Abstract
Background
The aim of this study was to investigate the imaging manifestations of early-stage coronavirus disease 2019 (COVID-19) and to provide imaging basis for early detection of suspected cases and stratified intervention.
Material/Methods
From 20 January 2020 to 2 February 2020, 6 patients diagnosed with COVID-19, including 1 male and 5 females, were retrospectively reviewed in Zhejiang Hospital. These cases were clinically assessed and classified as common COVID-19. All patients underwent thoracic high-resolution computed tomography (HRCT) within 2 days after the onset of symptoms, and their images were viewed by 2 radiologists who were blind to their clinical records.
Results
CT images of 6 confirmed patients were collected. Two of the 6 patients (33.3%) had bilateral lung involvements and 4 (66.7%) had single-lung involvement. Two cases (33.3%) had a single lesion, 2 cases (33.3%) had 2 lesions, and 2 cases (33.3%) had multiple lesions. There were 2 cases (33.3%) with focal subpleural distribution and 1 case (16.7%) along the bronchial vascular bundle. Five cases (83.3%) had ground-glass opacities, 4 cases (66.7%) had ground-glass nodules, 1 case (16.7%) had thickened lobular septum, 2 cases (33.3%) had thickened bronchial wall, 2 cases (33.3%) had halo sign, 1 case (16.7%) had crazy-paving sign, and 1 case (16.7%) had tree-in-bud sign.
Conclusions
The imaging manifestations of early-stage COVID-19 are relatively mild, and the imaging findings of some patients are not typical, which can easily lead to missed diagnoses. Thus, suspected cases need to be closely monitored, and epidemiological history and clinical laboratory examination should also be considered during diagnosis.
MeSH Keywords: Coronavirus Infections; COVID-19; Pneumonia, Viral; X-Ray Computed Tomography
Background
Since December 2019, a series of unexplained pneumonia cases spread in Wuhan, China. The clinical manifestations of pneumonia were similar to those of viral pneumonia. The source of the infection was a novel coronavirus, which was known as 2019 novel coronavirus (2019-nCoV), and the disease was then named coronavirus disease 2019 (COVID-19) [1–3]. At present, COVID-19 has spread throughout the world with an increasing number of confirmed and suspected cases. Thoracic high-resolution computed tomography (HRCT), a highly feasible imaging method, plays an important role in the screening and treatment evaluation of COVID-19. We retrospectively reviewed 6 cases diagnosed with COVID-19 in our hospital to better understand the imaging features of early-stage pneumonia and provide radiologists with key diagnostic points.
Material and Methods
From 20 January 2020 to 2 February 2020, 6 patients diagnosed with COVID-19 in our hospital were recruited, including 1 male and 5 females (average age 40±10 years) (Table 1). All patients underwent HRCT within 2 days after the onset of symptoms. All 6 patients had visited Wuhan or had contact with a confirmed COVID-19 patient. The clinical manifestations of these patients included fever, cough, sore throat, and fatigue. All patients were positive for 2019 novel coronavirus nucleic acid via laboratory testing of respiratory secretions obtained by bronchoalveolar lavage, endotracheal aspirate, nasopharyngeal swab, or oropharyngeal swab. HRCT images were acquired using a GE scanner (GE Medical Systems Optima CT540) with slice thickness of 1.25 mm. The images were transmitted to the workstation and viewed in the PACS system.
Table 1.
Demographic and lung lesions in HRCT of the included 6 patients.
| No. | |
|---|---|
| Age | 40 (y)±10 |
| M/F | 1/5 |
| Number of lesions | |
| 1 lesion | 2 (33.3%) |
| 2 lesions | 2 (33.3%) |
| ≥3 lesions | 2 (33.3%) |
| GGO | 5 (83.3%) |
| Nodules | 4 (66.7%) |
| Halo sign | 2 (33.3%) |
| Thickened lobular septum | 1 (16.7%) |
| Tree-in-bud sign | 1 (16.7%) |
Data are presented as numbers (%) or median (IQR).
CT images were evaluated by 2 experienced radiologists. In case of disagreement, a third senior radiologist offered an opinion and made the decision. Imaging features were evaluated in the following patterns:
Location of involved lung lobes: bilateral lungs were divided into right upper lobe, right middle lobe, right lower lobe, left upper lobe, and left lower lobe;
Number of lesions: divided into 1 lesion, 2 lesions, and ≥3 lesions;
Lesion distribution: subpleural distributed, bronchial vascular bundle distributed;
Imaging manifestations: ground-glass opacities, consolidation, nodules, halo signs, fibrosis around the lesion, air bronchogram, thickening of the lobular septum, thickening of the bronchial wall, and other pleural and mediastinal abnormalities: emphysema, cavitation, pleural thickening, pleural effusion, and enlarged mediastinal lymph nodes.
Results
CT imaging features of COVID-19 in our 6 patients (Figure 1) are summarized below:
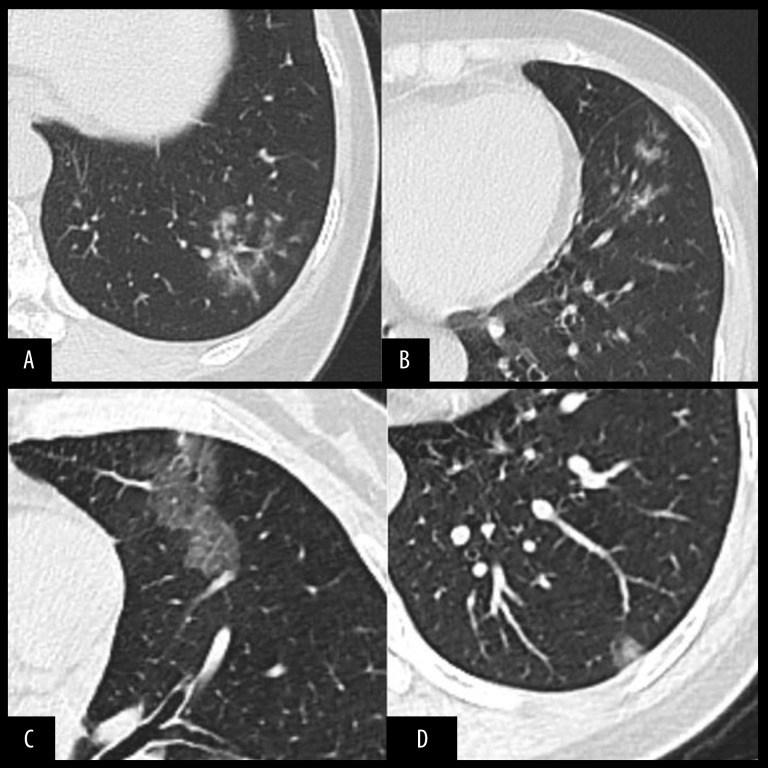
Figure 1.
(A, B) Shows the HRCT images of a 53-year-old female with fever for 5 days. Ground-glass opacity around bronchial trees can be seen in the left lower lobe with tree-in-bud sign. (C) Shows the HRCT image of a 52-year-old female with fever (highest temperature 38°C). Ground-glass opacity with thickened lobular septum can be seen in left upper lobe. (D) Shows the HRCT image of a 30-year-old female with shortness of breath and cough. Ground-glass nodule can be seen in the peri-pleural region of left lower lobe.
Distribution: 2 cases (33.3%) had bilateral lung involvement and 4 cases (66.7%) had single-lung involvement. In details, 1 case (16.7%) had right upper-lobe involvement, 3 cases (50%) had right middle-lobe involvement, and 1 (16.7%) had right lower-lobe involvement, 3 (50%) had left upper-lobe involvement, and 3 (50%) had left lower-lobe involvement.
Number of lesions: 2 cases (33.3%) only had a single lesion, 2 cases (33.3%) had 2 lesions, and 2 cases (33.3%) had multiple lesions.
Lesion distribution: There were 2 cases (33.3%) with subpleural lesions and 1 case (16.7%) along the bronchial vascular bundle.
Imaging features: 5 cases (83.3%) had ground-glass opacities; consolidation was not found in any patient; 4 cases (66.7%) had ground-glass nodules; 1 case (16.7%) had thickened lobular septum; 2 cases (66.7%) had thickened bronchial wall; 2 cases (33.3%) had focal halo sign;1 case (16.7%) had crazy-paving sign; 1 case (16.7%) had tree-in-bud sign; and 1 case (16.7%) had proliferation and calcification in the right upper lobe, which was considered as chronic tuberculosis.
Discussion
COVID-19 cases are clinically categorized into 4 types – mild, normal, severe, and critical – according to the “Diagnosis and Treatment Plan for Novel Coronavirus Pneumonia (Fifth Edition)”. Based on their imaging feathers, COVID-19 can also be categorized into early stage, progressive stage, peak stage and absorption stage [4]. Studies show that early-stage COVID-19 usually manifests as localized inflammatory infiltration, with subpleural ground-glass opacity (GGO) in both lungs. Lesions are usually associated with thickened micro-vessels and thick-walled bronchi. If an air bronchogram accompanied with or without thickened interlobular septum can be seen within the lesion, a halo sign may also appear around the lesion. In rare cases, initial CT images are normal, while follow-up scans are positive [5].
The imaging features we observed in the present study are similar to other studies, with minor differences. Two patients with a single lesion only showed small-nodule or small-patchy GGO. One patient who presented with bronchiolitis showed tree-in-bud (TIB) sign (Figure 1A, 1B), which is a rare imaging sign in viral infections, and this is the first report of this in a COVID-19 patient. The pathological basis of TIB is that mucus or pus blocking alveolar duct, respiratory bronchioles, and terminal bronchioles causes bronchiectasis, thickening of the bronchiole wall, and peribronchial inflammation [6]. Tree-in-bud sign can be seen in viral infection patients with immune dysfunction [7].
Conclusions
We found that some of the imaging features of COVID-19 are atypical, especially at the early stage, and this can lead to missed diagnoses. Thus, clinicians should use multiple diagnostic methods such as epidemiological history, clinical characteristics, laboratory tests, and etiological characteristics to make the final diagnosis. Among these, HRCT is of great importance due to its feasibility, which allows it to be widely used in screening and treatment response evaluation.
Footnotes
Source of support: Departmental sources
References
- 1.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–73. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhu N, Zhang DY, Wang WL, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–33. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pan F, Ye T, Sun P, et al. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology. 2020 doi: 10.1148/radiol.2020200370. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lei J, Li J, Li X, et al. CT imaging of the 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;295(1):18. doi: 10.1148/radiol.2020200236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Im JG, Itoh H, Shim YS, et al. Pulmonary tuberculosis: CT findings – early active disease and sequential change with antituberculous therapy. Radiology. 1993;186(3):653–60. doi: 10.1148/radiology.186.3.8430169. [DOI] [PubMed] [Google Scholar]
- 7.Elicker BM, Schwartz BS, Liu C, et al. Thoracic CT findings of novel influenza A (H1N1) infection in immunocompromised patients. Emerg Radiol. 2010;17(4):299–307. doi: 10.1007/s10140-010-0859-x. [DOI] [PMC free article] [PubMed] [Google Scholar]