Introduction
Subcutaneous implantable cardioverter-defibrillators (S-ICD) have demonstrated a high efficacy for the treatment of ventricular tachycardia and ventricular fibrillation (VF).1 S-ICDs are associated with a relatively low rate of lead failure and with absence of endocarditis or vascular complications. However, the Achilles heel of this device remains its detection capacities. We here report a case of S-ICD sensing modification after catheter ablation of premature ventricular beat.
Case report
A 60-year-old man was hospitalized after ventricular fibrillation. After excluding structural cardiomyopathy and primary electrical disorder, diagnosis of idiopathic VF was retained and an EMBLEM S-ICD (Boston Scientific, Marlborough, MA) was implanted. This device had the SMART-PASS technology.
A recurrence of VF was appropriately identified and treated 15 days after implantation of the device. After identifying an early premature ventricular beat responsible for the VF, a catheter ablation was performed targeting distal Purkinje potential in front of the mitral lateral papillary muscle zone (Figure 1). Two days later, multiple inappropriate shocks occurred owing to QRS and T-wave oversensing (Figure 2A). No lead dysfunction was observed. However, while S-ICD automatic and manual sensing was effective in the 3 vectors before ablation during standing and supine positions, it failed just after. Interestingly, slight changes of the electrocardiogram (ECG) were observed in lead II for the conduction (widened QRS, diminution of R-wave amplitude) and repolarization parameters (Figure 2B and C; Figure 3), leading to modifications of the R/T wave ratio. We did not have satisfying sensibility in front on the right precordial location. Finally, the only choice we had was to replace the S-ICD with a transvenous ICD.
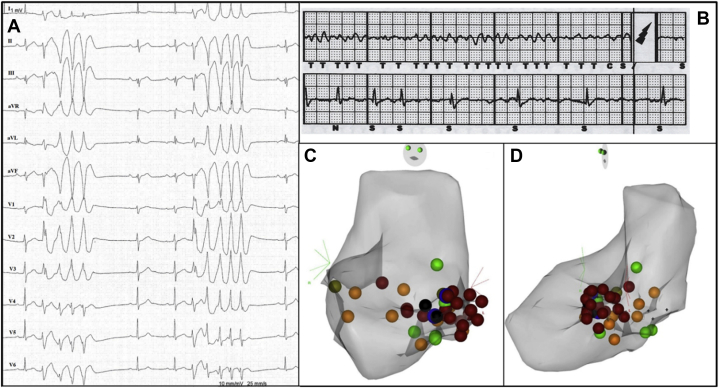
Figure 1.
A: Twelve-lead electrocardiogram with premature ventricular beats inducing recurrent nonsustained tachycardias. B: Subcutaneous implantable cardioverter-defibrillator recording: appropriate shock of a recurrence of ventricular fibrillation. C,D: Three-dimensional cartography of the catheter ablation procedure: points represent ablation lesions (C: anterior posterior view; D: left profile view).
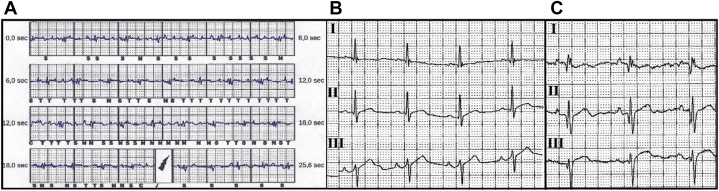
Figure 2.
A: Inappropriate therapy owing to QRS and T-wave oversensing, secondary to modification of the R/T wave ratio. B: Subcutaneous implantable cardioverter-defibrillator (S-ICD) screening before catheter ablation: OK in primary and secondary leads. C: S-ICD screening after catheter ablation: widened QRS, Q wave, modification of the R/T ratio inducing loss of detection abilities.
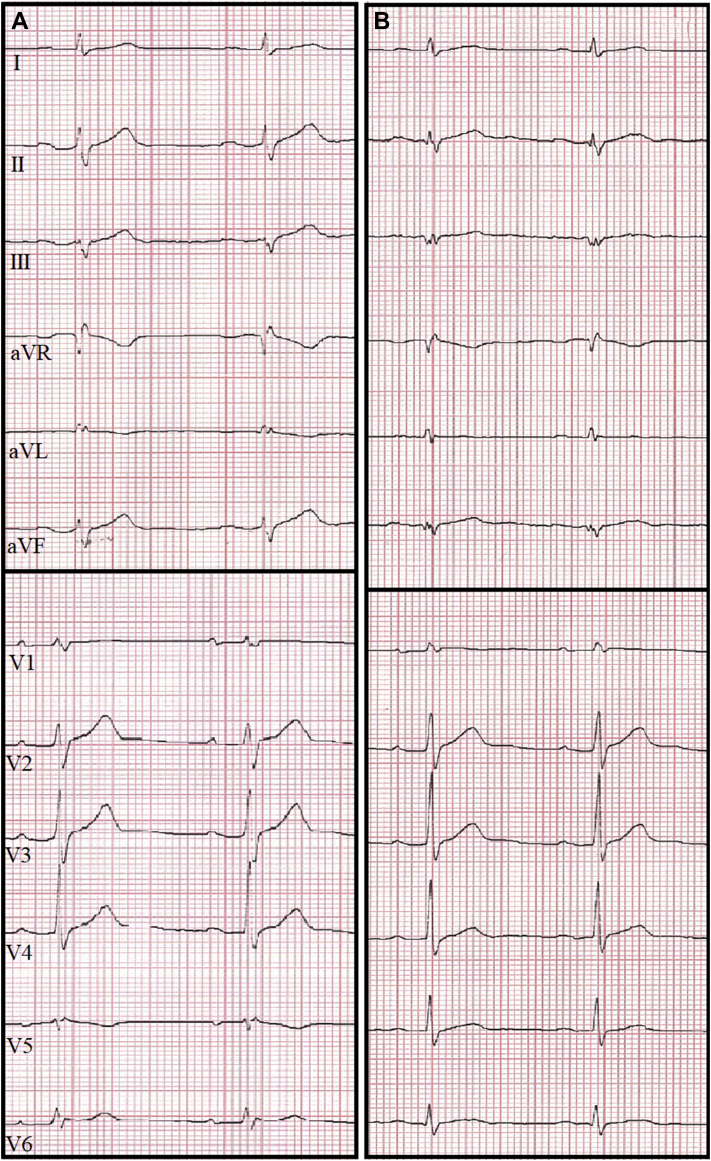
Figure 3.
A: Twelve-lead electrocardiogram (ECG) before catheter ablation. B: Twelve-lead ECG after catheter ablation: widened QRS, Q wave in DIII.
Discussion
As S-ICD avoids transvenous lead–related complications, it is increasingly implanted.1
The 3-year inappropriate shock rate observed from the Pooled Analysis of the IDE Study and EFFORTLESS S-ICD Registry was 13%. Causes of inappropriate shocks were mainly T-wave oversensing and supraventricular arrhythmia above the discrimination zone (respectively, in 39% and 24%).2 Oversensing occurs more frequently in the presence of factors that affect the morphology and the ratio of the R wave and the T wave, like bundle branch block, digoxin use, and abnormal repolarization.3 We can also mention cases of S-ICD T-wave oversensing after alcohol septal ablation in patients with hypertrophic cardiomyopathy.4
ECG modifications have already been described after catheter ablation, resulting from changes of impulse propagation in the Purkinje arborization.5 Haïssaguerre and colleagues5 described in 2002 that in some cases of idiopathic VF ablations, endocardial records after ablation showed the abolition of local Purkinje potentials, a slight delay in the onset of the local ventricular electrogram, associated with prolonged QRS at the ECG. The same anomalies probably occurred in our case, resulting in slight changes of the QRS in the front leads.
Our report is the first observation of slight ECG changes secondary to endocardial ablation that lead to sensing inability of the S-ICD system.
Feasibility and safety of a management approach that incorporates ventricular tachycardia / premature ventricular beat ablation and S-ICD implantation in secondary prevention patients are still questioned.6 When catheter ablation is indicated at the same time as ICD implantation, it should be done before S-ICD screening and implantation to avoid this unfortunate complication.
These observations should encourage us to carefully select the most suitable patients for catheter ablation after S-ICD implantation. We also have to perform systematic device screening after procedures.
Conclusion
We report here an inappropriate therapy in an S-ICD after catheter ablation of idiopathic left ventricular tachycardia. Purkinje-guided ablation can result in sensing inability of the S-ICD system. This case must be kept in mind when a combination of ventricular ablation and ICD implantation is indicated. Otherwise, a systematic device screening should be done after procedures.
Key Teaching Points.
-
•
Electrocardiogram modifications should be observed after premature ventricular beat (PVB) or ventricular tachycardia (VT) catheter ablations, resulting from changes of impulse propagation in the Purkinje arborization. These changes can lead to subcutaneous implantable cardioverter-defibrillator (S-ICD) sensing modifications.
-
•
When catheter ablation of PVB or VT is indicated at the same time as implantable cardioverter-defibrillator, it should be done before S-ICD screening and implantation. This strategy prevents S-ICD sensing modifications after catheter ablation.
-
•
Systematic S-ICD screening should be done after VT/PVB ablation to check that no sensing modifications appeared. This can avoid an underdetection of ventricular fibrillation or an inappropriate therapy.
References
- 1.Boersma L., Barr C., Knops R. Implant and midterm outcomes of the Subcutaneous Implantable Cardioverter-Defibrillator Registry: The EFFORTLESS Study. J Am Coll Cardiol. 2017;70:830–841. doi: 10.1016/j.jacc.2017.06.040. [DOI] [PubMed] [Google Scholar]
- 2.Burke M.C., Gold M.R., Knight B.P. Safety and efficacy of the totally subcutaneous implantable defibrillator: 2-year results from a pooled analysis of the IDE Study and EFFORTLESS Registry. J Am Coll Cardiol. 2015;65:1605–1615. doi: 10.1016/j.jacc.2015.02.047. [DOI] [PubMed] [Google Scholar]
- 3.Kooiman K.M., Knops R.E., Olde Nordkamp L. Inappropriate subcutaneous implantable cardioverter-defibrillator shocks due to T-wave oversensing can be prevented: implications for management. Heart Rhythm. 2014;11:426–434. doi: 10.1016/j.hrthm.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 4.Dijk V.F.V., Liebregts M., Luermans J.G.L.M. Inappropriate shock due to t-wave oversensing by a subcutaneous ICD after alcohol septal ablation for hypertrophic cardiomyopathy. Pacing Clin Electrophysiol. 2016;39:307–309. doi: 10.1111/pace.12784. [DOI] [PubMed] [Google Scholar]
- 5.Haïssaguerre M., Shoda M., Jaïs P. Mapping and ablation of idiopathic ventricular fibrillation. Circulation. 2002;106:962–967. doi: 10.1161/01.cir.0000027564.55739.b1. [DOI] [PubMed] [Google Scholar]
- 6.Subcutaneous ICD Therapy Combined With VT Ablation for the Secondary Prevention of Sudden Cardiac Death. https://clinicaltrials.gov/ct2/show/NCT03622307 Available at.