Governments will not be able to minimise both deaths from coronavirus disease 2019 (COVID-19) and the economic impact of viral spread. Keeping mortality as low as possible will be the highest priority for individuals; hence governments must put in place measures to ameliorate the inevitable economic downturn. In our view, COVID-19 has developed into a pandemic, with small chains of transmission in many countries and large chains resulting in extensive spread in a few countries, such as Italy, Iran, South Korea, and Japan.1 Most countries are likely to have spread of COVID-19, at least in the early stages, before any mitigation measures have an impact.
What has happened in China shows that quarantine, social distancing, and isolation of infected populations can contain the epidemic.1 This impact of the COVID-19 response in China is encouraging for the many countries where COVID-19 is beginning to spread. However, it is unclear whether other countries can implement the stringent measures China eventually adopted. Singapore and Hong Kong, both of which had severe acute respiratory syndrome (SARS) epidemics in 2002–03, provide hope and many lessons to other countries. In both places, COVID-19 has been managed well to date, despite early cases, by early government action and through social distancing measures taken by individuals.
The course of an epidemic is defined by a series of key factors, some of which are poorly understood at present for COVID-19. The basic reproduction number (R0), which defines the mean number of secondary cases generated by one primary case when the population is largely susceptible to infection, determines the overall number of people who are likely to be infected, or more precisely the area under the epidemic curve. For an epidemic to take hold, the value of R0 must be greater than unity in value. A simple calculation gives the fraction likely to be infected without mitigation. This fraction is roughly 1–1/R0. With R0 values for COVID-19 in China around 2·5 in the early stages of the epidemic,2 we calculate that approximately 60% of the population would become infected. This is a very worst-case scenario for a number of reasons. We are uncertain about transmission in children, some communities are remote and unlikely to be exposed, voluntary social distancing by individuals and communities will have an impact, and mitigation efforts, such as the measures put in place in China, greatly reduce transmission. As an epidemic progresses, the effective reproduction number (R) declines until it falls below unity in value when the epidemic peaks and then decays, either due to the exhaustion of people susceptible to infection or the impact of control measures.
The speed of the initial spread of the epidemic, its doubling time, or the related serial interval (the mean time it takes for an infected person to pass on the infection to others), and the likely duration of the epidemic are determined by factors such as the length of time from infection to when a person is infectious to others and the mean duration of infectiousness. For the 2009 influenza A H1N1 pandemic, in most infected people these epidemiological quantities were short with a day or so to infectiousness and a few days of peak infectiousness to others.3 By contrast, for COVID-19, the serial interval is estimated at 4·4–7·5 days, which is more similar to SARS.4
First among the important unknowns about COVID-19 is the case fatality rate (CFR), which requires information on the denominator that defines the number infected. We are unaware of any completed large-scale serology surveys to detect specific antibodies to COVID-19. Best estimates suggest a CFR for COVID-19 of about 0·3–1%,4 which is higher than the order of 0·1% CFR for a moderate influenza A season.5
The second unknown is the whether infectiousness starts before onset of symptoms. The incubation period for COVID-19 is about 5–6 days.4, 6 Combining this time with a similar length serial interval suggests there might be considerable presymptomatic infectiousness (appendix 1). For reference, influenza A has a presymptomatic infectiousness of about 1–2 days, whereas SARS had little or no presymptomatic infectiousness.7 There have been few clinical studies to measure COVID-19 viraemia and how it changes over time in individuals. In one study of 17 patients with COVID-19, peak viraemia seems to be at the end of the incubation period,8 pointing to the possibility that viraemia might be high enough to trigger transmission for 1–2 days before onset of symptoms. If these patterns are verified by more extensive clinical virological studies, COVID-19 would be expected to be more like influenza A than SARS. For SARS, peak infectiousness took place many days after first symptoms, hence the success of quarantine of patients with SARS soon after symptoms started7 and the lack of success for this measure for influenza A and possibly for COVID-19.
The third uncertainty is whether there are a large number of asymptomatic cases of COVID-19. Estimates suggest that about 80% of people with COVID-19 have mild or asymptomatic disease, 14% have severe disease, and 6% are critically ill,9 implying that symptom-based control is unlikely to be sufficient unless these cases are only lightly infectious.
The fourth uncertainty is the duration of the infectious period for COVID-19. The infectious period is typically short for influenza A, but it seems long for COVID-19 on the basis of the few available clinical virological studies, perhaps lasting for 10 days or more after the incubation period.8 The reports of a few super-spreading events are a routine feature of all infectious diseases and should not be overinterpreted.10
What do these comparisons with influenza A and SARS imply for the COVID-19 epidemic and its control? First, we think that the epidemic in any given country will initially spread more slowly than is typical for a new influenza A strain. COVID-19 had a doubling time in China of about 4–5 days in the early phases.3 Second, the COVID-19 epidemic could be more drawn out than seasonal influenza A, which has relevance for its potential economic impact. Third, the effect of seasons on transmission of COVID-19 is unknown;11 however, with an R0 of 2–3, the warm months of summer in the northern hemisphere might not necessarily reduce transmission below the value of unity as they do for influenza A, which typically has an R0 of around 1·1–1·5.12 Closely linked to these factors and their epidemiological determinants is the impact of different mitigation policies on the course of the COVID-19 epidemic.
A key issue for epidemiologists is helping policy makers decide the main objectives of mitigation—eg, minimising morbidity and associated mortality, avoiding an epidemic peak that overwhelms health-care services, keeping the effects on the economy within manageable levels, and flattening the epidemic curve to wait for vaccine development and manufacture on scale and antiviral drug therapies. Such mitigation objectives are difficult to achieve by the same interventions, so choices must be made about priorities.13 For COVID-19, the potential economic impact of self-isolation or mandated quarantine could be substantial, as occurred in China.
No vaccine or effective antiviral drug is likely to be available soon. Vaccine development is underway, but the key issues are not if a vaccine can be developed but where phase 3 trials will be done and who will manufacture vaccine at scale. The number of cases of COVID-19 are falling quickly in China,4 but a site for phase 3 vaccine trials needs to be in a location where there is ongoing transmission of the disease. Manufacturing at scale requires one or more of the big vaccine manufacturers to take up the challenge and work closely with the biotechnology companies who are developing vaccine candidates. This process will take time and we are probably a least 1 year to 18 months away from substantial vaccine production.
So what is left at present for mitigation is voluntary plus mandated quarantine, stopping mass gatherings, closure of educational institutes or places of work where infection has been identified, and isolation of households, towns, or cities. Some of the lessons from analyses of influenza A apply for COVID-19, but there are also differences. Social distancing measures reduce the value of the effective reproduction number R. With an early epidemic value of R0 of 2·5, social distancing would have to reduce transmission by about 60% or less, if the intrinsic transmission potential declines in the warm summer months in the northern hemisphere. This reduction is a big ask, but it did happen in China.
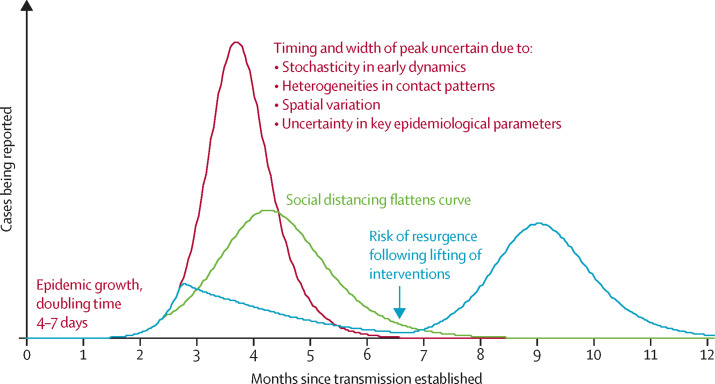
School closure, a major pillar of the response to pandemic influenza A,14 is unlikely to be effective given the apparent low rate of infection among children, although data are scarce. Avoiding large gatherings of people will reduce the number of super-spreading events; however, if prolonged contact is required for transmission, this measure might only reduce a small proportion of transmissions. Therefore, broader-scale social distancing is likely to be needed, as was put in place in China. This measure prevents transmission from symptomatic and non-symptomatic cases, hence flattening the epidemic and pushing the peak further into the future. Broader-scale social distancing provides time for the health services to treat cases and increase capacity, and, in the longer term, for vaccines and treatments to be developed. Containment could be targeted to particular areas, schools, or mass gatherings. This approach underway in northern Italy will provide valuable data on the effectiveness of such measures. The greater the reduction in transmission, the longer and flatter the epidemic curve (figure ), with the risk of resurgence when interventions are lifted perhaps to mitigate economic impact.
Figure.
Illustrative simulations of a transmission model of COVID-19
A baseline simulation with case isolation only (red); a simulation with social distancing in place throughout the epidemic, flattening the curve (green), and a simulation with more effective social distancing in place for a limited period only, typically followed by a resurgent epidemic when social distancing is halted (blue). These are not quantitative predictions but robust qualitative illustrations for a range of model choices.
The key epidemiological issues that determine the impact of social distancing measures are what proportion of infected individuals have mild symptoms and whether these individuals will self-isolate and to what effectiveness; how quickly symptomatic individuals take to isolate themselves after the onset of symptoms; and the duration of any non-symptomatic infectious period before clear symptoms occur with the linked issue of how transmissible COVID-19 is during this phase.
Individual behaviour will be crucial to control the spread of COVID-19. Personal, rather than government action, in western democracies might be the most important issue. Early self-isolation, seeking medical advice remotely unless symptoms are severe, and social distancing are key. Government actions to ban mass gatherings are important, as are good diagnostic facilities and remotely accessed health advice, together with specialised treatment for people with severe disease. Isolating towns or even cities is not yet part of the UK Government action plan.15 This plan is light on detail, given the early stages of the COVID-19 epidemic and the many uncertainties, but it outlines four phases of action entitled contain, delay, research, and mitigate.15 The UK has just moved from contain to delay, which aims to flatten the epidemic and lower peak morbidity and mortality. If measures are relaxed after a few months to avoid severe economic impact, a further peak is likely to occur in the autumn (figure). Italy, South Korea, Japan, and Iran are at the mitigate phase and trying to provide the best care possible for a rapidly growing number of people with COVID-19.
The known epidemiological characteristics of COVID-19 point to urgent priorities. Shortening the time from symptom onset to isolation is vital as it will reduce transmission and is likely to slow the epidemic (appendices 2, 3) However, strategies are also needed for reducing household transmission, supporting home treatment and diagnosis, and dealing with the economic consequences of absence from work. Peak demand for health services could still be high and the extent and duration of presymptomatic or asymptomatic transmission—if this turns out to be a feature of COVID-19 infection—will determine the success of this strategy.16
Contact tracing is of high importance in the early stages to contain spread, and model-based estimates suggest, with an R0 value of 2·5, that about 70% of contacts will have to be successfully traced to control early spread.17 Analysis of individual contact patterns suggests that contact tracing can be a successful strategy in the early stages of an outbreak, but that the logistics of timely tracing on average 36 contacts per case will be challenging.17 Super-spreading events are inevitable, and could overwhelm the contact tracing system, leading to the need for broader-scale social distancing interventions.
Data from China, South Korea, Italy, and Iran suggest that the CFR increases sharply with age and is higher in people with COVID-19 and underlying comorbidities.18 Targeted social distancing for these groups could be the most effective way to reduce morbidity and concomitant mortality. During the outbreak of Ebola virus disease in west Africa in 2014–16, deaths from other causes increased because of a saturated health-care system and deaths of health-care workers.19 These events underline the importance of enhanced support for health-care infrastructure and effective procedures for protecting staff from infection.
In northern countries, there is speculation that changing contact patterns and warmer weather might slow the spread of the virus in the summer.11 With an R0 of 2·5 or higher, reductions in transmission by social distancing would have to be large; and much of the changes in transmission of pandemic influenza in the summer of 2009 within Europe were thought to be due to school closures, but children are not thought to be driving transmission of COVID-19. Data from the southern hemisphere will assist in evaluating how much seasonality will influence COVID-19 transmission.
Model-based predictions can help policy makers make the right decisions in a timely way, even with the uncertainties about COVID-19. Indicating what level of transmission reduction is required for social distancing interventions to mitigate the epidemic is a key activity (figure). However, it is easy to suggest a 60% reduction in transmission will do it or quarantining within 1 day from symptom onset will control transmission, but it is unclear what communication strategies or social distancing actions individuals and governments must put in place to achieve these desired outcomes. A degree of pragmatism will be needed for the implementation of social distancing and quarantine measures. Ongoing data collection and epidemiological analysis are therefore essential parts of assessing the impacts of mitigation strategies, alongside clinical research on how to best manage seriously ill patients with COVID-19.
There are difficult decisions ahead for governments. How individuals respond to advice on how best to prevent transmission will be as important as government actions, if not more important. Government communication strategies to keep the public informed of how best to avoid infection are vital, as is extra support to manage the economic downturn.
Acknowledgments
RMA was a Non-Executive Director of GlaxoSmithKline (GSK) for 10 years up to May, 2018, and had past advisory roles for SARS and Influenza A for WHO and the UK Government. DK works at the National Institute for Public Health and the Environment in the Netherlands and is as such involved in advising the Dutch Government on infectious disease control. HH and TDH declare no competing interests.
Supplementary Materials
References
- 1.WHO Coronavirus disease 2019 (COVID-19) situation report—44. March 4, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200304-sitrep-44-covid-19.pdf?sfvrsn=783b4c9d_2 (accessed March 5, 2020).
- 2.Imperial College London, MRC Centre for Global Infectious Disease Analysis News / COVID-19—report 3: transmissibility of 2019-nCoV. 2020. Feb 21, 2010. https://www.imperial.ac.uk/mrc-global-infectious-disease-analysis/news–wuhan-coronavirus/ (accessed March 5, 2020).
- 3.Fraser C, Riley S, Anderson RM, Ferguson NM. Factors that make an infectious disease outbreak controllable. Proc Natl Acad Sci USA. 2004;101:6146–6151. doi: 10.1073/pnas.0307506101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO Coronavirus disease (COVID-2019) situation report—30. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200219-sitrep-30-covid-19.pdf?sfvrsn=3346b04f_2 (accessed March 5, 2020).
- 5.Li L, Wong JY, Wu P, Bond HS, Lau EH, Sullivan SG, Cowling BJ. Heterogeneity in estimates of the impact of influenza on population mortality: a systematic review. Am J Epidemiol. 2018;187:378–388. doi: 10.1093/aje/kwx270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020 doi: 10.1056/NEJMoa2001316. published online Jan 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anderson RM, Fraser F, et al. Epidemiology, transmission dynamics and control of SARS: the 2002–2003 epidemic. Phil Trans Roy Soc Ser B. 2004;359:1091–1490. doi: 10.1098/rstb.2004.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zou L, Ruan F, Huang M, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020 doi: 10.1056/NEJMc2001737. published online Feb 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.European Centre for Disease Prevention and Control Daily risk assessment on COVID-19. 2020. https://www.ecdc.europa.eu/en/current-risk-assessment-novel-coronavirus-situation (accessed March 5, 2020).
- 10.Lloyd-Smith JO, Schreiber SJ, Kopp PE, Getz WM. Superspreading and the effect of individual variation on disease emergence. Nature. 2005;438:355–359. doi: 10.1038/nature04153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lipsitch M. Will COVID-19 go away on its own in warmer weather? Center for Communicable Disease Dynamics (CCDD) at the Harvard T.H. Chan School of Public Health. 2020. https://ccdd.hsph.harvard.edu/will-covid-19-go-away-on-its-own-in-warmer-weather/ (accessed March 5, 2020).
- 12.Boëlle PY, Ansart S, Cori A, Valleron AJ. Transmission parameters of the A/H1N1 (2009) influenza virus pandemic: a review. Influenza Other Respir Viruses. 2011;5:306–316. doi: 10.1111/j.1750-2659.2011.00234.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hollingsworth TD, Klinkenberg D, Heesterbeek H, Anderson RM. Mitigation strategies for pandemic influenza A: balancing conflicting policy objectives. PLoS Comput Biol. 2011;7:e1001076. doi: 10.1371/journal.pcbi.1001076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cauchemez S, Ferguson NM, Wachtel C, et al. Closure of schools during an influenza pandemic. Lancet Infect Dis. 2009;9:473–481. doi: 10.1016/S1473-3099(09)70176-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.UK Government, Department of Health and Social Care Coronavirus action plan. March 3, 2020. https://www.gov.uk/government/publications/coronavirus-action-plan (accessed March 5, 2020).
- 16.Hellewell J, Abbott S, Gimma A, et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob Health. 2020 doi: 10.1016/S2214-109X(20)30074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Keeling MJ, Hollingsworth TD, Read JM. The efficacy of contact tracing for the containment of the 2019 novel coronavirus (COVID-19) medRxiv. 2020 doi: 10.1101/2020.02.14.20023036. published online Feb 17. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team The epidemiological characteristics of an outbreak of 2019 novel coronavirus disease (COVD-19) China CDC Weekly. 2020;2:113–122. [PMC free article] [PubMed] [Google Scholar]
- 19.Elston JW, Cartwright C, Ndumbi P, Wright J. The health impact of the 2014–15 Ebola outbreak. Public Health. 2017;143:60–70. doi: 10.1016/j.puhe.2016.10.020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.