Abstract
Background
ACE inhibitors are widely prescribed for hypertension so it is essential to determine and compare their effects on blood pressure (BP), heart rate and withdrawals due to adverse effects (WDAE).
Objectives
To quantify the dose‐related systolic and/or diastolic BP lowering efficacy of ACE inhibitors versus placebo in the treatment of primary hypertension.
Search methods
We searched CENTRAL (The Cochrane Library 2007, Issue 1), MEDLINE (1966 to February 2007), EMBASE (1988 to February 2007) and reference lists of articles.
Selection criteria
Double‐blind, randomized, controlled trials evaluating the BP lowering efficacy of fixed‐dose monotherapy with an ACE inhibitor compared with placebo for a duration of 3 to 12 weeks in patients with primary hypertension.
Data collection and analysis
Two authors independently assessed the risk of bias and extracted data. Study authors were contacted for additional information. WDAE information was collected from the trials.
Main results
Ninety two trials evaluated the dose‐related trough BP lowering efficacy of 14 different ACE inhibitors in 12 954 participants with a baseline BP of 157/101 mm Hg. The data do not suggest that any one ACE inhibitor is better or worse at lowering BP. A dose of 1/8 or 1/4 of the manufacturer's maximum recommended daily dose (Max) achieved a BP lowering effect that was 60 to 70% of the BP lowering effect of Max. A dose of 1/2 Max achieved a BP lowering effect that was 90% of Max. ACE inhibitor doses above Max did not significantly lower BP more than Max. Combining the effects of 1/2 Max and higher doses gives an estimate of the average trough BP lowering efficacy for ACE inhibitors as a class of drugs of ‐8 mm Hg for SBP and ‐5 mm Hg for DBP. ACE inhibitors reduced BP measured 1 to 12 hours after the dose by about 11/6 mm Hg.
Authors' conclusions
There are no clinically meaningful BP lowering differences between different ACE inhibitors. The BP lowering effect of ACE inhibitors is modest; the magnitude of trough BP lowering at one‐half the manufacturers' maximum recommended dose and above is ‐8/‐5 mm Hg. Furthermore, 60 to 70% of this trough BP lowering effect occurs with recommended starting doses. The review did not provide a good estimate of the incidence of harms associated with ACE inhibitors because of the short duration of the trials and the lack of reporting of adverse effects in many of the trials.
Keywords: Humans, Angiotensin-Converting Enzyme Inhibitors, Angiotensin-Converting Enzyme Inhibitors/adverse effects, Angiotensin-Converting Enzyme Inhibitors/therapeutic use, Antihypertensive Agents, Antihypertensive Agents/therapeutic use, Blood Pressure, Blood Pressure/drug effects, Heart Rate, Heart Rate/drug effects, Hypertension, Hypertension/drug therapy, Randomized Controlled Trials as Topic
Plain language summary
ACE inhibitors for the treatment of high blood pressure
The class of drugs called ACE inhibitors is commonly used for the treatment of elevated blood pressure. This class includes drugs such as ramipril (brand name: Altace), captopril (Capoten), enalapril (Vasotec), fosinopril (Monopril), lisinopril (Prinivil, Zestril) and quinapril (Accupril). We asked how much this class of drugs lowers blood pressure and whether there is a difference between individual drugs within the class. The available scientific literature was searched to find all the trials that had assessed this question.
We found 92 trials that randomly assigned participants to take either an ACE inhibitor or an inert substance (placebo). These trials evaluated the blood pressure lowering ability of 14 different ACE inhibitors in 12 954 participants. The trials followed participants for approximately 6 weeks (though people are typically expected to take anti‐hypertension drugs for the rest of their lives). The blood pressure lowering effect was modest. There was an 8‐point reduction in the upper number that signifies the systolic pressure and a 5‐point reduction in the lower number that signifies the diastolic pressure. Most of the blood pressure lowering effect (about 70%) can be achieved with the lowest recommended dose of the drugs. No ACE inhibitor drug appears to be any better or worse than others in terms of blood pressure lowering ability.
Most of the trials in this review were funded by companies that make ACE inhibitors and serious adverse effects were not reported by the authors of many of these trials. This could mean that the drug companies are withholding unfavorable findings related to their drugs. Due to incomplete reporting of the number of participants who dropped out of the trials due to adverse drug reactions, as well as the short duration of these trials, this review could not provide a good estimate of the harms associated with this class of drugs. Prescribing the least expensive ACE inhibitor in lower doses will lead to substantial cost savings, and possibly a reduction in dose‐related adverse events.
Background
ACE inhibitors are widely used as pharmacological agents for the treatment of hypertension. Hypertension is an important health problem and it is associated with an increased risk of death, stroke, and heart disease. Considerable scientific evidence shows that blood pressure reduction with different drug treatments reduces death, stroke, and heart disease. However, evidence also suggests the blood pressure lowering effect of antihypertensive agents may not always parallel with reductions in mortality or cardiovascular morbidity. In other words, blood pressure lowering does not always explain better health outcomes. Other factors may contribute to the reductions in mortality and vascular morbidity with antihypertensive drugs. Such factors may be independent of the blood pressure lowering effect of the drug, or the mechanism by which these drugs lower blood pressure. Nevertheless, blood pressure reduction remains an important factor. One of the main difficulties of managing a patient with hypertension using ACE inhibitors is deciding which dose of ACE inhibitor should be prescribed. This decision should be made primarily on the basis of the best available evidence of effectiveness. Despite over 20 years of research evidence and clinical use of ACE inhibitors, the dose‐related blood pressure lowering effect of this anti‐hypertensive drug class is still not known.
A systematic review of the dose‐related blood pressure lowering efficacy of ACE inhibitors has not been previously performed. The aims of this systematic review are: 1) to quantify the dose‐related blood pressure lowering efficacy of ACE inhibitors in patients with primary hypertension; and 2) to establish dose equivalencies of different drugs within the ACE inhibitor class. The information derived from this review should facilitate future reviews of head‐to‐head comparisons with other drug classes and assist clinicians in choosing optimal doses of ACE inhibitors.
Objectives
Primary objective
To quantify the dose‐related systolic and/or diastolic blood pressure lowering efficacy of angiotensin converting enzyme (ACE) inhibitors versus placebo in the treatment of primary hypertension.
Secondary objectives
To determine the effects of ACE inhibitors on variability of blood pressure.
To determine the effects of ACE inhibitors on pulse pressure.
To quantify the dose‐related effects of ACE inhibitors on heart rate.
To quantify the dose‐related effect of ACE inhibitors on withdrawals due to adverse effects.
Methods
Criteria for considering studies for this review
Types of studies
Included studies must be randomized controlled trials (RCTs) and their design must meet the following criteria:
double‐blind
random allocation to ACE inhibitor group(s) and parallel placebo group
duration of follow‐up of at least three weeks
office blood pressure measurements at baseline (following washout) and at one or more time points between 3 and 12 weeks post‐treatment
Types of participants
Participants must have an office baseline blood pressure of at least 140 mm Hg systolic and/or a diastolic blood pressure of at least 90 mm Hg. Patients must not have creatinine levels greater than 1.5 times the normal level, thereby excluding patients with secondary hypertension due to renal failure. Participants who were taking medications that affect blood pressure other than the study medications were excluded. Participants were not restricted by age, gender, baseline risk or any other co‐morbid conditions.
Types of interventions
Monotherapy with any ACE inhibitor, including alacepril, altiopril, benazepril, captopril, ceronapril, cilazapril, delapril, derapril, enalapril, fosinopril, idapril, imidapril, lisinopril, moexipril, moveltipril, pentopril, perindopril, quinapril, ramipril, spirapril, temocapril, trandolapril, and zofenopril.
Trials in which titration to a higher dose was based on blood pressure response were not eligible if the titration occurred before 3 weeks of treatment because dose‐response relationships cannot be analyzed if patients within each randomized group are taking different doses. However, trials in which a response‐dependent titration took place during or after the 3‐12 week interval were eligible if pre‐titration data were given. For forced titration trials, data from the lowest dose were extracted, provided this dose was given for a 3 to 12 week period.
Types of outcome measures
Primary outcomes
Change from baseline of trough and/or peak systolic and diastolic blood pressure at 3 to 12 weeks, compared with placebo. If blood pressure measurements were available at more than one time within the accepted window, the weighted means of blood pressures taken in the 3 to 12 week range were used.
Secondary outcomes
Standard deviation of the change in blood pressure compared with placebo.
Change in standard deviation of blood pressure compared with placebo.
Change in pulse pressure compared with placebo.
Change in heart rate compared with placebo.
Number of patient withdrawals due to adverse effects compared with placebo.
Search methods for identification of studies
To identify randomized, double‐blind, placebo‐controlled trials of ACE inhibitors, Cochrane Central Register of Controlled Trials (The Cochrane Library 2007, Issue 1), Medline (1966 to February 2007), EMBASE (1988 to February 2007), and bibliographic citations were searched. Previously published meta‐analyses on dose‐response of ACE inhibitors, as well as narrative reviews, were used to help identify references to trials. No language restrictions were applied.
A modified, expanded version of the standard search strategy of the Cochrane Hypertension Group, with additional terms related to ACE inhibitors, was used to identify relevant articles (Heran 2002).
MEDLINE
randomized controlled trial.pt
randomized controlled trial$.mp
controlled clinical trial.pt
controlled clinical trial$.mp
random allocation.mp
exp double‐blind method/
double‐blind.mp
exp single‐blind method/
single‐blind.mp
10. or/1‐9
ANIMALS.sh. not HUMAN.sh.
10 not 11
clinical trial.pt
clinical trial$.mp
exp clinical trials/
(clin$ adj25 trial$).mp
((singl$ or doubl$ or tripl$ or trebl$) adj25 (blind$ or mask$)).mp
random$.mp
exp research design/
research design.mp
or/13‐20
21 not 11
22 not 12
comparative stud$.mp
exp evaluation studies/
evaluation stud$.mp
follow‐up stud$.mp
prospective stud$.mp
(control$ or prospectiv$ or volunteer$).mp
or/24‐29
30 not 11
31 not (12 or 23)
12 and 23 and 32
exp angiotensin‐converting enzyme inhibitors/
angiotensin‐converting enzyme inhibitor$.mp
alacepril.mp
altiopril.mp
benazepril.mp
captopril.mp
ceronapril.mp
cilazapril.mp
delapril.mp
derapril.mp
exp enalapril/
enalapril.mp
fosinopril.mp
idapril.mp
imidapril.mp
lisinopril.mp
moexipril.mp
moveltipril.mp
pentopril.mp
perindopril.mp
quinapril.mp
ramipril.mp
spirapril.mp
temocapril.mp
trandolapril.mp
zofenopril.mp
or/34‐59
exp hypertension/
hypertension.mp
exp blood pressure/
blood presure.mp
or/61‐64
60 and 65
33 and 66
placebo$.mp
67 and 68
EMBASE
1. randomized controlled trial$.mp. 2. exp controlled clinical trials/ 3. controlled clinical trial$.mp. 4. exp random allocation/ 5. random allocation.mp. 6. double‐blind.mp. 7. single‐blind.mp. 8. or/1‐7 9. exp animal/ 10. 8 not 9 11. exp clinical trials/ 12. clinical trial$.mp. 13. (clin$ adj25 trial$).mp. 14. ((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).mp. 15. random$.mp. 16. exp research design/ 17. research design.mp. 18. or/11‐17 19. 18 not 9 20. 19 not 10 21. exp comparative study/ 22. comparative stud$.mp. 23. exp evaluation studies/ 24. evaluation stud$.mp. 25. exp follow up studies/ 26. follow up stud$.mp. 27. prospective stud$.mp. 28. (control$ or prospectiv$ or volunteer$).mp. 29. or/21‐28 30. 29 not 9 31. 30 not (10 or 20) 32. 10 and 20 and 31 33. exp angiotensin‐converting enzyme inhibitors/ 34. angiotensin‐converting enzyme inhibitor$.mp. 35. alacepril.mp. 36. altiopril.mp. 37. benazepril.mp. 38. captopril.mp. 39. exp ceronapril/ 40. ceronapril.mp. 41. cilazapril.mp. 42. delapril.mp. 43. derapril.mp. 44. enalapril.mp. 45. fosinopril.mp. 46. idapril.mp. 47. imidapril.mp. 48. lisinopril.mp. 49. moexipril.mp. 50. exp moveltipril/ 51. pentopril.mp. 52. perindopril.mp. 53. quinapril.mp. 54. ramipril.mp. 55. spirapril.mp. 56. temocapril.mp. 57. trandolapril.mp. 58. zofenopril.mp. 59. or/33‐58 60. exp hypertension/ 61. hypertension.mp. 62. exp blood pressure/ 63. blood pressure.mp. 64. or/60‐63 65. 59 and 64 66. 32 and 65 67. placebo$.mp. 68. 66 and 67
Data collection and analysis
Study Selection
The databases listed above were searched using the updated search strategy to identify citations with potential relevance. The initial screen of these abstracts excluded articles whose titles and/or abstracts were clearly irrelevant. The full text of remaining articles was then retrieved (and translated into English where required) to assess whether the trials met the prespecified inclusion criteria. The bibliographies of pertinent articles, reviews and texts were searched for additional citations. Two independent reviewers assessed the eligibility of the trials using a trial selection form. A third reviewer resolved discrepancies. Trials with more than one publication were counted only once.
Data Extraction
Data were extracted independently by two reviewers using a standard form and then cross‐checked. If data were presented numerically (in tables or text) and graphically (in figures), the numeric data were preferred because of possible measurement error when estimating from graphs. All numeric calculations and extractions from graphs or figures were confirmed by a second reviewer.
The position of the patient during blood pressure measurement may affect the blood pressure lowering effect. However, in order not to lose valuable data, if only one position was reported, data from that position were extracted. When blood pressure measurement data were available in more than one position, data were extracted in accordance with the following order of preference: 1) sitting; 2) standing; and 3) supine.
In the case of missing information in the included studies, investigators were contacted (by email, letter and/or fax) to obtain the missing information. In the case of missing values for standard deviation of the change in blood pressure or heart rate, the standard deviation was imputed based on the information in the same trial or from other trials using the same dose. The following hierarchy (listed from high to low preference) was used to impute standard deviation values:
Pooled standard deviation calculated either from the t‐statistic corresponding to an exact p‐value reported or from the 95% confidence interval of the mean difference between treatment group and placebo.
Standard deviation of change in blood pressure/heart rate from a different position than that of the blood pressure data/heart rate used.
Standard deviation of blood pressure/heart rate at the end of treatment.
Standard deviation of blood pressure/heart rate at the end of treatment measured from a different position than that of the blood pressure/heart rate data used.
Standard deviation of blood pressure/heart rate at baseline (except if this measure was used for entry criteria).
Weighted mean standard deviation of change in blood pressure/heart rate from other trials using the same class of drug (at any dose).
Quality Assessment
The quality of all included trials was assessed by two independent reviewers using the following two approaches:
1. The Cochrane approach to assessment of allocation concealment:
Grade A: Adequate
Centralized (central office unaware of subject characteristics) or pharmacy‐controlled randomization; pre‐numbered or coded identical containers that are administered serially to patients; on‐site computer system with allocations kept in a locked computer file that can be accessed only after patients enter; sequentially numbered, sealed, opaque envelopes.
Grade B: Unclear
Allocation concealment is not reported, or despite a description that reports adequate concealment (the use of a list, table or sealed envelopes), there are other features that lead the reviewer to be suspicious.
Grade C: Inadequate
Consists of the following methods: alternation; use of case record numbers, dates of birth or date at which the patient is invited to participate in the study; any procedure that is transparent before allocation, such as an open list of random numbers.
Grade D: Allocation concealment not used
Allocation concealment was not used to assess validity.
2. A 5‐point scoring system described by Jadad 1996 and summarised as follows:
Was the study described as randomised? (1=yes; 0=no)
Was the study described as double‐blind? (1=yes; 0=no)
Was there a description of withdrawals and dropouts? (1=yes; 0=no)
Was the method of randomisation well described and appropriate? (1=yes; 0=no)
Was the method of double blinding well described and appropriate? (1=yes; 0=no)
Deduct 1 point if methods for randomisation were inappropriate.
Deduct 1 point if methods for blinding were inappropriate.
A score of 0‐2 reflects low quality, a score of 3‐4 indicates moderate quality and a score of 5 represents a high quality study.
Data Analysis and Statistical Considerations
Data synthesis and analyses were done using the Cochrane Review Manager software, RevMan 4.2.8.
Data for changes from baseline in blood pressure and heart rate were combined using a weighted mean difference method. The withdrawals due to adverse effects was analyzed using relative risk, risk difference, and number needed to harm.
When possible, subgroup analyses were used to examine the results for specific categories of participants. Possible subgroup analyses included:
Race: Black, white, other.
Age: Adults (18‐69 years), older people (70 years and older).
Baseline severity of hypertension: Mild, moderate, severe.
The robustness of the results was tested using several sensitivity analyses, including:
Trials of high quality versus poor quality.
Trials that are industry‐sponsored versus non‐industry sponsored.
Trials that assess drug as primary drug of investigation versus trials that assess drug as comparator.
Trials with blood pressure data measured in the sitting position versus other measurement positions.
Trials with published standard deviations of blood pressure change versus imputed standard deviations.
Direct and indirect comparisons
When possible, direct and indirect comparisons of effect sizes between doses were performed for each ACE inhibitor drug. In the direct method, only trials that randomized participants to different doses were included in the analysis. In the indirect method, an "adjusted indirect comparison" and the associated standard error were calculated using the method described by Bucher 1997 and Song 2003.
A p value less than 0.05 (p < 0.05) was considered statistically significant for all comparisons. If there was statistically significant heterogeneity associated with an effect estimate, a random effects model was applied. This model provides a more conservative statistical comparison of the difference between ACE inhibitor treatment and placebo because a confidence interval around the effect estimate is wider than a confidence interval around a fixed effect estimate. If a statistically significant difference was still present using the random effects model, the fixed effect pooled estimate and confidence interval were reported because of the tendency of smaller trials, which are more susceptible to publication bias, to be overweighted with a random effects analysis.
Results
Description of studies
Search findings
The search strategy identified 4156 citations, of which only 92 (2.2%) trials met the inclusion criteria and had extractable data to evaluate the dose‐related blood pressure lowering efficacy of 14 ACE inhibitors (Figure 1).
1.
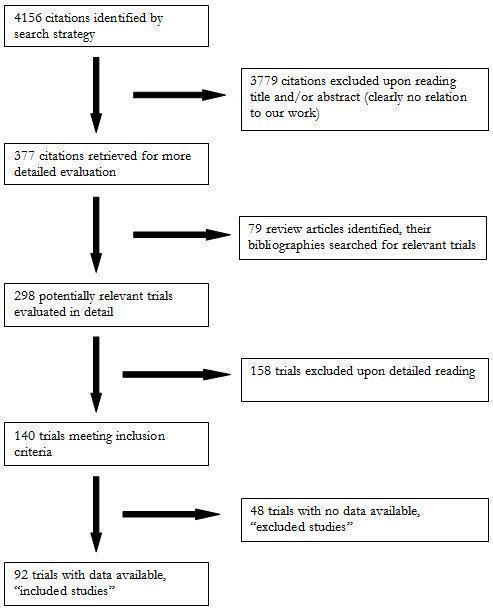
QUOROM flow diagram
Each included study is summarized in the "Characteristics of included studies". One hundred fifty eight studies were excluded because they did not meet the pre‐specified inclusion criteria. An additional 48 trials met the inclusion criteria but did not have extractable data and therefore were excluded. The reasons for exclusion are detailed in the "Characteristic of excluded studies". Of the 92 included studies, 87 (95%) were published in English, 3 (3%) in German, and 2 (2%) in Portuguese. Seventy (76%) of the included studies were industry‐sponsored while the remaining 22 (24%) did not report the source of funding. Twenty four duplicate publications of 17 included trials were also identified. Seventy six (82%) of the included studies randomized patients to fixed‐dose monotherapy during double‐blind treatment, 8 (9%) were forced‐titration studies and 8 (9%) were titration to BP response at pre‐specified intervals during the double‐blind treatment phase. Only the pre‐titration BP data were used in the analysis of these latter 16 studies.
Trials evaluating the antihypertensive efficacy of ACE inhibitor monotherapy using office blood pressure measurements were first published in 1983 (Figure 2). There was a steady increase in the number of published studies through the 1980s and early 90s, peaking at 11 trials published in 1994. After 1994 the number of trials published annually steadily declined.
2.
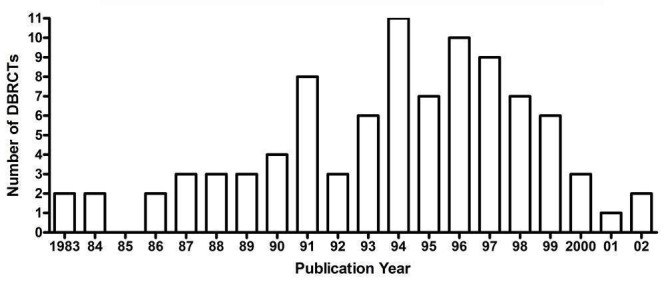
Number of included studies according to publication year
Figure 3 and Table 1 demonstrate that there is sufficient RCT evidence for the various ACE inhibitors to generate dose‐response curves for systolic and diastolic BP reduction as well as accomplish the secondary goals of this review. These studies investigate most ACE inhibitors over a dose range that is wider than what is recommended by the manufacturers. Enalapril is the most extensively studied ACE inhibitor with 19 published studies investigating the antihypertensive efficacy of daily doses ranging from 5 to 40 mg daily (Figure 3).
3.
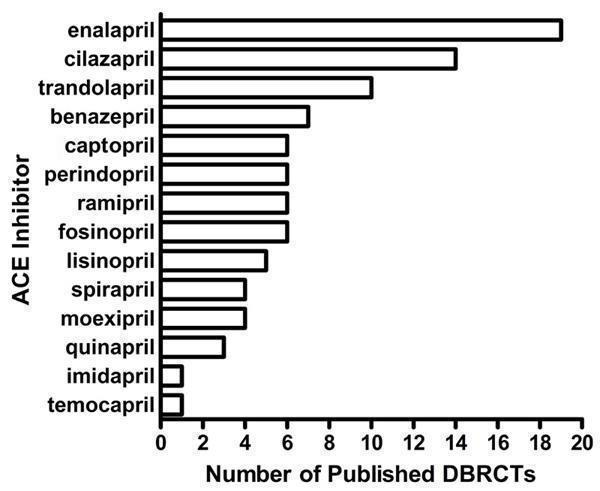
Number of included studies according to ACE inhibitor studied
1. Overview of the 92 included studies investigating ACE inhibitors as monotherapy.
| ACE inhibitor | Dose range (mg/day) | Number of studies | ACEI patients (n) | Placebo patients (n) | Mean duration (wks) | Mean age (yrs) | Baseline BP (mm Hg) | Baseline PP (mm Hg) |
| Benazepril | 2 ‐ 80 | 7 | 591 | 335 | 6.0 | 56.3 | 159.5/103.5 | 56.0 |
| Captopril | 37.5 ‐ 200 | 6 | 660 | 383 | 6.5 | 54.9 | 155.0/100.1 | 54.9 |
| Cilazapril | 0.5 ‐ 10 | 14 | 1054 | 448 | 4.9 | 53.3 | 153.5/101.0 | 52.5 |
| Enalapril | 5 ‐ 20 | 19 | 1477 | 1331 | 6.5 | 54.2 | 157.5/100.5 | 57.0 |
| Fosinopril | 2.5 ‐ 40 | 6 | 481 | 168 | 5.0 | 52.5 | 152.1/101.2 | 50.9 |
| Imidapril | 5 ‐ 40 | 1 | 127 | 35 | 4.0 | 51.9 | 160.7/101.5 | 59.2 |
| Lisinopril | 1.25 ‐ 80 | 5 | 484 | 357 | 5.7 | 55.2 | 154.5/101.8 | 52.7 |
| Moexipril | 7.5 ‐ 15 | 4 | 274 | 159 | 10.7 | 60.5 | 160.4/101.7 | 58.7 |
| Perindopril | 2 ‐ 16 | 6 | 658 | 396 | 7.1 | 55.9 | 159.4/99.9 | 59.5 |
| Quinapril | 20 | 3 | 99 | 97 | 4.0 | 52.6 | 161.7/105.6 | 56.1 |
| Ramipril | 1.25 ‐ 10 | 6 | 548 | 199 | 6.6 | 51.2 | 156.6/100.9 | 55.7 |
| Spirapril | 3 ‐24 | 4 | 586 | 189 | 5.6 | 52.3 | 164.3/103.5 | 60.8 |
| Temocapril | 20 | 1 | 19 | 11 | 6.0 | 57.0 | 158.0/97.6 | 60.4 |
| Trandolapril | 0.25 ‐ 16 | 10 | 1152 | 636 | 6.1 | 53.4 | 155.4/100.7 | 54.7 |
| TOTAL | 92 | 8210 | 4744 | 6.2 | 54.4 | 157.1/101.2 | 55.9 |
Characteristics of excluded studies
Forty eight studies that met the inclusion criteria were excluded from this review. Some of the reasons for exclusion were: failure to report adequate blood pressure data or the number of patients studied in each arm; crossover trials that did not report pre‐crossover data, as well as parallel group trials with a forced titration schedule and trials in which patients were titrated to a pre‐specified blood pressure response were also excluded if pre‐titration data was not reported. Reasons for excluding each trial are listed in the "Characteristics of excluded studies" table.
Overview of included studies
Baseline characteristics of the 92 included studies are provided in Table 1. A total of 12 954 participants with a mean age of 54.4 years and baseline BP of 157.1/101.2 mm Hg were treated for a mean duration of 6.2 weeks. In most cases, the number of patients treated with an ACE inhibitor was larger than the number of placebo‐treated patients because many of the included studies have multiple treatment arms comparing different doses of an ACE inhibitor with a single placebo arm.
Imputation of missing variance data
Standard deviation of blood pressure change
Forty (44%) of the included trials reported the standard deviation of the change in blood pressure. These values were pooled for the ACE inhibitor and placebo groups and weighted mean estimates of the standard deviation of the change in SBP and DBP were determined. Three trials (Chan 1997; Guitard 1994; Messerli 1998) were excluded from the calculation, and the weighted mean estimates were adjusted, because they reported standard deviation values that were so low they were more than 3 standard deviations away from the weighted mean SD of BP change. The weighted mean standard deviations of the change in SBP and DBP were 13.90 (SD 2.2) mm Hg and 8.1 (SD 1.4) mm Hg for the ACE inhibitor group, respectively. For the placebo group, the standard deviation of the change was 13.40 (SD 3.8) mm Hg for SBP and 7.7 (SD 2.2) mm Hg for DBP. There was no statistically significant difference between the ACE inhibitor and placebo groups for SD of SBP change, or SD of DBP change. These values were used according to the imputation hierarchy for trials that did not report SD of BP change or reported an outlier SD value.
The SD of BP change was imputed for 55 (60%) of the included studies. Of these studies, 29 (32%) were imputed using endpoint SD, 13 (14%) were imputed using baseline SD for SBP, 11 (12%) were imputed using the weighted mean SD of SBP change from other trials, and 7 (8%), were imputed using the weighted mean SD of DBP change from other trials.
Risk of bias in included studies
The Jadad and Cochrane scales were used in this review to assess the quality of the included studies. Eighty seven (94.6%) of the included trials did not report allocation concealment, while the remaining five (5.4%) trials reported an adequate method of concealment. The Jadad score for each included study is provided in the 'Notes' section of the "Characteristics of included studies" table. Using the Jadad quality score, 75 (81.5%) of the included studies were of good quality, 2 (2.2%) were of excellent quality, and 15 (16.3%) studies were of poor quality. Removing the studies that were considered poor according to the Jadad method did not alter the results of the meta‐analysis. Rather, the Jadad score was not very useful for assessing the quality of trials included in this review because its scoring criteria were similar to two of the criteria for inclusion of studies in our systematic review; the studies had to be randomized and double‐blind. Thus all included studies would score at least 2 on the Jadad scale. Furthermore, it was clear to us that the Jadad and Cochrane quality assessment scales were not evaluating the methodological quality of the trials but instead the quality of reporting in the published studies.
The most crucial factor in the included studies, which is not considered in the Jadad and Cochrane quality assessment scales, is the accuracy of blood pressure measurement (and the reporting of this outcome). The quality of the blood pressure results in the included trials appeared to be independent of the quality of reporting of the methodology.
Effects of interventions
Dose‐ranging BP lowering efficacy of individual ACE inhibitor drugs
Summarized below are the dose‐related trough blood pressure lowering efficacy estimates of 13 of the 14 ACE inhibitors that were administered once daily in the included studies. Captopril was administered twice or three times daily in nearly all the trials evaluating this drug. The weighted mean placebo effect across all trials was ‐3.2 (95% CI ‐3.6, ‐2.9; range ‐14.7 to 3.7) mm Hg and ‐3.7 (95% CI ‐3.9, ‐3.5; range ‐10.1 to 3.0) mm Hg for SBP and DBP, respectively. Therefore, to determine the magnitude of the BP lowering efficacy of each ACE inhibitor, a weighted mean difference from placebo (ACEI effect size minus placebo effect size) with a 95% confidence interval (in parentheses) was calculated.
Dose‐ranging BP lowering efficacy of benazepril
Seven of the included trials assessed benazepril at doses ranging from 2 mg/day to 80 mg/day. The log dose‐response curve for benazepril is presented in Figure 4. Benazepril doses of 2 to 10 mg/day did not significantly reduce BP compared with placebo. Benazepril at 20 mg/day was the lowest dose that demonstrated a significantly greater reduction in SBP and DBP as compared to placebo.
4.
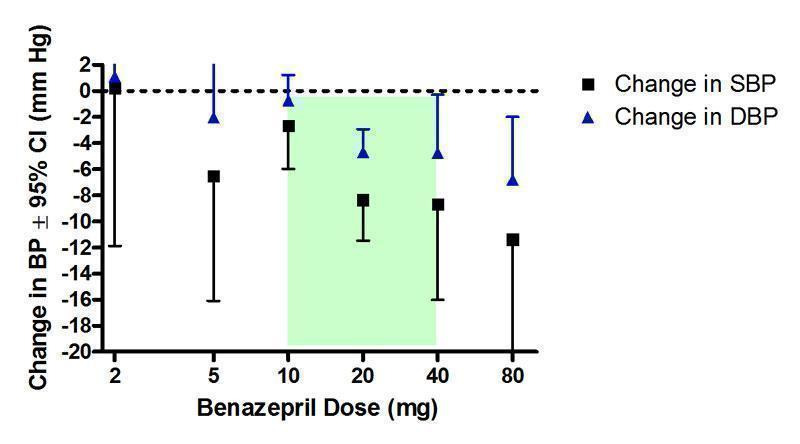
Log dose‐response curve of benazepril 2 ‐ 80 mg/day (Shaded area represents manufacturer's recommended dose range)
Only two trials (Moser 1991; Weinberger 1990) allowed a direct comparison analysis of the effect size for each dose and there was no statistically significant difference in the effect sizes between doses.
An indirect comparison demonstrated a statistically significant difference between the 10 and 20 mg/day groups, which is evidence of a dose‐response effect for benazepril. Due to a paucity of data at 40 and 80 mg/day, reflected in the wide confidence intervals, the 20 mg/day group did not show a statistically significant difference between the 40 and 80 mg/day groups.
Based on the available evidence, the best estimate of the near maximal BP lowering efficacy of benazepril occurs between 20 and 80 mg/day. The best estimate of the blood pressure lowering effect across this dosage range is ‐8.70 (95% CI: ‐11.43, ‐5.97) mm Hg for SBP and ‐ 4.92 (95% CI: ‐6.47, ‐3.36) mm Hg for DBP.
Dose‐ranging BP lowering efficacy of captopril
Captopril was the only ACE inhibitor that was usually prescribed as twice or three times daily dosing in the included trials. Three of the five trials assessed captopril at twice daily dosing (Drayer 1983; Dupui 1993; Muiesan 1987), one trial at three times daily dosing (VA Study Group 1984), and one trial assessed captopril 50 mg once daily (Kayanakis 1987). Sensitivity analyses were performed to assess the robustness of the results, which were unchanged whether the dosing was once, twice or three times daily.
All doses tested significantly lowered BP compared with placebo and there was no statistically significant difference between any of the doses using indirect comparisons (Figure 5). However, the paucity of data at doses other than 50 mg/day ‐ the manufacturer's recommended starting dose ‐ makes it difficult to adequately assess a dose‐response relationship. The lowest effective dose appears to be 37.5 mg/day, the lowest dosage studied. The lowest effective dose could be lower but there are no data available below 37.5 mg/day. Based on the available evidence, the best estimate of the near maximal blood pressure lowering effect of captopril is ‐9.68 (95% CI ‐11.73, ‐7.63) mm Hg and ‐5.43 (95% CI ‐6.47, ‐4.40) mm Hg for SBP and DBP, respectively.
5.
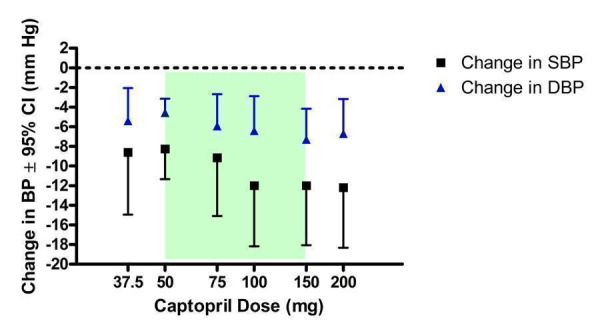
Log dose‐response curve of captopril 37.5 ‐ 200 mg/day (Shaded area represents manufacturer's recommended dose range)
Dose‐ranging BP lowering efficacy of cilazapril
Nine of the included trials assessed the SBP lowering efficacy of cilazapril at doses ranging from 2.5 to 10 mg/day, whereas 14 trials assessed the effect on DBP at a wider dosage range of 0.5 to 10 mg/day (Figure 6). There was no statistically significant difference compared with placebo for change in DBP at 0.5 and 1 mg/day. The three doses encompassing the manufacturer's recommended range did result in a statistically significant reduction in SBP and DBP and there was no statistically significant difference between all three doses. This suggests that the lowest effective dose of 2.5 mg/day ‐ which is the manufacturer's recommended starting dose ‐ is at the plateau of the dose‐response curve and thus also the lowest dose with near maximal BP lowering efficacy.
6.
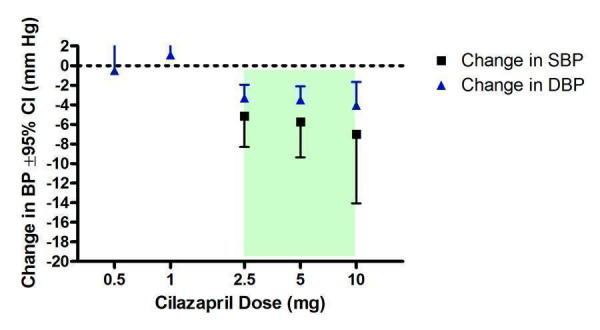
Log dose‐response curve of cilazapril 0.5 ‐ 10 mg/day (Shaded area represents manufacturer's recommended dose range)
The best estimate of the near maximal trough blood pressure lowering effect for doses of 2.5 to 10 mg/day is ‐5.58 (95% CI ‐7.84, ‐3.52) mm Hg and ‐3.50 (95% CI ‐4.40, ‐2.60) mm Hg for SBP and DBP, respectively.
Dose‐ranging BP lowering efficacy of enalapril
Nineteen of the included studies assessed the BP lowering efficacy of enalapril from 5 to 20 mg/day but there was no data available at 40 mg/day, the manufacturer's maximum recommended daily dosage (Figure 7). Compared with placebo, all doses demonstrated a statistically significant reduction in SBP and DBP. Based on the available evidence, the lowest effective dose is 5 mg/day. It is possible the lowest effective dose may be lower than 5 mg/day but there are no available data. Indirect comparisons showed a statistically significant difference in effect sizes between the 10 and 20 mg/day doses.
7.
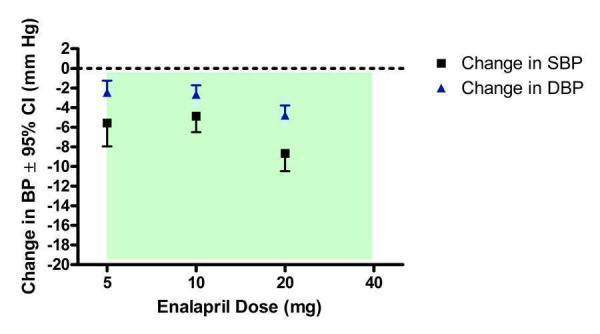
Log dose‐response curve of enalapril 5 ‐ 40 mg/day (Shaded area represents manufacturer's recommended dose range)
There was statistically significant heterogeneity in the effect estimate of DBP in the 10 mg/day group (Chi2 = 23.73, p = 0.001, I2 = 70.5%) as well as the SBP effect estimate at 20 mg/day (Chi2 = 17.34, p = 0.02, I2 = 59.6%). The random effects model still demonstrated a statistically significant difference from placebo for both groups. The heterogeneity in the two groups can be partly explained by two trials (Kuppers 1997; Prichard 2002) that report large reductions in BP with enalapril (‐14.10/‐7.60 mm Hg for 10 mg/day group in Kuppers 1997; ‐20.70/‐9.60 mm Hg for 20 mg/day group in Prichard 2002). Both studies were funded by the same company and used enalapril as an active comparator against their centrally acting antihypertensive drug, moxonidine. When these trials are removed from the analysis, the heterogeneity at 20 mg/day is no longer statistically significant and the SBP effect size is reduced from ‐9.61 (95% CI ‐11.35, ‐7.86) mm Hg to ‐8.66 (95% CI ‐10.48, ‐6.84) mm Hg. The heterogeneity in the 10 mg/day dose for DBP is reduced but is still statistically significant (Chi2 = 14.42, p = 0.03, I2 = 58.4%) and a random effects model still yielded a significant reduction in DBP for 10 mg/day compared with placebo. The remaining heterogeneity is explained by one large trial (Waeber 1999), which contributes 66% by weight to the estimate of the DBP lowering efficacy at 10 mg/day with enalapril. Waeber 1999 was designed to compare a fixed dose felodipine‐metoprolol combination with the active comparator enalapril as well as placebo; 318 patients were randomized to enalapril 10 mg/day and 300 patients to placebo. This trial reported a SBP reduction of ‐3.80 (95% CI ‐5.76, ‐1.84) and DBP reduction of ‐1.60 (95% CI ‐2.75, ‐0.45) compared with placebo.
From the data that are available, it appears that the lowest dose with near maximal BP lowering efficacy is 20 mg/day. Further increases in BP may be achieved at doses higher than 20 mg/day but there are no available data. The best estimate of the near maximal blood pressure lowering efficacy of enalapril at 20 mg/day is ‐8.66 (95% CI ‐10.48, ‐6.84) mm Hg for SBP and ‐4.80 (95% CI ‐5.81, ‐3.79) mm Hg for DBP.
Dose‐ranging BP lowering efficacy of fosinopril
Six of the included trials evaluated fosinopril from 2.5 to 40 mg/day but there were few studies at each dose and therefore insufficient data to demonstrate a statistically significant difference between any of the doses using indirect comparisons (Figure 8). The 2.5 and 5 mg/day groups did not have a statistically significant difference from placebo. The manufacturer's recommended starting dose of 10 mg/day significantly reduced DBP, but not SBP, as compared to placebo. The lowest effective dose appears to be between the 10 and 20 mg/day. Compared with placebo, the 20 and 40 mg/day groups had a statistically significant reduction in SBP and DBP.
8.
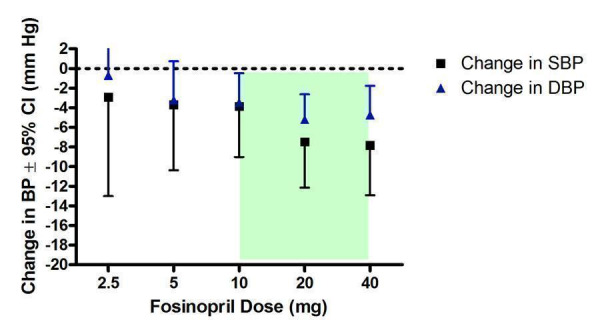
Lose dose‐response curve of fosinopril 2.5 ‐ 40 mg/day (Shaded area represents manufacturer's recommended dose range)
The best estimate of the lowest dose at which near maximal BP lowering efficacy occurs is 20 mg/day (‐9.26/‐7.79 mm Hg). However, there was statistically significant heterogeneity in this group. One trial (Zamboulis 1996) accounted for the heterogeneity in the 20 mg/day effect estimate because of its remarkably large reduction in BP (‐26.40/‐19.60 mm Hg). This small trial did not report the time of the BP measurement. The baseline BP differed between the treatment and placebo groups by 8 mm Hg for SBP and 13 mm Hg for DBP, which brings into question the quality of randomization in this trial. Furthermore, the baseline DBP in the benazepril group was 108 mm Hg whereas the weighted mean DBP in the other trials was 100 mm Hg. Thus, Zamboulis 1996 has been excluded from this analysis. Removal of this trial eliminated the heterogeneity and reduced the change in SBP to ‐7.46 (95% CI ‐12.15, ‐2.77) mm Hg and the change in DBP to ‐5.20 (95% CI ‐7.77, ‐2.63) mm Hg.
Based on the available data, the best estimate of the near maximal BP lowering occurs at doses of 20 mg/day and above and has a magnitude of ‐7.62 (95% CI ‐11.07, ‐4.17) mm Hg for SBP and ‐5.00 (95% CI ‐6.94, ‐3.05) mm Hg for DBP.
Dose‐ranging BP lowering efficacy of imidapril
Only one included multi‐arm trial assessed imidapril at doses of 5, 10, 20 and 40 mg/day (Vandenburg 1994). Compared with placebo, there was no statistically significant difference in change in DBP for any of the doses studied (Figure 9). Only the 20 mg/day group had a significantly greater reduction in SBP compared with placebo. When all doses were combined to establish an overall effect with imidapril, there was a statistically significant reduction in SBP and DBP compared with placebo.
9.
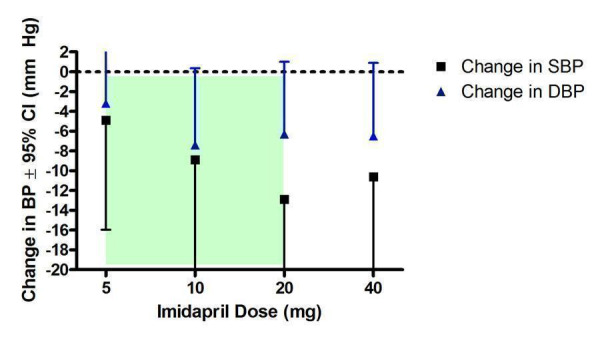
Log dose‐response curve of imidapril 5 ‐ 40 mg/day (Shaded area represents manufacturer's recommended dose range)
Due to a lack of data for each dose, a dose‐response relationship with imidapril could not be statistically established. A visual inspection of the log dose‐response curve (Figure 9) indicates that the BP lowering efficacy is approaching near maximal at 10 mg/day with a magnitude of ‐8.90 (95% CI ‐20.02, 2.22) mm Hg for SBP and ‐7.40 (95% CI ‐15.16, 0.36) mm Hg for DBP.
Based on the results of this one trial, the best estimate of the near maximal BP lowering efficacy for imidapril for 10 to 40 mg/day is ‐9.30 (95% CI ‐14.83, ‐3.78) mm Hg and ‐5.76 (95% CI ‐9.44, ‐2.07) mm Hg for SBP and DBP, respectively.
Dose‐ranging BP lowering efficacy of lisinopril
Although it appears in Figure 10 that lisinopril has been studied over a wide dosage range (1.25 ‐ 80 mg/day), 4 of the 5 included studies assessed lisinopril at 10 mg/day only, while only one small trial investigated lisinopril at all other doses (Gomez 1989). None of the included trials assessed the BP lowering efficacy at the manufacturer's recommended maintenance dosage of 40 mg/day.
10.
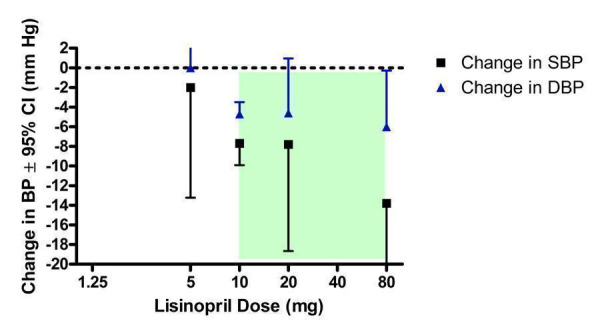
Lose dose‐response curve of lisinopril 1.25 ‐ 80 mg/day (Shaded area represents manufacturer's recommended dose range)
Only the 10 and 80 mg/day groups significantly decreased BP compared with placebo. There is insufficient data below 10 mg/day to determine whether or not there is a lower effective dose and 10 mg/day does appear to be the lowest dose with near maximal BP lowering.
Indirect comparisons showed that there was no statistically significant difference between the effect sizes of 20 and 80 mg/day doses compared with the 10 mg/day dose. Based on the available evidence, the near maximal blood pressure lowering efficacy of lisinopril for doses 10 to 80 mg/day is ‐8.00 (95% CI ‐10.14, ‐5.85) mm Hg for SBP and ‐4.76 (95% CI ‐5.92, ‐3.60) mm Hg for DBP.
Dose‐ranging BP lowering efficacy of moexipril
Four of the included trials assessed moexipril at 7.5 and 15 mg/day (Figure 11). Compared with placebo, only the 15 mg/day group had a statistically significant reduction in BP. An estimate of the near maximal BP lowering efficacy cannot be determined because there were no data for doses above 15 mg/day, including the manufacturer's maximum recommended dose of 30 mg/day.
11.
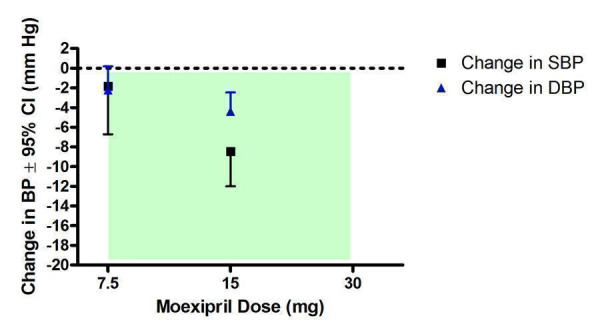
Log dose‐response curve of moexipril 7.5 ‐ 30 mg/day (Shaded area represents manufacturer's recommended dose range)
The lowest effective dose is 15 mg/day and, based on the available data, BP lowering at this dosage has a magnitude of ‐8.45 (95% CI ‐11.99, ‐4.91) mm Hg for SBP and ‐4.38 (95% CI ‐6.29, ‐2.46) mm Hg for DBP.
Dose‐ranging BP lowering efficacy of perindopril
Six of the included trials assessed perindopril at a dose range of 2 to 16 mg/day (Figure 12). All 6 trials studied perindopril at 4 mg/day, the manufacturer's recommended starting dose, but there was limited trial evidence at the other doses. Only 2 trials (Luccioni 1988; Myers 1996) provided data at 2 and 8 mg/day, and one trial assessed perindopril at 16 mg/day.
12.
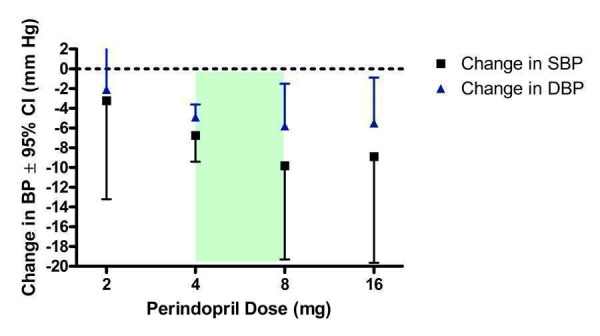
Log dose‐response curve of perindopril 2 ‐ 16 mg/day (Shaded area represents manufacturer's recommended dose range)
Perindopril 2 mg/day did not demonstrate a statistically significant reduction in BP compared with placebo. The lowest effective dose is 4 mg/day. Due to the wide confidence intervals for the 8 and 16 mg/day doses, indirect comparisons with 4 mg/day did not show a statistically significant difference. Because of the lack of data above and below 4 mg/day, there is very limited information regarding the dose‐response of perindopril.
Based on the available data, the best estimate of the near maximal blood pressure lowering efficacy for perindopril 4 to 16 mg/day is ‐7.09 (95% CI ‐9.56, ‐4.61) mm Hg for SBP and ‐5.02 (95% CI ‐6.22, ‐3.82) mm Hg for DBP.
Dose‐ranging BP lowering efficacy of quinapril
Two of the included trials assessed the BP lowering efficacy of quinapril at 20 mg/day (Figure 13). There were no data available for 10 and 40 mg/day, the manufacturer's recommended starting and maximum dose, respectively. At 20 mg/day, quinapril had a statistically significant reduction in BP compared with placebo. However, it cannot be established if the lowest effective dose is 20 mg/day. Furthermore, because there were no data for doses above 20 mg/day, the near maximal blood pressure lowering efficacy cannot be estimated. The magnitude of the BP lowering efficacy of quinapril at 20 mg/day is ‐7.05 (95% CI ‐11.26, ‐2.84) mm Hg for SBP and ‐3.35 (95% CI ‐5.98, ‐0.72) mm Hg for DBP.
13.
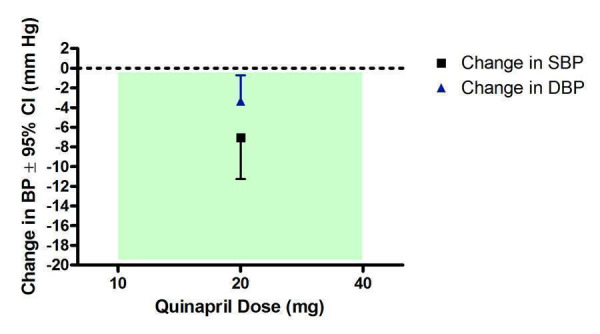
Log dose‐response curve of quinapril 10 ‐ 40 mg/day (Shaded area represents manufacturer's recommended dose range)
Dose‐ranging BP lowering efficacy of ramipril
Six of the included studies assessed ramipril at doses ranging from 1.25 to 10 mg/day (Figure 14). Compared with placebo, the manufacturer's recommended starting dose did not significantly reduce BP. A significant decrease in SBP and DBP was seen at 5 and 10 mg/day but there was no statistically significant difference between the two doses based on an indirect comparison. No included trials assessed the manufacturer's maximum recommended dose of 20 mg/day.
14.
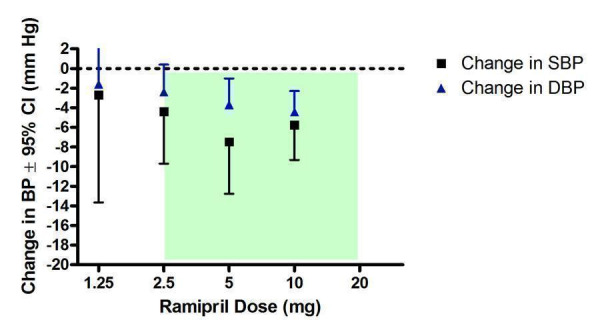
Log dose‐response curve of ramipril 1.25 ‐ 20 mg/day (Shaded area represents manufacturer's recommended dose range)
The lowest effective dose is 5 mg/day. Due to a lack of data, it cannot be determined if doses above 10 mg/day have greater efficacy. Thus, an estimate of the near maximal BP lowering efficacy of ramipril cannot be made. Based on the results of the two doses that were effective, the best estimate of the BP lowering effect of ramipril at 5 to 10 mg/day is ‐6.29 (95% CI ‐9.26, ‐3.32) mm Hg for SBP and ‐4.14 (95% CI ‐5.81, ‐2.48) mm Hg for DBP.
Dose‐ranging BP lowering efficacy of spirapril
The patent for spirapril expired in 2003 and it is no longer marketed in North America. The recommended starting dose and the maximum daily dose for the treatment of primary hypertension could not be found, explaining the lack of a shaded region in Figure 15.
15.
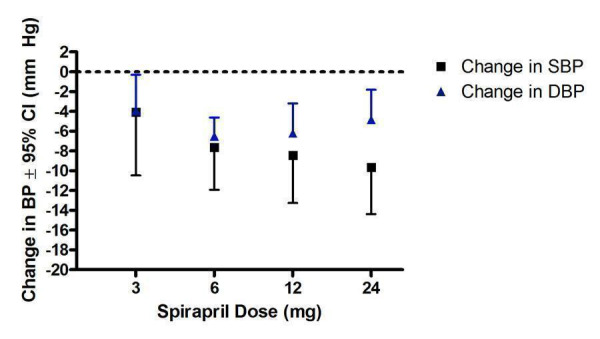
Log dose‐response curve of spirapril 3 ‐ 24 mg/day
All doses significantly reduced BP compared with placebo except for change in SBP at 3 mg/day. The lowest effective dose appears to be 3 and 6 mg/day. For SBP and DBP, there was no statistically significant difference in effect sizes between 6 and 24 mg/day using indirect comparisons. Thus, the estimate of the lowest dose at which near maximal BP lowering occurs is 6 mg/day. The best estimate of the near maximal BP lowering efficacy for spirapril is ‐8.54 (95% CI ‐11.18, ‐5.89) mm Hg and ‐6.08 (95% CI ‐7.50, ‐4.66) mm Hg for SBP and DBP, respectively.
Dose‐ranging BP lowering efficacy of temocapril
There were no included trials that assessed the BP lowering efficacy of temocapril within the manufacturer's recommended dose range of 1 to 4 mg/day (Figure 16). One included trial assessed temocapril at 20 mg/day (Lerch 1999). The 20 mg/day dose did not show a statistically significant difference compared with placebo but, as indicated by the extremely wide confidence intervals, this is likely due to the lack of data at this dose.
16.
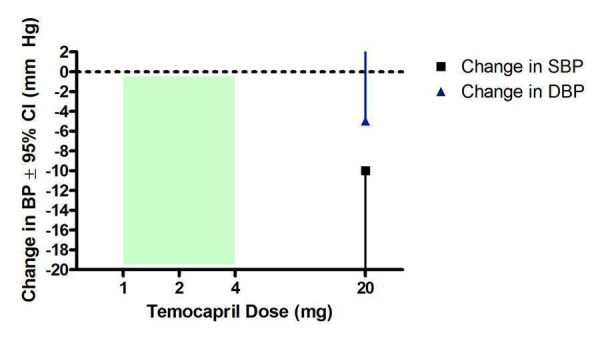
Log dose‐response curve of temocapril 1 ‐ 20 mg/day (Shaded area represents manufacturer's recommended dose range)
Dose‐ranging BP lowering efficacy of trandolapril
All doses of trandolapril above 0.5 mg/day resulted in a statistically significant reduction in BP compared with placebo (Figure 17). The manufacturer's recommended starting dose of 1 mg/day is the lowest effective dose that showed a statistically significant difference from 0.5 mg/day. Indirect comparisons showed that increasing the daily dose beyond 1 mg/day does not significantly reduce BP further.
17.
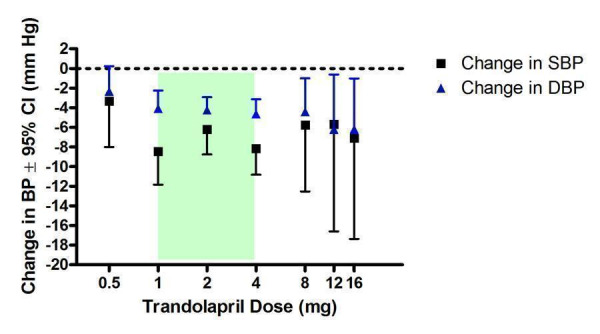
Log dose‐response curve of trandolapril 0.5 ‐ 16 mg/day (Shaded area represents manufacturer's recommended dose range)
Two trandolapril trials (DeQuattro 1997; Weir 1995) assessed the BP lowering efficacy of 8 mg/day in black patients, and only one trial (Weir 1995) assessed black patients after treatment with trandolapril at 0.5, 12 and 16 mg/day. However, very few black patients were studied at these doses to statistically assess whether there is a difference in efficacy between black and non‐black patients.
The lowest dose with near maximal BP lowering efficacy is 1 mg/day. Based on the available trial evidence, the best estimate of the near maximal BP lowering effect of trandolapril for doses of 1 to 16 mg/day is ‐7.31 (95% CI ‐8.85, ‐5.77) mm Hg for SBP and ‐4.42 (95% CI ‐5.24, ‐3.60) mm Hg for DBP.
Summary of the blood pressure lowering efficacy of ACE inhibitors
Table 2 provides an overview of the lowest effective dose, the lowest dose with near maximal blood pressure lowering and the near maximal blood pressure lowering effect of each ACE inhibitor studied in this review. The lowest effective dose is defined as the lowest dose for which there is a statistically significant difference from placebo. The lowest dose with near maximal blood pressure lowering efficacy is defined as the dose that demonstrates a statistically significantly greater response than doses below it, but does not exhibit a statistically significant difference in effect size compared with higher doses. If there was any discrepancy between SBP and DBP, SBP was used to define the doses.
2. Summary of the blood pressure lowering efficacy of ACE inhibitors.
| ACE Inhibitor | Lowest effective dose (mg/day) | Lowest dose with near maximal BP lowering (mg/day) | Near maximal trough SBP lowering (mm Hg), 95% CI | Near maximal trough DBP lowering (mm Hg), 95% CI |
| benazepril | 20 | 20 | ‐8.70 (‐11.43, ‐5.97) | ‐4.92 (‐6.47, ‐3.36) |
| captopril | 37.5 | 37.5 | ‐9.68 (‐11.73, ‐7.63) | ‐5.43 (‐6.47, ‐4.40) |
| cilazapril | 2.5 | 2.5 | ‐5.58 (‐7.84, ‐3.32) | ‐3.50 (‐4.40, ‐2.60) |
| enalapril | 5 | 20 | ‐8.66 (‐10.48, ‐6.84) | ‐4.80 (‐5.81, ‐3.79) |
| fosinopril | 10‐20 | 20 | ‐7.62 (‐11.07, ‐4.17) | ‐5.00 (‐6.94, ‐3.05) |
| imidapril | Not estimable | Not estimable | ‐9.30 (‐14.83, ‐3.78) | ‐5.76 (‐9.44, ‐2.07) |
| lisinopril | 10 | 10 | ‐8.00 (‐10.14, ‐5.85) | ‐4.76 (‐5.92, ‐3.60) |
| moexipril | 15 | Not estimable | ‐8.45 (‐11.99, ‐4.91) | ‐4.38 (‐6.29, ‐2.46) |
| perindopril | 4 | 4 | ‐7.09 (‐9.56, ‐4.61) | ‐5.02 (‐6.22, ‐3.82) |
| quinapril | Not estimable | Not estimable | ‐7.05 (‐11.26, ‐2.84) | ‐3.35 (‐5.98, ‐0.72) |
| ramipril | 5 | 5 | ‐6.29 (‐9.26, ‐3.32) | ‐4.14 (‐5.81, ‐2.48) |
| spirapril | 3‐6 | 6 | ‐8.54 (‐11.18, ‐5.89) | ‐6.08( ‐7.50, ‐4.66) |
| temocapril | Not estimable | Not estimable | ‐10.00 (‐23.87, 3.87) | ‐5.00 (‐13.34, 3.34) |
| trandolapril | 1 | 1 | ‐7.31 (‐8.85, ‐5.77) | ‐4.42 (‐5.24, ‐3.60) |
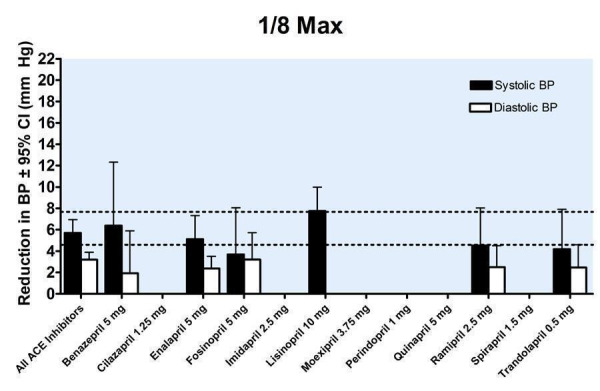
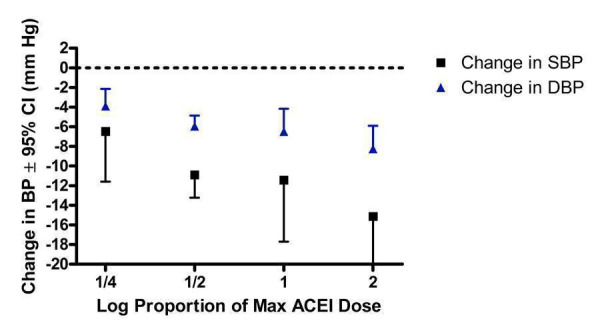
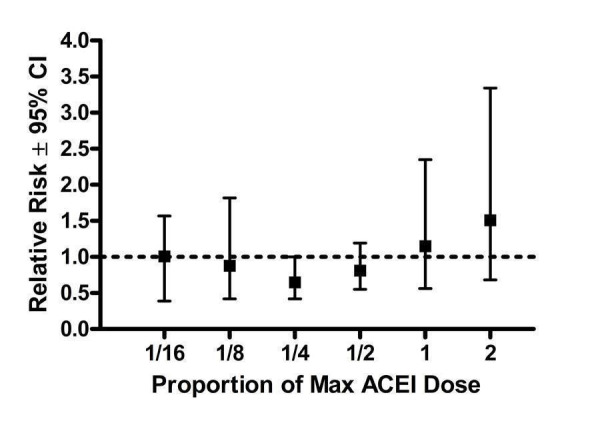
ACE inhibitors were analyzed as a class by pooling all trials reporting trough blood pressure and categorizing individual doses as proportions of the manufacturers' maximum recommended daily dose (Max). The pooled efficacy data ranged from 1/16 Max to 2 Max (Figure 18, 1/8 Max to Max; Figure 19, 1/16 Max; Figure 20, 1/8 Max; Figure 21, 1/4 Max; Figure 22, 1/2 Max; Figure 23, Max; Figure 24, 2 Max).
18.
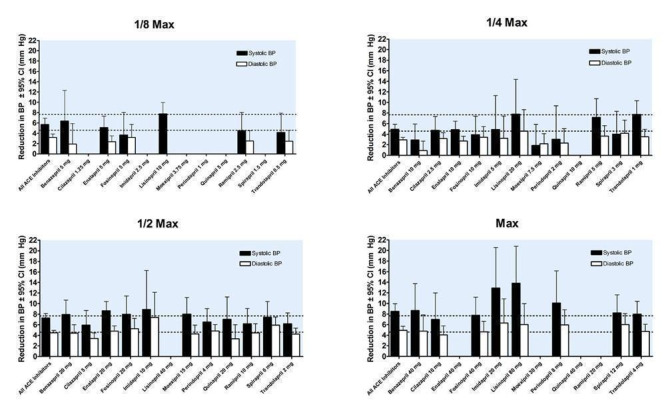
Blood pressure lowering efficacy of ACE inhibitors according to proportions of Max
19.
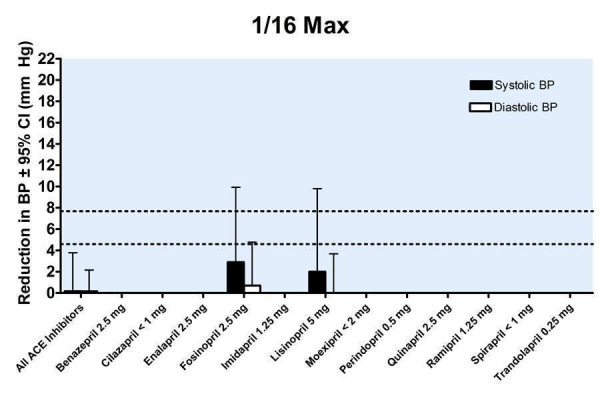
Blood pressure lowering efficacy of ACE inhibitors according to proportions of Max
20.
Blood pressure lowering efficacy of ACE inhibitors according to proportions of Max
21.
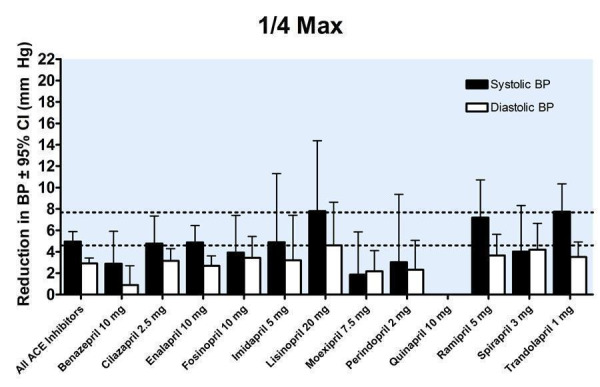
Blood pressure lowering efficacy of ACE inhibitors according to proportions of Max
22.
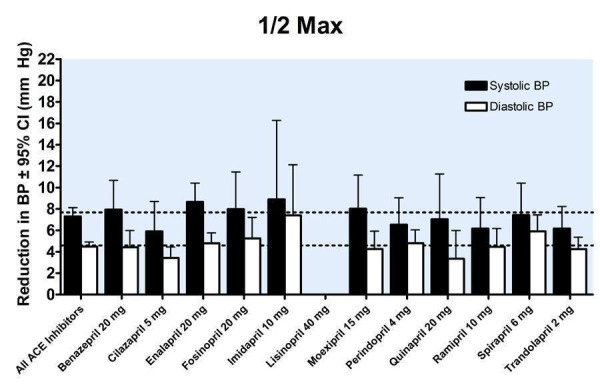
Blood pressure lowering efficacy of ACE inhibitors according to proportions of Max
23.
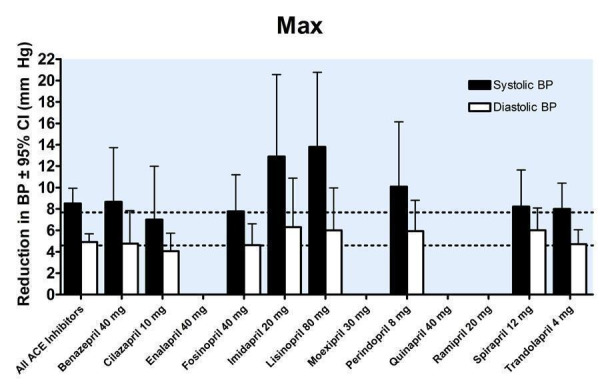
Blood pressure lowering efficacy of ACE inhibitors according to proportions of Max
24.
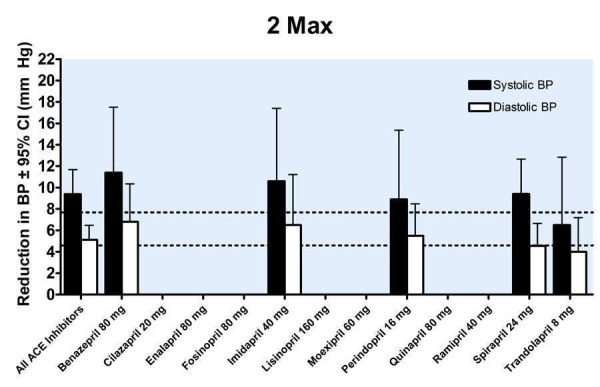
Blood pressure lowering efficacy of ACE inhibitors according to proportions of Max
The pooled efficacy data were evaluated for the presence of a dose‐response relationship. As shown in Figure 25, a dose‐response is present with a statistically significant difference between 1/4 Max and 1/2 Max. Further increases in the dosage beyond 1/2 Max did not result in a statistically significantly greater reduction in blood pressure.
25.
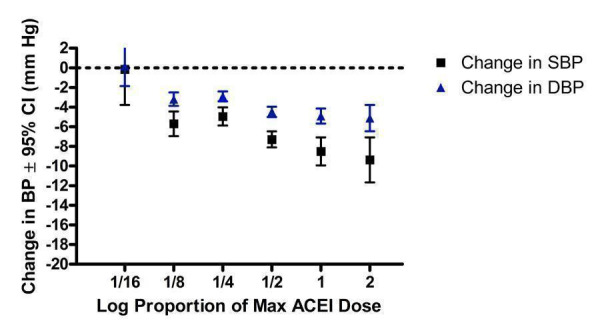
Log dose‐response curve of ACE inhibitors according to proportions of Max
Thus, near maximal blood pressure lowering is achieved at half of the manufacturers' recommended maximum dose and above (Figure 26). Using this definition the best estimate of the near maximal blood pressure lowering for the ACE inhibitor class of drugs is ‐7.68 (95% CI ‐8.45, ‐6.91) mm Hg for SBP and ‐4.59 (95% CI ‐4.99, ‐4.19) mm Hg for DBP.
26.
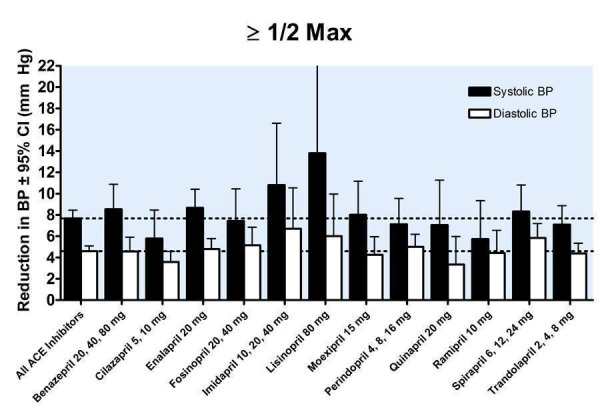
Near maximal blood pressure lowering efficacy of ACE inhibitors
Analysis of publication bias
Funnel plots
In order to test for the possibility of publication bias in the ACE inhibitor review funnel plots were created of the trough SBP (Figure 27) and DBP (Figure 28) lowering effects of all doses of 1/2 Max and higher. These plots were reasonably symmetrical and there did not appear to be a paucity of smaller trials with small or absent BP lowering effect.
27.
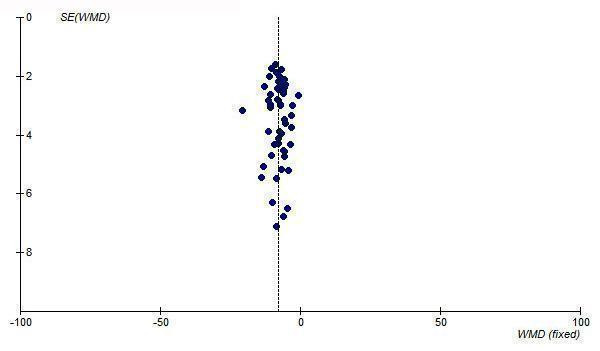
Funnel plot of near maximal change in trough SBP for ACE inhibitors at 1/2 Max and higher doses
28.
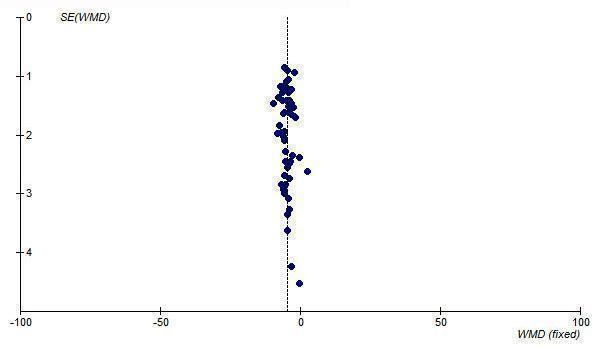
Funnel plot of near maximal change in trough DBP for ACE inhibitors at 1/2 Max and higher doses
Tertile analysis based on trial size
To further test for possible publication bias, a post‐hoc tertile analysis was performed to determine if the magnitude of BP lowering differed according to trial size. Once again all ACE inhibitor doses of 1/2 Max and above were divided into tertiles according to the sample size in the active treatment arms. The lowest, middle and highest tertiles represented the smallest, medium‐sized and largest trials, respectively. The mean effect size of the largest trials (highest tertile) was compared with that of the smallest trials (lowest tertile) using an unpaired t test (the indirect method).
As shown in Figure 29, this tertile analysis did not suggest the presence of publication bias in the ACE inhibitor systematic review; there were no statistically significant differences in effect size between the largest (n=82‐253 patients) and smallest (n=10‐41 patients) trials for both SBP (p=0.9) and DBP (p=1.0).
29.
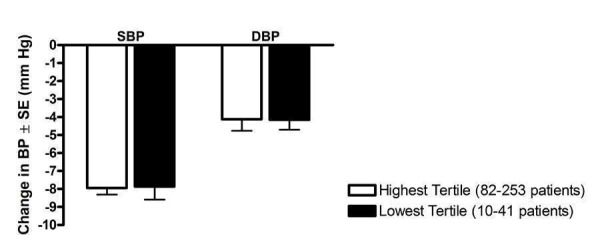
Post‐hoc tertile analysis of the effect of trial size on reported trough BP lowering
Tertile analysis based on publication year
Another possible source of bias in the ACE inhibitor review is bias introduced because the patients chosen for the trial were already known to respond well to ACE inhibitors. If this were occurring, it was hypothesized that there would be little possibility for this to happen in the earliest published trials and that it would be more likely to occur in later published trials when use of the class was more common. A post‐hoc tertile analysis was done to determine the effect of the year of publication of trials on the BP lowering effect. This analysis was done for all ACE inhibitor doses at 1/2 Max and above (Figure 30). The mean effect size of the latest tertile (1997‐2002) was compared with that of the earliest tertile (1987‐1993) using the indirect method and there was no statistically significant difference for SBP (p=0.5) or DBP (p=0.8) between the tertiles.
30.
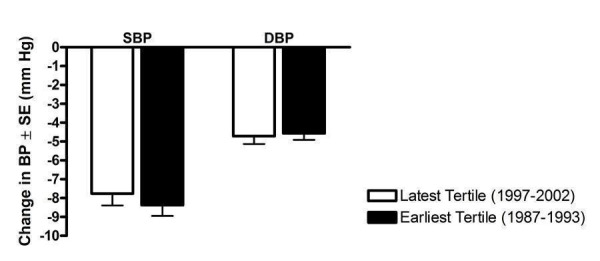
Post‐hoc tertile analysis of the effect of publication year on reported trough BP lowering
Blood pressure variability
The variability of blood pressure at both baseline and endpoint was reported for 26 (28%) of the included trials. In Table 3, the number of observations represents the number of active treatment arms in these 26 trials. Ninety (98%) of the studies had diastolic hypertension entry criteria, 2 (2.2%) trials had systo‐diastolic hypertension entry criteria (Dupui 1993; Kayanakis 1987), and no trials had isolated systolic hypertension entry criteria.
3. Variability of SBP and DBP at end of treatment.
| ACE Inhibitor | Placebo | ||
| SBP | Weighted mean SD | 16.6 | 16.8 |
| SD of weighted mean SD | 3.1 | 3.0 | |
| Weighted mean SBP | 146.0 | 152.9 | |
| Weighted mean coefficient of variation (CV) | 11.2 | 11.0 | |
| SD of weighted mean CV | 2.1 | 2.0 | |
| Number of observations | 22 | 19 | |
| DBP | Weighted mean SD | 9.0 | 8.9 |
| SD of weighted mean SD | 1.7 | 1.8 | |
| Weighted mean DBP | 91.8 | 96.4 | |
| Weighted mean coefficient of variation (CV) | 9.8 | 9.2 | |
| SD of weighted mean CV | 1.8 | 1.9 | |
| Number of observations | 20 | 18 | |
| t‐test | SD of SBP vs SD of DBP | p < 0.0001 | p < 0.0001 |
| t‐test | CV SBP vs CV DBP | p = 0.0227 | p = 0.0045 |
Systolic versus diastolic blood pressure variability
The weighted mean standard deviations for SBP and DBP were compared in order to determine whether SBP varies to the same degree as DBP. For both the ACE inhibitor group and placebo group, the absolute variability of SBP is statistically significantly greater than that of DBP (Table 3). The coefficient of variation in SBP was also significantly greater than the coefficient of variation in DBP for both the ACE inhibitor and placebo groups.
ACE inhibitors versus placebo
Table 3 shows the weighted mean endpoint SD of SBP was 16.6 mm Hg for the ACE inhibitor group and 16.8 mm Hg for the placebo group (p = 0.8). The weighted mean SD of DBP was 9.0 mm Hg for the ACE inhibitor group and 8.9 mm Hg for the placebo group (p = 0.8). Based on the available evidence, there was no statistically significant difference in the endpoint blood pressure variability between the ACE inhibitor and placebo groups.
The effect of blood pressure entry criteria on variability
The included trials were categorized according to blood pressure entry criteria used: 1) diastolic hypertension; 2) systolic hypertension; and 3) systo‐diastolic hypertension. None of the included studies had isolated systolic hypertension entry criteria. Only 2 trials had systo‐diastolic hypertension entry criteria (Dupui 1993; Kayanakis 1987) and therefore a comparison with this subgroup was not feasible. To determine the effect of diastolic blood pressure entry criteria on baseline BP variability, the weighted mean baseline standard deviations of these trials were compared.
Baseline versus endpoint variability
As shown in Table 4, the standard deviations of blood pressure at baseline and endpoint were compared for trials with DBP entry criteria. For the ACE inhibitor group and placebo group, there was no statistically significant difference between the variability of SBP at baseline and endpoint. DBP variability at endpoint was significantly higher than at baseline in both the ACE inhibitor and placebo groups.
4. SD of BP at baseline vs endpoint in trials with DBP entry criteria.
| ACE Inhibitor | Placebo | ||
| Weighted mean SD of SBP | At baseline (SD) | 14.8 (3.0) | 14.9 (2.8) |
| At endpoint (SD) | 16.6 (3.1) | 16.8 (3.0) | |
| t‐test | baseline vs endpoint | p = 0.06 | p = 0.05 |
| Weighted mean SD of DBP | At baseline (SD) | 5.1 (1.5) | 5.1 (1.6) |
| At endpoint (SD) | 9.0 (1.7) | 8.9 (1.8) | |
| t‐test | baseline vs endpoint | p < 0.0001 | p < 0.0001 |
Dose‐ranging peak blood pressure lowering efficacy
Nine of the included trials reported the peak blood pressure lowering efficacy of ACE inhibitors. Peak blood pressure data were pooled across trials by categorizing individual doses as proportions of Max, ranging from 1/4 to 2 Max (Figure 31). All doses exhibited a statistically significant reduction in peak SBP and DBP compared with placebo. Indirect comparison analysis of the results for each proportion of Max showed evidence of a dose‐response since there was a greater reduction in blood pressure with 2 Max compared with 1/4 Max. There was no statistically significant difference in the effect sizes between 1/2 Max and 2 Max. Pooling the effects of all doses from 1/2 Max to 2 Max provides an estimate of the peak blood pressure lowering effect of ACE inhibitors, ‐11.43 (95% CI ‐13.40, ‐9.45) mm Hg for SBP and ‐6.35 (95% CI ‐7.19, ‐5.50) mm Hg for DBP.
31.
Log dose‐response curve of peak blood pressure lowering efficacy of ACE inhibitors according to proportions of Max
Dose‐ranging effect on pulse pressure
Pulse pressure was not reported as an outcome in any of the included trials so the change in pulse pressure was calculated by subtracting the change in DBP from the change in SBP for each trial that reported both SBP and DBP. Seventy four (80%) of the included studies provided data to calculate the change in trough pulse pressure. A weighted mean and weighted standard deviation of the change in pulse pressure from baseline was then computed for each proportion of the recommended maximum dose (Table 5).
5. Change in pulse pressure according to proportions of Max.
| Proportion of recommended maximum dose (Max) | Number of studies | Weighted mean change from baseline in pulse pressure (95% CI) | |
| ACE inhibitors | 1/8 Max | 18 | ‐1.2 (‐2.0, ‐0.4) |
| 1/4 Max | 40 | ‐1.8 (‐2.6, ‐0.9) | |
| 1/2 Max | 50 | ‐2.5 (‐3.2, ‐1.9) | |
| Max | 16 | ‐3.7 (‐5.5, ‐1.9) | |
| 2 Max | 6 | ‐4.1 (‐6.3, ‐1.9) | |
| 1/2 Max and above | 54 | ‐2.9 (‐3.5, ‐2.3) | |
| Placebo | 74 | 0.6 (0.1, 1.1) |
Based on the available evidence, there was a marginal increase from baseline in pulse pressure in patients randomized to placebo. All doses of ACE inhibitors demonstrated statistically significant reductions from baseline in pulse pressure compared with placebo. At 1/2 Max and above, where near maximal BP lowering is achieved, the estimate of the average reduction in pulse pressure was 2.9 and when this was compared to placebo it became 3.5 (95% CI 2.7, 4.3) mm Hg.
Dose‐ranging effect on heart rate
Of the 92 included studies, 16 (17%) reported dose‐related trough heart rate data. There were few trials to adequately assess the heart rate effect of individual ACE inhibitors. Thus the data were pooled across all trials that reported this outcome and categorized as proportions of the manufacturers' maximum recommended daily dose. Based on the available evidence, there was no statistically significant change in heart rate compared with placebo over the range of 1/8 Max to Max (Figure 32).
32.
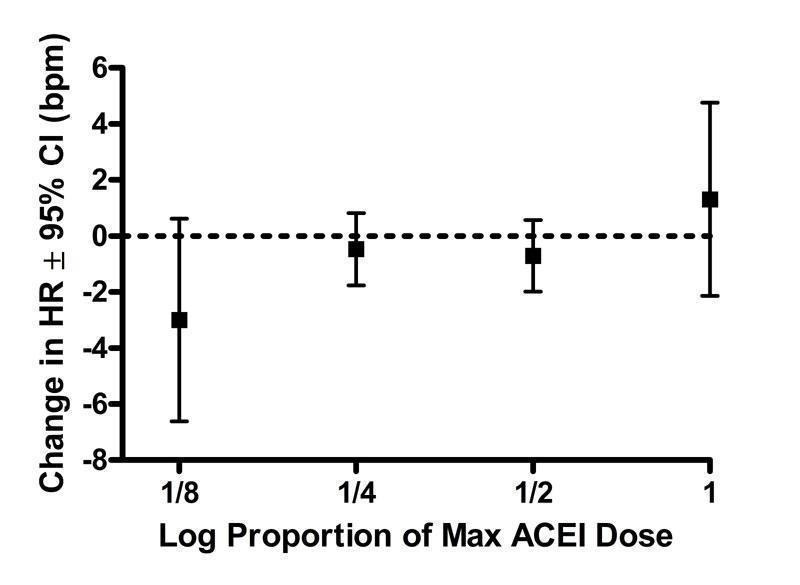
Log dose‐response curve assessing the effect of ACE inhibitors on heart rate
Dose‐ranging effect on withdrawals due to adverse effects
Fifty five of the included studies (60%) reported dose‐related withdrawals due to adverse effects (WDAE) during the 3 to 12 week treatment period. There were not enough data to construct a meaningful dose‐response relationship for individual ACE inhibitors. The data are therefore categorized according to the proportions of Max over a dose range of 1/8 Max to Max (Figure 33).
33.
Log dose‐response curve assessing the effect of ACE inhibitors on withdrawals due to adverse effects
At 1/4 Max, there was a marginally non‐significant [RR 0.65 (95% CI 0.42, 1.00)] reduction in WDAE and there was a trend towards an increased WDAE with higher doses, but none of the doses demonstrated a statistically significant difference compared with placebo. A pooled estimate for all doses resulted in a statistically non‐significant relative risk of 0.85 (95% CI 0.67, 1.07). The doses at which near maximal BP lowering efficacy is achieved (1/2 Max and above) also showed no statistically significant difference in WDAE [0.96 (95% CI 0.70, 1.31)] compared with placebo.
Discussion
Ninety two trials with a mean duration of 6 weeks met the pre‐specified inclusion criteria and reported data on 12 954 participants (8210 treated with ACE inhibitors and 4744 treated placebo) with a mean age of 54 years, mean baseline blood pressure of 157/101 mm Hg and a mean pulse pressure of 56 mm Hg.
Is there a difference in the magnitude of BP lowering effect between individual drugs in the ACE inhibitor class?
This review provides a reasonable amount of data to assess the trough BP lowering effect of 14 different ACE inhibitors. When the different ACE inhibitors are compared, there is a remarkable similarity in their BP lowering effects at trough. When the best estimate of the BP lowering efficacy of these 14 drugs is compared, they range from ‐6/‐4 mm Hg to ‐9/‐5 mm Hg. The data are most consistent with the near maximum BP lowering effect of the each of the drugs being the same. However, for most of the drugs there are insufficient data over a broad dose range. It is therefore impossible with this analysis to be certain that there are no blood pressure lowering differences between one or more of the drugs. It would require head‐to‐head trials of different ACE inhibitors at equivalent BP lowering doses to assess whether or not there are differences between different drugs. This review will provide useful information for estimating equivalent doses and thereby designing trials to compare different ACE inhibitors. However, at the present time given that all the drugs are working by the same mechanism and the similarities in the blood pressure lowering effect it is most likely that the near maximal BP lowering of the different ACE inhibitors is the same.
What is the dose‐related blood pressure lowering effect of ACE inhibitors as a class?
Based on the assumption of no difference between the different ACE inhibitors and the fact that the trough BP lowering effects of the different ACE inhibitors were so similar, the data for 13 of the 14 drugs that had the manufacturers' dosage information available were pooled. Data were pooled for 13 ACE inhibitors by categorizing individual doses as proportions of the manufacturers' maximum recommended daily dose (Max). It is recognized that this approach has its limitations but it provided a non‐arbitrary method for pooling the drugs. Using this method, as a class ACE inhibitors demonstrated a dose‐response relationship. A dose of 1/16 Max had no measurable BP lowering effect. A dose of 1/8 or 1/4 Max achieved a BP lowering effect that was 60 to 70% of the BP lowering effect of the maximum recommended dose. A dose of 1/2 Max achieved a BP lowering effect that was 90% of the maximum recommended dose.
Combining the effects of half maximum recommended doses and above gives a reasonable estimate of the near maximal trough blood pressure lowering efficacy for the ACE inhibitors as a class, ‐8 mm Hg for SBP and ‐5 mm Hg for DBP. This was accompanied by an average reduction in pulse pressure of 3 mm Hg. This is quite a modest effect and is likely considerably less than most clinicians would estimate can be achieved with these drugs. However, this effect is at trough and is obtained after subtracting the placebo effect which on average reduced BP by 3/4 mm Hg. Furthermore, most doctors probably do not measure BP in their patients at trough. In this review, there were much less data for BP measured 1 to 12 hours after the doses. From these data, we were able to estimate the average effect of ACE inhibitors 1 to 12 hours after the dose and it was modestly higher, averaging ‐11.4/‐6.4 mm Hg.
For each ACE inhibitor, do the manufacturer's dosage recommendations coincide with the findings of this review?
Assuming that the lowest effective dose should be the manufacturer's recommended starting dose, for 6 of the ACE inhibitors there is agreement between the manufacturer's recommended dose and the lowest effective dose determined by this systematic review (see Table 6). For benazepril, moexipril and ramipril, the lowest effective doses were determined to be higher than the manufacturer's recommended starting doses. Three of the ACE inhibitors (imidapril, quinapril and temocapril) did not have data available at lower doses to determine the lowest effective dose and thus no comparison could be made with the manufacturer's recommendations. For one ACE inhibitor, captopril, the lowest effective dose from this review was less than that which the manufacturer's recommended. Spirapril is not shown in Table 6 as it has no manufacturer's recommended dose that we are aware of.
6. Comparison of manufacturers' dosage recommendations and findings of this review.
| ACE Inhibitor | Lowest effective dose (mg/day) | Manufacturer's recommended starting dose (mg/day) | Lowest dose with near maximal BP lowering (mg/day) | Manufacturer's recommended maximum dose (mg/day) |
| benazepril | 20 | 10 | 20 | 40 |
| captopril | 37.5 | 50 | 37.5 | 150 |
| cilazapril | 2.5 | 2.5 | 2.5 | 10 |
| enalapril | 5 | 5 | 20 | 40 |
| fosinopril | 10‐20 | 10 | 20 | 40 |
| imidapril | Not estimable | 5 | Not estimable | 30 |
| lisinopril | 10 | 10 | 10 | 80 |
| moexipril | 15 | 7.5 | Not estimable | 30 |
| perindopril | 4 | 4 | 4 | 8 |
| quinapril | Not estimable | 10 | Not estimable | 40 |
| ramipril | 5 | 2.5 | 5 | 20 |
| temocapril | Not estimable | 1 | Not estimable | 4 |
| trandolapril | 1 | 1 | 1 | 4 |
For 9 of the ACE inhibitors the lowest dose with near maximal BP lowering was achieved at 1/4 to 1/2 of the manufacturer's recommended maximum daily dose. For lisinopril, most of the blood pressure lowering effect was achieved at only 1/8 of the recommended maximum dose. Quinapril and three other ACE inhibitors (imidapril, moexipril and temocapril) did not have data at higher doses to determine the lowest dose with near maximal blood pressure lowering.
What is the effect of ACE inhibitors on BP variability?
The endpoint variabilities of the ACE inhibitor and placebo groups were compared in order to determine the effect of ACE inhibitors on blood pressure variability. Compared with placebo, ACE inhibitors did not change the variability in blood pressure. It appears that blood pressure criteria for entry into the trial does have an effect on the variability at baseline. In the trials with DBP entry criteria, the baseline standard deviations were substantively lower than the endpoint values in the ACE inhibitor and placebo groups. This effect is likely due to truncation of the distribution of blood pressures at the threshold and due to participants with slightly lower DBP than the threshold level for entry into the trial being entered as having a DBP at the threshold.
Is there evidence of a dose‐response relationship for heart rate?
There is a possibility of selective reporting bias of resting heart rate since less than 20% of the trials reported data for this outcome. Based on the few trials for which data were available, there were insufficient data at higher doses to determine a dose‐related effect on heart rate. The available data demonstrate that for all doses ACE inhibitors did not have an effect on resting heart rate.
Is there evidence of a dose‐response relationship for withdrawals due to adverse effects?
There were not enough data to construct a meaningful dose‐response relationship for individual ACE inhibitors and when combined there still were insufficient data at higher doses to determine a dose‐related effect on WDAE. The available data demonstrate that for all doses ACE inhibitors did not change WDAE compared with placebo. However, only about half the trials reported the number of WDAE, so selective reporting bias is a distinct possibility. A description of the type and severity of the adverse effects that led to premature withdrawal was rarely reported. Short‐term trials are not the best type of trial to assess adverse effects and longer trials and other types of data can assist, such as non‐randomized trials or post‐marketing surveillance studies. However, there is no justification for not reporting all withdrawals due to adverse effects in all completed trials.
Limitations of the review
Many trials required imputation of the standard deviations of the blood pressure change because they did not report these values. However, our average estimates of the blood pressure lowering effect of these drugs were insensitive to the imputation strategy used.
One of the main limitations of this review is that not all the trials assessing the efficacy of ACE inhibitors have been published. We know that because many of the doses that have been approved by regulators are not included in this review. For example, quinapril has been approved for a dose range of 10 to 40 mg in Canada and 10 to 80 mg in the USA. We only found data for the effect of 20 mg of quinapril and we know that trials must have been completed and provided to the regulators for the other doses.
The use of maximum recommended dose by the manufacturer as a way of trying to compare equivalent doses of the drugs is imperfect but served our purposes in this review. Since this is planned to be published as a Cochrane review, it will be necessary to update it at least every 2 years. As more data for a wider range of doses become available, it may be possible to estimate the ED‐50 for each drug and thus use that criteria to combine the equieffective doses of the different ACE inhibitors.
What are the potential sources of bias?
Sequence generation, allocation concealment
Nearly all the trial publications simply reported that the trial was "randomized" but did not provide any details about the randomization method or the method of allocation concealment. Details of the methods for generation of the sequence of allocations or allocation concealment were reported in only 5 of the 92 (5.4%) included studies. Such vague reporting is insufficient to be confident that the allocation sequence was properly randomized and adequately concealed given the fact that many investigators use the term "randomized" when it is not justified. Authors should report their methods of sequence generation and allocation concealment clearly.
Blinding bias
Nearly all the trial publications simply reported that the trial was "double‐blind" but did not provide any details about the blinding methods. There was a potential for loss of blinding in the trials studying ACE inhibitors since these drugs have a well known side effect that is unique to this class of drugs, namely a refractory cough. However, none of the included studies reported a significantly higher rate of cough or withdrawals due to cough over placebo in patients treated with ACE inhibitors. The success of blinding in patients or investigators was not assessed in any of the included trials.
Attrition bias
It is unlikely that attrition bias would have had an impact on the systematic review since 89 to 100 percent of patients randomized to fixed‐dose monotherapy in each trial completed the double‐blind treatment period.
Selective reporting bias
This would not affect the blood pressure measurements as these were the primary outcome of most of these trials. As mentioned above, there is a potential for selective reporting bias for heart rate and withdrawals due to adverse effects.
Other potential sources of bias
Another potential source of bias that we became aware of in working on this review is selection bias. One of the exclusion criteria reported in nearly all trials was participants with a known hypersensitivity to ACE inhibitors. Although hypersensitivity to an ACE inhibitor may not have any connection to cough, it suggests that investigators have knowledge of each participant's prior experience with this drug class and thus may select for patients who have responded favorably to ACE inhibitors in terms of BP lowering or have been found to tolerate ACE inhibitor treatment. However, it was not possible to prove selection bias as none of the included trials described in detail these details of patient recruitment.
One could hypothesize that those patients who are known responders in previous trials tend to be recruited to participate in subsequent trials, so more recent trials may show a greater magnitude of blood pressure lowering efficacy. This hypothesis was tested by performing a post‐hoc tertile analysis according to the year of trial publication. The trials were divided into three groups and the oldest group of trials was compared with the group of most recent trials for mean blood pressure lowering efficacy. This analysis did not show a statistically significant difference in blood pressure lowering between the oldest and most recent group of trials. This finding does not support the hypothesis, however, it does not rule out the possibility of some selection bias occurring during both the older and newer trials.
Publication Bias
Yet another source of bias that may skew the results of systematic reviews is publication bias, which results from the selective publication of trials with positive results. This review was evaluated for the existence of publication bias since it only included and appraised published trial evidence. In the absence of bias, the funnel plot should resemble a symmetrical inverted funnel since the precision in the estimation of the true blood pressure lowering decreases as the study size decreases. Thus small studies will scatter more widely at the bottom of the graph (Cochrane Handbook). The most common way to investigate whether or not a review is subject to publication bias is to examine for funnel plot asymmetry as smaller studies with null results remained unpublished. The funnel plots generated from the results of the ACE inhibitor review did not demonstrate any signs of asymmetry.
A post‐hoc tertile analysis was conducted for the class of ACE inhibitors to corroborate the reasonable symmetry observed in the funnel plots. The studies were divided into three groups according to sample size in order to compare the mean effect estimates between the largest trials (highest tertile) and smallest trials (lowest tertile). The results of this analysis demonstrated no statistically significant difference in the estimate of the blood pressure lowering efficacy of ACE inhibitors between the smallest and largest trials. In this case, publication bias did not impact our estimate of the true effect size.
Visual examination of the funnel plots also showed little resemblance to a characteristic inverted funnel as there was an absence of smaller sized studies that scattered more widely at the bottom of the graph. One explanation for this is that smaller studies included in this systematic review were conducted and analyzed with similar methodological rigor as larger trials so the reported treatment effects are of similar precision. Another possibility is that smaller studies are of lower methodological quality than larger studies and have less precise estimates of the effect size, but those trials with little or no reduction in blood pressure and those trials with exaggerated effect estimates remain unpublished.
The results of this review underscore the need for all studies, regardless of the findings, to be published and accessible for secondary analysis. Trial registration has been recognized in order to improve transparency in research and knowledge sharing. In recent years, regulatory bodies around the world, led by the World Health Organization (WHO), have set standards for trial registration and reporting and are urging research institutions and companies to register all medical studies that test treatments on humans (WHO‐ICTRP). Initiatives such as the WHO's International Clinical Trials Registry Platform will help improve transparency and reduce the risk of publication bias skewing the results of future systematic reviews.
Authors' conclusions
Implications for practice.
Specific findings of the review
The review provides data on the dose‐related blood pressure lowering efficacy of 14 different ACE inhibitors at trough. The best estimate of the blood pressure lowering efficacy of these 14 drugs ranges from ‐6/‐4 to ‐9/‐5 mm Hg. The data do not suggest that any one ACE inhibitor is better or worse at lowering blood pressure when used at doses of one‐half the manufacturer's maximal recommended dose and above.
A dose‐response relationship for the blood pressure lowering effect of the ACE inhibitors was evident. A dose of 1/16 of the maximum recommended dose had no measurable blood pressure lowering effect. A dose of 1/8 or 1/4 of the maximum recommended daily achieved a blood pressure lowering effect that was 60 to 70% of the blood pressure lowering effect of the maximum recommended dose. A dose of 1/2 of the maximum recommended dose achieved a blood pressure lowering effect that was 90% of the maximum recommended dose.
ACE inhibitor doses above the maximum recommended dose did not significantly lower blood pressure more than the maximum recommended dose.
Combining the effects of half maximum recommended doses and higher gives an estimate of the average trough blood pressure lowering efficacy for ACE inhibitors as a class of drugs of ‐8 mm Hg for SBP and ‐5 mm Hg for DBP.
ACE inhibitors reduced blood pressure measured 1 to 12 hours after the dose by about 11/6 mm Hg.
ACE inhibitors reduced trough pulse pressure by about 3 mm Hg.
ACE inhibitors did not significantly affect resting blood pressure variability or heart rate.
All doses of ACE inhibitors, whether analyzed individually or combined, did not change WDAE as compared to placebo; however, this outcome was not reported for about half the trials so there is judged to be a high risk of selective reporting bias.
Implications of these findings
This systematic review provides the best available published evidence about the dose‐related blood pressure lowering efficacy of ACE inhibitors for the treatment of primary hypertension. These findings have the potential to change prescribing behavior and drug funding policies around the world. The evidence from this review suggests that there are no clinically meaningful differences between ACE inhibitors for lowering blood pressure. Thus, substantial cost savings can be achieved by prescribing the least expensive ACE inhibitor.
The major limitation of this review is that it is limited to published trials and it is evident that a lot of trials that manufacturers would have needed to gain marketing approval have not been published. Thus even though there was no evidence of publication bias using standard methods to asses this, there remains a high risk for publication bias. It is also estimated that there is a high risk of patient selection bias that could have led to overestimation of the blood pressure lowering effect. For these reasons the magnitude of blood pressure lowering found is this review is probably an overestimate of the true effect. This observation makes even more surprising that the estimates of trough and peak blood pressure lowering effects of the ACE inhibitors are modest at best and lower than commonly believed can be achieved by this class of drugs. In addition, the review demonstrates that 60 to 70% of the blood pressure lowering effect occurs with recommended starting doses and that there is no evidence for using doses higher than half the manufacturer’s maximum recommended daily dose. If physicians prescribing ACE inhibitors were aware of this evidence they would prescribe lower doses leading to substantial cost savings, and possibly leading to a reduction in dose‐related adverse events.
This review did not provide any evidence of an increase in withdrawals due to adverse effects overall and the trend towards higher withdrawals with higher doses was not statistically significant. However, this finding is severely limited by the short duration of the included trials and a high risk of both selective reporting bias and patient selection bias. Therefore, this systematic review is not a good measure of the incidence of adverse effects of this class of drugs.
Implications for research.
It is evident that for some of the ACE inhibitors studied (eg. quinapril and others) trials reporting data on doses recommended for use are not published. It should be mandatory that all clinical trials be registered and the results of these trials be published or otherwise made available in full detail.
Full dose‐response data for doses within the recommended and beyond the recommended dose range are needed to properly analyze the dose‐response relationship for each ACE inhibitor.
Trials should measure and report blood pressure data for peak effects as well as trough effects.
All trials should report withdrawals due to adverse effects and serious adverse events.
What's new
| Date | Event | Description |
|---|---|---|
| 18 June 2009 | Amended | In the plain language summary, the correct brand name for lisinopril was entered. |
History
Protocol first published: Issue 3, 2002 Review first published: Issue 4, 2008
| Date | Event | Description |
|---|---|---|
| 18 February 2009 | Amended | Plain language summary was edited to improve readability. |
Acknowledgements
The authors would like to acknowledge the assistance provided by Mr. Stephen Adams who retrieved the papers for this review.
Data and analyses
Comparison 1. Benazepril vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in trough SBP | 7 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 2 mg | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐11.87, 12.27] |
| 1.2 4 mg | 1 | 71 | Mean Difference (IV, Fixed, 95% CI) | ‐5.5 [‐12.17, 1.17] |
| 1.3 5 mg | 2 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐6.52 [‐16.09, 3.06] |
| 1.4 10 mg | 3 | 284 | Mean Difference (IV, Fixed, 95% CI) | ‐2.68 [‐5.98, 0.61] |
| 1.5 20 mg | 6 | 422 | Mean Difference (IV, Fixed, 95% CI) | ‐8.30 [‐11.14, ‐5.46] |
| 1.6 40 mg (Max Dose) | 2 | 74 | Mean Difference (IV, Fixed, 95% CI) | ‐8.68 [‐14.00, ‐1.35] |
| 1.7 80 mg | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | ‐11.40 [‐19.95, ‐2.85] |
| 2 Change in trough DBP | 7 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 2 mg | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | 1.1 [‐6.54, 8.74] |
| 2.2 4 mg | 1 | 71 | Mean Difference (IV, Fixed, 95% CI) | ‐4.10 [‐7.95, ‐0.25] |
| 2.3 5 mg | 2 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐2.04 [‐8.60, 4.53] |
| 2.4 10 mg | 3 | 283 | Mean Difference (IV, Fixed, 95% CI) | ‐0.72 [‐2.67, 1.22] |
| 2.5 20 mg | 6 | 422 | Mean Difference (IV, Fixed, 95% CI) | ‐4.53 [‐6.14, ‐2.93] |
| 2.6 40 mg (Max Dose) | 2 | 74 | Mean Difference (IV, Fixed, 95% CI) | ‐4.73 [‐9.15, ‐0.31] |
| 2.7 80 mg | 1 | 51 | Mean Difference (IV, Fixed, 95% CI) | ‐6.80 [‐11.60, 0.00] |
1.1. Analysis.
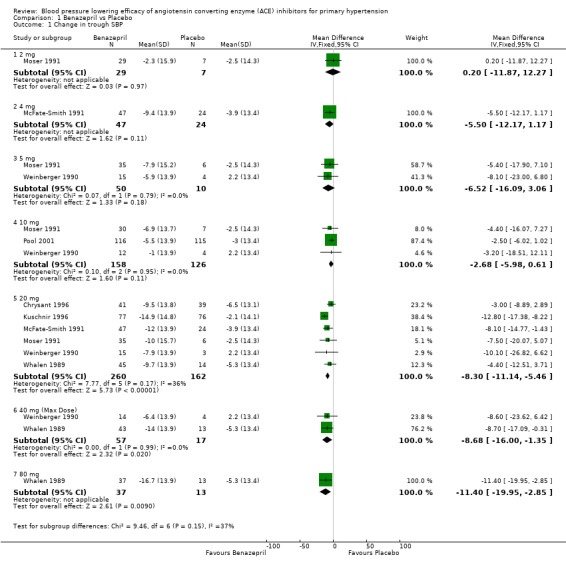
Comparison 1 Benazepril vs Placebo, Outcome 1 Change in trough SBP.
1.2. Analysis.
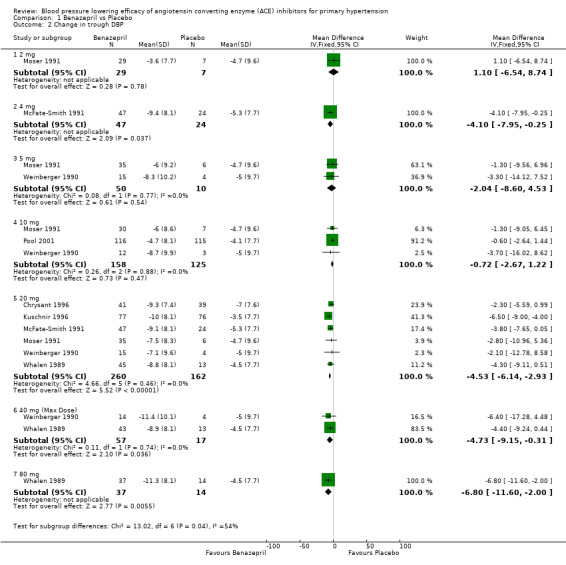
Comparison 1 Benazepril vs Placebo, Outcome 2 Change in trough DBP.
Comparison 2. Captopril vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in SBP | 5 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 37.5 mg | 1 | 111 | Mean Difference (IV, Fixed, 95% CI) | ‐8.6 [‐14.95, ‐2.25] |
| 1.2 50 mg | 3 | 324 | Mean Difference (IV, Fixed, 95% CI) | ‐8.25 [‐11.34, ‐5.16] |
| 1.3 75 mg | 2 | 124 | Mean Difference (IV, Fixed, 95% CI) | ‐9.16 [‐15.09, ‐3.23] |
| 1.4 100 mg | 1 | 96 | Mean Difference (IV, Fixed, 95% CI) | ‐12.0 [‐18.17, ‐5.83] |
| 1.5 150 mg (Max Dose) | 1 | 117 | Mean Difference (IV, Fixed, 95% CI) | ‐12.0 [‐18.06, ‐5.94] |
| 1.6 200 mg | 1 | 94 | Mean Difference (IV, Fixed, 95% CI) | ‐12.20 [‐18.32, ‐6.08] |
| 2 Change in DBP | 6 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 37.5 mg | 1 | 111 | Mean Difference (IV, Fixed, 95% CI) | ‐5.40 [‐8.74, ‐2.06] |
| 2.2 50 mg | 4 | 500 | Mean Difference (IV, Fixed, 95% CI) | ‐4.58 [‐6.02, ‐3.15] |
| 2.3 75 mg | 2 | 124 | Mean Difference (IV, Fixed, 95% CI) | ‐5.92 [‐9.16, ‐2.68] |
| 2.4 100 mg | 1 | 97 | Mean Difference (IV, Fixed, 95% CI) | ‐6.4 [‐9.91, ‐2.89] |
| 2.5 150 mg (Max Dose) | 1 | 117 | Mean Difference (IV, Fixed, 95% CI) | ‐7.3 [‐10.43, ‐4.17] |
| 2.6 200 mg | 1 | 94 | Mean Difference (IV, Fixed, 95% CI) | ‐6.70 [‐10.23, ‐3.17] |
2.1. Analysis.
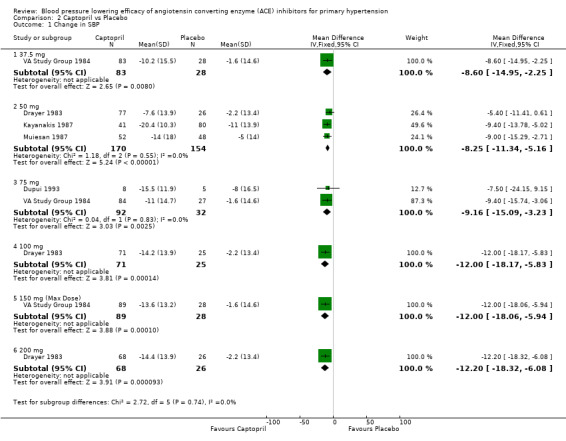
Comparison 2 Captopril vs Placebo, Outcome 1 Change in SBP.
2.2. Analysis.
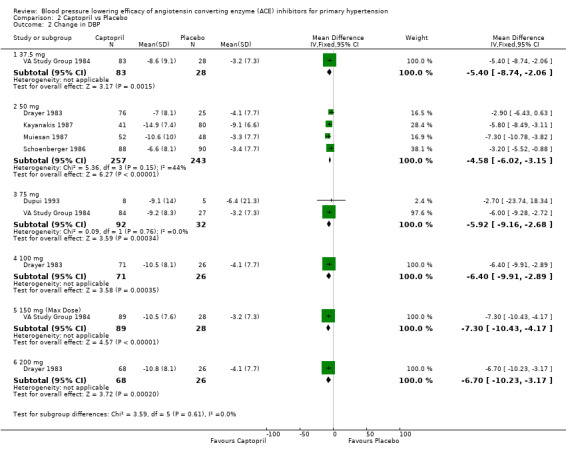
Comparison 2 Captopril vs Placebo, Outcome 2 Change in DBP.
Comparison 3. Cilazapril vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in trough SBP | 9 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 2.5 mg | 9 | 361 | Mean Difference (IV, Fixed, 95% CI) | ‐5.16 [‐8.32, 0.00] |
| 1.2 5 mg | 5 | 277 | Mean Difference (IV, Fixed, 95% CI) | ‐5.75 [‐9.38, ‐2.12] |
| 1.3 10 mg (Max Dose) | 1 | 67 | Mean Difference (IV, Fixed, 95% CI) | ‐7.0 [‐14.07, 0.07] |
| 2 Change in trough DBP | 14 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 0.5 mg | 1 | 129 | Mean Difference (IV, Fixed, 95% CI) | ‐0.5 [‐3.45, 2.45] |
| 2.2 1 mg | 1 | 56 | Mean Difference (IV, Fixed, 95% CI) | 1.1 [‐3.66, 5.86] |
| 2.3 2.5 mg | 13 | 558 | Mean Difference (IV, Fixed, 95% CI) | ‐3.32 [‐4.70, ‐1.94] |
| 2.4 5 mg | 9 | 569 | Mean Difference (IV, Fixed, 95% CI) | ‐3.49 [‐4.87, ‐2.11] |
| 2.5 10 mg (Max Dose) | 2 | 190 | Mean Difference (IV, Fixed, 95% CI) | ‐4.06 [‐6.44, ‐1.67] |
3.1. Analysis.
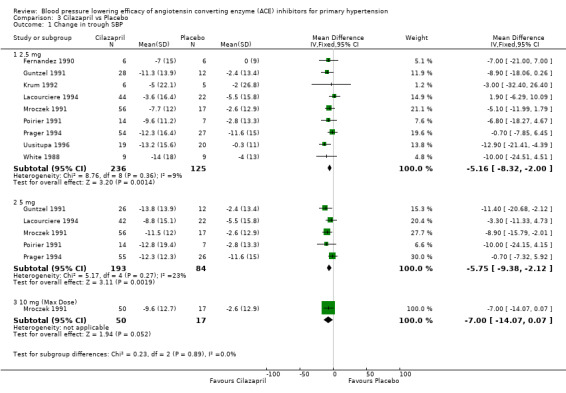
Comparison 3 Cilazapril vs Placebo, Outcome 1 Change in trough SBP.
3.2. Analysis.
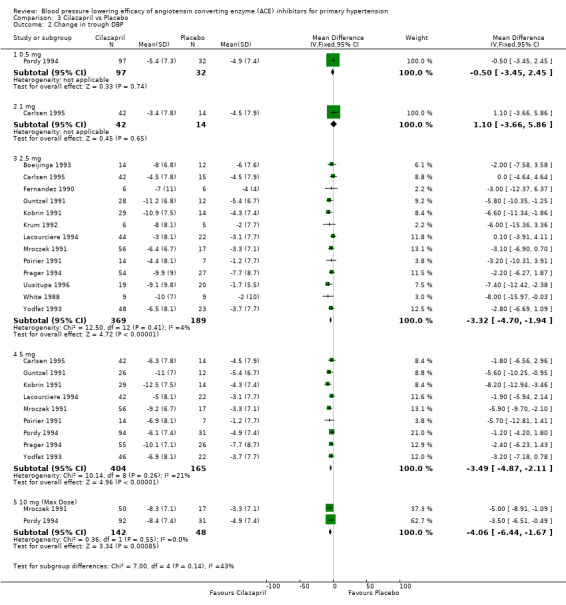
Comparison 3 Cilazapril vs Placebo, Outcome 2 Change in trough DBP.
Comparison 4. Enalapril vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in trough SBP | 17 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 5 mg | 4 | 552 | Mean Difference (IV, Fixed, 95% CI) | ‐5.56 [‐7.95, ‐3.18] |
| 1.2 10 mg | 8 | 1122 | Mean Difference (IV, Fixed, 95% CI) | ‐5.42 [‐5.00, ‐3.84] |
| 1.3 20 mg | 8 | 911 | Mean Difference (IV, Fixed, 95% CI) | ‐9.61 [‐11.35, ‐7.86] |
| 2 Change in trough DBP | 19 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 5 mg | 5 | 702 | Mean Difference (IV, Fixed, 95% CI) | ‐2.46 [‐3.67, ‐1.25] |
| 2.2 10 mg | 8 | 1122 | Mean Difference (IV, Fixed, 95% CI) | ‐3.10 [‐3.99, ‐2.20] |
| 2.3 20 mg | 9 | 984 | Mean Difference (IV, Fixed, 95% CI) | ‐5.34 [‐6.29, ‐4.38] |
4.1. Analysis.
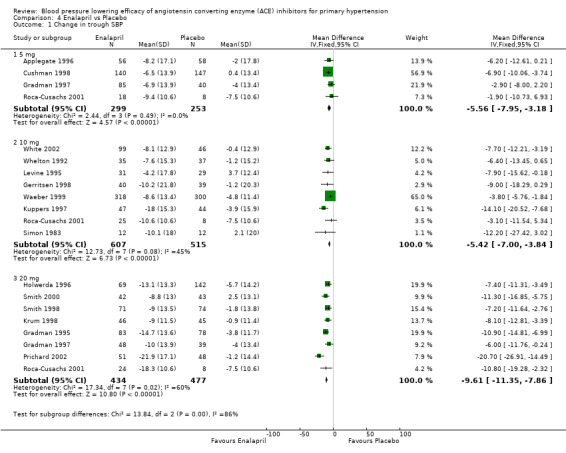
Comparison 4 Enalapril vs Placebo, Outcome 1 Change in trough SBP.
4.2. Analysis.
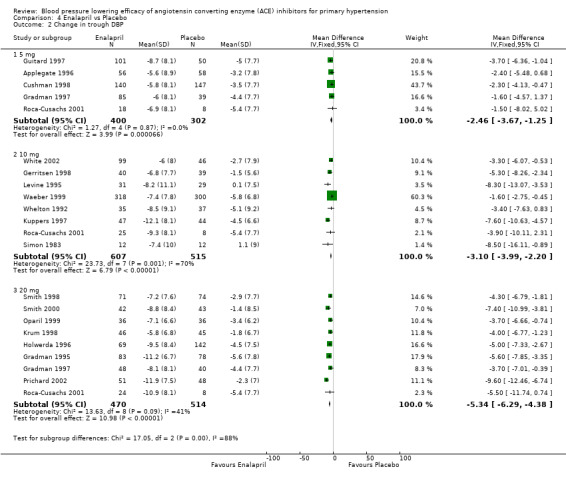
Comparison 4 Enalapril vs Placebo, Outcome 2 Change in trough DBP.
Comparison 5. Fosinopril vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in trough SBP | 6 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 2.5 mg | 1 | 38 | Mean Difference (IV, Fixed, 95% CI) | ‐2.9 [‐13.01, 7.21] |
| 1.2 5 mg | 1 | 94 | Mean Difference (IV, Fixed, 95% CI) | ‐3.70 [‐10.37, 2.97] |
| 1.3 10 mg | 3 | 151 | Mean Difference (IV, Fixed, 95% CI) | ‐3.86 [‐9.03, 1.30] |
| 1.4 20 mg | 5 | 208 | Mean Difference (IV, Fixed, 95% CI) | ‐9.26 [‐13.72, ‐4.79] |
| 1.5 40 mg (Max Dose) | 3 | 158 | Mean Difference (IV, Fixed, 95% CI) | ‐7.81 [‐12.91, ‐2.72] |
| 2 Change in trough DBP | 6 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 2.5 mg | 1 | 39 | Mean Difference (IV, Fixed, 95% CI) | ‐0.70 [‐6.31, 4.91] |
| 2.2 5 mg | 1 | 93 | Mean Difference (IV, Fixed, 95% CI) | ‐3.20 [‐7.12, 0.72] |
| 2.3 10 mg | 3 | 151 | Mean Difference (IV, Fixed, 95% CI) | ‐3.45 [‐6.42, ‐0.47] |
| 2.4 20 mg | 5 | 209 | Mean Difference (IV, Fixed, 95% CI) | ‐7.79 [‐10.12, ‐5.46] |
| 2.5 40 mg (Max Dose) | 3 | 157 | Mean Difference (IV, Fixed, 95% CI) | ‐4.73 [‐7.69, ‐1.76] |
5.1. Analysis.
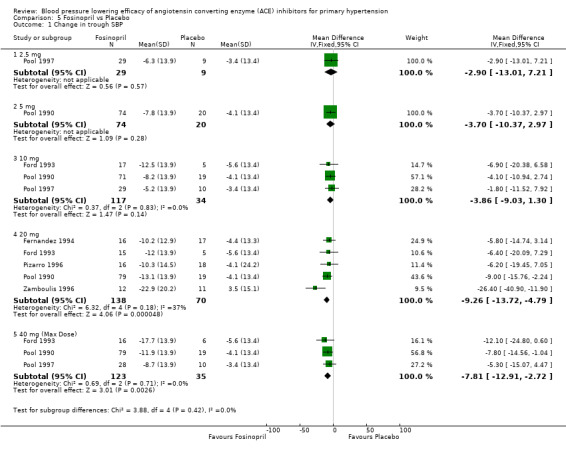
Comparison 5 Fosinopril vs Placebo, Outcome 1 Change in trough SBP.
5.2. Analysis.
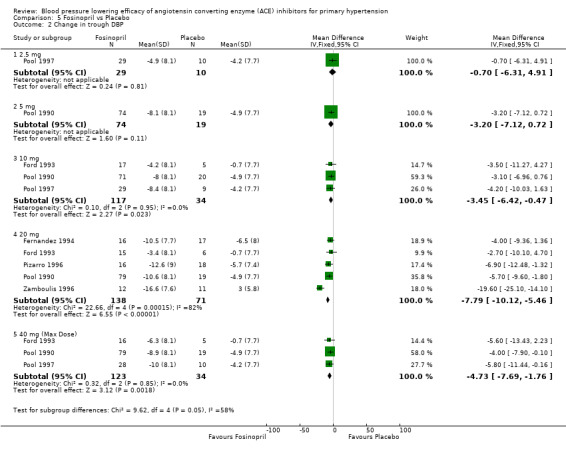
Comparison 5 Fosinopril vs Placebo, Outcome 2 Change in trough DBP.
Comparison 6. Imidapril vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in trough SBP | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 5 mg | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | ‐4.90 [‐15.96, 6.16] |
| 1.2 10 mg | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐8.90 [‐20.02, 2.22] |
| 1.3 20 mg (Max Dose) | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐12.90 [‐24.22, ‐1.58] |
| 1.4 40 mg | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | ‐10.60 [‐21.36, 0.16] |
| 2 Change in trough DBP | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 5 mg | 1 | 42 | Mean Difference (IV, Fixed, 95% CI) | ‐3.2 [‐10.28, 3.88] |
| 2.2 10 mg | 1 | 39 | Mean Difference (IV, Fixed, 95% CI) | ‐7.40 [‐15.16, 0.36] |
| 2.3 20 mg (Max Dose) | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐6.3 [‐13.60, 1.00] |
| 2.4 40 mg | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | ‐6.50 [‐13.89, 0.89] |
6.1. Analysis.
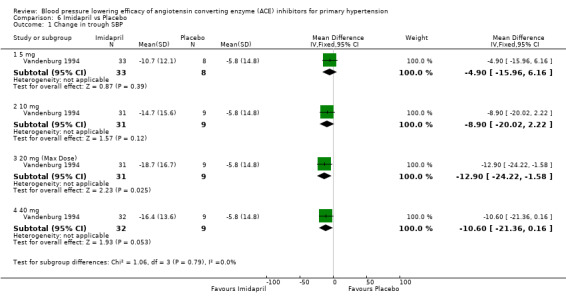
Comparison 6 Imidapril vs Placebo, Outcome 1 Change in trough SBP.
6.2. Analysis.
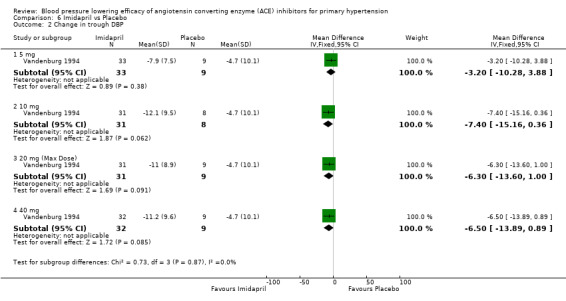
Comparison 6 Imidapril vs Placebo, Outcome 2 Change in trough DBP.
Comparison 7. Lisinopril vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in trough SBP | 5 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 1.25 mg | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | 3.2 [‐5.00, 13.40] |
| 1.2 5 mg | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | ‐2.0 [‐13.22, 9.22] |
| 1.3 10 mg | 4 | 648 | Mean Difference (IV, Fixed, 95% CI) | ‐7.75 [‐9.98, ‐5.51] |
| 1.4 20 mg | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | ‐7.80 [‐18.67, 3.07] |
| 1.5 80 mg (Max Dose) | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | ‐13.8 [‐24.46, ‐3.14] |
| 2 Change in trough DBP | 5 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 1.25 mg | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | 2.8 [‐2.34, 7.94] |
| 2.2 5 mg | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐5.32, 5.32] |
| 2.3 10 mg | 4 | 648 | Mean Difference (IV, Fixed, 95% CI) | ‐4.71 [‐5.92, ‐3.50] |
| 2.4 20 mg | 1 | 51 | Mean Difference (IV, Fixed, 95% CI) | ‐4.6 [‐10.17, 0.97] |
| 2.5 80 mg (Max Dose) | 1 | 49 | Mean Difference (IV, Fixed, 95% CI) | ‐6.00 [‐11.72, ‐0.28] |
7.1. Analysis.
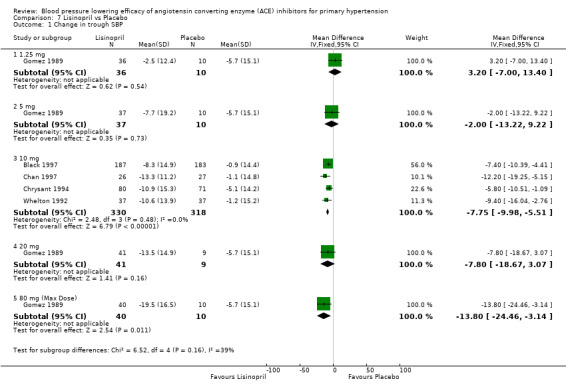
Comparison 7 Lisinopril vs Placebo, Outcome 1 Change in trough SBP.
7.2. Analysis.
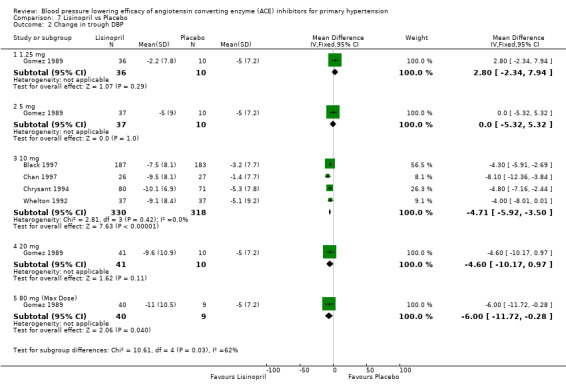
Comparison 7 Lisinopril vs Placebo, Outcome 2 Change in trough DBP.
Comparison 8. Moexipril vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in trough SBP | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 7.5 mg | 3 | 168 | Mean Difference (IV, Fixed, 95% CI) | ‐1.83 [‐6.71, 3.05] |
| 1.2 15 mg | 4 | 265 | Mean Difference (IV, Fixed, 95% CI) | ‐8.45 [‐11.99, ‐4.91] |
| 2 Change in trough DBP | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 7.5 mg | 3 | 167 | Mean Difference (IV, Fixed, 95% CI) | ‐2.23 [‐4.63, 0.16] |
| 2.2 15 mg | 4 | 266 | Mean Difference (IV, Fixed, 95% CI) | ‐4.38 [‐6.29, ‐2.46] |
8.1. Analysis.
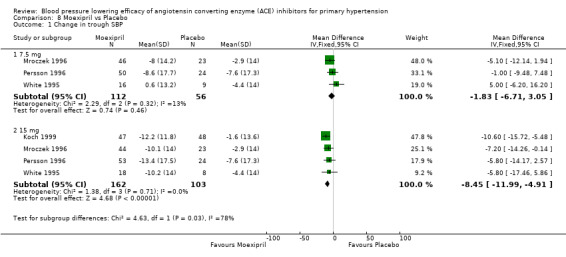
Comparison 8 Moexipril vs Placebo, Outcome 1 Change in trough SBP.
8.2. Analysis.
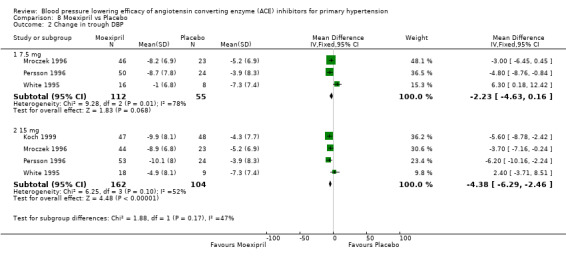
Comparison 8 Moexipril vs Placebo, Outcome 2 Change in trough DBP.
Comparison 9. Perindopril vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in trough SBP | 6 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 2 mg | 2 | 85 | Mean Difference (IV, Fixed, 95% CI) | ‐3.24 [‐13.20, 6.72] |
| 1.2 4 mg | 6 | 820 | Mean Difference (IV, Fixed, 95% CI) | ‐6.76 [‐9.41, ‐4.12] |
| 1.3 8 mg (Max Dose) | 2 | 82 | Mean Difference (IV, Fixed, 95% CI) | ‐9.81 [‐19.32, ‐0.31] |
| 1.4 16 mg | 1 | 67 | Mean Difference (IV, Fixed, 95% CI) | ‐8.9 [‐19.65, 1.85] |
| 2 Change in trough DBP | 6 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 2 mg | 2 | 85 | Mean Difference (IV, Fixed, 95% CI) | ‐2.10 [‐6.40, 2.20] |
| 2.2 4 mg | 6 | 820 | Mean Difference (IV, Fixed, 95% CI) | ‐4.91 [‐6.21, ‐3.61] |
| 2.3 8 mg (Max Dose) | 2 | 82 | Mean Difference (IV, Fixed, 95% CI) | ‐5.81 [‐10.11, ‐1.52] |
| 2.4 16 mg | 1 | 67 | Mean Difference (IV, Fixed, 95% CI) | ‐5.50 [‐10.09, ‐0.91] |
9.1. Analysis.
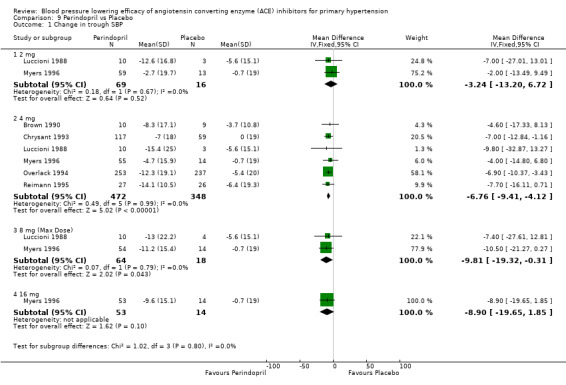
Comparison 9 Perindopril vs Placebo, Outcome 1 Change in trough SBP.
9.2. Analysis.
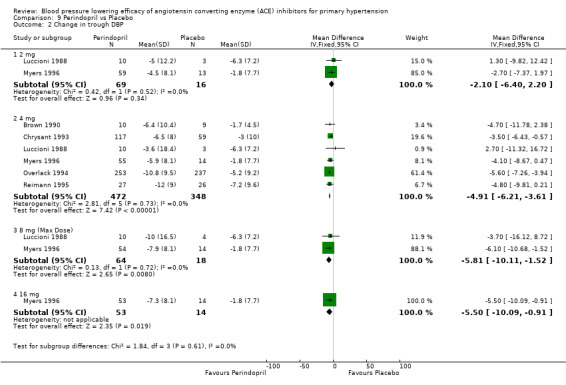
Comparison 9 Perindopril vs Placebo, Outcome 2 Change in trough DBP.
Comparison 10. Quinapril vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in trough SBP | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 20 mg | 3 | 196 | Mean Difference (IV, Fixed, 95% CI) | ‐5.87 [‐9.75, ‐1.99] |
| 2 Change in trough DBP | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 20 mg | 3 | 196 | Mean Difference (IV, Fixed, 95% CI) | ‐3.26 [‐5.85, ‐0.68] |
10.1. Analysis.
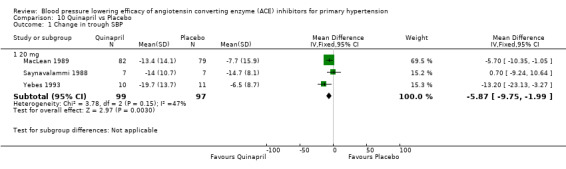
Comparison 10 Quinapril vs Placebo, Outcome 1 Change in trough SBP.
10.2. Analysis.
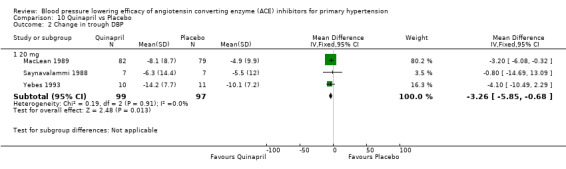
Comparison 10 Quinapril vs Placebo, Outcome 2 Change in trough DBP.
Comparison 11. Ramipril vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in trough SBP | 6 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 1.25 mg | 2 | 98 | Mean Difference (IV, Fixed, 95% CI) | 4.06 [‐1.97, 10.08] |
| 1.2 2.5 mg | 4 | 197 | Mean Difference (IV, Fixed, 95% CI) | ‐4.38 [‐9.71, 0.95] |
| 1.3 5 mg | 4 | 195 | Mean Difference (IV, Fixed, 95% CI) | ‐7.47 [‐12.76, ‐2.19] |
| 1.4 10 mg | 4 | 257 | Mean Difference (IV, Fixed, 95% CI) | ‐5.74 [‐9.33, ‐2.16] |
| 2 Change in trough DBP | 6 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 1.25 mg | 2 | 97 | Mean Difference (IV, Fixed, 95% CI) | 1.78 [‐1.83, 5.39] |
| 2.2 2.5 mg | 4 | 195 | Mean Difference (IV, Fixed, 95% CI) | ‐2.39 [‐5.18, 0.39] |
| 2.3 5 mg | 4 | 197 | Mean Difference (IV, Fixed, 95% CI) | ‐3.70 [‐6.38, ‐1.02] |
| 2.4 10 mg | 4 | 258 | Mean Difference (IV, Fixed, 95% CI) | ‐4.42 [‐6.54, ‐2.30] |
11.1. Analysis.
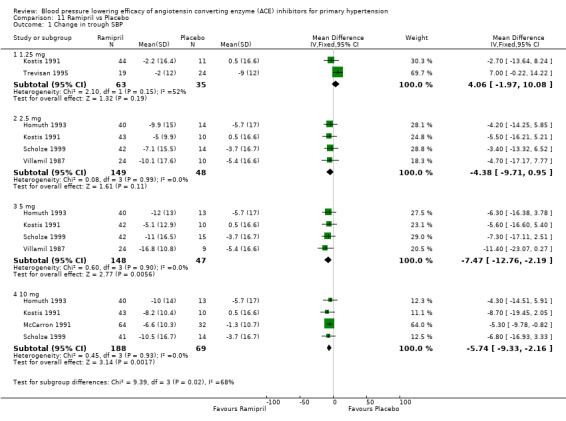
Comparison 11 Ramipril vs Placebo, Outcome 1 Change in trough SBP.
11.2. Analysis.
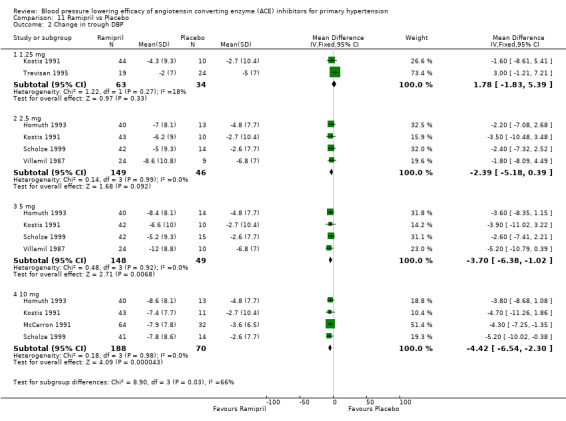
Comparison 11 Ramipril vs Placebo, Outcome 2 Change in trough DBP.
Comparison 12. Spirapril vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in trough SBP | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 3 mg | 2 | 130 | Mean Difference (IV, Fixed, 95% CI) | ‐4.09 [‐10.47, 2.29] |
| 1.2 6 mg | 3 | 210 | Mean Difference (IV, Fixed, 95% CI) | ‐7.66 [‐11.93, ‐3.40] |
| 1.3 12 mg (Max Dose) | 2 | 146 | Mean Difference (IV, Fixed, 95% CI) | ‐8.46 [‐13.27, ‐3.66] |
| 1.4 24 mg | 2 | 139 | Mean Difference (IV, Fixed, 95% CI) | ‐9.67 [‐14.39, ‐4.95] |
| 2 Change in trough DBP | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 3 mg | 2 | 130 | Mean Difference (IV, Fixed, 95% CI) | ‐3.91 [‐7.52, ‐0.29] |
| 2.2 6 mg | 4 | 359 | Mean Difference (IV, Fixed, 95% CI) | ‐6.52 [‐8.42, ‐4.62] |
| 2.3 12 mg (Max Dose) | 2 | 146 | Mean Difference (IV, Fixed, 95% CI) | ‐6.20 [‐9.20, ‐3.20] |
| 2.4 24 mg | 2 | 140 | Mean Difference (IV, Fixed, 95% CI) | ‐4.84 [‐7.86, ‐1.83] |
12.1. Analysis.
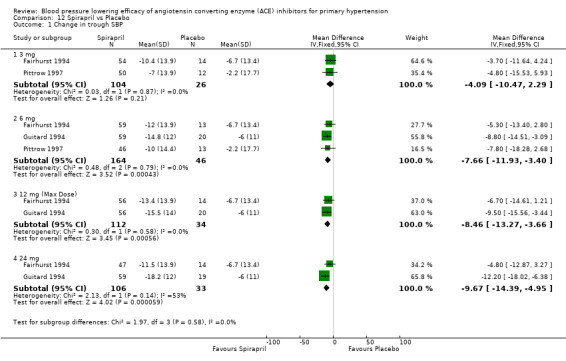
Comparison 12 Spirapril vs Placebo, Outcome 1 Change in trough SBP.
12.2. Analysis.
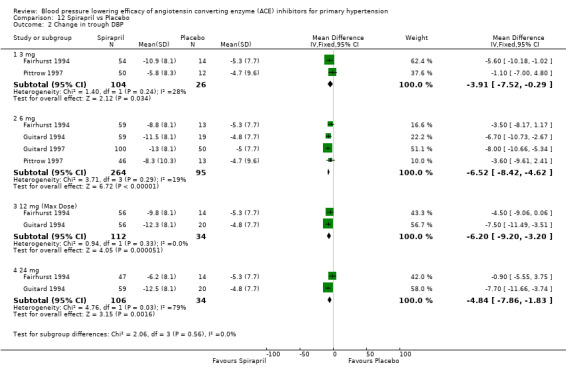
Comparison 12 Spirapril vs Placebo, Outcome 2 Change in trough DBP.
Comparison 13. Temocapril vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in trough SBP | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 20 mg | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | ‐10.0 [‐23.87, 3.87] |
| 2 Change in trough DBP | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 20 mg | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | ‐5.0 [‐13.34, 3.34] |
13.1. Analysis.
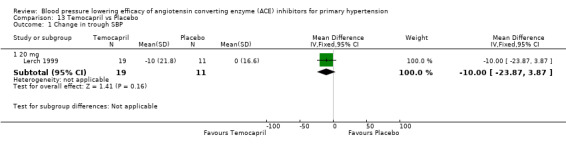
Comparison 13 Temocapril vs Placebo, Outcome 1 Change in trough SBP.
13.2. Analysis.
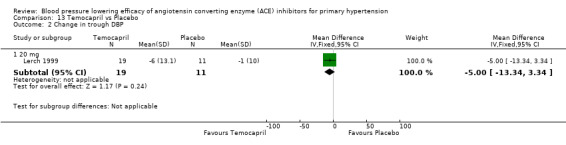
Comparison 13 Temocapril vs Placebo, Outcome 2 Change in trough DBP.
Comparison 14. Trandolapril vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in trough SBP | 10 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 0.25 mg | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | ‐2.7 [‐13.26, 7.86] |
| 1.2 0.5 mg | 4 | 185 | Mean Difference (IV, Fixed, 95% CI) | ‐3.33 [‐6.00, 1.33] |
| 1.3 1 mg | 4 | 294 | Mean Difference (IV, Fixed, 95% CI) | ‐8.45 [‐11.84, ‐5.06] |
| 1.4 2 mg | 7 | 636 | Mean Difference (IV, Fixed, 95% CI) | ‐6.21 [‐8.76, ‐3.66] |
| 1.5 4 mg (Max Dose) | 3 | 430 | Mean Difference (IV, Fixed, 95% CI) | ‐8.15 [‐10.82, ‐5.49] |
| 1.6 8 mg | 2 | 111 | Mean Difference (IV, Fixed, 95% CI) | ‐5.74 [‐12.52, 1.05] |
| 1.7 12 mg | 1 | 49 | Mean Difference (IV, Fixed, 95% CI) | ‐5.7 [‐16.60, 5.20] |
| 1.8 16 mg | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐7.10 [‐17.36, 3.16] |
| 2 Change in trough DBP | 10 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 0.25 mg | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | 0.6 [‐4.46, 5.66] |
| 2.2 0.5 mg | 4 | 184 | Mean Difference (IV, Fixed, 95% CI) | ‐2.33 [‐4.90, 0.24] |
| 2.3 1 mg | 4 | 294 | Mean Difference (IV, Fixed, 95% CI) | ‐4.07 [‐5.89, ‐2.25] |
| 2.4 2 mg | 7 | 637 | Mean Difference (IV, Fixed, 95% CI) | ‐4.24 [‐5.55, ‐2.94] |
| 2.5 4 mg (Max Dose) | 3 | 431 | Mean Difference (IV, Fixed, 95% CI) | ‐4.62 [‐6.10, ‐3.13] |
| 2.6 8 mg | 2 | 110 | Mean Difference (IV, Fixed, 95% CI) | ‐4.41 [‐7.82, ‐1.01] |
| 2.7 12 mg | 1 | 49 | Mean Difference (IV, Fixed, 95% CI) | ‐6.2 [‐11.78, ‐0.62] |
| 2.8 16 mg | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐6.2 [‐11.38, ‐1.02] |
14.1. Analysis.
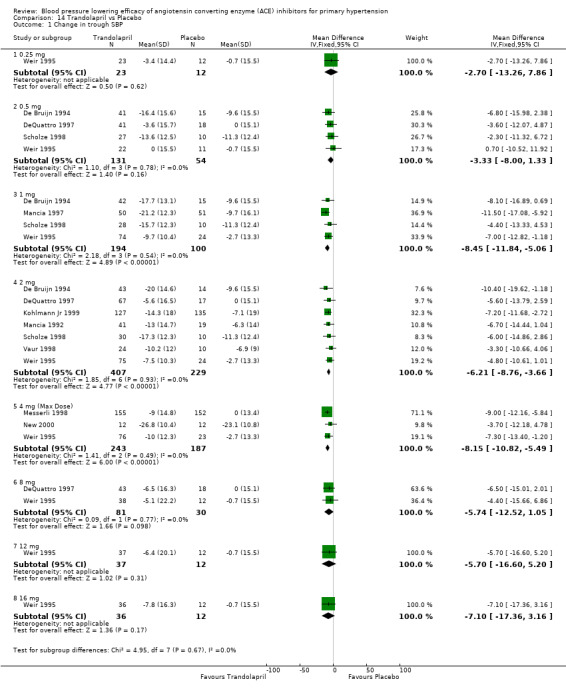
Comparison 14 Trandolapril vs Placebo, Outcome 1 Change in trough SBP.
14.2. Analysis.
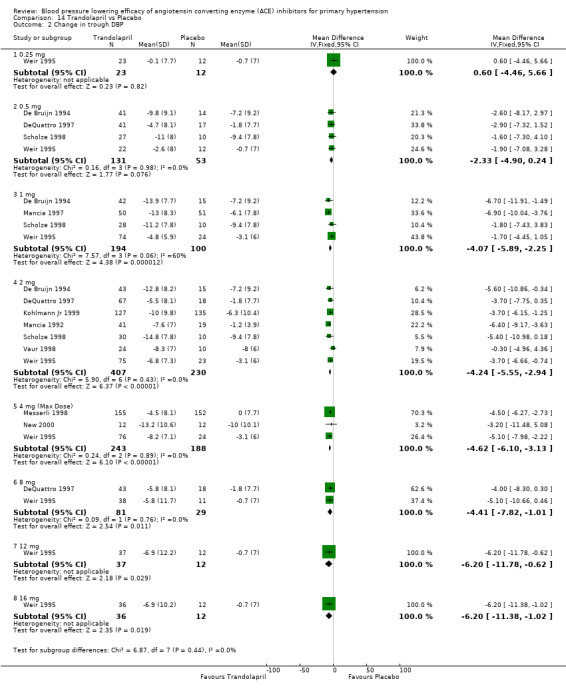
Comparison 14 Trandolapril vs Placebo, Outcome 2 Change in trough DBP.
Comparison 15. 1/16 Max Dose vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in trough SBP | 4 | 262 | Mean Difference (IV, Fixed, 95% CI) | ‐0.16 [‐3.78, 3.46] |
| 1.1 Fosinopril 2.5 mg | 1 | 58 | Mean Difference (IV, Fixed, 95% CI) | ‐2.9 [‐9.93, 4.13] |
| 1.2 Lisinopril 5 mg | 1 | 76 | Mean Difference (IV, Fixed, 95% CI) | ‐2.0 [‐9.79, 5.79] |
| 1.3 Ramipril 1.25 mg | 2 | 128 | Mean Difference (IV, Fixed, 95% CI) | 2.01 [‐3.02, 7.05] |
| 2 Change in trough DBP | 4 | 262 | Mean Difference (IV, Fixed, 95% CI) | 0.15 [‐1.86, 2.16] |
| 2.1 Fosinopril 2.5 mg | 1 | 58 | Mean Difference (IV, Fixed, 95% CI) | ‐0.70 [‐4.77, 3.37] |
| 2.2 Lisinopril 5 mg | 1 | 76 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐3.68, 3.68] |
| 2.3 Ramipril 1.25 mg | 2 | 128 | Mean Difference (IV, Fixed, 95% CI) | 0.70 [‐2.28, 3.67] |
15.1. Analysis.
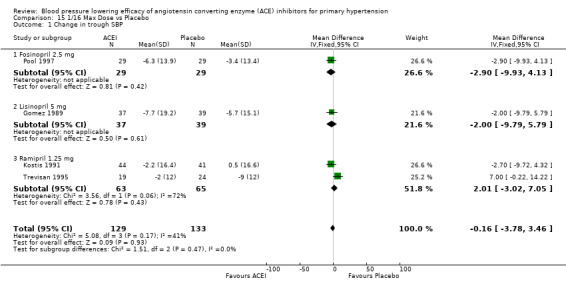
Comparison 15 1/16 Max Dose vs Placebo, Outcome 1 Change in trough SBP.
15.2. Analysis.
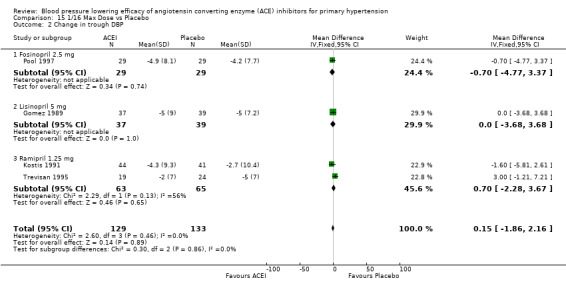
Comparison 15 1/16 Max Dose vs Placebo, Outcome 2 Change in trough DBP.
Comparison 16. 1/8 Max Dose vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in trough SBP | 18 | 2025 | Mean Difference (IV, Fixed, 95% CI) | ‐5.70 [‐6.95, ‐4.45] |
| 1.1 Benazepril 5 mg | 2 | 91 | Mean Difference (IV, Fixed, 95% CI) | ‐6.39 [‐12.32, ‐0.47] |
| 1.2 Enalapril 5 mg | 4 | 607 | Mean Difference (IV, Fixed, 95% CI) | ‐5.12 [‐7.33, ‐2.92] |
| 1.3 Fosinopril 5 mg | 1 | 151 | Mean Difference (IV, Fixed, 95% CI) | ‐3.7 [‐8.06, 0.66] |
| 1.4 Lisinopril 10 mg | 4 | 648 | Mean Difference (IV, Fixed, 95% CI) | ‐7.75 [‐9.98, ‐5.51] |
| 1.5 Ramipril 2.5 mg | 4 | 292 | Mean Difference (IV, Fixed, 95% CI) | ‐4.52 [‐8.05, ‐0.98] |
| 1.6 Trandolapril 0.5 mg | 3 | 236 | Mean Difference (IV, Fixed, 95% CI) | ‐4.19 [‐7.91, ‐0.46] |
| 2 Change in trough DBP | 19 | 2176 | Mean Difference (IV, Fixed, 95% CI) | ‐3.19 [‐3.88, ‐2.51] |
| 2.1 Benazepril 5 mg | 2 | 91 | Mean Difference (IV, Fixed, 95% CI) | ‐1.92 [‐5.89, 2.05] |
| 2.2 Enalapril 5 mg | 5 | 758 | Mean Difference (IV, Fixed, 95% CI) | ‐2.37 [‐3.52, ‐1.23] |
| 2.3 Fosinopril 5 mg | 1 | 151 | Mean Difference (IV, Fixed, 95% CI) | ‐3.20 [‐5.72, ‐0.68] |
| 2.4 Lisinopril 10 mg | 4 | 648 | Mean Difference (IV, Fixed, 95% CI) | ‐4.71 [‐5.92, ‐3.50] |
| 2.5 Ramipril 2.5 mg | 4 | 292 | Mean Difference (IV, Fixed, 95% CI) | ‐2.50 [‐4.50, ‐0.51] |
| 2.6 Trandolapril 0.5 mg | 3 | 236 | Mean Difference (IV, Fixed, 95% CI) | ‐2.46 [‐4.59, ‐0.33] |
16.1. Analysis.
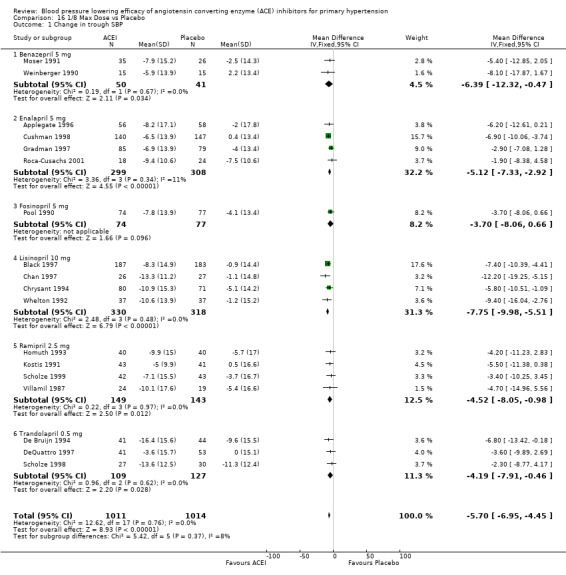
Comparison 16 1/8 Max Dose vs Placebo, Outcome 1 Change in trough SBP.
16.2. Analysis.
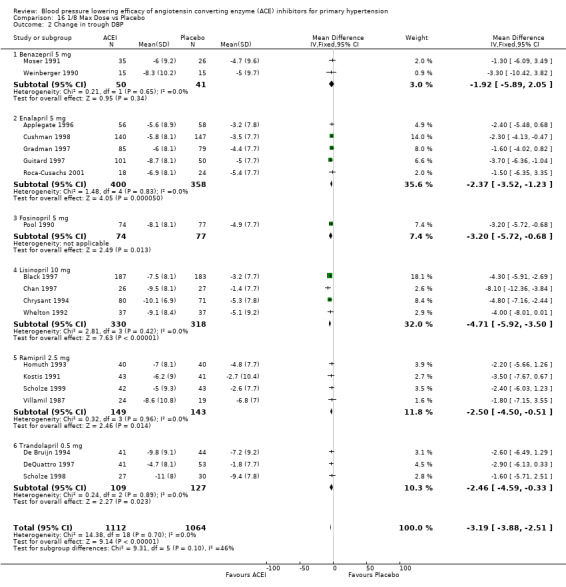
Comparison 16 1/8 Max Dose vs Placebo, Outcome 2 Change in trough DBP.
Comparison 17. 1/4 Max Dose vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in trough SBP | 40 | 3523 | Mean Difference (IV, Fixed, 95% CI) | ‐5.14 [‐6.05, ‐4.22] |
| 1.1 Benazepril 10 mg | 3 | 314 | Mean Difference (IV, Fixed, 95% CI) | ‐2.88 [‐5.92, 0.15] |
| 1.2 Cilazapril 2.5 mg | 9 | 462 | Mean Difference (IV, Fixed, 95% CI) | ‐4.76 [‐7.34, ‐2.18] |
| 1.3 Enalapril 10 mg | 8 | 1138 | Mean Difference (IV, Fixed, 95% CI) | ‐5.40 [‐6.93, ‐3.87] |
| 1.4 Fosinopril 10 mg | 3 | 239 | Mean Difference (IV, Fixed, 95% CI) | ‐3.93 [‐7.39, ‐0.46] |
| 1.5 Imidapril 5 mg | 1 | 68 | Mean Difference (IV, Fixed, 95% CI) | ‐4.90 [‐11.31, 1.51] |
| 1.6 Lisinopril 20 mg | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐7.8 [‐14.38, ‐1.22] |
| 1.7 Moexipril 7.5 mg | 3 | 223 | Mean Difference (IV, Fixed, 95% CI) | ‐1.86 [‐5.86, 2.14] |
| 1.8 Perindopril 2 mg | 2 | 134 | Mean Difference (IV, Fixed, 95% CI) | ‐3.02 [‐9.36, 3.31] |
| 1.9 Ramipril 5 mg | 4 | 291 | Mean Difference (IV, Fixed, 95% CI) | ‐7.19 [‐10.71, ‐3.67] |
| 1.10 Spirapril 3 mg | 2 | 184 | Mean Difference (IV, Fixed, 95% CI) | ‐4.02 [‐8.33, 0.28] |
| 1.11 Trandolapril 1 mg | 4 | 390 | Mean Difference (IV, Fixed, 95% CI) | ‐7.74 [‐10.34, ‐5.15] |
| 2 Change in trough DBP | 43 | 3758 | Mean Difference (IV, Fixed, 95% CI) | ‐3.04 [‐3.53, ‐2.54] |
| 2.1 Benazepril 10 mg | 3 | 314 | Mean Difference (IV, Fixed, 95% CI) | ‐0.89 [‐2.70, 0.93] |
| 2.2 Cilazapril 2.5 mg | 12 | 697 | Mean Difference (IV, Fixed, 95% CI) | ‐3.15 [‐4.29, 0.00] |
| 2.3 Enalapril 10 mg | 8 | 1138 | Mean Difference (IV, Fixed, 95% CI) | ‐3.11 [‐2.00, ‐2.23] |
| 2.4 Fosinopril 10 mg | 3 | 239 | Mean Difference (IV, Fixed, 95% CI) | ‐3.42 [‐5.43, ‐1.42] |
| 2.5 Imidapril 5 mg | 1 | 68 | Mean Difference (IV, Fixed, 95% CI) | ‐3.2 [‐7.41, 1.01] |
| 2.6 Lisinopril 20 mg | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐4.6 [‐8.63, ‐0.57] |
| 2.7 Moexipril 7.5 mg | 3 | 223 | Mean Difference (IV, Fixed, 95% CI) | ‐2.18 [‐4.11, ‐0.24] |
| 2.8 Perindopril 2 mg | 2 | 134 | Mean Difference (IV, Fixed, 95% CI) | ‐2.31 [‐5.06, 0.45] |
| 2.9 Ramipril 5 mg | 4 | 291 | Mean Difference (IV, Fixed, 95% CI) | ‐3.65 [‐5.62, ‐1.67] |
| 2.10 Spirapril 3 mg | 2 | 184 | Mean Difference (IV, Fixed, 95% CI) | ‐4.20 [‐6.66, ‐1.74] |
| 2.11 Trandolapril 1 mg | 4 | 390 | Mean Difference (IV, Fixed, 95% CI) | ‐3.52 [‐4.92, ‐2.11] |
17.1. Analysis.
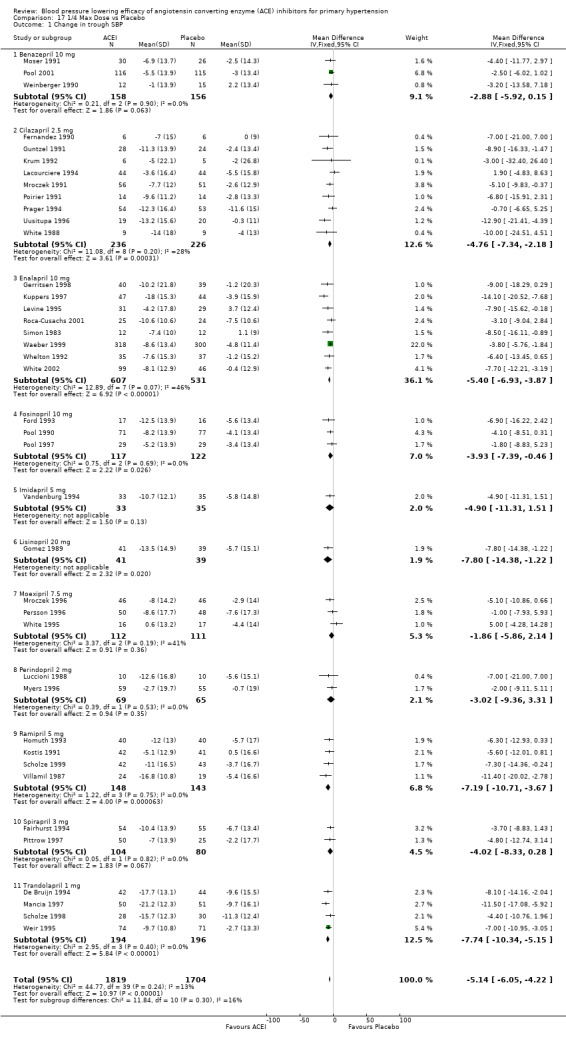
Comparison 17 1/4 Max Dose vs Placebo, Outcome 1 Change in trough SBP.
17.2. Analysis.
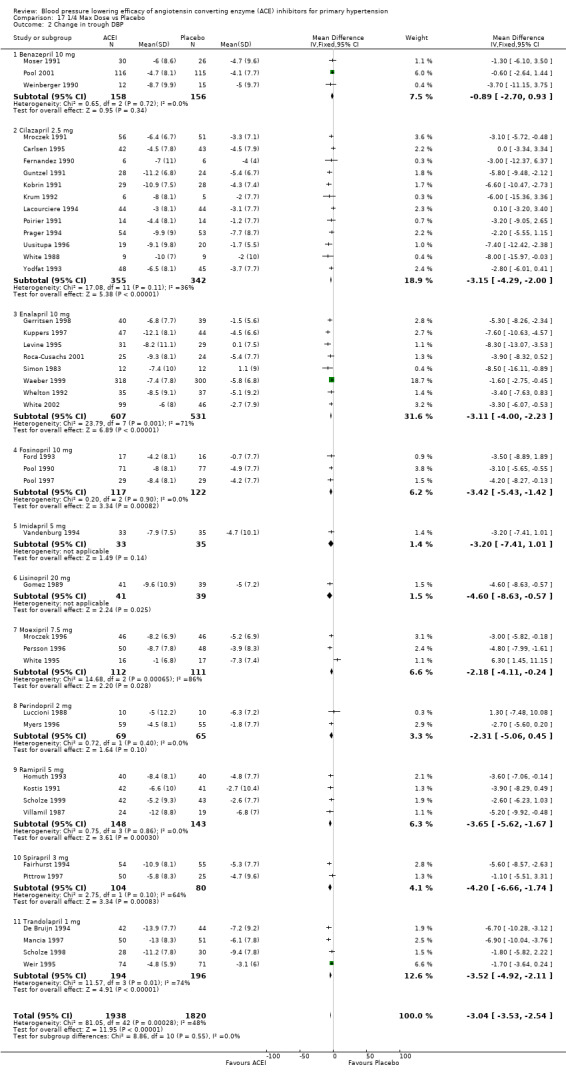
Comparison 17 1/4 Max Dose vs Placebo, Outcome 2 Change in trough DBP.
Comparison 18. 1/2 Max Dose vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in trough SBP | 51 | 4980 | Mean Difference (IV, Fixed, 95% CI) | ‐7.60 [‐8.40, ‐6.79] |
| 1.1 Benazepril 20 mg | 6 | 504 | Mean Difference (IV, Fixed, 95% CI) | ‐7.97 [‐10.41, ‐5.52] |
| 1.2 Cilazapril 5 mg | 5 | 379 | Mean Difference (IV, Fixed, 95% CI) | ‐5.92 [‐8.70, ‐3.14] |
| 1.3 Enalapril 20 mg | 8 | 967 | Mean Difference (IV, Fixed, 95% CI) | ‐9.54 [‐11.22, ‐7.86] |
| 1.4 Fosinopril 20 mg | 5 | 277 | Mean Difference (IV, Fixed, 95% CI) | ‐8.99 [‐12.35, ‐5.62] |
| 1.5 Imidapril 10 mg | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | ‐8.90 [‐16.26, ‐1.54] |
| 1.6 Lisinopril 40 mg | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.7 Moexipril 15 mg | 4 | 321 | Mean Difference (IV, Fixed, 95% CI) | ‐8.02 [‐11.16, ‐4.88] |
| 1.8 Perindopril 4 mg | 6 | 868 | Mean Difference (IV, Fixed, 95% CI) | ‐6.53 [‐9.04, ‐4.02] |
| 1.9 Quinapril 20 mg | 2 | 182 | Mean Difference (IV, Fixed, 95% CI) | ‐7.05 [‐11.26, ‐2.84] |
| 1.10 Ramipril 10 mg | 4 | 344 | Mean Difference (IV, Fixed, 95% CI) | ‐6.17 [‐9.07, ‐3.27] |
| 1.11 Spirapril 6 mg | 3 | 303 | Mean Difference (IV, Fixed, 95% CI) | ‐7.43 [‐10.41, ‐4.46] |
| 1.12 Trandolapril 2 mg | 7 | 769 | Mean Difference (IV, Fixed, 95% CI) | ‐6.17 [‐8.24, ‐4.10] |
| 2 Change in trough DBP | 57 | 5623 | Mean Difference (IV, Fixed, 95% CI) | ‐4.67 [‐5.09, ‐4.25] |
| 2.1 Benazepril 20 mg | 6 | 504 | Mean Difference (IV, Fixed, 95% CI) | ‐4.30 [‐5.70, ‐2.90] |
| 2.2 Cilazapril 5 mg | 9 | 800 | Mean Difference (IV, Fixed, 95% CI) | ‐3.40 [‐4.45, ‐2.36] |
| 2.3 Enalapril 20 mg | 9 | 1039 | Mean Difference (IV, Fixed, 95% CI) | ‐5.29 [‐6.22, ‐4.37] |
| 2.4 Fosinopril 20 mg | 5 | 277 | Mean Difference (IV, Fixed, 95% CI) | ‐6.86 [‐8.70, ‐5.02] |
| 2.5 Imidapril 10 mg | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | ‐7.40 [‐12.13, ‐2.67] |
| 2.6 Lisinopril 40 mg | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.7 Moexipril 15 mg | 4 | 321 | Mean Difference (IV, Fixed, 95% CI) | ‐4.26 [‐5.93, ‐2.60] |
| 2.8 Perindopril 4 mg | 6 | 868 | Mean Difference (IV, Fixed, 95% CI) | ‐4.81 [‐6.04, ‐3.58] |
| 2.9 Quinapril 20 mg | 2 | 182 | Mean Difference (IV, Fixed, 95% CI) | ‐3.35 [‐5.98, ‐0.72] |
| 2.10 Ramipril 10 mg | 4 | 344 | Mean Difference (IV, Fixed, 95% CI) | ‐4.47 [‐6.17, ‐2.76] |
| 2.11 Spirapril 6 mg | 4 | 453 | Mean Difference (IV, Fixed, 95% CI) | ‐5.92 [‐7.45, ‐4.39] |
| 2.12 Trandolapril 2 mg | 7 | 769 | Mean Difference (IV, Fixed, 95% CI) | ‐4.24 [‐5.35, ‐3.14] |
18.1. Analysis.
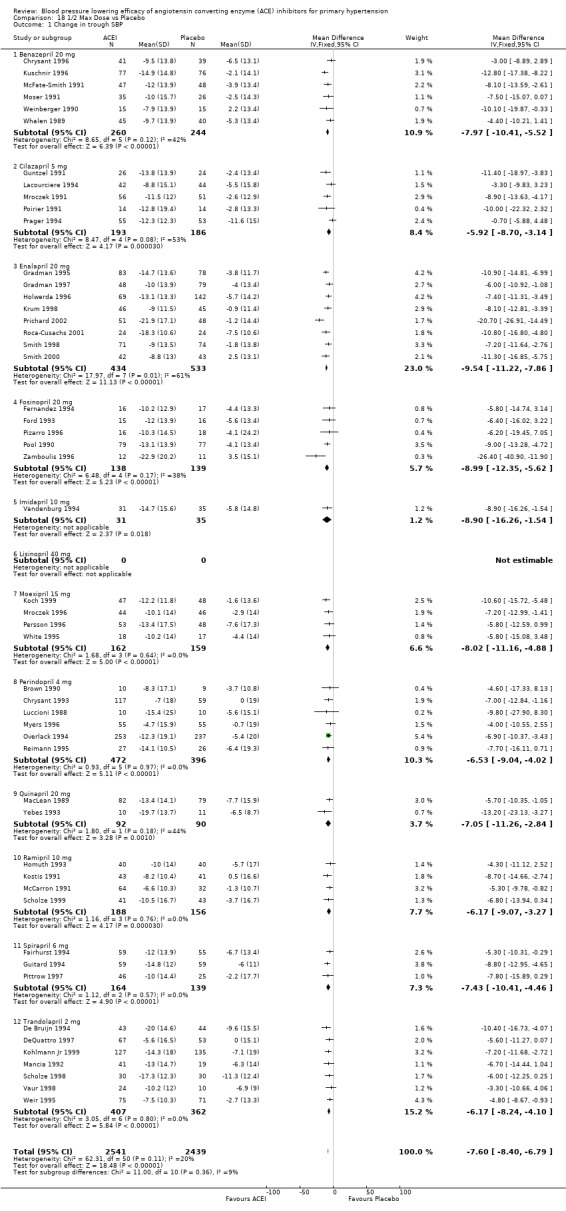
Comparison 18 1/2 Max Dose vs Placebo, Outcome 1 Change in trough SBP.
18.2. Analysis.
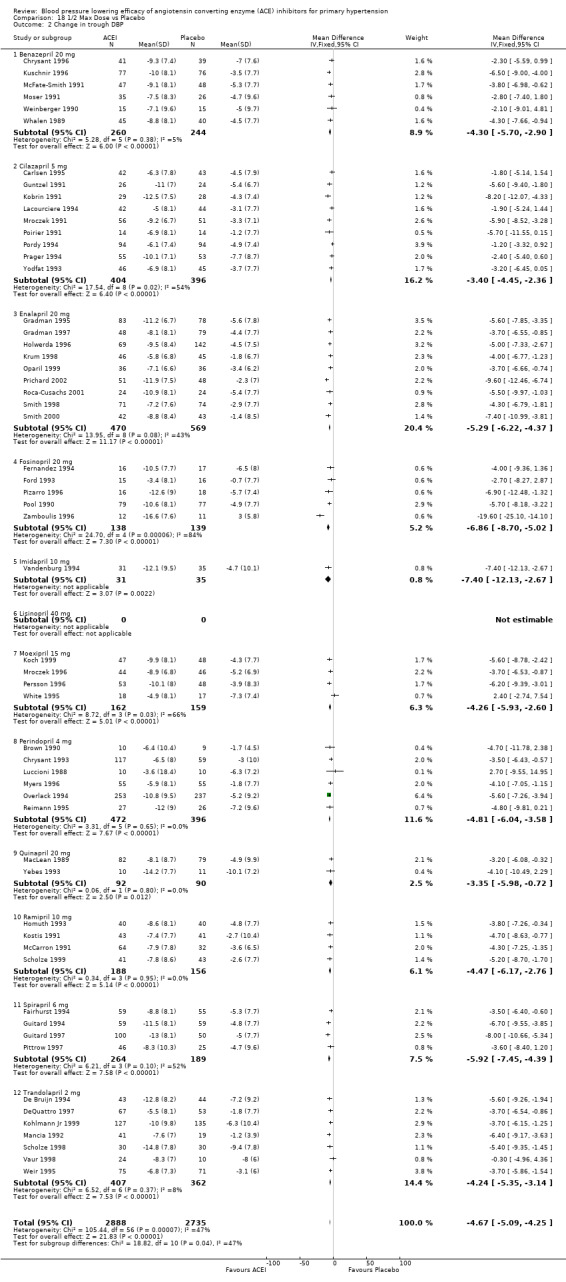
Comparison 18 1/2 Max Dose vs Placebo, Outcome 2 Change in trough DBP.
Comparison 19. Max Dose vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in trough SBP | 16 | 1450 | Mean Difference (IV, Fixed, 95% CI) | ‐8.48 [‐9.91, ‐7.06] |
| 1.1 Benazepril 40 mg | 2 | 112 | Mean Difference (IV, Fixed, 95% CI) | ‐8.67 [‐13.73, ‐3.62] |
| 1.2 Cilazapril 10 mg | 1 | 101 | Mean Difference (IV, Fixed, 95% CI) | ‐7.0 [‐11.99, ‐2.01] |
| 1.3 Enalapril 40 mg | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.4 Fosinopril 40 mg | 3 | 245 | Mean Difference (IV, Fixed, 95% CI) | ‐7.78 [‐11.20, ‐4.36] |
| 1.5 Imidapril 20 mg | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | ‐12.90 [‐20.56, ‐5.24] |
| 1.6 Lisinopril 80 mg | 1 | 79 | Mean Difference (IV, Fixed, 95% CI) | ‐13.8 [‐20.77, ‐6.83] |
| 1.7 Moexipril 30 mg | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.8 Perindopril 8 mg | 2 | 129 | Mean Difference (IV, Fixed, 95% CI) | ‐10.09 [‐16.14, ‐4.05] |
| 1.9 Quinapril 40 mg | 1 | 14 | Mean Difference (IV, Fixed, 95% CI) | ‐6.0 [‐20.16, 8.16] |
| 1.10 Ramipril 20 mg | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.11 Spirapril 12 mg | 2 | 226 | Mean Difference (IV, Fixed, 95% CI) | ‐8.23 [‐11.65, ‐4.82] |
| 1.12 Trandolapril 4 mg | 3 | 478 | Mean Difference (IV, Fixed, 95% CI) | ‐6.00 [‐10.41, ‐5.59] |
| 2 Change in trough DBP | 17 | 1636 | Mean Difference (IV, Fixed, 95% CI) | ‐4.95 [‐5.71, ‐4.20] |
| 2.1 Benazepril 40 mg | 2 | 112 | Mean Difference (IV, Fixed, 95% CI) | ‐4.76 [‐7.84, ‐1.69] |
| 2.2 Cilazapril 10 mg | 2 | 287 | Mean Difference (IV, Fixed, 95% CI) | ‐4.06 [‐5.74, ‐2.37] |
| 2.3 Enalapril 40 mg | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.4 Fosinopril 40 mg | 3 | 245 | Mean Difference (IV, Fixed, 95% CI) | ‐4.63 [‐6.61, ‐2.65] |
| 2.5 Imidapril 20 mg | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | ‐6.3 [‐10.88, ‐1.72] |
| 2.6 Lisinopril 80 mg | 1 | 79 | Mean Difference (IV, Fixed, 95% CI) | ‐6.00 [‐9.96, ‐2.04] |
| 2.7 Moexipril 30 mg | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.8 Perindopril 8 mg | 2 | 129 | Mean Difference (IV, Fixed, 95% CI) | ‐5.94 [‐8.81, ‐3.07] |
| 2.9 Quinapril 40 mg | 1 | 14 | Mean Difference (IV, Fixed, 95% CI) | ‐9.0 [‐17.78, ‐0.22] |
| 2.10 Ramipril 20 mg | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.11 Spirapril 12 mg | 2 | 226 | Mean Difference (IV, Fixed, 95% CI) | ‐6.02 [‐8.09, ‐3.96] |
| 2.12 Trandolapril 4 mg | 3 | 478 | Mean Difference (IV, Fixed, 95% CI) | ‐4.71 [‐6.05, ‐3.37] |
19.1. Analysis.
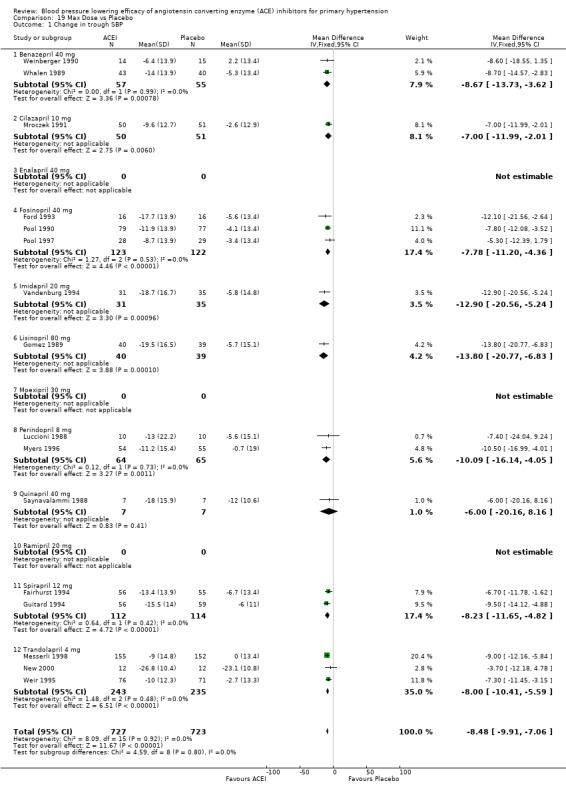
Comparison 19 Max Dose vs Placebo, Outcome 1 Change in trough SBP.
19.2. Analysis.
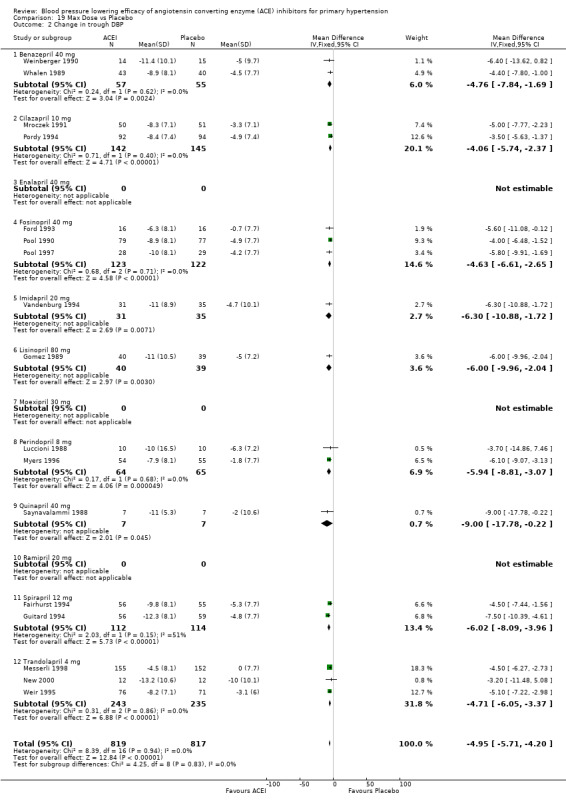
Comparison 19 Max Dose vs Placebo, Outcome 2 Change in trough DBP.
Comparison 20. 2 Max and Higher Doses vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in trough SBP | 7 | 738 | Mean Difference (IV, Fixed, 95% CI) | ‐8.81 [‐10.92, ‐6.70] |
| 1.1 Benazepril 80 mg | 1 | 77 | Mean Difference (IV, Fixed, 95% CI) | ‐11.40 [‐17.51, ‐5.29] |
| 1.2 Imidapril 40 mg | 1 | 67 | Mean Difference (IV, Fixed, 95% CI) | ‐10.60 [‐17.40, ‐3.80] |
| 1.3 Perindopril 16 mg | 1 | 108 | Mean Difference (IV, Fixed, 95% CI) | ‐8.9 [‐15.36, ‐2.44] |
| 1.4 Spirapril 24 mg | 2 | 220 | Mean Difference (IV, Fixed, 95% CI) | ‐9.40 [‐12.67, ‐6.12] |
| 1.5 Trandolapril 8, 12, 16 mg | 2 | 266 | Mean Difference (IV, Fixed, 95% CI) | ‐6.03 [‐10.14, ‐1.93] |
| 2 Change in trough DBP | 7 | 738 | Mean Difference (IV, Fixed, 95% CI) | ‐5.25 [‐6.45, ‐4.05] |
| 2.1 Benazepril 80 mg | 1 | 77 | Mean Difference (IV, Fixed, 95% CI) | ‐6.80 [‐10.34, ‐3.26] |
| 2.2 Imidapril 40 mg | 1 | 67 | Mean Difference (IV, Fixed, 95% CI) | ‐6.5 [‐11.22, ‐1.78] |
| 2.3 Perindopril 16 mg | 1 | 108 | Mean Difference (IV, Fixed, 95% CI) | ‐5.5 [‐8.48, ‐2.52] |
| 2.4 Spirapril 24 mg | 2 | 220 | Mean Difference (IV, Fixed, 95% CI) | ‐4.56 [‐6.66, ‐2.47] |
| 2.5 Trandolapril 8, 12, 16 mg | 2 | 266 | Mean Difference (IV, Fixed, 95% CI) | ‐5.02 [‐7.12, ‐2.93] |
20.1. Analysis.
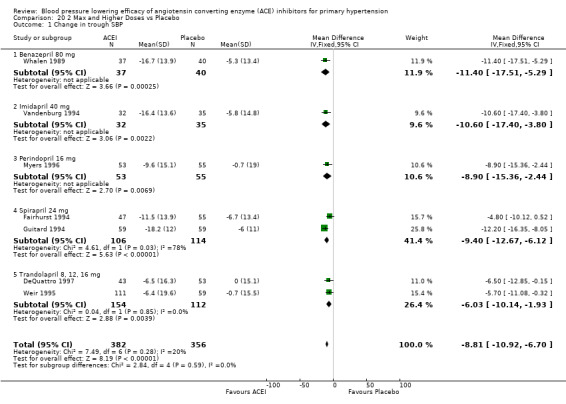
Comparison 20 2 Max and Higher Doses vs Placebo, Outcome 1 Change in trough SBP.
20.2. Analysis.
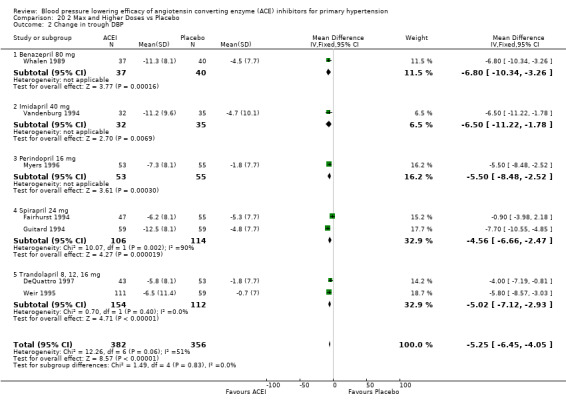
Comparison 20 2 Max and Higher Doses vs Placebo, Outcome 2 Change in trough DBP.
Comparison 21. 1/2 Max and Higher Doses vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in trough SBP | 53 | 6113 | Mean Difference (IV, Fixed, 95% CI) | ‐7.85 [‐8.60, ‐7.09] |
| 1.1 Benazepril 20, 40, 80 mg | 6 | 598 | Mean Difference (IV, Fixed, 95% CI) | ‐8.54 [‐10.87, ‐6.21] |
| 1.2 Cilazapril 5, 10 mg | 5 | 429 | Mean Difference (IV, Fixed, 95% CI) | ‐5.79 [‐8.46, ‐3.12] |
| 1.3 Enalapril 20, (40) mg | 8 | 967 | Mean Difference (IV, Fixed, 95% CI) | ‐9.54 [‐11.22, ‐7.86] |
| 1.4 Fosinopril 20, 40 mg | 4 | 359 | Mean Difference (IV, Fixed, 95% CI) | ‐7.44 [‐10.44, ‐4.44] |
| 1.5 Imidapril 10, 20, 40 mg | 1 | 129 | Mean Difference (IV, Fixed, 95% CI) | ‐10.8 [‐16.60, ‐5.00] |
| 1.6 Lisinopril (40), 80 mg | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | ‐13.8 [‐24.46, ‐3.14] |
| 1.7 Moexipril 15, (30) mg | 4 | 321 | Mean Difference (IV, Fixed, 95% CI) | ‐8.02 [‐11.16, ‐4.88] |
| 1.8 Perindopril 4, 8, 16 mg | 6 | 985 | Mean Difference (IV, Fixed, 95% CI) | ‐7.12 [‐9.55, ‐4.70] |
| 1.9 Quinapril 20, (40) mg | 2 | 182 | Mean Difference (IV, Fixed, 95% CI) | ‐7.05 [‐11.26, ‐2.84] |
| 1.10 Ramipril 10, (20) mg | 4 | 257 | Mean Difference (IV, Fixed, 95% CI) | ‐5.74 [‐9.33, ‐2.16] |
| 1.11 Spirapril 6, 12, 24 mg | 3 | 521 | Mean Difference (IV, Fixed, 95% CI) | ‐8.31 [‐10.80, ‐5.82] |
| 1.12 Trandolapril 2, 4, 8, 12, 16 mg | 9 | 1315 | Mean Difference (IV, Fixed, 95% CI) | ‐7.02 [‐8.70, ‐5.34] |
| 2 Change in trough DBP | 59 | 6861 | Mean Difference (IV, Fixed, 95% CI) | ‐4.73 [‐5.13, ‐4.34] |
| 2.1 Benazepril 20, 40, 80 mg | 6 | 598 | Mean Difference (IV, Fixed, 95% CI) | ‐4.56 [‐5.91, ‐3.22] |
| 2.2 Cilazapril 5, 10 mg | 9 | 942 | Mean Difference (IV, Fixed, 95% CI) | ‐3.58 [‐4.57, ‐2.60] |
| 2.3 Enalapril 20, (40) mg | 9 | 1039 | Mean Difference (IV, Fixed, 95% CI) | ‐5.29 [‐6.22, ‐4.37] |
| 2.4 Fosinopril 20, 40 mg | 4 | 359 | Mean Difference (IV, Fixed, 95% CI) | ‐5.15 [‐6.85, ‐3.45] |
| 2.5 Imidapril 10, 20, 40 mg | 1 | 129 | Mean Difference (IV, Fixed, 95% CI) | ‐6.7 [‐10.54, ‐2.86] |
| 2.6 Lisinopril (40), 80 mg | 1 | 79 | Mean Difference (IV, Fixed, 95% CI) | ‐6.00 [‐9.96, ‐2.04] |
| 2.7 Moexipril 15, (30) mg | 4 | 321 | Mean Difference (IV, Fixed, 95% CI) | ‐4.26 [‐5.93, ‐2.60] |
| 2.8 Perindopril 4, 8, 16 mg | 6 | 985 | Mean Difference (IV, Fixed, 95% CI) | ‐5.01 [‐6.18, ‐3.84] |
| 2.9 Quinapril 20, (40) mg | 2 | 182 | Mean Difference (IV, Fixed, 95% CI) | ‐3.35 [‐5.98, ‐0.72] |
| 2.10 Ramipril 10, (20) mg | 4 | 257 | Mean Difference (IV, Fixed, 95% CI) | ‐4.42 [‐6.55, ‐2.29] |
| 2.11 Spirapril 6, 12, 24 mg | 4 | 671 | Mean Difference (IV, Fixed, 95% CI) | ‐5.84 [‐7.19, ‐4.49] |
| 2.12 Trandolapril 2, 4, 8, 12, 16 mg | 9 | 1299 | Mean Difference (IV, Fixed, 95% CI) | ‐4.65 [‐5.55, ‐3.74] |
21.1. Analysis.
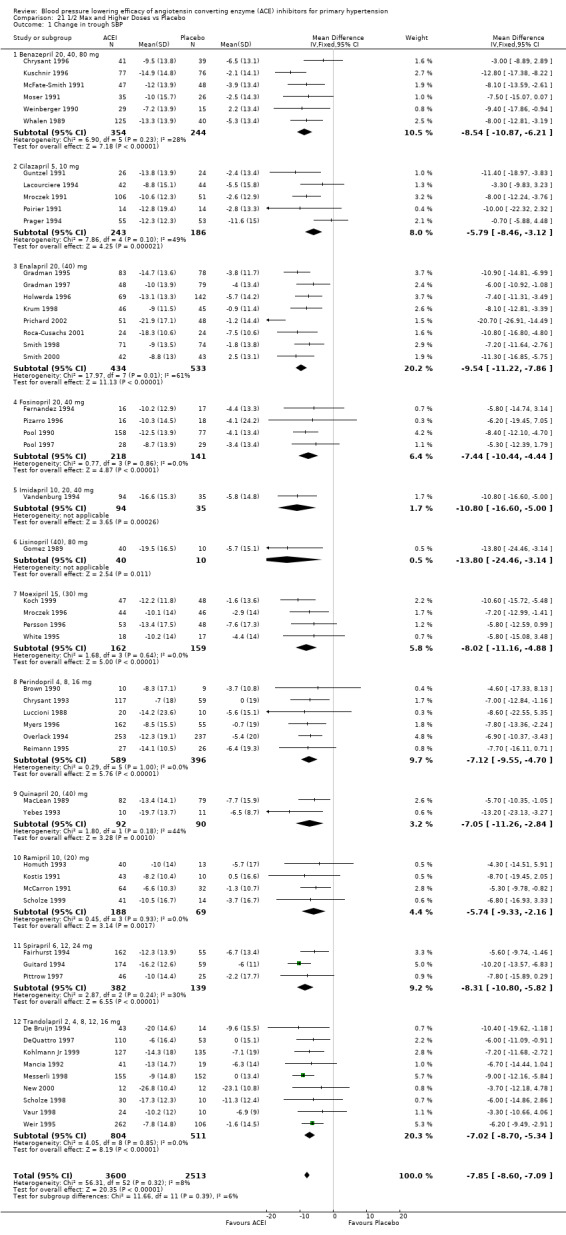
Comparison 21 1/2 Max and Higher Doses vs Placebo, Outcome 1 Change in trough SBP.
21.2. Analysis.
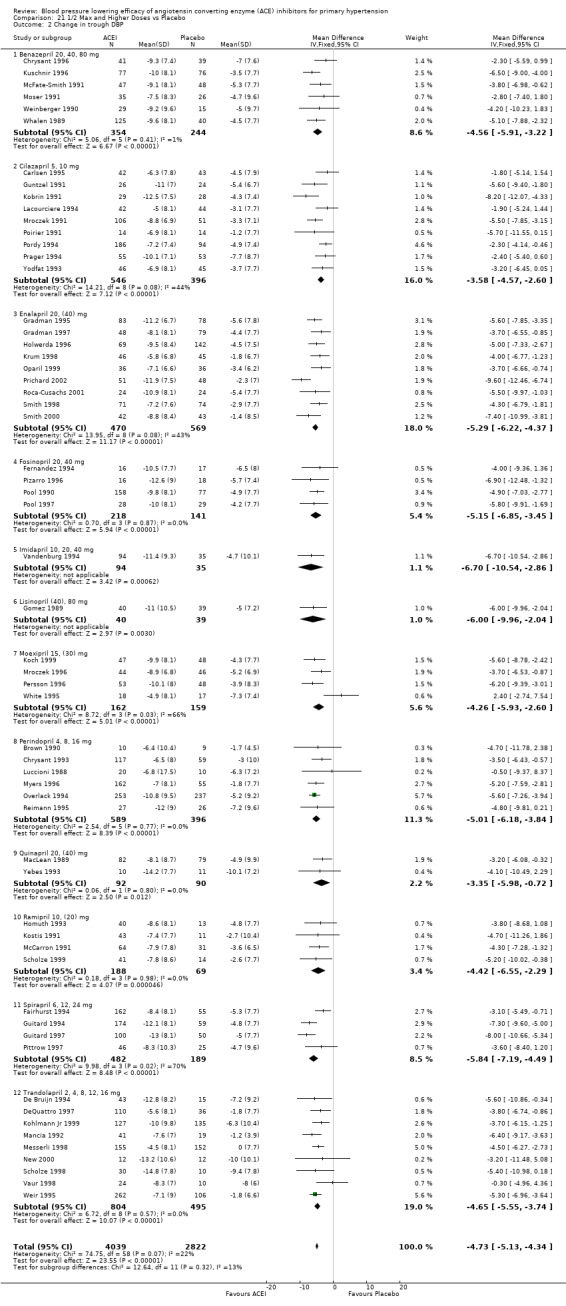
Comparison 21 1/2 Max and Higher Doses vs Placebo, Outcome 2 Change in trough DBP.
Comparison 22. ACE Inhibitors vs Placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in peak SBP [1/2 Max and Higher Doses Only] | 11 | 1154 | Mean Difference (IV, Fixed, 95% CI) | ‐11.53 [‐13.27, ‐9.78] |
| 1.1 1/2 Max Dose | 11 | 783 | Mean Difference (IV, Fixed, 95% CI) | ‐11.06 [‐13.11, ‐9.02] |
| 1.2 Max Dose | 3 | 143 | Mean Difference (IV, Fixed, 95% CI) | ‐11.48 [‐17.37, ‐5.60] |
| 1.3 2 Max Dose | 3 | 228 | Mean Difference (IV, Fixed, 95% CI) | ‐13.36 [‐17.40, ‐9.31] |
| 2 Change in peak DBP [1/2 Max and Higher Doses Only] | 15 | 1485 | Mean Difference (IV, Fixed, 95% CI) | ‐6.37 [‐7.15, ‐5.58] |
| 2.1 1/2 Max Dose | 15 | 1103 | Mean Difference (IV, Fixed, 95% CI) | ‐6.02 [‐6.95, ‐5.08] |
| 2.2 Max Dose | 4 | 157 | Mean Difference (IV, Fixed, 95% CI) | ‐6.49 [‐8.81, ‐4.16] |
| 2.3 2 Max Dose | 3 | 225 | Mean Difference (IV, Fixed, 95% CI) | ‐7.69 [‐9.56, ‐5.82] |
| 3 Change in peak SBP [All Doses] | 11 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 1/8 Max Dose | 1 | 11 | Mean Difference (IV, Fixed, 95% CI) | ‐11.3 [‐30.46, 7.86] |
| 3.2 1/4 Max Dose | 6 | 326 | Mean Difference (IV, Fixed, 95% CI) | ‐6.03 [‐9.93, ‐2.13] |
| 3.3 1/2 Max Dose | 11 | 724 | Mean Difference (IV, Fixed, 95% CI) | ‐10.97 [‐13.14, ‐8.80] |
| 3.4 Max Dose | 3 | 136 | Mean Difference (IV, Fixed, 95% CI) | ‐11.43 [‐17.69, ‐5.16] |
| 3.5 2 Max Dose | 3 | 211 | Mean Difference (IV, Fixed, 95% CI) | ‐13.58 [‐18.03, ‐9.13] |
| 4 Change in peak DBP [All Doses] | 15 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 1/8 Max Dose | 3 | 154 | Mean Difference (IV, Fixed, 95% CI) | ‐9.51 [‐12.64, ‐6.38] |
| 4.2 1/4 Max Dose | 9 | 451 | Mean Difference (IV, Fixed, 95% CI) | ‐3.69 [‐5.24, ‐2.15] |
| 4.3 1/2 Max Dose | 15 | 981 | Mean Difference (IV, Fixed, 95% CI) | ‐5.98 [‐7.02, ‐4.94] |
| 4.4 Max Dose | 4 | 157 | Mean Difference (IV, Fixed, 95% CI) | ‐6.49 [‐8.81, ‐4.16] |
| 4.5 2 Max Dose | 3 | 212 | Mean Difference (IV, Fixed, 95% CI) | ‐7.78 [‐9.74, ‐5.83] |
| 5 Change in trough heart rate | 16 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 1/8 Max Dose | 1 | 114 | Mean Difference (IV, Fixed, 95% CI) | ‐3.0 [‐6.62, 0.62] |
| 5.2 1/4 Max Dose | 10 | 587 | Mean Difference (IV, Fixed, 95% CI) | ‐0.47 [‐1.76, 0.81] |
| 5.3 1/2 Max Dose | 9 | 917 | Mean Difference (IV, Fixed, 95% CI) | ‐0.71 [‐1.99, 0.57] |
| 5.4 Max Dose | 2 | 89 | Mean Difference (IV, Fixed, 95% CI) | 1.31 [‐2.15, 4.76] |
| 6 Total withdrawals due to adverse effects | 56 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 1/16 Max Dose | 4 | 282 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.39, 2.57] |
| 6.2 1/8 Max Dose | 9 | 842 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.42, 1.82] |
| 6.3 1/4 Max Dose | 32 | 3385 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.42, 1.00] |
| 6.4 1/2 Max Dose | 38 | 3568 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.55, 1.19] |
| 6.5 Max Dose | 8 | 840 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.56, 2.35] |
| 6.6 2 Max Dose | 5 | 567 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.51 [0.68, 3.34] |
22.1. Analysis.
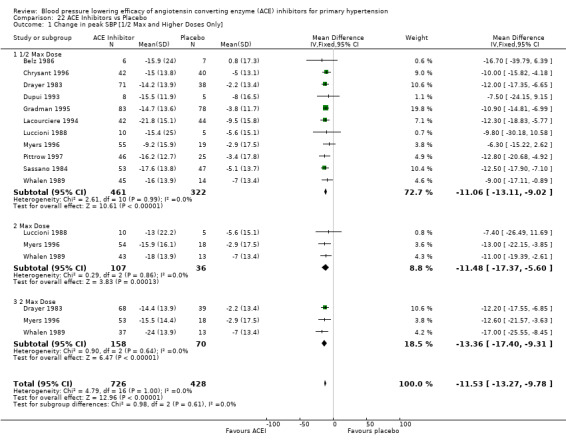
Comparison 22 ACE Inhibitors vs Placebo, Outcome 1 Change in peak SBP [1/2 Max and Higher Doses Only].
22.2. Analysis.
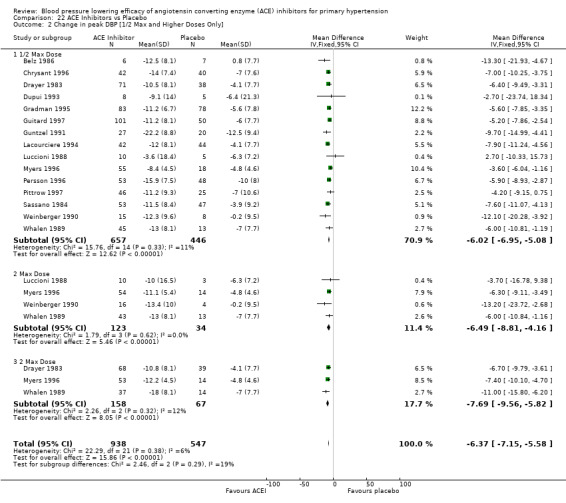
Comparison 22 ACE Inhibitors vs Placebo, Outcome 2 Change in peak DBP [1/2 Max and Higher Doses Only].
22.3. Analysis.
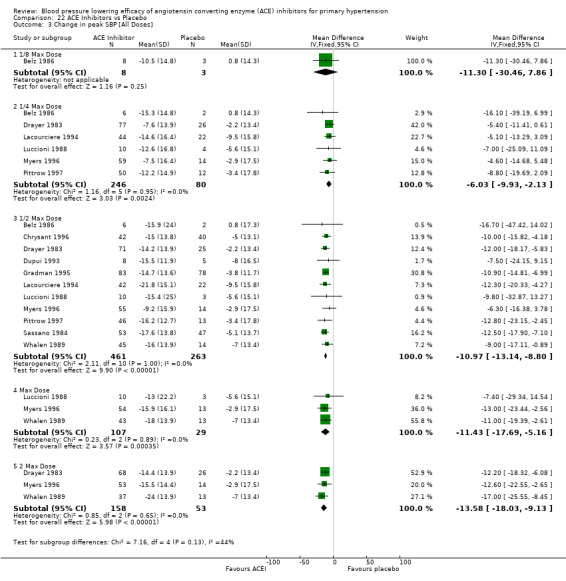
Comparison 22 ACE Inhibitors vs Placebo, Outcome 3 Change in peak SBP [All Doses].
22.4. Analysis.
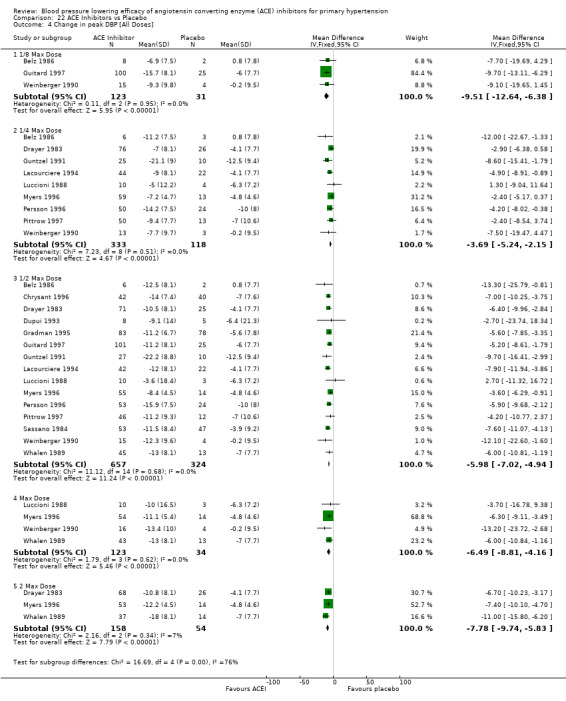
Comparison 22 ACE Inhibitors vs Placebo, Outcome 4 Change in peak DBP [All Doses].
22.5. Analysis.
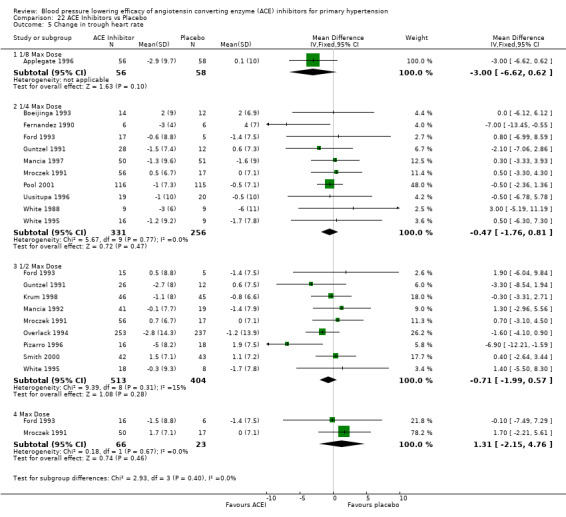
Comparison 22 ACE Inhibitors vs Placebo, Outcome 5 Change in trough heart rate.
22.6. Analysis.
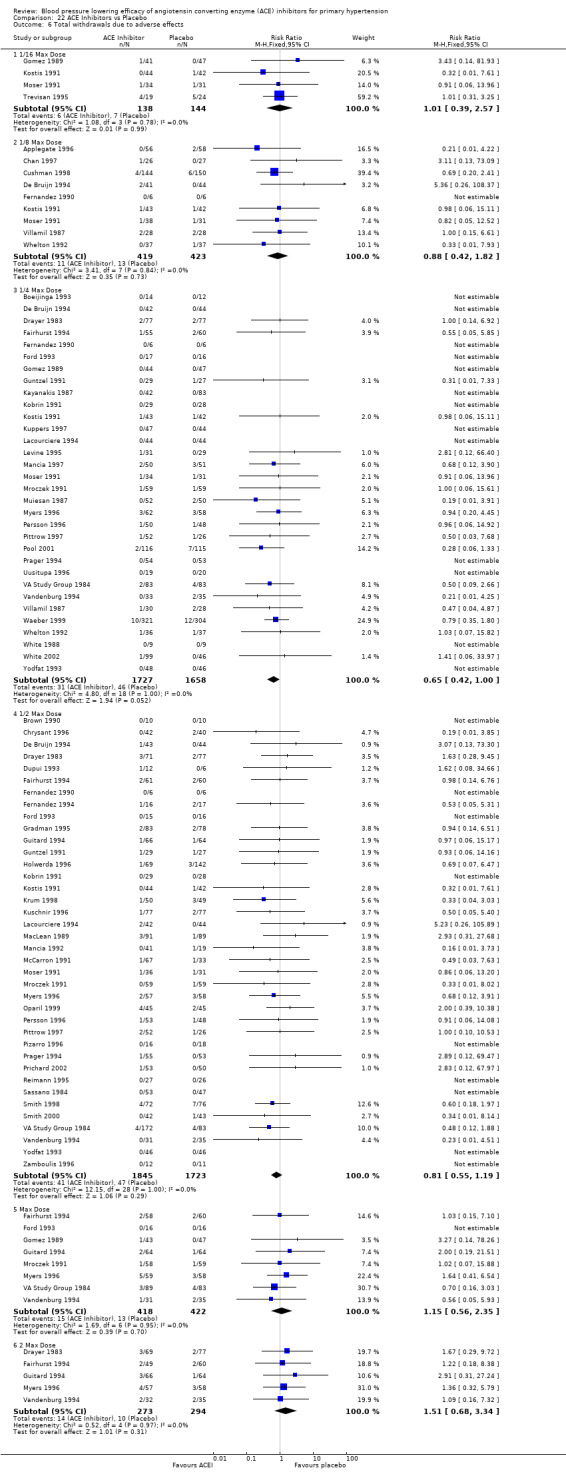
Comparison 22 ACE Inhibitors vs Placebo, Outcome 6 Total withdrawals due to adverse effects.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Applegate 1996.
| Methods | 7‐day washout period; 4‐week single‐blind placebo baseline phase; inclusion criteria= average sitting DBP 95‐115 mm Hg of week 2 and 4 of baseline phase recordings; 6‐week double‐blind treatment | |
| Participants | Enalapril 5 mg: n=56(38 males,18 females); mean age=52.5(11.2) years; baseline SBP=152.8(17.3) mm Hg, DBP=100.5(5.2) mm Hg, HR=77.4(9.2) bpm; Placebo: n=58(39 males,19 females); mean age=54.2(10.2) years; baseline SBP=152.5(13.0) mm Hg, DBP=100.4(4.8) mm Hg, HR=76.8(10.0) bpm | |
| Interventions | Enalapril 5 mg once daily; Placebo; administered in the morning (between 7:30 AM and 10:00 AM) | |
| Outcomes | Adjusted mean change from baseline in SBP/DBP using mercury sphygmomanometer; Trough sitting SBP/DBP using mercury sphygmomanometer; HR; WDAE | |
| Notes | Adjusted BP change reported, SD of change not reported, endpoint BP and SD reported; imputed endpoint SD for SD of change; used endpoint BP and SD data to calculate change in BP instead of entering adjusted BP change data; BP data from Table II, p. 53; Jadad score=4; funding source= Merck | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Belz 1986.
| Methods | 4‐week placebo washout; inclusion criteria= DBP 95‐114 mm Hg; 4‐week double‐blind treatment | |
| Participants | Cilazapril 1.25 mg: n=8(4 males,4 females); mean age=47.8(7.1) years; baseline sitting SBP=154.1(10.6) mm Hg, DBP=103.6(6.7) mm Hg; Cilazapril 2.5 mg: n=6(3 males,3 females); mean age=47.2(9.1) years; baseline sitting SBP=149.8(13.2) mm Hg, DBP=100.2(4.4) mm Hg; Cilazapril 5 mg: n=6(2 males,4 females); mean age=51.5(9.1) years; baseline sitting SBP=162.2(24.0) mm Hg, DBP=104.3(5.5) mm Hg; Placebo: n=7(3 males,4 females); mean age=52.7(9.6) years; baseline sitting SBP=148.3(17.3) mm Hg, DBP=98.3(4.9) mm Hg | |
| Interventions | Cilazapril 1.25 mg once daily; Cilazapril 2.5 mg once daily; Cilazapril 5 mg once daily; Placebo; administered in the morning at approximately 7 AM | |
| Outcomes | Peak sitting SBP/DBP | |
| Notes | BP change and SD of change not reported, endpoint BP and SD reported; imputed endpoint SD for SD of change; BP data from Table 2, p. 526; lying and standing BP data also available; Jadad score=2; funding source= Hoffmann‐La Roche AG | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Black 1997.
| Methods | 2‐ to 4‐week placebo run‐in; inclusion criteria= sitting DBP 95‐115 mm Hg after run‐in; 12‐week total double‐blind treatment, 4‐week double‐blind treatment at initial fixed dose, non‐responders were up‐titrated after 4 weeks | |
| Participants | Lisinopril 10 mg: n=187(112 males,75 females); mean age=53.9(10.7) years; baseline sitting SBP=153.9(14.9) mm Hg, DBP=101.0(4.5) mm Hg; Placebo: n=183(113 males,70 females); mean age=54.0(11.8) years; baseline sitting SBP=154.1(14.4) mm Hg, DBP=101.0(4.4) mm Hg | |
| Interventions | Lisinopril 10 mg once daily; Placebo; administered at approximately 8 AM | |
| Outcomes | Least mean square change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer | |
| Notes | Used week 4 BP data only; BP change reported, SD of change not reported, endpoint BP and SD not reported; imputed SBP SD of change from baseline SBP SD of change, imputed overall trial mean DBP SD of change; SBP data from Figure 1, p. 487, DBP data from text, p. 485; Jadad score=2; funding source= Ciba‐Geigy | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Boeijinga 1993.
| Methods | Inclusion criteria= sitting DBP 90‐105 mm Hg before start of study; 3‐week double‐blind treatment | |
| Participants | Cilazapril 2.5 mg: n=14(11 males,3 females); mean age=63.7(4.2) years; baseline SBP=139 mm Hg, DBP=92 mm Hg; Placebo: n=12(10 males,2 females); mean age=63.3(7.8) years; baseline SBP=135 mm Hg, DBP=92 mm Hg | |
| Interventions | Cilazapril 2.5 mg once daily; Placebo; administered in the morning before breakfast | |
| Outcomes | Peak (2‐3 h after dosing) supine SBP/DBP using mercury sphygmomanometer; Peak (2‐3 h after dosing) HR; WDAE | |
| Notes | Used DBP only since patients did not have SBP >/= 140 mm Hg at baseline; BP change and SD of change not reported, endpoint BP and SD reported; imputed endpoint SD for SD of change; BP data from text, p. 446; Jadad score=3; funding source= Hoffman‐La Roche Ltd. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Brown 1990.
| Methods | 2‐week single‐blind placebo run‐in; inclusion criteria= supine DBP 95‐115 mm Hg after run‐in; 4‐week double‐blind treatment | |
| Participants | All patients: n=40(19 males,21 females); mean age=58 years; baseline upright SBP=154(15) mm Hg, DBP=102(7) mm Hg | |
| Interventions | Perindopril 4 mg once daily; Placebo | |
| Outcomes | Mean change from baseline in trough erect SBP/DBP using mercury sphygmomanometer; Mean change from baseline in trough supine SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SEM of change reported, endpoint BP and SD not reported; calculated SD of change from N and SEM of change; BP data from Table 2, p. 329; Jadad score=4; funding source= Servier | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Carlsen 1995.
| Methods | 4‐week single‐blind placebo run‐in; inclusion criteria= mean pre‐dose sitting DBP 100‐115 mm Hg after 3 and 4 weeks of run‐in, mean baseline DBP >/= 100 mm Hg at hourly measurements 21‐24 h post‐placebo and also during whole BP profile (i.e. hourly measurements 1‐8 h and 21‐24 h post‐dose); 8‐week double‐blind treatment | |
| Participants | Cilazapril 1 mg: n=42(26 males,16 females); mean age=53 years; baseline sitting BP not reported; Cilazapril 2.5 mg: n=42(28 males,14 females); mean age=52 years; baseline sitting BP not reported; Cilazapril 5 mg: n=42(27 males,15 females); mean age=48 years; baseline sitting BP not reported; Placebo: n=43(22 males,21 females); mean age=56 years; baseline sitting BP not reported | |
| Interventions | Cilazapril 1 mg once daily; Cilazapril 2.5 mg once daily; Cilazapril 5 mg once daily; Placebo; taken at approximately 12 noon before meal | |
| Outcomes | Mean change from baseline in trough sitting DBP using mercury sphygmomanometer | |
| Notes | SBP change not reported; DBP change and SE of change reported, endpoint DBP and SD not reported; calculated DBP SD of change from N and SE of change; BP data from text, p. 224; Jadad score=2; funding source= Roche Ltd. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Chan 1997.
| Methods | 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 95‐114 mm Hg at last 2 visits of run‐in; 12‐week double‐blind treatment | |
| Participants | Lisinopril 10 mg: n=26(18 males,8 females); mean age=70.5 years; baseline sitting SBP=163.8(13.0) mm Hg, DBP=104.9(5.0) mm Hg, HR=62.5 bpm; Placebo: n=27(15 males,12 females); mean age=73.4 years; baseline sitting SBP=167.9(14.8) mm Hg, DBP=105.5(5.4) mm Hg, HR=61.9 bpm | |
| Interventions | Lisinopril 10 mg once daily; Placebo; taken between 8 AM and 10 AM | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SD of change reported, endpoint BP and SD reported; SD of change values are too low; imputed endpoint SBP SD for SBP SD of change; imputed overall trial mean DBP SD of change; SBP data from Table 2, p. 745; DBP data from Table 3, p. 746; Jadad score=3; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Chrysant 1993.
| Methods | 4‐week single‐blind placebo run‐in; inclusion criteria= supine DBP 95‐114 mm Hg after run‐in; 16‐week double‐blind treatment, forced‐titration of dose by 4 mg every 4 weeks to maximum 16 mg daily | |
| Participants | Perindopril 4‐16 mg once daily: n=117(65 males,52 females); mean age=55(10) years; baseline upright SBP=154(15) mm Hg, DBP=102(7) mm Hg; baseline supine SBP=157(16) mm Hg, DBP=100(5) mm Hg; Perindopril 2‐8 mg twice daily: n=113(73 males,40 females); mean age=53(12) years; baseline upright SBP=150(15) mm Hg, DBP=101(6) mm Hg; baseline supine SBP=152(15) mm Hg, DBP=100(4) mm Hg; Placebo: n=59(45 males,15 females); mean age=51(12) years; baseline upright SBP=161(14) mm Hg, DBP=103(8) mm Hg; baseline supine SBP=153(10) mm Hg, DBP=101(5) mm Hg | |
| Interventions | Perindopril 4 mg once daily (wk 0‐4), perindopril 8 mg once daily (wk 4‐8), Perindopril 12 mg once daily (wk 8‐12), perindopril 16 mg once daily (wk 12‐16); Perindopril 2 mg twice daily (wk 0‐4), perindopril 4 mg twice daily (wk 4‐8), perindopril 6 mg twice daily (wk 8‐12), perindopril 8 mg twice daily (wk 12‐16); Placebo | |
| Outcomes | Once daily dosing: upright and supine SBP/DBP 24 ± 2 h after last dose; Twice daily dosing: upright and supine SBP/DBP 12 ± 2 h after last dose; WDAE | |
| Notes | Used week 4 supine data only; BP change reported, SD of change not reported, endpoint BP and SD reported; imputed endpoint SD for SD of change; BP data from Figure 1, p. 481; BP measurement device not reported; Jadad score=3; funding source= RW Johnson Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Chrysant 1994.
| Methods | 4‐week single‐blind placebo period; inclusion criteria= sitting DBP 100‐114 mm Hg after placebo period; 8‐week double‐blind treatment | |
| Participants | Lisinopril 10 mg: n=85; mean age=54 years; baseline sitting SBP=154 mm Hg, DBP=104 mm Hg, HR=77 bpm; baseline upright SBP=154 mm Hg, DBP=103 mm Hg, HR=78 bpm; Placebo: n=81; mean age=53 years; baseline sitting SBP=155 mm Hg, DBP=103 mm Hg, HR=77 bpm; baseline upright SBP=154 mm Hg, DBP=104 mm Hg, HR=79 bpm | |
| Interventions | Lisinopril 10 mg once daily; Placebo | |
| Outcomes | Trough sitting SBP/DBP using mercury sphygmomanometer; Trough upright SBP/DBP using mercury sphygmomanometer | |
| Notes | BP change and SD of change not reported, endpoint BP reported and SEM reported; calculated endpoint SD from N and endpoint SEM; imputed endpoint SD for SD of change; BP data from Figure 1, p. 739; Jadad score=2; funding source= ICI Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Chrysant 1996.
| Methods | 1‐week washout; 1‐ to 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 95‐114 mm Hg at 2 consecutive visits during run‐in, with a difference of 10 mm Hg or less between 2 visits; 6‐week double‐blind treatment | |
| Participants | Benazepril 20 mg: n=42(28 males,14 females); mean age=53.7 years; baseline sitting SBP=153 mm Hg, DBP=104 mm Hg; Placebo: n=40(22 males,18 females); mean age=53.5 years; baseline sitting SBP=153 mm Hg, DBP=103 mm Hg | |
| Interventions | Benazepril 20 mg once daily; Placebo | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer; Mean change from baseline in peak sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change reported and SE of change reported, endpoint BP reported; endpoint SD not reported, SD of change calculated from N and SE of change; BP data from Fagan abstract; SD of change data from Figure 1, p. 8; Jadad score=4; funding source= Ciba Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Cushman 1998.
| Methods | 7‐day washout; 4‐week single‐blind placebo baseline; inclusion criteria= mean sitting DBP 95‐115 mm Hg of week 2 and week 4 baseline recordings with difference in these means </= 7 mm Hg, mean sitting SBP had to be < 210 mm Hg at each baseline visit; 12‐week double‐blind treatment | |
| Participants | Enalapril 5 mg: n=144(94 males,50 females); mean age=56.1(10.0) years; baseline sitting SBP=155.2 mm Hg, DBP=101.6(5.5) mm Hg; Placebo: n=150(104 males,46 females); mean age=55.8(11.4) years; baseline sitting SBP=155.4 mm Hg, DBP=101.6(5.6) mm Hg | |
| Interventions | Enalapril 5 mg once daily; Placebo; administered between 6:30 AM and 10:00 AM | |
| Outcomes | Trough sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SD of change not reported; endpoint BP reported; endpoint SD not reported; imputed overall trial mean SD of change for SBP and DBP; BP data from Table 2, p. 26; Jadad score=4; funding source= Merck | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
De Bruijn 1994.
| Methods | 4‐week placebo run‐in; inclusion criteria= supine and standing DBP 95‐115 mm Hg after run‐in; 4‐week double‐blind treatment | |
| Participants | Trandolapril 0.5 mg: n=41(17 males,24 females); mean age=49(13) years; baseline SBP=163.8(12.8) mm Hg, DBP=99.5(5.8) mm Hg; Trandolapril 1 mg: n=42(8 males,38 females); mean age=48(13) years; baseline SBP=159.9(14.3) mm Hg, DBP=99.9(5.2) mm Hg; Trandolapril 2 mg: n=43(23 males,20 females); mean age=46(13) years; baseline SBP=161.1(13.1) mm Hg, DBP=99.8(5.9) mm Hg; Placebo: n=44(18 males,26 females); mean age=50(7) years; baseline SBP=157.3(16.6) mm Hg, DBP=99.2(6.0) mm Hg | |
| Interventions | Trandolapril 0.5 mg once daily; Trandolapril 1 mg once daily; Trandolapril 2 mg once daily; Placebo; administered in the morning | |
| Outcomes | Trough supine SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SD of change reported, endpoint BP and SD not reported; BP data from Figures 1 and 2, pp. S61‐S62; Jadad score=3; funding source= Roussel Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
DeQuattro 1997.
| Methods | 4‐week placebo run‐in; inclusion criteria= sitting DBP 95‐114 mm Hg during final 2 wks of run‐in; 6‐week double‐blind treatment | |
| Participants | Trandolapril 0.5 mg: n=41; baseline SBP=155.4(15.7) mm Hg, DBP=100.3(4.4) mm Hg; Trandolapril 2 mg: n=67; baseline SBP=151.4(16.5) mm Hg, DBP=99.8(4.6) mm Hg; Trandolapril 8 mg: n=43; baseline SBP=150.7(16.3) mm Hg, DBP=99.5(4.2) mm Hg; Placebo: n=53; baseline SBP=154.8(15.1) mm Hg, DBP=100.3(4.6) mm Hg; All patients (trandolapril monotherapy, verapamil monotherapy + verapamil/trandolapril combination treatment arms): n=726(456 males,270 females); mean age=54.7(10.9) years; baseline sitting SBP=151.8(16.2) mm Hg, DBP=100.4(6.1) mm Hg | |
| Interventions | Trandolapril 0.5 mg once daily; Trandolapril 2 mg once daily; Trandolapril 8 mg once daily; Placebo; administered in the morning (8 AM ± 1 h) | |
| Outcomes | Mean change from baseline in trough supine SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | Supine baseline BP reported in duplicate publication for each treatment arm; BP change reported, SD of change not reported, endpoint BP and SD not reported; imputed baseline SBP SD for SBP SD of change; imputed overall trial mean DBP SD of change; data from Table II, p. 367; duplicate publications=Levine 97, DeQuattro 97(NEJM); Jadad score=3; funding source= Knoll Pharma Change in sitting SBP data is not the same as data reported in Levine 1997. Reviewers have decided to use data from DeQuattro 1997 (primary reference) because unadjusted endpoint data is provided. At this time, DBP data that is only available in Levine 1997 will not be used unless an explanation for the discrepancy in BP data is adequately explained by authors. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Drayer 1983.
| Methods | 4‐ to 6‐week placebo run‐in; inclusion criteria= supine DBP 95‐115 mm Hg on 2 consecutive visits after beginning of placebo run‐in; 8‐week double‐blind treatment | |
| Participants | Captopril 25 mg twice daily: n=77(60 males,17 females); mean age=52 years; baseline supine SBP=156 mm Hg, DBP=101 mm Hg; Captopril 50 mg twice daily: n=71(50 males,21 females); mean age=52 years; baseline supine SBP=154 mm Hg, DBP=101 mm Hg; Captopril 100 mg twice daily: n=69(44 males,25 females); mean age=55 years; baseline supine SBP=158 mm Hg, DBP=102 mm Hg; Placebo: n=77(53 males,24 females); mean age=53 years; baseline supine SBP=157 mm Hg, DBP=102 mm Hg | |
| Interventions | Captopril 25 mg twice daily; Captopril 50 mg twice daily; Captopril 100 mg twice daily; Placebo | |
| Outcomes | Percent change from baseline in trough supine SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change reported, SD of change not reported, endpoint BP and SD not reported; baseline SD not reported; imputed overall trial mean SD of change for SBP and DBP; percent change in SBP data from text, p. III‐110; percent change in DBP data from Figure 1, p. III‐110; percent change in BP has been converted to absolute BP change data; Jadad score=3; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Dupui 1993.
| Methods | Inclusion criteria= SBP 160‐210 mm Hg and DBP 95‐115 mm Hg based on 3 separate measurements over a period of several days; approximately 8‐week (60 days) double‐blind treatment | |
| Participants | All patients: n=13(4 males,9 females); Captopril 75 mg daily: n=8(3 males,5 females); mean age=63(9) years; baseline upright SBP=155.3(7.9) mm Hg, DBP=94.4(10.9) mm Hg; baseline lying SBP=164.3(10.4) mm Hg, DBP=96.5(10.7) mm Hg; baseline HR=64.5(10.7) bpm; Placebo: n=5(1 male,4 females); mean age=63(4) years; baseline upright SBP=157.1(10.6) mm Hg, DBP=103.0(16.2) mm Hg; baseline lying SBP=168.1(7.0) mm Hg, DBP=100.4(11.1) mm Hg; baseline HR=66.2(4.9) bpm | |
| Interventions | Captopril 75 mg daily (50 mg in the morning, 25 mg at bedtime); Placebo | |
| Outcomes | Upright SBP/DBP using Dynamap automated oscillometric device; WDAE | |
| Notes | BP change and SD of change not reported; endpoint BP and SD reported; imputed endpoint SD for SD of change; BP data from Table III, p. 150; lying BP data also available; Jadad score=3; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Fairhurst 1994.
| Methods | 3‐ to 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 100‐115 mm Hg, as determined by mean of 3 consecutive BP measurements using either mercury or random‐zero sphygmomanometer; 6‐week double‐blind treatment | |
| Participants | All patients: n=283(157 males,126 females); mean age=55 years; Spirapril 3 mg: n=55; Spirapril 6 mg: n=61; Spirapril 12 mg: n=58; Spirapril 24 mg: n=49; Placebo: n=60 | |
| Interventions | Spirapril 3 mg once daily; Spirapril 6 mg once daily; Spirapril 12 mg once daily; Spirapril 24 mg once daily; Placebo; administered in the morning before breakfast | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change reported, SD of change not reported; endpoint BP and SD of change not reported; imputed overall trial mean SBP/DBP SD of change; BP data from Figure 1, p. 78; baseline BP for all patients is not reported; Jadad score=3; funding source= Sandoz Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Fernandez 1990.
| Methods | 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 94‐114 mm Hg on 2 consecutive visits (one week apart) of run‐in; 4‐week double‐blind treatment | |
| Participants | Cilazapril 1.25 mg: n=6(5 males,1 female); age=41(5) years; baseline sitting SBP=133(7) mm Hg, DBP=97(3) mm Hg, HR=77(5) bpm; Cilazapril 2.5 mg: n=6(5 males,1 female); age=44(13) years; baseline sitting SBP=146(17) mm Hg, DBP=100(10) mm Hg, HR=77(13) bpm; Cilazapril 5 mg: n=6(4 males,2 females); age=42(9) years; baseline sitting SBP=144(8) mm Hg, DBP=98(4) mm Hg, HR=72(8) bpm; Placebo: n=6(3 males,3 females); age=48(8) years; baseline sitting SBP=150(10) mm Hg, DBP=101(3) mm Hg, HR=65(9) bpm | |
| Interventions | Cilazapril 1.25 mg once daily; Cilazapril 2.5 mg once daily; Cilazapril 5 mg once daily; Placebo; taken at 8 AM | |
| Outcomes | Trough supine SBP/DBP using mercury sphygmomanometer; Trough erect SBP/DBP using mercury sphygmomanometer; Trough supine HR; Trough erect HR; WDAE | |
| Notes | Only cilazapril 2.5 mg and placebo groups have BP >/= 140/90 mm Hg after placebo run‐in; used supine BP for cilazapril 2.5 mg and placebo groups only; BP change reported and SD of change not reported, endpoint BP and SD reported; imputed endpoint SD for SD of change; data from Table 4, p. 55; Jadad score=3; funding source= Hoffman‐La Roche | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Fernandez 1994.
| Methods | 4‐ to 5‐week single‐blind placebo run‐in; inclusion criteria= mean sitting DBP 95‐110 mm Hg at 2 consecutive visits 1 week apart; 8‐week double‐blind treatment | |
| Participants | Fosinopril 20 mg: n=16(7 males,9 females); mean age=48.8(11.6) years; baseline sitting SBP=149.7(12.0) mm Hg, DBP=101.9(4.4) mm Hg, HR=72.9 bpm; Placebo: n=17(2 males,15 females); mean age=53.2(7.0) years; baseline sitting SBP=146.6(9.9) mm Hg, DBP=100.3(3.7) mm Hg, HR=73.4 bpm | |
| Interventions | Fosinopril 20 mg once daily; Placebo | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SD of change reported; endpoint BP and SD not reported; BP data from Table 2, p. I‐209; Jadad score=3; funding source= Bristol‐Myers Squibb | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Ford 1993.
| Methods | 4‐week single‐blind placebo run‐in; inclusion criteria= mean supine DBP 95‐115 mm Hg at 2 separate visits following discontinuation or tapering of antihypertensive medication (all patients had received antihypertensive therapy that was discontinued during the first 2 weeks of placebo run‐in); 4‐week double‐blind treatment; 1‐week single‐blind placebo washout period | |
| Participants | Fosinopril 10 mg: n=17(4 males,13 females); mean age=49(9.1) years; baseline supine SBP=163.8 mm Hg, DBP=102.2 mm Hg; baseline HR=77.4 bpm; Fosinopril 20 mg: n=15(6 males,9 females); mean age=55(8.1) years; baseline supine SBP=161.2 mm Hg, DBP=100.2 mm Hg; baseline HR=73.9 bpm; Fosinopril 40 mg: n=16(9 males,7 females); mean age=51(9.6) years; baseline supine SBP=164.4 mm Hg, DBP=101.8 mm Hg; baseline HR=77.8 bpm; Placebo: n=16(0 males,16 females); mean age=56(14) years; baseline supine SBP=154.7 mm Hg, DBP=99.8 mm Hg; baseline HR=74.2 bpm | |
| Interventions | Fosinopril 10 mg once daily, Fosinopril 20 mg once daily, Fosinopril 40 mg once daily, Placebo; administered in morning | |
| Outcomes | Trough supine SBP/DBP using mercury sphygmomanometer; Trough HR; WDAE | |
| Notes | BP change and SD of change not reported, endpoint BP reported, endpoint SD not reported; imputed overall trial mean SBP and DBP SD of change; BP data from Table II, p. 327; trough and peak BP data also available in Figures 1 and 2, p.327; 2 sets of baseline BP are reported; Jadad score=3; funding source= Bristol‐Myers Squibb | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Gerritsen 1998.
| Methods | 3‐week washout period; 4‐week placebo run‐in; inclusion criteria= sitting DBP 90‐115 mm Hg and SBP </= 200 mm Hg during run‐in; 8‐week double‐blind treatment, dosage of enalapril doubled after 4 weeks of treatment if DBP >/= 85 mm Hg | |
| Participants | Enalapril 10 mg: n=40(28 males,12 females); mean age=58.8(9.5) years; baseline SBP=165(15) mm Hg, DBP=92(7.8) mm Hg, HR=81.2(13.3) bpm; Placebo: n=41(26 males,15 females); mean age=61.9(7.8) years; baseline SBP=166(18) mm Hg, DBP=93(8.2) mm Hg, HR=81.2(14.3) bpm | |
| Interventions | Enalapril 10 mg once daily; Placebo; administered in the morning | |
| Outcomes | Trough sitting SBP/DBP using automated device (Dinamap); WDAE | |
| Notes | Used week 4 BP data only; BP change and SD of change not reported; endpoint BP and SD reported; imputed endpoint SD for SD of change; position of BP measurement not reported but likely sitting; BP data from Figure 1, p. 693; Jadad score=4; funding source= Bayer | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Gomez 1989.
| Methods | 4‐week single‐blind placebo washout; inclusion criteria= supine DBP 95‐115 mm Hg after washout; 6‐week double‐blind treatment | |
| Participants | Lisinopril 1.25 mg: n=41(38 males,3 females); mean age=58 years; baseline BP not reported for all randomized patients; Lisinopril 5 mg: n=41(37 males,4 females); mean age=56 years; baseline BP not reported for all randomized patients; Lisinopril 20 mg: n=44(42 males,2 females); mean age=54 years; baseline BP not reported for all randomized patients; Lisinopril 80 mg: n=43(37 males,6 females); mean age=57 years; baseline BP not reported for all randomized patients; Placebo: n=47(40 males,7 females); mean age=56 years; baseline BP not reported for all randomized patients | |
| Interventions | Lisinopril 1.25 mg once daily; Lisinopril 5 mg once daily; Lisinopril 20 mg once daily Lisinopril 80 mg once daily (patients received 40 mg once daily for the first 2 weeks and then 80 mg once daily for the last 4 weeks); Placebo; administered at 9 AM | |
| Outcomes | Trough erect SBP/DBP using mercury sphygmomanometer; Trough supine SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and 95% CI reported, endpoint BP reported, endpoint SD not reported; calculated SD of change from 95% CI; erect BP data from Table 3, p. 418; supine BP data from Table 2, p. 417; Jadad score=3; funding source= Merck Sharp & Dohme | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Gradman 1995.
| Methods | 7‐day washout period; total 4‐week single‐blind placebo run‐in, patients' supine DBP >/= 95 mm Hg after initial 2‐week single‐blind placebo phase; additional 2‐week single‐blind placebo phase; inclusion criteria= mean supine DBP 100‐115 mm Hg, and two BP readings during weeks 2 and 4 of single‐blind placebo phase could not differ by > 7 mm Hg; 8‐week double‐blind treatment | |
| Participants | Enalapril 20 mg: n=83(56 males,27 females); median age=53 years; baseline SBP=155.4 mm Hg, DBP=103.1 mm Hg; Placebo: n=78(47 males,31 females); median age=53 years; baseline SBP=157.9 mm Hg, DBP=103.3 mm Hg | |
| Interventions | Enalapril 20 mg once daily; Placebo | |
| Outcomes | Mean change from baseline in trough supine SBP/DBP; Mean change from baseline in peak supine SBP/DBP; WDAE | |
| Notes | BP change and SD of change reported, endpoint BP reported; endpoint SD not reported, BP data from Table 2, p. 1348; BP measurement device not reported; Jadad score=3; funding source= Merck | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Gradman 1997.
| Methods | 4‐week single‐blind placebo baseline; inclusion criteria= sitting DBP 95‐115 mm Hg; 8‐week double‐blind treatment | |
| Participants | All patients: n=707(457 males,250 females); mean age=53.5(10.5) years; baseline sitting SBP=155.5(17.7) mm Hg, DBP=101.9(5.7) mm Hg; Enalapril 5 mg: n=85; Enalapril 20 mg: n=48; Placebo: n=79 | |
| Interventions | Enalapril 5 mg once daily; Enalapril 20 mg once daily; Placebo; administered in the morning | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change reported; SD of change not reported; endpoint BP and SD not reported; baseline SBP SD for all groups reported; imputed baseline SBP SD for SD of change; imputed systematic review overall mean SD of change for DBP; DBP data from Figure 1, p. 432; SBP data from Figure 2, p. 433; Jadad score=3; funding source= Astra Merck, Inc. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Guitard 1994.
| Methods | 3‐ to 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 100‐119 mm Hg; 6‐week double‐blind treatment | |
| Participants | Spirapril 6 mg: n=66(32 males,34 females); mean age=58(11) years; baseline sitting SBP=171(12) mm Hg, DBP=106(4) mm Hg, HR=76(10) bpm; Spirapril 12 mg: n=64(23 males,41 females); mean age=58(9) years; baseline sitting SBP=168(14) mm Hg, DBP=105(4) mm Hg, HR=73(9) bpm; Spirapril 24 mg: n=66(35 males,31 females); mean age=58(11) years; baseline sitting SBP=170(12) mm Hg, DBP=106(4) mm Hg, HR=74(9) bpm; Placebo: n=64(24 males, 40 females); mean age=57(11) years; baseline sitting SBP=167(11) mm Hg, DBP=105(3) mm Hg, HR=73(9) bpm | |
| Interventions | Spirapril 6 mg once daily; Spirapril 12 mg once daily; Spirapril 24 mg once daily; Placebo; administered in the morning before breakfast | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change reported, SD of change reported but values are too low, endpoint SBP not reported, endpoint DBP reported, endpoint SD not reported; change in trough BP data from Table II, p. 83; SD of change data from Figure 2, p. 85; change in peak DBP data in subgroup of patients (from one study center) in Figure 3, p. 85; Table II provides data for both efficacy and intention‐to‐treat (ITT) analysis, ITT analysis BP data used instead of efficacy analysis BP data; imputed baseline SBP SD for SBP SD of change; imputed overall trial mean DBP SD of change; Jadad score=3; funding source= Sandoz Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Guitard 1997.
| Methods | 4‐week placebo washout; inclusion criteria= mean DBP >/= 100 mm Hg at end of washout period and mean DBP 100‐115 mm Hg 24 hours after capsule intake during placebo phase; 8‐week double‐blind treatment, titrated to response at 4 weeks | |
| Participants | Enalapril 5 mg: n=101(54 males,47 females); mean age=56.2(9.7) years; baseline SBP=163.2(16.4) mm Hg, DBP=99.5(6.1) mm Hg; Spirapril 6 mg: n=101(50 males,50 females); mean age=58.0(7.9) years; baseline SBP=161.8(16.3) mm Hg, DBP=99.7(6.6) mm Hg; Placebo: n=50(32 males,18 females); mean age=56.5(8.2) years; baseline SBP=161.3(18.2) mm Hg, DBP=98.2(6.9) mm Hg | |
| Interventions | Enalapril 5 mg once daily; Spirapril 6 mg once daily; Placebo | |
| Outcomes | Adjusted mean change from baseline in trough sitting DBP; Adjusted mean change from baseline in peak sitting DBP | |
| Notes | Used week 4 BP data only; BP change reported, SD of change not reported, endpoint BP reported, endpoint SD not reported; imputed overall trial mean DBP SD of change; DBP data from Table 5, p. 455; BP measurement device not reported; Jadad score=2; funding source= Novartis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Guntzel 1991.
| Methods | 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 100‐115 mm Hg at end of 3rd and 4th week of run‐in as well as during baseline BP profile (BP measured hourly during first 10 hours and last 4 hours after last placebo capsule); 8‐week double‐blind treatment | |
| Participants | Cilazapril 2.5 mg: n=29(17 males,12 females); mean age=56(7) years; baseline DBP=103.5 mm Hg; Cilazapril 5 mg: n=29(22 males,7 females); mean age=49(8) years; baseline DBP=103.1 mm Hg; Placebo: n=27(17 males,10 females); mean age=52(9) years; baseline DBP=104.3 mm Hg | |
| Interventions | Cilazapril 2.5 mg once daily; Cilazapril 5 mg once daily; Placebo; taken at 10 AM | |
| Outcomes | Trough sitting SBP/DBP using mercury sphygmomanometer; Trough HR; WDAE | |
| Notes | Endpoint (week 8) BP change and DBP SE of change reported, endpoint BP and SD reported; BP also reported at weeks 4,6,8; calculated DBP SD of change from N and SE of change; imputed overall trial mean SBP SD of change; BP data from Figure 1, p. 10; Jadad score=3; funding source= Hoffman‐La Roche Ltd. Duplication publication = Study 2 of Kobrin 1991. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Holwerda 1996.
| Methods | 1‐week washout; 2‐week placebo run‐in; inclusion criteria= sitting DBP 95‐115 mm Hg after run‐in; 8‐week double‐blind treatment | |
| Participants | Enalapril 20 mg: n=69(40 males,29 females); mean age=52.5(10.3) years; baseline sitting SBP=161.5(10.4) mm Hg, DBP=102.2(4.2) mm Hg; Valsartan 80 mg: n=137(65 males,72 females); mean age=53.1(12.4) years; baseline sitting SBP=161.7(11.6) mm Hg, DBP=101.2(4.5) mm Hg; Placebo: n=142(76 males,66 females); mean age=53.1(12.9) years; baseline sitting SBP=161.0(11.5) mm Hg, DBP=101.8(4.4) mm Hg | |
| Interventions | Enalapril 20 mg once daily; Valsartan 80 mg once daily; Placebo; taken in the morning | |
| Outcomes | Trough sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SD of change not reported, endpoint BP and SD reported; imputed endpoint SD for SD of change; BP data from Table 3, p. 1150; Jadad score=3; funding source= Ciba‐Geigy | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Homuth 1993.
| Methods | 2‐week placebo run‐in; inclusion criteria= DBP 100‐115 mm Hg after run‐in; 6‐week double‐blind treatment | |
| Participants | Ramipril 2.5 mg: n=40(26 males,14 females); mean age=47(10) years; baseline SBP=159(15) mm Hg, DBP=107(5) mm Hg; Ramipril 5 mg: n=40(23 males,17 females); mean age=48(8) years; baseline SBP=159(13) mm Hg, DBP=107(6) mm Hg; Ramipril 10 mg: n=40(24 males,16 females); mean age=47(9) years; baseline SBP=160(14) mm Hg, DBP=109(5) mm Hg; Placebo: n=40(22 males,18 females); mean age=46(10) years; baseline SBP=161(17) mm Hg, DBP=109(5) mm Hg | |
| Interventions | Ramipril 2.5 mg once daily; Ramipril 5 mg once daily; Ramipril 10 mg once daily; Placebo; administered in the morning | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change reported, SD of change not reported, endpoint BP and SD not reported; imputed baseline SBP SD for SBP SD of change; imputed overall trial mean DBP SD of change; BP data from Figures 1 and 2, p. 669; Jadad score=3; funding source= Cassella AG | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Kayanakis 1987.
| Methods | 2‐week placebo run‐in; inclusion criteria= SBP 160‐200 mm Hg and DBP 95‐120 mm Hg at 2 consecutive measurements; 8‐week double‐blind treatment | |
| Participants | Captopril 50 mg: n=42(23 males,19 females); mean age=52.8(10.6) years; baseline supine SBP=175.5(8.9) mm Hg, DBP=104.5(4.4) mm Hg; Placebo: n=83(47 males,36 females); mean age=52.8(9.0) years; baseline supine SBP=172.0(7.7) mm Hg, DBP=102.5(3.8) mm Hg | |
| Interventions | Captopril 50 mg once daily; Placebo | |
| Outcomes | Trough supine SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SD of change not reported, endpoint BP and SD reported; imputed endpoint SD for SD of change for SBP and DBP; SBP data from Figure 1, p. 91S; DBP data from Figure 2, p. 91S; Jadad score=3; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Kobrin 1991.
| Methods | 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 100‐115 mm Hg at last 2 visits of run‐in; 4‐week double‐blind treatment | |
| Participants | Cilazapril 2.5 mg: n=29(18 males,11 females); mean age=50(9) years; Cilazapril 5 mg: n=29(16 males,13 females); mean age=48(9) years; Placebo: n=28(13 males,15 females); mean age=52(8) years | |
| Interventions | Cilazapril 2.5 mg once daily; Cilazapril 5 mg once daily; Placebo | |
| Outcomes | Mean change from baseline in trough sitting DBP using mercury sphygmomanometer; WDAE | |
| Notes | SBP change not reported; DBP change and SE of change reported, endpoint BP and SD not reported; calculated DBP SD of change from N and SE of change; BP data from Table II, p. 34; Jadad score=3; funding source= Hoffman‐La Roche Ltd. Kobrin 1991 reports results for 2 independent RCTs. Study 2 is same RCT as reported in Guntzel 1991. Data for Study 1 is entered as Kobrin 1991. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Koch 1999.
| Methods | 1‐week washout; 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 95‐114 mm Hg at end of placebo run‐in; 12‐week double‐blind treatment | |
| Participants | 95 postmenopausal women taking HRT regimens that were held constant throughout experimental period; Moexipril 15 mg: n=47; mean age=56.1(8.0) years; baseline sitting SBP=154.6(11.8) mm Hg, DBP=99.5(3.8) mm Hg, HR=72.7(7.7) bpm; Placebo: n=48; mean age=57.0(6.8) years; baseline sitting SBP=158.5(13.6) mm Hg, DBP=100.0(3.7) mm Hg, HR=72.4(6.3) bpm | |
| Interventions | Moexipril 15 mg once daily; Placebo | |
| Outcomes | Adjusted mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer | |
| Notes | BP change reported, SD of change not reported, endpoint BP and SD not reported; baseline SD reported; imputed baseline SBP SD for SBP SD of change; imputed overall trial mean SD of change for DBP; change in BP data from text and Figure 1, p. 339; Jadad score=3; funding source= Schwarz Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Kohlmann Jr 1999.
| Methods | 2‐week placebo run‐in; inclusion criteria= DBP 95‐115 mm Hg after run‐in; 8‐week double‐blind treatment | |
| Participants | Trandolapril 2 mg: n=135(55 males,80 females); mean age=53.1(11.3) years; baseline SBP=157.3(15) mm Hg, DBP=101.0(6.3) mm Hg, HR=75.6(9.1) bpm; Placebo: n=135(55 males,80 females); mean age=53.1(11.3) years; baseline SBP=156.1(18) mm Hg, DBP=100.3(6.6) mm Hg, HR=75.6(9.1) bpm | |
| Interventions | Trandolapril 2 mg once daily; Placebo | |
| Outcomes | SBP/DBP | |
| Notes | BP change and SD of change not reported, endpoint BP and SD reported; imputed endpoint SD for SD of change; endpoint BP (week 8) data from text, p. 549; BP data for weeks 5 and 8 provided in Figures 1 and 2, p. 550; BP measurement device not reported; time of post‐dose BP measurement not reported; Jadad score=3; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Kostis 1991.
| Methods | 2‐to 4‐week single‐blind placebo washout; inclusion criteria= supine DBP 95‐114 mm Hg after washout; 12‐week double‐blind treatment | |
| Participants | Ramipril 1.25 mg: n=44(18 males,26 females); mean age=52.3 years; baseline SBP=159(15) mm Hg, DBP=99.9(3.7) mm Hg; Ramipril 2.5 mg: n=43(27 males,16 females); mean age=49.4 years; baseline supine DBP=99.8(3.7) mm Hg; Ramipril 5 mg: n=43(23 males,20 females); mean age=53.4 years; baseline supine DBP=100.7(5.1) mm Hg; Ramipril 10 mg: 44(29 males,15 females); mean age=52.1 years; baseline supine DBP=101.2(4.4) mm Hg; Placebo: n=42(22 males,20 females); mean age=51.3 years; baseline supine DBP=99.3(3.6) mm Hg | |
| Interventions | Ramipril 1.25 mg once daily; Ramipril 2.5 mg once daily; Ramipril 5 mg once daily; Ramipril 10 mg once daily; Placebo; administered in the morning | |
| Outcomes | Mean change from baseline in trough standing SBP/DBP using mercury sphygmomanometer; Mean change from baseline in trough supine SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SD of change reported, endpoint BP and SD not reported; BP data from Table 3, p. 13, SD data from Figures II and III, p. 12; Jadad score=3; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Krum 1992.
| Methods | 3‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 95‐115 mm Hg after run‐in; 4‐week double‐blind treatment | |
| Participants | All patients: n=22; mean age=59(11) years; Cilazapril 2.5 mg: n=6; baseline sitting SBP=173(22) mm Hg, DBP=110(7.4) mm Hg; Placebo: n=5; baseline sitting SBP=159(27) mm Hg, DBP=101(13.4) mm Hg | |
| Interventions | Cilazapril 2.5 mg once daily; Placebo; taken at approximately 8 AM | |
| Outcomes | Trough sitting SBP/DBP using oscillometric device (Dinamap); Trough standing SBP/DBP using oscillometric device (Dinamap) | |
| Notes | BP change and SD of change not reported, endpoint BP and SE reported; calculated endpoint SD from N and SE; endpoint SD values are too low; imputed SBP SD of change from baseline SBP SD of change, imputed overall trial mean DBP SD of change; BP data from Table 2, p. 455; Jadad score=2; funding source= Roche Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Krum 1998.
| Methods | 4‐ to 6‐week placebo run‐in; inclusion criteria= mean sitting DBP 95‐115 mm Hg after run‐in, DBP could not differ by more than 7 mm Hg on 3 consecutive visits; 4‐week double‐blind treatment | |
| Participants | Enalapril 20 mg: n=50(33 males,17 females); mean age=59(10) years; baseline SBP=161.9(14.3) mm Hg, DBP=102.2(5.0) mm Hg, HR=76.2(8.4) bpm; Placebo: n=49(27 males,22 females); mean age=56(9) years; baseline SBP=158.3(14.1) mm Hg, DBP=101.7(4.5) mm Hg, HR=71.8(7.8) bpm | |
| Interventions | Enalapril 20 mg once daily; Placebo; administered in the morning | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer; Mean change from baseline in trough sitting HR; WDAE | |
| Notes | BP change and SD of change reported; endpoint BP and SD not reported; SBP/DBP data from Table 2, p. 788; Jadad score=3; funding source= Hoffman‐La Roche | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Kuppers 1997.
| Methods | 2‐week placebo run‐in; inclusion criteria= 1) sitting DBP=95‐114 mm Hg during last 2 weeks of run‐in, and also on day 0, the first day of active treatment, and 2) mean daytime (0600‐2159h) >/= 85mm Hg by ambulatory BP monitoring; consecutive measurements; 8‐week double‐blind treatment | |
| Participants | Enalapril 10 mg once daily: n=77(32 males,45 females); mean age=55.8(8.7) years; baseline sitting SBP=166.8(14.8) mm Hg, DBP=106.7(4.6) mm Hg; Placebo: n=77(33 males,44 females); mean age=57.2(9.5) years; baseline sitting SBP=166.4(14.1) mm Hg, DBP=106.9(4.7) mm Hg | |
| Interventions | Enalapril 10 mg once daily, Placebo; administered at approximately 8AM | |
| Outcomes | Trough sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SD of change not reported, endpoint BP and SD reported; imputed endpoint SD for SD of change; BP data from Figure 1, p. 95; Jadad score=4; funding source= Solvay Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Kuschnir 1996.
| Methods | 2‐to 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 100‐120 mm Hg after run‐in; 8‐week double‐blind treatment | |
| Participants | Benazepril 20 mg: n=77(32 males,45 females); mean age=55.8(8.7) years; baseline sitting SBP=166.8(14.8) mm Hg, DBP=106.7(4.6) mm Hg; Placebo: n=77(33 males,44 females); mean age=57.2(9.5) years; baseline sitting SBP=166.4(14.1) mm Hg, DBP=106.9(4.7) mm Hg | |
| Interventions | Benazepril 20 mg once daily; Placebo; administered at approximately 8 AM | |
| Outcomes | Trough sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SD of change not reported, endpoint BP reported, endpoint SD not reported, baseline SBP SD reported, imputed baseline SBP SD for SBP SD of change, imputed overall trial mean DBP SD of change; BP data from Table II, p. 1218; Jadad score=3; funding source= Ciba‐Geigy | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Lacourciere 1994.
| Methods | 2‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 95‐109 mm Hg after run‐in; 4‐week double‐blind treatment | |
| Participants | All patients: n=130; 102(79%) caucasian, 25(19%) black, 3(2%) oriental; Cilazapril 2.5 mg: n=44(22 males,22 females); mean age=52.5(9.0) years; baseline sitting SBP=153.6(16.4) mm Hg, DBP=102.0(4.7) mm Hg; Cilazapril 5 mg: n=42(31 males,11 females); mean age=50.4(9.1) years; baseline sitting SBP=154.8(15.1) mm Hg, DBP=101.0(4.3) mm Hg; Placebo: n=44(29 males,15 females); mean age=53.6(8.5) years; baseline sitting SBP=157.5(15.8) mm Hg, DBP=101.1(3.8) mm Hg | |
| Interventions | Cilazapril 2.5 mg once daily; Cilazapril 5 mg once daily; Placebo | |
| Outcomes | Trough sitting SBP/DBP using mercury sphygmomanometer; Peak sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SD of change not reported, endpoint BP reported, endpoint SD not reported; baseline SBP SD reported, imputed baseline SBP SD for SBP SD of change, imputed overall trial mean DBP SD of change; BP data from Table 3, p. 608; Jadad score=3; funding source= Hoffman‐La Roche Ltd. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Lerch 1999.
| Methods | 4‐week placebo run‐in; inclusion criteria= supine DBP 90‐115 mm Hg after run‐in; 6‐week double‐blind treatment | |
| Participants | Temocapril 20 mg: n=19(13 males,6 females); mean age=57.6(8.3) years; baseline SBP=162(22) mm Hg, DBP=98(9) mm Hg; Placebo: n=11(8 males,3 females); mean age=56.1(5.6) years; baseline SBP=151(13) mm Hg, DBP=97(7) mm Hg | |
| Interventions | Temocapril 20 mg once daily; Placebo; administered between 7 AM and 8 AM | |
| Outcomes | Trough supine SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SD of change not reported, endpoint BP and SE reported, calculated endpoint SD from N and endpoint SE, imputed endpoint SD for SD of change; BP data from Table 1, p. 529; Jadad score=3; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Levine 1995.
| Methods | 2‐week placebo run‐in period; inclusion criteria= supine DBP >/= 95 mm Hg after run‐in; 12‐week double‐blind treatment, forced titration (dose doubled) every 4 weeks starting at 10 mg | |
| Participants | Enalapril 10 mg: n=31(17 males,14 females); mean age=56 years; baseline SBP=152.5(13.4) mm Hg, DBP=102.5(5.0) mm Hg; Placebo: n=29(17 males,12 females); mean age=53 years; baseline SBP=149.8(14.5) mm Hg, DBP=100.2(4.3) mm Hg | |
| Interventions | Enalapril 10 mg once daily; Placebo; average dosing time 9 AM | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | Used week 4 BP data only; BP change and SE of change reported, endpoint BP and endpoint SE reported, calculated SD of change from N and SE of change; SBP data from Table 2, p. 496; DBP data from Table 3, p. 497; Jadad score=3; funding source= Lederle Laboratories | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Luccioni 1988.
| Methods | 2‐week placebo run‐in period; inclusion criteria= supine DBP >/= 95 mm Hg after run‐in; 4‐week double‐blind treatment | |
| Participants | All patients: n=40(31 males,9 females); mean age=56.6(9.5) years; baseline BP not reported for all patients | |
| Interventions | Perindopril 2 mg once daily; Perindopril 4 mg once daily; Perindopril 8 mg once daily; Placebo | |
| Outcomes | Supine SBP/DBP using mercury sphygmomanometer | |
| Notes | BP change and SD of change not reported, endpoint BP and endpoint SE reported, calculated endpoint SD from N and endpoint SE, imputed endpoint SD for SD of change; BP data from Figure 2, p. 1133; time of BP measurement not reported (but most likely measured during the first 8 h post‐dose since ambulatory measurements were taken during that period); Jadad score=2; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
MacLean 1989.
| Methods | 4‐week single‐blind placebo washout; inclusion criteria= sitting DBP >/= 95 mm Hg after washout; 12‐week double‐blind treatment, forced titration (dose doubled) every 4 weeks starting at 20 mg daily | |
| Participants | Quinapril once daily: n=91(64 males,27 females); median age=49 years; baseline SBP=163 mm Hg, DBP=107 mm Hg; Quinapril twice daily: n=90(61 males,29 females); median age=51 years; baseline SBP=164 mm Hg, DBP=106 mm Hg; Placebo: n=89(56 males,33 females); median age=52 years; baseline SBP=162 mm Hg, DBP=105 mm Hg | |
| Interventions | Quinapril 20, 40, 80 mg once daily (morning administration of active drug); Quinapril 20, 40, 80 mg twice daily (2 capsules taken 12 h apart); Placebo | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | Used week 4 BP data only; BP change and SE of change reported, endpoint BP and SD not reported, calculated SD of change from N and change SE; BP data from Table III, p. 375; Jadad score=3; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Mancia 1992.
| Methods | 4‐week placebo run‐in; inclusion criteria= supine and standing clinic DBP >/= 95 mm Hg after run‐in; 6‐week double‐blind treatment | |
| Participants | Trandolapril 2 mg: n=42(31 males,11 females); mean age=51.4(9.7) years; baseline supine SBP=159.8(12.8) mm Hg, DBP=102.4(5.1) mm Hg, HR=72.1(8.3) bpm; Placebo: n=20(15 males, 5 females); mean age=51.1(7.6) years; baseline supine SBP=158.0(13.5) mm Hg, DBP=102.3(4.8) mm Hg, HR=73.9(8.3) bpm | |
| Interventions | Trandolapril 2 mg once daily; Placebo; administered at approximately 9 AM | |
| Outcomes | Trough supine SBP/DBP using mercury sphygmomanometer; Trough supine HR; WDAE | |
| Notes | BP change and SD of change not reported, endpoint BP and SE reported, calculated endpoint SD from N and SE; imputed endpoint SD for SD of change; BP data from Table II, p. 62D; duplicate publication=Ravogli 94; Jadad score=3; funding source= Roussel Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Mancia 1997.
| Methods | 4‐week placebo run‐in; inclusion criteria= sitting DBP 100‐110 mm Hg at end of run‐in; 8‐week double‐blind treatment | |
| Participants | Trandolapril 1 mg: n=50; mean age=51(10) years; baseline sitting SBP=159.3(12.4) mm Hg, DBP=103.6(3.1) mm Hg, HR=73.2(10.6) bpm; Placebo: n=51; mean age=52(9) years; baseline sitting SBP=158.2(13.5) mm Hg, DBP=103.5(3.4) mm Hg, HR=75.4(8.2) bpm | |
| Interventions | Trandolapril 1 mg once daily; Placebo; administered at approximately 9 AM after breakfast | |
| Outcomes | Trough sitting SBP/DBP using mercury sphygmomanometer; Peak sitting SBP/DBP using mercury sphygmomanometer; Trough sitting HR; WDAE | |
| Notes | BP change and SD of change not reported; endpoint BP and SD reported; imputed endpoint SD for SD of change; trough BP data from Table 1, p. 493; peak BP data (using 24h ambulatory BP monitoring) in Figure 3, p. 496; Jadad score=3; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
McCarron 1991.
| Methods | 3‐ to 4‐week single‐blind placebo run‐in; inclusion criteria= supine DBP 100‐114 mm Hg; 4‐week double‐blind treatment | |
| Participants | Ramipril 10 mg: n=67(44 males,23 females); mean age=53.8(9.8) years; baseline supine SBP=152.7(11.4) mm Hg, DBP=102.9(3.0) mm Hg; Placebo: n=33(23 males,10 females); mean age=52.3(11.7) years; baseline supine SBP=151.9(13.2) mm Hg, DBP=102.1(3.0) mm Hg | |
| Interventions | Ramipril 10 mg once daily; Placebo; administered in the morning | |
| Outcomes | Mean change from baseline in trough standing SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SE of change reported, endpoint BP and SE reported, calculated SD of change from N and SE of change; BP data from Table III, p. 740; Jadad score=3; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
McFate‐Smith 1991.
| Methods | 2‐ to 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 95‐115 mm Hg after run‐in; 4‐week double‐blind treatment | |
| Participants | All patients: n=202; mean age=70 years; baseline sitting SBP=177 mm Hg, DBP=103 mm Hg; Benazepril 2 mg BID: n=50; Benazepril 10 mg BID: n=50; Placebo: n=50 | |
| Interventions | Benazepril 2 mg twice daily; Benazepril 10 mg twice daily; Placebo | |
| Outcomes | Mean change from baseline in sitting SBP/DBP; BP measured 10‐14 h post‐dose | |
| Notes | BP change reported; SD of change not reported, endpoint BP and SD not reported; imputed overall trial mean SD of change; BP data from Table 1, p. IV‐81; BP measurement device not reported; Jadad score=3; funding source= Ciba‐Geigy Inc. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Messerli 1998.
| Methods | 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 95‐114 mm Hg after run‐in; 6‐week double‐blind treatment | |
| Participants | Trandolapril 4 mg: n=159(106 males,53 females); mean age=54.3 years; baseline SBP=151.8(14.8) mm Hg, DBP=101.3(5.0) mm Hg; Placebo: n=152(103 males,49 females); mean age=53.8 years; baseline SBP=153.6(13.4) mm Hg, DBP=100.5(4.5) mm Hg | |
| Interventions | Trandolapril 4 mg once daily; Placebo; administered in the morning | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer | |
| Notes | BP change and SD of change reported, endpoint BP and SD not reported; SD of change values reported are low; imputed baseline SBP SD for SBP SD of change, imputed overall trial mean DBP SD of change; BP data from Table 2, p. 325; Jadad score=3; funding source= Knoll Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Moser 1991.
| Methods | 2‐ to 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 95‐114 mm Hg on 2 consecutive visits (weeks 2 and 4 of run‐in) with </= 10 mm Hg difference between 2 visits; 4‐week double‐blind treatment | |
| Participants | Benazepril 2 mg once daily: n=34(24 males,10 females); mean age=50.4 years; baseline sitting SBP=151.6(15.9) mm Hg, DBP=102.1(5.6) mm Hg; Benazepril 5 mg once daily: n=38(23 males,15 females); mean age=51.1 years; baseline sitting SBP=152.7(15.2) mm Hg, DBP=101.2(5.3) mm Hg; Benazepril 10 mg once daily: n=34(23 males,11 females); mean age=51.9 years; baseline sitting SBP=153.1(13.7) mm Hg, DBP=101.8(5.7) mm Hg; Benazepril 20 mg once daily: n=36(23 males,13 females); mean age=50.4 years; baseline sitting SBP=151.9(15.7) mm Hg, DBP=101.7(4.7) mm Hg; Placebo: n=31(21 males,10 females); mean age=48.2 years; baseline sitting SBP=150.7(14.3) mm Hg, DBP=101.7(4.9) mm Hg | |
| Interventions | Benazepril 2 mg once daily; Benazepril 5 mg once daily; Benazepril 10 mg once daily; Benazepril 20 mg once daily; Placebo | |
| Outcomes | Trough sitting DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SD of change not reported, endpoint BP and SE reported, calculated endpoint SD from N and endpoint SE, imputed endpoint SD for SD of change; DBP data from Table III, p. 325; Jadad score=3; funding source= Ciba‐Geigy | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Mroczek 1991.
| Methods | 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 95‐114 mm Hg at each of last 2 visits during run‐in; 4‐week double‐blind treatment | |
| Participants | Cilazapril 2.5 mg: n=59(45 males,14 females); mean age=52.4 years; baseline sitting SBP=146.3 mm Hg, DBP=101.1 mm Hg, HR=75.5 bpm; Cilazapril 5 mg: n=59(41 males,18 females); mean age=52.9 years; baseline sitting SBP=148.4 mm Hg, DBP=101.3 mm Hg, HR=76.2 bpm; Cilazapril 10 mg: n=58(34 males,24 females); mean age=50.3 years; baseline sitting SBP=144.3 mm Hg, DBP=100.8 mm Hg, HR=75.1 bpm; Placebo: n=59(36 males,23 females); mean age=54.0 years; baseline sitting SBP=149.8 mm Hg, DBP=100.7 mm Hg, HR=77.3 bpm | |
| Interventions | Cilazapril 2.5 mg once daily; Cilazapril 5 mg once daily; Cilazapril 10 mg once daily; Placebo; taken in the morning after light breakfast | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer; Mean change from baseline in trough sitting HR; WDAE | |
| Notes | BP change and SE of change reported, endpoint BP and SE reported; calculated SD of change from N and SE of change; BP data from text and Table 2, p. 1424; Jadad score=3; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Mroczek 1996.
| Methods | 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 95‐114 mm Hg at last 2 consecutive visits of placebo run‐in, with difference between visits of 10 mm Hg or less; 12‐week double‐blind treatment | |
| Participants | Moexipril 7.5 mg: n=51(31 males,20 females); mean age=54.9 years; baseline sitting SBP=152.2 mm Hg, DBP=101.8 mm Hg, HR=75.8 bpm; baseline standing SBP=148.4 mm Hg, DBP=100.9 mm Hg; Moexipril 15 mg: n=47(30 males,17 females); mean age=56.0 years; baseline sitting SBP=154.0 mm Hg, DBP=100.9 mm Hg, HR=73.6 bpm; baseline standing SBP=150.4 mm Hg, DBP=100.2 mm Hg; Placebo: n=51(37 males,14 females); mean age=55.3 years; baseline sitting SBP=154.2 mm Hg, DBP=101.2 mm Hg, HR=74.7 bpm; baseline standing SBP=150.9 mm Hg, DBP=101.1 mm Hg | |
| Interventions | Moexipril 7.5 mg once daily; Moexipril 15 mg once daily; Placebo | |
| Outcomes | Adjusted mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer; Trough sitting DBP using mercury sphygmomanometer; Trough standing SBP/DBP using mercury sphygmomanometer | |
| Notes | BP change and SD of change reported; endpoint SBP not reported, endpoint DBP reported, endpoint SD not reported; change in SBP data from Table 3, p. 85; change in DBP data from Table 2, p. 83; Jadad score=3; funding source= Schwarz Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Muiesan 1987.
| Methods | 3‐week placebo run‐in; inclusion criteria= supine DBP 100‐110 mm Hg during run‐in; 4‐week double‐blind treatment | |
| Participants | All patients: n=152(77 males,75 females); mean age=69(4) years; Captopril 25 mg: n=52; baseline standing SBP=173(13) mm Hg, DBP=106(5) mm Hg; baseline supine SBP=176(14) mm Hg, DBP=105(5) mm Hg; Placebo: n=50; baseline standing SBP=172(14) mm Hg, DBP=106(5) mm Hg; baseline supine SBP=176(14) mm Hg, DBP=104(5) mm Hg; | |
| Interventions | Captopril 25 mg twice daily; Placebo | |
| Outcomes | Standing SBP/DBP using mercury sphygmomanometer; Supine SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SD of change not reported, endpoint BP and SD reported; imputed endpoint SD for SD of change in captopril group; imputed baseline SBP SD for SBP SD of change in placebo group; in placebo group, imputed systematic review overall mean SD of change for DBP; BP data from text and Figure 1, p. S600; baseline supine SBP/DBP and SD for placebo group from Table 1, p. S601; supine BP data also available; Jadad score=3; funding source= Squibb Italia SpA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Myers 1996.
| Methods | 4‐week single‐blind placebo run‐in; inclusion criteria= supine DBP 95‐114 mm Hg after run‐in; 12‐week double‐blind treatment; 293 patients included in safety analysis; 260 patients included in efficacy analyses | |
| Participants | Perindopril 2 mg: n=62(39 males,23 females); mean age=51(16) years; baseline SBP/DBP not reported for all 62 patients; Perindopril 4 mg: n=57(32 males,25 females); mean age=51(15) years; baseline SBP/DBP not reported for all 57 patients; Perindopril 8 mg: n=59(32 males,27 females); mean age=51(15) years; baseline SBP/DBP not reported for all 59 patients; Perindopril 16 mg: n=57(35 males,22 females); mean age=51(15) years; baseline SBP/DBP not reported for all 57 patients; Placebo: n=58(30 males,28 females); mean age=53(15) years; baseline SBP/DBP not reported for all 58 patients | |
| Interventions | Perindopril 2 mg once daily; Perindopril 4 mg once daily; Perindopril 8 mg once daily; Perindopril 16 mg once daily; Placebo; administered in the morning | |
| Outcomes | Mean change from baseline in trough supine SBP/DBP using mercury sphygmomanometer; Mean change from baseline in peak supine SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change reported, SD of change not reported, endpoint BP and SD not reported, baseline SEM reported, calculated baseline SD from N and baseline SEM, imputed baseline SBP SD for SBP SD of change; imputed overall trial mean DBP SD of change; BP data from Table 2, p. 1193; Jadad score=3; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
New 2000.
| Methods | No placebo run‐in; inclusion criteria= patients with established Type 2 DM and BP > 75th centile for age and sex, taking no anti‐hypertensive medication; 3‐week double‐blind treatment | |
| Participants | Trandolapril 4 mg: n=12(10 males,2 females); mean age=58(11) years; baseline SBP=168(13) mm Hg, DBP=98(10) mm Hg; Placebo: n=12(9 males,3 females); mean age=60(12) years; baseline SBP=165(14) mm Hg, DBP=93(6) mm Hg | |
| Interventions | Trandolapril 4 mg once daily; Placebo; administered at 8 AM | |
| Outcomes | Trough supine SBP/DBP using mercury sphygmomanometer | |
| Notes | BP change and SD of change not reported; endpoint BP and SD reported; imputed endpoint SD for SD of change; SBP/DBP data from Figure 1, p. 137; Jadad score=2; funding source= Hoechst Marion Rousell | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Oparil 1999.
| Methods | 4‐ to 5‐week single‐blind placebo run‐in during which previous antihypertensive medication withdrawn; patients qualified for 3‐ to 4‐week enalapril challenge period if sitting DBP 95‐114 mm Hg and difference between their average sitting DBP values for last 2 visits of placebo run‐in period did not exceed 12 mm Hg; during enalapril challenge patients received enalapril 20 mg daily (10 mg for first 3 days); patients who developed persistent, nonproductive cough while receiving enalapril were then given placebo for 2‐4 weeks to allow cough to clear; eligible patients (those meeting inclusion criteria for enalapril challenge and whose cough subsequently cleared during placebo washout period) then entered 6‐week double‐blind treatment | |
| Participants | Enalapril 20 mg: n=45(23 males,22 females); baseline sitting SBP=154.6(14.1) mm Hg, DBP=100.9(4.7) mm Hg, HR=74.8(9.4) bpm; Placebo:n=45(21 males,24 females); baseline sitting SBP=154.1(14.1) mm Hg, DBP=99.8(4.0) mm Hg, HR=74.4(8.1) bpm | |
| Interventions | Enalapril 20 mg once daily (10 mg for first 3 days); Placebo | |
| Outcomes | Mean change from baseline in sitting DBP; WDAE | |
| Notes | DBP change and SD of change reported, endpoint BP and SD not reported, DBP data from text (p. 8) and Figure 3, p. 10; BP measurement device not reported; time of BP measurement not reported; Jadad score=4; funding source= SmithKline Beecham Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Overlack 1994.
| Methods | 3‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 95‐104 mm Hg after run‐in; 6‐week double‐blind treatment | |
| Participants | Perindopril 4 mg: n=253(130 males,123 females); mean age=59.3(11.1) years; baseline SBP=161.7(17.5) mm Hg, DBP=99.4(4.8) mm Hg, HR=78.5(14.3) bpm; Placebo: n=237(133 males,104 females); mean age=59.1(10.8) years; baseline SBP=160.3(16.9) mm Hg, DBP=99.5(4.6) mm Hg, HR=79.3(13.9) bpm | |
| Interventions | Perindopril 4 mg once daily; Placebo; administered in the morning | |
| Outcomes | Trough sitting SBP/DBP using automatic device; HR | |
| Notes | BP change and SD of change not reported, endpoint BP and SEM reported, calculated endpoint SD from N and endpoint SEM, imputed endpoint SD for SD of change; BP data from Table III, p. 129; Jadad score=3; funding source= Servier | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Persson 1996.
| Methods | Washout phase; 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 95‐114 mm Hg, with a difference of 10 mm Hg or less at last 2 consecutive visits of run‐in; subjects with DBP =/> 110 mm Hg could be included directly following minimum of 7 days single‐blind placebo; 8‐week double‐blind treatment | |
| Participants | Moexipril 7.5 mg: n=50(21 males,29 females); mean age=70.4 years; baseline sitting SBP=173 mm Hg, DBP=102 mm Hg, HR=76.7 bpm; Moexipril 15 mg: n=53(31 males,22 females); mean age=69.2 years; baseline sitting SBP=169 mm Hg, DBP=102 mm Hg, HR=73.9 bpm; Placebo: n=48(33 males,15 females); mean age=70.7 years; baseline sitting SBP=172 mm Hg, DBP=103 mm Hg, HR=72.7 bpm | |
| Interventions | Moexipril 7.5 mg once daily; Moexipril 15 mg once daily; Placebo | |
| Outcomes | Adjusted mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer; Placebo‐corrected adjusted change from baseline in peak sitting DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SD of change reported, endpoint SBP not reported, endpoint DBP reported, endpoint SD not reported; change in trough BP data from Table 2, p. 261; placebo‐corrected change in peak DBP data from Table 4, p. 262; endpoint BP data used instead of weighted mean of BP change for 3 measurements (at weeks 4,6,8) because N values not reported for weeks 4 and 6; Jadad score=3; funding source= Schwarz Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Pittrow 1997.
| Methods | 2‐week washout; 2‐week single‐blind placebo run‐in; inclusion criteria= mean sitting DBP 100‐114 mm Hg; 6‐week double‐blind treatment phase at fixed dose, patients with inadequate BP response had their doses doubled and were treated for another 6 weeks | |
| Participants | Spirapril 3 mg: n= 52(32 males,20 females); mean age=55.8 years; baseline sitting SBP=159.0 mm Hg, DBP=104.6 mm Hg (trough data); baseline sitting SBP=156.7 mm Hg, DBP=103.4 mm Hg (peak data); Spirapril 6 mg: n= 52(28 males,24 females); mean age=53.6 years; baseline sitting SBP=159.0 mm Hg, DBP=104.8 mm Hg (trough data); baseline sitting SBP=157.6 mm Hg, DBP=102.9 mm Hg (peak data); Placebo: n= 26(18 males,8 females); mean age=54.2 years; baseline sitting SBP=154.2 mm Hg, DBP=104.1 mm Hg (trough data); baseline sitting SBP=151.6 mm Hg, DBP=102.8 mm Hg (peak data) | |
| Interventions | Spirapril 3 mg once daily; Spirapril 6 mg once daily; Placebo; taken in the morning before breakfast | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer; Mean change from baseline in peak sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | Used week 6 BP data only; BP change and SD of change reported, endpoint BP reported, endpoint SD not reported; change in trough and peak BP data from Table 2A, p. 624; Jadad score=3; funding source= Novartis Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Pizarro 1996.
| Methods | 2‐week placebo run‐in; inclusion criteria= mean sitting DBP 95‐110 mm Hg; 6‐week double‐blind treatment | |
| Participants | Fosinopril 20 mg: n=16(4 males,12 females); mean age=56.4(8.1) years; baseline sitting SBP=151.8(14.0) mm Hg, DBP=100.8(4.8) mm Hg, HR=75.9(11.9) bpm; Placebo: n=18(2 males,15 females); mean age=53.2(7.0) years; baseline sitting SBP=160.1(22.1) mm Hg, DBP=100.1(2.4) mm Hg, HR=72.3(6.1) bpm | |
| Interventions | Fosinopril 20 mg once daily; Placebo | |
| Outcomes | Trough sitting SBP/DBP; Trough HR; WDAE | |
| Notes | SBP change not reported, DBP change reported; SD of change not reported, endpoint BP and SD reported; imputed endpoint SD for SD of change; BP data from text, p. 496 and p. 460; BP measurement device not reported; Jadad score=3; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Poirier 1991.
| Methods | 2‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 95‐109 mm Hg, within 10 mm Hg on 2 consecutive weekly visits during run‐in; 4‐week double‐blind treatment | |
| Participants | All patients: n=42(27 males,15 females); all white; Cilazapril 2.5 mg: n=14; mean age=53.6(8.0) years; baseline sitting SBP=153.6(16.4) mm Hg, DBP=102.0(4.7) mm Hg; Cilazapril 5 mg: n=14; mean age=53.1(8.2) years; baseline sitting SBP=154.8(15.1) mm Hg, DBP=101.0(4.3) mm Hg; Placebo: n=14; mean age=55.1(7.7) years; baseline sitting SBP=157.5(15.8) mm Hg, DBP=101.1(3.8) mm Hg | |
| Interventions | Cilazapril 2.5 mg once daily; Cilazapril 5 mg once daily; Placebo; taken in the morning | |
| Outcomes | Trough sitting SBP/DBP using mercury sphygmomanometer | |
| Notes | BP change and SD of change not reported, endpoint BP reported, endpoint SD not reported; baseline SBP SD reported, imputed baseline SBP SD for SBP SD of change, imputed overall trial mean DBP SD of change; BP data from Table 1, p. 914; Jadad score=3; funding source= Hoffman‐La Roche Ltd. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Pool 1990.
| Methods | 4‐ to 6‐week placebo run‐in; inclusion criteria= sitting DBP 95‐114 mm Hg on 2 consecutive visits after beginning of placebo run‐in; 4‐week double‐bind treatment at fixed dose; after 4 weeks, patients with inadequate BP response had their doses doubled during the second 4 weeks; hydrochlorothiazide 25 mg was added during final 4 weeks | |
| Participants | All patients: n=418 patients randomized to double‐blind treatment; n=380 who completed 4 weeks of double‐blind treatment included in efficacy analysis; Fosinopril 5 mg: n=83 randomized; for efficacy analysis n=74(53 males,21 females); mean age=53.2 years; baseline sitting SBP=151.7 mm Hg, DBP=101.4 mm Hg; Fosinopril 10 mg: n=84 randomized; for efficacy analysis n=71(55 males,16 females); mean age=53.5 years; baseline sitting SBP=148.6 mm Hg, DBP=100.9 mm Hg; Fosinopril 20 mg: n=84 randomized; for efficacy analysis n=79(51 males,28 females); mean age=54.2 years; baseline sitting SBP=153.2 mm Hg, DBP=102.4 mm Hg; Fosinopril 40 mg: n=85 randomized; for efficacy analysis n=79(52 males, 27 females); mean age=50.9 years; baseline sitting SBP=153.0 mm Hg, DBP=102.2 mm Hg; Placebo: n=82 randomized; for efficacy analysis n=77(52 males,25 females); mean age=53.2 years; baseline sitting SBP=151.7 mm Hg, DBP=101.4 mm Hg | |
| Interventions | Fosinopril 5 mg once daily; Fosinopril 10 mg once daily; Fosinopril 20 mg once daily; Fosinopril 40 mg once daily; Placebo | |
| Outcomes | Mean change in trough sitting SBP/DBP using mercury sphygmomanometer; Mean change in trough standing SBP/DBP using mercury sphygmomanometer | |
| Notes | BP change reported, SD of change not reported, endpoint BP and SD not reported; baseline SD not reported; imputed overall trial mean SD of change for SBP and DBP; change in SBP data from Figure 2, p. 524; change in DBP data from Table II, p. 526; Jadad score=3; funding source= Bristol‐Myers Squibb | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Pool 1997.
| Methods | 4‐ to 5‐week single‐blind placebo run‐in; inclusion criteria= mean sitting DBP 95‐110 mm Hg at consecutive visits (third and fourth weeks, or fourth and fifth weeks) during run‐in; 8‐week double‐blind treatment | |
| Participants | All patients: n=548(335 males,213 females); mean age=51.5(11.0) years; baseline sitting SBP=149.5(15.7) mm Hg, DBP=100.1(4.0) mm Hg; Fosinopril 2.5 mg: n=33 randomized; BP data reported for n=29; baseline sitting SBP=153.0 mm Hg, DBP=100.4 mm Hg; Fosinopril 10 mg: n=30 randomized; BP data reported for n=29; baseline sitting SBP=147.4 mm Hg, DBP=99.6 mm Hg; Fosinopril 40 mg: n=32 randomized; BP data reported for n=28; baseline sitting SBP=147.2 mm Hg, DBP=98.6 mm Hg; Placebo: n=32 randomized; BP data reported for n=29; baseline sitting SBP=150.4 mm Hg, DBP=99.8 mm Hg | |
| Interventions | Fosinopril 2.5 mg once daily; Fosinopril 10 mg once daily; Fosinopril 40 mg once daily; Placebo | |
| Outcomes | Adjusted mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer; Trough sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | Adjusted BP change reported, SD of change not reported, endpoint BP reported; endpoint SD not reported; baseline SD not reported; imputed overall trial mean SD of change for SBP and DBP; used endpoint BP data to calculated change in BP instead of entering adjusted BP change data; BP data from Tables 3 and 4, p. 120; Jadad score=3; funding source= Bristol‐Myers Squibb | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Pool 2001.
| Methods | 2‐ to 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 100‐115 mm Hg after run‐in; 8‐week double‐blind treatment | |
| Participants | All patients: n=454(286 males,168 females); mean age=53.8 years; Benazepril 10 mg: n=116; baseline SBP=155.3 mm Hg, DBP=104.2 mm Hg, HR=74.2 bpm; Placebo: n=115; baseline SBP=156.1 mm Hg, DBP=105.1 mm Hg, HR=74.4 bpm | |
| Interventions | Benazepril 10 mg once daily; Placebo; administered at approximately 8 AM | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer; Mean change from baseline in trough sitting HR; WDAE | |
| Notes | BP change reported, SD of change not reported; endpoint BP and SD not reported, baseline SD not reported, imputed overall trial mean SBP and DBP SD of change; BP and HR data from Table 1, p. 497; Jadad score=5; funding source= Novartis Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Pordy 1994.
| Methods | 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 95‐115 mm Hg after run‐in; 4‐week double‐blind treatment | |
| Participants | Cilazapril 0.5‐10 mg: n=288(166 males,122 females); mean age=53.9(12.1) years; baseline sitting DBP=100.4 mm Hg; Placebo: n=97(57 males,40 females); mean age=53.0(11.9) years; baseline sitting DBP=100.3 mm Hg | |
| Interventions | Cilazapril 0.5 mg once daily; Cilazapril 5 mg once daily; Cilazapril 10 mg once daily; Placebo; taken between 8 AM and 10 AM | |
| Outcomes | Mean change from baseline in trough sitting DBP using mercury sphygmomanometer; WDAE | |
| Notes | SBP not reported; DBP change and SD of change reported, endpoint BP and SD not reported; BP data from Table 3, p. 315; Jadad score=3; funding source= Hoffmann‐La Roche Ltd. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Prager 1994.
| Methods | 4‐week single‐blind placebo run‐in; inclusion criteria= DBP 95‐115 mm Hg after run‐in; 4‐week double‐blind treatment | |
| Participants | Cilazapril 2.5 mg: n=54(36 males,18 females); mean age=55.6(10.1) years; baseline sitting SBP=162.5(15.1) mm Hg, DBP=102.4(5.4) mm Hg; Cilazapril 5 mg: n=55(32 males,23 females); mean age=55.6(10.8) years; baseline sitting SBP=158.8(16.5) mm Hg, DBP=100.8(4.3) mm Hg; Placebo: n=53(29 males,24 females); mean age=58.1(9.5) years; baseline sitting SBP=161.4(16.5) mm Hg, DBP=102.1(5.7) mm Hg | |
| Interventions | Cilazapril 2.5 mg once daily; Cilazapril 5 mg once daily; Placebo; taken in the morning | |
| Outcomes | Trough supine SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SD of change not reported, endpoint BP and SD reported; imputed endpoint SD for SD of change; BP data from Table 2, p. S95; Jadad score=3; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Prichard 2002.
| Methods | 4‐week placebo run‐in; inclusion criteria= 1) sitting DBP=95‐114 mm Hg and sitting SBP</=200mm Hg during 2 weeks immediately prior to randomization, and on day 0, the first day of active treatment, with variation in DBP of not more than 10 mm Hg between the last week of run‐in phase and day 0, and 2) mean daytime (0600‐2159h) DBP>/=85 mm Hg by ambulatory BP monitoring on day immediately preceding randomization; 8‐week double‐blind treatment | |
| Participants | Enalapril 20 mg once daily: n=53(35 males,18 females); mean age=52.2(10.3) years; baseline sitting SBP=165.2(14.5) mm Hg, DBP=101.1(4.4) mm Hg; baseline HR=78.0(7.3) bpm; Placebo: n=50(29 males,21 females); mean age=53.7(8.7) years; baseline sitting SBP=162.8(14.5) mm Hg, DBP=99.9(3.9) mm Hg; baseline HR=76.6(8.8) bpm | |
| Interventions | Enalapril 20 mg once daily, Placebo; administered in morning (8.00+/‐2 h) | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SD of change reported, endpoint BP and SD reported, BP data from Table II, p. 169; Jadad score=4; funding source= Solvay Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Reimann 1995.
| Methods | 3‐week placebo run‐in; inclusion criteria= DBP 95‐104 mm Hg; 6‐week double‐blind treatment | |
| Participants | Perindopril 4 mg: n=27(20 males,7 females); mean age=54(9.8) years; baseline sitting SBP=161.3(12.5) mm Hg, DBP=100.4(3.8) mm Hg; Placebo: n=26(14 males,12 females); mean age=55(8.5) years; baseline sitting SBP=159.6(17.3) mm Hg, DBP=100.7(3.2) mm Hg | |
| Interventions | Perindopril 4 mg once daily; Placebo | |
| Outcomes | SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SD of change not reported, endpoint BP and SD reported; imputed endpoint SD for SD of change; BP data from Table 3, p. 190; time and position of BP measurement not reported; Jadad score=3; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Roca‐Cusachs 2001.
| Methods | 1‐week washout (only for patients previously treated with anti‐hypertensive therapy); 2‐week single‐blind placebo run‐in; inclusion criteria= DBP 90‐109 mm Hg (which differed < 10mm Hg from that observed in previous visit) after run‐in; 6‐week double‐blind treatment | |
| Participants | All patients (per protocol population): n=342(137 males,205 females); mean age=55.6(9.9) years; baseline sitting SBP=158.3(10.6) mm Hg, DBP=98.6(5.3) mm Hg | |
| Interventions | Enalapril 5 mg once daily; Enalapril 10 mg once daily; Enalapril 20 mg once daily; Placebo; taken in the morning; patients assigned to receive either 10 or 20 mg received 5 mg for the first week of treatment before titration to dose assigned | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer | |
| Notes | BP change and SD of change not reported, endpoint BP reported; endpoint SD not reported; baseline SD reported; imputed baseline SBP SD for SD of change; imputed overall trial mean DBP SD of change; BP data from Figure 1, p. 844; Jadad score=2; funding source= VITA INVEST | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Sassano 1984.
| Methods | 15‐day washout; 15‐day placebo run‐in; inclusion criteria= DBP 95‐120 mm Hg after run‐in; 4‐week double‐blind treatment | |
| Participants | Enalapril 20 mg: n=53(40 males,13 females); mean age=47.4 years; baseline supine SBP=161.4(13.0) mm Hg, DBP=103.3(6.3) mm Hg; Placebo: n=47(31 males,16 females); mean age=46.8 years; baseline supine SBP=163.5(13.8) mm Hg, DBP=104.6(7.0) mm Hg | |
| Interventions | Enalapril 20 mg once daily; Placebo | |
| Outcomes | Peak supine SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SD of change not reported, endpoint BP and SD reported; imputed endpoint SD for SD of change; BP data from Table I, p. 19; Jadad score=3; funding source= Merck Sharpe and Dohme | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Saynavalammi 1988.
| Methods | 4‐week single‐blind placebo phase; inclusion criteria= DBP 100‐115 mm Hg after placebo phase; 12‐week double‐blind treatment, dosage doubled every 4 weeks (10‐40 mg twice daily) | |
| Participants | Quinapril: n=7(2 males,5 females); mean age=48(11) years; baseline SBP=159(8) mm Hg, DBP=105(3) mm Hg; Placebo: n=7(3 males,4 females); mean age=47(13) years; baseline SBP=162(21) mm Hg, DBP=105(5) mm Hg | |
| Interventions | Quinapril 10 mg twice daily; Placebo | |
| Outcomes | Trough (12h after previous dose) sitting SBP/DBP using mercury sphygmomanometer | |
| Notes | Used week 4 BP data only; BP change and SD of change not reported, endpoint BP and SEM reported, calculated endpoint SD from N and endpoint SEM, imputed endpoint SD for SD of change; BP data from Figure 2, p. 90; Jadad score=2; funding source= Warner‐Lambert/Parke‐Davis Co. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Schoenberger 1986.
| Methods | 4‐ to 6‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 92‐109 mm Hg on last 2 visits of run‐in; 4‐week double‐blind treatment at fixed dose, after 4‐weeks captopril dosage doubled in all randomized patients for additional 4 weeks | |
| Participants | Captopril 50 mg once daily: n=88(58 males,30 females); mean age=52 years; baseline sitting SBP=149.3 mm Hg, DBP=98.2 mm Hg; Captopril 50 mg twice daily: n=91(60 males,31 females); mean age=52 years; baseline sitting SBP=151.2 mm Hg, DBP=100.1 mm Hg; Placebo: n=90(58 males,32 females); mean age=51 years; baseline sitting SBP=148.7 mm Hg, DBP=98.5 mm Hg | |
| Interventions | Captopril 50 mg once daily; Captopril 50 mg twice daily; Placebo; patients in daily schedule groups received their active medication in the morning and placebo in the evening | |
| Outcomes | Sitting DBP | |
| Notes | Used week 4 BP data only; BP change not reported, SD of change not reported, endpoint SBP not reported; endpoint DBP reported; endpoint SD not reported; baseline SD not reported; imputed overall trial mean SD of change for DBP; DBP data from Table 3, p. 382; BP measurement device not reported; Jadad score=2; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Scholze 1998.
| Methods | 1‐week washout period (for patients previously treated with antihypertensive therapy); 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 100‐115 mm Hg (which differed by less than 10 mm Hg from that observed on the previous visit) after run‐in; 6‐week double‐blind treatment | |
| Participants | Trandolapril 0.5‐2 mg: n=85; baseline SBP/DBP not reported; Placebo: n=30; baseline SBP/DBP not reported | |
| Interventions | Trandolapril 0.5 mg once daily; Trandolapril 1 mg once daily; Trandolapril 2 mg once daily; Placebo; administered with or immediately after breakfast | |
| Outcomes | Mean change from baseline in trough supine SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | Adjusted and non‐adjusted BP data reported; non‐adjusted BP entered in Revman; BP change reported, SD of change not reported; 95% confidence interval of change reported; endpoint BP and SD not reported; calculated SD of change from 95% CI of change; BP data from Table 1, p. 493; Jadad score=3; funding source= Knoll AG | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Scholze 1999.
| Methods | 2‐ to 4‐week single‐blind placebo run‐in; inclusion criteria= supine DBP 100‐115 mm Hg after run‐in; 6‐week double‐blind treatment | |
| Participants | All patients: n=507(327 males,180 females); mean age=50.2 years; baseline SBP/DBP not reported | |
| Interventions | Ramipril 2.5 mg once daily; Ramipril 5 mg once daily; Ramipril 10 mg once daily; Placebo | |
| Outcomes | Mean change from baseline in trough supine SBP/DBP using mercury sphygmomanometer | |
| Notes | BP change and SEM of change reported, endpoint BP and SD not reported; calculated SD of change from N and change SE; BP data from Table 1, p. 1453; Jadad score=3; funding source= Hoechst AG | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Simon 1983.
| Methods | 4‐week placebo run‐in; inclusion criteria= not reported but baseline DBP for all groups is at least 90 mm Hg; 12‐week total double‐blind treatment; increasing doses of enalapril 10, 20, and 40 mg daily every 4 weeks | |
| Participants | All patients: n= 34(33 male,1 female) white patients; Enalapril once and twice daily: n=21; mean age=52(11) years; baseline SBP=143(15) mm Hg, DBP=93(5) mm Hg; Placebo: n=12; mean age=50(17) years; baseline SBP=150(14) mm Hg, DBP=92(7) mm Hg | |
| Interventions | Enalapril 10 mg once daily; Enalapril 10 mg twice daily; Placebo; first dose taken in the morning | |
| Outcomes | Trough sitting SBP/DBP | |
| Notes | Used week 4 DBP only since patients treated with enalapril 10 mg once daily did not have SBP >/= 140mm Hg at baseline; BP change and SD of change not reported; endpoint BP reported; endpoint SD not reported; imputed overall trial mean SD of change; BP data from Figure 1, p. 461; BP measurement device not reported; Jadad score=2; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Smith 1998.
| Methods | 2‐ to 3‐week screening/washout period; 4‐week single‐blind placebo run‐in; inclusion criteria= supine DBP 95‐114 mm Hg; 12‐week double‐blind treatment | |
| Participants | Enalapril 20 mg: n=72(44 males,28 females); mean age=53.1(11.0) years; baseline supine SBP=153.8(13.8) mm Hg, DBP=100.4(4.2) mm Hg; Placebo: n=76(49 males,27 females); mean age=55.6(9.6) years; baseline supine SBP=154.8(11.8) mm Hg, DBP=100.4(4.5) mm Hg | |
| Interventions | Enalapril 20 mg once daily; Placebo | |
| Outcomes | Mean change from baseline in trough supine SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SE of change reported; endpoint BP and SD not reported; calculated SD of change from N and SE of change; change in BP data from Figures 1 and 2, p. 235; SE of change data from Table 2, p. 234; Jadad score=3; funding source= Boehringer Ingelheim Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Smith 2000.
| Methods | Minimum 7‐day washout; 4‐week single‐blind placebo run‐in; inclusion criteria= supine DBP 100‐114 mm Hg during final 2 weeks of run‐in, mean supine DBP could not vary by more than 7 mm Hg between weeks 2 and 3 or weeks 3 and 4 of run‐in, or by more than 10 mm Hg between weeks 2 and 4 of run‐in; 4‐week double‐blind treatment | |
| Participants | Enalapril 20 mg: n=42(31 males,11 females); mean age=52.0 years; baseline supine SBP=155.3 mm Hg, DBP=103.3 mm Hg, HR=72.7 bpm; Placebo: n=43(24 males,19 females); mean age=52.0 years; baseline supine SBP=159.5 mm Hg, DBP=104.9 mm Hg, HR=72.5 bpm | |
| Interventions | Enalapril 20 mg once daily; Placebo; taken with water (120 mL) between 6 AM and 9 AM and at least 1 h before breakfast | |
| Outcomes | Mean change from baseline in trough standing SBP/DBP using mercury sphygmomanometer; Mean change from baseline in trough supine SBP/DBP using mercury sphygmomanometer; Mean change from baseline in trough standing HR; Mean change from baseline in trough supine HR; WDAE | |
| Notes | BP change and SE of change reported; endpoint BP and SD not reported; calculated SD of change from N and SE of change; change in BP data from Table II, p. 1385; Jadad score=4; funding source= Boehringer Ingelheim Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Trevisan 1995.
| Methods | No minimal BP inclusion criteria; 24‐week total double‐blind treatment, report BP at week 4 of double‐blind treatment | |
| Participants | All patients (normotensive and hypertensive) with non‐insulin‐dependent diabetes mellitus: Ramipril 1.25 mg: n=60(44 males,16 females); mean age=56(7) years; baseline SBP=147(15) mm Hg, DBP=90(6) mm Hg; Placebo: n=62(50 males,12 females); mean age=58(7) years; baseline SBP=151(14) mm Hg, DBP=91(6) mm Hg; Subgroup of patients with BP >/= 160/95 mm Hg: Ramipril 1.25 mg: n=19; baseline SBP=156(12) mm Hg, DBP=95(4) mm Hg; Placebo: n=24; baseline SBP=161(9) mm Hg, DBP=95(3) mm Hg | |
| Interventions | Ramipil 1.25 mg once daily; Placebo | |
| Outcomes | Mean change from baseline in sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | Used week 4 BP data only; no minimal BP inclusion criteria, trial included both hypertensive and non‐hypertensive patients; Used BP data from subgroup with BP >/= 160/95 mm Hg; BP change and SD of change not reported; endpoint BP and SD reported; imputed endpoint SD of change; BP data from Table 5, p. 881; time of BP measurement not reported; Jadad score=4; funding source= Hoechst | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Uusitupa 1996.
| Methods | 4‐week normal sodium, placebo run‐in (week 0‐4); inclusion criteria= mean supine DBP 95‐114 mm Hg and mean daytime ambulatory DBP 90‐105 mm Hg after run‐in; 8‐week low‐sodium placebo period (week 4‐12); 12‐week double‐blind treatment (week 12‐24) | |
| Participants | Cilazapril 2.5 mg: n=19(10 males,9 females); mean age=53.7(5.7) years; baseline sitting SBP=157.3(17.1) mm Hg, DBP=104.0(8.0) mm Hg, HR=70(13) bpm; Placebo: n=20(14 males,6 females); mean age=50.5(9.5) years; baseline sitting SBP=147.0(10.3) mm Hg, DBP=99.4(5.3) mm Hg, HR=70(10) bpm | |
| Interventions | Cilazapril 2.5 mg once daily; Placebo; taken before breakfast in the morning between 7 AM and 9 AM | |
| Outcomes | Trough sitting SBP/DBP using mercury sphygmomanometer; Trough sitting HR | |
| Notes | BP change reported; SD of change not reported; 95% confidence interval of change reported; calculated SD of change from 95% CI of change; endpoint BP and SD reported; BP change data from Table 6, p. 323; endpoint BP data from Table 4, p. 322; Jadad score=3; funding source= Hoffmann‐La Roche Ltd. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
VA Study Group 1984.
| Methods | 2‐ to 5‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 92‐109 mm Hg on 2 consecutive clinic visits during run‐in; 7‐week double‐blind treatment | |
| Participants | Captopril 12.5 mg TID: n=83(all males); mean age=55.7(9.8) years; baseline sitting SBP=147.8(14.6) mm Hg, DBP=97.0(3.6) mm Hg; Captopril 25 mg TID: n=84(all males); mean age=55.7(8.1) years; baseline sitting SBP=147.4(11.9) mm Hg, DBP=97.9(3.7) mm Hg; Captopril 37.5 mg BID: n=88(all males); mean age=54.9(7.9) years; baseline sitting SBP=149.0(13.1) mm Hg, DBP=97.5(4.7) mm Hg; Captopril 50 mg TID: n=89(all males); mean age=55.1(8.0) years; baseline sitting SBP=148.2(16.0) mm Hg, DBP=98.1(4.7) mm Hg; Placebo: n=83(all males); mean age=54.4(8.0) years; baseline sitting SBP=146.3(14.6) mm Hg, DBP=97.8(4.6) mm Hg | |
| Interventions | Captopril 12.5 mg three times daily, Captopril 25 mg three times daily, Captopril 37.5 mg twice daily, Captopril 50 mg three times daily, Placebo; all patients were directed to take the capsules at least 1 h before breakfast, 2 h after lunch, and at bedtime, ie, at least 2 h after dinner | |
| Outcomes | Mean change from baseline in sitting SBP/DBP using mercury sphygmomanometer; WDAE; visits were scheduled approx 3 h from the time the patient took his last dose of medication | |
| Notes | BP change and SE of change reported; endpoint BP and SD reported; calculated SD of change from N and change SE; BP data from Table 4, p. 1953; Jadad score=4; funding source= E.R. Squibb & Sons Inc. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Vandenburg 1994.
| Methods | 2‐week placebo run‐in; inclusion criteria= sitting DBP 95‐115 mm Hg; 4‐week double‐blind treatment | |
| Participants | Imidapril 5 mg: n=33(21 males,12 females); mean age=53.2(12.1) years; baseline sitting DBP=102.3(5.7) mm Hg; Imidapril 10 mg: n=31(18 males,13 females); mean age=52.3(11.7) years; baseline sitting DBP=100.8(4.5) mm Hg; Imidapril 20 mg: n=31(16 males,15 females); mean age=52.5(10.0) years; baseline sitting DBP=101.0(5.6) mm Hg; Imidapril 40 mg: n=32(21 males,11 females); mean age=49.8(13.6) years; baseline sitting DBP=102.2(5.1) mm Hg; Placebo: n=35(20 males,15 females); mean age=51.9(11.8) years; baseline sitting DBP=101.3(5.3) mm Hg | |
| Interventions | Imidapril 5 mg once daily; Imidapril 10 mg once daily; Imidapril 20 mg once daily; Imidapril 40 mg once daily; Placebo | |
| Outcomes | Trough sitting SBP/DBP using mercury sphygmomanometer; Trough standing SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SD of change reported; endpoint BP and SD reported; change in BP data from Table 4, p. 271; Jadad score=3; funding source= Tanabe Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Vaur 1998.
| Methods | 2‐week washout; 2‐week single‐blind placebo run‐in; inclusion criteria= mean supine DBP 95‐114 mm Hg after run‐in; 4‐week double‐blind treatment | |
| Participants | Trandolapril 2 mg: n=24(15 males,9 females); mean age=56(10) years; baseline sitting SBP=163(16) mm Hg, DBP=101(6) mm Hg; Placebo: n=10(5 males,5 females); mean age=53(12) years; baseline SBP=157(14) mm Hg, DBP=100(7) mm Hg | |
| Interventions | Trandolapril 2 mg once daily; Placebo; administered in the morning | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer | |
| Notes | BP change and SD of change reported; endpoint BP and SD not reported; SBP/DBP data from Table 3, p. 110; Jadad score=3; funding source= Roussel Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Villamil 1987.
| Methods | 2‐week placebo run‐in; inclusion criteria= supine and standing DBP 95‐120 mm Hg after run‐in; 4‐week double‐blind treatment | |
| Participants | Ramipril 2.5 mg: n=28(12 males,16 females); median age=54 years; baseline SBP=162.0 mm Hg, DBP=101.1 mm Hg; Ramipril 5 mg: n=29(11 males,18 females); median age=53 years; baseline SBP=166.8 mm Hg, DBP=103.2 mm Hg; Placebo: n=27(15 males,12 females); median age=52 years; baseline SBP=166.6 mm Hg, DBP=101.5 mm Hg | |
| Interventions | Ramipril 2.5 mg once daily; Ramipril 5 mg once daily; Placebo; administered between 6 AM and 8 AM | |
| Outcomes | Mean change from baseline in trough standing SBP/DBP using mercury sphygmomanometer; Mean change from baseline in trough supine SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SEM of change reported, endpoint BP and SD not reported; calculated SD of change from N and change SE; BP data from Tables III and IV, p. 112D; Jadad score=3; funding source= Hoechst AG | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Waeber 1999.
| Methods | 4‐week placebo run‐in; inclusion criteria= sitting DBP 95‐110 mm Hg after run‐in; 12‐week total double‐blind treatment, titrated to response at 4 weeks | |
| Participants | Enalapril 10 mg: n=321(188 males,133 females); mean age=52.4(10.2) years; baseline sitting SBP=158.0(15.4) mm Hg, DBP=100.9(4.6) mm Hg; Placebo: n=304(165 males,135 females); mean age=51.0(10.7) years; baseline SBP=157.2(15.3) mm Hg, DBP=101.0(4.4) mm Hg | |
| Interventions | Enalapril 10 mg once daily; Placebo | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | Used week 4 BP data only; BP change and SD of change reported, endpoint BP and SD not reported; BP data from Figure I, p. 917; Jadad score=3; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Weinberger 1990.
| Methods | 2‐ to 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 95‐114 mm Hg, inclusive, on 2 consecutive visits (weeks 2 and 4 of run‐in) with </= 10mm Hg difference between 2 visits; 4‐week double‐blind treatment | |
| Participants | Benazepril 5 mg: n=38(23 males,15 females); mean age=51.1 years; baseline sitting SBP=152.7(15.2) mm Hg, DBP=101.2(5.3) mm Hg; Benazepril 10 mg: n=34(23 males,11 females); mean age=51.9 years; baseline sitting SBP=153.1(13.7) mm Hg, DBP=101.8(5.7) mm Hg; Benazepril 20 mg: n=36(23 males,13 females); mean age=50.4 years; baseline sitting SBP=151.9(15.7) mm Hg, DBP=101.7(4.7) mm Hg; Benazepril 40 mg: n=34(24 males,10 females); mean age=50.4 years; baseline sitting SBP=151.6(15.9) mm Hg, DBP=102.1(5.6) mm Hg; Placebo: n=31(21 males,10 females); mean age=48.2 years; baseline sitting SBP=150.7(14.3) mm Hg, DBP=101.7(4.9) mm Hg | |
| Interventions | Benazepril 5 mg once daily; Benazepril 10 mg once daily; Benazepril 20 mg once daily; Benazepril 40 mg once daily; Placebo | |
| Outcomes | Trough sitting DBP using mercury sphygmomanometer; Mean change from baseline in peak sitting DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SE of change reported, endpoint BP reported, endpoint SE not reported; calculated SD of change from N and SE of change; DBP data from Table III, p. 325; Jadad score=2; funding source= Ciba‐Geigy | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Weir 1995.
| Methods | 4‐week single‐blind placebo run‐in; inclusion criteria= mean supine DBP 95‐114 mm Hg during both of final 2 consecutive weeks of run‐in; 6‐week double‐blind treatment | |
| Participants | Black and white patients reported in Weir 1995: Trandolapril 1 mg: n=51(33 males,18 females); mean age=58.3(11.4) years; baseline sitting SBP=154.8(15.0) mm Hg, DBP=100.3(4.3) mm Hg; Trandolapril 2 mg: n=53(36 males,17 females); mean age=57.3(10.9) years; baseline sitting SBP=151.9(13.1) mm Hg, DBP=101.7(5.1) mm Hg; Trandolapril 4 mg: n=53(28 males,25 females); mean age=53.0(12.4) years; baseline sitting SBP=147.6(13.8) mm Hg, DBP=99.9(4.4) mm Hg; Placebo: n=50(35 males,15 females); mean age=60.6(9.9) years; baseline SBP=152.1(14.9) mm Hg, DBP=100.9(5.0) mm Hg Only black patients reported in Weir 1998 (duplicate publication): Trandolapril 0.25 mg: n=23(12 males,11 females); mean age=48.6(12.7) years; baseline supine SBP=159.1(13.5) mm Hg, DBP=101.7(5.3) mm Hg; Trandolapril 0.5 mg: n=22(9 males,13 females); mean age=49.4(12.3) years; baseline supine SBP=152.1(11.7) mm Hg, DBP=101.6(4.9) mm Hg; Trandolapril 1 mg: n=23(7 males,16 females); mean age=52.7(11.1) years; baseline supine SBP=150.7(13.1) mm Hg, DBP=99.7(3.5) mm Hg (same patients as Weir 1995); Trandolapril 2 mg: n=22(10 males,12 females); mean age=53.0(10.2) years; baseline supine SBP=146.1(11.4) mm Hg, DBP=99.1(3.2) mm Hg (same patients as Weir 1995); Trandolapril 4 mg: n=60(28 males,32 females); mean age=53.6(10.8) years; baseline supine SBP=156.2(16.1) mm Hg, DBP=101.7(4.9) mm Hg (same patients as Weir 1995); Trandolapril 8 mg: n=38(19 males,19 females); mean age=55.3(11.9) years; baseline supine SBP=158.7(19.3) mm Hg, DBP=101.4(4.3) mm Hg; Trandolapril 12 mg: n=38(19 males,19 females); mean age=53.1(13.5) years; baseline supine SBP=153.0(12.4) mm Hg, DBP=100.9(4.1) mm Hg; Trandolapril 16 mg: n=36(15 males,21 females); mean age=54.4(12.2) years; baseline supine SBP=159.5(17.3) mm Hg, DBP=100.5(3.7) mm Hg; Placebo: n=60(27 males,33 females); mean age=53.5(10.0) years; baseline supine SBP=155.7(15.5) mm Hg, DBP=100.6(4.2) mm Hg | |
| Interventions | Trandolapril 0.25 mg once daily (black patients only); Trandolapril 0.5 mg once daily (black patients only); Trandolapril 1 mg once daily (black and white patients); Trandolapril 2 mg once daily (black and white patients); Trandolapril 4 mg once daily (black and white patients); Trandolapril 8 mg once daily (black patients only); Trandolapril 12 mg once daily (black patients only); Trandolapril 16 mg once daily (black patients only); Placebo; administered between 8 AM and 10 AM | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer (Trandolapril 1, 2, 4 mg treatment arms); Mean change from baseline in trough supine SBP/DBP using mercury sphygmomanometer (Trandolapril 0.25, 0.5, 8, 12, 16 mg treatment arms); WDAE | |
| Notes | Weir 1995: BP change and SE of change reported; calculated SD of change from N and SE of change; endpoint BP and SD not reported; SBP/DBP data from Table 2, p. 126; Jadad score=3; funding source= Knoll Pharma Weir 1998: BP change and SE of change reported for trandalopril groups; SBP SE of change in placebo group not reported; DBP SE of change in placebo group reported; imputed baseline SBP SE for SE of change; calculated SD of change from N and SE of change; endpoint BP and SD not reported; SBP/DBP data from Table 2, p. 191 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Whalen 1989.
| Methods | 2‐ to 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 95‐114 mm Hg after run‐in; 8‐week double‐blind treatment | |
| Participants | All patients: n=165; Benazepril 20 mg: n=50; baseline sitting SBP=156 mmHg, DBP=103 mm Hg; Benazepril 40 mg: n=50; baseline sitting SBP=154 mmHg, DBP=102 mm Hg; Benazepril 80 mg: n=37; baseline sitting SBP=161 mmHg, DBP=104 mm Hg; Placebo: n=50; baseline sitting SBP=154 mmHg, DBP=103 mm Hg | |
| Interventions | Benazepril 20 mg once daily; Benazepril 40 mg once daily; Benazepril 80 mg once daily; Placebo | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP; Mean change from baseline in peak sitting SBP/DBP | |
| Notes | BP change reported; SD of change not reported, endpoint BP and SD not reported; imputed overall trial mean SD of change; BP data from abstract; BP measurement device not reported; Jadad score=2; funding source= Ciba‐Geigy Inc. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Whelton 1992.
| Methods | 2‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 95‐114 mm Hg during run‐in; 4‐week double‐blind treatment | |
| Participants | Enalapril 10 mg: n=36(24 males,12 females); mean age=53 years; baseline sitting SBP=152.9 mm Hg, DBP=100.5 mm Hg; Lisinopril 10 mg: n=37(22 males,15 females); mean age=51 years; baseline sitting SBP=146.9 mm Hg, DBP=99.1 mm Hg; Placebo: n=37(23 males,14 females); mean age=50 years; baseline sitting SBP=149.9 mm Hg, DBP=99.5 mm Hg | |
| Interventions | Enalapril 10 mg once daily; Lisinopril 10 mg once daily; Placebo; administered between 8 AM and 9 AM | |
| Outcomes | Baseline adjusted mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SE of change reported, endpoint BP and SD not reported; calculated SD of change from N and change SE; BP data from Table II, p. 328; Jadad score=3; funding source= ICI Americas Inc. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
White 1988.
| Methods | 4‐week single‐blind placebo run‐in; inclusion criteria= DBP 95‐114 mm Hg after run‐in; 4‐week double‐bind treatment at fixed dose; after 4 weeks (week 0‐4), patients with inadequate BP response had their doses doubled during the second 4 weeks (week 4‐8); hydrochlorothiazide 12.5 mg (in a single morning dose) was added during final 4 weeks (week 8‐12) | |
| Participants | All patients: n=18(10 males,8 females); mean age=52(12) years; Cilazapril 2.5 mg: n=9; baseline sitting SBP=155(15) mm Hg, DBP=104(4) mm Hg, HR=77(8) bpm; Placebo: n=9; baseline sitting SBP=152(15) mm Hg, DBP=100(4) mm Hg, HR=83(8) bpm | |
| Interventions | Cilazapril 2.5 mg once daily; Placebo | |
| Outcomes | Trough sitting SBP/DBP using mercury sphygmomanometer; Trough standing SBP/DBP using mercury sphygmomanometer; Trough sitting HR; Trough standing HR; WDAE | |
| Notes | Used week 4 BP data only; BP change and SD of change not reported; endpoint BP and SD reported; imputed endpoint SD for SD of change; BP data from Table 1, p. 174; Jadad score=3; funding source= Hoffmann‐La Roche Ltd. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
White 1995.
| Methods | Minimum 1‐week washout; 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 95‐114 mm Hg on 2 separate visits at end of placebo run‐in, with difference between visits of 10 mm Hg or less; 8‐week double‐blind treatment | |
| Participants | Moexipril 7.5 mg: n=16(12 males,4 females); mean age=56(12) years; baseline sitting SBP=161(12) mm Hg, DBP=103(4) mm Hg, HR=76(8) bpm; Moexipril 15 mg: n=18(16 males,2 females); mean age=58(9) years; baseline sitting SBP=157(13) mm Hg, DBP=104(4) mm Hg, HR=78(13) bpm; Placebo: n=17(15 males,2 females); mean age=50(12) years; baseline sitting SBP=149(17) mm Hg, DBP=106(4) mm Hg, HR=77(8) bpm | |
| Interventions | Moexipril 7.5 mg once daily; Moexipril 15 mg once daily; Placebo | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer; Mean change from baseline in trough sitting HR | |
| Notes | BP change and SD of change reported, endpoint BP and SD not reported; change in BP data from Table II, p. 235; Jadad score=2; funding source= Schwarz Pharma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
White 2002.
| Methods | 1‐ to 2‐week washout period for patients who were currently receiving antihypertensive therapy; 2‐ to 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 95‐115 mm Hg during 2 consecutive weeks of run‐in; also required that ambulatory awake DBP >/= 85 mm Hg; total 8‐week double‐blind treatment: 4‐week low‐dose treatment (week 0‐4), forced titration at week 4 to high‐dose, 4‐week high‐dose treatment (week 4‐8) | |
| Participants | Enalapril 10 mg: n=99(58 males,41 females); mean age=54(10) years; baseline SBP=145(16) mm Hg, DBP=93(8) mm Hg; baseline HR=72(10) bpm; Placebo: n=46(30 males,16 females); mean age=56(11) years; baseline SBP=148(12) mm Hg, DBP=95(6) mm Hg; baseline HR=71(9) bpm | |
| Interventions | Enalapril 10 mg once daily; Placebo; administered in the morning | |
| Outcomes | Mean change from baseline in trough sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | Used week 4 BP data only; BP change and SD of change reported, endpoint BP and SD not reported; BP data from Table IV, p. 663; Jadad score=3; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Yebes 1993.
| Methods | 4‐week single‐blind placebo washout; inclusion criteria= sitting DBP > 100 and < 115 mm Hg after washout; 8‐week double‐blind treatment, randomized to either placebo or quinapril 20 mg once daily for 4 weeks with optional titration to 40 mg once daily for subsequent 4 weeks based on diastolic response | |
| Participants | Quinapril: n=10; mean age=55(14.9) years; baseline SBP=161(22.2) mm Hg, DBP=105(5.6) mm Hg; Placebo: n=11; mean age=50(9.9) years; baseline SBP=154(20.6) mm Hg, DBP=103(5.0) mm Hg | |
| Interventions | Quinapril 20 mg once daily; Placebo | |
| Outcomes | Mean change from baseline in sitting SBP/DBP | |
| Notes | Used week 4 BP data only; BP change and SD of change reported, endpoint BP and SD reported; time of dosing not reported; time of BP measurement not reported; SBP data from Table IA, p. 321, DBP data from Table IIA, p. 323; time of BP measurement not reported; BP measurement device not reported; Jadad score=3; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Yodfat 1993.
| Methods | 4‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP > 100 mm Hg after run‐in; 8‐week double‐blind treatment | |
| Participants | Cilazapril: n=94(67 males,27 females); mean age=52.4(8.1) years; baseline BP not reported; Placebo: n=46(28 males,18 females); mean age=54.1(7.0) years; baseline BP not reported | |
| Interventions | Cilazapril 2.5 mg once daily; Cilazapril 5 mg once daily; Placebo; taken at approximately 12 PM before meal | |
| Outcomes | Mean change from baseline in trough sitting DBP using mercury sphygmomanometer; WDAE | |
| Notes | SBP change not reported; DBP change reported; SD of change not reported, endpoint SBP/DBP and SD not reported; imputed overall trial mean SD of change for DBP; baseline BP not reported; BP data from Figure 1, p. 119; Jadad score=3; funding source= not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Zamboulis 1996.
| Methods | 4‐week washout; 2‐week single‐blind placebo run‐in; inclusion criteria= sitting DBP 95‐114 mm Hg at end of placebo run‐in; 4‐week double‐blind treatment | |
| Participants | Fosinopril 20 mg: n=12(8 males,4 females); mean age=51 years; baseline seated SBP=150.8(15.9) mm Hg, DBP=108.8(4.7) mm Hg; baseline HR=76.9(5.3) bpm; Placebo: n=11(7 males,4 females); mean age=45 years; baseline seated SBP=143.0(20.0) mm Hg, DBP=95.5(12.6) mm Hg; baseline HR=79.0(9.8) bpm | |
| Interventions | Fosinopril 20 mg once daily; Placebo | |
| Outcomes | Sitting SBP/DBP using mercury sphygmomanometer; WDAE | |
| Notes | BP change and SD of change not reported, endpoint BP and SD reported; imputed endpoint SD for SD of change; time of BP measurement (peak and/or trough) not reported; BP data from Table 1, p. 254; Jadad score=3; funding source= Bristol‐Myers Squibb | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
BP=blood pressure, DBP=diastolic blood pressure; SBP=systolic blood pressure; SD=standard deviation; WDAE=withdrawal due to adverse effects; bpm=beats per minute
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bainbridge 1993 | Crossover trial with no pre‐crossover data for first 4 weeks of treatment (ramipril 2.5 mg/day vs. placebo). |
| Bakris 2002 | Parallel group trial with 8‐week treatment period, forced titration at 4 weeks. Pre‐titration data not reported (enalapril 10 mg/day vs. losartan 50 mg/day vs. placebo). |
| Beaulieu 1993 | Crossover trial with no pre‐crossover data for first 4 weeks of treatment (fosinopril 20 mg/day vs. placebo). |
| Bergstrand 1985 | Balanced, two‐period, incomplete‐block design with 2 treatment periods of 3‐weeks duration. First treatment period data not reported (enalapril 2.5, 5, 10, 20, 40 vs. placebo). |
| Bohlen 1996 | Parallel group trial with 6‐week treatment period, titration in non‐responders at 4 weeks. Pre‐titration data not reported (perindopril 4 mg/day vs. placebo). |
| Canter 1994 | Parallel group trial with 8‐week treatment period. Number of patients per treatment arm not reported (quinapril 2.5, 10, 40 mg/day vs. placebo). |
| Canter 1994a | Crossover trial with no pre‐crossover data for first 4 weeks of treatment (quniapril 20 mg/day vs. placebo). |
| Cleroux 1994 | Crossover trial with no pre‐crossover data for first 4 weeks of treatment. 8‐week treatment periods but titration in non‐responders after 4 weeks treatment (quinapril 10 mg/day vs. placebo). |
| Cuspidi 1997 | Crossover trial with no pre‐crossover data for first 4 weeks of treatment (lisinopril 20 mg/day vs. placebo). |
| Duprez 1986 | Crossover trial with no pre‐crossover data for first 6 weeks of treatment (enalapril 20 mg/day vs. placebo). |
| Fagard 2001 | Crossover trial with no pre‐crossover data reported for first 6 weeks of treatment (enalapril 20 mg/day vs. losartan 50 mg/day vs. placebo). |
| Gall 1992 | Crossover trial with no pre‐crossover data for first 4 weeks of treatment. 8‐week treatment periods but titration in non‐responders after 4 weeks treatment (captopril 50 mg/day vs. placebo). |
| Gans 1993 | Parallel group trial with 8‐week treatment period, titration in non‐responders at 4 weeks. Pre‐titration data not reported (cilazapril 2.5 mg/day vs. placebo). |
| Gleerup 1996 | Crossover trial with no pre‐crossover data reported for first 4 weeks of treatment (spirapril 6 mg/day vs. placebo). |
| Guitard 1994a | Crossover trial with no pre‐crossover data reported for first 3 weeks of treatment (spirapril 3, 6, 12, 24 mg/day vs. placebo). |
| Gupta 1990 | Crossover trial with no pre‐crossover data for first 4 weeks of treatment (quinapril 40 mg/day vs. placebo). |
| Homuth 1993a | Parallel group trial with 6‐week treatment period. BP data not extractable from figures (ramipril 2.5, 10, 20 mg/day vs. placebo). |
| Hu 1999 | Parallel group trial with 12‐week treatment period, titration in non‐responders every 4 weeks. Pre‐titration data not reported (captopril 50 mg/day vs. placebo). |
| Kahan 1999 | Crossover trial with no pre‐crossover data reported for first 6 weeks of treatment (ramipril 5 mg/day vs. placebo). |
| Karlberg 1987 | Parallel group trial with 4‐week treatment period. BP data for placebo group not reported at week 4 (ramipril 5 mg/day vs. ramipril 10 mg/day vs. placebo). |
| Kjeldsen 1992 | Crossover trial with no pre‐crossover data reported for first 4 weeks of treatment (quinapril 40 mg/day vs. placebo). |
| Lacourciere 1999 | Parallel group trial with 8‐week treatment period. BP data for placebo group not reported (lisinopril 20 mg/day vs. telmisartan 80 mg/day vs. placebo). |
| Lavezzaro 1990 | Crossover trial with no pre‐crossover data reported for first 4 weeks of treatment (captopril 100 mg/day vs. placebo). |
| Leonetti 1991 | Parallel group trial with 8‐week treatment period, titration in non‐responders at 4 weeks. Pre‐titration data not reported (captopril 50 mg/day vs. placebo). |
| Littler 1990 | Crossover trial with no pre‐crossover data reported for first 6 weeks of treatment (perindopril 8 mg/day vs. placebo). |
| Louis 1992 | Parallel group trial with 4‐week treatment period. Only maximum BP reduction is reported (perindopril 2, 4, 8 mg/day vs. placebo). |
| Miyajima 1999 | Parallel group trial with 12‐week treatment period, titration in non‐responders at 4 weeks. Pre‐titration data not reported (imidapril 5 mg/day vs. placebo). |
| Morgan 2001 | Crossover trial with no pre‐crossover data for first 4 weeks of treatment. 8‐week treatment periods but titration in non‐responders after 4 weeks treatment (enalapril 20 mg/day vs. perindopril 4 mg/day vs. placebo). |
| Petersen 1996 | Crossover trial with no pre‐crossover data reported for first 4 weeks of treatment (spirapril 24 mg/day vs. placebo). |
| Petrie 2000 | Crossover trial with no pre‐crossover data reported for first 4 weeks of treatment (trandolapril 2 mg/day vs. placebo). |
| Petrov 2001 | Crossover trial with no pre‐crossover data reported for first 6 weeks of treatment (enalapril 20 mg/day vs. losartan 50 mg/day vs. placebo). |
| Plouin 1991 | Parallel group trial with 8‐week treatment period, titration in non‐responders at 4 weeks. Pre‐titration data not reported (perindopril 4 mg/day vs. placebo). |
| Pritchard 1996 | Crossover trial with no pre‐crossover data reported for first 3 weeks of treatment (trandolapril 2 mg/day vs. placebo). |
| Reisin 1997 | Parallel group trial with 12‐week treatment period, titration in non‐responders every 4 weeks. Pre‐titration data not reported (lisinopril 10 mg/day vs. placebo). |
| Salvetti 1987 | Crossover trial with no baseline data and no pre‐crossover data reported for first 4 weeks of captopril 100 mg/day vs. placebo. Only mean arterial blood pressure values given. |
| Salvetti 1988 | Crossover trial with no pre‐crossover data reported for first 4 weeks of treatment (captopril 50, 100 mg/day vs. placebo). |
| Salvetti 1989 | Crossover trial with no pre‐crossover data reported for first 4 weeks of treatment (enalapril 10, 20, 40 mg/day vs. placebo). |
| Samuelsson 1992 | Parallel group trial with 8‐week treatment period, titration in non‐responders at 2 or 4 weeks. Pre‐titration data not reported (lisinopril 20 mg/day vs. placebo). |
| Sassano 1984a | Parallel group trial with 6‐month treatment period. Additional BP lowering drugs added to enalapril 20 mg in non‐responders at 4 weeks. Data during first 4 weeks not reported. |
| Scholze 1993 | Parallel group trial with 6‐week treatment period. Number of patients per treatment arm not reported (ramipril 2.5, 5, 10 mg/day vs. placebo). |
| Thurig 1995 | Crossover trial with no pre‐crossover data reported for first 8 weeks of treatment (lisinopril 20 mg/day vs. placebo). |
| Tomei 1992 | Crossover trial with no pre‐crossover data reported for first 4 weeks of treatment (lisinopril 20 mg/day vs. placebo). |
| Wiggam 1998 | Crossover trial with no pre‐crossover data reported for first 8 weeks of treatment (captopril 100 mg/day vs. placebo). |
| Wilkins 1983 | Parallel group trial with 12‐week treatment period, titration in non‐responders every 4 weeks. Pre‐titration data not reported (enalapril 10 mg/day vs. placebo). |
| Wing 1987 | Crossover trial with no pre‐crossover data reported for first 4 weeks of treatment (enalapril 20 mg/day vs. placebo). |
| Wing 1988 | Crossover trial with no pre‐crossover data reported for first 4 weeks of treatment (enalapril 20 mg/day vs. placebo). |
| Youssef 1993 | Parallel group trial with 8‐week treatment. Highly suspicious data (enalapril 20 mg/day vs. benazepril 10 mg/day vs. placebo). |
| Zanchetti 2001 | Parallel group trial with 8‐week treatment period, titration in non‐responders at 4 weeks. Pre‐titration data not reported (enalapril 10 mg/day vs. candesartan 4 mg/day vs. placebo). |
Contributions of authors
Dr. James M. Wright conceived, designed and secured funding for the review, assisted with the analysis and interpretation of data, as well as provided a clinical perspective.
Dr. Balraj S. Heran designed the search strategy, undertook the search, screened search results, collected data for the review, screened retrieved papers against eligibility criteria, appraised quality of papers, extracted data from papers, wrote to authors of papers for additional information, entered data into RevMan, analyzed and interpreted data, and wrote the review.
Dr. Michelle Wong and Inderjit K. Heran screened retrieved papers against eligibility criteria, appraised quality of papers and extracted data from papers.
Sources of support
Internal sources
Department of Anesthesiology, Pharmacology & Therapeutics, University of British Columbia, Canada.
External sources
Canadian Institutes of Health Research (CIHR), Canada.
Declarations of interest
No conflicts of interest declared.
Edited (no change to conclusions)
References
References to studies included in this review
Applegate 1996 {published data only}
- Applegate WB, Cohen JD, Wolfson P, Davis A, Green S. Evaluation of blood pressure response to the combination of enalapril (single dose) and diltiazem ER (four different doses) in systemic hypertension. American Journal of Cardiology 1996;78:51‐5. [DOI] [PubMed] [Google Scholar]
Belz 1986 {published data only}
- Belz GG, Lange H, Tschollar W, Neis W. Cilazapril in essential hypertension: A placebo‐controlled double‐blind study to establish the dosage [Cilazapril bei essentieller hypertonie: Eine placebokontrollierte doppelblindstudie zur dosisfindung]. Medizinische Klinik 1986;81(15‐16):524‐9. [PubMed] [Google Scholar]
Black 1997 {published data only}
- Black HR, Graff A, Shute D, Stoltz R, Ruff D, Levine J, Shi Y, Mallows S. Valsartan, a new angiotensin II antagonist for the treatment of essential hypertension: efficacy, tolerability and safety compared to an angiotensin‐converting enzyme inhibitor, lisinopril. Journal of Human Hypertension 1997;11(8):483‐9. [DOI] [PubMed] [Google Scholar]
Boeijinga 1993 {published data only}
- Boeijinga JK, Kraaij CJ, Kleinbloesem H, Cohen AF, Breimer DD. The influence of cilazapril on anticoagulants in hypertensive patients treated with coumarins. Current Therapeutic Research 1993;54(4):443‐51. [Google Scholar]
Brown 1990 {published data only}
- Brown CL, Backhouse CI, Grippat JC, Santoni JP. The effect of perindopril and hydrochlorothiazide alone and in combination on blood pressure and on the renin‐angiotensin system in hypertensive subjects. European Journal of Clinical Pharmacology 1990;39(4):327‐32. [DOI] [PubMed] [Google Scholar]
Carlsen 1995 {published data only}
- Carlsen JE, Buchmann M, Hoglund C, Pellinen T, Honkanen T, Soerensen OH, Leth A, Maltbaek N. 24‐hour antihypertensive effect of oral cilazapril? A placebo‐controlled study evaluating 1, 2.5 and 5 mg once daily. Clinical Drug Investigation 1995;10(4):221‐7. [Google Scholar]
Chan 1997 {published data only}
- Chan P, Lin CN, Tomlinson B, Lin TH, Lee YS. Additive effects of diltiazem and lisinopril in the treatment of elderly patients with mild‐to‐moderate hypertension. American Journal of Hypertension 1997;10(7):743‐9. [DOI] [PubMed] [Google Scholar]
Chrysant 1993 {published data only}
- Chrysant SG, McDonald RH, Wright JT, Barden PL, Weiss RJ. Perindopril as monotherapy in hypertension: A multicenter comparison of two dosing regimens. Archives of Internal Medicine 1993;53(4):479‐84. [DOI] [PubMed] [Google Scholar]
Chrysant 1994 {published data only}
- Chrysant S. Antihypertensive effectiveness of low‐dose lisinopril‐hydrochlorothiazide combination. Archives of Internal Medicine 1994;154(7):737‐43. [PubMed] [Google Scholar]
Chrysant 1996 {published data only}
- Chrysant SG, Fagan T, Glazer R, Kriegman A. Effects of benazepril and hydrochlorothiazide, given alone and in low‐ and high‐dose combinations, on blood pressure in patients with hypertension. Archives of Family Medicine 1996;5(1):17‐24. [DOI] [PubMed] [Google Scholar]
- Fagan T, Head K, DeSilva J, Whalen J. Double‐blind comparison of once daily benazepril, hydrochlorothiazide and placebo in mild to moderate hypertension. American Journal of Hypertension 1989;2(5, Part 2):78A. [Google Scholar]
- Gomez HJ. Dose‐response studies with benazepril in mild to moderate hypertension. Clinical Cardiology 1991;14(Suppl IV):IV‐22‐7. [DOI] [PubMed] [Google Scholar]
Cushman 1998 {published data only}
- Cushman WC, Cohen JD, Jones RP, Marbury TC, Rhoades RB, Smith LK. Comparison of the fixed combination of enalapril/diltiazem ER and their monotherapies in stage 1 to 3 essential hypertension. American Journal of Hypertension 1998;11(1):23‐30. [DOI] [PubMed] [Google Scholar]
De Bruijn 1994 {published data only}
- Bruijn JHB, Orofiamma BA, Pauly NC. Efficacy and tolerability of trandolapril (0.5‐2 mg) administered for 4 weeks in patients with mild‐to‐moderate hypertension. Journal of Cardiovascular Pharmacology 1994;23(Suppl 4):S60‐S64. [PubMed] [Google Scholar]
DeQuattro 1997 {published data only}
- DeQuattro V, Lee D, Messerli F. Efficacy of combination therapy with trandolapril and verapamil SR in primary hypertension: A 4 X 4 trial design. Clinical and Experimental Hypertension 1997;19(3):373‐87. [DOI] [PubMed] [Google Scholar]
- DeQuattro V, Lee D, and the Trandolapril Study Group. Fixed‐dose combination therapy with trandolapril and verapamil SR is effective in primary hypertension. American Journal of Hypertension 1997;10(7 Pt 2):138S‐145S. [DOI] [PubMed] [Google Scholar]
- Levine JH, Applegate WB. Trandolapril and verapamil slow release in the treatment of hypertension: A dose‐response assessment with the use of a multifactorial trial design. Current Therapeutic Research 1997;58(6):361‐74. [Google Scholar]
Drayer 1983 {published data only}
- Drayer J, Weber MA. Monotherapy of essential hypertension with a converting‐enzyme inhibitor. Hypertension 1983;5(Suppl III):III108‐13. [DOI] [PubMed] [Google Scholar]
Dupui 1993 {published data only}
- Dupui P, Larrue V, Pavy‐Le Traon A, Allavoine T, Geraud G, Bes A. Effects of a captopril‐induced decrease of the arterial blood pressure on the cerebral blood flow of elderly subjects with moderate hypertension [Consequences d'une diminution de la pression sanguine arterielle induite par le captopril sur l'hemodynamique cerebrale du sujet age moderement hypertendu]. Circulation et metabolisme du cerveau 1993;10(3‐4):143‐56. [Google Scholar]
- Larrue V, Dupui P, Pave‐Le Traon A, Allavoine T, Geraud G, Bes A. Cerebral blood flow changes induced by a chronic treatment with captopril in previously untreated elderly hypertensive subjects [Effets du captopril sur le debit sanguin cerebral du sujet age hypertendu]. Archives des Maladies du Coeur et des Vaisseaux 1994;87(8):997‐1000. [PubMed] [Google Scholar]
Fairhurst 1994 {published data only}
- Fairhurst GJ. A multicentre multidose study of the efficacy and safety of spirapril in mild‐to‐moderate essential hypertension. Blood Pressure 1994;3(Suppl 2):77‐80. [PubMed] [Google Scholar]
Fernandez 1990 {published data only}
- Fernandez PG, Bolli P, Lee C. The 24 h blood pressure responses of hypertensives to a once‐a‐day cilazapril regimen. Canadian Journal of Cardiology 1990;6(2):53‐8. [PubMed] [Google Scholar]
- Fernandez PG, Bolli P, Lee C, Vasdev S. Cilazapril inhibits vascular responses to baroreflex‐stimulated sympathetic neural activity in hypertensive patients. Canadian Journal of Cardiology 1990;6(1):9‐14. [PubMed] [Google Scholar]
Fernandez 1994 {published data only}
- Fernandez M, Madero R, Gonzalez D, Camacho P, Villalpando J, Arriaga J. Combined versus single effect of fosinopril and hydrochlorothiazide in hypertensive patients. Hypertension 1994;23(Suppl 1):I207‐10. [DOI] [PubMed] [Google Scholar]
Ford 1993 {published data only}
- Ford NF, Fulmor IE, Nichola PS, Alpin PG, Herron JM. Fosinopril monotherapy: Relationship between blood pressure reduction and time of administration. Clinical Cardiology 1993;16(4):324‐30. [DOI] [PubMed] [Google Scholar]
Gerritsen 1998 {published data only}
- Gerritsen TA, Bak AAA, Stolk RP, Jonker JJC, Grobbee DE. Effects of nitrendipine and enalapril on left ventricular mass in patients with non‐insulin‐dependent diabetes mellitus and hypertension. Journal of Hypertension 1998;16(5):689‐96. [DOI] [PubMed] [Google Scholar]
Gomez 1989 {published data only}
- Gomez HJ, Cirillo VJ, Sromosky JA, Otterbein ES, Shaw WC, Rush JE, Chrysant SG, Gradman AH, Leon AS, MacCarthy P, Nelson EB, Pool J, Vedin A. Lisinopril dose‐response relationship in essential hypertension. British Journal of Clinical Pharmacology 1989;28(4):415‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gradman 1995 {published data only}
- Gradman AH, Arcuri KE, Goldberg AI, Ikeda LS, Nelson EB, Snavely DB, Sweet CS. A randomized, placebo‐controlled, double‐blind, parallel study of various doses of losartan potassium compared with enalapril maleate in patients with essential hypertension. Hypertension 1995;25(6):1345‐50. [DOI] [PubMed] [Google Scholar]
Gradman 1997 {published data only}
- Gradman AH, Cutler NR, Davis PJ, Robbins JA, Weiss RJ, Wood BC. Combined enalapril and felodipine extended release (ER) for systemic hypertension. American Journal of Cardiology 1997;79(4):431‐5. [DOI] [PubMed] [Google Scholar]
Guitard 1994 {published data only}
- Guitard C, Alvisi V, Maibach E, Franck J, Cocco G, Boxho G, Mellein B, Waite R. Placebo‐controlled comparison of spirapril at 6, 12 and 24 mg/day in mild to severe essential hypertension. Blood Pressure 1994;3(Suppl 2):81‐7. [PubMed] [Google Scholar]
Guitard 1997 {published data only}
- Guitard C, Lohmann FW, Alfiero R, Ruina M, Alvisi V. Comparison of efficacy of spirapril and enalapril in control of mild‐to‐moderate hypertension. Cardiovascular Drugs and Therapy 1997;11(3):449‐57. [DOI] [PubMed] [Google Scholar]
Guntzel 1991 {published data only}
- Guntzel P, Kobrin I, Pasquier C, Zimlichman R, Viskoper JR. The effect of cilazapril, a new angiotensin converting enzyme inhibitor, on peak and trough blood pressure measurements in hypertensive patients. Journal of Cardiovascular Pharmacology 1991;17(1):8‐12. [DOI] [PubMed] [Google Scholar]
- Kobrin I, Guntzel P, Viskoper R, Paran E, Zimlichman R. Antihypertensive duration of action of cilazapril in patients with mild to moderate essential hypertension. Drugs 1991;41(Suppl. 1):31‐6. [DOI] [PubMed] [Google Scholar]
Holwerda 1996 {published data only}
- Holwerda NJ, Fogari R, Angeli P, Porcellati C, Hereng C, Oddou‐Stock P, Heath R, Bodin F. Valsartan, a new angiotensin II antagonist for the treatment of essential hypertension: efficacy and safety compared with placebo and enalapril. Journal of Hypertension 1996;14(9):1147‐51. [DOI] [PubMed] [Google Scholar]
Homuth 1993 {published data only}
- Homuth V, Faulhaber H‐D, Loose U, Loffler K, Luft FC. Usefulness of piretanide plus ramipril for systemic hypertension: A multicenter trial. American Journal of Cardiology 1993;72(9):666‐71. [DOI] [PubMed] [Google Scholar]
Kayanakis 1987 {published data only}
- Kayanakis JG, Baulac L. Comparative study of once‐daily administration of captopril 50 mg, hydrochlorothiazide 25 mg and their combination in mild to moderate hypertension. British Journal of Clinical Pharmacology 1987;23(23 Suppl 1):89S‐92S. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kobrin 1991 {published data only}
- Kobrin I, Guntzel P, Viskoper R, Paran E, Zimlichman R. Antihypertensive duration of action of cilazapril in patients with mild to moderate essential hypertension. Drugs 1991;41(Suppl 1):31‐6. [DOI] [PubMed] [Google Scholar]
Koch 1999 {published data only}
- Koch B, Oparil S, Stimpel M. Co‐administration of an ACE‐inhibitor (moexipril) and hormonal replacement therapy in postmenopausal women. Journal of Human Hypertension 1999;13(5):337‐42. [DOI] [PubMed] [Google Scholar]
Kohlmann Jr 1999 {published data only}
- Kohlmann Jr O, Jardim PCBV, Oigman W. Brazilian multicenter study on efficacy and tolerability of trandolapril in mild‐to‐moderate essential arterial hypertension: EMBATHE substudy with ambulatory blood pressure monitoring [Estudo multicentrico brasileiro de avaliacao da eficacia e tolerabilidade de trandolapril na hipertensao arterial essencial leve a moderada: EMBATHE subestudo com monitorizacao arterial de pressao arterial]. Arquivos Brasileiros de Cardiologia 1999;72(5):547‐52. [DOI] [PubMed] [Google Scholar]
Kostis 1991 {published data only}
- Kostis JB. Double‐blind study of ascending doses of ramipril in patients with mild to moderate hypertension. Advances in Therapy 1991;8(1):6‐17. [Google Scholar]
- Schnaper HW. Dose‐response relationship of ramipril in patients with mild‐to‐moderate hypertension. Journal of Cardiovascular Pharmacology 1991;18(Suppl 2):S128‐S130. [PubMed] [Google Scholar]
Krum 1992 {published data only}
- Krum H, Jackson B, Conway EL, Howes LG, Johnston CI, Louis WJ. Steady‐state pharmacokinetics and pharmacodynamics of cilazapril in the presence and absence of cyclopenthiazide. Journal of Cardiovascular Pharmacology 1992;20(3):451‐7. [DOI] [PubMed] [Google Scholar]
Krum 1998 {published data only}
- Krum H, Viskoper RJ, Lacourciere Y, Budde M, Charlon V. The effect of an endothelin‐receptor antagonist, bosentan, on blood pressure in patients with essential hypertension. New England Journal of Medicine 1998;338(12):784‐90. [DOI] [PubMed] [Google Scholar]
Kuppers 1997 {published data only}
- Kuppers HE, Jager BA, Luszick JH, Grave MA, Hughes PR, Kaan EC. Placebo‐controlled comparison of the efficacy and tolerability of once‐daily moxonidine and enalapril in mild‐to‐moderate essential hypertension. Journal of Hypertension 1997;15:93‐7. [DOI] [PubMed] [Google Scholar]
Kuschnir 1996 {published data only}
- Kuschnir E, Acuna E, Sevilla D, Vasquez J, Bendersky M, Resk J, Glazer R. Treatment of patients with essential hypertension: Amlodipine 5 mg/benazepril 20 mg compared with amlodipine 5 mg, benazepril 20 mg, and placebo. Clinical Therapeutics 1996;18(6):1213‐24. [DOI] [PubMed] [Google Scholar]
Lacourciere 1994 {published data only}
- Lacourciere Y, Leenen F, Rangno R, Spence JD, Lenis JH, Myers MG. Discrepancies between clinic and ambulatory blood pressure responses to cilazapril therapy. Canadian Journal of Cardiology 1994;10(6):605‐10. [PubMed] [Google Scholar]
Lerch 1999 {published data only}
- Lerch M, Weidmann P, Ho MP, Gerber P, Eckenberger P, Kaemmereit A, Teuscher AU. Metabolic effects of temocapril in hypertensive patients with diabetes mellitus type 2. Journal of Cardiovascular Pharmacology 1999;33(4):527‐33. [DOI] [PubMed] [Google Scholar]
Levine 1995 {published data only}
- Levine JH, Ferdinand KC, Cargo P, Laine H, Lefkowitz M. Additive effects of verapamil and enalapril in the treatment of mild to moderate hypertension. American Journal of Hypertension 1995;8(5 Pt 1):494‐9. [DOI] [PubMed] [Google Scholar]
Luccioni 1988 {published data only}
- Luccioni R, Gass FR, Schwab C, Santoni JP, Perret L. Evaluation of the dose‐effect relationship of a new ace inhibitor (perindopril) by an automatic blood pressure recorder. European Heart Journal 1988;9:1131‐6. [DOI] [PubMed] [Google Scholar]
MacLean 1989 {published data only}
- Maclean D. Quinapril: A double‐blind, placebo‐controlled trial in essential hypertension. Angiology 1989;40(4 Pt 2):370‐81. [DOI] [PubMed] [Google Scholar]
Mancia 1992 {published data only}
- Mancia G, Cesaris R, Fogari R, Lattuada S, Montemurro G, Palomba C, Porcellati C, Ranieri G, Tettamanti F, Verdecchia P, Marelli C, Omboni S, Ravogli A, Zanchetti A. Evaluation of the antihypertensive effect of once‐a‐day trandolapril by 24‐hour ambulatory blood pressure monitoring. American Journal of Cardiology 1992;70(12):60D‐66D. [DOI] [PubMed] [Google Scholar]
- Ravogli A, Omboni S, Cesaris R, Fogari R, Lattuada S, Montemurro G, Palombo C, Porcellati C, Ranieri G, Tettamanti F, Verdecchia P, Marelli C, Zanchetti A, Mancia G. Twenty‐four hour ambulatory blood pressure monitoring and antihypertensive treatment: Focus on ACE inhibitors. Journal of Cardiovascular Pharmacology 1994;23(Suppl 1):S15‐S19. [DOI] [PubMed] [Google Scholar]
Mancia 1997 {published data only}
- Mancia G, Agabiti‐Rosei E, Benetti G, Calcagnini G, Campa PP, Carretta R, Casati R, Coca A, Sierra A, Federighi G, Fogari R, Fontana S, Gomez B, Infelise V, Nami R, Pasotti C, Pirrelli A, Otero L, Vidal L. Effects of verapamil SR, trandolapril, and their fixed combination on 24‐h blood pressure: The Veratran Study. American Journal of Hypertension 1997;10(5 Pt 1):492‐9. [DOI] [PubMed] [Google Scholar]
McCarron 1991 {published data only}
- Burris JF. The effect of ramipril on ambulatory blood pressure: A multicenter trial. Journal of Cardiovascular Pharmacology 1991;18(Suppl 2):S131‐S133. [PubMed] [Google Scholar]
- McCarron D. 24‐hour blood pressure profiles in hypertensive patients administered ramipril or placebo once daily: magnitude and duration of antihypertensive effects. Cardiology 1991;14(9):737‐42. [DOI] [PubMed] [Google Scholar]
McFate‐Smith 1991 {published data only}
- Gomez HJ, Glazer R, Mallows S, Silva J. Benazepril in the treatment of older and elderly hypertensive patients. Benazepril: Profile of a new ACE inhibitor. Royal Society of Medicine Services International Congress and Symposium Series. London: Royal Society of Medicine Services Limited, 1990, issue 166:111‐21.
- McFate Smith W, Gomez HJ. The use of benazepril in hypertensive patients age 55 and over. Clinical Cardiology 1991;14(Suppl IV):IV79‐82. [DOI] [PubMed] [Google Scholar]
Messerli 1998 {published data only}
- Messerli F, Frishman WH, Elliott WJ. Effects of verapamil and trandolapril in the treatment of hypertension. American Journal of Hypertension 1998;11(3 Pt 1):322‐7. [DOI] [PubMed] [Google Scholar]
Moser 1991 {published data only}
- Gomez HJ. Dose‐response studies with benazepril in mild to moderate hypertension. Clinical Cardiology 1991;14(Suppl IV):IV‐22‐7. [DOI] [PubMed] [Google Scholar]
- Moser M, Abraham PA, Bennett WM, Brachfeld N, Goodman RP, McKenney JM, Hollifield JW, Kirkendall WM, Lasseter KC, Leon AS, Lunn JA, Miller K, Morganroth J, Ruddy MC, Sambhi MP, Stein WJ, Weber MA, Williams RL, Zawada ET, DeSilva J, Gourley LA, Whalen JJ. The effects of benazepril, a new angiotensin‐converting enzyme inhibitor, in mild to moderate essential hypertension: A multicenter study. Clinical Pharmacology and Therapeutics 1991;49(3):322‐9. [DOI] [PubMed] [Google Scholar]
- Moser M, Whalen J, Gourley L, DeSilva J. Double‐blind comparison of benazepril, hydrochlorothiazide, and placebo in mild to moderate hypertension. American Journal of Hypertension 1989;2(5 Pt 2):44A. [Google Scholar]
Mroczek 1991 {published data only}
- Mroczek WJ, Klein J, Burris JF. Dose‐finding study of cilazapril (Inhibace(TM)) in patients with uncomplicated essential hypertension. Clinical and Experimental Hypertension ‐ Theory and Practice 1991;13(8):1415‐32. [DOI] [PubMed] [Google Scholar]
Mroczek 1996 {published data only}
- Mroczek WJ, Stimpel M. A double‐blind evaluation of moexipril versus hydrochlorothiazide in hypertension. Advances in Therapy 1996;13(2):79‐87. [Google Scholar]
Muiesan 1987 {published data only}
- Muiesan G, Agabiti‐Rosei E, Buoninconti R, Cagli V, Carotti A, Corea L, Innocenti P, Malerba M, Paciaroni E, Pirrelli A, Toso M, Botta G. Antihypertensive efficacy and tolerability of captopril in the elderly: Comparison with hydrochlorothiazide and placebo in multicentre, double‐blind study. Journal of Hypertension 1987;5(Suppl 5):S599‐S602. [PubMed] [Google Scholar]
Myers 1996 {published data only}
- Myers MG. A dose‐response study of perindopril in hypertension: Effects on blood pressure 6 and 24 h after dosing. Canadian Journal of Cardiology 1996;12(11):1191‐6. [PubMed] [Google Scholar]
New 2000 {published data only}
- New JP, Bilous RW, Walker M. Insulin sensitivity in hypertensive type 2 diabetic patients after 1 and 19 days' treatment with trandolapril. Diabetic Medicine 2000;17(2):134‐40. [DOI] [PubMed] [Google Scholar]
Oparil 1999 {published data only}
- Oparil S. Eprosartan versus enalapril in hypertensive patients with angiotensin‐converting enzyme inhibitor‐induced cough. Current Therapeutic Research 1999;60(1):1‐4. [Google Scholar]
Overlack 1994 {published data only}
- Bonner G, Lederle RM, Scholze J, Stumpe KO. Therapeutic safety of perindopril in the treatment of mild hypertension with concomitant therapy. Arzneimittel‐Forschung 1993;43(8):852‐5. [PubMed] [Google Scholar]
- Middeke M, Krone W. Effects of perindopril on serum lipids in hypertensive patients with hyperlipidemia. Journal of Cardiovascular Pharmacology 1994;23(4):629‐31. [DOI] [PubMed] [Google Scholar]
- Overlack A, Adamczak M, Bachmann W, Bonner G, Bretzel RG, Derichs R, Krone W, Lederle RM, Reimann HJ, Zschiedrich H, Stumpe KO. ACE‐inhibition with perindopril in essential hypertensive patients with concomitant diseases. American Journal of Medicine 1994;97(2):126‐34. [DOI] [PubMed] [Google Scholar]
- Overlack A, Kronig B, Stumpe KO. Clinical and functional course of COPD in hypertensive patients with concomitant chronic bronchitis and emphysema during treatment with an ACE inhibitor, perindopril. Journal of Drug Development 1993;6(1):5‐9. [Google Scholar]
- Stumpe KO, Overlack A. A new trial of the efficacy, tolerability, and safety of angiotensin‐converting enzyme inhibition in mild systemic hypertension with concomitant diseases and therapies. American Journal of Cardiology 1993;71(17):32E‐37E. [DOI] [PubMed] [Google Scholar]
- Stumpe KO, Overlack A. Angiotensin‐converting enzyme inhibition in mild hypertension with concomitant diseases and therapies: an efficacy, safety, and compatibility study of novel design, the Perindopril Therapeutic Safety Study. The American Journal of Medicine 1992;92(4B):98S‐101S. [DOI] [PubMed] [Google Scholar]
Persson 1996 {published data only}
- Persson B, Stimpel M. Evaluation of the antihypertensive efficacy and tolerability of moexipril, a new ACE inhibitor, compared to hydrochlorothiazide in elderly patients. European Journal of Clinical Pharmacology 1996;50:259‐64. [DOI] [PubMed] [Google Scholar]
Pittrow 1997 {published data only}
- Pittrow DB, Antlsperger A, Welzel D, Wambach G, Schardt W, Weldinger G. Evaluation of the efficacy and tolerability of a low‐dose combination of isradipine and spirapril in the first‐line treatment of mild to moderate essential hypertension. Cardiovascular Drugs and Therapy 1997;11(5):619‐27. [DOI] [PubMed] [Google Scholar]
Pizarro 1996 {published data only}
- Pizarro M, Lima J, Domingues J, Gouveia AC, Monteiro A, Carrageta M, Freitas AF. Antihypertensive effect of fosinopril in mild hypertension [Efeito anti‐hipertensor do fosinopril na hipertensao arterial ligeira]. Revista Portuguesa de Cardiologia 1996;15(6):495‐7,460. [PubMed] [Google Scholar]
Poirier 1991 {published data only}
- Lacourciere Y, Poirier L, Pyzyk M. 2.5 and 5 mg cilazapril once daily compared with placebo in hypertension: A comparative out‐patient study of 24‐hour blood pressure monitoring [2,5 und 5 mg cilazapril einmal taglich verglichen mit plazebo bei hypertonie: Eine vergleichsstudie mit ambulantem 24‐studen‐monitoring]. Cardiology 1993;82(Suppl 2):78‐82. [DOI] [PubMed] [Google Scholar]
- Poirier L, Pyzyk M, Provencher P, Lacourciere Y. Comparative effects of 2.5 and 5 mg cilazapril versus placebo on daily blood pressure load. American Journal of Hypertension 1991;4(11):913‐5. [DOI] [PubMed] [Google Scholar]
Pool 1990 {published data only}
- Pool JL. Antihypertensive effect of fosinopril, a new angiotensin converting enzyme inhibitor: Findings of the fosinopril study group II. Clinical Therapeutics 1990;12(6):520‐33. [PubMed] [Google Scholar]
Pool 1997 {published data only}
- Pool JL, Cushman WC, Saini RK, Nwachuku CE, Battikha JP. Use of the factorial design and quadratic response surface models to evaluate the fosinopril and hydrochlorothiazide combination therapy in hypertension. American Journal of Hypertension 1997;10(1):117‐23. [DOI] [PubMed] [Google Scholar]
Pool 2001 {published data only}
- Pool J, Kaihlanen P, Lewis G, Ginsberg D, Oparil S, Glazer R, Messerli FH. Once‐daily treatment of patients with hypertension: a placebo‐controlled study of amlodipine and benazepril vs amlodipine or benazepril alone. Journal of Human Hypertension 2001;15(7):495‐8. [DOI] [PubMed] [Google Scholar]
Pordy 1994 {published data only}
- Pordy RC. Cilazapril plus hydrochlorothiazide: Improved efficacy without reduced safety in mild to moderate hypertension. Cardiology 1994;85(5):311‐22. [DOI] [PubMed] [Google Scholar]
Prager 1994 {published data only}
- Prager G, Klein P, Schmitt M, Prager R. Antihypertensive efficacy of cilazapril 2.5 and 5.0 mg once‐daily versus placebo on office blood pressure and 24‐hour blood pressure profile. Journal of Cardiovascular Pharmacology 1994;24(Suppl 3):S93‐9. [PubMed] [Google Scholar]
Prichard 2002 {published data only}
- Prichard BN, Jager BA, Luszick JH, Kuster LJ, Verboom CN, Hughes PR, Sauermann W, Kuppers HE. Placebo‐controlled comparison of the efficacy and tolerability of once‐daily moxonidine and enalapril in mild to moderate essential hypertension. Blood Pressure 2002;11(3):166‐72. [DOI] [PubMed] [Google Scholar]
Reimann 1995 {published data only}
- Reimann HJ, Muller M, Trinczek‐Gartner H, Kirchhoff R, Kirchhoff G. ACE inhibition in hypertensive patients with concomitant NSAID therapy [ACE‐hemmung bei patienten mit hypertonie und gleichzeitiger NSAR‐therapie]. Munchener Medizinische Wochenschrift 1995;137(12):187‐91. [Google Scholar]
Roca‐Cusachs 2001 {published data only}
- Roca‐Cusachs A, Torres F, Horas M, Rios J, Calvo G, Delgadillo J, Teran M. Nitrendipine and enalapril combination therapy in mild to moderate hypertension: Assessment of dose‐response relationship by a clinical trial of factorial design. Journal of Cardiovascular Pharmacology 2001;38(6):840‐9. [DOI] [PubMed] [Google Scholar]
Sassano 1984 {published data only}
- Sassano P, Chatellier G, Alhenc‐Gelas F, Corvol P, Menard J. Antihypertensive effect of enalapril as first‐step treatment of mild and moderate uncomplicated essential hypertension. American Journal of Medicine 1984;77(2A):18‐22. [DOI] [PubMed] [Google Scholar]
Saynavalammi 1988 {published data only}
- Saynavalammi P, Porsti I, Porsti P, Nurmi AK, Seppala E, Manninen V, Vapaatalo H. Effects of the converting enzyme inhibitor quinapril (CI‐906) on blood pressure, renin‐angiotensin system, and prostanoids in essential hypertension. Journal of Cardiovascular Pharmacology 1988;12(1):88‐93. [DOI] [PubMed] [Google Scholar]
Schoenberger 1986 {published data only}
- Schoenberger JA, Wilson DJ. Once‐daily treatment of essential hypertension with captopril. Journal of Clinical Hypertension 1986;2(4):379‐87. [PubMed] [Google Scholar]
Scholze 1998 {published data only}
- Scholze J, Zilles P, Compagnone D. Verapamil SR and trandolapril combination therapy in hypertension ‐ a clinical trial of factorial design. British Journal of Clinical Pharmacology 1998;45(5):491‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Scholze 1999 {published data only}
- Scholze J, Bauer B, Massaro J. Antihypertensive profiles with ascending dose combinations of ramipril and felodipine ER. Clinical and Experimental Hypertension 1999;21(8):1447‐62. [DOI] [PubMed] [Google Scholar]
Simon 1983 {published data only}
- Morioka S, Simon G, Cohn JN. Cardiac and hormonal effects of enalapril in hypertension. Clinical Pharmacology and Therapeutics 1983;34(5):583‐9. [DOI] [PubMed] [Google Scholar]
- Simon G, Morioka S, Snyder DK, Cohn JN. Increased renal plasma flow in long‐term enalapril treatment of hypertension. Clinical Pharmacology and Therapeutics 1983;34(4):459‐65. [DOI] [PubMed] [Google Scholar]
Smith 1998 {published data only}
- Smith DHG, Neutel JM, Morgenstern P. Once‐daily telmisartan compared with enalapril in the treatment of hypertension. Advances in Therapy 1998;15(4):229‐40. [Google Scholar]
Smith 2000 {published data only}
- Smith DHG, Matzek KM, Kempthorne‐Rawson J. Dose response and safety of telmisartan in patients with mild to moderate hypertension. Journal of Clinical Pharmacology 2000;40(12 Pt 1):1380‐90. [PubMed] [Google Scholar]
Trevisan 1995 {published data only}
- Trevisan R, Tiengo A. Effect of low‐dose ramipril on microalbuminuria in normotensive or mild hypertensive non‐insulin‐dependent diabetic patients. American Journal of Hypertension 1995;8(9):876‐83. [DOI] [PubMed] [Google Scholar]
Uusitupa 1996 {published data only}
- Uusitupa M, Korhonen M, Litmanen, Niskanen L, Vaisanen S, Rauramaa R. Effects of moderate salt restriction alone and in combination with cilazapril on office and ambulatory blood pressure. Journal of Human Hypertension 1996;10(5):319‐26. [PubMed] [Google Scholar]
VA Study Group 1984 {published data only}
- Veterans Administration Cooperation Study Group on Antihypertensive Agents. Low‐dose captopril for the treatment of mild to moderate hypertension. Archives of Internal Medicine 1984;144(10):1947‐53. [DOI] [PubMed] [Google Scholar]
- Veterans Administration Cooperative Study Group on Antihypertensive Agents. Racial differences in response to low‐dose captopril are abolished by the addition of hydrochlorothiazide. British Journal of Clinical Pharmacology 1982;14(Suppl 2):97S‐101S. [PMC free article] [PubMed] [Google Scholar]
Vandenburg 1994 {published data only}
- Vandenburg MJ, MacKay EM, Dews I, Pullan T, Brugier S. Dose finding studies with imidapril ‐ a new ACE inhibitor. British Journal of Clinical Pharmacology 1994;37(3):265‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vaur 1998 {published data only}
- Vaur L, Dubroca I, Dutrey‐Dupagne C, Genes N, Chatellier G, Bouvier‐d'Yvoire M, Elkik F, Menard J. Superiority of home blood pressure measurements over office measurements for testing antihypertensive drugs. Blood Pressure Monitoring 1998;3(2):107‐14. [PubMed] [Google Scholar]
Villamil 1987 {published data only}
- Villamil AS, Cairns V, Witte PU, Bertolasi CA. A double‐blind study to compare the efficacy, tolerance and safety of two doses of the angiotensin converting enzyme inhibitor ramipril with placebo. American Journal of Cardiology 1987;59(10):110D‐14D. [DOI] [PubMed] [Google Scholar]
Waeber 1999 {published data only}
- Waeber B, Detry JM, Dahlof B, Puig JG, Gundersen T, Hosie J, Januszewicz W, Lindstrom CJ, Magometschnigg D, Safar M, Tanser P, Toutouzas P. Felodipine‐metoprolol combination tablet: A valuable option to initiate antihypertensive therapy?. American Journal of Hypertension 1999;12(9 Pt 1):915‐20. [DOI] [PubMed] [Google Scholar]
Weinberger 1990 {published data only}
- Gomez HJ. Dose‐response studies with benazepril in mild to moderate hypertension. Clinical Cardiology 1991;14(8 Suppl IV):IV22‐7. [DOI] [PubMed] [Google Scholar]
- Weinberger MH, Black HR, Lasseter KC, Lewis GP, MacLeod CM, Pascual AV, Zager PG, DeSilva J, Gourley LA, Bennett DA, Whalen JJ. Diurnal blood pressure in patients with mild‐to‐moderate hypertension treated with once‐daily benazepril hydrochloride. Clinical Pharmacology and Therapeutics 1990;47(5):608‐17. [DOI] [PubMed] [Google Scholar]
Weir 1995 {published data only}
- Weir MR, Gray JM, Paster R, Saunders E. Differing mechanisms of action of angiotensin‐converting enzyme inhibition in black and white hypertensive patients. Hypertension 1995;26(1):124‐30. [DOI] [PubMed] [Google Scholar]
- Weir MR, Saunders E. Renin status does not predict the anti‐hypertensive response to angiotensin‐converting enzyme inhibition in African‐Americans. Journal of Human Hypertension 1998;12(3):189‐94. [DOI] [PubMed] [Google Scholar]
Whalen 1989 {published data only}
- Gomez HJ. Dose‐response studies with benazepril in mild to moderate hypertension. Clinical Cardiology 1991;14(8 Suppl IV):IV22‐7. [DOI] [PubMed] [Google Scholar]
- Whalen J, Skalky C, DeSilva J, Weber M. Peak and trough effects of 3 once daily dose levels of benazepril in mild‐moderate hypertension. American Journal of Hypertension 1989;2(5 Pt 2):45A. [Google Scholar]
Whelton 1992 {published data only}
- Whelton A, Dunne Jr B, Glazer N, Kostis JB, Miller WE, Rector DJ, Tresznewsky ON. Twenty‐four hour blood pressure effect of once‐daily lisinopril, enalapril, and placebo in patients with mild to moderate hypertension. Journal of Human Hypertension 1992;6(4):325‐31. [PubMed] [Google Scholar]
White 1988 {published data only}
- White WB, McCabe EJ, Hager WD, Schulman P. The effects of the long‐acting angiotensin‐converting enzyme inhibitor cilazapril on casual, exercise, and ambulatory blood pressure. Clinical Pharmacology and Therapeutics 1988;44(2):173‐8. [DOI] [PubMed] [Google Scholar]
White 1995 {published data only}
- White WB, Whelton A, Fox A, Stimpel M, Kaihlanen PM. Tricenter assessment of the efficacy of the ACE inhibitor, moexipril, by ambulatory blood pressure monitoring. Journal of Clinical Pharmacology 1995;35(3):233‐8. [DOI] [PubMed] [Google Scholar]
White 2002 {published data only}
- White WB, Sica DA, Calhoun D, Mansoor GA, Anders RJ. Preventing increases in early‐morning blood pressure, heart rate, and the rate‐pressure product with controlled onset extended release verapamil at bedtime versus enalapril, losartan, and placebo on arising. American Journal of Hypertension 2002;144(4):657‐65. [DOI] [PubMed] [Google Scholar]
Yebes 1993 {published data only}
- Yebes RB. A placebo‐controlled double blind study to evaluate the efficacy of once daily quinapril in patients with mild to moderate hypertension. Philippine Journal of Internal Medicine 1993;31(6):317‐26. [Google Scholar]
Yodfat 1993 {published data only}
- Yodfat Y, Zimilchman R. Dose‐finding and dose justification of once‐daily cilazapril in combination with hydrochlorothiazide in non‐obese patients with mild‐to‐moderate essential hypertension. Journal of Drug Development 1993;6(3):117‐21. [Google Scholar]
Zamboulis 1996 {published data only}
- Zamboulis C, Karagiannis A, Gotzamani‐Psarrakou A, Deligianni K, Spyridonidis T, Fragos S, Psarrakos K. Effects of fosinopril on renal function in patients with mild to moderate essential hypertension. Clinical Drug Investigation 1996;12(5):251‐8. [Google Scholar]
References to studies excluded from this review
Bainbridge 1993 {published data only}
- Bainbridge AD, MacFadyen RJ, Stark S, Lees KR, Reid JL. The antihypertensive efficacy and tolerability of a low dose combination of ramipril and felodipine ER in mild to moderate essential hypertension. British Journal of Clinical Pharmacology 1993;36(4):323‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bakris 2002 {published data only}
- Bakris G, Sica D, Ram V, Fagan T, Vaitkus PT, Anders RJ. A comparative trial of controlled‐onset, extended‐release verapamil, enalapril, and losartan on blood pressure and heart rate changes. American Journal of Hypertension 2002;15(1 I):53‐7. [DOI] [PubMed] [Google Scholar]
Beaulieu 1993 {published data only}
- Beaulieu M, Lacourciere Y, Cleroux J. Unchanged neurogenic vasoconstrictor response after exercise during angiotensin converting enzyme inhibition with fosinopril. American Journal of Hypertension 1994;7(8):763‐6. [DOI] [PubMed] [Google Scholar]
- Beaulieu M, Nadeau A, Lacourciere Y, Cleroux J. Post‐exercise reduction in blood pressure in hypertensive subjects: Effects of angiotensin converting enzyme inhibition. British Journal of Clinical Pharmacology 1993;36(4):331‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bergstrand 1985 {published data only}
- Bergstrand R, Herlitz H, Johansson S, Berglund G, Vedin A, Wilhelmsson C, et al. Effective dose range of enalapril in mild to moderate essential hypertension. British Journal of Clinical Pharmacology 1985;19(5):605‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bohlen 1996 {published data only}
- Bohlen L, Bienz R, Doser M, Papiri M, Shaw S, Riesen W, et al. Metabolic neutrality of perindopril: focus on insulin sensitivity in overweight patients with essential hypertension. Journal of Cardiovascular Pharmacology 1996;27(6):770‐6. [DOI] [PubMed] [Google Scholar]
Canter 1994 {published data only}
- Canter D, Frank GJ, Knapp LE, Phelps M, Quade M, Texter M. Quinapril and hydrochlorothiazide combination for control of hypertension: assessment by factorial design. Quinapril Investigator Group [see comments]. Journal of Human Hypertension 1994;8(3):155‐62. [PubMed] [Google Scholar]
Canter 1994a {published data only}
- Canter DA, Texter MJ, McLain RW. Ambulatory blood pressure monitoring can play an integral role in patient selection, dosage adjustment and efficacy assessment in clinical trials of antihypertensive agents. Journal of Hypertension ‐ Supplement 1994;12(7):S33‐8. [PubMed] [Google Scholar]
Cleroux 1994 {published data only}
- Cleroux J, Beaulieu M, Kouame N, Lacourciere Y. Comparative effects of quinapril, atenolol, and verapamil on blood pressure and forearm hemodynamics during handgrip exercise. American Journal of Hypertension 1994;7(6):566‐70. [DOI] [PubMed] [Google Scholar]
Cuspidi 1997 {published data only}
- Cuspidi C, Lonati L, Sampieri L, Leonetti G, Muiesan ML, Agabiti‐Rosei E, et al. Lack of effect of short‐term lisinopril administration on left ventricular filling dynamics in hypertensive patients with diastolic dysfunction. Blood Pressure 1997;6(5):307‐12. [DOI] [PubMed] [Google Scholar]
Duprez 1986 {published data only}
- Duprez D, Clement DL. Vasodilator effects of enalapril in patients with arterial hypertension. Acta Cardiologica 1986;41(5):359‐64. [PubMed] [Google Scholar]
Fagard 2001 {published data only}
- Fagard R, Lijnen P, Pardaens K, Thijs L, Vinck W. A randomised, placebo‐controlled, double‐blind, crossover study of losartan and enalapril in patients with essential hypertension. Journal of Human Hypertension 2001;15(3):161‐7. [DOI] [PubMed] [Google Scholar]
Gall 1992 {published data only}
- Gall MA, Rossing P, Skott P, Hommel E, Mathiesen ER, Gerdes LU, et al. Placebo‐controlled comparison of captopril, metoprolol, and hydrochlorothiazide therapy in non‐insulin‐dependent diabetic patients with primary hypertension. American Journal of Hypertension 1992;5(5 Pt 1):257‐65. [DOI] [PubMed] [Google Scholar]
Gans 1993 {published data only}
- Gans RO, Stehouwer CD, Bilo HJ, Goggin T, Kraaij CJ, Donker AJ, et al. Effect of cilazapril on glucose tolerance and lipid profile in hypertensive patients with non‐insulin‐dependent diabetes mellitus. Netherlands Journal of Medicine 1993;43(3‐4):163‐73. [PubMed] [Google Scholar]
Gleerup 1996 {published data only}
- Gleerup G, Petersen JR, Mehlsen J, Winther K. Effect of spirapril and hydrochlorothiazide on platelet function and euglobulin clot lysis time in patients with mild hypertension. Angiology 1996;47(10):951‐5. [DOI] [PubMed] [Google Scholar]
Guitard 1994a {published data only}
- Guitard C, Alvisi V, Maibach E, Franck J, Cocco G, Boxho G, et al. Placebo‐controlled comparison of spirapril at 6, 12 and 24 mg/day in mild to severe essential hypertension. Blood Pressure 1994;Supplement. 2:81‐7. [PubMed] [Google Scholar]
Gupta 1990 {published data only}
- Gupta RK, Kjeldsen SE, Krause L, Kneisley J, Posvar E, Weder AB, et al. Hemodynamic effects of quinapril, a novel angiotensin‐converting enzyme inhibitor. Clinical Pharmacology & Therapeutics 1990;48(1):41‐9. [DOI] [PubMed] [Google Scholar]
- Gupta RK, Kjeldsen SE, Motley E, Weder AB, Zweifler AJ, Julius S. Platelet function during antihypertensive treatment with quinapril, a novel angiotensin converting enzyme inhibitor. Journal of Cardiovascular Pharmacology 1991;17(1):13‐9. [DOI] [PubMed] [Google Scholar]
Homuth 1993a {published data only}
- Homuth V, Faulhaber HD, Loose U, Loffler K, Luft FC. Usefulness of piretanide plus ramipril for systemic hypertension: a multicenter trial. American Journal of Cardiology 1993;72(9):666‐71. [DOI] [PubMed] [Google Scholar]
Hu 1999 {published data only}
- Hu Y, Zhu J. Quality of life of patients with mild hypertension treated with captopril: A randomized double‐blind placebo‐controlled clinical trial. Chinese Medical Journal 1999;112(4):302‐7. [PubMed] [Google Scholar]
Kahan 1999 {published data only}
- Kahan T, Eliasson K. The influence of long‐term ACE inhibitor treatment on circulatory responses to stress in human hypertension. American Journal of Hypertension 1999;12(12 I):1188‐94. [DOI] [PubMed] [Google Scholar]
Karlberg 1987 {published data only}
- Karlberg BE, Lindstrom T, Rosenqvist U, Ohman KP. Efficacy, tolerance and hormonal effects of a new oral angiotensin converting enzyme inhibitor, ramipril (HOE 498), in mild to moderate primary hypertension. American Journal of Cardiology 1987;59(10):104D‐9D. [DOI] [PubMed] [Google Scholar]
Kjeldsen 1992 {published data only}
- Kjeldsen SE, Gupta RK, Krause L, Weder AB, Julius S. Does blood pressure reduction necessarily compromise cardiac function or renal hemodynamics? Effects of the angiotensin‐converting enzyme inhibitor quinapril. American Heart Journal 1992;123(5):1433‐8. [DOI] [PubMed] [Google Scholar]
Lacourciere 1999 {published data only}
- Lacourciere Y, Bittar N, Blanchard E, Kilpatrick FW, Schumacher D, Chappel C, et al. The incidence of cough: A comparison of lisinopril, placebo and telmisartan, a novel angiotensin II antagonist. International Journal of Clinical Practice 1999;53(2):99‐103. [PubMed] [Google Scholar]
Lavezzaro 1990 {published data only}
- Lavezzaro G, Ladetto PE, Valente M, Stramignoni D, Zanna C, Assogna G, et al. Ketanserin and captopril interaction in the treatment of essential hypertensives. Cardiovascular Drugs & Therapy 1990;4(SUPPL. 1):119‐22. [DOI] [PubMed] [Google Scholar]
Leonetti 1991 {published data only}
- Leonetti G, Mazzola C, Pasotti C, Angioni L, Vaccarella A, Capra A, et al. Treatment of hypertension in the elderly: Effects on blood pressure, heart rate, and physical fitness. American Journal of Medicine 1991;90(SUPPL.3A):12S‐3S. [DOI] [PubMed] [Google Scholar]
Littler 1990 {published data only}
- Littler WA, West JW. Twenty‐four hour action of ACE inhibitors. Journal of Human Hypertension 1990;4(SUPPL. 4):13‐6. [PubMed] [Google Scholar]
Louis 1992 {published data only}
- Louis WJ, Workman BS, Conway EL, Worland P, Rowley K, Drummer O, et al. Single‐dose and steady‐state pharmacokinetics and pharmacodynamics of perindopril in hypertensive subjects. Journal of Cardiovascular Pharmacology 1992;20(3):505‐11. [DOI] [PubMed] [Google Scholar]
Miyajima 1999 {published data only}
- Miyajima E, Shigemasa T, Yamada Y, Tochikubo O, Ishii M. Angiotensin II blunts, while an angiotensin‐converting enzyme inhibitor augments, reflex sympathetic inhibition in humans. Clinical & Experimental Pharmacology & Physiology 1999;26(10):797‐802. [DOI] [PubMed] [Google Scholar]
Morgan 2001 {published data only}
- Morgan TO, Anderson AI, MacInnis RJ. ACE inhibitors, beta‐blockers, calcium blockers, and diuretics for the control of systolic hypertension. American Journal of Hypertension 2001;14(3):241‐7. [DOI] [PubMed] [Google Scholar]
Petersen 1996 {published data only}
- Petersen JR, Drabaek H, Gleerup G, Mehlsen J, Petersen LJ, Winther K. ACE inhibition with spirapril improves diastolic function at rest independent of vasodilation during treatment with spirapril in mild to moderate hypertension. Angiology 1996;47(3):233‐40. [DOI] [PubMed] [Google Scholar]
Petrie 2000 {published data only}
- Petrie JR, Morris AD, Ueda S, Small M, Donnelly R, Connell JM, et al. Trandolapril does not improve insulin sensitivity in patients with hypertension and type 2 diabetes: a double‐blind, placebo‐controlled crossover trial. Journal of Clinical Endocrinology & Metabolism 2000;85(5):1882‐9. [DOI] [PubMed] [Google Scholar]
Petrov 2001 {published data only}
- Petrov VV, Fagard RH, Lijnen PJ. T‐lymphocyte and plasma angiotensin‐converting enzyme activity during enalapril and losartan administration in humans. Journal of Cardiovascular Pharmacology 2001;38(4):578‐83. [DOI] [PubMed] [Google Scholar]
Plouin 1991 {published data only}
- Plouin PF, Battaglia C, Alhenc‐Gelas F, Corvol P. Are angiotensin converting enzyme inhibition and aldosterone antagonism equivalent in hypertensive patients over fifty?. American Journal of Hypertension 1991;4(4 Pt 1):356‐62. [DOI] [PubMed] [Google Scholar]
Pritchard 1996 {published data only}
- Pritchard G, Lyons D, Webster J, Petrie JC, MacDonald TM. Do trandolapril and indomethacin influence renal function and renal functional reserve in hypertensive patients?. British Journal of Clinical Pharmacology 1997;44(2):145‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pritchard G, Lyons D, Webster J, Petrie JC, MacDonald TM. Indomethacin does not attenuate the hypotensive effect of trandolapril. Journal of Human Hypertension 1996;10(11):763‐7. [PubMed] [Google Scholar]
Reisin 1997 {published data only}
- Reisin E, Weir MR, Falkner B, Hutchinson HG, Anzalone DA, Tuck ML. Lisinopril versus hydrochlorothiazide in obese hypertensive patients: a multicenter placebo‐controlled trial. Treatment in Obese Patients With Hypertension (TROPHY) Study Group. Hypertension 1997;30(1 Pt 1):140‐5. [DOI] [PubMed] [Google Scholar]
Salvetti 1987 {published data only}
- Salvetti A, Innocenti PF, Iardella M, Pambianco F, Saba GC, Rossetti M, et al. Captopril and nifedipine interactions in the treatment of essential hypertensives: a crossover study. Journal of Hypertension ‐ Supplement 1987;5(4):S139‐42. [DOI] [PubMed] [Google Scholar]
Salvetti 1988 {published data only}
- Salvetti A, Circo A, Raciti S, Gulizia M, Cardillo R, Miceli S, et al. Captopril at 50 mg as well as at 100 mg once a day reduces blood pressure for up to 24 h: a double‐blind randomized crossover study in mild to moderate hypertensives. Journal of Hypertension ‐ Supplement 1988;6(4):S666‐8. [DOI] [PubMed] [Google Scholar]
Salvetti 1989 {published data only}
- Salvetti A, Arzilli F. Chronic dose‐response curve of enalapril in essential hypertensives. An Italian multicenter study. American Journal of Hypertension 1989;2(5 Pt 1):352‐4. [DOI] [PubMed] [Google Scholar]
Samuelsson 1992 {published data only}
- Samuelsson O, Hedner T, Ljungman S, Herlitz H, Widgren B, Pennert K. A comparative study of lisinopril and atenolol on low degree urinary albumin excretion, renal function and haemodynamics in uncomplicated, primary hypertension. European Journal of Clinical Pharmacology 1992;43(5):469‐75. [DOI] [PubMed] [Google Scholar]
Sassano 1984a {published data only}
- Sassano P, Chatellier G, Amiot AM, Alhenc‐Gelas F, Corvol P, Menard J. A double‐blind randomized evaluation of converting enzyme inhibition as the first‐step treatment of mild to moderate hypertension. Journal of Hypertension ‐ Supplement 1984;2(2):S75‐80. [PubMed] [Google Scholar]
Scholze 1993 {published data only}
- Scholze J, Breitstadt A, Cairns V, Bauer B, Bender N, Priestley C, et al. Short report: ramipril and hydrochlorothiazide combination therapy in hypertension: a clinical trial of factorial design. The East Germany Collaborative Trial Group. Journal of Hypertension 1993;11(2):217‐21. [DOI] [PubMed] [Google Scholar]
Thurig 1995 {published data only}
- Thurig C, Bohlen L, Schneider M, Courten M, Shaw SG, Riesen W, et al. Lisinopril is neutral to insulin sensitivity and serum lipoproteins in essential hypertensive patients. European Journal of Clinical Pharmacology 1995;49(1‐2):21‐6. [DOI] [PubMed] [Google Scholar]
Tomei 1992 {published data only}
- Tomei R, Rossi L, Carbonieri E, Franceschini L, Molon G, Zardini P. Antihypertensive effect of lisinopril assessed by 24‐hour ambulatory monitoring: a double‐blind, placebo‐controlled, cross‐over study. Journal of Cardiovascular Pharmacology 1992;19(6):911‐4. [DOI] [PubMed] [Google Scholar]
Wiggam 1998 {published data only}
- Wiggam MI, Hunter SJ, Atkinson AB, Ennis CN, Henry JS, Browne JN, et al. Captopril does not improve insulin action in essential hypertension: a double‐blind placebo‐controlled study. Journal of Hypertension 1998;16(11):1651‐7. [DOI] [PubMed] [Google Scholar]
Wilkins 1983 {published data only}
- Wilkins LH, Dustan HP, Walker JF, Oparil S. Enalapril in low‐renin essential hypertension. Clinical Pharmacology & Therapeutics 1983;34(3):297‐302. [DOI] [PubMed] [Google Scholar]
Wing 1987 {published data only}
- Wing LM, Chalmers JP, West MJ, Bune AJ, Russell AE, Elliott JM, et al. Treatment of hypertension with enalapril and hydrochlorothiazide or enalapril and atenolol: contrasts in hypotensive interactions. Journal of Hypertension ‐ Supplement 1987;5(5):S603‐6. [PubMed] [Google Scholar]
Wing 1988 {published data only}
- Wing LM, Chalmers JP, West MJ, Russell AE, Morris MJ, Cain MD, et al. Enalapril and atenolol in essential hypertension: attenuation of hypotensive effects in combination. Clinical & Experimental Hypertension ‐ Part A, Theory & Practice 1988;10(1):119‐33. [DOI] [PubMed] [Google Scholar]
Youssef 1993 {published data only}
- Youssef S, Osman L, Sabbour MS. Serum lipoprotein profile under different antihypertensive therapy. Cardiovascular Risk Factors 1993;3(2):107‐11. [PubMed] [Google Scholar]
Zanchetti 2001 {published data only}
- Zanchetti A, Omboni S. Comparison of candesartan versus enalapril in essential hypertension. Italian Candesartan Study Group. American Journal of Hypertension 2001;14(2):129‐34. [DOI] [PubMed] [Google Scholar]
Additional references
Bucher 1997
- Bucher HC, Guyatt GH, Griffith LE, Walter D. The results of direct and indirect treatment comparisons in meta‐analysis of randomized controlled trials. Journal of Clinical Epidemiology 1997;50(6):683‐91. [DOI] [PubMed] [Google Scholar]
Cochrane Handbook
- Sterne JAC, Egger M, Moher D (editors). Chapter 10: Addressing reporting biases. In: Higgins JPT, Green S editor(s). Cochrane Handbook for Systematic Reviews of Intervention. The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org, Version 5.0.0 (updated February 2008). [Google Scholar]
Heran 2002
- Heran BS, Jauca CD, Wright JM. Development of an optimal search strategy for finding trials demonstrating ACE inhibitor blood pressure lowering efficacy. 10th International Cochran Colloquium, Stavenger, Norway 2002.
Jadad 1996
- 88.Jadad AR, Moore RA, Carrol D, et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary?. Controlled Clinical Trials 1996;17:1‐12. [DOI] [PubMed] [Google Scholar]
Song 2003
- Song F, Altman DG, Glenny AM Deeks JJ. Validity of indirect comparison for estimating efficacy of competing interventions: emperical evidence from published meta‐analyses. British Medical Journal 2003;326:472‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO‐ICTRP
- World Health Organization. International Clinical Trials Registry Platform (ICTRP). Available from: http://www.who.int/ictrp/en 2006 [cited 2008 Feb 29].


