Abstract
COVID-19 is a novel coronavirus that was reported by the world health organization in late December 2019. As an unexplained respiratory disease epidemic, which is similar to respiratory syndrome coronavirus SARS-CoV, it rapidly spread all over the world. The study aims to compare several parameters of COVID-19 and SARS-CoV infectious diseases in terms of incidence, mortality, and recovery rates. The publicly available dataset Worldometer (extracted on April 5, 2020) confirmed by WHO report was available for meta-analysis purposes using the Meta-MUMS tool. And, the reported outcomes of the analysis used a random-effects model to evaluate the event rate, and risk ratios thorough subgroup analysis forest plots. Seventeen countries for COVID-19 and eight countries of SARS infections, including COVID-19 group n = 1124243, and SARS-CoV group n = 8346, were analyzed. In this meta-analysis, a random effect model of relations of incidence, mortality, and recovery rates of COVID-19 and SARS world infections were determined. The meta-analysis and forest plots of two viral world infections showed that the incidence rate of COVID-19 infection is more than SARS infections, while recovery and mortality event rates of SARS-CoV are more than COVID-19 infection. And subgroup analysis showed that the mortality and recovery rates were higher in both SARS-CoV wand COVID-19 in comparison to incidence and mortality rates, respectively. In conclusion, the meta-analysis approach on the abovementioned dataset revealed the epidemiological and statistical analyses for comparing COVID-19 and SARS-CoV outbreaks.
Key Words: COVID-19, SARS-CoV, Meta-analysis, Meta-MUMS, Epidemiology
Introduction
The world health organization (WHO) reported the severe acute respiratory syndrome coronavirus-2 known as COVID-19 in late December 2019 in China. As of April 5, 2020, based on the WHO report (i.e., https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports), the numbers of laboratory-confirmed cases and mortalities were 1133758? and 62784?, respectively. Moreover, the sequence similarity scores of COVID-19 with Bat SARS-like, SARS-CoV, and MERS-CoV were about 99, 96, and 50%, respectively (1).
Epidemiologically, the COVID-19 outbreak has spread to more than 200 countries resulting in WHO risk assessment status as “very high”. For this purpose, several authors have recently carried out their researches on COVID-19, which were mostly based on clinical and epidemiological views and included the potential symptoms, the ways of COVID-19 transmission, and epidemic issues (2). Among them, Hellewell et al. proposed a stochastic transmission model that resulted in the case and contact isolations to control the COVID-19 outbreak (3). Moreover, Peeri et al. compared the epidemics of three types of coronaviruses, namely SARS, MERS, and COVID-19. They concluded that there were no frequent outbreaks found from two previous ones, and the challenges for the COVID-19 should be covered by the applications of the Internet of Things (IoT), which will be beneficial for control the incidence among people (4). Two systematic reviews and meta-analysis studies were available in the literature. They proposed five useful factors (i.e., clinical, laboratory, imaging features, procalcitonin measurements, outcomes of confirmed cases) in predicting the severity of the COVID-19 disease (5, 6, 7).
In the current study, the comparisons between incidence and mortality, as well as recovery and death rates among the countries for COVID-19 and SARS-CoV with the higher incidence rates, were performed using the meta-analysis approach developed in the Meta-MUMS tool. The statistical analyses used both subgroup forest plots using event rate and risk ratio statistics.
Materials and Methods
Data Sources
Data for meta-analysis could be extracted from open datasets (8). The original and well-known data resources for COVID-19 were World Health Organization (WHO), i.e., https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports, and Worldometers, i.e., https://www.worldometers.info/coronavirus/. The retrieved parameters for the countries to be meta-analyzed were total sample size, cumulative confirmed cases, cumulative mortalities, and total recovered cases; And, the data for high-risk countries in terms of incidence related to COVID-19 was extracted up to April 5, 2020. Moreover, the summary table of SARS-CoV was available from https://www.who.int/csr/sars/country/country2003_08_15.pdf?ua=1 for the period November 16, 2002–August 7, 2003.
Statistical Analysis
The analysis environment was the Meta-MUMS tool as a comprehensive meta-analysis tool without any limitations in number size and data entry (9,10). Analysis of dichotomous data was done with a 95% confidence interval to set lower and upper limits based on risk ratio (RR) as well as event rate (ER) when no interventions are involved (11). In all calculations and analyses, the p-values less than 0.05 were statistically significant.
The evaluation of heterogeneity between the analyzed countries was by calculating the I2 test and Cochrane's Q test. And, whenever a significant heterogeneity was present, a random-effects model was used; otherwise, we utilize a fixed-effects model. Additionally, subgroup analysis was carried out among the target countries to compare the effect sizes of “incidence vs. mortality” and “recovery vs. mortality” using risk ratio. And, subgroup analysis was performed for comparing effect sizes of incidence, mortality, and recovery rates using event rate.
Results and Discussion
In the current meta-analysis, n = 1124243 patients of COVID-19 infection, and n = 8346 of SARS-CoV were available and retrieved from the initial research of WHO and Worldometer freely accessible databases. The “incidence vs. mortality” and “recovery vs. mortality” ratios are also determined. Indeed, subgroup analyses were also performed for evaluation of learning significant differences of ER and RR.
Event rates of incidence, recovery, and mortality of COVID-19, and SARS-CoV infections are as the following:
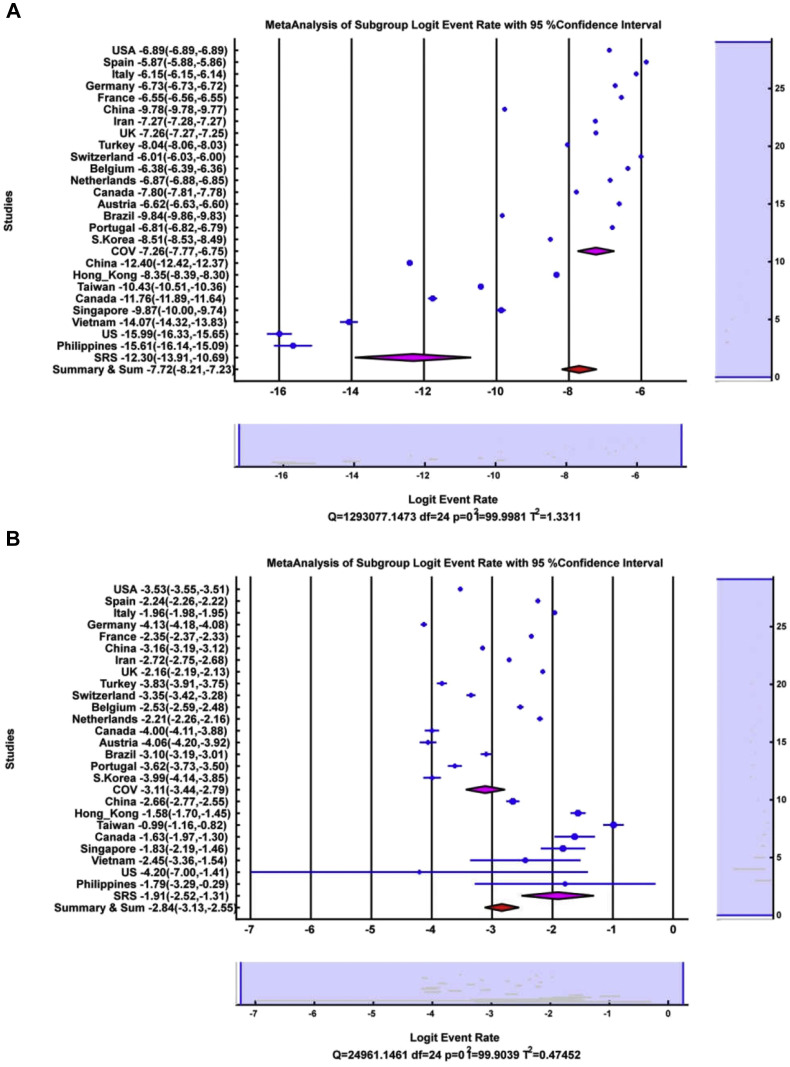
The incidence event rates of COVID-19 and SARS-CoV infections are as below, and the forest plots are illustrated in Figure 1 A, showing the relationships between two infectious diseases.
| Logit ER = −7.257, LL = −7.768, UL = −6.747, p <0.001 |
| Logit ER = −12.303, LL = −13.910, UL = −10.695, p <0.001 |
Figure 1.
(A) Forest plot for Logit event rate statistics of incidence of COVID-19 and SARS-CoV, (B) Forest plot for Logit event rate statistics of mortality of COVID-19 and SARS-CoV.
So, the incidence rate of COVID-19 is more than SARS-CoV (p <0.001) and the same outcomes apply to the cumulative incidence rates with (p <0.001).
The mortality event rates of COVID-19 and SARS-CoV infections are as follows, where the forest plots Figure 1B shows the relationships between two viral diseases.
| Logit ER = −3.113, LL = −3.439, UL = −2.786, p <0.001 |
| Logit ER = −1.914, LL = −2.515, UL = −1.312, p <0.001 |
The mortality rate of SARS-CoV infection is more than COVID-19 infection (p <0.001), by also considering their cumulative mortality rate with p <0.001.
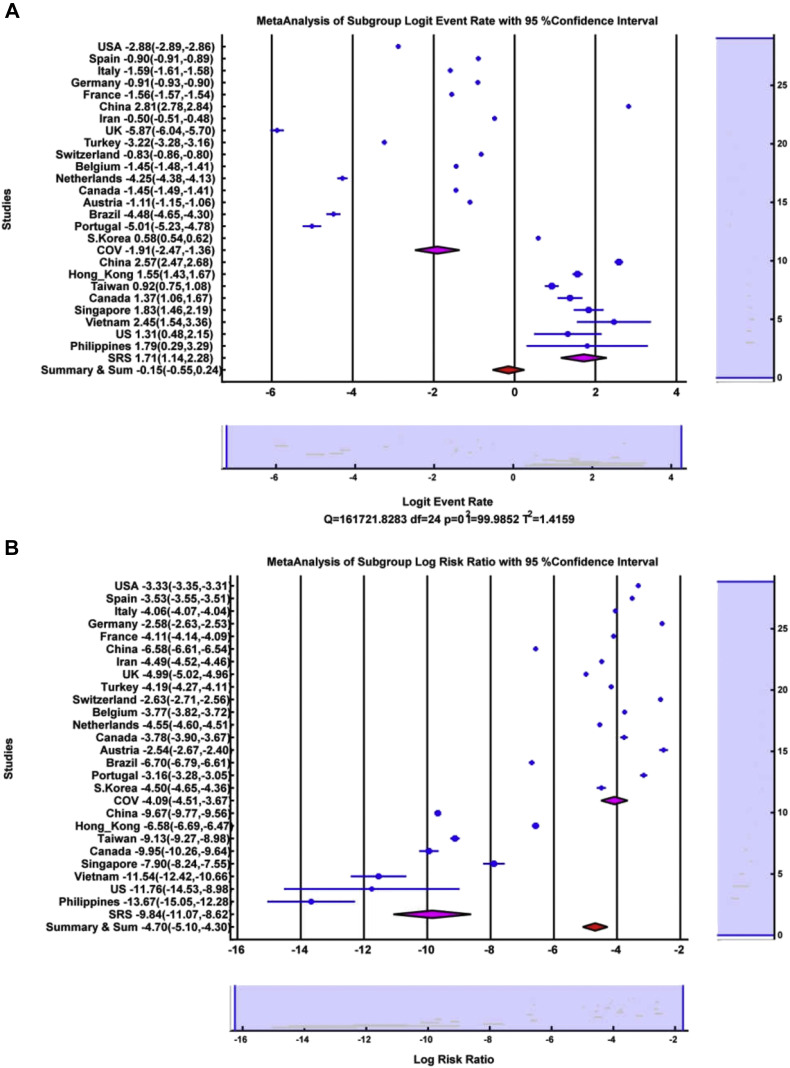
Recovery event rate of COVID-19 and SARS-CoV infections are as below, and the forest plots are illustrated in Figure 2 A, showing the relations between both diseases.
| Logit ER = −1.913, LL = −2.4675, UL = −1.359, p <0.001 |
| Logit ER = 1.706, LL = 1.137, UL = 2.276, p <0.001 |
Figure 2.
(A) Forest plot for Logit event rate statistics of recovery of COVID-19 and SARS-CoV, (B) Forest plot for Logit event rate statistics of incidence vs. mortality of COVID-19 and SARS-CoV.
So, the recovery rate of SARS-CoV infection is more than COVID-19 infection (p <0.001) with the same results using the cumulative recovery rate with p <0.001.
Incidence vs. mortality results of COVID-19 and SARS-CoV infections are as below. The forest plots illustrated in Figure 2B show the relations between the two diseases.
| Log RR = −4.089, LL = −4.512, UL = −3.666, p <0.001 |
| Log RR = −9.845, LL = −11.074, UL = −8.615, p <0.001 |
And, the mortality rate is higher than the incidence rate in both infection groups, and subgroup analysis showed that in SARS infection, the mortality rate is more than incidence rate in comparison to COVID-19 disease (p <0.001). Cumulative incidence vs. mortality rateof COVID-19 and SARS-CoV infections reflected the above results with p <0.001.
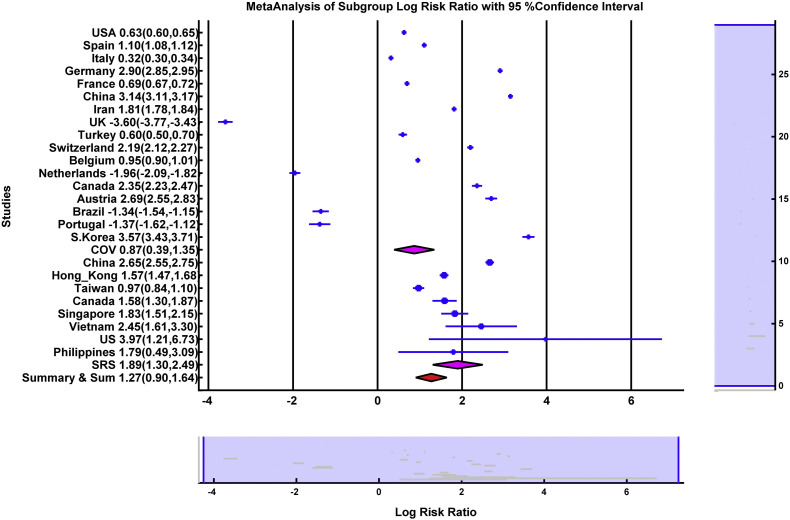
Recovery vs. mortality results of COVID-19 and SARS-CoV infections are as below. The forest plots are illustrated in Figure 3 , showing the relations between the two diseases.
| Log RR = 0.867, LL = 0.389, UL = 1.345, p <0.001 |
| Log RR = 1.895, LL = 1.300, UL = 2.489, p <0.001 |
Figure 3.
Forest plot for Logit event rate statistics of recovery vs. mortality of COVID-19 and SARS-CoV.
Which resulted, the recovery rate is more than the mortality rate in both infectious groups, And subgroup analysis has shown that in SARS infection, the recovery rate vs. mortality rate is higher than that of COVID-19 (p <0.008). And, cumulative recovery rate vs. mortality rate of COVID-19 and SARS-CoV infections reflected the above results with p <0.001.
Some recent news reported that the COVID-19 has more mortality rate than the combination of SARS and MERS (12). However, one should note that, while this comes to statistical analysis, the whole population of the world and countries are essential factors.
The rapid virus spread, known as also super spreading people, played a vital role in previous SARS-CoV (case fatality rate of 9.6%) and MERS (case fatality rate of about 38%) outbreaks, and also needs special attention in COVID-19 as well (13).
In summary, we demonstrated the statistical analyses of incidence, mortality, and recovery rates between COVID-19 and SARS-CoV, along with their subgroups analysis. And, hopefully, this would shed more evidence in controlling the new infectious disease.
The limitations of the current meta-analysis are as below:
-
•
The use of open datasets.
-
•
All data were observational numbers reported for incidence, mortality, and recovery values.
-
•
Only the countries with higher incidence values (those which are high-risk countries based on WHO criteria assessment) are involved in the current meta-analysis, which might be influenced by selection bias in the future.
-
•
Due to the nature of the meta-analysis, the evaluation of publication bias was not possible.
Conclusions
The current meta-analysis provided more information on incidence, mortality, and recovery rates between COVID-19 and SARS-CoV infectious diseases. Based on event rate evaluation, the incidence rate of COVID-19 was higher than SARS-CoV's where mortality and recovery rates for SARS-CoV were higher in comparison with COVID-19. On the other hand, the risk ratio and subgroup analysis of “incidence vs. mortality” and “recovery vs. mortality” for both COVID-19 and SARS-CoV revealed new findings. Those were the higher mortality and recovery rates of both SARS-CoV and COVID-19 in comparison to incidence and mortality rates, respectively.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Acknowledgments
The authors would like to thank the Research Council of Mashhad University of Medical Sciences, Mashhad, Iran and Nuclear Medicine Research Center of Mashhad University of Medical Sciences, Mashhad, Iran for providing facilities and support under PhD thesis No. 931507.
(ARCMED_2020_431)
Contributor Information
Ramin Sadeghi, Email: raminsadeghi1355@yahoo.com.
Babak Sokouti, Email: b.sokouti@gmail.com.
References
- 1.Kannan S., Shaik Syed Ali P., Sheeza A. COVID-19 (Novel Coronavirus 2019) - recent trends. Eur Rev Med Pharmacol Sci. 2020;24:2006–2611. doi: 10.26355/eurrev_202002_20378. [DOI] [PubMed] [Google Scholar]
- 2.Rothan H.A., Byrareddy S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020:102433. doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hellewell J., Abbott S., Gimma A. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob Health. 2020;8:e488–e496. doi: 10.1016/S2214-109X(20)30074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peeri N.C., Shrestha N., Rahman M.S. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned? Int J Epidemiol. 2020 doi: 10.1093/ije/dyaa033. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lippi G., Plebani M. Procalcitonin in patients with severe coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chim Acta. 2020;505:190–191. doi: 10.1016/j.cca.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lippi G., Plebani M., Michael Henry B. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clinica Chimica Acta. 2020;506:145–148. doi: 10.1016/j.cca.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodriguez-Morales A.J., Cardona-Ospina J.A., Gutiérrez-Ocampo E. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020:101623. doi: 10.1016/j.tmaid.2020.101623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Culina A., Crowther T.W., Ramakers J.J. How to do meta-analysis of open datasets. Nat Ecol Evol. 2018;2:1053–1056. doi: 10.1038/s41559-018-0579-2. [DOI] [PubMed] [Google Scholar]
- 9.Sokouti M., Sadeghi R., Pashazadeh S. Treating empyema thoracis using video-assisted thoracoscopic surgery and open decortication procedures: a systematic review and meta-analysis by meta-mums tool. Arch Med Sci. 2019;15:912–935. doi: 10.5114/aoms.2018.77723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sokouti M., Sadeghi R., Pashazadeh S. A systematic review and meta-analysis on the treatment of liver hydatid cyst using meta-MUMS tool: comparing PAIR and laparoscopic procedures. Arch Med Sci. 2019;15:284–308. doi: 10.5114/aoms.2018.73344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li H., Li J., Yu X. The incidence rate of cancer in patients with schizophrenia: a meta-analysis of cohort studies. Schizophr Res. 2018;195:519–528. doi: 10.1016/j.schres.2017.08.065. [DOI] [PubMed] [Google Scholar]
- 12.Mahase E. Coronavirus: covid-19 has killed more people than SARS and MERS combined, despite lower case fatality rate. Br Med J. 2020;368:m641. doi: 10.1136/bmj.m641. [DOI] [PubMed] [Google Scholar]
- 13.Wong G., Liu W., Liu Y. MERS, SARS, and Ebola: the role of super-spreaders in infectious disease. Cell Host Microbe. 2015;18:398–401. doi: 10.1016/j.chom.2015.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]