Highlights
-
•
POCUS can assist in the evaluation of suspected/confirmed COVID-19 infection.
-
•
A cardiopulmonary POCUS protocol is provided and implications discussed.
-
•
A device-cleaning check-list is provided.
Keywords: Point-of-care ultrasound, COVID-19, Lung ultrasound
Abbreviations: ASE, American Society of Echocardiography; COVID-19, Coronavirus disease 2019; POCUS, Point-of-care ultrasound; PPE, Personal protective equipment; SARS-CoV-2, Severe acute respiratory syndrome coronavirus-2; TTE, Transthoracic echocardiography
Why Conduct Point-of-Care Ultrasound in Coronavirus Disease 2019 Infection?
Although lung injury is common in coronavirus disease 2019 (COVID-19) infection, myocardial injury may be present in more than a quarter of patients with critical disease.1 Thus the rapid, bedside assessment of the heart, chest, and vessels using point-of-care ultrasound (POCUS) has propelled this tool to the front lines of the fight against the COVID-19 pandemic. POCUS is usually conducted by the treating provider to obtain real-time information for management decisions. Cardiac views are frequently obtained, along with noncardiac views such as the chest (lung, pleura) and vessels (neck and leg veins, aorta). In infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in particular, POCUS may help triage patients with dyspnea and determine need for subsequent imaging (echocardiography, computed tomography, etc.). A modified version of the American Society of Echocardiography (ASE) POCUS protocol may be of value in suspected or confirmed COVID-19 infection (Figure 1 ). The base ASE POCUS protocol can be accessed free online at https://aseuniversity.org/ase/lessons/47.2
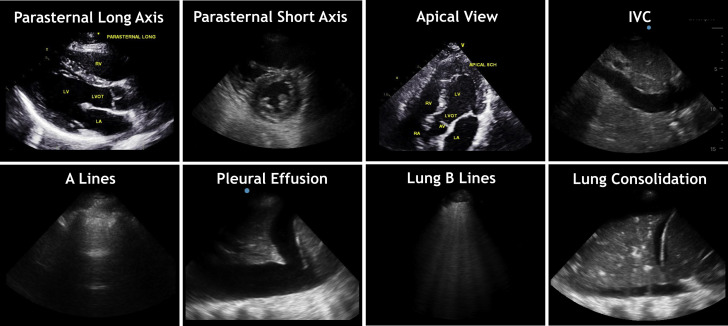
Figure 1.
ASE POCUS protocol imaging views in suspected or confirmed COVID-19. The ASE modified POCUS protocol includes basic cardiac views, subcostal views for inferior vena cava (IVC) and pericardial fluid, and chest views. This protocol may assist in the initial cardiopulmonary assessment of patients with COVID-19 if POCUS is deemed indicated.
Cardiac POCUS
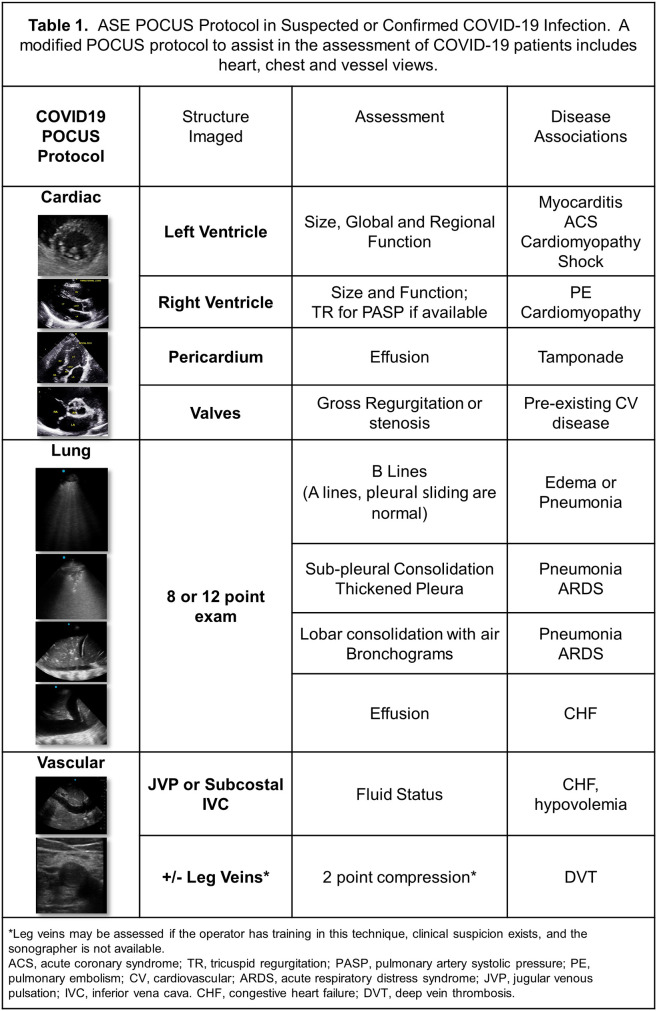
A well-illustrated case series of the application of focused ultrasound in patients with severe COVID-19 and associated cardiovascular disease from Wuhan, China, was recently presented.3 Figure 2 lists cardiac POCUS findings and indications. Early reports suggest that cardiac POCUS indications in COVID-19 include the following:
-
1.
Detection or characterization of preexisting cardiovascular disease.
-
2.
Early identification of worsening cardiac function, either due to known preexisting disease or associated with the infection.
-
3.
Monitoring and examination: POCUS may be able to assess changes in cardiac function over time through quick routine examinations, perhaps in lieu of heart and lung auscultation, which can be challenging in critical care settings because of pronation, ambient noise, and personal protective equipment (PPE).
-
4.Elucidation of cardiovascular abnormalities potentially associated with COVID-19:
-
a.Early reports suggest that some patients develop pericardial effusion and/or myocarditis that can progress to shock.4
-
b.A hypercoagulable state may be associated, leading to deep vein thrombosis and pulmonary embolism with associated right ventricular findings and acute pulmonary hypertension.
-
c.Left ventricular systolic dysfunction, either global or regional, may be associated with myocarditis, a stress-induced cardiomyopathy pattern, or epicardial or microvascular coronary thrombosis.
-
a.
Figure 2.
ASE POCUS protocol in suspected or confirmed COVID-19 infection: modified POCUS protocol to assist in the assessment of patients with COVID-19 includes heart, chest, and vessel views.
Lung POCUS
When radiographic studies such as computed tomography might be limited, lung POCUS can be used to trend the severity of COVID-19 pneumonia as an adjunct to oximetry and physical examination. Lung and vascular POCUS applications in COVID-19 are listed in Figure 2. Characteristic lung findings in preliminary publications are consistent with a viral pneumonia: a thickened and irregular pleural line and scattered B-lines (mild disease). In severe disease, this can progress to confluent B-lines with pulmonary consolidation, including air bronchograms. POCUS is useful to exclude other chest pathologies in critically ill patients, such as pneumothorax (particularly in patients on positive pressure ventilation) and symptomatic large pleural effusion.
Vascular POCUS for procedural guidance and access is well established in acute settings. Assessment of the inferior vena cava and/or jugular venous pulsation plays an important role in the hemodynamic assessment of critically ill patients to enhance the physical examination and in the assessment of fluid status. Deep vein thrombosis risk increases with any critically ill bedbound patient; moreover, early reports indicate an association between COVID-19 and a prothrombotic state. A unilateral deep vein thrombosis study performed by a sonographer is relatively quick and focused. However, in case a sonographer is not available, and in context of the pandemic, the two-point compression POCUS technique may be considered by practitioners trained in the technique.5
When to Perform POCUS in COVID-19?
Not all patients with COVID-19 require a POCUS examination. However, if cardiac and chest ultrasound is indicated, some institutions may choose POCUS as the first-line application of ultrasound. Deterioration in clinical status may then trigger a more extensive examination, such as a limited transthoracic echocardiography (TTE) guided by the POCUS images. The primary advantage of using POCUS first in a patient with COVID-19 is reduction of exposure to other personnel and locations, permitting conservation of PPE. Disadvantages include potentially poorer imaging resolution compared with systems used for comprehensive TTE, missed findings, operator inexperience, archiving issues, and inability to immediately convert the POCUS study to a comprehensive examination if needed.
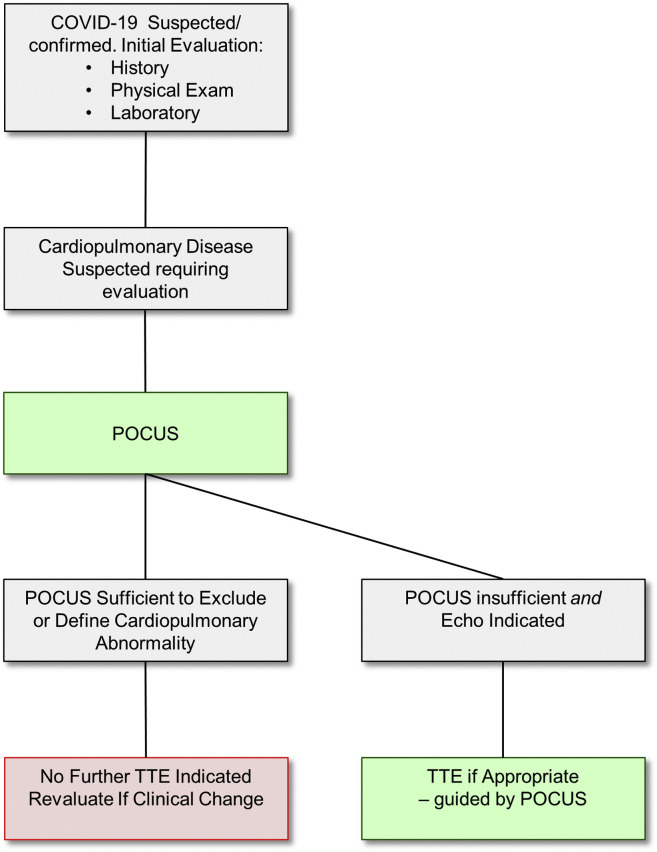
A work-flow algorithm for patients with COVID-19 in whom further cardiopulmonary ultrasound is indicated is provided in Figure 3 . If POCUS examination is available, and the scan sufficiently answers the clinical question, then the need for subsequent TTE may be obviated. If the POCUS scan is insufficient, or reveals findings requiring comprehensive evaluation, TTE may be considered appropriate. Limited TTE can be planned and guided by the POCUS findings to minimize sonographer exposure. In some instances, POCUS may be insufficient to exclude a suspected cardiac abnormality, for example, in the case of difficult image acquisition, and it may be more efficient for a skilled sonographer to rapidly scan the patient, rather than have a POCUS operator struggle with prolonged attempts. Judicious use of ultrasound must be considered to avoid unnecessary exposure of personnel to contagion and conserve the use of limited resources such as PPE. Caution must be exercised to ensure that the suggested POCUS work-flow algorithm is not increasing the utilization of unnecessary or inappropriate TTE.
Figure 3.
POCUS work flow in suspected or confirmed COVID-19. Potential work flow for POCUS during the COVID-19 pandemic, in the instance that cardiopulmonary ultrasound is indicated. If available, and there is suspicion of cardiopulmonary abnormality requiring further evaluation, POCUS can be the first-line ultrasound examination performed. If the POCUS performed by a trained operator is sufficient to either exclude or define the cardiopulmonary abnormality, further TTE may not be required. If the POCUS is insufficient, limited or comprehensive TTE may be considered as appropriate.
How to Perform POCUS in COVID-19?
Safety and Cleaning
PPE implementation for sonographers and machine cleaning principles are described in the parent document to this supplement and apply to POCUS. Because of the size and flexibility of POCUS devices, institutions may decide to dedicate these devices to a fixed location, such as an isolated COVID-19 unit, with meticulous cleaning between patient examinations and at the end of each day in a dedicated cleaning storage facility within the unit. The suggestions for scanning and cleaning are summarized in Table 1 (modified from the American College of Emergency Physicians).6 This is a suggested checklist, but specific steps, procedures, and their order may vary depending upon institutional guidance, the care environment, and the management pathway. It is important to recognize that institutions may develop their own protocols for decontamination and that these should be posted clearly. Additional information on transducer cleaning can be found on the American Institute of Ultrasound in Medicine website.7
Table 1.
Example POCUS device cleaning checklist in suspected or confirmed COVID-19
| 1 | Review PPE precautions Plan scans to minimize time and risk Remove excess items from machine before entering room Mask patient (institution specific) |
| 2 | After scan: inspect and wipe probe/device wearing PPE |
| 3 | Initial cleaning in patient's room |
| 4 | Push machine out of room while doffing gown Sanitize hands, new gloves, keep mask and face shield on |
| 5 | Reinspect machine and perform low-level disinfection cleaning with appropriate agent using product recommended wet time (usually 2 min), allow dry time Remove other PPE Remove gloves, sanitize hands again Record personnel, document scan |
| Other considerations | |
| 6 | Consider using aliquot or single-use gel packets |
| 7 | Consider probe/device covers (institution specific) |
| 8 | Consider dedicating machine to unit (institution specific) |
| 9 | Hold in-service for users, share knowledge |
| 10 | Periodically review institutional and society guidance |
Archiving and Storage
Given the potential for deterioration in patients with COVID-19, every attempt should be made to store, archive, and document POCUS results to allow image comparison. This helps reduce the need for repeat scans that would impinge upon scarce PPE resources and the risk for exposure. At the very least, results should be documented in the physical examination or investigations section of the patient's chart.
Who Should Perform POCUS?
All POCUS practitioners should operate within their skill sets as described by the ASE recommendations for echocardiography laboratories participating in POCUS and critical care echocardiography training.8 Some users may have POCUS credentials from societies such as the American College of Chest Physicians and/or the Society for Hospital Medicine. Many institutions have planned for the possibility of a tiered response to the crisis, as proposed by the Society of Critical Care Medicine.9 In such a response, nonintensivist physicians might be directly managing patients with COVID-19. Novice practitioners may be recruited to use POCUS in the midst of a surge of patients. These individuals should receive proper training, but the usual modes of teaching by practicing on patients are currently inadvisable. Simulators are an approach to introduce POCUS image acquisition and interpretation. Several online modules are available that offer an ability to learn background knowledge, such as the ASE modules2 and introductory lung modules available at PocusJournal.com.10 To enhance training and enable access to experts, commercially available platforms now exist that use interactive teleconsultative tools for remote guidance and supervision.
Summary
When cardiopulmonary ultrasound is indicated in a patient with COVID-19, POCUS may be considered the first-line ultrasound examination performed, which then guides the need for further imaging. This approach may help conserve personnel and PPE, as well as limit exposure to other personnel and locations. Given the potential for rapid clinical deterioration in patients with COVID-19, every attempt should be made to store and document POCUS results to reduce the need for repeat examination. Meticulous cleaning of any POCUS device is critical to reduce the risk for SARS-CoV-2 transmission. POCUS must be performed by individuals with the correct skill set, an understanding of the limitations of this technology, and meticulous attention to PPE and machine cleaning.
Footnotes
Notice and Disclaimer: This statement reflects recommendations based on expert opinion, national guidelines, and available evidence. Our knowledge with regard to COVID-19 continues to evolve, as do our institutional protocols for dealing with invasive and noninvasive procedures and practice of personal protective equipment. Readers are urged to follow national guidelines and their institutional recommendations regarding best practices to protect their patients and themselves. These reports are made available by the American Society of Echocardiography (ASE) as a courtesy reference source for its members. The reports contain recommendations only and should not be used as the sole basis to make medical practice decisions or for disciplinary action against any employee. The statements and recommendations contained in these reports are primarily based on the opinions of experts, rather than on scientifically verified data. ASE makes no express or implied warranties regarding the completeness or accuracy of the information in these reports, including the warranty of merchantability or fitness for a particular purpose. In no event shall ASE be liable to you, your patients, or any other third parties for any decision made or action taken by you or such other parties in reliance on this information. Nor does your use of this information constitute the offering of medical advice by ASE or create any physician-patient relationship between ASE and your patients or anyone else.
Dr. Mulvagh is a consultant for Lantheus Medical Imaging and serves on the steering committee of the SOUL trial for NovoNordisk.
References
- 1.Clerkin K.J., Fried J.A., Raikhelkar J., Sayer G., Griffin J.M., Masoumi A. Coronavirus disease 2019 (COVID-19) and cardiovascular disease. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.120.046941 Circulation. Available at: [DOI] [PubMed]
- 2.American Society of Echocardiography Cardiovascular point-of-care imaging for the medical student and novice user. https://aseuniversity.org/ase/lessons/47 Available at:
- 3.Zhang L., Wang B., Zhou J., Kirkpatrick J., Xie M., Johri A.M. Bedside focused cardiac ultrasound in COVID-19 from the Wuhan epicenter: the role of cardiac point-of-care ultrasound, limited transthoracic echocardiography, and critical care echocardiography. J Am Soc Echocardiogr. 2020;33:676–682. doi: 10.1016/j.echo.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Driggin E., Madhavan M.V., Bikdeli B., Chuich T., Laracy J., Bondi-Zoccai G. Cardiovascular considerations for patients, health care workers, and health systems during the coronavirus disease 2019 (COVID-19) pandemic. http://www.onlinejacc.org/content/early/2020/03/18/j.jacc.2020.03.031 J Am Coll Cardiol. Available at: [DOI] [PMC free article] [PubMed]
- 5.Lee J.H., Lee S.H., Yun S.J. Comparison of 2-point and 3-point point-of-care ultrasound techniques for deep vein thrombosis at the emergency department: a meta-analysis. Medicine (Baltimore) 2019;98:e15791. doi: 10.1097/MD.0000000000015791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American College of Emergency Physicians Ultrasound machine cleaning process for COVID-19. http://www.acep.org/globalassets/images/acep-us-machine-cleaning-covid-19.pdf Available at:
- 7.American Institute of Ultrasound in Medicine Guidelines for cleaning and preparing external- and internal-use ultrasound transducers and equipment between patients as well as safe handling and use of ultrasound coupling gel. http://www.aium.org/officialStatements/57 Available at: [DOI] [PubMed]
- 8.Kirkpatrick J.N., Grimm R., Johri A.M., Kimura B.J., Kort S., Labovitz A.J. Recommendations for echocardiography laboratories participating in cardiac point of care cardiac ultrasound (POCUS) and critical care echocardiography training: report from the American Society of Echocardiography. J Am Soc Echocardiogr. 2020;33:409–422.e4. doi: 10.1016/j.echo.2020.01.008. [DOI] [PubMed] [Google Scholar]
- 9.Society of Critical Care Medicine United States resource availability for COVID-19. http://sccm.org/Blog/March-2020/United-States-Resource-Availability-for-COVID-19?_zs=jxpjd1&_zl=w9pb6 Available at:
- 10.Wu L., Nihal S., Montague S., Johri A. Introduction to lung POCUS. http://pocusjournal.com/education/introduction-to-lung-pocus POCUS Journal. Available at: