Introduction
Precise appreciation of the living anatomy of the pericardial space is important to ensure procedural success without compromising safety during the epicardial approach. However, comprehensive 3-dimensional appreciation of the pericardial anatomy is extremely difficult. Thus far, learning sources of 3-dimensional pericardial anatomy have been limited to the dissection images and/or illustrations.1, 2, 3, 4, 5, 6 Visualization of the entire picture of the pericardial space has been challenging. We herein presented comprehensible volume-rendered images of the pericardial space, reconstructed from the case of cardiac tamponade.
Case report
An 82-year-old woman presented with sudden chest pain and dizziness. On admission, her blood pressure was 76/61 mm Hg, with a regular pulse rate of 90 beats per minute. Electrocardiogram showed ST-segment depression in leads V1–V3, with an elevation in serum troponin I level (1.50 ng/mL). Transthoracic echocardiography findings revealed pericardial effusion, compatible with cardiac tamponade. Non-electrocardiogram-gated contrast-enhanced computed tomography (SOMATOM Force; Siemens Healthcare, Forchheim, Germany; acquisition mode, high-pitch dual spiral scan; tube voltage, 120 kVp; section thickness, 1.0 mm; rotation time, 250 ms; and temporal resolution, 66 ms) suggested a distal occlusion of the inferolateral branch of the right coronary artery presumably due to spontaneous coronary artery dissection and oozing rupture of the inferolateral left ventricle, with bloody pericardial fluid. Emergent surgery confirmed the findings and resulted in a successful repair.
Using the computed tomographic datasets, which happened to be acquired during diastole, volume-rendered images were reconstructed (Figure 1, Figure 2, Figure 3, Supplementary Movies 1–5). This approach successfully visualized the 3-dimensional extent of the transverse sinus and its extensions, including superior and inferior aortic recesses, and oblique sinus. All analyses were performed using a commercially available workstation (ZioCube version 1.0.0.4; Ziosoft Inc, Tokyo, Japan).
Figure 1.
Three-dimensional anatomy of the pericardial space viewed from the left anterior oblique direction. The right panel shows the pericardial space itself subtracting the heart from the left panel. Red and white arrows indicate the superior and inferior aortic recesses, respectively. AAo = ascending aorta; LAA = left atrial appendage; LPA = left pulmonary artery; LV = left ventricle; OS = oblique sinus; RA = right atrium; RPA = right pulmonary artery; TS = transverse sinus (red-dotted curve).
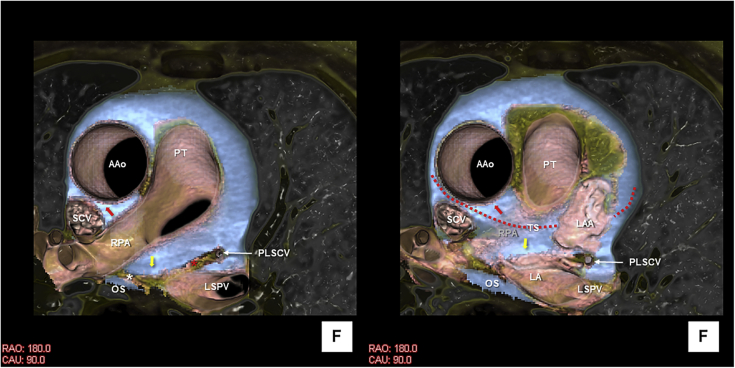
Figure 2.
Three-dimensional anatomy of the pericardial space viewed from the inferior direction. Red and yellow arrows indicate superior aortic recess and posterior extension of the transverse sinus, respectively. White asterisk shows fused reflections between the transverse and oblique sinuses. Red asterisk denotes the vestigial fold. AAo = ascending aorta; LA = left atrium; LAA = left atrial appendage; LSPV = left superior pulmonary vein; OS = oblique sinus; PLSCV = persistent left superior caval vein; PT = pulmonary trunk; RPA = right pulmonary artery; SCV = superior caval vein; TS = transverse sinus (red-dotted curve).
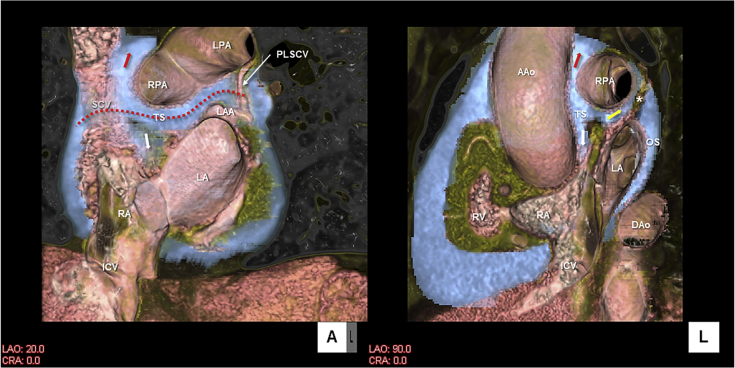
Figure 3.
Three-dimensional anatomy of the pericardial space viewed from the left anterior oblique (left panel) and left lateral (right panel) directions. Red, white, and yellow arrows indicate superior and inferior aortic recesses, and posterior extension of the transverse sinus, respectively. Transverse and oblique sinuses are separated by fused reflections (white asterisk). AAo = ascending aorta; Dao = descending aorta; ICV = inferior caval vein; LA = left atrium; LAA = left atrial appendage; LPA = left pulmonary artery; OS = oblique sinus; PLSCV = persistent left superior caval vein; RA = right atrium; RPA = right pulmonary artery; RV = right ventricle; SCV = superior caval vein; TS = transverse sinus (red-dotted curve).
Discussion
The pericardium is conventionally divided into the parietal and visceral pericardial layers. Visceral pericardium is conventionally referred to as the “epicardium.” However, beneath the visceral pericardial layer there is epicardial fat, which surrounds the myocardium, containing the coronary vessels. Within the pericardial space between the parietal pericardium and “epicardium,” normally <50 mL of serous fluid lubricates the surface of the heart.1
The pericardial reflections compose 2 orifices (Supplementary Figure); the first one is located superiorly, surrounding the pulmonary trunk and ascending aorta.2,3 The second one is located posteriorly (also referred to as the “hilum of the heart”), surrounding the pulmonary veins and caval veins.2 The 2 orifices work as a window for the extracardiac nerves and vessels to enter the epicardial layer of the heart. In this regard, this area is directly facing the extracardiac mediastinum.
The transverse sinus is located between these 2 orifices. Accordingly, through the transverse sinus, the probe can be passed from the space around the left atrial appendage to the space between the ascending aorta and superior caval vein (Figure 1, Figure 2, Figure 3, Supplementary Figure). Posterior to the ascending aorta, the transverse sinus has superior and inferior extensions, called superior and inferior aortic recesses (Figure 1, Figure 2, Figure 3). The superior aortic recess is also referred to as the aortocaval recess (Supplementary Figure).3
The roof of the left atrium and the antrum of the pulmonary veins is the exact location of the second orifice directly facing the extrapericardial right pulmonary artery at the “hilum of the heart” between the transverse and oblique sinuses.3 In the present case, however, the posterior reflection of the transverse sinus and superior reflection of the oblique sinus fuse, forming the partition between these sinuses (Figures 2 and 3). Accordingly, the right pulmonary artery does not have an extrapericardial area of contact with the left atrial roof. This anatomical variation was already described in the textbook by McAlpine.3 The 3-dimensional appreciation of this space is required for proper interpretation of clinical images acquired from computed tomographic scans and cardiac magnetic resonance imaging.4
In the present case, the thin persistent left superior caval vein is also observed (Figures 2 and 3). It descends along the left side of the left pulmonary artery toward the fold between the base of the left atrial appendage and left pulmonary veins, then connects to the coronary sinus. It runs within the fused fold of reflection, connecting to the second orifice in a similar manner that the superior caval vein is surrounded by the fold of reflection of the second orifice (Supplementary Figure).3 In the normal development, this vein regresses to create the ligament of Marshall1,3; then the fused fold is called the vestigial fold (Figure 2, Supplementary Figure),3 located between the transverse sinus and left pulmonic recess.1,3,5
With the development of the percutaneous epicardial ablation and cardiac resynchronization therapy, exact knowledge of the pericardial anatomy along with surrounding structures is important for cardiac electrophysiologists.6,7 Any invasive approaches within the pericardial space potentially affect surrounding structures located on both visceral8, 9, 10 and parietal11, 12, 13, 14 sides, including the epicardial fat, coronary arteries, coronary veins, cardiac ganglionated plexus, phrenic nerve, esophagus, vertebra, descending aorta, intercostal arteries, pleura and lungs, internal mammary arteries, and other mediastinal structures. However, 3-dimensional demonstration of anatomy of the pericardial space is difficult,5,15 as it is thin and only a “potential space” in health. Therefore, conventional attempts to describe pericardial anatomy include illustrations and/or photographs of the specimen,3 mainly focusing on the reflections creating 2 orifices, with an indirect indication of the pericardial space, including recesses (Supplementary Figure). In the present case, extensive pericardial effusion and excellent image quality without motion artifact, combined with sufficient contrast between bloody pericardial fluid and epicardial fat, enable us to create a comprehensible 3-dimensional image of the pericardial space. To the best of our knowledge, this is the first image reconstructed from the living heart dataset that shows the 3-dimensional morphology and relationship between the transverse and oblique sinuses in a single image (Figure 1). Continuous investigation will be necessary to further reveal the living anatomy of the pericardial sinuses and recesses in association with the heart and surrounding structures. Accumulated knowledge will surely help clinical electrophysiologists create sophisticated strategies using the pericardial access and/or avoid inadvertent complications.
Key Teaching Points.
-
•
The pericardial reflections compose 2 orifices: the first one is located superiorly, surrounding the pulmonary trunk and ascending aorta; and the second one is located posteriorly, surrounding the pulmonary veins and caval veins. The transverse sinus is located between these 2 orifices.
-
•
The 2 orifices work as a window for the extracardiac nerves and extracardiac vessels to enter the epicardial layer of the heart.
-
•
The roof of the left atrium and the antrum of the pulmonary veins is the exact location of the second orifice directly facing the extrapericardial mediastinum. The transverse and oblique sinuses are separated by this second orifice.
Acknowledgments
The authors thank Dr Yu Izawa, Dr Takayoshi Toba, and Dr Hiroyuki Toh from the Division of Cardiovascular Medicine, Department of Internal Medicine, Kobe University Graduate School of Medicine, for their cooperation for data collection and image analysis.
Footnotes
Funding: This work was made possible by support from NIH grants HL084261 and OT2OD023848 to KS.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.hrcr.2019.12.009
Appendix A. Supplementary data
Three-dimensional anatomy of the pericardial space with the heart.
Three-dimensional anatomy of the pericardial space without the heart.
Three-dimensional sectional anatomy of the pericardial space viewed from the inferior direction.
Three-dimensional sectional anatomy of the pericardial space viewed from the left anterior oblique direction.
Three-dimensional sectional anatomy of the pericardial space viewed from the left lateral direction.
Supplementary Figure.

Schematic diagram of the pericardial space and reflections. Reproduced from McAlpine Collection (Copyright UCLA Cardiac Arrhythmia Center). Red-dotted curve indicates the transverse sinus. Thick black lines denote the two orifices composed by pericardial reflections.
References
- 1.Rodriguez E.R., Tan C.D. Structure and anatomy of the human pericardium. Prog Cardiovasc Dis. 2017;59:327–340. doi: 10.1016/j.pcad.2016.12.010. [DOI] [PubMed] [Google Scholar]
- 2.Pauza D.H., Pauziene N., Tamasauskas K.A., Stropus R. Hilum of the heart. Anat Rec. 1997;248:322–324. doi: 10.1002/(SICI)1097-0185(199707)248:3<322::AID-AR3>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 3.McAlpine W.A. Springer-Verlag; New York: 1975. Heart and Coronary Arteries: An Anatomical Atlas for Clinical Diagnosis, Radiological Investigation, and Surgical Treatment; pp. 123–132. [Google Scholar]
- 4.Choe Y.H., Im J.G., Park J.H., Han M.C., Kim C.W. The anatomy of the pericardial space: a study in cadavers and patients. AJR Am J Roentgenol. 1987;149:693–697. doi: 10.2214/ajr.149.4.693. [DOI] [PubMed] [Google Scholar]
- 5.Żurada A., Ustymowicz A., Loukas M., Michalak M., Czyżewska D., Gielecki J. Computerized tomography of the transverse pericardial sinus: normal or pathologic? Clin Anat. 2017;30:61–70. doi: 10.1002/ca.22778. [DOI] [PubMed] [Google Scholar]
- 6.Boyle N.G., Shivkumar K. Epicardial interventions in electrophysiology. Circulation. 2012;126:1752–1769. doi: 10.1161/CIRCULATIONAHA.111.060327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tung R., Michowitz Y., Yu R. Epicardial ablation of ventricular tachycardia: an institutional experience of safety and efficacy. Heart Rhythm. 2013;10:490–498. doi: 10.1016/j.hrthm.2012.12.013. [DOI] [PubMed] [Google Scholar]
- 8.Tung R., Nakahara S., Ramirez R., Lai C., Fishbein M.C., Shivkumar K. Distinguishing epicardial fat from scar: analysis of electrograms using high-density electroanatomic mapping in a novel porcine infarct model. Heart Rhythm. 2010;7:389–395. doi: 10.1016/j.hrthm.2009.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nishimori M., Kiuchi K., Mori S. Atypical inferoseptal accessory pathway connection associated with an aneurysm of the coronary sinus: insight from a three-dimensional combined image of electroanatomic mapping and computed tomography. HeartRhythm Case Rep. 2018;4:389–392. doi: 10.1016/j.hrcr.2018.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hanna P., Shivkumar K. Targeting the cardiac ganglionated plexi for atrial fibrillation: modulate or destroy? JACC Clin Electrophysiol. 2018;4:1359–1361. doi: 10.1016/j.jacep.2018.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vaseghi M., Cesario D.A., Ji S. Beyond coronary sinus angiography: the value of coronary arteriography and identification of the pericardiophrenic vein during left ventricular lead placement. Pacing Clin Electrophysiol. 2005;28:185–190. doi: 10.1111/j.1540-8159.2005.09548.x. [DOI] [PubMed] [Google Scholar]
- 12.Buch E., Nakahara S., Shivkumar K. Intra-pericardial balloon retraction of the left atrium: a novel method to prevent esophageal injury during catheter ablation. Heart Rhythm. 2008;5:1473–1475. doi: 10.1016/j.hrthm.2008.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nagamatsu Y., Mori S., Fukuzawa K. Anatomical characteristics of the superior epigastric artery for epicardial ablation using the anterior approach. J Cardiovasc Electrophysiol. 2019;30:1339–1340. doi: 10.1111/jce.14035. [DOI] [PubMed] [Google Scholar]
- 14.Pai R.K., Boyle N.G., Child J.S., Shivkumar K. Transient left recurrent laryngeal nerve palsy following catheter ablation of atrial fibrillation. Heart Rhythm. 2005;2:182–184. doi: 10.1016/j.hrthm.2004.10.030. [DOI] [PubMed] [Google Scholar]
- 15.de Schlichting E., Robert Y., Selek L., Palombi O., Chaffanjon P. A three-dimensional (3D) representation of pericardial cavity based on computed tomography (CT) Surg Radiol Anat. 2015;37:199–204. doi: 10.1007/s00276-014-1362-y. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Three-dimensional anatomy of the pericardial space with the heart.
Three-dimensional anatomy of the pericardial space without the heart.
Three-dimensional sectional anatomy of the pericardial space viewed from the inferior direction.
Three-dimensional sectional anatomy of the pericardial space viewed from the left anterior oblique direction.
Three-dimensional sectional anatomy of the pericardial space viewed from the left lateral direction.