Abstract
Purpose
Given the increased risk of accidents in patients with attention deficit and hyperactivity disorder (ADHD) or maternal anxiety/depression, we aimed to investigate the frequency of the two diseases in children with penetrating eye injury (PEI).
Methods
Altogether 79 children, 39 with PEIs and 40 healthy individuals (control group), aged 5–15 years, underwent a complete ophthalmologic examination. Afterwards, schedule for affective disorders and schizophrenia for school-aged children was conducted to assess the psychiatric diagnosis of all children. Turgay diagnostic and statistical manual of mental disorders (DSM-IV)-based child and adolescent behavior disorders screening and rating scale (T-DSM-IV-S) was filled by parents to evaluate the severity of ADHD symptoms. The depression and anxiety levels of mothers of each group were evaluated by two self-report measures: the Beck depression scale and the state-trait anxiety inventory (STAI), respectively. Data were analyzed by IBM SPSS version 22.0. The Chi-square and Fisher's exact test were used to determine whether there is a significant difference between qualitative variables while independent sample t and Mann-Whitney U tests to compare quantitative variables.
Results
The only diagnostic difference was a significantly higher frequency of ADHD among patients with PEIs (48.7% in PEI vs. 17.5% in control group, χ2 = 7.359, p = 0.007). The total scores of the T-DSM-IV-S (attention subscale U = 418.000, p = 0.006; hyperactivity subscale U = 472.000, p = 0.022) and maternal state-trait anxiety inventory (maternal STAI-state U = 243.000, p = 0.003; maternal STAI-trait U = 298.000, p = 0.021) were significantly higher in the PEI group than in control group. In logistic regression, children with PEI had a tendency to have a 3.5-fold increased risk for ADHD (OR = 3.538, CI = 0.960–13.039, p = 0.058).
Conclusion
ADHD was detected almost 1 in 2 children with PEIs. Besides, the maternal anxiety level was significantly higher in the PEI group than in the control group. This association should be further explored via a future prospective longitudinal study. Since a proper treatment of ADHD in children and anxiety treatment in mothers may prevent vision loss following PEIs in children.
Keywords: Attention deficit and hyperactivity disorder, Child, Ocular trauma, Penetrating eye injury, Maternal anxiety
Introduction
Attention deficit and hyperactivity disorder (ADHD) is a neurodevelopmental psychiatric disorder, which is characterized by inattention and/or hyperactivity-impulsivity. Although the prevalence of ADHD is about 5% in most cultures, it is estimated to be more common in Turkey, approximately 12.7%, than those detected in Western population.1,2
Children with ADHD have an elevated risk for various injuries.3, 4, 5 A recent meta-analysis has reported that ADHD is associated with a 1.96-fold increased risk of injury.6 The most common injuries in ADHD are sprains and strains of joints; open wounds of head, neck and trunk, and upper/lower limbs; and fractures of upper/lower limb.7,8 In addition, severe injuries (e.g. fractures of skull, neck and trunk and intracranial hemorrhage) are more strongly associated with ADHD than less severe ones.7
Although the incidence of ocular injuries is about 650/100,000 among pediatric population,9 ocular injuries are of the utmost important factor leading to acquired unilateral blindness in this population.10,11 Penetrating eye injuries (PEIs) are the second leading cause of pediatric ocular injuries.12 PEIs have poor prognosis since they usually render visual impairment and require surgery.12 Surprisingly, very limited research to date has focused on ADHD in pediatric PEIs. Bayar et al.13 presented the first and only data which underlined a possible association between PEIs and ADHD. However, they assessed ADHD by using Conner's parent rating scale and they did not report the prevalence of ADHD or other psychiatric disorders in pediatric PEIs. According to National Institute for Health and Care Excellence guideline for ADHD, the diagnosis of ADHD should not be made solely on the basis of a rating scale.14 This is why in our study we used schedule for affective disorders and schizophrenia for school aged children, present and lifetime version (K-SADS-PL) that is an established semi-structured interview, which has good validity for ADHD and is effective for diagnosing major childhood psychiatric disorders.15
In addition to ADHD, depression/anxiety symptoms in mothers are pertinent to an increased risk of injury in their children.16,17 In a cohort study, ascending of 1 point in maternal depressive symptoms was associated with 4% increased risk of injury.18 Besides, elevated risk of child poisoning, fractures, and burns were reported during maternal depression/anxiety episodes in a longitudinal study recruited over 200,000 mother-child pairs from England.16
To the best of our knowledge, there is no study investigating association between PEIs, ADHD, and the maternal anxiety/depression levels. The first aim of the current research was to detect the frequency of ADHD and other psychiatric disorders in children with PEIs. The second aim was to explore the anxiety and depression levels of the mothers of these children.
Methods
Participants
Thirty-nine children aged between 6 and 15 years who admitted to department of ophthalmology, Ege University School of Medicine, Turkey because of PEIs between January 2014 and June 2017 were recruited. Forty children aged between 5 and 15 years who had never experienced PEIs but applied to the ophthalmology outpatient clinic due to refractive error, conjunctivitis, or routine eye examination were recruited as a control group. Children with intellectual disability, autism spectrum disorder, or eye injuries completely due to external factors (i.e., traffic accidents) were excluded. Patients were verbally informed, and written informed consent was obtained from the parents. This research is conducted in accordance with the Declaration of Helsinki. Clinical researches ethical committee approved the study (17–10/1).
Assessment and materials
All patients underwent a complete ophthalmologic examination as best corrected visual acuity (BCVA), anterior and posterior segment evaluation. The cause of PEIs, severity of injuries, initial and final BCVA were obtained from hospital records and parents. “The initial BCVA” was described as BCVA immediately after PEIs before ocular surgery. “The final BCVA” was defined as last BCVA after ocular surgery. Pediatric penetrating ocular trauma score (POTS) was calculated for each child with the history of PEIs according to Acar et al.'s19 study. Patients were divided into five groups based on POTS. A higher score of POTS (total 100) is related to better outcome19: Group 1, <45 points; Group 2, 46–64 points; Group 3, 65–79 points; Group 4, 80–89 points; Group 5, 90–100 points.
After ophthalmic examination, the PEI and control groups were referred to the department of child and adolescence psychiatry clinic, Ege University School of Medicine. The characteristics of children and family, i.e. age, gender, early risk factors for ADHD (preterm birth, low birth weight, prenatal exposure to drugs, nicotine, alcohol, head injury, and parental mental health issues), parents’ educational level, and the history of ADHD in family, were assessed by a socio-demographic form that was based on ADHD child evaluation semi structural interview.20 Afterwards, K-SADS-PL was conducted to assess the psychiatric diagnosis of all the children. One of the authors (Ozbaran B) appraised each patient according to the diagnostic and statistical manual of mental disorders, fifth edition (DSM-5). Patients were re-evaluated at a consensus meeting in case of dissidence between diagnosis of K-SADS-PL and the assessment of the author. Turgay diagnostic and statistical manual of mental disorders fourth edition (DSM-IV) based child and adolescent behavior disorders screening and rating scale (T-DSM-IV-S, Supplementary data 1) was filled by parents to assess the severity of ADHD symptoms.
The depression and anxiety levels of the mothers of all the children were evaluated by self-report measures: the Beck depression scale (Supplementary data 2) and the state-trait anxiety inventory (STAI, Supplementary data 3 and 4), respectively.
K-SADS-PL
The K-SADS-PL is a semi-structured interview to determine psychopathology in children and adolescents with regard to the DSM-IV-text revision criteria.15 The Turkish adaptation study was published by Gökler et al.21 Combination of answers and examination of child or adolescent, parents and physician leads to decision of the presence and severity of symptoms.
T-DSM-IV-S
This scale was developed by Turgay in 1994 and Turkish validation and reliability were determined by Ercan et al.22 in 2001. The T-DSM-IV-S is based on the DSM-IV diagnostic criteria, and assesses hyperactivity-impulsivity (9 items), inattention (9 items), opposition-defiance (8 items), and conduct disorder (15 items). The symptoms are scored by assigning a severity estimate for each symptom on a 4-point Likert-type scale (namely, 0 = not at all; 1 = just a little; 2 = quite a bit; and 3 = very much). Subscale scores on the T-DSM-IV-S are calculated by summing the scores on the items of each subscale.
Self-reports of the anxiety and depression levels of the mothers
The maternal anxiety and depression levels were evaluated via two self-report measures: the Beck depression scale and STAI, respectively. The Beck depression scale is a widely used instrument consisting of 21 symptoms or attitudes commonly seen in patients suffering from depression (e.g. sadness, negative self-concept, sleep and appetite disturbances). The symptoms are rated from ‘0’ to ‘3’ in intensity. This test was developed and revised by Beck and Steer in 1987, and adapted to Turkish by Hisli.23,24 The STAI is a 20-item self-report rating scale for measuring state and trait of anxiety. The state anxiety scale requires people to describe how they feel at the moment, and increases in response to situational stress, and declines under relaxed conditions; while the trait anxiety scale asks people to describe how they generally feel, and reflects relatively stable individual differences in anxiety proneness that are impervious to situational stress. The items are rated on a scale of 1–4. Total scores range from 20 to 80. STAI was developed by Spielberg et al.29 and Turkish edition was adapted by Le Compte and Oner.25
Statistical analysis
Descriptive statistics including mean, standard deviation (SD), frequencies, ratio and group statistics were conducted. The Chi-square test and Fisher's exact test were used to determine whether there is a significant difference between qualitative variables (i.e., gender/early risk factors for ADHD, history of ADHD in family, and diagnosis of psychiatric disorders). Independent sample t and Mann-Whitney U tests were used to compare quantitative variables (i.e., age, maternal/paternal education level, the sub-scores of T-DSM-IV-S) between control group and PEI patients in the case of normal and abnormal distribution, respectively. Spearman's correlation analysis was utilized to examine correlations among the POTS, the subscales of T-DSM-IV-S, Beck depression scale, and STAI. Logistic regression analysis was applied to determine the factors associated with PEIs.
Data were analyzed by IBM SPSS version 22.0 for Mac. Statistically significance was determined as p < 0.05 at the 95% confidence interval (CI), which were calculated with upper and lower limits.
Results
Socio-demographic and clinical characteristics
This study included 39 children with PEIs and 40 healthy volunteers (control group). The groups did not differ in age or gender (Table 1, Table 2). Parents’ educational levels were significantly lower in PEI group than in control group (maternal education level U = 127.000, p < 0.001; paternal education level U = 166.000, p < 0.001). The prevalence of early risk factors for ADHD (χ2 = 8.015, p = 0.005) and the history of ADHD in family (χ2 = 8.015, p = 0.005) were significantly higher in PEIs (Table 2).
Table 1.
Socio-demographic characteristics (quantitative variables) of 79 participants.
| Variables | PEI (n = 39) |
Control (n = 40) |
t/U value | p value | ||
|---|---|---|---|---|---|---|
| Mean (SD) | 95% CI | Mean (SD) | 95% CI | |||
| Age (years) | 10.3 (2.7) | 9.3–11.3 | 9.9 (2.6) | 9.0–10.7 | 1.548 | 0.126a |
| Maternal education level | 5.4 (3.2) | 4.2–6.4 | 12.1 (3.6) | 10.9–13.3 | 127.000 | <0.001b,∗ |
| Paternal education level | 7.5 (3.2) | 6.4–8.6 | 12.8 (2.9) | 11.8–13.8 | 166.000 | <0.001b,∗ |
PEI: penetrating eye injury, SD: standard deviation, CI: confidence interval.
∗Significant difference.
Independent samples t-test.
Mann Whitney U test.
Table 2.
Socio-demographic characteristics (qualitative variables) of 79 participants, n (%).
| Variables | PEI (n = 39) | Control (n = 40) | χ2 | p value |
|---|---|---|---|---|
| Gender | ||||
| Female | 7 (17.9) | 16 (40.0) | 3.646 | 0.056 |
| Male | 32 (82.1) | 24 (60.0) | ||
| Early risk factors | 17 (43.6) | 5 (12.5) | 8.015 | 0.005∗ |
| Preterm birth | 3 (7.7) | 0 (0) | n.a | 0.116 |
| Low birth weight | 3 (7.7) | 2 (5.0) | n.a | 0.675 |
| Prenatal exposure to drugs, alcohol, nicotine | 4 (10.3) | 0 (0) | n.a | 0.055 |
| Head injury | 3 (7.7) | 0 (0) | n.a | 0.116 |
| Parental mental health issues | 13 (33.3) | 5 (12.5) | 3.759 | 0.053 |
| History of ADHD in family | 17 (43.6) | 5 (12.5) | 8.015 | 0.005∗ |
PEI: Penetrating eye injury, n.a: non-applicable, ∗Significant difference.
Ophthalmic assessments of children with PEIs
The first and second most common cause of PEIs were glass (10, 25.6%) and knife injury (8, 20.5%), respectively. Other injury mechanisms included stone (4, 10.3%), thorn (4, 10.3%), pop cap (3, 77%), wood, pencil, iron rod, squib (each 2 cases, 5.1%), needle (1, 2.6%) and unknown (1, 2.6%). Median duration between the date of PEIs and the assessment was 12 (interquartile range = 48.25, min = 1, max = 66) months.
The severity of injury and initial BCVA of 8 children with PEIs were not able to be collected from hospital records. Therefore, the POTS score of these patients was not calculated.
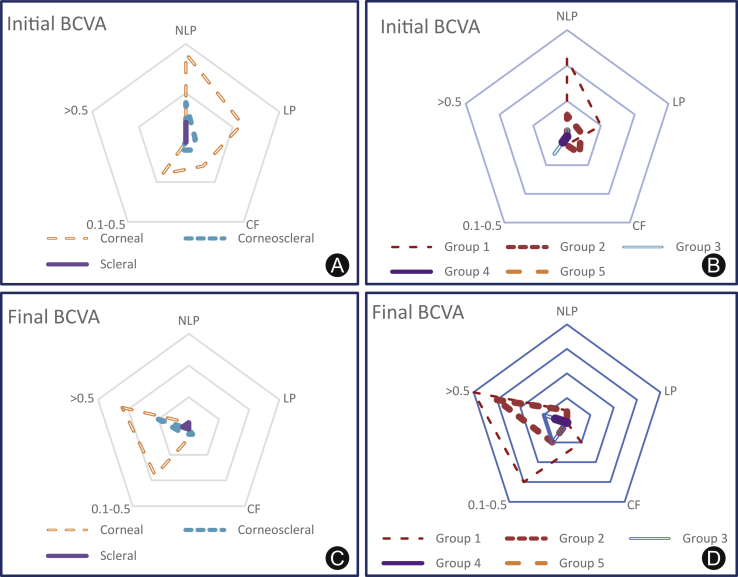
For the 31 PEI patients with complete data, cornea (22, 71.0%) was most frequently involved, followed by corneosclera (7, 22.6%) and sclera (2, 6.5%). The initial BCVA was noted as no light perception (NLP) in 15 (48.4), light perception (LP) to hand motion (HM) in 7 (22.6%), counting fingers (CF) in 4 (12.9%) and Snellen chart 0.1–0.5 in 5 patients (16.1%), which after surgery were improved to NLP in 2 (6.5%); CF in 2 (6.5%); Snellen chart 0.1–0.5 in 10 (32.3%) and Snellen chart ≥0.6 in 17 patients (54.9%) (Fig. 1).
Fig. 1.
Initial and final BCVA according to the location of injury (A and C) and the groups of POTS (B and D). BCVA: best corrected visual acuity, POTS: pediatric ocular trauma scores, NLP: no light perception, LP: light perception, CF: counting fingers, 0.1–0.5 (Snellen chart), >0.5 (Snellen chart).
The results of POTS calculation showed that most PEIs were in Group 1 and none of them was in Group 5. Group 1 had the worst prognosis among all groups, since almost all of the patients had NLP or LP at the initial ophthalmic examination. Moreover, in Group 1, some of the patients still had a 0.1–0.5 visual acuity (Snellen chart) or could only count fingers in spite of the surgery (Fig. 1).
Psychiatric evaluation of the children
The only diagnostic difference between PEI group and control group was a significantly higher proportion of ADHD (χ2 = 7.359, p = 0.007), especially predominantly hyperactive/impulsive presentation among PEIs (p = 0.002, Table 3).
Table 3.
Distribution of psychiatric disorders within groups, n (%).
| Variables | PEI (n = 39) | Control (n = 40) | χ2 | p value |
|---|---|---|---|---|
| Any psychiatric disorder | 26 (66.7) | 10 (25) | 1.813 | 0.178 |
| Comorbid psychiatric disorder | 10 (25.6) | 4 (10) | 2.327 | 0.127 |
| ADHD | 19 (48.7) | 7 (17.5) | 7.359 | 0.007∗ |
| Inattention | 4 (10.3) | 2 (5) | n.a | 0.432 |
| Hyperactivity/Impulsivity | 8 (20.5) | 0 (0) | n.a | 0.002∗ |
| Combine | 7 (17.9) | 5 (12.5) | 0.130 | 0.178 |
| Anxiety disorder | 9 (23.1) | 6 (27.3) | 0.134 | 0.715 |
| Oppositional defiant disorder | 3 (7.7) | 3 (7.5) | n.a | 1.000 |
| Conduct disorder | 1 (2.6) | 0 (0) | n.a | n.a |
| Speech disorder | 3 (7.7) | 1 (2.5) | n.a | 0.359 |
| Specific learning disability | 4 (10.3) | 0 (0) | n.a | 0.055 |
| Post-traumatic stress disorder | 1 (2.6) | 0 (0) | n.a | n.a |
| Obsessive compulsive disorder | 1 (2.6) | 1 (2.5) | n.a | 1.000 |
| Major depressive disorder | 2 (5.1) | 0 (0) | n.a | 0.241 |
| Tic disorder | 1 (2.6) | 2 (5) | n.a | 1.000 |
PEI: Penetrating eye injury, ADHD: attention deficit and hyperactivity disorder, n.a: non applicable.
∗Significant difference.
The attention (U = 418.000, p = 0.006) and hyperactivity subscales (U = 472.000, p = 0.022) of T-DSM-IV-S were significantly higher in PEI group than in control group. No correlation was found between the POTS and the scores of Beck depression scale, STAI, and the subscales of T-DSM-IV-S (all p > 0.05). Mothers of PEIs group had significantly higher STAI-state and STAI-trait scores than those of mothers of control group (p < 0.05) (Table 4). However, no difference was found between the groups in term of maternal Beck depression scale scores (p = 0.393). Moreover, we also compared maternal anxiety levels between mothers of children with ADHD and those mothers with none-ADHD children. Mothers of children with ADHD (mean = 44.3, SD = 8.4) had significantly higher score of STAI-state than mothers of non-ADHD children (mean = 41.3, SD = 5.7) (U = 233.500, p = 0.030). Maternal STAI-trait and Beck depression scale score did not differ between the mothers of children with ADHD and those mothers with non-ADHD children (p > 0.05).
Table 4.
Evaluation of the groups according to ADHD severity and maternal anxiety/depression levels.
| Variables | PEI (n = 39) |
Control (n = 40) |
U value | p value | ||
|---|---|---|---|---|---|---|
| Mean (SD) | CI | Mean (SD) | CI | |||
| T-DSM-IV-S-Attention | 7.8 (7.1) | 5–10.6 | 4.2 (4.3) | 2.7–5.6 | 418.000 | 0.006∗ |
| T-DSM-IV-S-Hyperactivity | 8.5 (8.5) | 5.2–11.8 | 5 (4.7) | 3.5–6.6 | 472.000 | 0.022∗ |
| T-DSM-IV-S-OD | 3.8 (4.4) | 2.1–5.5 | 3.5 (3.9) | 2.2–4.8 | 537.500 | 0.913 |
| T-DSM-IV-S-CD | 0.6 (1.9) | −0.1–1.4 | 0.4 (1.0) | 0.1–0.8 | 501.500 | 0.438 |
| Maternal Beck depression scale | 6.9 (6.8) | 3.8–10 | 6.9 (4.1) | 5.5–8.3 | 363.000 | 0.393 |
| Maternal STAI-state | 44.4 (7.6) | 40.9–47.9 | 40.5 (5.7) | 38.7–42.4 | 243.000 | 0.003∗ |
| Maternal STAI-trait | 46.4 (8.2) | 42.6–50.1 | 42.5 (7.4) | 40.1–44.9 | 298.000 | 0.021∗ |
PEI: Penetrating eye injury, CI: confidence interval, n.a: non applicable, T-DSM-IV-S: Turgay DSM-IV based child and adolescent behavior disorders screening and rating scale, OD: opposition defiance, CD conduct disorder.
∗Significant difference.
Logistic regression analysis was employed to determine the factors associated with PEIs. The binary logistic regression model explained 21.4% of the variance. Children with PEIs had a tendency to have 3.538 fold increased risk for ADHD (OR = 3.538, CI = 0.960–13.039, p = 0.058, Table 5).
Table 5.
Logistic regression analysis to determine the factors associated with PEIs.
| Wald | df | OR | p value | |
|---|---|---|---|---|
| Presence of ADHD | 3.606 | 1 | 3.538 | 0.058 |
| Maternal Beck depression scale | 0.644 | 1 | 0.951 | 0.422 |
| Maternal STAI-state | 1.817 | 1 | 1.053 | 0.366 |
| Maternal STAI-trait | 1.519 | 1 | 1.066 | 0.218 |
PEI: penetrating eye injury, ADHD: attention deficit and hyperactivity disorder; T-DSM-IV-S: Turgay DSM-IV based child and adolescent behavior disorders screening and rating scale, STAI: state-trait anxiety inventory.
Discussion
Ocular injuries are the most important cause of acquired unilateral blindness and monocular visual impairment in the pediatric population.26 Pizzarello et al.27 stated that 90% of all ocular injuries are preventable. Elucidating underlying factors of eye injuries may diminish the incidence of ocular trauma.12 Considering an elevated risk of unintended injuries in ADHD and maternal anxiety/depression, the present cross-sectional study investigated the frequency of ADHD and the level of maternal anxiety/depression in children with PEIs.
Consistent with previous work,13 we found that ADHD was significantly more frequent in PEI group than in control group. Importantly, almost half of children with PEIs had ADHD, specifically predominantly hyperactive/impulsive presentation. Children with PEIs had a significantly higher prevalence of the early risk factors for ADHD and a history of ADHD in their family. According to logistic regression analysis, it was found that children with PEIs had a tendency to have a 3.5-fold increased risk for ADHD. Thus, it seems that PEIs is associated with ADHD in children. Several probable reasons may explain the elevated risk of injuries among children with ADHD. Compared with non-ADHD children, children with ADHD reported having difficulties in anticipating severe consequences of risky behavior.28 Thus, these children are more prone to engage in risky situations. Besides, hyperactivity, impulsivity, being easily distracted, and motor dysfunctions may lead to injuries in children with ADHD.7,28, 29, 30, 31, 32
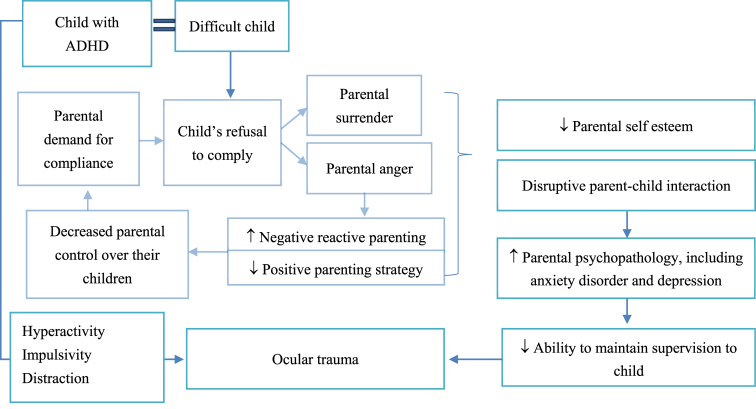
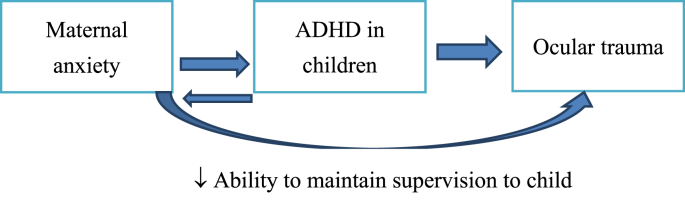
In the current study, higher anxiety level was found in mothers of PEI kids. In the light of the findings of higher maternal anxiety and higher prevalence of ADHD in the PEIs group, we contemplated three theories to explain the link between PEIs, ADHD, and maternal anxiety (Fig. 2, Fig. 3, Fig. 4).
Fig. 2.
Theory 1: ADHD in children may have increased distress/anxiety in mothers. Both ADHD and high maternal anxiety may have caused penetrating ocular trauma.
Fig. 3.
Theory 2: Antenatal maternal anxiety may have caused ADHD. Both ADHD and high anxiety levels of mothers may have led to ocular trauma. ADHD: attention deficit and hyperactivity disorder.
Fig. 4.
Theory 3: ADHD may have increased the risk of PEI in children. The mothers of children with PEI may have become anxious after the trauma of their children. ADHD: attention deficit and hyperactivity disorder.
Theory 1. ADHD in children may have increased anxiety in mothers. Both ADHD-related symptoms in children and high maternal anxiety may cause PEIs (Fig. 2). The symptoms of ADHD in children present a significant challenge for parents and cause disruptive parent-child interaction which can lead to parental psychopathology including depression, anxiety.33,34 In line with this, we found that the anxiety level of the mothers of children with ADHD was significantly higher than those of non-ADHD children. Increased parental mental distress in maternal anxiety/depression is related to decreased ability of mothers to maintain supervision to their children.35 Thus, children whose mothers suffering from depression and anxiety have an increased rate of subsequent unintended injuries.16,36
Theory 2. High anxiety levels of mothers during pregnancy may have caused ADHD in their children (Fig. 3). Prospective longitudinal studies have revealed that children of mothers with high anxiety during 12–22 months of pregnancy have a more clinical diagnosis of ADHD, ADHD symptoms, conduct disorders, and emotional problems.37,38 Both symptoms related to ADHD in children and the lack of supervision of these children due to high anxiety levels of mothers may have led to PEIs.
Theory 3: ADHD may have increased the risk of PEIs in children. The mothers of children who had experienced PEIs may have become anxious after the trauma of their children (Fig. 4). Consistent with this theory, Wesson et al.39 reported a significantly high level of anxiety and depression symptoms in mothers of patients experiencing traumatic injury.
Due to the cross-sectional design of our study, it is hard to decide which theory is the best to explain the relationship between PEIs, ADHD, and maternal anxiety. However, we believe that enlightening the mechanism underlying this relationship can provide important implications for clinical practice. By elucidating causal relationship between ADHD and PEIs, following benefits can be obtained: (1) treatment of ADHD may prevent vision loss due to ocular injuries in children, (2) treatment of ADHD in children with PEIs may hinder repetition of injuries and may prevent further impairments related to ADHD. Comprehending the link between maternal anxiety, PEIs and ADHD can provide implications include the following: (1) monitoring and treating maternal anxiety during pregnancy may prevent ADHD in children, (2) the anxiety level of mothers can be assessed during the routine pediatric visits of their children; and early intervention to maternal anxiety can hinder vision loss because of PEIs. Consequently, a future longitudinal study should be designed to enlighten the link between PEIs, ADHD, and maternal anxiety.
Limitation and strength of our study require consideration. Causing by the rarity of PEIs (the incidence rate is 650/100,000) in children, the limited sample size was a disadvantage of the current study; thus, it is not enough to make generalizations. However, from the comparison of those limited number, we could detect that the prevalence of ADHD was significantly higher in children with PEIs than those that did not have a history of ocular trauma. Besides, the lack of the assessment of maternal depressive/anxiety symptoms in the period when their children had experienced PEIs is another disadvantage of this study. Despite these limitations, this is the first study reporting a possible link between PEIs, ADHD and maternal anxiety. The strength of this research was utilizing two steps diagnostic verification (semi-structured psychiatric interview performed by a qualified child and adolescent psychiatrist and re-appraisal of patients by the author (Ozbaran B) and complete ophthalmologic examination together).
In conclusion, an association between PEIs, ADHD, and maternal anxiety was found in the current study. Identifying the causes and features of PEIs, and taking precautions by education and legislation are of utmost importance in preventing these injuries in children. Thus, this association should be further explored and a prospective longitudinal study should be designed. ADHD is a treatable psychiatric disorder if can be diagnosed properly. Therefore, suitable diagnosis and treatment of ADHD might prevent vision loss due to PEIs in children. If a causal relation can be detected between high maternal anxiety and PEIs, the assessment of the maternal anxiety level during the routine pediatric visits of children might also be useful for preventing ocular injuries.
Funding
Nil.
Ethical Statement
Patients were verbally informed, and written informed consent was obtained from the parents. This research is conducted in accordance with the Declaration of Helsinki. Clinical researches ethical committee approved the study (17–10/1).
Declaration of Competing Interest
The authors declare no conflict of interest.
Footnotes
Peer review under responsibility of Chinese Medical Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.cjtee.2019.11.008.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Association AP . American Psychiatric Association; Arlington, VA: 2013. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®) [Google Scholar]
- 2.Ercan E.S., Bilaç Ö., Özaslan T.U. Is the prevalence of ADHD in Turkish elementary school children really high? Soc Psychiatr Psychiatr Epidemiol. 2015;50:1145–1152. doi: 10.1007/s00127-015-1071-9. [DOI] [PubMed] [Google Scholar]
- 3.Rowe R., Maughan B., Goodman R. Childhood psychiatric disorder and unintentional injury: findings from a national cohort study. J Pediatr Psychol. 2004;29:119–130. doi: 10.1093/jpepsy/jsh015. [DOI] [PubMed] [Google Scholar]
- 4.Pastor P.N., Reuben C.A. Identified attention-deficit/hyperactivity disorder and medically attended, nonfatal injuries: US school-age children, 1997–2002. Ambul Pediatr. 2006;6:38–44. doi: 10.1016/j.ambp.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 5.Kang J., Lin H., Chung S. Attention-deficit/hyperactivity disorder increased the risk of injury: a population-based follow-up study. Acta Paediatr. 2013;102:640–643. doi: 10.1111/apa.12213. [DOI] [PubMed] [Google Scholar]
- 6.Amiri S., Sadeghi-Bazargani H., Nazari S. Attention deficit/hyperactivity disorder and risk of injuries: a systematic review and meta-analysis. J Inj Violence Res. 2017;9:95. doi: 10.5249/jivr.v9i2.858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Merrill R.M., Lyon J.L., Baker R.K. Attention deficit hyperactivity disorder and increased risk of injury. Adv Med Sci. 2009;54:20–26. doi: 10.2478/v10039-009-0022-7. [DOI] [PubMed] [Google Scholar]
- 8.Marcus S.C., Wan G.J., Zhang H.F. Injury among stimulant-treated youth with ADHD. J Atten Disord. 2008;12:64–69. doi: 10.1177/1087054707305168. [DOI] [PubMed] [Google Scholar]
- 9.Bućan K., Matas A., Lovrić J.M. Epidemiology of ocular trauma in children requiring hospital admission: a 16–year retrospective cohort study. J Global Health. 2017;7 doi: 10.7189/jogh.07.010415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liggett P.E., Pince K.J., Barlow W. Ocular trauma in an urban population. Ophthalmology. 1990;97:581–584. doi: 10.1016/s0161-6420(90)32539-3. [DOI] [PubMed] [Google Scholar]
- 11.Brophy M., Sinclair S.A., Hostetler S.G. Pediatric eye injury-related hospitalizations in the United States. Pediatrics. 2006;117:e1263–e1271. doi: 10.1542/peds.2005-1950. [DOI] [PubMed] [Google Scholar]
- 12.MacEwen C., Baines P., Desai P. Eye injuries in children: the current picture. Br J Ophthalmol. 1999;83(8):933–936. doi: 10.1136/bjo.83.8.933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bayar H., Coskun E., Öner V. Association between penetrating eye injuries and attention deficit hyperactivity disorder in children. Br J Ophthalmol. 2015;99:1109–1111. doi: 10.1136/bjophthalmol-2014-306248. [DOI] [PubMed] [Google Scholar]
- 14.National Collaborating Centre for Mental Health (UK) British Psychological Society; Leicester (UK): 2018. Attention Deficit Hyperactivity Disorder: Diagnosis and Management of ADHD in Children, Young People and Adults.http://www.ncbi.nlm.nih.gov/books/NBK493361/ Accessed. [PubMed] [Google Scholar]
- 15.Kaufman J., Birmaher B., Brent D. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 16.Baker R., Kendrick D., Tata L.J. Association between maternal depression and anxiety episodes and rates of childhood injuries: a cohort study from England. Inj Prev. 2017;23:396–402. doi: 10.1136/injuryprev-2016-042294. [DOI] [PubMed] [Google Scholar]
- 17.O'Connor T.G., Davies L., Dunn J. Distribution of accidents, injuries, and illnesses by family type. Pediatrics. 2000;106:e68. doi: 10.1542/peds.106.5.e68. [DOI] [PubMed] [Google Scholar]
- 18.Phelan K., Khoury J., Atherton H. Maternal depression, child behavior, and injury. Inj Prev. 2007;13:403–408. doi: 10.1136/ip.2006.014571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Acar U., Tok O.Y., Acar D.E. A new ocular trauma score in pediatric penetrating eye injuries. Eye. 2011;25:370–374. doi: 10.1038/eye.2010.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Young S. 2015. ADHD Child Evaluation. A diagnostic interview of ADHD in children.www.psychology-services.uk.com [Google Scholar]
- 21.Gökler B., Ünal F., Pehlivantürk B. Reliability and validity of schedule for affective disorders and schizophrenia for school age children-present and lifetime version-Turkish version (K-SADS-PL-T) Turkish J Child Adolesc Ment Health. 2004;11:109–116. [Google Scholar]
- 22.Ercan E.S., Amado S., Somer O. Development of a test battery for the assessment of attention deficit hyperactivity disorder. Turkish J Child Adolesc Ment Health. 2001;8:132–144. [Google Scholar]
- 23.Beck A.T., Steer R.A. Psychological Corporation; San Antonio, TX: 1987. Manual for the Revised Beck Depression Inventory. [Google Scholar]
- 24.Hisli N. A study on the validity of Beck's depression inventory. Psychol J. 1988;6:118–122. [Google Scholar]
- 25.Le Compte W.A., Oner N. Development of the Turkish edition of the state-trait anxiety inventory. Cross Cult Anxiety. 1976;1:51–67. [Google Scholar]
- 26.Jandeck C., Kellner U., Bornfeld N. Open globe injuries in children. Graefes Arch Clin Exp Ophthalmol. 2000;238:420–426. doi: 10.1007/s004170050373. [DOI] [PubMed] [Google Scholar]
- 27.Pizzarello L.D. Ocular trauma: time for action. Ophthalmic Epidemiol. 1998;5:115–116. doi: 10.1076/opep.5.3.115.8366. [DOI] [PubMed] [Google Scholar]
- 28.Farmer J.E., Peterson L. Injury risk factors in children with attention deficit hyperactivity disorder. Health Psychol. 1995;14:325–332. doi: 10.1037/0278-6133.14.4.325. [DOI] [PubMed] [Google Scholar]
- 29.Badger K., Anderson L., Kagan R.J. Attention deficit-hyperactivity disorder in children with burn injuries. J Burn Care Res. 2008;29:724–729. doi: 10.1097/BCR.0b013e31818480e1. [DOI] [PubMed] [Google Scholar]
- 30.DiScala C., Lescohier I., Barthel M. Injuries to children with attention deficit hyperactivity disorder. Pediatrics. 1998;102:1415–1421. doi: 10.1542/peds.102.6.1415. [DOI] [PubMed] [Google Scholar]
- 31.Ghanizadeh A. Small burns among out-patient children and adolescents with attention deficit hyperactivity disorder. Burns. 2008;34:546–548. doi: 10.1016/j.burns.2007.07.015. [DOI] [PubMed] [Google Scholar]
- 32.Tervo R.C., Azuma S., Fogas B. Children with ADHD and motor dysfunction compared with children with ADHD only. Dev Med Child Neurol. 2002;44:383–390. doi: 10.1017/s0012162201002250. [DOI] [PubMed] [Google Scholar]
- 33.Bailey J., Barton B., Vignola A. Coping with Children with ADHD: coping styles of mothers with children with ADHD or challenging behaviors. Early Child Dev Care. 1999;148:35–50. [Google Scholar]
- 34.Lee P., Lin K., Robson D. Parent–child interaction of mothers with depression and their children with ADHD. Res Dev Disabil. 2013;34:656–668. doi: 10.1016/j.ridd.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 35.Schwebel D.C., Brezausek C.M. How do mothers and fathers influence pediatric injury risk in middle childhood? J Pediatr Psychol. 2010;35:806–813. doi: 10.1093/jpepsy/jsp130. [DOI] [PubMed] [Google Scholar]
- 36.Hope S., Deighton J., Micali N. Maternal mental health and childhood injury: evidence from the UK millennium cohort study. Arch Dis Child. 2019;104:268–274. doi: 10.1136/archdischild-2017-313809. [DOI] [PubMed] [Google Scholar]
- 37.Van den Bergh B.R., Marcoen A. High antenatal maternal anxiety is related to ADHD symptoms, externalizing problems, and anxiety in 8- and 9-year-olds. Child Dev. 2004;75:1085–1097. doi: 10.1111/j.1467-8624.2004.00727.x. [DOI] [PubMed] [Google Scholar]
- 38.van den Bergh B.R., Mennes M., Stevens V. ADHD deficit as measured in adolescent boys with a continuous performance task is related to antenatal maternal anxiety. Pediatr Res. 2006;59:78–82. doi: 10.1203/01.pdr.0000191143.75673.52. [DOI] [PubMed] [Google Scholar]
- 39.Wesson D.E., Scorpio R.J., Spence L.J. The physical, psychological, and socioeconomic costs of pediatric trauma. J Trauma. 1992;33:252–255. doi: 10.1097/00005373-199208000-00015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.