient), brain abscess (1 patient) and disease progression (3 patients). bDeaths in the phase 2 part of the study were due to tumor lysis syndrome (fatal adverse event, 1 patient) and disease progression (1 patient). cPatients still on study as of the data cutoff date (24 August 2017). alloHSCT, allogeneic hematopoietic stem cell transplantation
Table 1.
Baseline demographics and clinical characteristics
| Blinatumomab 9‐28 µg/day | ||
|---|---|---|
|
Phase 1b N = 5 |
Phase 2 N = 21 |
|
| Sex, n (%) | ||
| Male | 1 (20) | 9 (43) |
| Female | 4 (80) | 12 (57) |
| Age, median (range), years | 58 (23‐75) | 43 (18‐55) |
| ECOG PS, n (%) | ||
| 0 | 1 (20) | 11 (52) |
| 1 | 3 (60) | 9 (43) |
| 2 | 1 (20) | 1 (5) |
| Bone marrow blasts, n (%) | ||
| ≤5% | 0 (0.0) | 0 (0.0) |
| >5% to <10% | 0 (0.0) | 2 (10) |
| 10% to <50% | 2 (40) | 6 (29) |
| ≥50% | 3 (60) | 13 (62) |
| B‐ALL subtype, n (%) | ||
| Pro–B‐ALL | 1 (20) | 2 (10) |
| Pre–B‐ALL | 1 (20) | 5 (24) |
| C‐ALL | 3 (60) | 10 (48) |
| B‐ALL with recurrent genetic abnormality | 0 (0) | 4 (19) |
| Extramedullary disease, n (%) | 1 (20) | 2 (10) |
| Prior HSCT, n (%) | 4 (80) | 9 (43) |
| 1 | 2 (40) | 9 (43) |
| 2 | 2 (40) | 0 (0) |
| Number of relapses, n (%) | ||
| 1 | 2 (40) | 13 (62) |
| 2 | 0 (0) | 4 (19) |
| >2 | 3 (60) | 0 (0) |
| Number of salvage therapies, n (%) | ||
| 0 | 1 (20) | 7 (33) |
| 1 | 1 (20) | 7 (33) |
| 2 | 2 (40) | 4 (19) |
| >2 | 1 (20) | 3 (14) |
Abbreviations: ALL, acute lymphoblastic leukemia; HSCT, hematopoietic stem cell transplantation.
3.2. Dosing
In the phase 1b part of the study, all patients received at least two cycles of blinatumomab with a median of 4 (range: 2‐5) cycles. The median duration of treatment was 108 (range: 56‐140) days. Two (40%) patients had blinatumomab interruptions, 1 due to an adverse event and 1 due to disease progression.
In the phase 2 part of the study, all patients received at least 1 cycle of blinatumomab with a median of 2 (range: 1‐3) cycles. The median duration of treatment was 56 (range: 5‐84) days. A total of 4 (19%) patients had drug interruptions due to adverse events.
3.3. Safety
None of the patients experienced DLT during the DLT‐evaluation period. All patients reported treatment‐emergent adverse events and most reported grade ≥3 adverse events. Serious adverse events were not reported in the phase 1b part but occurred in 7 patients in the phase 2 part (Table 2). The most common treatment‐emergent adverse events were CRS (4 patients, 80%) and headache (3 patients, 60%) in the phase 1b part, and pyrexia (15 patients, 71%), febrile neutropenia (10 patients, 48%) and nausea (9 patients, 43%) in the phase 2 part. The most common grade ≥3 treatment‐emergent adverse events were febrile neutropenia, neutropenia, anemia, decreased neutrophil count and decreased platelet count (Table 2). Serious treatment‐emergent adverse events reported in the phase 2 part were grade 4 decreased neutrophil count in 2 patients and grade 3 bacteremia, colitis, CRS, decreased appetite and device‐related infection in 1 patient each (Table 2).
Table 2.
Patient incidence of adverse events
| Blinatumomab (9‐28 μg/day) | ||
|---|---|---|
|
Phase 1b N = 5 |
Phase 2 N = 21 |
|
| Treatment‐emergent adverse events, n (%) | 5 (100) | 21 (100) |
| Grade ≥3 | 4 (80) | 21 (100) |
| Serious | 0 (0) | 7 (33) |
| Leading to interruption of blinatumomab | 1 (20) | 3 (14) |
| Leading to discontinuation of blinatumomab | 0 (0) | 1 (5) |
| Fatal | 0 (0) | 1 (5) |
| Treatment‐related adverse events, n (%) | 5 (100) | 21 (100) |
| Grade ≥3 | 2 (40) | 18 (86) |
| Serious | 0 (0) | 4 (19) |
| Leading to interruption of blinatumomab | 1 (20) | 1 (5) |
| Leading to discontinuation of blinatumomab | 0 (0) | 1 (5) |
| Fatal | 0 (0) | 0 (0) |
| Grade ≥3 treatment‐emergent adverse events in >20% of patients,a n (%) | ||
| Febrile neutropenia | 2 (40) | 10 (48) |
| Neutropenia | 2 (40) | 4 (19) |
| Anemia | 0 (0) | 7 (33) |
| Neutrophil count decreased | 0 (0) | 6 (29) |
| Platelet count decreased | 1 (20) | 5 (24) |
| Serious treatment‐emergent adverse events, n (%) | 0 (0) | 7 (33) |
| Decreased neutrophil countb | 0 (0) | 2 (10) |
| Bacteremia | 0 (0) | 1 (5) |
| Colitis | 0 (0) | 1 (5) |
| Cytokine release syndromeb | 0 (0) | 1 (5) |
| Decreased appetiteb | 0 (0) | 1 (5) |
| Device‐related infection | 0 (0) | 1 (5) |
In the phase 1b or phase 2 part.
Considered related to blinatumomab.
Treatment‐related adverse events were reported by all patients, the most common being CRS (4 patients, 80%) and fatigue, headache and nausea (2 patients, 40% each) in the phase 1b part, and pyrexia (11 patients, 52%), CRS (8 patients, 38%) and decreased neutrophil count (6 patients, 29%) in the phase 2 part. The grade 4 CRS that occurred in 1 patient in the phase 2 part was considered related to blinatumomab and resulted in the only discontinuation from the study. The event started on day 6 and ended on day 137, during which time the patient was hospitalized and received a transfusion and antibiotics.
All patients in the phase 1b and phase 2 parts of the study had adverse events of interest (Table 3). In the phase 2 part, 1 patient had a grade 4 CRS adverse event (described above), 1 patient had a grade 3 neurologic event of hypophagia and 1 patient had a fatal adverse event of tumor lysis syndrome in the setting of disease progression. None of the patients in the phase 1b part had a fatal adverse event during the study.
Table 3.
Patient incidence of adverse events of interest by category
| Blinatumomab (9‐28 μg/day) | ||
|---|---|---|
|
Phase 1b N = 5 |
Phase 2 N = 21 |
|
| Adverse events of interest, n (%) | 5 (100) | 21 (100) |
| Central nervous system eventsa | 3 (60) | 9 (43) |
| Grade ≥3 | 0 (0) | 1 (5) |
| Cytokine release syndromes | 4 (80) | 8 (38) |
| Grade ≥3 | 0 (0) | 1 (5) |
| Cytopenias | 3 (60) | 19 (91) |
| Grade ≥3 | 3 (60) | 17 (81) |
| Decreased immunoglobulins | 2 (40) | 6 (29) |
| Grade ≥3 | 0 (0) | 0 (0) |
| Elevated liver enzymes | 1 (20) | 6 (29) |
| Grade ≥3 | 0 (0) | 2 (10) |
| Infections | 4 (80) | 15 (71) |
| Grade ≥3 | 2 (40) | 8 (38) |
| Infusion reactions considering durationb | 5 (100) | 15 (71) |
| Grade ≥3 | 0 (0) | 2 (10) |
| Lymphopenia | 1 (20) | 5 (24) |
| Grade ≥3 | 1 (20) | 5 (24) |
| Neurologic events | 3 (60) | 9 (43) |
| Grade ≥3 | 0 (0) | 1 (5) |
| Neutropenia | 3 (60) | 17 (81) |
| Grade ≥3 | 3 (60) | 16 (76) |
| Thromboembolic events | 0 (0) | 7 (33)c |
| Grade ≥3 | 0 (0) | 0 (0) |
| Tumor lysis syndrome | 0 (0) | 1 (5) |
| Grade ≥3 | 0 (0) | 1 (5) |
Phase 1b included headache, somnolence and lethargy; phase 2 included headache, insomnia, tremor, aphasia, disorientation, dizziness postural, dysgeusia, extrapyramidal disorder, hypophagia, intention tremor, neuralgia and presyncope.
Potential infusion‐related toxicities were identified using a narrow search strategy for infusion reactions with an onset within 48 h of infusion start and no restriction in duration.
All grade 2 events: 1 case of grade 2 deep vein thrombosis and 6 cases of grade 2 disseminated intravascular coagulation.
Interruption of the blinatumomab infusion due to adverse events occurred in both parts of the study. One patient in the phase 1b part had treatment‐related grade 2 CRS that started on day 1 and ended on day 6. The patient received dexamethasone, and the blinatumomab infusion was restarted. Three patients in the phase 2 part had treatment interruptions, 1 due to febrile neutropenia (related to blinatumomab), 1 due to infection (not related to blinatumomab) and 1 due to cytomegaloviral pneumonia (not related to blinatumomab).
No patients tested positive for anti–blinatumomab antibodies.
3.4. Pharmacokinetics
Samples from 26 patients were available for PK analysis. During continuous IV infusion of 9 and 28 μg/day blinatumomab in cycle 1, the mean (SD) steady‐state serum concentration (Css) of blinatumomab was 191 (90.8) pg/mL and 948 (488) pg/mL, respectively. The estimated mean (SD) systemic clearance (CL), terminal half‐life (t 1/2,z), and volume of distribution (Vz) were 1.59 (0.812) L/hour, 2.38 (1.36) hours and 6.02 (6.09) L, respectively.
3.5. Efficacy
Overall, 26 patients were evaluable for response (Table 4). CR/CRh during the first two cycles was achieved by 4 (80%) patients in the phase 1b part and 8 (38%) patients in the phase 2 part. Among patients who achieved CR/CRh and had evaluable MRD, 4 (100%) in the phase 1b part and 3 (38%) in the phase 2 part had a complete MRD response.
Table 4.
Best response during the first two cycles of treatment
| Blinatumomab (9‐28 µg/day) | ||
|---|---|---|
|
Phase 1b N = 5 n (%) [95% CI] |
Phase 2 N = 21 n (%) [95% CI] |
|
| Response | ||
| CR/CRh | 4 (80) [28‐100] | 8 (38) [18‐62] |
| CR | 3 (60) [15‐95] | 5 (24) [8‐47] |
| CRh | 1 (20) [0.5‐72] | 3 (14) [3‐36] |
| CRi | 0 (0) [0‐52] | 0 (0) [0‐16] |
| Blast‐free hypoplastic or aplastic bone marrow without CRh or CRi | 0 (0) [0‐52] | 6 (29) [11‐52] |
| PR | 0 (0) [0‐52] | 0 (0) [0‐16] |
| Nonresponse | ||
| No response | 1 (20) [0.5‐72] | 5 (24) [8‐47] |
| Hematological relapse | 0 (0) [0‐52] | 0 (0) [0‐16] |
| PD | 0 (0) [0‐52] | 2 (10) [1‐30] |
| Not evaluable | 0 (0) [0‐52] | 0 (0) [0‐16] |
| Patients with CR/CRh and evaluable MRD | 4 | 7 |
| MRD response | 4 (100) [40‐100] | 5 (71) [29‐96] |
| MRD complete response | 4 (100) [40‐100] | 3 (43) [10‐82] |
Abbreviations: CI, confidence interval; CR, complete remission; CRh, complete remission with partial hematological recovery; CRi, complete remission with incomplete hematological recovery; MRD, minimal residual disease; PD, progressive disease; PR, partial remission.
Among the 4 patients in the phase 1b part who achieved CR/CRh during the first two cycles of treatment, 1 patient relapsed at 4.2 months, 1 patient died due to liver failure at 9.9 months, and 2 patients died due to disease progression at 13.0 and 19.8 months. Among the 8 patients in the phase 2 part who achieved CR/CRh during the first two cycles, the median RFS was 5 (95% CI: 3.5‐6.4) months; the Kaplan‐Meier estimate of RFS was 100%, 50% and 0% at 3, 6 and 12 months, respectively.
At the data cutoff date, 2 patients in the phase 2 part had died at 2.7 and 7.4 months; all patients were followed up for a median of 6.3 months and median OS was not estimable (95% CI: 7.4 months, not estimable). The Kaplan‐Meier estimate of survival was 95% at 3 and 6 months and 79.2% at 12 months.
Fourteen (67%) patients in the phase 2 part received an HSCT during long‐term follow up, 10 (48%) of whom did not receive other anticancer therapy before HSCT (5 of the 10 patients had achieved CR/CRh during the blinatumomab treatment period).
3.6. Effect of serum cytokines and lymphocyte subsets on response to blinatumomab
Serum samples for analysis of cytokine levels were available for 26 patients. Serum levels of IL‐6, IL‐10, IFN‐γ and TNF‐ during cycle 1 were mostly below the lower limit of quantitation (125 pg/mL); IL‐2 was below the limit of detection; and IL‐4 was not detected. There were no significant associations between maximum cytokine levels of IL‐6, IL‐10, IFN‐ and TNF‐ during cycle 1 and patient response (CR/CRh) to blinatumomab treatment (the false discovery rate was ≥5% for each association) (Figure 2).
Figure 2.
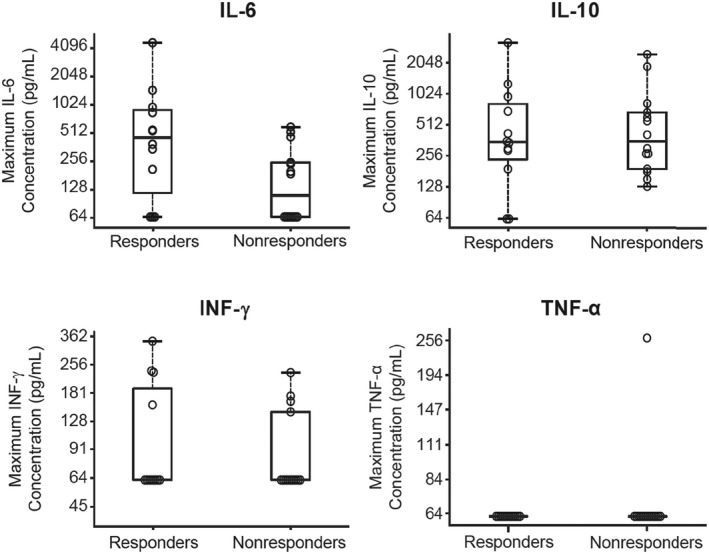
Cytokine levels grouped by patient response (CR/CRh) to blinatumomab treatment. Individual patient maximum cytokine levels in cycle 1 are shown with 1st, 2nd and 3rd quartiles (box) and outliers (whiskers). The horizontal line denotes the median. Results below the lower limit of quantitation (LLOQ, 125 pg/mL) were imputed to half of the LLOQ. CR, complete remission; CRh, complete remission with partial hematological recovery; IFN, interferon; IL, interleukin; TNF, tumor necrosis factor
Samples for analysis of cell subsets were available for 26 patients. For most patients, there was a transient dip in CD3+, CD4+ and CD8+ T cells on day 2 of cycle 1, recovering by day 8. In addition, there was rapid depletion of CD19+ B cells, which was sustained throughout cycle 1 (Figure 3). Fold change from baseline (95% CI) at day 2 in number per mm3 of CD3+, CD4+ and CD8 + T cells was –27‐fold (–41.5, –17.6), –24‐fold (–36.5, –15.3) and –37‐fold (–58.3, –23.0), respectively. Change from baseline (95% CI) at day 8 in percentage of CD19+ B cells was –9.4% (–14.7%, –4.1%). We assessed whether there was an association between response to blinatumomab and baseline or maximum cycle 1 percentages of CD3+ T cells, CD4+ T cells, CD8+ T cells, CD19+ B cells, granulocytes, lymphocytes, monocytes and CD3− CD16+ CD56+ natural killer cells. None of these baseline biomarkers predicted response to blinatumomab (Figure 4).
Figure 3.
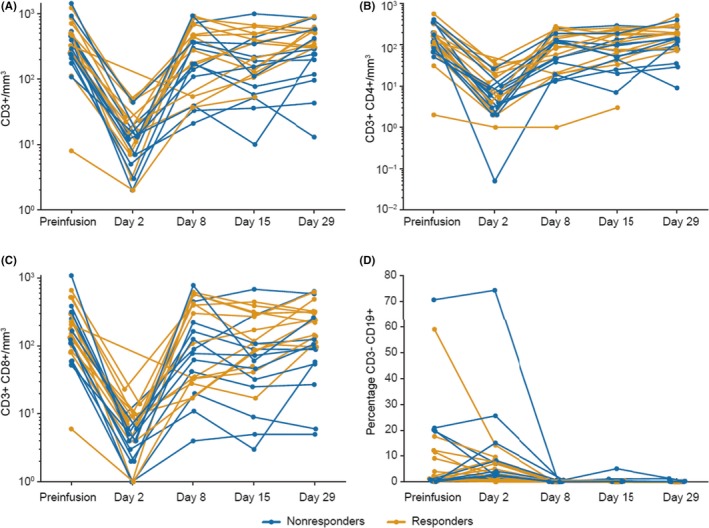
Individual patient levels of T cells and B cells during cycle 1. A, CD3+ cells/mm3. B, CD3+CD4+ cells/mm2. C, CD3+CD8+ cells/mm2. D, Percentage of CD3− CD19+ cells
Figure 4.
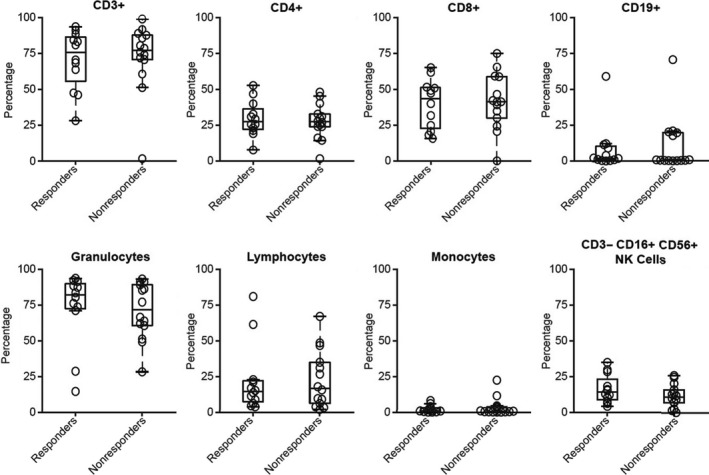
Baseline percentages of specific cell subsets grouped by patient response (CR/CRh) to blinatumomab treatment. CR, complete remission; CRh, complete remission with partial hematological recovery; NK, natural killer
4. DISCUSSION
This open‐label, single‐arm, multicenter, phase 1b/2 study demonstrated the efficacy and safety of the global recommended dosage of single‐agent blinatumomab in Japanese adults with R/R Ph‐negative B‐cell precursor ALL. In this small population of patients, response rates, incidence and types of adverse events, and PK parameters were consistent with those observed in global studies.
In the phase 1b part of the study, 4 of 5 (80%) patients achieved a CR/CRh within two cycles; 4 of 4 (100%) patients had a complete MRD response. Responses were also observed in the phase 2 part of the study, with 8 of 21 (38%) patients achieving a CR/CRh within two cycles of treatment, among whom 7 had evaluable MRD; 3 of these patients (42.9%) had a complete MRD response. These results are consistent with the global phase 2 and phase 3 studies using single‐agent blinatumomab to treat R/R Ph‐negative B‐cell precursor ALL. In the phase 2 study, 43% of patients achieved a CR/CRh within two cycles, and in the phase 3 study, 44% of patients achieved a CR/CRh/CR with incomplete hematologic recovery.13, 14 The median RFS in Japanese patients was also comparable to patients who achieved CR/CRh in the phase 2 global study, 5 months vs 5.9 months,13 respectively.
No DLT were observed and no new safety signals were identified in this study. Adverse events were consistent with those reported with singe‐agent blinatumomab in previous adult blinatumomab studies, with grade ≥3 cytopenias occurring in a substantial proportion of patients across studies. In addition, CRS and neurologic events reported in previous studies with blinatumomab were also reported in this study. As expected, blinatumomab‐related CRS occurred in several patients, with 1 patient having discontinued the study due to grade 4 CRS that was deemed related to treatment with blinatumomab. In addition, 1 patient had a grade 3 neurologic event of hypophagia. The only fatal adverse event, tumor lysis syndrome, was due to disease progression and was not related to treatment with blinatumomab.
Pharmacokinetics of blinatumomab were approximately linear with estimates of PK parameters in adult Japanese R/R ALL patients, generally within the range of those previously reported for adult non–Japanese R/R ALL patients in global studies.
Previous studies have shown that blinatumomab infusion resulted in rapid, robust and sustained depletion of B cells, and redistribution of T cells.17, 21 Consistent with those data, most patients in the current study had depletion of CD19+ B cells and transient reduction in T‐cell subsets after infusion of blinatumomab. We did not observe any associations between peak cytokine levels and response to blinatumomab. Similarly, we did not observe any associations between baseline or peak levels of cell subsets and response to blinatumomab. Our analysis of associations between cytokines/cell subsets and response to blinatumomab was likely impacted by the small sample size. A previous analysis of a much larger patient population (N = 189) showed that response to blinatumomab was associated with higher peak levels of IL‐10, higher proportions of CD3+ T cells, lower proportions of CD19+ B cells and higher proportions of granulocytes at baseline.21
This study was limited by the small sample size, and the time‐to‐event endpoints should be interpreted with caution. No baseline assessments of cytokines were done for this study, and most of the cytokine results were below the assay’s lower limit of quantitation.
In conclusion, single‐agent blinatumomab appeared to be safe and efficacious in Japanese adults with R/R ALL. Response rates in Japanese patients were consistent with those in global studies, and no new safety signals were identified. Single‐agent blinatumomab is now approved in Japan to treat adult and pediatric patients with B‐cell precursor R/R ALL.
CONFLICT OF INTEREST
This clinical trial was funded by Amgen and Amgen Astellas BioPharma KK (ClinicalTrials.gov: NCT02412306). Blinatumomab was provided by Amgen. The funder contributed to the study design, data collection, data analysis and data interpretation, and funded a professional medical writer to assist with writing the report. The authors had full access to all data in the study and had final responsibility for the decision to submit for publication. Hitoshi Kiyoi has received research funding from Astellas, Celgene, Chugai, Eisai, FUJIFILM, Kyowa Hakko Kirin, Nippon Shinyaku, Novartis Pharma KK, Otsuka, Pfizer Japan, Sanofi, Sumitomo Dainippon, Takeda and Zenyaku Kogyo; and honoraria from Amgen, Astellas, Astellas BioPharma KK, Bristol‐Myers Squibb, Daiichi Sankyo and Novartis Pharma KK. Tomoko Hata, Iekuni Oh and Yasuhiro Nakashima have nothing to disclose. Yoshinobu Maeda has received research funding from Astellas. Hironobu Minami has received research funding from Chugai, and honoraria from Celgene, Astellas, Janssen and Novartis. Toshihiro Miyamoto has received honoraria from Amgen and Bristol‐Myers Squibb. Toru Sakura has received research funding from AbbVie GK, Astellas Pharma, Amgen Astellas BioPharma KK, Daiichi Sankyo and Otsuka. Hiroatsu Iida has received research funding from Chugai and honoraria from Astellas, Novartis, Celgene and Janssen. Abraham Anderson, Yuqi Chen, Joan D Morris and Catherine A. Tuglus are employees and stockholders of Amgen. Cedric Dos Santos and James Kalabus are ex‐employees and stockholders of Amgen. Yukio Kobayashi has received lecture fees/honoraria from Astellas.
Supporting information
ACKNOWLEDGMENTS
Writing support was funded by Amgen and was provided by Kathryn Boorer, PhD of KB Scientific Communications. The authors thank Zachary Zimmerman, MD, and Min Zhu, PhD, for their contributions to this study. These data were presented in part at the 80th Annual Meeting of the Japanese Society of Hematology, 12‒14 October 2018, Osaka, Japan.
Kiyoi H, Morris JD, Oh I, et al. Phase 1b/2 study of blinatumomab in Japanese adults with relapsed/refractory acute lymphoblastic leukemia. Cancer Sci. 2020;111:1314–1323. 10.1111/cas.14322
REFERENCES
- 1. Gökbuget N, Stanze D, Beck J, et al. Outcome of relapsed adult lymphoblastic leukemia depends on response to salvage chemotherapy, prognostic factors, and performance of stem cell transplantation. Blood. 2012;120:2032‐2041. [DOI] [PubMed] [Google Scholar]
- 2. O’Brien S, Thomas D, Ravandi F, et al. Outcome of adults with acute lymphocytic leukemia after second salvage therapy. Cancer. 2008;113:3186‐3191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Oriol A, Vives S, Hernández‐Rivas JM, et al. Outcome after relapse of acute lymphoblastic leukemia in adult patients included in four consecutive risk‐adapted trials by the PETHEMA Study Group. Haematologica. 2010;95:589‐596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wei G, Wang J, Huang H, Zhao Y. Novel immunotherapies for adult patients with B‐lineage acute lymphoblastic leukemia. J Hematol Oncol. 2017;10:150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. El Fakih R, Ahmed S, Alfraih F, Hanbali A. Hematopoietic cell transplantation for acute lymphoblastic leukemia in adult patients. Hematol Oncol Stem Cell Ther. 2017;10:252‐258. [DOI] [PubMed] [Google Scholar]
- 6. Marks DI, Alonso L, Radia R. Allogeneic hematopoietic cell transplantation in adult patients with acute lymphoblastic leukemia. Hematol Oncol Clin North Am. 2014;28:995‐1009. [DOI] [PubMed] [Google Scholar]
- 7. Aldoss I, Stein AS. Advances in adult acute lymphoblastic leukemia therapy. Leuk Lymphoma. 2018;59:1033‐1050. [DOI] [PubMed] [Google Scholar]
- 8. Blum S, Martins F, Lübbert M. Immunotherapy in adult acute leukemia. Leuk Res. 2017;60:63‐73. [DOI] [PubMed] [Google Scholar]
- 9. Löffler A, Gruen M, Wuchter C, et al. Efficient elimination of chronic lymphocytic leukaemia B cells by autologous T cells with a bispecific anti–CD19/anti–CD3 single‐chain antibody construct. Leukemia. 2003;17:900‐909. [DOI] [PubMed] [Google Scholar]
- 10. Bargou R, Leo E, Zugmaier G, et al. Tumor regression in cancer patients by very low doses of a T cell‐engaging antibody. Science. 2008;321:974‐977. [DOI] [PubMed] [Google Scholar]
- 11. Raponi S, De Propris MS, Intoppa S, et al. Flow cytometric study of potential target antigens (CD19, CD20, CD22, CD33) for antibody‐based immunotherapy in acute lymphoblastic leukemia: analysis of 552 cases. Leuk Lymphoma. 2011;52:1098‐1107. [DOI] [PubMed] [Google Scholar]
- 12. Piccaluga PP, Arpinati M, Candoni A, et al. Surface antigens analysis reveals significant expression of candidate targets for immunotherapy in adult acute lymphoid leukemia. Leuk Lymphoma. 2011;52:325‐327. [DOI] [PubMed] [Google Scholar]
- 13. Topp MS, Gökbuget N, Stein AS, et al. Safety and activity of blinatumomab for adult patients with relapsed or refractory B‐precursor acute lymphoblastic leukaemia: a multicentre, single‐arm, phase 2 study. Lancet Oncol. 2015;16:57‐66. [DOI] [PubMed] [Google Scholar]
- 14. Kantarjian H, Stein A, Gökbuget N, et al. Blinatumomab versus chemotherapy for advanced acute lymphoblastic leukemia. N Engl J Med. 2017;376:836‐847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Stein AS, Schiller G, Benjamin R, et al. Neurologic adverse events in patients with relapsed/refractory acute lymphoblastic leukemia treated with blinatumomab: management and mitigating factors. Ann Hematol. 2019;98:159‐167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. van der Velden VH, Cazzaniga G, Schrauder A, et al. Analysis of minimal residual disease by Ig/TCR gene rearrangements: guidelines for interpretation of real‐time quantitative PCR data. Leukemia. 2007;21:604‐611. [DOI] [PubMed] [Google Scholar]
- 17. Nägele V, Kratzer A, Zugmaier G, et al. Changes in clinical laboratory parameters and pharmacodynamic markers in response to blinatumomab treatment of patients with relapsed/refractory ALL. Exp Hematol Oncol. 2017;6:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zhu M, Wu B, Brandl C, et al. Blinatumomab, a bispecific T‐cell engager (BiTE®) for CD‐19 targeted cancer immunotherapy: clinical pharmacology and its implications. Clin Pharmacokinet. 2016;55:1271‐1288. [DOI] [PubMed] [Google Scholar]
- 19. Simon R. Optimal two‐stage designs for phase II clinical trials. Control Clin Trials. 1989;10:1‐10. [DOI] [PubMed] [Google Scholar]
- 20. Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Statist Soc B. 1995;57:289‐300. [Google Scholar]
- 21. Zhu M, Kratzer A, Johnson J, et al. Blinatumomab pharmacodynamics and exposure‐response relationships in relapsed/refractory acute lymphoblastic leukemia. J Clin Pharmacol. 2018;58:168‐179. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


