Key Points
Question
Is preemptive therapy (based on the initiation of antiviral therapy for early asymptomatic cytomegalovirus [CMV] viremia detected by surveillance testing) more effective than antiviral prophylaxis (administered to all patients for 100 days) for the prevention of CMV disease in CMV-seronegative liver transplant recipients with seropositive donors?
Findings
In this randomized clinical trial that included 205 CMV-seronegative liver transplant recipients with seropositive donors, the use of antiviral preemptive therapy with valganciclovir, 900 mg twice daily, compared with antiviral prophylaxis with valganciclovir, 900 mg once daily, resulted in CMV disease incidence over 12 months of 9% vs 19%, a difference that was statistically significant.
Meaning
The use of preemptive therapy, compared with antiviral prophylaxis, reduced the 12-month incidence of CMV disease.
Abstract
Importance
Despite the use of a cytomegalovirus (CMV) prevention strategy of antiviral prophylaxis for high-risk CMV-seronegative liver transplant recipients with seropositive donors, high rates of delayed-onset postprophylaxis CMV disease occur. An alternate approach, preemptive therapy (initiation of antiviral therapy for early asymptomatic CMV viremia detected by surveillance testing), has not previously been directly compared with antiviral prophylaxis in these patients.
Objective
To compare preemptive therapy with antiviral prophylaxis in CMV-seronegative liver transplant recipients with seropositive donors for the prevention of CMV disease.
Design, Setting, and Participants
Randomized clinical trial of preemptive therapy vs antiviral prophylaxis in 205 CMV-seronegative liver transplant recipients with seropositive donors aged older than 18 years. The trial was conducted at 6 academic transplant centers in the United States between October 2012 and June 2017, with last follow-up in June 2018.
Interventions
Patients were randomized 1:1 to receive either preemptive therapy (valganciclovir, 900 mg, twice daily until 2 consecutive negative tests a week apart) for viremia detected by weekly plasma CMV polymerase chain reaction for 100 days (n = 100) or valganciclovir, 900 mg, daily for 100 days as antiviral prophylaxis (n = 105).
Main Outcomes and Measures
The primary outcome was incidence of CMV disease by 12 months, defined as CMV syndrome (CMV viremia and clinical or laboratory findings) or end-organ disease. Secondary outcomes included acute allograft rejection, opportunistic infections, graft and patient survival, and neutropenia.
Results
Among 205 patients who were randomized (mean age, 55 years; 62 women [30%]), all 205 (100%) completed the trial. The incidence of CMV disease was significantly lower with preemptive therapy than antiviral prophylaxis (9% [9/100] vs 19% [20/105]; difference, 10% [95% CI, 0.5% to 19.6%]; P = .04]). The incidence of allograft rejection (28% vs 25%; difference, 3% [95% CI, −9% to 15%]), opportunistic infections (25% vs 27%; difference, 2% [95% CI, −14% to 10%]), graft loss (2% vs 2%; difference, <1% [95% CI, −4% to 4%]), and neutropenia (13% vs 10%; difference, 3% [95% CI, −5% to 12%]) did not differ significantly for the preemptive therapy vs antiviral prophylaxis group, respectively. All-cause mortality at last follow-up was 15% in the preemptive therapy vs 19% in the antiviral prophylaxis group (difference, 4% [95% CI, −14% to 6%]; P = .46).
Conclusions and Relevance
Among CMV-seronegative liver transplant recipients with seropositive donors, the use of preemptive therapy, compared with antiviral prophylaxis, resulted in a lower incidence of CMV disease over 12 months. Further research is needed to replicate these findings and assess long-term outcomes.
Trial Registration
ClinicalTrials.gov Identifier: NCT01552369
This randomized trial compares preemptive therapy vs antiviral prophylaxis with valganciclovir in cytomegalovirus (CMV)-seronegative liver transplant recipients with seropositive donors for the prevention of CMV disease.
Introduction
Cytomegalovirus (CMV) is a major pathogen in recipients of solid organ transplants, particularly in CMV-seronegative patients with seropositive donors, who have the highest risk for CMV-associated complications.1 Antiviral prophylaxis with valganciclovir (typically for 3-6 months) is the most widely used prevention strategy in this setting, including for liver transplant recipients.2,3,4 However, among patients who receive antiviral prophylaxis, postprophylaxis (delayed-onset) CMV disease commonly develops3,5,6,7 and has been independently associated with mortality.6 Strategies such as longer duration of prophylaxis beyond 3 months and monitoring for CMV viremia after discontinuation of antiviral prophylaxis have not been consistently effective and are not routinely recommended in guidelines for CMV-seronegative liver transplant recipients with seropositive donors.8
Preemptive therapy is an approach in which patients are monitored for early replication (ie, viremia by polymerase chain reaction [PCR]), and antiviral drug is administered only when CMV replication is detected to prevent its progression to higher-grade viremia and CMV disease. To our knowledge, prior direct comparisons of preemptive therapy with antiviral prophylaxis have been performed either in non–high-risk CMV-seropositive transplant recipients,9 used insensitive assays for initiating preemptive therapy,10 or included only small numbers of CMV-seronegative patients with seropositive donors.11 Small, noncomparative studies have suggested lower rates of CMV disease (especially delayed-onset disease) with preemptive compared with antiviral prophylaxis in CMV-seronegative liver transplant recipients with seropositive donors.12,13,14 However, there have been no adequately powered direct comparative clinical trials of preemptive therapy vs antiviral prophylaxis in these patients. This randomized trial compared preemptive therapy vs antiviral prophylaxis in high-risk CMV-seronegative liver transplant recipients with seropositive donors with the goals of assessing CMV disease, other clinical outcomes, and the development of CMV-specific immune responses.
Methods
Study Design
This was a randomized clinical trial of preemptive therapy vs antiviral prophylaxis using valganciclovir in CMV-seronegative liver transplant recipients with seropositive donors recruited between October 2012 and June 2017 at 6 academic transplant centers in the United States. The National Institute of Allergy and Infectious Diseases (NIAID), institutional review boards at all sites, and the data monitoring committee approved the study. The data monitoring committee and end point committees were convened by the NIAID and were independent of the study investigators. All CMV disease events were adjudicated by an independent end point committee through blinded review of source data. The study was conducted under NIAID oversight. Study monitoring and source data verification were overseen by the NIAID and conducted by its designee. Written informed consent was obtained from all patients or their legally authorized representatives. All information and materials in the article are original.
Patients
Inclusion criteria were first orthotopic liver transplant (deceased or live donor) within 10 days prior; 18 years of age or older; recipient with CMV-seronegative status and donor with CMV-seropositive status; negative pregnancy test (if female); and absolute neutrophil count greater than 1000/μL at randomization (Supplement 1). Exclusion criteria were participation in another investigational agent trial; hypersensitivity to the study drug; known HIV infection; receipt of multiorgan or prior organ transplant; or life expectancy of less than 72 hours.
Randomization
Eligible patients were randomized within 10 days of transplant in a 1:1 ratio to preemptive therapy or antiviral prophylaxis by computer-generated web-based allocation using permuted blocks of 4. Randomization at each site was stratified by receipt of lymphocyte-depleting antibody and need for kidney replacement therapy at enrollment.
Interventions
Patients in the preemptive therapy group underwent weekly testing for CMV viremia for 100 days using a previously described highly sensitive real-time plasma CMV PCR assay (limit of detection of 20 IU/mL) performed at a central laboratory15 (University of Washington, Diagnostic Virology Laboratory). On detection of viremia at any level, valganciclovir, 900 mg, orally twice daily was administered until 2 consecutive negative tests resulted 1 week apart. Because replication kinetics of CMV are rapid in CMV-seronegative patients,16 detection of viremia at any level (ie, rather than a quantitative threshold) was used as the criterion for initiation of preemptive therapy. Recurrent viremia within 100 days in the preemptive therapy group was treated similarly to the initial episode. Patients assigned to antiviral prophylaxis received valganciclovir, 900 mg, orally once daily for 100 days initiated within 10 days of transplant. All drug dosages were adjusted based on creatinine clearance per the manufacturer’s recommendations.
Because CMV viremia is uncommon while taking valgancicolvir prophylaxis, surveillance CMV PCR testing was not performed during the period of antiviral prophylaxis, which is consistent with clinical guidelines.8,17 Valganciclovir (or intravenous ganciclovir) use for the first 10 days after transplant prior to randomization per local standards did not preclude enrollment. However, valganciclovir after randomization was given only as dictated by the study protocol. The preemptive therapy group received acyclovir, 400 mg, orally twice daily for 28 days for herpes simplex virus prophylaxis; acyclovir was discontinued during valganciclovir therapy. Patients were followed up for at least 12 months (or until death, if it occurred earlier) and until the last enrolled patient in the overall study completed 12 months of follow-up after transplant.
Outcomes
The primary outcome was the incidence of CMV disease by 12 months after transplant. Standard criteria were used for the definition of CMV disease in accordance with previously reported clinical trials and guidelines (Box).18,19 Secondary outcomes were delayed-onset CMV disease (between day 100 and 12 months), biopsy-proven acute rejection, opportunistic bacterial and fungal infections, graft loss (retransplant), all-cause mortality by 12 months, neutropenia (absolute neutrophil count <500/μL), and requirement for granulocyte colony-stimulating factor from randomization until 7 days after completion of preemptive therapy or prophylaxis (day 107). Exploratory end points were clinical outcomes that included time to onset of CMV disease, opportunistic bacterial and fungal infections, graft loss and retransplantation, mortality, new malignancy, and requirement of kidney replacement therapy at last follow-up, and immunologic end points (CMV-specific neutralizing antibody [nAb] and T-cell responses) at day 100, 6 months, and 12 months. The exploratory cost-effectiveness analysis is not reported in this article.
Box. Protocol Definition of Cytomegalovirus (CMV) Disease (CMV Syndrome or End-Organ CMV Disease) for Primary Efficacy Analysis.
CMV Syndrome
The patient has CMV infection (viremia) identified by a nucleic acid–based assay (CMV DNA polymerase chain reaction [PCR], pp67mRNA, or digene hybridization [nonamplification assay]) or antigenemia assay or viral culture
AND at least 1 of the following clinical/laboratory findings:
Temperature ≥38 °C (100.4 °F)
Severe malaise
Leukopenia defined as:
White blood cell (WBC) count of <3500/μL if the WBC count prior to the development of WBC or decrease of >20% if the WBC count prior to the development of clinical symptoms is <4000/μL
Atypical lymphocytosis ≥5%
Thrombocytopenia defined as:
Platelet count of <100 000/μL if the platelet count prior to the development of clinical symptoms is ≥115 000/μL or decrease of >20% if the platelet count prior to the development of clinical symptoms is <115 000/μL
Tissue Invasive CMV Disease
A diagnosis of organ-specific tissue invasive CMV disease detected by viral culture, histopathology/cytology (CMV inclusion cells), immunohistochemical analysis, or in situ hybridization for CMV in a biopsy or other appropriate sample such as bronchoalveolar lavage (BAL), cerebrospinal fluid, AND symptoms or signs of organ dysfunction. Detection of CMV by PCR in the tissue will be insufficient for the diagnosis of tissue invasive CMV disease.
Criteria to be met for diagnoses of specific organ CMV tissue invasive disease are as follows:
CMV Hepatitis
Liver biopsy with CMV detected by viral culture, CMV inclusions by histopathology/cytology, immunohistochemical analysis, or in situ hybridization (other pathogens or etiologies of hepatic dysfunction such as rejection may be present and do not exclude the diagnosis of CMV hepatitis)
CMV Gastrointestinal Tract Disease (includes esophagitis, gastritis, enteritis, colitis):
Detection of CMV in tissue biopsy by viral culture, histopathology/cytology with CMV inclusions, immunohistochemical analysis, or in situ hybridization
In addition, the patient has upper or lower gastrointestinal tract symptoms and/or signs such as nausea, vomiting, anorexia, dysphagia, odynophagia, cramping, diarrhea, or abdominal pain. (Other pathogens, for example, Clostridioides difficile, may be present without excluding the diagnosis of CMV gastrointestinal disease.)
CMV Pneumonia
Presence of symptoms and/or signs of pulmonary disease
AND the detection of CMV in the BAL or lung biopsy. Detection of CMV in the BAL or biopsy may be performed by viral culture, histopathology/cytology with CMV inclusions, immunohistochemical analysis, or in situ hybridization for CMV. Detection of CMV by PCR alone is insufficient for the diagnosis of CMV pneumonia. Other pathogens may coexist without excluding the diagnosis of CMV pneumonia.
CMV Retinitis
Dilated fundus examination and diagnosis of CMV retinitis by an ophthalmologist.
Central Nervous System Disease
Detection of CMV in the cerebrospinal fluid by viral culture, CMV DNA/RNA PCR assay, or in a biopsy sample by culture, histopathology/cytology (CMV inclusions) immunohistochemical analysis, or in situ hybridization
AND presence of central nervous system symptoms
Other Tissue Invasive CMV Disease
Detection of CMV by viral culture, histopathology/cytology with CMV inclusions, immunohistochemical analysis, or in situ hybridization in a biological specimen (eg, tissue biopsy)
AND the patient exhibits signs or symptoms of relevant organ dysfunction
Serum nAb responses specific to the pentameric complex of CMV were evaluated using a previously described assay to measure neutralization of viral entry and replication.15 T-cell responses were quantified using a 17-color intracellular cytokine staining assay of cryopreserved peripheral blood mononuclear cells stimulated with a CMV pp65 peptide pool for CMV-specific responses or nonspecific mitogen Staphylococcus aureus enterotoxin B (SEB) as a measure of general immune competence. The primary response variables were the magnitude of CD4+ and CD8+ cells that expressed either interferon-γ (IFN-γ) or IFN-γ plus at least 1 other marker as a measure of polyfunctional response: cytokine expression (tumor necrosis factor-α, interleukin-2, and interleukin-4); degranulation marker perforin; and T-cell activation marker CD154. Responses that were greater than .05% above background and at least 3-fold greater than background in the cell population of interest were considered positive.20,21 All immune assays were performed by personnel blinded to clinical data. Only patients who had samples available for both the nAb and T-cell assays were included in analyses of CMV immunity. Further details for both assays appear in eMethods in Supplement 2; the gating strategy is shown in eFigure 1 in Supplement 2.
Statistical Analysis
The primary null hypothesis was that CMV disease rate would be equal in the 2 groups. The null hypothesis would be rejected if preemptive therapy was superior to antiviral prophylaxis at the .05 level. The mean CMV disease rate in existing studies weighted for study size was 0.78% (95% CI, 0%-2.4%) and 30.6% (95% CI, 24.1%-37.1%) with preemptive therapy and antiviral prophylaxis, respectively (Supplement 1). On the basis of power calculations using the lowest observed rate for CMV disease in antiviral prophylaxis studies and the highest observed rate in preemptive therapy studies, it was estimated that CMV disease would occur in 5% of the patients in the preemptive therapy group and 20% of the patients in the antiviral prophylaxis group. A sample size of 160 patients (80 per group) would detect this difference with 80% power and α = .05 using the 2-sided Fisher exact test for independent proportions. Allowing for dropouts and withdrawals, up to 205 patients could be enrolled.
All analyses and descriptive statistics were generated using Stata/SE (version 15.1, Stata Corp LLC). Baseline demographics and risk factors were compared between the 2 groups. Binary and categorical variables were compared using the Pearson χ2 or Fisher exact test as appropriate. Continuous variables were compared using the t test or log-rank test. All statistical tests were 2-sided and P < .05 was considered statistically significant. Because of the potential for type I error due to multiple comparisons, findings for analyses of secondary end points should be interpreted as exploratory. The primary end point analysis compared the incidence of CMV disease in all randomized patients according to their randomization group by applying the Mantel-Haenszel estimate. Point estimates and 95% CIs were calculated for the incidence rates and the difference between the 2 study groups. There were no missing data for primary and secondary outcomes. In the event of missing data, the date was imputed to be that of the first diagnostic test documenting CMV positivity for CMV disease events. For adverse events, missing dates were imputed to be the date of study drug initiation.
Post hoc analyses included viremia in patients in the preemptive therapy group and breakthrough CMV disease within 100 days and valganciclovir use during and after the study intervention period in both groups. Because the study was conducted at 6 sites, to examine the effect of study site on CMV disease, a post hoc generalized linear mixed model was used with site as a random-effects variable. Additional post hoc analysis included the probability of developing disease over time (with participants censored at death, retransplant, or 12 months after transplant), and a competing-risk survival regression model to account for death as a competing risk when comparing the cumulative incidence functions for CMV disease between groups. Kaplan-Meier estimates were generated, and a log-rank test was performed to calculate the equality of the 2 survivor functions for all-cause mortality.
Results
Participants
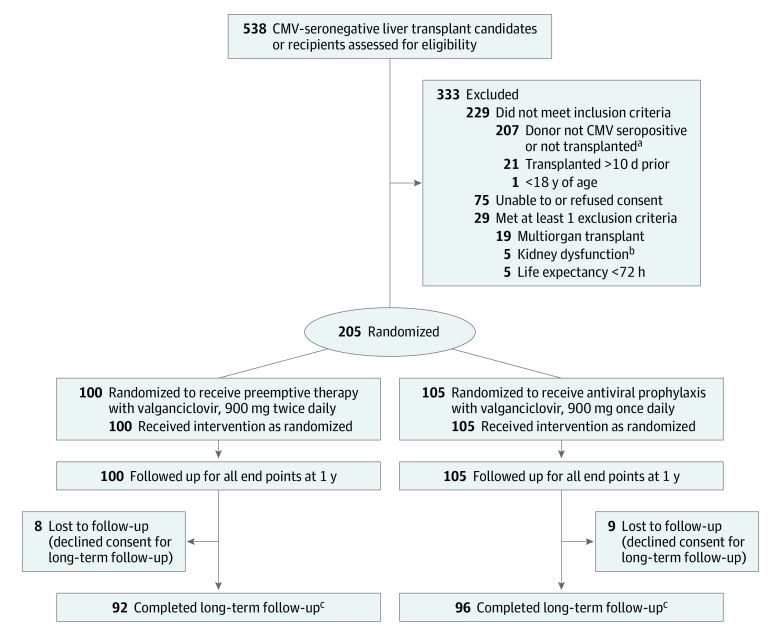
Among 538 CMV-seronegative eligible participants, the most common reason for ineligibility was failure to meet the primary inclusion criterion of donor CMV-seropositive serostatus due to liver transplant from CMV-seronegative donor (Figure 1). Patients were randomized at a median of 4 days (interquartile range [IQR], 2-6 days) after transplant. Baseline characteristics were similar between the groups (Table 1). Of 205 randomized patients, 30% were women (n = 62), and the mean age was 55 years. The median score for the model of end-stage liver disease was 30 (IQR, 25-35), 21% (44/205) required kidney replacement therapy at randomization, and 16% (33/205) received antilymphocyte-depleting antibody induction.
Figure 1. Screening, Randomization, and Follow-up.
aCytomegalovirus (CMV)-seronegative liver transplant candidates awaiting liver transplant could be screened and consented. Ultimately, 207 of 538 eligible patients either did not receive CMV-seropositive donor allograft or did not undergo transplant.
bDefined as creatinine clearance less than 10 mL/min or kidney replacement therapy; an amendment (after 19 patients had been enrolled) eliminated kidney dysfunction as an exclusion.
cLong-term follow-up was a median of 3.2 years (range, 1-5.2 years).
Table 1. Baseline Characteristics of the Study Population According to Study Group.
| Variable | No. (%) | |
|---|---|---|
| Preemptive therapy (n = 100)a | Antiviral prophylaxis (n = 105)a | |
| Demographics | ||
| Age, y | ||
| Median (IQR) | 57 (50-63) | 58 (51-63) |
| >65 | 19 (19) | 16 (15) |
| Sex | ||
| Male | 65 (65) | 78 (74) |
| Female | 35 (35) | 27 (26) |
| Medical history and comorbid conditions | ||
| Underlying liver disease(s)b | ||
| Hepatocellular carcinoma (any) | 37 (37) | 37 (35) |
| Alcoholic liver disease | 32 (32) | 38 (36) |
| Hepatitis C virus | 30 (30) | 37 (35) |
| Nonalcoholic steatohepatitis | 19 (19) | 26 (25) |
| Primary sclerosing cholangitis | 9 (9) | 5 (5) |
| Cryptogenic/autoimmune | 7 (7) | 9 (9) |
| Primary biliary cirrhosis | 6 (6) | 3 (3) |
| Other liver disease | 20 (20) | 22 (21) |
| Diabetes | 23 (23) | 31 (30) |
| Insulin dependent | 16 (16) | 16 (15) |
| Cardiovascular disease | 43 (43) | 46 (44) |
| Kidney replacement therapy at enrollment | 19 (19) | 24 (23) |
| MELD score, median (IQR)c | 30 (25-35) | 30 (25-35) |
| Source of donor graft | ||
| Deceased donation | 94 (94) | 102 (97) |
| Living donation | 6 (6) | 3 (3) |
| Valganciclovir use (before randomization) | 31 (31) | 28 (27) |
| Duration, median (IQR), d | 3 (1-5) | 2 (1-4) |
| Lymphocyte-depleting antibody inductiond | 15 (15) | 18 (17) |
| Primary immunosuppressive agente | ||
| Tacrolimus | 99 (99) | 105 (100) |
| Cyclosporine | 1 (1) | 0 |
Abbreviations: IQR, interquartile range; MELD, Model for End Stage Liver Disease.
The groups were well balanced at baseline for all baseline characteristics.
Some patients had more than 1 underlying liver disease.
The MELD score ranges from 6 to 40, with high scores indicating more severe disease. A waitlist MELD score of 30 has a 3-month mortality probability of about 50% without a liver transplant.
Lymphocyte-depleting antibody consisted of thymoglobulin in all cases.
Tacrolimus was the initial immunosuppressive agent for 204 of 205 patients, 5 patients (5%) in the preemptive therapy group and 7 patients (6.7%) in the prophylaxis group were later switched to cyclosporine.
Primary Outcome
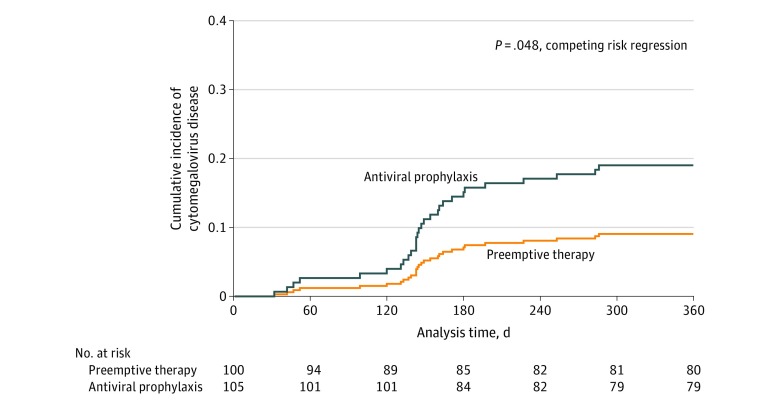
The incidence of CMV disease by 12 months was significantly lower in the preemptive therapy vs antiviral prophylaxis group (9%, 9/100 [95% CI, 3.3%-14.7%] vs 19%, 20/105 [95% CI, 14.4%-26.7%], respectively; P = .04; difference, 10% [95% CI, 0.5%-19.6%]), and resulted primarily from a reduction in delayed-onset disease (beyond day 100) (6% [6/100] vs 17% [18/105]; P = .01; difference, 11% [95% CI, 2.4%-19.9%]) (Table 2). CMV disease criteria in both groups are shown in eTable 1 in Supplement 2. The cumulative incidence of CMV disease, with death as a competing risk, is shown in Figure 2.
Table 2. Primary, Secondary, and Exploratory Outcomes in the Study Groups.
| No. (%) | P valuea | ||
|---|---|---|---|
| Preemptive therapy (n = 100) | Antiviral prophylaxis (n = 105) | ||
| Primary outcome (adjudicated CMV disease events) | |||
| CMV disease | 9 (9) | 20 (19) | .04 |
| Type of CMV disease | |||
| Syndromeb | 5 (5) | 11 (11) | .14 |
| End organb | 4 (4) | 9 (9) | .18 |
| Hepatitis, No. | 2 | 6 | |
| Gastrointestinal, No. | 2 | 1 | |
| Multiorgan, No. | 0 | 2 | |
| Time to onset after transplant | |||
| Within 100 d | 3 (3) | 2 (2) | .60 |
| After 100 d (postintervention period) | 6 (6) | 18 (17) | .01 |
| Secondary outcomes (up to 12 mo) | |||
| Allograft rejection | 28 (28) | 26 (25) | .60 |
| Graft lossc | 2 (2) | 2 (2) | .96 |
| Opportunistic infections (total)d | 25 (25) | 28 (27) | .79 |
| Bacterial infectionse | 23 (23) | 26 (25) | .77 |
| Bacteremiaf | 13 (13) | 14 (13) | .94 |
| Pneumonia | 3 (3) | 9 (9) | .13 |
| Intra-abdominal | 14 (14) | 13 (12) | .73 |
| Other | 5 (5) | 5 (5) | .92 |
| Invasive fungal infectionse | 4 (4) | 9 (9) | .18 |
| candidiasis | 2 (2) | 6 (6) | .17 |
| aspergillosis | 0 | 2 (2) | .50 |
| Otherg | 2 (2) | 1 (1) | .61 |
| Preemptive therapy (n = 92)h | Antiviral prophylaxis (n = 96)h | P valuea | |
| Exploratory outcomes (after 12 mo until end of follow-up)i | |||
| Allograft rejection | 9 (10) | 7 (7) | .54 |
| Graft lossb | 2 (2) | 0 | .24 |
| Opportunistic infections (total)c | 8 (8) | 8 (8) | .92 |
| Bacterial infectionsd | 8 (8) | 8 (8) | .93 |
| Bacteremiae | 4 (4) | 3 (3) | .66 |
| Pneumonia | 2 (2) | 0 | .24 |
| Intra-abdominal | 5 (5) | 3 (3) | .49 |
| Other | 1 (1) | 2 (2) | .59 |
| Invasive fungal infections | 2 (2) | 1 (1) | .62 |
| candidiasis | 1 (1) | 0 | .49 |
| Cryptococcosis | 0 | 1 (1) | .52 |
| Otherj | 1 (1) | 0 | .49 |
| Malignancies | 18 (20) | 18 (19) | .89 |
| Recurrent liver neoplasms, No. | 4 | 5 | |
| Hepatocellular carcinoma | (2) | (5) | |
| Neuroendocrine tumors and adenocarcinoma | (2) | (0) | |
| Posttransplant lymphoproliferative disorder, No. | 0 | 2 | |
| Other malignancies, No. | 14k | 11l | |
| End-stage kidney disease | |||
| Any KRT requirement | 7 (8) | 17 (18) | .07 |
| Kidney transplant | 1 (1) | 0 | .49 |
Abbreviations: CMV, cytomegalovirus; KRT, kidney replacement therapy.
CMV disease comparison was done using the Mantel-Haenszel test, all other categorical data were compared using the χ2 test.
See Box.
Graft loss was due to retransplant in all cases.
Some patients had both bacterial and fungal infections.
Numbers represent unique patients with infection.
Patients may have had more than 1 type of infection.
Includes 1 case with mucormycosis and 1 unknown fungus in the preemptive therapy group and 1 dematiaceous mold in the prophylaxis group.
Eight patients in the preemptive therapy group and 9 in the prophylaxis group declined long-term follow-up.
Follow-up was a median of 3.2 years (range, 1-5.2 years).
Includes 1 unknown fungus in the preemptive group.
Includes 7 patients with cutaneous and 1 patient each with lung, breast, prostate, oropharyngeal, lymphatic, heart, and donor-derived adenocarcinoma.
Includes 9 patients with cutaneous and 1 patient each with breast and esophageal malignancy.
Figure 2. Cumulative Incidence of Cytomegalovirus (CMV) Disease With Death as a Competing Risk.
Cumulative incidence curves of CMV disease show that the antiviral prophylaxis group had more postprophylaxis (delayed-onset) CMV disease than the preemptive therapy group (P = .048); the curves begin to separate about 4 to 6 weeks after the study drug administration period. Death prior to CMV disease was considered a competing risk. The number at risk is patients alive without CMV disease. The median follow-up for patients was 1152 days (interquartile range, 541 to 1537 days) in the preemptive therapy group and 1020 days (interquartile range, 588 to 1450 days) in the antiviral prophylaxis group.
Secondary Outcomes
The incidence of rejection (28% vs 25%; difference, 3% [95% CI, −9% to 15%]), opportunistic infections (25% vs 27%; difference, 2% [95% CI, −14% to 10%]), graft loss due to retransplantation (2% vs 2%; difference, <1% [95% CI, −4% to 4%]), neutropenia (absolute neutrophil count <500/μL) (13% vs 10%; difference, 3% [95% CI, −5% to 12%]), and receipt of 1 or more doses of granulocyte colony-stimulating factor for the management of neutropenia (6% vs 7%; difference, 1% [95% CI, −7% to 6%) did not differ significantly for preemptive therapy vs antiviral prophylaxis, respectively (Table 2; eTable 2 in Supplement 2). All-cause mortality at last follow-up was 15% for the preemptive therapy group vs 19% for the antiviral prophylaxis group (difference, 4% [95% CI, −14% to 6%]; P = .46) (eFigure 2 in Supplement 2).
Exploratory Outcomes
The median time to onset of CMV disease was day 139 (IQR, 99-180) in the preemptive therapy group and day 148 (IQR, 140-167) in the antiviral prophylaxis group (P = .34). Other clinical outcomes, including opportunistic infections, graft loss due to retransplant, new malignancy, requirement of kidney replacement therapy (Table 2), and all-cause mortality (eFigure 2 in Supplement 2), did not differ significantly between the 2 groups. Among 205 randomized patients, 174 had a sufficient sample for nAb assay (preemptive therapy, 83/100 [83%]; antiviral prophylaxis, 91/105 [87%]) and 152 for T-cell analyses (preemptive therapy, 73/100 [73%]; antiviral prophylaxis, 79/105 [75%]).
nAb to Pentameric Complex
The proportion of patients who developed nAb at day 100 was significantly higher with preemptive therapy vs antiviral prophylaxis: 42.5% (31/73) vs 26.6% (21/79) (difference, 15.9% [95% CI, 0.8%-31%]; P = .04), respectively. Within the preemptive therapy group, nAbs were more likely to develop in those with preceding viremia than without viremia: 30/63 (47.6%) vs 1/10 (10%) (difference, 37.6% [95% CI, 4.8%-70.5%]; P = .03).
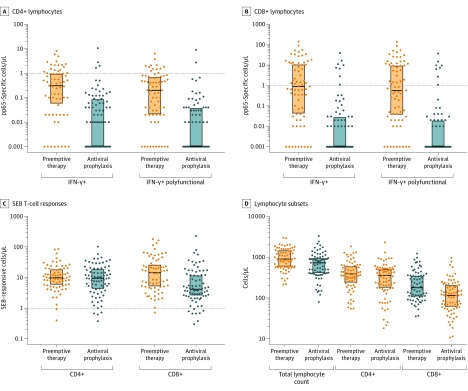
CMV-Specific T-Cell Responses
CMV-specific responses expressed as the number of T-cells producing IFN-γ or IFN-γ and at least 1 other marker (ie, polyfunctional) per microliter of blood are shown in Figure 3. The median CD4+ (Figure 3A) and CD8+ (Figure 3B) T-cell IFN-γ and IFN-γ polyfunctional responses were significantly higher for preemptive therapy vs antiviral prophylaxis: IFN-γ, 0.31 vs 0.01 cells/μL (difference, 0.24 [95% CI, 0.09-0.45]; P = .009) and 0.87 vs 0 cells/μL (difference, 0.64 [95% CI, 0.31-1.46]; P < .001); IFN-γ polyfunctional, 0.2 vs 0 cells/μL (difference, 0.16 [95% CI, 0.04-0.40]; P = .02) and 0.56 vs 0 cells/μL (difference, 0.53 [95% CI, 0.19-1.41]; P = .001), respectively. Corresponding T-cell IFN-γ responses to mitogen Staphylococcus aureus enterotoxin B (Figure 3C) were not significantly different between groups for CD4+ T cells but were higher for CD8+ T cells in the preemptive therapy group. Among patients undergoing preemptive therapy, CD8+ T-cell responses were significantly higher in those with preceding viremia vs without viremia: IFN-γ, 52/63 (82.5% [95% CI, 70.9%-90.9%]) vs 0/10 (0% [95% CI, 0%-30.8%], P < .001); IFN-γ polyfunctional, 49/63 (77.8% [95% CI, 65.5%-87.3%]) vs 0/10 (0% [95% CI, 0%-30.8%]; P < .001). Exploratory immune outcomes at 6 and 12 months are not reported in this article.
Figure 3. Cytomegalovirus (CMV)-Specific T-Cell Responses and Lymphocyte Subsets.
CMV pp65-specific T-cell responses were stronger following preemptive therapy than with antiviral prophylaxis in both CD4+ (A) or CD8+ (B) T cells expressing interferon-γ (IFN-γ) without regard for other markers (IFN-γ; left side of x-axis; CD4+, P = .009; CD8+, P < .001) or IFN-γ and at least 1 other marker (IFN-γ polyfunctional; right side of x-axis; CD4+, P = .02; CD8+, P < .001). C, Staphylococcal enterotoxin B (SEB)–responsive T cells expressing any marker, a measure of global immune function, were only different for CD8+ T cells between preemptive therapy and antiviral prophylaxis groups (P = .01). D, Lymphocyte subset counts were greater following preemptive therapy (total lymphocyte count; P = .006), with significantly more CD8+ T cells after preemptive therapy than antiviral prophylaxis (P < .001). The higher number of SEB-responsive CD8+ T cells following preemptive therapy may relate to greater clonal expansion of CMV-specific CD8+ T cells. Box edges represent the third (upper) and first (lower) quartiles, and the central line denotes the median. The dots indicate actual data points for the data depicted along the y-axis. For all comparisons, there were 73 patients in the preemptive therapy group and 79 in the antiviral prophylaxis group.
Post Hoc Outcomes
Eighty-one percent (81/100) of the preemptive therapy group developed CMV viremia within a median of 24 days after transplant (IQR, 17-29). Median initial viral load was 120 IU/mL (IQR, 41-360). Preemptive therapy was initiated a median of 2 days (IQR, 1-4) after the detection of viremia. In the preemptive therapy group, 92% (1207/1313) of the surveillance samples were collected within protocol-specified intervals. Forty-eight percent (48/100) of patients in the preemptive therapy group had recurrent viremia. Duration of valganciclovir use during the intervention period was a median of 57 days (IQR, 39-66.5) vs 97 days (IQR, 90-99) (P = .001) in the preemptive therapy and antiviral prophylaxis groups, respectively. The total amount of valganciclovir used was 7023 g for 100 patients (70.2 g/patient) for preemptive therapy and 7068 g for 105 patients (67.3g/patient) for antiviral prophylaxis (difference, 2.9 [95% CI, −23 to 33]; P = .43).
Three patients in the preemptive therapy group and 2 in the antiviral prophylaxis group developed CMV disease within 100 days. All 3 patients with CMV in the preemptive therapy group had preceding viremia. These included 1 thymoglobulin recipient with CMV hepatitis who had a 10-day delay in drug initiation after detection of viremia, 1 patient who developed CMV syndrome on day 98 during a 5-day period when antiviral drug was withheld due to abdominal discomfort, and 1 patient with CMV syndrome on day 32 who had diarrhea due to Clostridioides difficile the week before that may have affected drug absorption. Two patients in the prophylaxis group developed breakthrough CMV disease (syndrome) within 100 days (days 47 and 52). Both had multiple preceding antiviral dose reductions for kidney dysfunction before developing disease.
In the generalized linear mixed model with site as a random effect, antiviral prophylaxis vs preemptive therapy was associated with an increased relative risk (RR) of CMV disease (RR, 1.11 [95% CI, 1.01-1.22]; P = .04) and of delayed-onset CMV disease (RR, 1.12 [95% CI, 1.03-1.22]; P = .01).
Because patients returned to standard of care after the study intervention period, non-CMV disease–related valganciclovir use after day 100 through 12 months was assessed for whether differential antiviral use after day 100 between groups had an effect on the primary outcome. The number of patients who received valganciclovir, total days of use in treated patients, and valganciclovir use per person did not differ significantly between the preemptive therapy vs antiviral prophylaxis groups (eTable 3 in Supplement 2).
Adverse Events
Protocol-specified adverse events occurred in 2% (2/100) of the patients in the preemptive therapy group (pericardial effusion in 1 patient and kidney stones in another patient) and none (0/105) in the antiviral prophylaxis group (eTable 2 in Supplement 2).
Discussion
In this randomized clinical trial in CMV-seronegative liver transplant recipients with seropositive donors, preemptive therapy compared with antiviral prophylaxis resulted in a lower incidence of CMV disease (in particular delayed-onset disease) by 12 months after transplant. Other clinical outcomes (acute allograft rejection, opportunistic infections, graft, and patient survival) did not differ significantly between the 2 groups.
CMV-specific immune responses were exploratory end points and, therefore, all findings should be considered tentative and, at best, hypothesis-generating. This study showed that T-cell responses (associated with protection against CMV replication or disease)21,22,23,24 and neutralizing antibodies (considered important in the context of primary CMV infection)25 were significantly increased with preemptive therapy compared with antiviral prophylaxis. Prior studies in CMV-seropositive hematopoietic cell transplant recipients have shown conflicting results regarding enhancement of CMV-specific immunity with preemptive therapy.26,27,28 The present study shows that complete viral suppression with antiviral prophylaxis vs controlled viral replication in preemptive therapy was associated with suboptimal CMV-specific immunity, with greater impairment in CD8+ than CD4+ T-cell responses (Figure 3). With the advent of CMV vaccines that are in early development and not yet in clinical use, it might become feasible to elicit these responses without the risk of CMV replication inherent in preemptive therapy.
Strengths of this study include the randomized trial design; the clinically relevant end point of CMV disease for efficacy that was adjudicated by an independent adjudication committee unaware of the study group assignment of the patients; and use of a central laboratory for virologic assays.29 Comprehensive immunologic assessments of both humoral and T-cell immune responses were performed and analyzed by blinded personnel, and the polyfunctional T-cell assay was developed and validated according to best practices in flow cytometry.
Limitations
This study has several limitations. First, blinding of the intervention was not feasible for logistical reasons. Second, given the known low rates (~ 2.5%) of breakthrough viremia during valganciclovir prophylaxis,30 CMV viremia was not assessed during antiviral prophylaxis (compatible with current guidelines), so a direct comparison of the relationship between viremia and immune responses was not feasible for the prophylaxis group. Third, because of important biologic and immunosuppression intensity differences among different organ transplants, these results should not be extrapolated to other recipient CMV-seronegative and donor CMV-seropositive organ transplant setting without further study. Fourth, because the observed difference in CMV disease rate between the 2 groups was less than predicted, if 1 additional CMV disease event in the preemptive therapy group and 1 less event in the prophylaxis group had occurred, the prespecified threshold for statistical difference would not have been met. Fifth, adherence to monitoring and timely initiation of antiviral therapy are important components of preemptive therapy that might not be feasible for all transplant programs. However, preemptive therapy has been the dominant strategy and standard of care for CMV prevention for approximately 30 years in hematopoietic cell transplant recipients who are much sicker than organ transplant patients31 and published data demonstrate feasibility of preemptive therapy in organ transplant recipients in clinical nonresearch settings as well.13,32,33,34 Regardless, each center should consider which approach is more suitable for CMV prevention at their particular institution based on their resources.
Conclusions
Among CMV-seronegative liver transplant recipients with seropositive donors, the use of preemptive therapy, compared with antiviral prophylaxis, resulted in a lower incidence of CMV disease over 12 months. Further research is needed to replicate these findings and assess long-term outcomes.
Trial Protocol
eMethods. Immune Assay Methods
eReferences
eFigure 1. Gating Strategy
eFigure 2. Kaplan-Meier Plot Showing Survival in the Study Groups
eTable 1. Number and Percentage of Participants With CMV Disease Diagnoses Based on Each Criterion
eTable 2. Adverse Events in the Study Participants
eTable 3. Non-CMV Disease–Related Valganciclovir Use After Day 100 in Study Participants
Data Sharing Statement
References
- 1.Griffiths P, Lumley S. Cytomegalovirus. Curr Opin Infect Dis. 2014;27(6):554-559. doi: 10.1097/QCO.0000000000000107 [DOI] [PubMed] [Google Scholar]
- 2.Levitsky J, Singh N, Wagener MM, Stosor V, Abecassis M, Ison MG. A survey of CMV prevention strategies after liver transplantation. Am J Transplant. 2008;8(1):158-161. [DOI] [PubMed] [Google Scholar]
- 3.Gardiner BJ, Chow JK, Price LL, Nierenberg NE, Kent DM, Snydman DR. Role of secondary prophylaxis with valganciclovir in the prevention of recurrent cytomegalovirus disease in solid organ transplant recipients. Clin Infect Dis. 2017;65(12):2000-2007. doi: 10.1093/cid/cix696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khurana MP, Lodding IP, Mocroft A, et al. Risk factors for failure of primary (Val)ganciclovir prophylaxis against cytomegalovirus infection and disease in solid organ transplant recipients. Open Forum Infect Dis. 2019;6(6):ofz215. doi: 10.1093/ofid/ofz215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boudreault AA, Xie H, Rakita RM, et al. Risk factors for late-onset cytomegalovirus disease in donor seropositive/recipient seronegative kidney transplant recipients who receive antiviral prophylaxis. Transpl Infect Dis. 2011;13(3):244-249. doi: 10.1111/j.1399-3062.2011.00624.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Limaye AP, Bakthavatsalam R, Kim HW, et al. Late-onset cytomegalovirus disease in liver transplant recipients despite antiviral prophylaxis. Transplantation. 2004;78(9):1390-1396. doi: 10.1097/01.TP.0000145989.22373.03 [DOI] [PubMed] [Google Scholar]
- 7.Natori Y, Humar A, Husain S, et al. Recurrence of CMV infection and the effect of prolonged antivirals in organ transplant recipients. Transplantation. 2017;101(6):1449-1454. doi: 10.1097/TP.0000000000001338 [DOI] [PubMed] [Google Scholar]
- 8.Kotton CN, Kumar D, Caliendo AM, et al. ; The Transplantation Society International CMV Consensus Group . The Third International Consensus Guidelines on the management of cytomegalovirus in solid-organ transplantation. Transplantation. 2018;102(6):900-931. doi: 10.1097/TP.0000000000002191 [DOI] [PubMed] [Google Scholar]
- 9.Witzke O, Hauser IA, Bartels M, Wolf G, Wolters H, Nitschke M; VIPP Study Group . Valganciclovir prophylaxis versus preemptive therapy in cytomegalovirus-positive renal allograft recipients: 1-year results of a randomized clinical trial. Transplantation. 2012;93(1):61-68. doi: 10.1097/TP.0b013e318238dab3 [DOI] [PubMed] [Google Scholar]
- 10.Paya CV, Wilson JA, Espy MJ, et al. Preemptive use of oral ganciclovir to prevent cytomegalovirus infection in liver transplant patients: a randomized, placebo-controlled trial. J Infect Dis. 2002;185(7):854-860. doi: 10.1086/339449 [DOI] [PubMed] [Google Scholar]
- 11.Reischig T, Jindra P, Hes O, Svecová M, Klaboch J, Treska V. Valacyclovir prophylaxis versus preemptive valganciclovir therapy to prevent cytomegalovirus disease after renal transplantation. Am J Transplant. 2008;8(1):69-77. [DOI] [PubMed] [Google Scholar]
- 12.Benmarzouk-Hidalgo OJ, Cisneros JM, Cordero E, et al. Therapeutic effect of the acquisition of cytomegalovirus-specific immune response during preemptive treatment. Transplantation. 2011;91(8):927-933. doi: 10.1097/TP.0b013e3182115ba2 [DOI] [PubMed] [Google Scholar]
- 13.Sun HY, Cacciarelli TV, Wagener MM, Singh N. Preemptive therapy for cytomegalovirus based on real-time measurement of viral load in liver transplant recipients. Transpl Immunol. 2010;23(4):166-169. doi: 10.1016/j.trim.2010.06.013 [DOI] [PubMed] [Google Scholar]
- 14.Mattes FM, Hainsworth EG, Hassan-Walker AF, et al. Kinetics of cytomegalovirus load decrease in solid-organ transplant recipients after preemptive therapy with valganciclovir. J Infect Dis. 2005;191(1):89-92. doi: 10.1086/425905 [DOI] [PubMed] [Google Scholar]
- 15.Limaye AP, Green ML, Edmison BC, et al. Prospective assessment of cytomegalovirus immunity in high-risk donor-seropositive/recipient-seronegative liver transplant recipients receiving either preemptive therapy or antiviral prophylaxis. J Infect Dis. 2019;220(5):752-760. doi: 10.1093/infdis/jiz181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Emery VC, Hassan-Walker AF, Burroughs AK, Griffiths PD. Human cytomegalovirus (HCMV) replication dynamics in HCMV-naive and -experienced immunocompromised hosts. J Infect Dis. 2002;185(12):1723-1728. doi: 10.1086/340653 [DOI] [PubMed] [Google Scholar]
- 17.Razonable RR, Humar A. Cytomegalovirus in solid organ transplant recipients: guidelines of the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019;33(9):e13512. doi: 10.1111/ctr.13512 [DOI] [PubMed] [Google Scholar]
- 18.Humar A, Lebranchu Y, Vincenti F, et al. The efficacy and safety of 200 days valganciclovir cytomegalovirus prophylaxis in high-risk kidney transplant recipients. Am J Transplant. 2010;10(5):1228-1237. doi: 10.1111/j.1600-6143.2010.03074.x [DOI] [PubMed] [Google Scholar]
- 19.Humar A, Michaels M; AST ID Working Group on Infectious Disease Monitoring . American Society of Transplantation recommendations for screening, monitoring and reporting of infectious complications in immunosuppression trials in recipients of organ transplantation. Am J Transplant. 2006;6(2):262-274. doi: 10.1111/j.1600-6143.2005.01207.x [DOI] [PubMed] [Google Scholar]
- 20.Horton H, Thomas EP, Stucky JA, et al. Optimization and validation of an 8-color intracellular cytokine staining (ICS) assay to quantify antigen-specific T cells induced by vaccination. J Immunol Methods. 2007;323(1):39-54. doi: 10.1016/j.jim.2007.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nebbia G, Mattes FM, Smith C, et al. Polyfunctional cytomegalovirus-specific CD4+ and pp65 CD8+ T cells protect against high-level replication after liver transplantation. Am J Transplant. 2008;8(12):2590-2599. doi: 10.1111/j.1600-6143.2008.02425.x [DOI] [PubMed] [Google Scholar]
- 22.Giménez E, Blanco-Lobo P, Muñoz-Cobo B, et al. Role of cytomegalovirus (CMV)-specific polyfunctional CD8+ T-cells and antibodies neutralizing virus epithelial infection in the control of CMV infection in an allogeneic stem-cell transplantation setting. J Gen Virol. 2015;96(9):2822-2831. doi: 10.1099/vir.0.000203 [DOI] [PubMed] [Google Scholar]
- 23.Snyder LD, Chan C, Kwon D, et al. Polyfunctional T-cell signatures to predict protection from cytomegalovirus after lung transplantation. Am J Respir Crit Care Med. 2016;193(1):78-85. doi: 10.1164/rccm.201504-0733OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Camargo JF, Wieder ED, Kimble E, et al. Deep functional immunophenotyping predicts risk of cytomegalovirus reactivation after hematopoietic cell transplantation. Blood. 2019;133(8):867-877. doi: 10.1182/blood-2018-10-878918 [DOI] [PubMed] [Google Scholar]
- 25.Gerna G, Lilleri D. Human cytomegalovirus (HCMV) infection/re-infection: development of a protective HCMV vaccine. New Microbiol. 2019;42(1):1-20. [PubMed] [Google Scholar]
- 26.Li CR, Greenberg PD, Gilbert MJ, Goodrich JM, Riddell SR. Recovery of HLA-restricted cytomegalovirus (CMV)-specific T-cell responses after allogeneic bone marrow transplant: correlation with CMV disease and effect of ganciclovir prophylaxis. Blood. 1994;83(7):1971-1979. doi: 10.1182/blood.V83.7.1971.1971 [DOI] [PubMed] [Google Scholar]
- 27.Hakki M, Riddell SR, Storek J, et al. Immune reconstitution to cytomegalovirus after allogeneic hematopoietic stem cell transplantation: impact of host factors, drug therapy, and subclinical reactivation. Blood. 2003;102(8):3060-3067. doi: 10.1182/blood-2002-11-3472 [DOI] [PubMed] [Google Scholar]
- 28.Boeckh M, Nichols WG, Chemaly RF, et al. Valganciclovir for the prevention of complications of late cytomegalovirus infection after allogeneic hematopoietic cell transplantation: a randomized trial. Ann Intern Med. 2015;162(1):1-10. doi: 10.7326/M13-2729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.US Department of Health and Human Services, US Food and Drug Administration, Center for Drug Evaluation and Research Cytomegalovirus in Transplantation: Developing Drugs to Treat or Prevent Disease Guidance for Industry. US Food and Drug Administration; 2018. [Google Scholar]
- 30.Paya C, Humar A, Dominguez E, et al. ; Valganciclovir Solid Organ Transplant Study Group . Efficacy and safety of valganciclovir vs oral ganciclovir for prevention of cytomegalovirus disease in solid organ transplant recipients. Am J Transplant. 2004;4(4):611-620. doi: 10.1111/j.1600-6143.2004.00382.x [DOI] [PubMed] [Google Scholar]
- 31.Goodrich JM, Mori M, Gleaves CA, et al. Early treatment with ganciclovir to prevent cytomegalovirus disease after allogeneic bone marrow transplantation. N Engl J Med. 1991;325(23):1601-1607. doi: 10.1056/NEJM199112053252303 [DOI] [PubMed] [Google Scholar]
- 32.Liu AW, Jutivorakool K, Fisher CE, et al. Comparison of preemptive therapy and antiviral prophylaxis for prevention of cytomegalovirus in seropositive liver transplant recipients. Transplantation. 2018;102(4):632-639. doi: 10.1097/TP.0000000000002029 [DOI] [PubMed] [Google Scholar]
- 33.Singh N, Wannstedt C, Keyes L, et al. Valganciclovir as preemptive therapy for cytomegalovirus in cytomegalovirus-seronegative liver transplant recipients of cytomegalovirus-seropositive donor allografts. Liver Transpl. 2008;14(2):240-244. doi: 10.1002/lt.21362 [DOI] [PubMed] [Google Scholar]
- 34.Atabani SF, Smith C, Atkinson C, et al. Cytomegalovirus replication kinetics in solid organ transplant recipients managed by preemptive therapy. Am J Transplant. 2012;12(9):2457-2464. doi: 10.1111/j.1600-6143.2012.04087.x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eMethods. Immune Assay Methods
eReferences
eFigure 1. Gating Strategy
eFigure 2. Kaplan-Meier Plot Showing Survival in the Study Groups
eTable 1. Number and Percentage of Participants With CMV Disease Diagnoses Based on Each Criterion
eTable 2. Adverse Events in the Study Participants
eTable 3. Non-CMV Disease–Related Valganciclovir Use After Day 100 in Study Participants
Data Sharing Statement