Introduction
Radiofrequency catheter ablation of scar-related ventricular tachycardia (VT) has been widely performed as a definitive therapy in patients with structural heart disease.1,2 An epicardial approach may sometimes be required to eliminate epicardial reentrant circuits on the left ventricular (LV) free wall. However, epicardial access can be difficult owing to pericardial adhesions, anticoagulation and/or antiplatelet therapies, extreme obesity, or the risk of bleeding complications based on anatomical backgrounds.3 We report a case of a scar-related monomorphic VT with LV epicardial reentrant circuit that was successfully eliminated by ethanol infusion into a coronary sinus (CS) branch.
Case report
A 69-year-old man with nonischemic cardiomyopathy and preserved LV systolic function was admitted to our hospital for recurrent episodes of a drug-refractory unstable VT that required multiple implantable cardioverter-defibrillator shocks. He previously underwent catheter ablation for a hemodynamic unstable VT and paroxysmal atrial fibrillation. However, the previous bilateral endocardial radiofrequency ablation of the estimated septal VT circuit was unsuccessful. The implantable cardioverter-defibrillator recordings during the recent bouts of tachycardia showed a monomorphic VT with cycle length of 280 ms (Figure 1A). Cardiac ultrasound showed abnormal LV wall motion localized in the basal posterolateral region. He underwent a repeat ablation procedure for the VT, which was refractory to 200 mg of amiodarone. Preparations were made for bipolar ablation and ethanol infusion into the septal branches of the left anterior descending coronary artery in case conventional endocardial unipolar ablation to the septal VT failed. A sustained monomorphic VT with right bundle branch block and superior axis morphology was induced by programmed stimulation during isoproterenol infusion (Figure 1B). However, the hemodynamic instability during the VT precluded the detailed activation mapping and entrainment pacing. The unipolar voltage map during sinus rhythm only demonstrated an isolated low-voltage area in the basal LV posterolateral region that suggested presence of an epicardial VT substrate (Figure 2A). Delayed potentials were also observed in the endocardial low-voltage area.4 However, pacing at this site did not produce a pace-map match to the induced VT. Meanwhile, pace mapping within the posterolateral CS branch matched the VT morphology (Figure 2B). In addition, the activation recorded at the pace-match site in the CS branch during VT preceded QRS onset by 30 ms (Figure 2C). At first, the radiofrequency applications were delivered to the LV endocardium close to the pace-match site, but failed to eliminate the VT (Figure 3A). Although we would normally consider an epicardial ablation first because of risk of myocardial damage from ethanol injection, which is a less targeted approach, we made the decision to perform ethanol ablation to a CS branch because the preprocedural computed tomography had demonstrated marked dilatation of the stomach, raising the concern of stomach injury owing to pericardial centesis. In addition, the patient was under uninterrupted anticoagulation therapy with 15 mg of rivaroxaban for atrial fibrillation, so a repeat procedure after withholding anticoagulants was a possibility, but the urgency of treating the patient’s VT storm was another factor in our decision to proceed. Coronary angiography showed no coronary artery branches in close proximity to the posterolateral CS branch before ethanol infusion. A total of 3 ethanol infusions (1.5 mL, 90 s for each infusion) into the posterolateral CS branch were performed with an over-the-wire balloon for angioplasty (diameter 1.5 mm, length 15 mm) (Figure 3B). Repetitive premature ventricular contractions with the same QRS morphology as that of the VT were observed during ethanol infusion. Ethanol ablation successfully eliminated the VT and no ventricular arrhythmias were inducible after the ablation. The patient remained symptom free and sustained VT of any kind has not been recorded during the 12 months of follow-up after the ablation. Although myocardial damage from the ethanol infusion was a concern, cardiac ultrasound showed no changes in either LV size or function immediately and 6 months after the ethanol ablation. In addition, chest radiographs after the procedure did not show any findings suggestive of left phrenic nerve injury.
Figure 1.
A: Intracardiac electrogram on implantable cardioverter-defibrillator recording showed an initiation of ventricular tachycardia with a cycle length of 280 ms. B: Twelve-lead electrocardiogram (ECG) during atrial pacing showed narrow QRS morphology (left). Meanwhile, 12-lead ECG during sustained monomorphic ventricular tachycardia showed wide QRS morphology with right bundle branch block and superior axis (right).
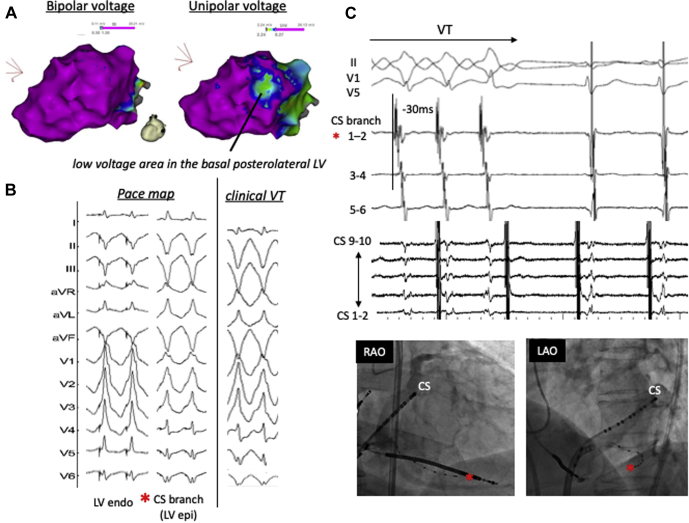
Figure 2.
A: The unipolar voltage map during sinus rhythm showed an isolated low-voltage area in the basal left ventricular (LV) posterolateral region. B: Pace-map match to the clinical ventricular tachycardia (VT) morphology was not observed at the posterolateral LV site with low voltages on endocardial unipolar voltage map but was obtained within a coronary sinus (CS) branch where the earliest ventricular activation during VT was recorded. C: The earliest ventricular activation during VT recorded within a CS branch is shown by a red asterisk, preceding QRS onset by 30 ms.
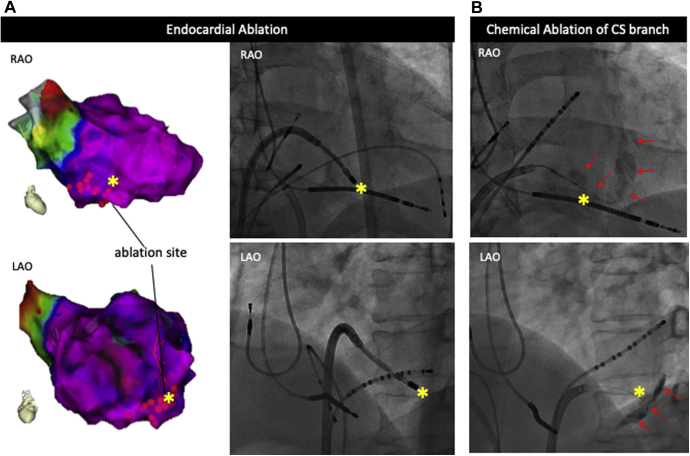
Figure 3.
A: Endocardial ablation in the posterolateral left ventricular region was not successful. B: Ethanol infusion into a posterolateral vein of the coronary sinus (CS) that eliminated an epicardial scar-related ventricular tachycardia circuit produced the ablation lesions, stained by contrast media, as shown by red arrows.
Discussion
Transarterial coronary ethanol ablation (TCEA) has been well investigated in previous reports.5, 6, 7, 8 Intra-arterial injection of ethanol has classically delivered cytotoxic injury through vasculature supplying the target myocardial tissue. TCEA-related complications, such as coronary artery thrombosis, dissection, conduction block, and myocardial infarction, could result in serious injury, especially in patients with LV dysfunction and scar-related VTs. In addition, it might be difficult to localize a terminal arrhythmia-related artery, especially in patients with coronary artery disease due to coronary stenosis. Moreover, the variety of vessel size and flow rate also may affect the cytotoxicity of ethanol, which makes the effects on the target myocardium difficult to predict. In contrast, retrograde coronary venous ethanol ablation (RCVEA) is not well established as a methodology for VT ablation.9, 10, 11 Kreidieh and colleagues9 described the safety and the efficacy of RCVEA in 7 patients who successfully underwent RCVEA for intractable VTs originating from the LV summit (5 patients) and LV posteroseptal (1 patient) and posterolateral regions (1 patient). There were no significant complications except for 1 patient who manifested pericardial and pleural effusion owing to pericardial instrumentation. This methodology should be particularly useful for VT substrate with an intramural origin or proximal to coronary arteries, and for patients in whom an epicardial approach is problematic for other reasons.9, 10, 11
RCVEA has been described as an alternative to TCEA. It overcomes some of the limitations of TCEA and avoids instrumentation of the coronary arteries. In fact, a previous animal study of RCVEA showed less damage to the coronary arteries.12 RCVEA also has an advantage in technical aspects over TCEA because electrophysiologists are familiar with placing mapping catheters in the CS, allowing RCVEA to be performed with relative ease. Although additional investigation with a larger cohort of patients will be required to elucidate the clinical safety and efficacy of RCVEA, this methodology should be selected as a bail-out approach for intractable VTs that fail radiofrequency ablation.
Key Teaching Points.
-
•
Epicardial mapping within coronary sinus branch and unsuccessful endocardial ablation predicted the presence of epicardial reentrant circuit.
-
•
Ethanol infusion to a coronary sinus branch was successfully performed without any complications.
-
•
Chemical ablation with ethanol infusion to a coronary sinus branch eliminated scar-related ventricular tachycardia with left ventricular epicardial reentrant circuit as an alternative method to epicardial ablation.
References
- 1.Stevenson W.G., Wilber D.J., Natale A. Irrigated radiofrequency catheter ablation guided by electroanatomic mapping for recurrent ventricular tachycardia after myocardial infarction: the multicenter thermocool ventricular tachycardia ablation trial. Circulation. 2008;118:2773–2782. doi: 10.1161/CIRCULATIONAHA.108.788604. [DOI] [PubMed] [Google Scholar]
- 2.Aliot E.M., Stevenson W.G., Almendral-Garrote J.M., European Heart Rhythm Association (EHRA); Registered Branch of the European Society of Cardiology (ESC); Heart Rhythm Society (HRS); American College of Cardiology (ACC); American Heart Association (AHA) EHRA/HRS expert consensus on catheter ablation of ventricular arrhythmias: developed in a partnership with the European Heart Rhythm Association (EHRA), a registered branch of the European Society of Cardiology (ESC), and the Heart Rhythm Society (HRS); in collaboration with the American College of Cardiology (ACC) and the American Heart Association (AHA) Heart Rhythm. 2009;6:886–933. doi: 10.1016/j.hrthm.2009.04.030. [DOI] [PubMed] [Google Scholar]
- 3.Baldinger S.H., Kumar S., Barbhaiya C.R. Epicardial radiofrequency ablation failure during ablation procedures for ventricular arrhythmias: reasons and implications for outcomes. Circ Arrhythm Electrophysiol. 2015;8:1422–1432. doi: 10.1161/CIRCEP.115.003202. [DOI] [PubMed] [Google Scholar]
- 4.Hutchinson M.D., Gerstenfeld E.P., Desjardins B. Endocardia unipolar voltage mapping to detect epicardial VT substrate in patients with nonischemic cardiomyopathy. Circ Arrhythm Electrophysiol. 2011;4:49–55. doi: 10.1161/CIRCEP.110.959957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sacher F., Sobiezczyk P., Tedrow U. Transcoronary ethanol ventricular tachycardia ablation in modern electrophysiology era. Heart Rhythm. 2008;5:62–68. doi: 10.1016/j.hrthm.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 6.Gabus V., Jeanrenaud X., Eeckhout E., Pruvot E. Transcoronary ethanol for incessant epicardial ventricular tachycardia. Heart Rhythm. 2014;11:143–145. doi: 10.1016/j.hrthm.2013.09.058. [DOI] [PubMed] [Google Scholar]
- 7.Tokuda M., Sobieszczyk P., Eisenhauer A. Transcoronary ethanol ablation for recurrent ventricular tachycardia after failed catheter ablation. Circ Arrhythm Electrophysiol. 2011;4:889–896. doi: 10.1161/CIRCEP.111.966283. [DOI] [PubMed] [Google Scholar]
- 8.Berte B., Derval N., Sacher F. A case of incessant VT from an intramural septal focus: ethanol or bipolar ablation? HeartRhythm Case Rep. 2015;1:89–94. doi: 10.1016/j.hrcr.2015.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kreidieh B., Rodriquez-Manero M., Schumann P., Ibarra-Cortez S.H., Dave A.S., Valderrabano M. Retrograde coronary venous ethanol infusion for ablation of refractory ventricular tachycardia. Circ Arrhythm Electrophysiol. 2016 July;9 doi: 10.1161/CIRCEP.116.004352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tavares L., Valderrabano M. Retrograde venous ethanol ablation for ventricular tachycardia. Heart Rhythm. 2019;16:478–483. doi: 10.1016/j.hrthm.2018.09.010. [DOI] [PubMed] [Google Scholar]
- 11.Okishige K., Shigeta T., Nishimura T. Chemical ablation of ventricular tachycardia arising from the left ventricular summit. Clin Case Rep. 2019;7:2036–2041. doi: 10.1002/ccr3.1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wright K.N., Morley T., Bicknell J., Bishop S.P., Walcott G.P., Kay G.N. Retrograde coronary venous infusion of ethanol for ablation of canine ventricular myocardium. J Cardiovasc Electrophysiol. 1998;9:976–984. doi: 10.1111/j.1540-8167.1998.tb00138.x. [DOI] [PubMed] [Google Scholar]