Abstract
Mandibular condylar fractures are among the most common facial fractures and some of the most difficult to manage. Opinions about the management of mandibular condylar fractures differ among surgeons. With the implementation of new technology, an increased understanding of fracture management, and better functional and morphological outcomes reported in the literature, open reduction and internal fixation is becoming many surgeons’ preferred choice for the treatment of condylar fractures. Because surgical treatment of such fractures is complex, certain factors must be considered to achieve satisfactory outcomes. In this article, we summarise six key points in the management of mandibular condylar fractures: virtual evaluation of condylar fracture, a suitable surgical approach, good reduction, stable internal fixation, repair of the articular disc, and restoration of the mandibular arch width. We believe that these points will help to improve the prognosis of mandibular condyle fractures.
Keywords: Mandibular fractures, Condylar fractures, Template
Introduction
The U-shaped mandible is the most prominent facial bone and a common site of trauma, constituting 12%–56% of facial fractures.1,2 Condylar fractures account for about 29%–52% of all mandibular fractures.3,4 The consequences of condylar fractures are mandibular movement disorders, temporomandibular joint (TMJ) dysfunction, malocclusion, and chewing dysfunction, all of which may affect the patient's physiologic function and mental health. If a condylar fracture is not managed properly, the patient may develop malocclusion, limited mouth opening, facial deformity, TMJ disorders, and ankylosis.5 Therefore, timely and suitable treatment of mandibular condyle fractures is indispensable for beneficial results.6
There are two principal management procedures for condylar fractures: conservative treatment and surgical treatment. Many authors have described conservative treatment as safe, non-invasive, easy, and low-cost, but they have also described complications including poor oral hygiene, gingivitis, facial deformity, TMJ dysfunction, and even TMJ ankylosis.5,7,8 Surgical treatment also has disadvantages such as its high cost, scar formation, intraoperative haemorrhage, facial nerve injury, and others.8 In recent years, with the implementation of new technology and improved understanding of fracture management, most complications of surgical treatment have been diminished and even avoided. Furthermore, many studies have shown that surgical treatment can provide better functional and morphological outcomes because it facilitates anatomic reduction, rigid internal fixation and faster functional restoration.9,10 In a study of 66 patients with displaced condylar fractures conducted by Schneider et al.,11 the functional results were better in the patients who underwent open reduction and internal fixation rather than conservative treatment. Similarly, a study by Mohammed et al.8 compared the outcomes of various parameters after open reduction with internal fixation versus nonsurgical treatment showed that better outcomes were obtained with surgical treatment in terms of deviation on mouth opening, the occlusal status, and anatomic reduction of the condyle. Thus, open reduction and internal fixation is becoming many surgeons’ preferred choice for the treatment of condylar fractures.
Although many authors are expressing a preference for surgical treatment, surgical treatment of condylar fractures is still more difficult than that of other mandibular fractures for several reasons. At first, there are many complex anatomic structures within a small area around the condyle, including the parotid gland, facial nerve, superficial temporal vessels, maxillary vessels, and others. At second, serious complications can occur intraoperatively or postoperatively, including massive bleeding, facial nerve injury, malocclusion, facial deformity, and even TMJ ankylosis. At third, mandibular growth disturbances and even severe mandibular deficiencies should be considered in growing patients.
In recent years, a number of studies were reported to solve above problems.12, 13, 14, 15 The treatment methods of condylar fracture have been enriched and the prognosis have been improved. Some new methods have been used to assist the surgical treatment of condylar fractures in our department, which include new surgical approach, surgical navigation, and so on. Satisfactory therapeutic effects have been obtained in recent years.
We herein summarise six key points in the surgical management of condylar fractures and anticipate that these points will help surgeons to achieve satisfactory results with minimal or no complications. These key points are virtual evaluation of condylar fracture, a suitable surgical approach, good reduction, stable internal fixation, repair of the articular disc, and restoration of the mandibular arch width.
Virtual evaluation of condylar fractures
There is a famous sentence in The Art of War written by Sun Tzu, an ancient Chinese military strategist Know the enemy and know yourself, and you'll fight a hundred battles without defeat. As in war, obtaining comprehensive and accurate preoperative information is a key to successful surgical treatment.
Although computed tomography is considered the gold standard examination technique for the diagnosis and classification of condylar fractures, it cannot provide a visualized view of the fracture site or detailed surgical data. Computer-assisted preoperative simulation, commonly known as virtual surgical planning (VSP), was recently introduced for the management of mandibular condylar fractures. VSP enables analysis of the fracture site from different aspects, allowing the surgeon to predict reduction and fixation of the fragment or stump.
In 2012, Yang et al.16 used a three-dimensional (3D) simulation system in which the fractured segment was reduced to the remaining mandibular segment and reference data for the position and size of the screw were obtained preoperatively. These preoperative references were implemented during the operative procedure. The authors concluded that pre-surgical virtual evaluation of condyle not only reduces the operating time and assists in better reduction but also reduces operational errors. Furthermore, it could help surgeons choose the most suitable plates and screws before the operation. In 2016, Boffano et al.17 also reported the benefits of using VSP to preoperatively determine the optimal length and position of screws along with the angle of the hole to be drilled for fixation of the fractured condylar segment, thus increasing the intraoperative efficiency of the procedure. Virtual evaluation of condyle also allows the surgeon to compare and optimise various surgical options. Voss et al.18 concluded that VSP provides surgeons a better understanding of the fracture pattern, aiding better anatomic reduction. It also provides an opportunity to compare various surgical approaches and fixation options.
Based on above-mentioned literature and our practical experience, the applications of VSP in condylar fracture management can be summarised as follows: (1) facilitation of a precise diagnosis; (2) assistance in choosing the best surgical protocol; (3) provision of detailed data for reduction and fixation19,20; (4) assistance in navigation and design of reposition templates21; (5) avoidance of unnecessary tissue manipulation, diminishing operative errors16; (6) prediction of the postoperative outcome; and (7) facilitation of communication between the patient and surgeon.22 We also believe that virtual evaluation along with VSP of fractured condyle can shorten the operating time, enhance precise reduction, and improve the accuracy of hardware placement, resulting in better postoperative outcomes. Therefore, we advocate the use of virtual evaluation for all condylar fractures and also preoperative surgical planning (Fig. 1).
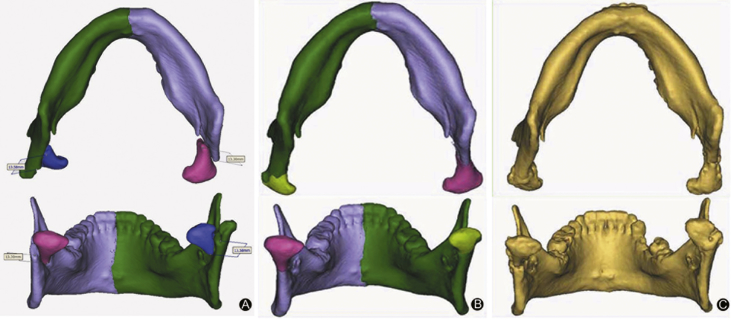
Fig. 1.
A 44-year-old man diagnosed with bilateral condylar fractures underwent surgical management assisted by virtual surgical planning. (A) Preoperative three-dimensional reconstruction showing bilateral condylar fractures using Mimics software; (B) Simulated reduction of the fractured condyles using Mimics software; (C) Postoperative three-dimensional reconstruction view of the reduced condyles.
Suitable surgical approach
A well-chosen surgical approach is the first and key step during the surgical procedure to maximally avoid complications associated with the procedure, such as facial nerve injuries and massive bleeding. Any surgical approach chosen must provide direct visualisation of the fractured segment, adequate accessibility for reduction and placement of fixation materials, and minimal invasiveness with few postoperative complications. The decision regarding the surgical approach that will be used to reach the condylar fracture mainly depends on the location and type of fracture. Several important anatomical structures must also be considered, including nerves, blood vessels, and the parotid gland.
Several different approaches for the treatment of condylar fractures have been described, including the preauricular, retromandibular, post-auricular, and submandibular approaches. Among these, the most widely used are the preauricular and retromandibular approaches. Surgical management has become easier since the introduction of endoscopic-assisted open reduction. Transoral endoscopic-assisted condylar fixation has gained popularity due to the surgeon's direct visualisation of the magnified and illuminated operative field and the assistant's unobstructed view, thus overcoming the problems of the intraoral approach. However, direct visualisation and accessibility of the fracture site are still difficult. Moreover, specialised instruments and training are necessary.
The preauricular approach was first described by Thoma in 1945 and is commonly preferred for condylar head and neck fractures. This approach is especially useful for medially displaced condylar fragments. Its advantages include excellent access to the fractured stump, convenient manipulation of the fractured segment, and minimal or invisible scar formation. The main risk associated with this approach is facial nerve injury. To maximally avoid the risk of facial nerve injury, we modified this technique to a supratemporalis approach.3 In contrast to the traditional preauricular approach, the separation plane in the supratemporalis approach is located between the deep temporal fascia and the temporalis. We have found that the supratemporalis approach prevents facial nerve injury and does not increase the frequency of other complications. Therefore, it should be routinely used as a safe treatment approach for condylar head fractures.
The retromandibular approach was first described by Hinds in 1967. This approach provides excellent visualisation of the neck and base of the condyle. Advantages of this approach include a shorter working distance from the skin incision to the condyle; good access and visualisation of the posterior border of the mandible and sigmoid notch, facilitating fracture manipulation and reduction; and a well hidden or inconspicuous scar.23,24 However, this method requires a bisecting incision through the parotid gland, increasing the risk of facial nerve injury and the formation of sialocoeles or salivary fistulas. Therefore, we designed the minor parotid anterior approach as a modified approach to treat condylar neck and base fractures.4 Both the clinical outcomes and the results of our study showed that the minor anterior parotid approach has many advantages: good exposure, minimal scarring, simple manipulation, a short operating time, and minimal risk to the facial nerve. Thus, it is the best treatment choice for condylar neck and base fractures.
In 2018, Al-Moraissi et al.25 evaluated the risk of facial nerve injury in reference to various surgical approaches. Similar to our findings, they concluded that the retromandibular approach with either trans-masseteric anteroparotid or subparotid dissection for condylar base and condylar neck fractures and the deep subfascial approach for condylar head fractures are associated with the lowest risk of nerve damage.
Good reduction
Good reduction is a key to successful treatment of any fracture. Detailed knowledge of the anatomy and position of the fracture along with proper manipulation allows for more ideal anatomic reduction. Reduction followed by stabilisation before fixation is also an important procedure. Reduction is accomplished by the use of small retractors to retract the surrounding structures and the use of hooks and periosteal elevators to manipulate the fractured portion and position it at the residual condyle. Although this procedure sounds simple and easy, it is difficult to handle the fractured portion and position it back to the anatomically ideal site in patients with condylar fractures because of the high number of anatomic structures, pulling of muscle tissues, and restricted view of the operative site.
Although minimally invasive surgical treatment has become more widespread during the past several decades, direct vision and accessibility are limited in some cases. In 2011, Klatt et al.26 showed that the use of intraoperative 3D C-arm cone-beam computed tomography enables monitoring of the result of reduction of the mandibular condylar process in all three planes, providing more accurate reduction.
Navigation-based surgical techniques were recently introduced to condylar fracture treatment, enabling real-time 3D intraoperative imaging that allows us to view the procedure while in progress, helping to guide reduction in the desired anatomical position. The authors reported a study on the treatment of condylar head fractures with a navigation technique in 2018.27 The results showed that surgeons can perform better reduction and fixation of intracapsular fractures, thus achieving satisfactory treatment outcomes. Although studies on achieving ideal anatomic reduction with newly developed technology in minimally invasive surgery are in progress, we cannot deny the benefits achieved by preoperative digital 3D reconstruction and planning for fracture reduction (Fig. 2).
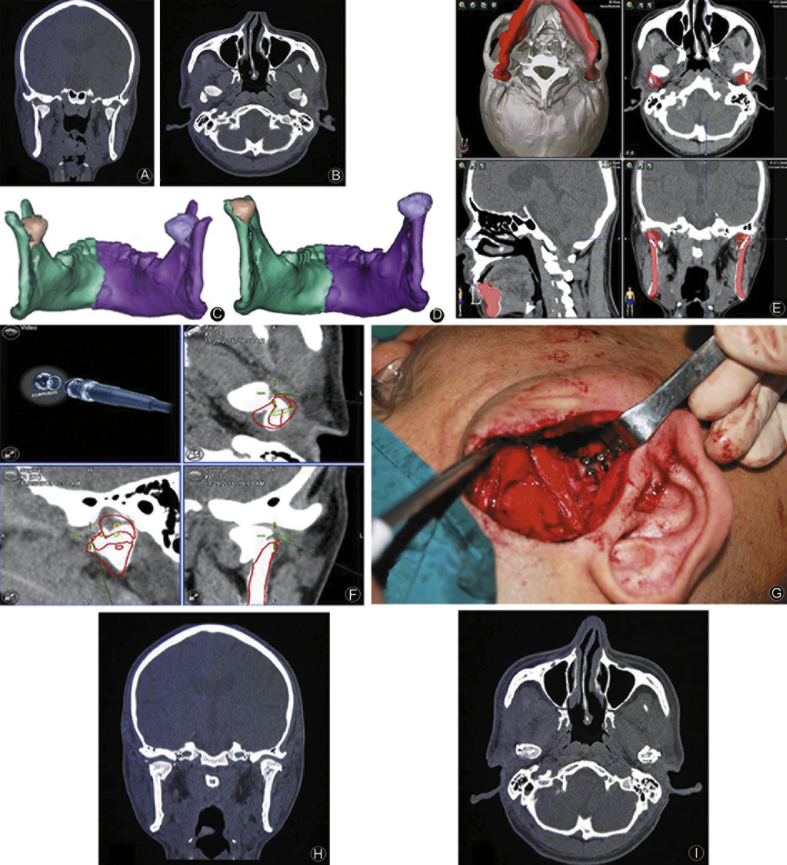
Fig. 2.
A 32-year-old man was diagnosed with bilateral condylar fractures and underwent surgical management using navigation technology. (A, B) Preoperative coronal and axial computed tomography view of the condylar fractures; (C) Preoperative design and simulation using Brainlab iPlan CMF software; (D) Preoperative three-dimensional reconstruction of the condyle; (E) Three-dimensional reconstruction after simulation reduction using Mimics software; (F, G) Intraoperative real-time navigation visualisation and tip of the navigation probe positioned at the fractured portion; (H, I) Postoperative coronal and axial computed tomography view of the condyle.
VSP can be transferred to a guided template and used to assist the reduction of the fractured portion.28, 29, 30 The use of guided templates is lacking in the field of condylar fractures, but such templates have been proven useful for good reduction in other fields. Therefore, we created digital templates and used them to assist in the reduction of condylar fractures. The results showed that the templates help in precise intraoperative reduction and decrease the operative time (Fig. 3). Use of a template confers no additional risk to critical anatomical structures. Moreover, the template aids in correct bending of the plates without distortion or over-bending, thus avoiding breakage of the instruments and facilitating ease of application. However, there are some limitations in using templates. The preoperative process is more complicated and time-consuming. Furthermore, extended detachments of the periosteum and muscles are often needed to place the templates, which sometimes bring more risk of postoperative bone resorption and infection. We therefore encourage the use of guided templates for the reduction of condylar fractures only when necessary.
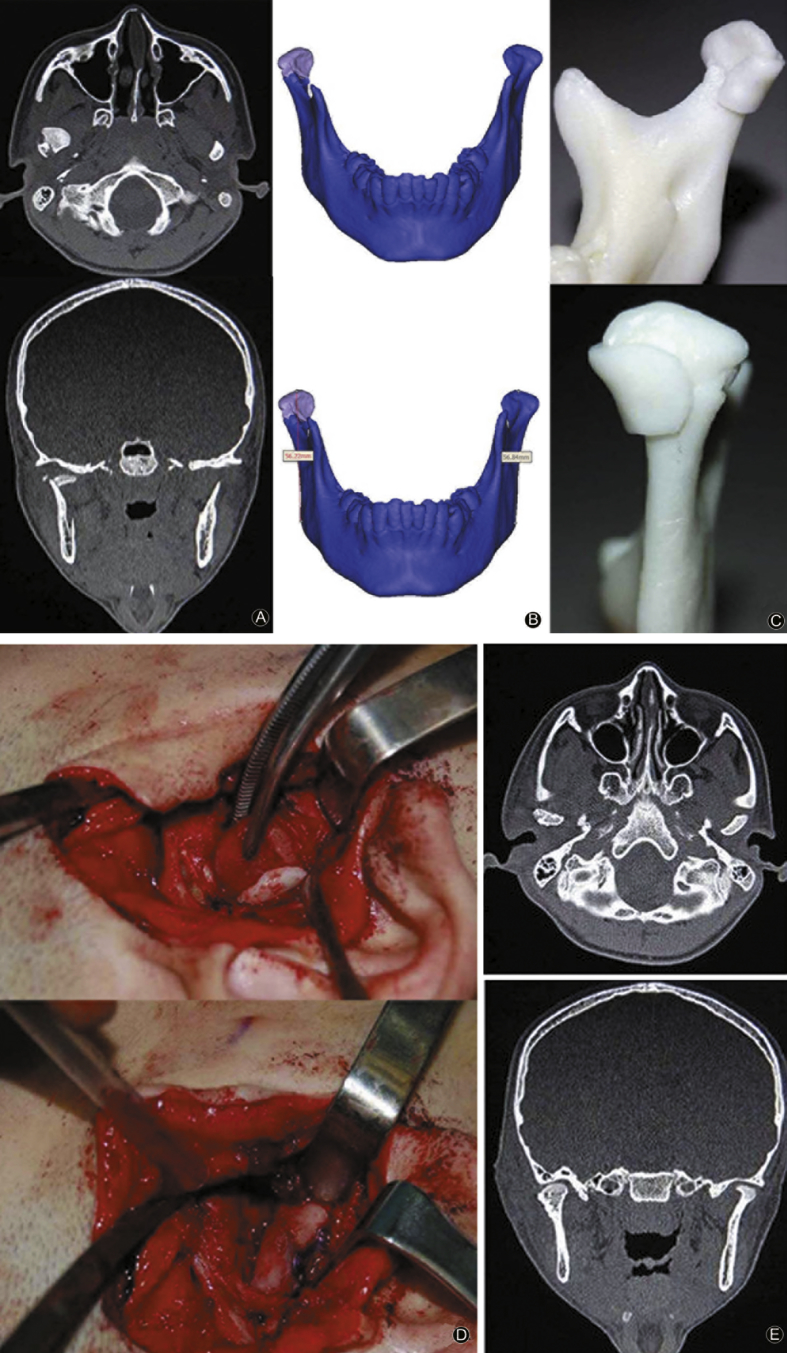
Fig. 3.
A 16-year-old female patient was diagnosed with a right condylar fracture and underwent surgical treatment assisted by a guided template. (A) Preoperative axial and coronal computed tomography views of the condylar fracture; (B) Three-dimensional reconstruction after simulated reduction using Mimics software; (C) Construction of guided template and preoperative analysis with three-dimensional constructed model; (D) Intraoperative positioning of the guided template for reduction and fixation; (E) Postoperative computed tomography view of the condyle.
Stable internal fixation
After successful reduction, the fractured portion must be stabilised and then fixed. Fixation with a sufficient number of titanium plates and screws at the proper site must be strong enough to withstand the functional loads sustained during bone healing. Champy established the scientific foundation for the use of a semi-rigid fixation technique in mandibular fractures. There are two ideal osteosynthesis lines: the superior line runs parallel under the sigmoid notch and is intended to restore the tension forces located in the condylar region, and the inferior line is located vertically in the axis of the condylar neck and is intended to maintain the reduction out of the sagittal plane as rotation strain (in the axial plane) and bending strain (in the frontal plane), which may occur during function.
For the condylar neck and base, we use two four-hole miniplates, either straight or L-shaped, with the two holes on either side of the fracture line. Advances in technology have led to the development of geometric condylar plates that may be trapezoidal, rhomboidal,31 or Y-shaped for stable and rigid fixation.32, 33, 34 Many authors have performed finite element analysis to determine the mechanical strength of these geometric condylar plates.33,35 Therefore, many surgeons currently prefer the use of two straight miniplates or the use of 3D trapezoidal plates for condylar neck and base fractures.
Condylar head fractures are more widely fixated with the use of two screws drilled through the lateral pole of the condyle, below the lateral attachment of the capsule or over the condylar neck. With medial displacement of the condylar head fragment, this intraoperative approach is difficult to achieve with minimal invasion. Therefore, the same preoperative digital planning that is used for accurate localisation and establishment of the number of fragments in the fractured portion also aids in preoperative approximation of the location, angulation, and length of the screw for better osteosynthesis.
Although titanium plates have long-term reliability and biocompatibility, they are still associated with a risk of future failure necessitating removal; the re-entry operation in such cases adds functional and aesthetic risks. Therefore, resorbable screws and plates made of polylactic acid, polyglycolic acid, or polydioxane have been introduced.36,37 Their main advantage is no need for re-entry. However, their use is not cost-effective, and they have not been adequately studied for treatment of condylar fractures. There is a risk of screw loosening and displacement with the use of resorbable fixation material.38
Repair of the articular disc
Successful management of condylar fractures requires not only stable osteosynthesis of the fracture segment but also restoration of the pre-traumatic anatomic reduction of the articular disc. Soft tissue injury within the TMJ after the condylar fracture includes displacement of the disc, tearing of retrodiscal tissue, and tearing of the lateral capsule. Articular disc displacement commonly occurs after a condylar fracture; the incidence of such displacement with intracapsular condylar fractures ranges from 79% to 100%.39 Displacement of the articular disc leads to TMJ disorders and may even result in ankylosis in the long term. Therefore, repair of the articular disc is also an important key factor for satisfactory outcomes of surgical treatment.
In most cases, the disc is displaced anteromedially and can be reduced to its anatomical position without difficulty. When the disc is difficult to reduce, the superior lateral pterygoid muscle is released, allowing passive repositioning of the disc. Additionally, when the disc is torn, it is sutured first and then reduced to its anatomical position. Repositioning is done by placing two nonabsorbable horizontal mattress sutures at the junction of the disc and retrodiscal tissue, then one suture is placed through the medial aspect of the posterior band and another through its lateral aspect. The suture is secured to the disc with knots and anchored to the screw positioned to the posterior condylar slope (Fig. 4). As the disc is repositioned, no gap should be present between the disc and fossa. If a gap is present, then the space should be filled with subcutaneous fat harvested from the preauricular region to prevent relapse caused by fibrosis and scar contracture. Correct disc positioning is assessed by gently translating the condyle forward onto the eminence and back into the fossa.40,41
Fig. 4.
Articular disc repositioning. (A) Reduction of articular disc using sutures; (B) Reduced articular disc anchored to the screw placed in the posterior condylar slope.
If the disc is damaged and cannot be reused, then it must be replaced with suitable interpositional material. Various tissue grafts are available, and each has advantages and disadvantages. Grafts that can be used as articular discs are the temporalis flap, dermis graft, fat graft, and tissue-engineered TMJ disc.42 The literature has also described the characteristics of an ideal interpositional graft, and no currently available materials fulfil all of these characteristics.43 The temporalis flap has been widely used for articular disc replacement of the TMJ with superior outcomes.43, 44, 45 The temporalis flap has several advantages when used as an articular disc in the TMJ, including (1) close proximity to the fracture site, (2) no need for an additional surgical site, (3) adequate blood supply, (4) autogenous in origin, and (5) preservation of the attachment to the coronoid process, which simulates the physiologic action of the disc during flap movement.46
Restoration of mandibular arch width
A condylar fracture can occur along with other mandibular body fractures. During trauma, the force directly applied to the body of the mandible is distributed along the total mandible. Compressive strain in the buccal region and tensile strain in the lingual region occurs; as a result, a lingual gap may develop despite the fact that no fracture is obvious buccally. This results in an increased arch width with lateral dislocation of the condyle. The combination of a condylar fracture and mandibular body fracture results in a clearly increased transverse dimension of the condyle and ramus, resulting in widening of the mandibular arch, occlusion disorders, and limited mouth opening. When this widened arch is not resolved, the tension of the suprahyoid, masseter, and temporalis muscles displaces the lateral pole of the condyle into a superolateral position, moving it into direct contact with the zygomatic arch and leading to ankylosis in the long term.
To restore the arch width and obtain better surgical treatment outcomes, the displaced condyle must be returned into its anatomic position. This can be accomplished when the assistant surgeon applies strong pressure on the gonial angle with the fingers or hands with simultaneous forward traction applied close to the bony edge, thus reducing the body fracture together with application of plates over the fractured area.47, 48, 49 The plates used for fractures of the mandibular body should be over-bent to apply compression to the lingual cortex and eliminate the tendency for gap formation.
In patients with segmental fractures, widening of the mandibular arch is more significant in the presence of the condylar fracture. Strong osteosynthesis in the mandibular body is essential to stabilise the condyle and maintain the transverse dimension of the face. Therefore, a reconstruction plate is often chosen to provide adequate stability and thus prevent further widening, malocclusion, possible joint derangement, and a cosmetically unacceptable result.50,51 It is also beneficial to over-bend the plate in the lingual direction.
Use of a miniplate can be problematic because of the diastasis of the lingual cortical surface. In such cases, use of a lag screw in the inferior and superior borders can help to achieve perfect stabilisation by bringing the fractured bone surface in contact.52
In addition to preoperative and intraoperative factors, postoperative rehabilitation is also equally important. Postoperative rehabilitation includes the period of inter-maxillary fixation, mouth opening exercises, and a soft diet, all of which are essential to achieve a superior functional outcome.
Although we have herein summarised the key points for successful surgical treatment, surgeons may still encounter many difficulties. VSP software that can effectively reduce imperfections during separation of the fractured segment has not yet been designed, and virtual reduction and exact simulation are sometimes difficult, mostly in cases of comminuted fractures.
There is a need for improvised instruments that can help to achieve better reduction and stabilisation of the fractured portion of the condyle before fixation. Additionally, many studies and experiments have been performed to assess the biomechanical properties and clinical effectiveness of different fixation materials for mandibular condyle fractures. Furthermore, new plating systems are being developed. However, no plates have yet been proven satisfactory. We believe that further development of pre-formed plates is needed to reduce the intraoperative time and increase stability.
The six key factors described in the present report are essential for successful surgical management of any condylar fracture. However, more research, better preoperative planning software, and the development of new instruments for reduction and fixation that minimise the operation time and facilitate easier surgical procedures are necessary.
Funding
Nil.
Ethical Statement
Not applicable.
Acknowledgements
We appreciate all patients in this study for their participation, understanding and cooperation.
Declaration of Competing Interest
The authors declared no conflicts of interest.
Footnotes
Peer review under responsibility of Chinese Medical Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.cjtee.2019.08.006.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Hackenberg B., Lee C., Caterson E.J. Management of subcondylar mandible fractures in the adult patient. J Craniofac Surg. 2014;25:166–171. doi: 10.1097/SCS.0000000000000498. [DOI] [PubMed] [Google Scholar]
- 2.Smith H., Peek-Asa C., Nesheim D. Etiology , diagnosis , and characteristics of facial fracture at a midwestern level I trauma center. J Trauma Nurs. 2012;19:57–65. doi: 10.1097/JTN.0b013e31823a4c0e. [DOI] [PubMed] [Google Scholar]
- 3.Li H., Zhang G., Cui J. A modified preauricular approach for treating intracapsular condylar fractures to prevent facial nerve injury: the supratemporalis approach. J Oral Maxillofac Surg. 2016;74:1013–1022. doi: 10.1016/j.joms.2015.12.013. [DOI] [PubMed] [Google Scholar]
- 4.Hou J., Chen L., Wang T. A new surgical approach to treat medial or low condylar fractures: the minor parotid anterior approach. J Oral Med Oral Surg Oral Pathol Oral Radiol. 2014;117:283–288. doi: 10.1016/j.oooo.2013.11.491. [DOI] [PubMed] [Google Scholar]
- 5.Choi K.Y., Yang J.D., Chung H.Y., Cho B.C. Current concepts in the mandibular condyle fracture management part I: overview of condylar fracture. Arch Plast Surg. 2012;39:291–300. doi: 10.5999/aps.2012.39.4.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fama F., Cicciu M., Sindoni A. Maxillofacial and concomitant serious injuries: an eight-year single center experience. Chin J Traumatol. 2017;20:4–8. doi: 10.1016/j.cjtee.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Valiati R., Ibrahim D., Abreu M.E. The treatment of condylar fractures: to open or not to open? A critical review of this controversy. Int J Med Sci. 2008;5(6):313–318. doi: 10.7150/ijms.5.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shiju M., Rastogi S., Gupta P. Fractures of the mandibular condyle - open versus closed - a treatment dilemma. J Cranio-Maxillofacial Surg. 2015;43:448–451. doi: 10.1016/j.jcms.2015.01.012. [DOI] [PubMed] [Google Scholar]
- 9.Chrcanovic B.R. Meta-analysis surgical versus non-surgical treatment of mandibular condylar fractures: a meta- analysis. Int J Oral Maxillofac Surg. 2015;44:158–179. doi: 10.1016/j.ijom.2014.09.024. [DOI] [PubMed] [Google Scholar]
- 10.Ragupathy K. Outcomes of surgical versus nonsurgical treatment of mandibular condyle fractures. Int Surg J. 2016;3:47–51. [Google Scholar]
- 11.Schneider M., Erasmus F., Gerlach K.L. Open reduction and internal fixation versus closed treatment and mandibulomaxillary fixation of fractures of the mandibular condylar process: a randomized, prospective, multicenter study with special evaluation of fracture level. J Oral Maxillofac Surg. 2008;66:2537–2544. doi: 10.1016/j.joms.2008.06.107. [DOI] [PubMed] [Google Scholar]
- 12.Cicci M., Cervino G., Herford A.S. Facial bone reconstruction using both marine or non-marine bone substitutes: evaluation of current outcomes in a systematic literature review. Mar Drugs. 2018;16:E27. doi: 10.3390/md16010027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cicciu M. Real opportunity for the present and a forward step for the future of bone tissue engineering. J Craniofac Surg. 2017;28:592–593. doi: 10.1097/SCS.0000000000003595. [DOI] [PubMed] [Google Scholar]
- 14.Cicciù M., Herford A.S., Cicciù D. Recombinant human bone morphogenetic protein-2 promote and stabilize hard and soft tissue healing for large mandibular new bone reconstruction defects. J Craniofac Surg. 2014;25:860–862. doi: 10.1097/SCS.0000000000000830. [DOI] [PubMed] [Google Scholar]
- 15.Herford A.S., Miller M., Lauritano F. The use of virtual surgical planning and navigation in the treatment of orbital trauma. Chin J Traumatol. 2017;20:9–13. doi: 10.1016/j.cjtee.2016.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang M.L., Zhang B., Zhou Q. Minimally-invasive open reduction of intracapsular condylar fractures with preoperative simulation using computer-aided design. Br J Oral Maxillofac Surg. 2013;51:29–33. doi: 10.1016/j.bjoms.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 17.Boffano P., Corre P., Righi S. The role of intra-articular surgery in the management of mandibular condylar head fractures. Atlas Oral Maxillofac Surg Clin North Am. 2017;25:25–34. doi: 10.1016/j.cxom.2016.10.001. [DOI] [PubMed] [Google Scholar]
- 18.Voss J.O., Varjas V., Raguse J.D. Computed tomography-based virtual fracture reduction techniques in bimandibular fractures. J Cranio-Maxillofacial Surg. 2016;44:177–185. doi: 10.1016/j.jcms.2015.11.010. [DOI] [PubMed] [Google Scholar]
- 19.Iwai T., Yajima Y., Matsui Y. Computer-assisted preoperative simulation for screw fixation of fractures of the condylar head. Br J Oral Maxillofac Surg. 2013;51:176–177. doi: 10.1016/j.bjoms.2012.03.021. [DOI] [PubMed] [Google Scholar]
- 20.O'Connor R.C., Shakib K., Brennan P.A. Recent advances in the management of oral and maxillofacial trauma. Br J Oral Maxillofac Surg. 2015;53:913–921. doi: 10.1016/j.bjoms.2015.08.261. [DOI] [PubMed] [Google Scholar]
- 21.Dreizin D., Nam A.J., Hirsch J. New and emerging patient-centered CT imaging and image-guided treatment paradigms for maxillofacial trauma. Emerg Radiol. 2018;25:533–545. doi: 10.1007/s10140-018-1616-9. [DOI] [PubMed] [Google Scholar]
- 22.Zhao L., Patel P.K., Cohen M. Application of virtual surgical planning with computer assisted design and manufacturing technology to cranio-maxillofacial surgery. Arch Plast Surg. 2012;39:309–316. doi: 10.5999/aps.2012.39.4.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mohan A.P., Jeevan K.A., Venkatesh V. Comparison of preauricular approach versus retromandibular approach in management of condylar fractures. J Maxillofac Oral Surg. 2012;11:435–441. doi: 10.1007/s12663-012-0350-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ebenezer V., Ramalingam B. Comparison of approaches for the rigid fixation of sub-condylar fractures. J Maxillofac Oral Surg. 2011;10:38–44. doi: 10.1007/s12663-010-0145-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Al-Moraissi E.A., Louvrier A., Colletti G. Does the surgical approach for treating mandibular condylar fractures affect the rate of seventh cranial nerve injuries? A systematic review and meta-analysis based on a new classification for surgical approaches. J Cranio-Maxillofacial Surg. 2018;46:398–412. doi: 10.1016/j.jcms.2017.10.024. [DOI] [PubMed] [Google Scholar]
- 26.Klatt J., Heiland M., Blessmann M. Clinical indication for intraoperative 3D imaging during open reduction of fractures of the neck and head of the mandibular condyle. J Cranio-Maxillofacial Surg. 2011;39:244–248. doi: 10.1016/j.jcms.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 27.Han C., Dilxat D., Zhang X. Does intraoperative navigation improve the anatomical reduction of intracapsular condylar fractures? J Oral Maxillofac Surg. 2018;76:2583–2591. doi: 10.1016/j.joms.2018.07.030. [DOI] [PubMed] [Google Scholar]
- 28.Chen X., Chen X., Zhang G. Accurate fixation of plates and screws for the treatment of acetabular fractures using 3D-printed guiding templates: an experimental study. Injury. 2017;48:1147–1154. doi: 10.1016/j.injury.2017.03.009. [DOI] [PubMed] [Google Scholar]
- 29.Zeng W., Lian X., Chen G. Digital diagnosis and treatment program for maxillofacial fractures: a retrospective analysis of 626 cases. J Oral Maxillofac Surg. 2018;76:1470–1478. doi: 10.1016/j.joms.2017.11.040. [DOI] [PubMed] [Google Scholar]
- 30.Emodi O., Shilo D., Israel Y. Three-dimensional planning and printing of guides and templates for reconstruction of the mandibular ramus and condyle using autogenous costochondral grafts. Br J Oral Maxillofac Surg. 2017;55:102–104. doi: 10.1016/j.bjoms.2016.05.021. [DOI] [PubMed] [Google Scholar]
- 31.Bischoff E.L., Carmichael R., Reddy L.V. Plating options for fixation of condylar neck and base fractures. Atlas Oral Maxillofac Surg Clin North Am. 2017;25:69–73. doi: 10.1016/j.cxom.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 32.de Souza G.M., Rodrigues D.C., Celegatti Filho T.S. In-vitro comparison of mechanical resistance between two straight plates and a Y-plate for fixation of mandibular condyle fractures. J Cranio-Maxillofacial Surg. 2018;46:168–172. doi: 10.1016/j.jcms.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 33.Celegatti Filho T.S., Rodrigues D.C., Lauria A. Development plates for stable internal fixation: study of mechanical resistance in simulated fractures of the mandibular condyle. J Cranio-Maxillofacial Surg. 2015;43:158–161. doi: 10.1016/j.jcms.2014.10.029. [DOI] [PubMed] [Google Scholar]
- 34.Weiss J.P., Sawhney R. Update on mandibular condylar fracture management. Curr Opin Otolaryngol Head Neck Surg. 2016;24:273–278. doi: 10.1097/MOO.0000000000000272. [DOI] [PubMed] [Google Scholar]
- 35.Kozakiewicz M., Świniarski J. Treatment of high fracture of the neck of the mandibular condylar process by rigid fixation performed by lag screws: finite element analysis. Dent Med Probl. 2017;54:223–228. [Google Scholar]
- 36.Kanno T., Sukegawa S., Furuki Y. Overview of innovative advances in bioresorbable plate systems for oral and maxillofacial surgery. Jpn Dent Sci Rev. 2018;54:127–138. doi: 10.1016/j.jdsr.2018.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Laughlin R.M., Block M.S., Wilk R. Resorbable plates for the fixation of mandibular fractures: a prospective study. J Oral Maxillofac Surg. 2007;65:89–96. doi: 10.1016/j.joms.2005.10.055. [DOI] [PubMed] [Google Scholar]
- 38.Chaithanyaa N., Rai K.K., Arun kumar K.V. Setbacks of bio-resorbable plates and screws in the management of condylar fractures: our experience. J Maxillofac Oral Surg. 2011;10:220–224. doi: 10.1007/s12663-011-0237-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zheng J., Zhang S., Yang C. Assessment of magnetic resonance images of displacement of the disc of the temporomandibular joint in different types of condylar fracture. Br J Oral Maxillofac Surg. 2016;54:74–79. doi: 10.1016/j.bjoms.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 40.He D., Yang C., Zhang S., Wilson J.J. Modified temporomandibular joint disc repositioning with miniscrew anchor: Part I - surgical technique. J Oral Maxillofac Surg. 2015;73 doi: 10.1016/j.joms.2014.06.452. 47.e1-e9. [DOI] [PubMed] [Google Scholar]
- 41.Zhou Q., Zhu H., He D. Modified temporomandibular joint disc repositioning with miniscrew anchor: Part II—stability evaluation by magnetic resonance imaging. J Oral Maxillofac Surg. 2018;77:273–279. doi: 10.1016/j.joms.2018.07.016. [DOI] [PubMed] [Google Scholar]
- 42.Johns D.E., Wong M.E., Athanasiou K.A. Clinically relevant cell sources for TMJ disc engineering. J Dent Res. 2008;87:548–552. doi: 10.1177/154405910808700609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dimitroulis G. A critical review of interpositional grafts following temporomandibular joint discectomy with an overview of the dermis-fat graft. Int J Oral Maxillofac Surg. 2011;40:561–568. doi: 10.1016/j.ijom.2010.11.020. [DOI] [PubMed] [Google Scholar]
- 44.Guruprasad Y., Chauhan D.S., Cariappa K.M. A retrospective study of temporalis muscle and fascia flap in treatment of TMJ ankylosis. J Maxillofac Oral Surg. 2010;9:363–368. doi: 10.1007/s12663-010-0139-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Karamese M., Duymaz A., Seyhan N. Management of temporomandibular joint ankylosis with temporalis fascia flap and fat graft. J Cranio-Maxillofacial Surg. 2013;41:789–793. doi: 10.1016/j.jcms.2013.01.027. [DOI] [PubMed] [Google Scholar]
- 46.Kumar R.A., Kumar S., Rastogi S. Use of temporalis fascia as an interpositional arthroplasty in temporomandibular joint ankylosis - a case report. J Dent Specialities. 2013;2:116–119. [Google Scholar]
- 47.Gerbino G., Boffano P., Bosco G.F. Symphyseal mandibular fractures associated with bicondylar fractures: a retrospective analysis. J Oral Maxillofac Surg. 2009;67:1656–1660. doi: 10.1016/j.joms.2009.03.069. [DOI] [PubMed] [Google Scholar]
- 48.Xu X., Shi J., Xu B. Treatment of mandibular symphyseal fracture combined with dislocated intracapsular condylar fractures. J Craniofac Surg. 2015;26:e181–e185. doi: 10.1097/SCS.0000000000001451. [DOI] [PubMed] [Google Scholar]
- 49.Chen S., Zhang Y., An J.G. Width-controlling Fixation of symphyseal/parasymphyseal fractures associated with bilateral condylar fractures with 2 2.0-mm miniplates: a retrospective investigation of 45 cases. J Oral Maxillofac Surg. 2016;74:315–327. doi: 10.1016/j.joms.2015.09.030. [DOI] [PubMed] [Google Scholar]
- 50.Klotch D. Application of reconstruction plates to the mandible. Oper Tech Otolaryngol Head Neck Surg. 1995;6:89–96. [Google Scholar]
- 51.Scolozzi P., Martinez A., Jaques B. Treatment of linear mandibular fractures using a single 2.0-mm AO locking reconstruction plate: is a second plate necessary? J Oral Maxillofac Surg. 2009;67:2636–2638. doi: 10.1016/j.joms.2009.04.050. [DOI] [PubMed] [Google Scholar]
- 52.Morrow B.T., Samson T.D., Schubert W. Evidence-based medicine: mandible fractures. Plast Reconstr Surg. 2014;134:1381–1390. doi: 10.1097/PRS.0000000000000717. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.