Abstract
Background
At present, serum Aspergillus IgG and IgM antibody detection is mainly used in the diagnosis of chronic pulmonary aspergillosis (CPA), but its value in the diagnosis of invasive pulmonary aspergillosis (IPA) in non-agranulocytic patients is still unclear. IgM can be used as a marker of acute infection to help diagnose acute infection-related diseases. IgG is a marker of long-term infection and is used to assist in the diagnosis of pre-existing or chronic infection-related diseases. The aim of this study was to investigate and compare the value of serum Aspergillus IgG and IgM antibody detection in the diagnosis of IPA and CPA in non-agranulocytic patients.
Methods
Fifty-eight cases of pulmonary aspergillosis (37 IPA and 21 CPA cases), 15 cases of community-acquired bacterial pneumonia and 50 cases in the healthy control group were collected. The serum (1,3)-β-D-glucan test (G test) was performed with a chromogenic method, and the galactomannan test (GM test) and Aspergillus IgG and IgM antibody detection were performed by commercial enzyme-linked immunosorbent assay (ELISA) in all patients. The sensitivity and specificity, cut-off value and area under the curve (AUC) of Aspergillus IgG and IgM antibodies were further obtained by receiver operating characteristic (ROC) curves.
Results
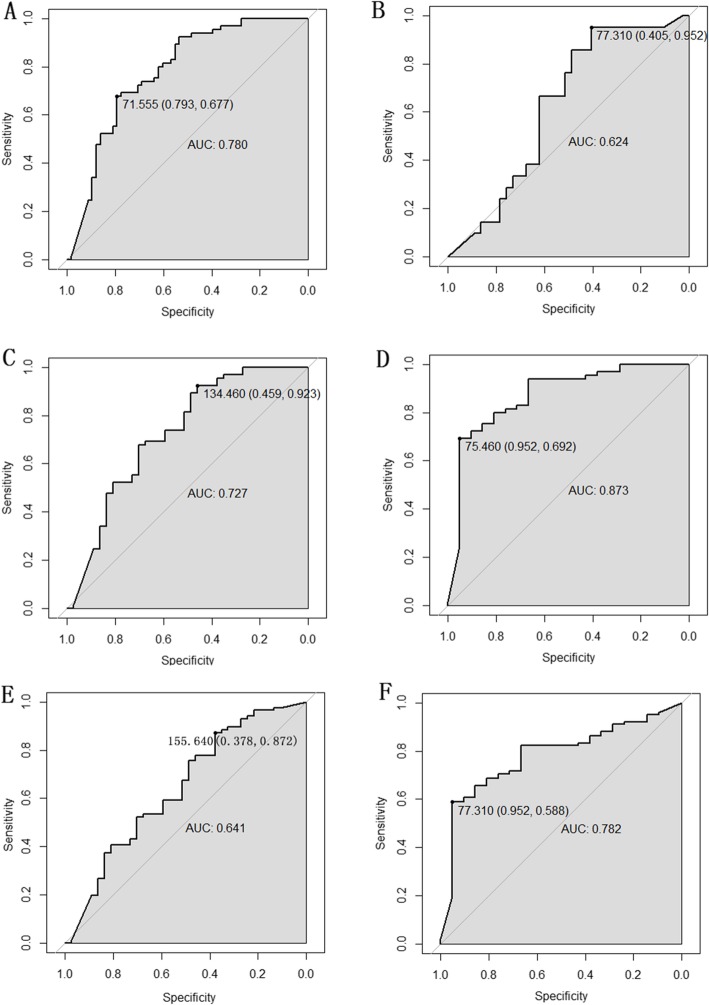
The positive rate of the G test, Aspergillus IgG antibody detection and the GM test also showed notable differences among the IPA, CPA, community-acquired bacterial pneumonia and healthy groups (P = 0.006, P < 0.001 and P = 0.217, respectively). Only the positive rate of the GM test showed a significant difference between the IPA and CPA groups (P = 0.04). ROC curves indicated that Aspergillus IgG antibody detection had a higher specificity in the IPA group than in the CPA group (0.952). The detection of Aspergillus IgG antibody can preferably distinguish IPA from community-acquired bacterial pneumonia and healthy controls (sensitivity = 0.923, specificity = 0.459, cut-off value = 134.46, AUC = 0.727). It can also distinguish CPA from community-acquired bacterial pneumonia and healthy controls (sensitivity = 0.952, specificity = 0.692, cut-off value = 75.46, AUC = 0.873).
Conclusions
Serum Aspergillus IgG antibody detection may have certain clinical value in the diagnosis of IPA and CPA in non-agranulocytic patients.
Keywords: Pulmonary aspergillosis, Non-agranulocytic patients, Serum Aspergillus IgG, Diagnosis
Background
Pulmonary aspergillosis is a type of lung disease caused by Aspergillus infection or the inhalation of Aspergillus antigen. Pulmonary aspergillosis is uncommon in non-agranulocytic patients, and only a small amount of data are available. Nevertheless, in recent years, the incidence of pulmonary aspergillosis in non-granulocytic patients has increased with ageing; the increase in chronic diseases; the use of broad-spectrum antibiotics, hormones, and immunosuppressive drugs; and invasive operations [1, 2]. Moreover, the clinical manifestations of these patients lack specificity, and the diagnosis is usually difficult, which leads to treatment delay and affects the prognosis. According to the clinical characteristics, pulmonary aspergillosis can be divided into allergic bronchopulmonary aspergillosis (ABPA), chronic pulmonary aspergillosis (CPA), invasive pulmonary aspergillosis (IPA), and subacute invasive aspergillosis (SAIA) [3]. Among them, CPA usually occurs in immunocompetent individuals with underlying respiratory disorders, and the prevalence of CPA worldwide is approximately 3 million [4]. Unfortunately, respiratory physicians may not detect CPA until the disease progresses to an advanced stage owing to the lack of specific clinical manifestations. More seriously, without timely diagnosis and long-term antifungal treatment, the 5-year mortality rate of patients with CPA reaches 80% [5]. Furthermore, invasive pulmonary aspergillosis (IPA) has become a common type of severe pneumonia with the highest mortality, and one of the important reasons the is difficulty in diagnosis [6]. In addition, patients with agranulocytosis are predominant among those with IPA, and relevant international guidelines for diagnosis and treatment also focus on them [7].
The diagnosis of pulmonary aspergillosis depends on histopathology and microbiological culture, but there are risks in obtaining tissue specimens. Traditional microbiological culture has a low positive rate, takes a long time, and has the possibility of contamination and colonization. However, serological diagnosis as a non-invasive diagnostic method is conducive to the early diagnosis of pulmonary aspergillosis but avoids over-diagnosis. However, this method has a false-positive reaction during the detection process, which reduces the sensitivity. The method has the advantages of high efficiency and time savings, high specificity, and high sensitivity and is suitable for the detection of a large number of samples. IgM antibody has a short half-life and disappears quickly; therefore, it can be detected in blood as an indicator of recent infection. IgG antibodies are characterized by late production, long maintenance time, slow disappearance and high concentration. Therefore, its detection in blood can be used as an indicator of long-term infection. Among the serological diagnoses, it is well known that serum Aspergillus IgG and IgM antibody detection is mainly used in the clinical diagnosis of CPA [8]. Related research demonstrated that Aspergillus fumigatus (A. fumigatus)-specific IgG was elevated in 98.4% (239/243) of CPA subjects [9]. In addition, at a cut-off value of 27 mgA/L, A. fumigatus-specific IgG is a reliable test for the diagnosis of CPA (area under the receiver operating characteristic curve (AUROC): 0.976, sensitivity: 95.6%, specificity: 100%) [10]. Synchronously, the serum G test and GM tests are mainly used for the diagnosis of IPA in agranulocytic patients. The G test detects (1,3)-β-D-glucan, and (1,3)-β-D-glucan is a polysaccharide component of the cell wall of yeast and filamentous fungi that is most useful as a fungal antigen. The GM test was used to detect galactomannan antigen, a component of the Aspergillus cell wall. However, these two tests have low positive rate and poor sensitivity in non-agranulocytic patients. In this study, we explored the value of the G test, GM test, and serum Aspergillus IgG and IgM antibody detection for the diagnosis of IPA and CPA in non-agranulocytic patients.
Methods
Patients and data collection
Fifty-eight pulmonary aspergillosis cases in non-agranulocytic patients admitted to Tianjin Chest Hospital from July 2017 to July 2018 were enrolled. The diagnostic criteria referred to the consensus of experts in the diagnosis and treatment of pulmonary mycosis and the criteria of the European Organization for Research and Treatment of Cancer (EORTC) [11, 12]. The exclusion criteria were as follows: (1) agranulocytic patients, (2) patients with other lung diseases, (3) patients with possible pulmonary aspergillosis, (4) patients with allergic bronchopulmonary aspergillosis, and (5) patients who were positive for human immunodeficiency virus (HIV).
The proven IPA patients required pathological histological evidence or a positive Aspergillus culture in a sterile site. The diagnostic criteria of probable IPA included the following: (1) patients had risk factors for pulmonary aspergillosis (such as neutropenia, transplantation, and immunosuppressive therapy), (2) patients had certain clinical manifestations of IPA, (3) imaging results were abnormal, and (4) there was microbiological evidence of IPA.
The diagnostic criteria of CPA were as follows: (1) chronic lung symptoms (cough, expectoration, haemoptysis, weight loss) for more than 3 months, (2) progressive imaging abnormalities (new or progressive cavities, infiltration around the cavity, thickening of the pleura, fungal balls), (3) microbiological evidence of CPA (the culture of sputum, bronchoalveolar lavage fluid and bronchoscopy was positive and the blood G test and GM test were positive), and (4) no or a low degree of immune impairment.
During the same period, 15 cases of community-acquired bacterial pneumonia and 50 healthy individuals served as control groups. The sex and age of the control groups were not significantly different from those of the pulmonary aspergillosis group. The following data were collected: demographic data (age, sex, weight), serum indexes, imaging features, biochemical indicators, bacterial and fungal culture results, bronchoscopic findings, and treatment outcomes. In addition, all participants signed informed consent voluntarily, and the study was approved by the ethics committee of Tianjin Chest Hospital (protocol number: 2018KY-009-01).
Serological testing
Five millilitres of venous blood was extracted before the administration of any antibiotics. Serum was separated from the blood for immediate testing or was stored frozen at − 80 °C for later testing.
G test
The serum (1,3)-β-D-glucan test (G test) was conducted with a chromogenic method using a (1–3)-β-D-glucan detection kit (Dynamiker Biotechnology Co., Ltd., Tianjin, China). In brief, a 5 μl serum sample was first pretreated for 10 min at 37 °C with 20 μl of a solution containing 0.6 M KCl and 0.125 M KOH and then assayed with Glucatell reagent in a kinetic, chromogenic format for 30 min at 37 °C. Subsequently, the optical densities at 405 nm (OD405) were read. Finally, the concentration of G in each sample was calculated by using a calibration curve with standard solutions of 6.25 to 100 pg/ml. Cases were judged positive if the level of G was ≥120 pg/ml in at least one serum sample [13].
GM test
The serum galactomannan test (GM test) was carried out with a commercial enzyme-linked immunosorbent assay (ELISA) kit (Dynamiker Biotechnology Co., Ltd. Tianjin, China) according to the manufacturer’s instructions. The judgement criteria for the GM test results were as follows: ≥ 0.85 μg/L was considered positive, < 0.65 μg/L was considered negative, and 0.65–0.85 μg/L was considered intermediate [14].
Aspergillus IgG
The commercial ELISA kit (Dynamiker Biotechnology Co., Ltd. Tianjin, China) was used to detect Aspergillus IgG antibody, and the experimental procedure followed the instructions. An Aspergillus IgG concentration ≥ 120 AU/ml was considered positive, < 80 AU/ml was considered negative, and 80–120 AU/ml was considered intermediate [15].
Aspergillus IgM
According to the manufacturer’s instructions, Aspergillus IgM antibody was detected by a commercial enzyme-linked immunosorbent assay (ELISA) kit (Dynamiker Biotechnology Co., Ltd. Tianjin, China). The judgement criteria for Aspergillus IgM detection included the following: ≥ 120 AU/ml was considered positive, < 80 AU/ml was considered negative, and 80–120 AU/ml was considered the intermediate [15].
Statistical analysis
SPSS 21.0 software was used for statistical analysis. Comparisons between groups were performed by the chi-squared test. Fisher’s test results were used when the sample size was small and the theoretical number was small. The Mann-Whitney U test was used in the course of disease, age and serum indicators except lymphocyte count indicators. An independent-sample t test was used for lymphocyte count indicators. The sensitivity, specificity and optimal threshold were determined by receiver operating characteristic (ROC) curve analysis in the pROC package. The best cut-off value was the value that maximized the sum of the sensitivity and specificity in the ROC curve. This study defined a P value < 0.05 as a significant difference.
Results
Patient characteristics
The characteristics of the 58 pulmonary aspergillosis patients are shown in Table 1. There were 36 males and 22 females, aged from 46 to 75 years (60.7 ± 14.6), and 37 IPA (63.8%) and 21 CPA cases (36.2%) were included. The IPA cases included 3 proven patients and 34 probable patients, with no possible patients. The CPA cases included 3 simple aspergilloma (SA), 10 chronic cavitary pulmonary aspergillosis (CCPA) and 8 subacute invasive aspergillosis (SAIA) cases [16]. Among these pulmonary aspergillosis patients, 7 patients (12.1%) has no other underlying diseases, 26 patients (44.8%) had chronic respiratory disease, and 15 patients (25.9%) had diabetes (Table 1).
Table 1.
Characteristics of 58 pulmonary aspergillosis cases in non-agranulocytic patients
| characteristics | No. of patients (n = 58) | % |
|---|---|---|
| Gender | ||
| Male | 36 | 62.07 |
| Female | 22 | 37.93 |
| Age | ||
| ≥ 60 | 32 | 55.17 |
| < 60 | 26 | 44.83 |
| Case classification | ||
| IPA | 37 | 63.79 |
| CPA | 21 | 36.21 |
| Underlying disease | ||
| chronic respicatory disease | 26 | 44.83 |
| Organ failure | 1 | 1.72 |
| Chronic cardiovascular disease | 5 | 8.62 |
| pulmonary tuberculosis | 4 | 6.90 |
| chronic liver disease | 1 | 1.72 |
| Diabetes | 15 | 25.86 |
| Autoimmune disease | 1 | 1.72 |
| Others | 8 | 13.79 |
| No underlying disease | 7 | 12.07 |
IPA invasive pulmonary aspergillosis, CPA, chronic pulmonary aspergillosis
Characteristics comparison between IPA and CPA cases
Clinical features between IPA and CPA cases were compared and are exhibited in Table 2, including microbiological findings, clinical symptoms, thoracic CT signs, the involved lobes of the lung, and serum indexes. It was obvious from Table 2 that the course of CPA cases was longer than that of IPA cases. Some clinical symptoms, such as fever, dyspnoea and haemoptysis, were very different between IPA and CPA cases (P < 0.05). Observable differences were found between the above two groups in terms of thoracic CT signs of patchy exudate shadows; air crescent sign and ground-glass opacity attenuation; the involvement of the right middle, right lower and left upper lobes of the lung; and serum indexes of LDH, albumin, PCT levels and lymphocyte count (P < 0.05, Table 2).
Table 2.
Comparison of clinical features between IPA and CPA cases
| Characteristics | IPA (n = 37) | CPA (n = 21) | Overall (n = 58) | P |
|---|---|---|---|---|
| Ratio of male to female patients | 23:14 | 13:8 | 36:22 | 0.985 |
| Age, median years | 64 (54.513, 72) | 60 (46.524, 66) | 64 (53.753, 70.248) | 0.128 |
| Course of disease (median, day) | 17 (10, 30) | 75 (23.251, 187.532) | 20 (13, 60) | < 0.001 |
| Microbiological findings | ||||
| Staphylococcus aureus | 1 (2.703) | 0 | 1 (1.724) | 1.000 |
| Pseudomonas aeruginosa | 1 (2.703) | 1 (4.762) | 2 (3.448) | 1.000 |
| Candida albicans | 1 (2.703) | 1 (4.762) | 2 (3.448) | 1.000 |
| Acinstobacter baumannii | 1 (2.703) | 1 (4.762) | 2 (3.448) | 1.000 |
| Klebsiella pneumoniae | 2 (5.405) | 0 | 2 (3.448) | 0.530 |
| Aspergillus | 8 (21.622) | 3 (14.286) | 11 (18.966) | 0.301 |
| Others | 2 (5.405) | 1 (4.762) | 3 (5.172) | 1.000 |
| Clinical symptoms, n(%) | ||||
| Cough | 34 (91.892) | 18 (85.714) | 52 (89.655) | 0.657 |
| Fever (> 38 °C) | 22 (59.459) | 3 (14.286) | 25 (43.103) | 0.001 |
| Dyspnoea | 25 (67.568) | 8 (38.095) | 33 (56.897) | 0.029 |
| Haemoptysis | 13 (35.135) | 13 (61.905) | 26 (44.828) | 0.049 |
| Chest Pain | 8 (21.622) | 2 (9.524) | 10 (17.241) | 0.301 |
| Expectoration | 33 (89.189) | 17 (80.952) | 50 (86.207) | 0.443 |
| Thoracic CT signs, n(%) | ||||
| Patchy exudate shadows | 36 (97.297) | 11 (52.381) | 47 (81.034) | < 0.001 |
| Nodules | 19 (51.351) | 9 (42.857) | 28 (48.276) | 0.534 |
| segmental areas of consolidation | 4 (10.811) | 7 (33.333) | 11(18.966) | 0.077 |
| Cavity | 17 (45.946) | 14 (66.667) | 31 (53.448) | 0.128 |
| Pleural effusion | 11 (29.730) | 2 (9.524) | 13 (22.414) | 0.106 |
| Air crescent sign | 2 (5.405) | 9 (42.857) | 11 (18.966) | 0.001 |
| ground-glass attenuation | 22 (59.459) | 5 (23.810) | 27 (46.552) | 0.009 |
| other | 1 (2.703) | 13 (61.905) | 14 (24.138) | < 0.001 |
| Involving lobes of lung, n(%) | ||||
| Right upper lobe | 28 (75.676) | 13 (61.905) | 41 (70.689) | 0.268 |
| Right middle lobe | 24 (64.865) | 3 (14.286) | 27 (46.552) | < 0.001 |
| Right lower lobe | 30 (81.081) | 9 (42.857) | 39 (67.241) | 0.003 |
| Left upper lobe | 28 (75.676) | 7 (33.333) | 35 (60.345) | 0.002 |
| Left lower lobe | 27 (72.973) | 12 (57.143) | 39 (67.241) | 0.217 |
| Serum indexs | ||||
| Erythrocyte sedimentation rate (mm/h) | 46 (26.515, 62) | 30 (19.525, 55) | 42 (25.514, 60.543) | 0.369 |
| White blood cell count (109cells/L) | 8.77 (5.534, 13.495) | 6.97 (5.862, 8.471) | 7.96 (5.788, 12.163) | 0.212 |
| Neutrophil count (109cells/L) | 7.3 (3.555, 11.205) | 4.31 (3.475, 6.685) | 5.31 (3.495, 9.945) | 0.083 |
| Eosinophilia count (109cells/L) | 0.07 (0.005, 0.135) | 0.1 (0.035, 0.223) | 0.085 (0.012, 0.153) | 0.104 |
| Monocyte count (109cells/L) | 0.45 (0.325, 0.57) | 0.57 (0.385, 0.695) | 0.49 (0.348, 0.603) | 0.113 |
| Platelet ((109cells/L)) | 273 (199.5385.5) | 257 (209,294.5) | 263.5 (208.75, 336.25) | 0.257 |
| Serum ALT level (U/L) | 21.8 (15.65, 41.55) | 20.2 (13.9, 30.4) | 21.65 (15.425, 34.775) | 0.32 |
| Serum creatinine level (μmol/L) | 67 (53.75, 78.75) | 67 (60, 77.5) | 67 (59, 78) | 0.715 |
| Serum albumin level (g/L) | 36.2 (28.725, 41) | 42.8 (39.5, 44.95) | 40.4 (35.6, 43.9) | <0.001 |
| Serum LDH level (U/L) | 262 (203, 373.5) | 225 (187.5, 236.5) | 233.5 (198, 326.75) | 0.025 |
| Serum CRP level (mg/L) | 4.09 (1.135, 11) | 1.7 (0.485, 7.335) | 2.85 (0.538, 8.615) | 0.174 |
| PCT (ng/ml) | 0.09 (0.050, 0.215) | 0.05 (0.05, 0.063) | 0.05 (0.05, 0.15) | 0.007 |
| Lymphocyte count (109cells/L) | 1.455 ± 0.63 | 1.890 ± 0.577 | 1.685 ± 0.639 | < 0.001 |
IPA invasive pulmonary aspergillosis, CPA chronic pulmonary aspergillosis, LDH lactate dehydrogenase, CRP C-reactive protein, PCT procalcitonin
Results of serum G test, GM test, and Aspergillus IgG and IgM antibody detection in each group
The results of the serum G test, Aspergillus IgG and Aspergillus IgM antibody detection and the GM test are listed in Tables 3, 4 and 5 for the different groups. Primitively, positive rates of the above serum indexes were found among the pulmonary aspergillosis, community-acquired bacterial pneumonia and healthy groups, and Table 3 shows the statistical results. The positive rates of the serum G test and Aspergillus IgG antibody detection in the pulmonary aspergillosis group were notably higher than those in the community-acquired bacterial pneumonia and healthy groups (P = 0.015 and < 0.0001, respectively) and were similar between the community-acquired bacterial pneumonia group and the healthy group. Afterwards, to study whether different types of pulmonary aspergillosis could be distinguished, the pulmonary aspergillosis group was divided into IPA and CPA groups according to the disease type. Table 4 shows the comparison results among the IPA, CPA, community-acquired bacterial pneumonia and healthy groups, and Table 5 shows the comparison between the IPA and the CPA groups. In addition to the G test and Aspergillus IgG antibody detection, the positive rate of the GM test also showed notable differences among the IPA, CPA, community-acquired bacterial pneumonia and healthy groups (P = 0.022) (Table 4). Nevertheless, the G test and Aspergillus IgG antibody detection results were not significantly different between the IPA and CPA groups (P ≥ 0.5), and the positive rate of the GM test was significantly different (P = 0.04) (Table 5).
Table 3.
Comparisons of serum G test, Aspergillus IgG antibody, Aspergillus IgM antibody and GM test among pulmonary aspergillosis, bacterial pneumonia and healthy groups
| Group | G test positive n (%) | Aspergillus IgG antibody positive n (%) | Aspergillus IgM antibody positive n (%) | GM test positive n (%) |
|---|---|---|---|---|
| pulmonary aspergillosis group | 14 (24.138) | 33 (56.897) | 14 (24.138) | 12 (20.690) |
| bacterial pneumonia group | 1 (6.667) | 3 (20.00) | 4 (26.667) | 2 (13.333) |
| healthy group | 3 (6.000) | 8 (16.000) | 9 (18.000) | 4 (8.000) |
| P | 0.015 | < 0.001 | 0.649 | 0.198 |
G test (1,3) beta glucan-D test, GM test galactomaunan test
Table 4.
Comparisons of serum G test, Aspergillus IgG antibody, Aspergillus IgM antibody and GM test among IPA, CPA, bacterial pneumonia and healthy groups
| Group | G test positive n (%) | Aspergillus IgG antibody positive n (%) | Aspergillus IgM antibody positive n (%) | GM test positive n (%) |
|---|---|---|---|---|
| IPA group | 12 (32.430) | 18 (48.650) | 6 (16.220) | 11 (29.730) |
| CPA group | 2 (9.523) | 15 (71.429) | 8 (38.095) | 1 (4.762) |
| bacterial pneumonia group | 1 (6.667) | 3 (20.000) | 4 (26.667) | 2 (13.333) |
| healthy group | 3 (6.000) | 8 (16.000) | 9 (18.000) | 4 (8.000) |
| P | 0.006 | < 0.001 | 0.217 | 0.022 |
G test (1,3) beta glucan-D test, GM test galactomaunan test, IPA invasive pulmonary aspergillosis, CPA chronic pulmonary aspergillosis
Table 5.
Comparisons of serum G test, Aspergillus IgG antibody, Aspergillus IgM antibody and GM test between IPA and CPA groups
| Group | G test positive n (%) | Aspergillus IgG antibody positive n (%) | Aspergillus IgM antibody positive n (%) | GM test positive n (%) |
|---|---|---|---|---|
| IPA group | 12 (32.432) | 18 (48.649) | 6 (16.216) | 11 (29.730) |
| CPA group | 2 (9.523) | 15 (71.429) | 8 (38.095) | 1 (4.762) |
| P | 0.050 | 0.092 | 0.061 | 0.040 |
G test (1,3) beta glucan-D test, GM test galactomaunan test, IPA invasive pulmonary aspergillosis, CPA, chronic pulmonary aspergillosis
ROC curves of serum Aspergillus IgG antibody in different groups
The ROC curves of Aspergillus IgG antibody in different groups were drawn. Figure 1 a-f and Supplementary Table 1 display ROC curves of Aspergillus IgG antibody with remarkable significance (P < 0.05), and the cut-off value (sensitivity, specificity) and the area under the curve (AUC) are also shown. Aspergillus IgG antibody detection had a higher specificity (0.952) in the IPA group than in the CPA group (Fig. 1b), with the highest sensitivity (0.952) in the CPA group compared with the IPA, community-acquired bacterial pneumonia and healthy groups (Fig. 1f), and with both the highest AUC (0.873) and the highest sensitivity (0.952) in the CPA group compared with the community-acquired bacterial pneumonia and healthy groups (Fig. 1d). Furthermore, the AUC value was larger in Fig. 1D than in Fig. 1c and was larger in Fig. 1f than that in Fig. 1e. That is, serum Aspergillus IgG antibody detection had a better performance for distinguishing CPA than for distinguishing IPA.
Fig. 1.
ROC curves of Aspergillus IgG antibody in different groups. a: The ROC curve of Aspergillus IgG antibody in the pulmonary aspergillosis group compared with the healthy group; the cut-off value (sensitivity, specificity) = 71.555 (0.793, 0.677) and AUC = 0.780, P < 0.001. b: The ROC curve of Aspergillus IgG antibody in the IPA group compared with the CPA group; the cut-off value (sensitivity, specificity) = 77.310 (0.405, 0.952) and AUC = 0.624, P < 0.001. c: The ROC curve of Aspergillus IgG antibody in the IPA group compared with the community-acquired bacterial pneumonia and healthy groups; the cut-off value (sensitivity, specificity) = 134.460 (0.459, 0.923) and AUC = 0.727, P < 0.001. d: The ROC curve of Aspergillus IgG antibody in the CPA group compared with the community-acquired bacterial pneumonia and healthy groups; the cut-off value (sensitivity, specificity) = 75.460 (0.952, 0.692) and AUC = 0.873, P < 0.001. e: The ROC curve of Aspergillus IgG antibody in the IPA group compared with the CPA, community-acquired bacterial pneumonia and healthy groups; the cut-off value (sensitivity, specificity) = 155.640 (0.378, 0.872) and AUC = 0.641, P = 0.013. f: The ROC curve of Aspergillus IgG antibody in the CPA group compared with the IPA, community-acquired bacterial pneumonia and healthy groups; the cut-off value (sensitivity, specificity) = 77.310 (0.952, 0.588) and AUC = 0.782, P < 0.001
Discussion
Although pulmonary aspergillosis in non-agranulocytic patients has increased with the development of society, the frequency remains low relative to that in agranulocytic patients. To date, few data are available in non-agranulocytic patients, and most of them are found in case reports [2, 17–19]. Consequently, more cases and more studies are urgently needed to understand non-agranulocytic pulmonary aspergillosis to provide more references or clues for the diagnosis and treatment of the disease. In this article, 58 cases were reported, and the sample size was rare and large. IPA is a life-threatening infection, mainly found in patients with prolonged neutropenia. One clinical challenge of non-agranulocytic IPA cases is the frequent lack of specific clinical features, especially in patients without underlying disease [20]. In our study, we comprehensively compared clinical features between IPA and CPA cases with relevant diagnostic methods commonly used in the clinic (Table 2), including microbial cultivation, thoracic CT and serum detection. Compared with CPA, some special characteristics for IPA were spotted, such as a shorter disease course, frequent patchy exudate shadows, a specific lung lobe involvement, and lower serum albumin level, which might be used for differential diagnosis or auxiliary diagnosis.
The diagnostic gold standard of pulmonary aspergillosis mainly relies on chest imaging, microbial culture and histopathological examination. However, the imaging manifestations are poor in specificity for non-agranulocytic patients, and the phenomena of “the same disease with different image, and the different disease with same image” exist [21, 22]. For microbiological and histopathological examination, it is difficult to obtain pathological specimens, the positive rate of culture is low, and the specimens can possibly be contaminated and colonized. Therefore, the clinical diagnosis of non-agranulocytic pulmonary aspergillosis is difficult, and it is not always feasible to obtain histopathological or cytopathological demonstration of the fungus to meet the gold standard [23]. As a non-invasive diagnostic method of pulmonary mycosis, the detection of serum antigens and antibodies has attracted increasing attention. The G test and GM test are mainly used for the clinical diagnosis of IPA in agranulocytic patients, but the positive rate of IPA in non-agranulocytic patients is too low to meet clinical needs [24, 25]. For patients with agranulocytosis or severe immunosuppression, it is difficult for the body to produce an immune response. Accordingly, the detection of specific antibodies against Aspergillus is of little significance. With the increase in non-agranulocytic and non-immunocompromised hosts, the diagnostic significance of antibody detection for pulmonary aspergillosis needs to be re-evaluated. Serum Aspergillus antibody detection is mainly used for the diagnosis of CPA [5, 26]. However, the diagnostic value of Aspergillus antibody detection is unclear for IPA in non-agranulocytic patients because of varying results [23]. Additionally, the diagnosis of chronic pulmonary aspergillosis (CPA) is complicated, and there are limited data available [27]. Here, we compared the performances of the G test, GM test, and Aspergillus IgG antibody detection by using serum samples from non-agranulocytic patients with underlying pulmonary aspergillosis diseases and further subdivided IPA and CPA cases (Tables 3 and 5). The results showed that there was no significant difference in serum Aspergillus IgM antibodies between pulmonary aspergillosis, community-acquired bacterial pneumonia and healthy people. The reasons may include the following: 1. IgM is the earliest immunoglobulin produced after infection or immunization. It has strong bactericidal and regulatory effects, but its content in blood is low, its half-life is short, and it is susceptible to interference factors. 2. Non-granulocyte-deficient hosts may undergo a period of Aspergillus colonization and slow invasion before infection due to their relatively sound immune function. There are several studies about serum Aspergillus IgM antibody detection and its significance in the diagnosis of pulmonary aspergillosis. A multicentre prospective study evaluated the clinical performance of a commercial specific IgM antibody against A. fumigatus for the first time, and the results revealed that the detection of serum IgM antibody specific to A.fumigatus is of little help in the current diagnosis of IPA and CPA in Chinese patients, which is consistent with our results [28, 29]. IgM often occurs in the early stage of infection. Therefore, Aspergillus IgG antibody detection is more significant than Aspergillus IgM antibody detection. Our results revealed that Aspergillus IgG antibody reflected the greatest differences among the pulmonary aspergillosis (even IPA and CPA subdivisions), community-acquired bacterial pneumonia and healthy groups (P < 0.0001) (Tables 3 and 4). It was indicated that Aspergillus IgG antibody might be a potential diagnostic index for pulmonary aspergillosis in non-agranulocytic patients, and its performance was further evaluated through ROC curve analysis.
As exhibited in Fig. 1, Aspergillus IgG had notable differences in pulmonary aspergillosis (even IPA and CPA subdivision), community-acquired bacterial pneumonia and the healthy group (P < 0.05), and the specificity and sensitivity were 40.5–95.2% and 58.8–95.2%, respectively, and the highest AUC was 0.873. Previous studies have shown that the sensitivity and specificity of Aspergillus IgG antibody detection for CPA diagnosis are 75–96% and 97–99%, respectively [30]. The specificity and sensitivity were lower than those in a previous report, which might be because the underlying conditions of the research population and the experimental methods are different. Our study further certified that serum Aspergillus IgG antibody had better performance for distinguishing CPA than IPA. From acute invasive infection to chronic consumptive diseases, different types of pulmonary aspergillosis can overlap with each other. Generally, IPA occurs in patients with various degrees of impaired immune function, while CPA occurs in patients without or with a lower degree of impaired immune function. Therefore, serum Aspergillus antibody levels differ in different types of pulmonary aspergillosis, which is more significant for patients with CPA. Above all, we suspected that serum Aspergillus IgG detection has certain clinical value in the diagnosis of pulmonary aspergillosis in non-agranulocytic patients, especially for non-agranulocytic CPA. However, it was believed that serum Aspergillus IgG could not replace the traditional isolation and culture of fungi and should be combined with other diagnostic methods and clinical practice. However, this study is an exploratory study, which has the defect of insufficient supporting research literature. And some low AUC values may be caused by our small sample size. The conclusion of this study is preliminary, and we will further prove and improve it in the future research.
Conclusions
In conclusion, serum Aspergillus IgG detection may have certain clinical value in the diagnosis of IPA and CPA in non-agranulocytic patients.
Supplementary information
Additional file 1: Table S1. The results of ROC analysis of Aspergillus IgG antibody in different groups
Acknowledgements
None.
Abbreviations
- CPA
Chronic pulmonary aspergillosis
- IPA
Invasive pulmonary aspergillosis
- AUC
Area under curve
- APA
Acute pulmonary aspergillosis
- GM test
Galactomannan test
- G test
(1,3)-β-D-glucan test
- ELISA
Enzyme-linked immunosorbent assay
- ROC
Receiver operating characteristic curve
Authors’ contributions
HP participated in the conceived of the study, design of the study and modify of manuscript; QY participated in the conceived of the study, carried out the studies, performed the statistical analysis, and draft the manuscript, JH, BX, XL, HQ, HZ and MX participated in its design, coordination, perform the statistical analysis and modified the manuscript. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
Data are available from the corresponding author upon a reasonable request.
Ethics approval and consent to participate
This study was approved by the ethics committee of Tianjin Chest Hospital (2018KY-009-01). All participants has signed the informed consent voluntarily.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12890-020-1125-y.
References
- 1.Bassetti M, Carnelutti A, Righi E. Issues in the management of invasive pulmonary aspergillosis in non-neutropenic patients in the intensive care unit: a role Bronchoalveolar lavage galactomannan for the diagnosis of chronic pulmonary aspergillosifor isavuconazole. Idcases. 2018;12:7–9. doi: 10.1016/j.idcr.2018.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Workum JD, Jong SWD, Gresnigt MS, Becker KL, Pickkers P, van de Veerdonk FL, et al. Microbiological and immunological characteristics of a lethal pulmonary Aspergillus Niger infection in a non-neutropenic patient. Med Mycol Case Rep. 2018;21:4–7. doi: 10.1016/j.mmcr.2018.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Soubani AO, Chandrasekar PH. The clinical spectrum of pulmonary aspergillosis. Chest. 2002;121(6):1988–1999. doi: 10.1378/chest.121.6.1988. [DOI] [PubMed] [Google Scholar]
- 4.Barac A, Kosmidis C, Alastruey-Izquierdo A, Salzer HJF. Chronic pulmonary aspergillosis update: A year in review. Med Mycol. 2019;57(Supplement_2):S104–S109. doi: 10.1093/mmy/myy070. [DOI] [PubMed] [Google Scholar]
- 5.Denning DW, Cadranel J, Beigelmanaubry C, Ader F, Chakrabarti A, Blot S, et al. Chronic pulmonary aspergillosis: rationale and clinical guidelines for diagnosis and management. Eur Respir J. 2016;47(1):45–68. doi: 10.1183/13993003.00583-2015. [DOI] [PubMed] [Google Scholar]
- 6.Swoboda-Kopeć E, Sikora M, Piskorska K, Gołaś M, Netsvyetayeva I, Przybyłowska D, et al. Diagnosis of invasive pulmonary Aspergillosis. Adv Exp Med Biol. 2017;944:27–33. doi: 10.1007/5584_2016_46. [DOI] [PubMed] [Google Scholar]
- 7.Kaya S, Gençalioğlu E, Sönmez M, Köksal I. The importance of risk factors for the prediction of patients with invasive pulmonary aspergillosis. Rev Assoc Med Bras. 2017;63(9):764–770. doi: 10.1590/1806-9282.63.09.764. [DOI] [PubMed] [Google Scholar]
- 8.Shin B, Koh WJ, Jeong BH, Yoo H, Park HY, Suh GY, et al. Serum galactomannan antigen test for the diagnosis of chronic pulmonary aspergillosis. J Inf Secur. 2014;68(5):494–499. doi: 10.1016/j.jinf.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 9.Sehgal IS, Dhooria S, Choudhary H, Aggarwal AN, Garg M, Chakrabarti A, et al. Utility of serum and Bronchoalveolar lavage fluid Galactomannan in diagnosis of chronic pulmonary Aspergillosis. J Clin Microbiol. 2019;57(3):e01821–e01818. doi: 10.1128/JCM.01821-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sehgal IS, Choudhary H, Dhooria S, Aggarwal AN, Garg M, Chakrabarti A, et al. Diagnostic cut-off of Aspergillus fumigatus-specific IgG in the diagnosis of chronic pulmonary aspergillosis. Mycoses. 2018;61(10):770–776. doi: 10.1111/myc.12815. [DOI] [PubMed] [Google Scholar]
- 11.De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/invasive fungal infections cooperative group and the National Institute of Allergy and Infectious Diseases mycoses study group (EORTC/MSG) consensus group. Clin Infect Dis. 2008;46(12):1813–1821. doi: 10.1086/588660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patterson TF, Thompson GR, 3rd, Denning DW, Fishman JA, Hadley S, Herbrecht R, et al. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;63(4):e1–e60. doi: 10.1093/cid/ciw326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pazos C, Ponton J, Palacio AD. Contribution of (1->3)-beta-D-glucan chromogenic assay to diagnosis and therapeutic monitoring of invasive aspergillosis in neutropenic adult patients: a comparison with serial screening for circulating galactomannan. J Clin Microbiol. 2005;43(1):299–305. doi: 10.1128/JCM.43.1.299-305.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu L, Li J, Dong H, Jiang L, Song H, Zhang S, et al. Diagnostic value of the combinations of bronchoalveolar lavage fluid galactomannan test and serum galactomannan test in invasive pulmonary aspergillosis. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2019;31(3):331–335. doi: 10.3760/cma.j.issn.2095-4352.2019.03.014. [DOI] [PubMed] [Google Scholar]
- 15.Li H, Rui Y, Zhou W, Liu L, He B, Shi Y, et al. Role of the Aspergillus-specific IgG and IgM test in the diagnosis and follow-up of chronic pulmonary aspergillosis. Front Microbiol. 2019;10:1438. doi: 10.3389/fmicb.2019.01438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hou X, Zhang H, Kou L, Lv W, Lv J, Li J. Clinical features and diagnosis of chronic pulmonary aspergillosis in Chinese patients. Medicine. 2017;96(42):e8315. doi: 10.1097/MD.0000000000008315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhirong Y, Wanqing L, Weihua P. Case reports. Invasive pulmonary aspergillosis in non-neutropenic patients treated with liposomal amphotericin B. Mycoses. 1999;42(11–12):679–682. doi: 10.1046/j.1439-0507.1999.00508.x. [DOI] [PubMed] [Google Scholar]
- 18.Xia ZF, Li HY, Liu L, Wang GY, Zhu SH, Huang Y, et al. Pulmonary aspergillosis in a non-neutropenic critical patient. J Trauma. 2010;69(4):E37. doi: 10.1097/TA.0b013e3181a5aa5b. [DOI] [PubMed] [Google Scholar]
- 19.Filippou N, Papachristou K, Ilias I, Pefanis A, Papaleftheris E, Iliopoulos I. Case report. Chronic necrotizing pulmonary aspergillosis in a non-neutropenic patient treated with liposomal amphotericin B. Mycoses. 2010;43(7–8):313–315. doi: 10.1046/j.1439-0507.2000.00579.x. [DOI] [PubMed] [Google Scholar]
- 20.Dai Z, Zhao H, Cai S, Lv Y, Tong W. Invasive pulmonary aspergillosis in non-neutropenic patients with and without underlying disease: a single-Centre retrospective analysis of 52 subjects. Respirology. 2013;18(2):323–331. doi: 10.1111/j.1440-1843.2012.02283.x. [DOI] [PubMed] [Google Scholar]
- 21.Kawel N, Schorer GM, Desbiolles L, Seifert B, Marincek B, Boehm T. Discrimination between invasive pulmonary aspergillosis and pulmonary lymphoma using CT. Eur J Radiol. 2011;77(3):417–425. doi: 10.1016/j.ejrad.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 22.Kuhlman JE, Fishman EK, Siegelman SS. Invasive pulmonary aspergillosis in acute leukemia: characteristic findings on CT, the CT halo sign, and the role of CT in early diagnosis. Radiology. 1985;157(3):611–614. doi: 10.1148/radiology.157.3.3864189. [DOI] [PubMed] [Google Scholar]
- 23.Trof RJ, Beishuizen A, Debets-Ossenkopp YJ, Girbes AR, Groeneveld AB. Management of invasive pulmonary aspergillosis in non-neutropenic critically ill patients. Intensive Care Med. 2007;33(10):1694–1703. doi: 10.1007/s00134-007-0791-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reichenberger F, Habicht JM, Gratwohl A, Tamm M. Diagnosis and treatment of invasive pulmonary aspergillosis in neutropenic patients. Eur Respir J. 2002;19(4):743–755. doi: 10.1183/09031936.02.00256102. [DOI] [PubMed] [Google Scholar]
- 25.Kim R, Koh Y, Shin DY, Choe PG, Kim NJ, Yoon SS, et al. The limited role of serum galactomannan assay in screening for invasive pulmonary aspergillosis in allogeneic stem cell transplantation recipients on micafungin prophylaxis: a retrospective study. Blood Res. 2017;52(4):300–306. doi: 10.5045/br.2017.52.4.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Page ID, Richardson MD, Denning DW. Siemens Immulite Aspergillus-specific IgG assay for chronic pulmonary aspergillosis diagnosis. Med Mycol. 2019;57(3):300–307. doi: 10.1093/mmy/myy024. [DOI] [PubMed] [Google Scholar]
- 27.Izumikawa K, Yamamoto Y, Mihara T, Takazono T, Morinaga Y, Kurihara S, et al. Bronchoalveolar lavage galactomannan for the diagnosis of chronic pulmonary aspergillosis. Med Mycol. 2012;50(8):811–817. doi: 10.3109/13693786.2012.682228. [DOI] [PubMed] [Google Scholar]
- 28.Yao Y, Zhou H, Shen Y, Yang Q, Ye J, Lu G, et al. Evaluation of a commercial quantitative Aspergillus fumigatus-specific IgM assay for the diagnosis of invasive pulmonary aspergillosis. Medicine. 2017;96(51):e9436. doi: 10.1097/MD.0000000000009436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yao Y, Zhou H, Shen Y, Yang Q, Ye J, Fu Y, et al. Evaluation of a quantitative serum Aspergillus fumigatus-specific IgM assay for diagnosis of chronic pulmonary aspergillosis. Clin Respir J. 2018;12(11):2566–2572. doi: 10.1111/crj.12957. [DOI] [PubMed] [Google Scholar]
- 30.Page ID, Richardson MD, Denning DW. Comparison of six Aspergillus-specific IgG assays for the diagnosis of chronic pulmonary aspergillosis (CPA) J Inf Secur. 2016;72(2):240–249. doi: 10.1016/j.jinf.2015.11.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. The results of ROC analysis of Aspergillus IgG antibody in different groups
Data Availability Statement
Data are available from the corresponding author upon a reasonable request.