Abstract
Flu vaccination is recommended among healthcare workers (HCWs). The low vaccination coverage registered in our hospital among HCWs called for new engaging approaches to improve flu vaccination coverage. The aim of this study was to evaluate the efficacy of different strategies implemented during the last four years (2015–2019). A quasi-experimental study was conducted, involving almost 4000 HCWs each year. Starting from the 2015–2016 campaign, new evidence-based strategies were progressively implemented. At the end of each campaign, an evaluation of the vaccination coverage rate reached was performed. Moreover, during the last three campaigns, differences in coverage among job category, wards involved or not in on-site vaccination (OSV) intervention, age classes and gender were analyzed. An increasing flu vaccination coverage rate was registered, from 6% in 2015–2016 to almost 22% at the end of 2018–2019. The overall number of vaccinated HCWs increased, especially at younger ages. OSV strategy always leads to better results, and physicians always show a higher vaccination coverage than nurses and other HCWs. The implemented strategies were effective in achieving higher flu vaccination coverage among HCWs in our hospital and therefore can be considered valuable examples of good prevention practices in hospital settings.
Keywords: flu vaccination, healthcare workers, teaching hospital, on-site vaccination, preventive medicine, vaccination coverage
1. Introduction
Influenza is an infectious disease with a high impact in terms of incidence, morbidity and mortality [1,2,3]. It is responsible for an increase in hospitalizations and direct and indirect costs all over the world, thus representing a serious public health issue [1,4,5,6]. Seasonal flu vaccination is one of the most important strategies for preventing influenza and reducing its healthcare, social and economic impact [5,7,8,9]. According to the World Health Organization (WHO) recommendations, at least 75% (optimal level: 95%) of at-risk individuals, including Healthcare Workers (HCWs), should be vaccinated in order to optimize the prevention and control of influenza and to reduce its impact [10]. In Italy, this recommendation has been included by the Ministry of Health in the National Vaccination Plan 2017–2019 (Piano Nazionale Prevenzione Vaccinale, PNPV) [11] and in a national law concerning health and safety at work [12]. These norms recommend, among HCWs exposed to biological agents, general and special protective evidence-based measures to prevent the transmission of influenza: washing and cleaning hands frequently, maintaining good respiratory hygiene, using facemasks and undergoing seasonal flu vaccination [11,12]. During the influenza season, in fact, HCWs can be affected by clinical and sub-clinical (oligosymptomatic or asymptomatic) flu and may therefore transmit influenza virus to patients, increasing their length of hospital stay, the costs for testing and treatment and the risk of complications, which can also lead to severe consequences [13,14,15,16]. Vaccination among HCWs involved in the everyday care of patients limits the spread of the virus, ensuring healthcare assistance continuity, thanks to both the individual and herd immunity [13,14,17,18]. Moreover, it reduces absenteeism [8,19,20].
Despite this, the vaccination coverage rate among HCWs is usually lower than what is recommended [10,21,22] for several reasons [23,24,25,26], even if rates achieved among different countries are frequently divergent. For instance, during the 2017–2018 season, in the USA, where vaccination is mandatory for HCWs, the coverage rate reached more than 90% among HCWs in hospital settings [27]. In Europe, where vaccination is not mandatory, the median HCWs vaccine coverage rate in 2016–2017 was 30.2% [22]. In Italy, the mean national influenza vaccination coverage among HCWs was 15.6% during the 2016–2017 influenza season [22], with huge differences among regions, hospitals and HCWs professionals [19,28,29,30,31]. According to two systematic reviews, in Italy, it is possible to estimate the influenza vaccination coverage close to 13% among nurses and 23% among physicians [32,33].
In our Fondazione Policlinico Universitario “A. Gemelli” IRCCS (FPG) hospital, a very low flu vaccination coverage rate among HCWs was registered during the 2014–2015 season [34]. Based on this result, increasing the vaccination coverage rate for influenza vaccination among HCWs represented (and still represents) a hard but essential challenge calling for new engaging, evidence-based approaches. For this reason, before the 2015–2016 flu campaign, a new internal program started with the scope of increasing flu vaccination coverage through the implementation of several initiatives.
The aim of this study was to evaluate the overall efficacy of the different strategies implemented in the FPG teaching hospital during the 2015–2016, 2016–2017, 2017–2018 and 2018–2019 influenza seasons to increase flu vaccination coverage among HCWs.
2. Materials and Methods
2.1. Setting, Study Design and Population
A quasi-experimental study was conducted in the Fondazione Policlinico Universitario Agostino Gemelli IRCCS (FPG), a large Italian Teaching Hospital located in Rome—Regione Lazio composed by two main buildings (the Policlinico Gemelli itself and the Presidio Columbus—CIC, a minor building nearby). It represents a regional and national excellence with 1500 beds and over 5500 employees. About 4000 of them are HCWs with daily contact with patients.
2.2. Implemented Strategies
Before the beginning of the 2015–2016 flu season, a multi-professional group focused on influenza vaccination was created to develop a “long-term, step-by-step” project aimed at increasing flu vaccination coverage rates among HCWs. Firstly, a literature search on vaccine hesitancy among HCWs and an internal audit with hospital key opinion leaders were performed. Concerns about safety, necessity and effectiveness of influenza vaccination, the lack of awareness of being potentially responsible for the transmission to patients, the lack of time and absent or inadequate vaccination policies and services were identified as main reasons to delay or refuse flu vaccination, both in the literature and in our setting [24,25,35,36,37,38]. Based on these evidences, starting from the 2015–2016 influenza season, different evidence-based strategies [24,39,40,41,42,43,44,45] were progressively implemented in the following seasons (Table 1).
Table 1.
Strategies implemented since 2015–2016 flu vaccination campaign.
| Strategy | Description | Flu Vaccination Campaign | |||
|---|---|---|---|---|---|
| 2015–2016 | 2016–2017 | 2017–2018 | 2018–2019 | ||
| Forum Theatre (FT) | Explained in the text | x | - | - | - |
| Opening ceremony | Opening ceremony of the influenza season campaign targeted at all HCWs: the results of the previous campaign were shown and people in attendance were invited to adhere to the campaign. | x | > | > | O award ceremony of the ward with the highest flu vaccination coverage reached in 2017–2018 |
| Opening hours extension | Opening hours extension of the ambulatory located in the teaching hospital that provided the vaccination service free of charge. Baseline: 1 h twice a week. | x | o 1 h and a half (from 1 p.m. to 2.30 p.m.) 3 days/week |
o 2 h (from 12.30 a.m. to 2.30 p.m.) 5 days/week |
> |
| Second ambulatory | Opening of a new ambulatory for vaccination, located in another strategic place to reach different population (especially student, not involved in this study). Opening hours: 2 h 5 days per week. | x | > | > | > |
| E-mail invitation and reminders | Invitation and reminders via e-mail to undergo vaccination from the General Director and Chief Executive Officer, explaining the importance of the immunization among HCWs and the whole community plus specific information about where and when the internal vaccination service was provided. | x | o the OSV was included in information details |
> | > |
| Promotional and informative material | Promotional and informative material including pins, flyers and advertising posters were placed in different strategic locations (e.g., main and secondary entrances, departments corridors, walls near to elevators). | - | x | o graphic changes |
o further graphic changes |
| The on-site vaccination (OSV) intervention | Explained in the text | - | x | o ward increase |
o all hospital wards involved |
| Academic Detailing | Also called educational outreach visit, university-based educational detailing or educational visiting is a peer-to-peer educational sessions [43] aimed at nurse coordinators in order to get them involved in promoting vaccination with their colleagues [44]. | - | - | x | o frontal lessons removed; peer-to-peer interventions incremented |
| Non-economic incentive (one-hour leave) | A non-economic incentive, consisting in a one hour leave to all HCWs who got vaccinated against influenza. This was supported by an economic evaluation performed in our setting during the previous campaign that demonstrate the potential cost-effectiveness of this measure [45]. | - | - | - | x |
Legend: x. newly implemented; o. changed during the campaign considered in comparison with the previous one, followed by the explanation of the improvement done; >. maintained in the campaign as in the previous one; -. not implemented.
2.3. Forum Theater (FT)
FT is a peculiar methodology used, especially in social and political settings, with the purpose of promoting knowledge, attitude and practice changes [46]. It is characterized by a participative and pro-active approach to discuss a problem, in which the audience (the “spect-actors”) is involved in the plot and encouraged to suggest different resolution for the play and to directly come on stage and act [46]. Although already implemented in communities and hospital setting, to our knowledge, our experience represented the first application in the field of flu vaccination among HCWs [42].
2.4. The On-Site Vaccination (OSV) Intervention
This new bottom-up approach has been carried out since the 2016–2017 campaign. This strategy emerged as request from HCWs who participated at the FT [42]. Thought, this project has been already used elsewhere, as reported in the scientific literature [39,47,48,49,50,51]. The OSV consisted of personal visit by 2 trained medical residents in Hygiene and Preventive Medicine (Public Health) and/or Occupational Medicine to wards to perform influenza immunization counseling and to vaccinate free of charge HCWs who wanted to be vaccinated. The date of each OSV intervention was previously settled according to the director of the operative unit and the nurse coordinator of the ward involved. Every OSV session was preceded by an email remind directed to the nursing coordinator. During the 2018–2019 season, nursing students were involved in performing the OSV visits in addition to medical residents.
Selection Criteria for the OSV Intervention Implemented during the Different Influenza Campaigns
Before the 2016–2017 influenza season campaign, the operative units and wards of the FPG were grouped in 36 macro-areas, according to clinical and functional characteristics (e.g., all cardiovascular wards were grouped in one macro-area; hematology, radiotherapy and medical oncology wards were grouped in the onco-hematology macro-area). For the 2016–2017 campaign, considering the healthcare workforce available to perform the OSV intervention, a random selection of 12 out of 36 macro-areas (33%) was done, using a random number generator without repetition in Excel. In the 2017–2018 season, the OSV intervention was extended to the wards nearby the ones involved during the previous campaign, utilizing therefore a “geographical” criterion (proximity) rather than the “functional” one used in the first year. During the last flu vaccination campaign (2018–2019 season), all the hospital wards were involved in the OSV intervention; therefore, no wards were available to be used as control (no-OSV) for the analysis.
2.5. Data Collection, Management and Ethical Committee
Data such as age, gender, professional category, and being vaccinated during the campaign and in the previous season (from 2017–2018 campaign) were collected and stored in an electronic database, accessible by password only to the data manager. In particular, to register vaccination status as “yes”, only the vaccinations administered by FPG staff inside the hospital were considered. HCWs were grouped per job categories in medical doctors (physicians), nurses and other HCWs (OHCWs; e.g., obstetricians, physiotherapists, etc.). Variable “age”, collected as continuous data, was subsequently grouped in 5 classes: min/34; 35/44; 45/54; 55/64; and 65/max. These class cutoffs were chosen because, in Italy, flu vaccination is recommended and offered for free to all the people over 65 years [11]. Moreover, during the 2018–2019 season, the role played by the leaders (both nurse coordinators and head physicians of each ward involved) in increasing the vaccination coverage of the HCWs directly employed was investigated, analyzing the vaccination coverage rate of the HCWs with a vaccinated leader compared to that one of the HCWs with a non-vaccinated leader.
The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee the FPG Teaching Hospital—Università Cattolica del Sacro Cuore, Rome (Reference n. 47616/17 ID 1786 and n. 41409/18 ID 2263).
2.6. Statistical Analysis
At the end of each influenza season (2015–2016, 2016–2017, 2017–2018 and 2018–2019), a cross-sectional study was carried out to evaluate the vaccination coverage rate reached and the overall efficacy of the implemented strategies. The 2015–2016 vaccination coverage was used as the “starting point” to evaluate the effectiveness of the strategies implemented during the following years, even though it was partially influenced by some of them, in particular by the FT (which, nevertheless, was not implemented again in the following campaigns). Data collected were summarized in terms of absolute and relative frequencies or mean and standard deviation (SD) for qualitative and quantitative variables, respectively. Statistically significant differences among groups were tested through χ2 test or t-test, where applicable. The percentage variations among seasons (2016–2017 and 2017–2018; 2017–2018 and 2018–2019) were calculated to better analyze changes before and after each campaign. A multivariate logistic regression analysis was performed to assess differences in flu vaccination coverage between groups for each of the last three campaigns (2016–2017, 2017–2018 and 2018–2019). The variables included in the multivariate analysis were age class, gender, job category and OSV. In the logistic analysis, we decided to use the discrete age classes instead of the continuous variable, because the continuous variable showed departure from linearity in the models. Statistical significance was set at 0.05. Analyses were performed by using STATA 15.1 Software (StataCorp, Texas).
3. Results
Starting from the 2015–2016 campaign, an increasing flu vaccination coverage rate among HCWs of the FPG teaching hospital was registered. Characteristics of the population investigated during the 3 following seasons (2016–2017, 2017–2018 and 2018–2019) are shown in Table 2; the results of the multivariate analysis (one for each flu vaccination campaign) are presented in Table 3.
Table 2.
Characteristics of the HCWs and univariate analysis for the 2016–2017, 2017–2018 and 2018–2019 flu vaccination campaigns and percentage of increasing from 2016–2017 to 2017–2018 and from 2017–2018 to 2018–2019.
| Variables | 2016–2017 | 2017–2018 | 2018–2019 | Δ% from 2016–2017 to 2017–2018 |
Δ% from 2017–2018 to 2018–2019 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Vaccinated | Total HCWs | % | p | Vaccinated | Total HCWs | % | p | Vaccinated | Total HCWs | % | p | |||
| Age class *§ | ||||||||||||||
| ≤34 | 31 | 653 | 4.75 | <0.001 | 63 | 652 | 9.66 | <0.001 | 163 | 868 | 18.78 | <0.001 | 103.37 | 94.41 |
| 35–44 | 81 | 1085 | 7.47 | 125 | 1071 | 11.67 | 262 | 1216 | 21.55 | 56.22 | 84.66 | |||
| 45–54 | 98 | 1104 | 8.88 | 156 | 1142 | 13.66 | 230 | 1224 | 18.79 | 53.83 | 37.55 | |||
| 55–64 | 105 | 673 | 15.60 | 150 | 748 | 20.05 | 245 | 821 | 29.84 | 28.53 | 48.83 | |||
| ≥65 | 15 | 41 | 36.59 | 20 | 51 | 39.22 | 33 | 119 | 27.73 | 7.19 | −29.30 | |||
| Gender * | ||||||||||||||
| F | 140 | 2304 | 6.08 | <0.001 | 257 | 2385 | 10.78 | <0.001 | 533 | 2767 | 19.26 | <0.001 | 77.30 | 78.66 |
| M | 190 | 1252 | 15.18 | 257 | 1279 | 20.09 | 400 | 1481 | 27.01 | 32.35 | 34.44 | |||
| Job Category | ||||||||||||||
| Physicians | 197 | 1015 | 19.41 | <0.001 | 256 | 1015 | 25.22 | <0.001 | 448 | 1323 | 33.86 | <0.001 | 29.93 | 34.26 |
| Nurses | 107 | 1959 | 5.46 | 183 | 1960 | 9.34 | 338 | 2005 | 16.86 | 71.06 | 80.51 | |||
| OHCWs | 36 | 680 | 5.29 | 75 | 689 | 10.89 | 147 | 920 | 15.98 | 105.86 | 46.74 | |||
| OSV | ||||||||||||||
| No | 183 | 2534 | 7.22 | <0.001 | 160 | 1806 | 8.86 | <0.001 | 22.71 | |||||
| Yes | 157 | 1120 | 14.02 | 354 | 1858 | 19.05 | 35.88 | |||||||
| Vaccinated during 2016–2017 | ||||||||||||||
| No | 279 | 3210 | 8.69 | <0.001 | 505 | 3134 | 16.11 | <0.001 | 85.39 | |||||
| Yes | 218 | 326 | 66.87 | 244 | 313 | 77.96 | 16.58 | |||||||
| Not present ° | 17 | 128 | 13.28 | 184 | 801 | 22.97 | 72.97 | |||||||
| Vaccinated during 2017–2018 | ||||||||||||||
| No | 412 | 3028 | 13.61 | <0.001 | ||||||||||
| Yes | 358 | 486 | 73.66 | |||||||||||
| Not present ° | 163 | 734 | 22.21 | |||||||||||
| Leader Vaccinated | ||||||||||||||
| No | 364 | 2256 | 16.13 | <0.001 | ||||||||||
| Yes | 569 | 1992 | 28.56 | |||||||||||
| Total | 340 | 3654 | 9.30 | 514 | 3664 | 14.03 | 933 | 4248 | 21.96 | 50.86 | 56.52 | |||
Legend: HCWs: healthcare workers; OSV: on-site vaccination; OHCWs: other HCWs (e.g., obstetricians, physiotherapists, etc.). * Ten data were missing during the 2016–2017 season. ° newly hired, return from parental leave or time off work. § Considering age as a continue variable the mean age ± SD among vaccinated vs. non-vaccinated during the different seasons was 49.4 ± 10.3 vs. 44.3 ± 10.3 (p < 0.001) in 2016–2017; 48.2 ± 10.5 vs. 44.7 ± 10.9 (p < 0.001) in 2017–2018; 46.3 ± 11.6 vs. 44.4 ± 10.9 (p < 0.001) in 2018–2019.
Table 3.
Logistic regression (one for each flu vaccination campaign). Vaccination (yes/no) during the relative influenza season is the dependent variable.
| Variables | 2016–2017 | 2017–2018 | 2018–2019 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| aOR | 95% CI | p | aOR | 95% CI | p | aOR | 95% CI | p | |
| Age class | |||||||||
| ≤34 | 1 | 1 | 1 | ||||||
| 35–44 | 1.19 | 0.77–1.85 | 0.44 | 1.00 | 0.71–1.39 | 0.99 | 1.00 | 0.80–1.25 | 0.99 |
| 45–54 | 1.69 | 1.10–2.58 | 0.02 | 1.41 | 1.02–1.94 | 0.04 | 0.96 | 0.77–1.21 | 0.74 |
| 55–64 | 2.41 | 1.55–3.73 | <0.001 | 1.93 | 1.38–2.70 | <0.001 | 1.58 | 1.25–1.99 | <0.001 |
| ≥65 | 4.20 | 1.94–9.10 | <0.001 | 3.07 | 1.59–5.94 | 0.001 | 0.86 | 0.55–1.36 | 0.53 |
| Gender | |||||||||
| F | 1 | 1 | 1 | ||||||
| M | 1.61 | 1.24–2.09 | <0.001 | 1.31 | 1.05–1.62 | 0.02 | 1.12 | 0.95–1.33 | 0.163 |
| Job Category | |||||||||
| Physicians | 1 | 1 | 1 | ||||||
| Nurses | 0.33 | 0.24–0.44 | <0.001 | 0.37 | 0.30–0.48 | <0.001 | 0.42 | 0.35–0.50 | <0.001 |
| OHCWs | 0.31 | 0.21–0.46 | <0.001 | 0.45 | 0.34–0.60 | <0.001 | 0.38 | 0.31–0.47 | <0.001 |
| OSV | |||||||||
| No | 1 | 1 | all hospital wards were involved in OSV | ||||||
| Yes | 2.30 | 1.80–2.92 | <0.001 | 2.64 | 2.15–3.25 | <0.001 | |||
3.1. The 2015–2016 Flu Vaccination Campaign
At the end of the 2015–2016 season, the vaccination coverage rate against influenza among HCWs was almost 6%. Moreover, more than 74% of the participants were satisfied about the FT experience and 70% of those who were interviewed considered this methodology a useful approach for other health issues [42].
3.2. The 2016–2017 Flu Vaccination Campaign
During the 2016–2017 campaign, the OSV intervention was performed in 12 of the 36 (33%) macro-areas, for a total of 1120 out of 3654 (30.7%) HCWs potentially involved in OSV (Table S1 in Supplementary Materials). The overall vaccination coverage rate among HCWs was 9.30%, significantly higher than that one reached in 2015–2016 (p < 0.0001). In 9 out of 12 (75%) macro-areas in which OSV was performed, the vaccination coverage among HCWs was higher than the overall coverage reached in all the hospital (Table S1). The overall flu vaccination coverage in HCWs working in wards involved in OSV intervention was 14.0% vs. 7.2% among HCWs not interested by OSV (p < 0.001). The mean age ± SD among vaccinated vs. non-vaccinated HCWs was 49.4 years ± 10.3 vs. 44.3 ± 10.3 (p < 0.001). The highest vaccination coverage rate was in the age class of 65 years old or more, the lowest in the youngest age class.
According to the multivariate analysis, age classes 45–54, 55–64 and more than 64 years old, male sex and working in wards reached by OSV were significantly associated with a higher influenza vaccination adherence. Moreover, being nurse or OHCWs was statistically related with lower influenza vaccination coverage in comparison with physicians.
3.3. The 2017–2018 Flu Vaccination Campaign
The flu vaccination campaign approached 3664 HCWs, including 1960 nurses, 1015 physicians and 689 OHCWs. The overall vaccination coverage during this campaign was 14.0% (n = 514). This result was significantly higher than the one achieved in 2016–2017 (p < 0.0001). The mean age ± SD among HCWs vaccinated was higher than non-vaccinated (p < 0.001). As in the previous season, the highest vaccination coverage rate was among HCWs of 65 years old or more, the lowest in the youngest age class even though this last was the age class with the highest increase from the previous season. The vaccine uptake was higher among men (20.1% vs. 10.8% in females; p < 0.001). Physicians were the most inclined professionals to undergo vaccination (25.2% of their category), while the OHCWs were the professionals with the highest increase (+105.9%), followed by nurses (+71.1%). The OSV sessions were extended to the wards nearby the ones involved during the previous year, potentially involving 1858 HCWs, more than half (50.7%) of the total HCWs (+65% compared to the previous season). Among the HCWs involved by the OSV intervention, vaccination coverage rate was 19.1% vs. 8.9% among HCWs not potentially involved (p < 0.001). Moreover, it seems that the vaccination status of the previous season had an impact on undergoing flu shot (Table 2).
According to the multivariate analysis, belonging to older-age classes (45–54 years old, 55–64 years old and more than 64 years old), being male and working in wards reached by the OSV were statistically significant in increasing influenza vaccination adherence. Instead, being nurses or OHCWs was statistically significant in lowering influenza vaccination coverage in comparison with physicians.
3.4. The 2018–2019 Flu Vaccination Campaign
During the last influenza season considered in the study (2018–2019), the overall vaccination coverage rate among HCWs was 22.0%, significantly higher than that one previously reached (p < 0.001). In the univariate analysis, vaccine uptake was significantly related to age class, with a decreasing trend (in the older age class, equal to −29.3%). Moreover, a statistically significant difference in vaccination coverage among professional categories was confirmed, with the highest increasing registered among nurses (+80.5%). Furthermore, statistical differences in flu vaccination coverage were reported when a comparison of the vaccination status during the two previous seasons (2016–2017 and 2017–2018) was done. Concerning the role played by the leaders, it seems that the HCWs with a vaccinated leader showed a higher vaccination coverage rate than the HCWs with a non-vaccinated leader (p < 0.001).
The results of a multivariate analysis showed that the 55–64 years old age class was statistically significant in influencing vaccination coverage during the 2018–2019 season in comparison with the youngest age class (aOR 1.58, 95% CI 1.25–1.99), such as being nurse (aOR 0.42, 95% CI 0.35–0.50) or OHCWs (aOR 0.38, 95% CI 0.31–0.47) in comparison with physician.
3.5. Overall Strategies Effectiveness
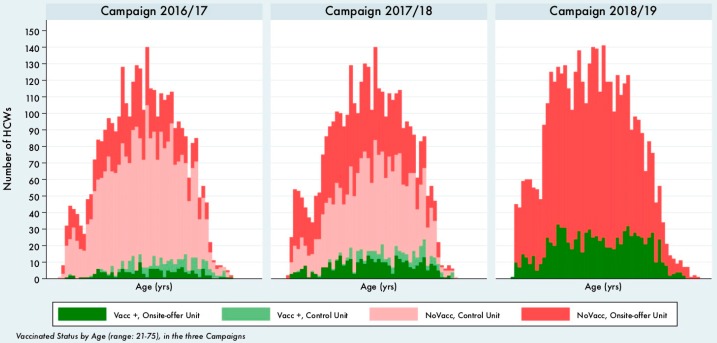
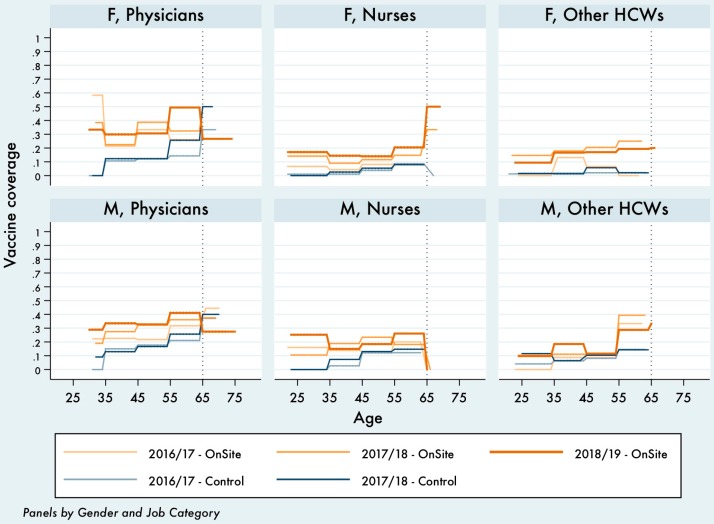
To evaluate the progression in the overall effectiveness of the following vaccination campaigns, we can compare the absolute number of vaccinated and non-vaccinated HCWs by year of age (Figure 1) or the vaccination coverage by 10-year age classes (Figure 2).
Figure 1.
Vaccination status by age, campaign 2016–2017, 2017–2018 and 2018–2019.
Figure 2.
Vaccination coverage by age class, gender, OSV and job category during the three campaigns (model without interaction, available in Table 3).
What clearly emerges from Figure 1 is that, not only the overall number of vaccinated HCWs increased (as already stated in the first sections of the results), but the increase was higher at younger ages.
This result is confirmed in Figure 2, in which the vaccination coverage by gender, job category and age class presented in Table 3 are shown. On-site vaccination strategy always leads to better results (orange lines), physicians always show higher vaccination coverage rates than nurses and OHCWs, but the progression among the three campaigns is particularly accentuated among professionals aged <45, which in on-site wards add an extra 5%–10% of vaccination coverage at each campaign.
Finally, Figures S1 and S2 (in Supplementary Materials) show the probability of being vaccinated, calculated using the same logistic model presented in Table 3 (S1) and using a different one (S2), which introduces a multiplicative interaction among HCW group, gender and age class (Table S2, in Supplementary Materials).
4. Discussion
Starting from the 2015–2016 season, an increasing overall flu vaccination coverage rate trend among HCWs was registered in the FPG teaching hospital, from 6% coverage in 2015–2016 to almost 22% at the end of the 2018–2019 season. One of the reasons of this increase was the implementation of the multicomponent strategy including the education of HCWs about vaccination, the active promotion of the vaccination campaign and the easy access to influenza vaccination free of charge, obtained mainly thanks to OSV intervention. Nevertheless, the overall vaccination coverage rate was lower than those reached in other international settings [22,27,29,51,52], thus remaining unsatisfactory and still far away by the minimum goal of 75% defined by the WHO and by the Italian PNPV (PNPV 2017–2019) [10,11]. However, the vaccination coverage registered in our teaching hospital represents an encouraging starting point and it is analogous, or even higher, than flu vaccination coverage rates registered in other national and regional settings [29,32,33,39,50,53,54,55]. Our results confirmed that physicians are the professionals most willing to get vaccinated, as reported in the literature [20,33,50,54], even though the overall increase was the lowest during the considered period if compared to nurses and OHCWs. The job category that registered the highest increase in coverage rate (compared to the previous years) were the OHCWs (+76.3%) and the nurses (+75.8%), proving that the implemented strategies were effective in reaching groups originally less inclined to vaccination, maybe due to the wrong perception of being at low risk of illness or transmitting the infection. A similar phenomenon was registered considering gender, as males had the highest vaccination coverage, but with a lower increase than women during the flu vaccination campaigns. Among the five-age class considered, the highest vaccination coverage was observed in the oldest two age classes in each of the last three campaigns, while the lowest in the youngest one. Nevertheless, the vaccination coverage has grown more in younger-age classes. Moreover, the performed multiple interactions analysis show probability estimated “high steps” for the age class of the over 65 (over 55 in Males other HCW professionals), rather independent from the on-site vaccination proposal, almost certainly due to the over 65 awareness of their status of higher-risk population. However, the performance of the OSV still works at any age and shows the possibility to reach a coverage around 40%–50% in many HCWs/gender groups in the age range 55–65, still confirming a rise in the coverage among physicians and nurses, even at younger ages, compared to the not-on-site wards in the first 2016–2017 campaign (Figure S2).
Vaccine hesitancy is a complex issue, especially amongst HCWs, and it requires ad hoc studies to understand the phenomenon in different contexts, in order to find ad hoc effective strategies to struggle it [24,26,40,41,56]. First of all, even and especially among healthcare personnel, it is necessary a have a cultural change about knowledge, attitudes and practices on vaccination through personalized training, such as academic detailing (educational outreach visit) and problem-based learning methodologies [43,44] or through the role of the occupational doctor who carries out annual health surveillance of workers [12]. As a matter of fact, this figure could play a key role by counseling HCWs with adequate information on the advantages and disadvantages of vaccination and non-vaccination, as defined by the Italian law [12]. Second, it could be useful to demonstrate and sustain the economic value of influenza vaccination among HCWs, by performing an economic analysis related to sickness absenteeism that occurs during seasonal flu periods, as already done by ourselves [45] and elsewhere [8,19,55,57]. Furthermore, mandatory vaccination among HCWs may be evaluated, as proposed by other authors [26,41,56], and already applied in other countries (e.g., USA) and to other vaccines, such as in Italy on the pediatric population [58].
Limitations
This study has several limitations. First of all, the exposure to the OSV intervention of HCWs pertaining to a specific macro-area is only “potential”: we assume that all of HCWs working in the ward involved in the OSV were present during the visit made by the trained medical residents that performed the OSV intervention, but there is no certain way to assess the presence of single HCWs at the time of every session. To limit this uncertainty, over the different flu vaccination campaigns, in many wards, more than one OSV intervention was carried out each year. Second, only the vaccinations administered inside the hospital were registered. Vaccination shots administered outside, by general practitioners or Local Health Authorities in primary care settings, were not collected/investigated. For this reason, the vaccination coverage rate registered among the HCWs in the FPG teaching hospital could be underestimated, overestimating, instead, the evaluation of the strategies implemented. This phenomenon, however, has less of an impact on the overall evaluation of the vaccination coverage rate than at the “starting point” of the program (2015–2016 season), thanks to the fundamental communication work done by the Health Management that every year spreads the news about the implemented strategies all over the hospital facilities, reducing the need to go outside the FPG to undergo flu vaccination.
5. Conclusions
Flu vaccination among HCWs is a fundamental measure to protect HCWs themselves, their patients and the hospital community. When low vaccination coverage is registered, new engaging approaches are necessary in order to sustain, encourage and promote the role of flu vaccination among HCWs. In our context, the OSV intervention and all the other strategies implemented resulted in being effective in achieving higher flu vaccination coverage and therefore can be considered a valuable example of good prevention practices in hospital settings. Moreover, though important, a single strategy has not proven to be sufficient to achieve the desired goal in vaccination coverage rates. For this reason, multiple approaches, including educational outreach visit, sickness absenteeism evaluation, cost-effective analysis, and mandatory vaccination and incentives or rewards to vaccinated HCWS, should be taken into consideration and assessed for implementation in different settings. Encouraging results in the younger age groups confirms the value of educational interventions.
Acknowledgments
The authors would like to thank all the collaborating group members for their support during the last seasonal influenza vaccination campaign: Andrea Poscia, Chiara de Waure, Concetta De Meo, Sara Manetta, Andrea Gentili, Gabriele Giubbini, Pasquale Serruto, Maurizio Zega, Anna Sguera, Claudia Mellucci, Gaspare Pascarella, Caterina Galletti, Maddalena Pozzi, Costanza Baratta, Bruno Piccoli, Daniele Piacentini, Sergio Riccardo Mastrodonato, Resident doctors in Publich Health and Occupational Medicine (Emanuela Bossi, Ilaria Capitanelli, Sabina Gini, Carolina Ianuale, Erika Lops, Paolo Parente, Anna Acampora, Alice Borghini, Elettra Carini, Angelo Maria Pezzullo, Adriano Grossi, Alice Corsaro, Andrea Di Pilla, Marco Mariani, Pasquale Cacciatore, Leuconoe Grazia Sisti, Veronica Ruggiero), and students of the master’s degree in nursing and midwifery sciences.
Supplementary Materials
The following are available online at https://www.mdpi.com/2076-393X/8/1/85/s1. Table S1: Vaccination coverage rates in the 36 clinical macro-areas randomized for the first on-site vaccination, during the influenza vaccination campaign 2016–2017. Figure S1: Probability of being vaccinated by age class, gender, OSV and job category during the three campaigns (model without interaction, available in Table 3 in main text). Figure S2: Probability of being vaccinated by age class, gender, OSV and job category during the three campaigns (model with multiple interaction, available in the Supplementary Materials). Table S2: Multivariate logistic regression model (nonlinear age + OSV + gender + job category with multiple interaction) by campaign.
Author Contributions
Conceptualization, A.B., D.I.L.M., and P.L.; methodology, A.B., D.I.L.M., and G.C.; acquisition of data, A.B., M.D.P., A.T. (Alessia Tognetto), A.T. (Andrea Tamburrano), D.V., C.V., S.C., and F.B.; formal analysis, A.B., D.I.L.M., and G.C.; interpretation of data: A.B., D.I.L.M., G.D., G.C., and P.L; writing—original draft preparation, A.B., M.D.P., A.T. (Alessia Tognetto), A.T. (Andrea Tamburrano), D.V., C.V., and S.C.; writing—review and editing, A.B., D.I.L.M., G.C., and P.L.; visualization: F.B., A.C., and G.D.; supervision: A.C., U.M., G.D., W.R., and P.L.; project administration, P.L. All authors have read and agreed to the submitted version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.Cassini A., Colzani E., Pini A., Mangen M.J.J., Plass D., McDonald S.A., Maringhini G., van Lier A., Haagsma J.A., Havelaar A.H., et al. Impact of infectious diseases on population health using incidence-based disability-adjusted life years (DALYs): Results from the burden of communicable diseases in Europe study, European Union and European economic countries, 2009 to 2013. Eurosurveillance. 2018;23:17–454. doi: 10.2807/1560-7917.ES.2018.23.16.17-00454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rosano A., Bella A., Gesualdo F., Acampora A., Pezzotti P., Marchetti S., Ricciardi W., Rizzo C. Investigating the impact of influenza on excess mortality in all ages in Italy during recent seasons (2013/14–2016/17 seasons) Int. J. Infect. Dis. 2019;88:127–134. doi: 10.1016/j.ijid.2019.08.003. [DOI] [PubMed] [Google Scholar]
- 3.Kwong J.C., Schwartz K.L., Campitelli M.A., Chung H., Crowcroft N.S., Karnauchow T., Katz K., Ko D.T., McGeer A.J., McNally D., et al. Acute myocardial infarction after laboratory-confirmed influenza infection. N. Engl. J. Med. 2018;378:345–353. doi: 10.1056/NEJMoa1702090. [DOI] [PubMed] [Google Scholar]
- 4.Molinari N.-A.M., Ortega-Sanchez I.R., Messonnier M.L., Thompson W.W., Wortley P.M., Weintraub E., Bridges C.B. The annual impact of seasonal influenza in the US: Measuring disease burden and costs. Vaccine. 2007;25:5086–5096. doi: 10.1016/j.vaccine.2007.03.046. [DOI] [PubMed] [Google Scholar]
- 5.Rittle C. Can Increasing Adult Vaccination Rates Reduce Lost Time and Increase Productivity? Workplace Health Saf. 2014;62:508–515. doi: 10.3928/21650799-20140909-02. [DOI] [PubMed] [Google Scholar]
- 6.Descalzo M.A., Clara W., Guzmn G., Mena R., Armero J., Lara B., Saenz C., Aragon A., Chacon R., El-Omeiri N., et al. Estimating the burden of influenza-associated hospitalizations and deaths in Central America. Influenza Other Respi. Viruses. 2016;10:340–345. doi: 10.1111/irv.12385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Osterholm M.T., Kelley N.S., Sommer A., Belongia E.A. Efficacy and effectiveness of influenza vaccines: A systematic review and meta-analysis. Lancet Infect. Dis. 2012;12:36–44. doi: 10.1016/S1473-3099(11)70295-X. [DOI] [PubMed] [Google Scholar]
- 8.Gianino M.M., Politano G., Scarmozzino A., Charrier L., Testa M., Giacomelli S., Benso A., Zotti C.M. Estimation of sickness absenteeism among Italian healthcare workers during seasonal influenza epidemics. PLoS ONE. 2017;12:e0182510. doi: 10.1371/journal.pone.0182510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Corson S., Robertson C., Reynolds A., McMenamin J. Modelling the population effectiveness of the national seasonal influenza vaccination programme in Scotland: The impact of targeting all individuals aged 65 years and over. Influenza Other Respi. Viruses. 2019;13:354–363. doi: 10.1111/irv.12583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO . Influenza (Seasonal) WHO; Geneva, Switzerland: 2018. [(accessed on 1 June 2019)]. Available online: https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal) [Google Scholar]
- 11.Ministero della Salute . Piano Nazionale Prevenzione Vaccinale (PNPV) 2017–2019. Ministero della Salute; Roma, Italy: 2017. [Google Scholar]
- 12.Italian Government . Legislative Decree No. 81/2008. Unique Text on Health and Safety at Work. Italian Government; Rome, Italy: 2008. [Google Scholar]
- 13.Potter J., Stott D.J., Roberts M.A., Elder A.G., Donnell B.O., Knight P.V., Carman W.F. Influenza Vaccination of Health Care Workers in Long-Term-Care Hospitals Reduces the Mortality of Elderly Patients. J. Infect. Dis. 1997;175:1–6. doi: 10.1093/infdis/175.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahmed F., Lindley M.C., Allred N., Weinbaum C.M., Grohskopf L. Effect of influenza vaccination of healthcare personnel on morbidity and mortality among patients: Systematic review and grading of evidence. Clin. Infect. Dis. 2014;58:50–57. doi: 10.1093/cid/cit580. [DOI] [PubMed] [Google Scholar]
- 15.Amodio E., Restivo V., Firenze A., Mammina C., Tramuto F., Vitale F. Can influenza vaccination coverage among healthcare workers influence the risk of nosocomial influenza-like illness in hospitalized patients? J. Hosp. Infect. 2014;86:182–187. doi: 10.1016/j.jhin.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 16.Weinstein R.A., Bridges C.B., Kuehnert M.J., Hall C.B. Transmission of Influenza: Implications for Control in Health Care Settings. Clin. Infect. Dis. 2003;37:1094–1101. doi: 10.1086/378292. [DOI] [PubMed] [Google Scholar]
- 17.Carman W.F., Elder A.G., Wallace L.A., McAulay K., Walker A., Murray G.D., Stott D.J. Effects of influenza vaccination of health-care workers on mortality of elderly people in long-term care: A randomised controlled trial. Lancet. 2000;355:93–97. doi: 10.1016/S0140-6736(99)05190-9. [DOI] [PubMed] [Google Scholar]
- 18.Music T. Protecting patients, protecting healthcare workers: A review of the role of influenza vaccination. Int. Nurs. Rev. 2012;59:161–167. doi: 10.1111/j.1466-7657.2011.00961.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amodio E., Anastasi G., Di Pasquale M., Gelsomino V., Morici M., Romano N., Torregrossa M.V., Cannova L., Calamusa G., Firenze A. Influenza vaccination among healthcare workers and absenteeism from work due to influenza-like illness in a teaching hospital in Palermo. Ital. J. Public Health. 2010;7 doi: 10.2427/5715. [DOI] [Google Scholar]
- 20.Costantino C., Casuccio A., Caracci F., Bono S., Calamusa G., Ventura G., Maida C.M., Vitale F., Restivo F. Impact of Communicative and Informative Strategies on Influenza Vaccination Adherence and Absenteeism from Work of Health Care Professionals Working at the University Hospital of Palermo, Italy: A Quasi-Experimental Field Trial on Twelve Influenza Seasons. Vaccines. 2019;8:5. doi: 10.3390/vaccines8010005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jorgensen P., Mereckiene J., Cotter S., Johansen K., Tsolova S., Brown C. How close are countries of the WHO European Region to achieving the goal of vaccinating 75% of key risk groups against influenza? Results from national surveys on seasonal influenza vaccination programmes, 2008/2009 to 2014/2015. Vaccine. 2018;36:442–452. doi: 10.1016/j.vaccine.2017.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.European Centre for Disease Prevention and Control (ECDC) Seasonal Influenza Vaccination and Antiviral Use in EU/EEA Member States—Overview of Vaccine Recommendations for 2017–2018 and Vaccination Coverage Rates for 2015–2016 and 2016–2017 Influenza Seasons. European Centre for Disease Prevention and Control (ECDC); Stockholm, Sweden: 2018. [DOI] [Google Scholar]
- 23.Karafillakis E., Dinca I., Apfel F., Cecconi S., Wűrz A., Takacs J., Suk J., Celentano L.P., Kramarz P., Larson H.J. Vaccine hesitancy among healthcare workers in Europe: A qualitative study. Vaccine. 2016;34:5013–5020. doi: 10.1016/j.vaccine.2016.08.029. [DOI] [PubMed] [Google Scholar]
- 24.Hollmeyer H., Hayden F., Mounts A., Buchholz U. Review: Interventions to increase influenza vaccination among healthcare workers in hospitals. Influenza Other Respi. Viruses. 2013;7:604–621. doi: 10.1111/irv.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hofmann F., Ferracin C., Marsh G., Dumas R. Influenza vaccination of healthcare workers: A literature review of attitudes and beliefs. Infection. 2006;34:142–147. doi: 10.1007/s15010-006-5109-5. [DOI] [PubMed] [Google Scholar]
- 26.Sullivan S.J., Jacobson R., Poland G.A. Mandating influenza vaccination for healthcare workers. Expert Rev. Vaccines. 2009;8:1469–1474. doi: 10.1586/erv.09.118. [DOI] [PubMed] [Google Scholar]
- 27.Black C.L., Yue X., Ball S.W., Donahue S.M.A., Izrael D., de Perio M.A., Laney S.A., Williams W.W., Lindley M.C., Graitcer S.B., et al. Influenza Vaccination Coverage Among Health Care Personnel—United States, 2014–2015 Influenza Season. Centert Dis. Control. Prev. Morb. Mortal. Wkly. Rep. 2015;64:993–999. doi: 10.15585/mmwr.mm6436a1. [DOI] [PubMed] [Google Scholar]
- 28.Genovese C., Picerno I.A.M., Trimarchi G., Cannavò G., Egitto G., Cosenza B., Merlina V., Icardi G., Panatto D., Amicizia D., et al. Vaccination coverage in healthcare workers: A multicenter cross-sectional study in Italy. J. Prev. Med. Hyg. 2019;60:E12–E17. doi: 10.15167/2421-4248/jpmh2019.60.1.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ministero della Salute . Quaderni del Ministero della Salute. Vaccinazioni: Stato Dell’Arte, Falsi Miti e Prospettive. Il Ruolo Chiave della Prevenzione. Ministero della Salute; Roma, Italy: 2017. [Google Scholar]
- 30.Blank P.R., Schwenkglenks M., Szucs T.D. Vaccination coverage rates in eleven European countries during two consecutive influenza seasons. J. Infect. 2009;58:446–458. doi: 10.1016/j.jinf.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 31.Esposito S., Bosis S., Pelucchi C., Tremolati E., Sabatini C., Semino M., Marchisio P., Della Croce F., Principi N. Influenza vaccination among healthcare workers in a multidisciplinary University hospital in Italy. BMC Public Health. 2008;8:422. doi: 10.1186/1471-2458-8-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.La Torre G., Mannocci A., Ursillo P., Bontempi C., Firenze A., Panico M.G., Sferrazza A., Ronga C., D’Anna A., Amodio E., et al. Prevalence of influenza vaccination among nurses and ancillary workers in Italy: Systematic review and meta analysis. Hum. Vaccines. 2011;7:728–733. doi: 10.4161/hv.7.7.15413. [DOI] [PubMed] [Google Scholar]
- 33.Mannocci A., Ursillo P., Bontempi C., Sferrazza A., La Torre G. Prevalence of influenza vaccination among physicians and related enhancing and preventing factors in Italy. Rev. Heal. Care. 2010;1:27–34. doi: 10.7175/rhc.v1i1.15. [DOI] [Google Scholar]
- 34.Health Management—Fondazione Policlinico Universitario A . Gemelli IRCCS. Confidential Communication, Fondazione Policlinico Universitario A. Gemelli IRCCS; Rome, Italy: 2015. [Google Scholar]
- 35.MacDonald N.E., Eskola J., Liang X., Chaudhuri M., Dube E., Gellin B., Goldstein S., Larson H., Manzo M.L., Reingold A., et al. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33:4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 36.Silvi G., Raineri C., Resi D., Casadio G.P., Bevilacqua L., Contarini V., Frassineti V. La vaccinazione antinfluenzale fra gli operatori dell’AUSL di Ravenna, anno 2010: Studio pilota. Not dell’Ist. Super. Sanità. 2013;26:iii–iv. [Google Scholar]
- 37.Böhmer M.M., Walter D., Falkenhorst G., Müters S., Krause G., Wichmann O. Barriers to pandemic influenza vaccination and uptake of seasonal influenza vaccine in the post-pandemic season in Germany. BMC Public Health. 2012;12:938. doi: 10.1186/1471-2458-12-938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Poland G.A. The 2009–2010 influenza pandemic: Effects on pandemic and seasonal vaccine uptake and lessons learned for seasonal vaccination campaigns. Vaccine. 2010;28:D3–D13. doi: 10.1016/j.vaccine.2010.08.024. [DOI] [PubMed] [Google Scholar]
- 39.Alicino C., Iudici R., Barberis I., Paganino C., Cacciani R., Zacconi M., Battistini A., Bellina D., Di Bella A.M., Talamini A., et al. Influenza vaccination among healthcare workers in Italy. The experience of a large tertiary acute-care teaching hospital. Hum. Vaccines Immunother. 2015;11:95–100. doi: 10.4161/hv.34362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dexter L.J., Teare M.D., Dexter M., Siriwardena A.N., Read R.C. Strategies to increase influenza vaccination rates: Outcomes of a nationwide cross-sectional survey of UK general practice. BMJ Open. 2012;2:e000851. doi: 10.1136/bmjopen-2011-000851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Simeonsson K., Summers-Bean C., Connolly A. Influenza vaccination of healthcare workers: Institutional strategies for improving rates. NC Med. J. 2004;65:323–329. [PubMed] [Google Scholar]
- 42.Corsaro A., Poscia A., de Waure C., De Meo C., Berloco F., Ricciardi W., Damiani G., Laurenti P., Collaborating Group Fostering Flu Vaccination in Healthcare Workers: Forum Theatre in a University Hospital. Med. Sci. Monit. 2017;23:4574–4578. doi: 10.12659/MSM.903009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.O’Brien M.A., Rogers S., Jamtvedt G., Oxman A.D., Odgaard-Jensen J., Kristoffersen D.T., Forsetlund L., Bainbridge D., Freemantle N., Davis D., et al. Educational outreach visits: Effects on professional practice and health care outcomes. Cochrane Database Syst. Rev. 2007 doi: 10.1002/14651858.CD000409.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tamburrano A., Mellucci C., Galletti C., Vitale D., Vallone D., Barbara A., Sguera A., Zega M., Damiani G., Laurenti P. Improving Nursing Staff Attitudes toward Vaccinations through Academic Detailing: The HProImmune Questionnaire as a Tool for Medical Management. Int. J. Environ. Res. Public Health. 2019;16:2006. doi: 10.3390/ijerph16112006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Colamesta V., Tamburrano A., Barbara A., Gentili A., La Milia D.I., Berloco F., Cicchetti A., Piacentini D., Galluzzi R., Mastrodonato S.R., et al. Cost-consequence analysis of influenza vaccination among the staff of a large teaching hospital in Rome, Italy: A pilot study. PLoS ONE. 2019;14:e0225326. doi: 10.1371/journal.pone.0225326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Séguin A., Rancourt C. The theatre: An effective tool for health promotion. World Health Forum. 1996;17:64–69. [PubMed] [Google Scholar]
- 47.Lee H.Y., Fong Y.T. On-site influenza vaccination arrangements improved influenza vaccination rate of employees of a tertiary hospital in Singapore. Am. J. Infect. Control. 2007;35:481–483. doi: 10.1016/j.ajic.2006.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.De Juanes J.R., García de Codes A., Arrazola M.P., Jaén F., Sanz M.I., González A. Influenza vaccination coverage among hospital personnel over three consecutive vaccination campaigns (2001–2002 to 2003–2004) Vaccine. 2007;25:201–204. doi: 10.1016/j.vaccine.2005.10.057. [DOI] [PubMed] [Google Scholar]
- 49.Bert F., Thomas R., Lo Moro G., Scarmozzino A., Silvestre C., Zotti C.M., Siliquini R. A new strategy to promote flu vaccination among health care workers: Molinette Hospital’s experience. J. Eval. Clin. Pract. 2019 doi: 10.1111/jep.13295. [DOI] [PubMed] [Google Scholar]
- 50.Vimercati L., Bianchi F.P., Mansi F., Ranieri B., Stefanizzi P., De Nitto S., Tafuri S. Influenza vaccination in health-care workers: An evaluation of an on-site vaccination strategy to increase vaccination uptake in HCWs of a South Italy Hospital. Hum. Vaccines Immunother. 2019;15:2927–2932. doi: 10.1080/21645515.2019.1625645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Oguz M.M. Improving influenza vaccination uptake among healthcare workers by on-site influenza vaccination campaign in a tertiary children hospital. Hum. Vaccines Immunother. 2019;15:1060–1065. doi: 10.1080/21645515.2019.1575164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mereckiene J., Cotter S., Nicoll A., Lopalco P., Noori T., Weber J.T., D’Ancona F., Lévy-Bruhl D., Dematte L., Giambi C., et al. Seasonal influenza immunisation in Europe. Overview of recommendations and vaccination coverage for three seasons: Pre-pandemic (2008/09), pandemic (2009/10) and post-pandemic (2010/11) Eurosurveillance. 2014;19:20780. doi: 10.2807/1560-7917.ES2014.19.16.20780. [DOI] [PubMed] [Google Scholar]
- 53.Tognetto A., Zorzoli E., Franco E., Gervasi G., Paglione L., Di Ninno F., De Soccio P., Barbara A., Orsi G.B., De Vito C., et al. Seasonal influenza vaccination among health-care workers: The impact of different tailored programs in four University hospitals in Rome. Hum. Vaccines Immunother. 2019:1–5. doi: 10.1080/21645515.2019.1632684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gilardi F., Gattinara G.C., Vinci M.R., Atti M.C.D., Santilli V., Brugaletta R., Santoro A., Montanaro R., Lavorato L., Raponi M., et al. Seasonal influenza vaccination in health care workers. A pre-post intervention study in an Italian paediatric hospital. Int. J. Environ. Res. Public Health. 2018;15:841. doi: 10.3390/ijerph15050841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zaffina S., Gilardi F., Rizzo C., Sannino S., Brugaletta R., Santoro A., Castelli Gattinara G., Ciofi degli Atti M.L., Raponi M., Vinci M.R. Seasonal influenza vaccination and absenteeism in health-care workers in two subsequent influenza seasons (2016/17 and 2017/18) in an Italian pediatric hospital. Expert Rev. Vaccines. 2019;18:411–418. doi: 10.1080/14760584.2019.1586541. [DOI] [PubMed] [Google Scholar]
- 56.Wicker S., Marckmann G. Vaccination of health care workers against influenza: Is it time to think about a mandatory policy in Europe? Vaccine. 2014;32:4844–4848. doi: 10.1016/j.vaccine.2013.09.062. [DOI] [PubMed] [Google Scholar]
- 57.Cella M.T., Corona G., Tuccillo E., Franco G. Valutazione di efficacia e impatto economico di una campagna di vaccinazione antinfluenzale in personale di una struttura sanitaria. Med. Lav. 2005;96:1–7. [PubMed] [Google Scholar]
- 58.Gazzetta Ufficiale della Repubblica Italiana . DECRETO-LEGGE 7 Giugno 2017, n. 73 Disposizioni Urgenti in Materia di Prevenzione Vaccinale. (17G00095) (GU Serie Generale n.130 del 07-06-2017) Gazzetta Ufficiale della Repubblica Italiana; Rome, Italy: 2017. [(accessed on 28 December 2019)]. Available online: https://www.gazzettaufficiale.it/eli/id/2017/06/07/17G00095/sg. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.