Abstract
In the global pandemic COVID-19, it is important for everyone including nuclear medicine personnel to know how to stop transmission and contain and prevent the spread of COVID-19. Here, we summarize our American College of Nuclear Medicine members’ experiences from Wuhan, China; Singapore; and the USA, so to provide advice to the nuclear medicine personnel for their clinical practice and management strategies in responding to COVID-19.
The novel coronavirus disease 2019 (COVID-19), which was first identified in Wuhan, China, in December 2019 [1], is evolving into an international public health emergency. On March 11, 2020, the World Health Organization formally announced the COVID-19 as a “global pandemic,” when there were a total of more than 120,000 cases in 114 countries including 4373 deaths [2]. On March 13, 2020, the US President Trump declared a national emergency to address the COVID-19 pandemic. According to the real time updated data from Johns Hopkins University [3], as of March 28, 2020, 06:50 CST, the virus has now killed 28,687 people and infected 614,884 in 177 countries/regions, and is continuing to spread into previously unaffected areas. Among the most infected countries, there are a total of 81,996 confirmed cases in China. Meanwhile, there are total 135,671 recovered cases, mainly from China, and only 894 recovered in the USA. Although the COVID-19 is slowing down and appears under control in China, the cases outside China have risen rapidly. Italy just expanded COVID-19 lockdown to the whole country and reported more than 10,000 cases and 631 deaths on March 9, 2020, while on March 28, the number rose to 86,498 confirmed cases and 9134 deaths. Although the first case was just detected on January 19, 2020 [4], the USA now has 104,837 confirmed cases, surpassed Italy and China, and became the most infected country with 1716 deaths on March 28, in merely 2 months [3]. The virus can spread from person-to-person very quickly not only through respiratory droplets but also through community spread and asymptomatic infected patients [5]. To protect and save lives, it is very important for every nuclear medicine personnel to know how to stop transmission, and contain and prevent the spread of COVID-19, meanwhile to support the healthcare workforce during this global epidemic.
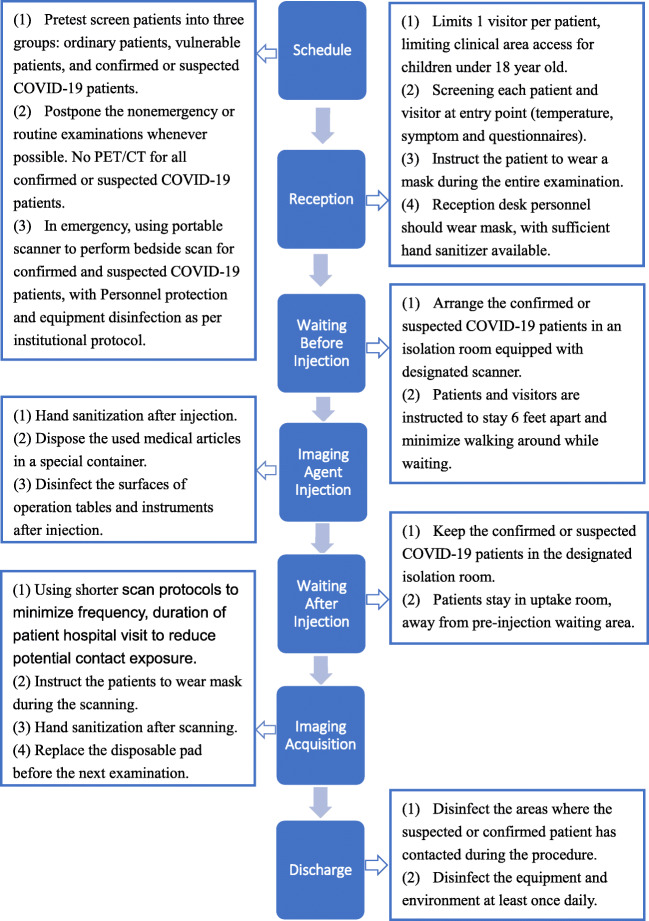
American College of Nuclear Medicine (ACNM) membership mainly comprises nuclear medicine physicians from the USA and other countries including China. We reached out to our ACNM international members from Wuhan, China, and Singapore who have participated in dealing with COVID-19 for the last 2 months, to learn from their lessons and experiences (Lan, Sun [6], [7, 8]), and adopted their measures in our busy nuclear medicine practice in the USA, which routinely consists ~ 100 general nuclear medicine studies including planar and SPECT/CT images, and ~ 130 PET/CT studies on a daily basis. Here, we summarized our ACNM members’ composite experiences, aiming to provide advices for nuclear medicine department/personnel in fighting this global pandemic COVID-19. Figure 1 summarizes the protection measures adopted for nuclear medicine procedures during COVID-19 epidemic in our ACNM members’ departments. We also want to emphasize the following key points for nuclear medicine management strategy.
Fig. 1.
Protection measures in the procedures of nuclear medical imaging
First, be adherent to institutional and/or WHO’s infection prevention and control recommendations, and be alert to people who have COVID-19-related symptoms and clinical features. When in contact with the suspected patients or visitors, nuclear medicine staff should maintain at least 3 ft distance, wear masks, and be mindful of hand hygiene. Before the COVID-19 got detected and known to the public, a later confirmed COVID-19 patient presented to the nuclear medicine department for FDG PET/CT exam in Wuhan [8]. The nuclear medicine staff and physicians were wearing masks and washed their hands frequently as routine for seasonal flu precaution. Fortunate enough, none of the nuclear medicine personnel got infected despite close contact with this COVID-19 patient, so is the situation in other 4 highly suspected COVID-19 cases in another PET/CT center in Wuhan [7].
Second, temporarily change routine clinical nuclear medicine practice to minimize the risk of infection for nuclear medicine personnel and patients. Measures that can be considered are (1) to reschedule and postpone outpatient nuclear medicine and PET/CT tests whenever possible; (2) to temporarily reject procedures and scans which bear high risk of respiratory communications and can be substituted or postponed, such as urea breath test, and convert V/Q scan to perfusion only with and without SPECT/CT; (3) to change scan protocols to minimize frequency and duration of patient hospital visit to reduce potential contact exposure. For example, use shorter scanning time for SPECT/CT, avoid unnecessary delayed time point or multi-day images, and convert any 2-day myocardial perfusion test to 1 day protocol; (4) to limit visitors to one adult at a time. Visitors must be age 18 or older to enter and must pass screening questions and must not have any respiratory viral symptoms. Screening assessment will include temperature assessment of all patients and visitors to clinical areas; (5) One person to the end policy—in case of any suspected or confirmed case for scan or any procedure, change of nurse or technician in the middle of the procedure is not allowed.
Third, temporarily change academic routine: switch all weekly teachings, peer review learnings, and tumor board meetings to online virtual meeting by using Zoom or Webex, etc.; cancel all the planned domestic and international business and personal travel when possible.
Fourth, segregation of nuclear medicine physicians and staff, as well as inpatients and outpatients so that there is as little as possible cross exposure risks. An onsite team stays in the main department responsible for all patient contacts including radiotracer administration, patient interview, and consultation; the team should be further separated into outpatient and inpatient groups; An offsite team stays away from patient contact, work from individual office or home, reading scans, and participating in online tumor boards, and provide telemedicine and online consultation to referring physicians and patients. The two teams are prohibited from having any direct contact. A fixed, designated physician should be assigned to cover the service in each satellite site to minimize possible inter-institutional transmission. The rotation is every 14 days. Ideally, there should be COVID-19 tests for onsite team members at the end of rotation. If intra-hospital transmission occurs, this approach would avoid shutdown of the entire department should a quarantine be required.
Lastly, if suspected CT and/or PET/CT findings of COVID-19 infection [7–10] be identified by nuclear medicine physician, the institutional COVID-19 team should be informed immediately, and the suspected patient and visitors, as well as nuclear medicine personnel who has been in contact with this patient, should be noticed, quarantined, and treated accordingly.
The above measures have been proactively and progressively implemented in our ACNM members’ departments since the onset of the COVID-19 outbreak in China and Singapore, and now adopted in the USA. There has been no single nuclear medicine personnel to get infected by COVID-19 in the author’s nuclear medicine departments. We suggest nuclear medicine personnel take references of these measures to make tailored institutional approaches in terms of planning for screening, rapid testing, and isolation and treatment procedures based on the available local resources.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent for publication
All the authors consent for publication if accepted.
Footnotes
This article is part of the Topical Collection on Infection and Inflammation
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coronavirus disease (COVID-19) outbreak. Situation updates: World Health Organization. 2020. https://www.who.int/. Accessed 28 March 2020.
- 3.Coronavirus COVID-19 global cases by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Johns Hopkins University; 2020. https://www.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6. Accessed 28 March 2020.
- 4.Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin C, Ding Y, Xie B, Sun Z, Li X, Chen Z, et al. Asymptomatic novel coronavirus pneumonia patient outside Wuhan: the value of CT images in the course of the disease. Clin Imaging. 2020;63:7–9. doi: 10.1016/j.clinimag.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lan X, Sun X, Win C, Ruan W, Hu J, Lin J, et al. Protection management and procedures of nuclear medicine imaging during novel coronavirus infection epidemic period. Chin J Nucl Med Mol Imaging. 2020;40:105–107. [Google Scholar]
- 7.Qin Chunxia, Liu Fang, Yen Tzu-Chen, Lan Xiaoli. 18F-FDG PET/CT findings of COVID-19: a series of four highly suspected cases. European Journal of Nuclear Medicine and Molecular Imaging. 2020;47(5):1281–1286. doi: 10.1007/s00259-020-04734-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zou S, Zhu X. FDG PET/CT of COVID-19. Radiology. 2020;200770. 10.1148/radiol.2020200770.
- 9.Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020;200642. 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed]
- 10.Xu Xi, Yu Chengcheng, Qu Jing, Zhang Lieguang, Jiang Songfeng, Huang Deyang, Chen Bihua, Zhang Zhiping, Guan Wanhua, Ling Zhoukun, Jiang Rui, Hu Tianli, Ding Yan, Lin Lin, Gan Qingxin, Luo Liangping, Tang Xiaoping, Liu Jinxin. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. European Journal of Nuclear Medicine and Molecular Imaging. 2020;47(5):1275–1280. doi: 10.1007/s00259-020-04735-9. [DOI] [PMC free article] [PubMed] [Google Scholar]