Abstract
Neuroblastoma is a clinically heterogenous pediatric cancer of the sympathetic nervous system that originates from neural crest cells. It is the most common extracranial solid tumor in childhood and prognosis ranges from spontaneous tumor regression to aggressive disease resistant to multimodal therapy. Prognosis depends on patient characteristics and tumor biology that determine risk classification. Advancements in therapy reductions are merited for low- and intermediate-risk neuroblastoma patients, who generally have excellent outcomes. Of the patients with high-risk disease, only 50% achieve long-term survival, and therapeutic advancements are needed. Over the past several decades, genomic features such as germline mutations, somatic genetic aberrations, chromosome copy number, transcriptomics, and epigenetics have proven to contribute to the pathogenesis of neuroblastoma. The primary predisposition genes in familial neuroblastoma are ALK and PHOX2B. Sporadic neuroblastoma arises with complex pathogenesis, but chromosomal abnormalities and single-nucleotide polymorphisms have been identified to cooperatively lead to oncogenesis. These advances have led to new therapeutic approaches with the potential to improve outcomes for children with neuroblastoma.
Keywords: Neuroblastoma, oncology, pediatrics
Identity
ICD-TOPO: C710-C714,C717-C719,C720-C725,C716,C700-C701,C709,C728-C729 Brain, & cranial nerves, & spinal cord, (Excl. ventricle, cerebellum)/cerebellum
ICD-MORPHO: 9500/3 Neuroblastoma, NOS, 9490/3 Ganglioneuroblastoma
ATLAS_ID: 5002
PHYLUM: Central Nervous system::Neuroblastoma
WHO/OMS CLASSIFICATION: Central Nervous system
OTHER NAMES: Neuroblastoma
Classification
NOTE: Peripheral neuroblastic tumors; are derived from developing neuronal cells of the sympathetic nervous system and are found mostly (but not exclusively) in infants and young children. In the text below, we will stick to the well-known term neuroblastoma instead of using the more precise but less common term peripheral neuroblastic tumors.
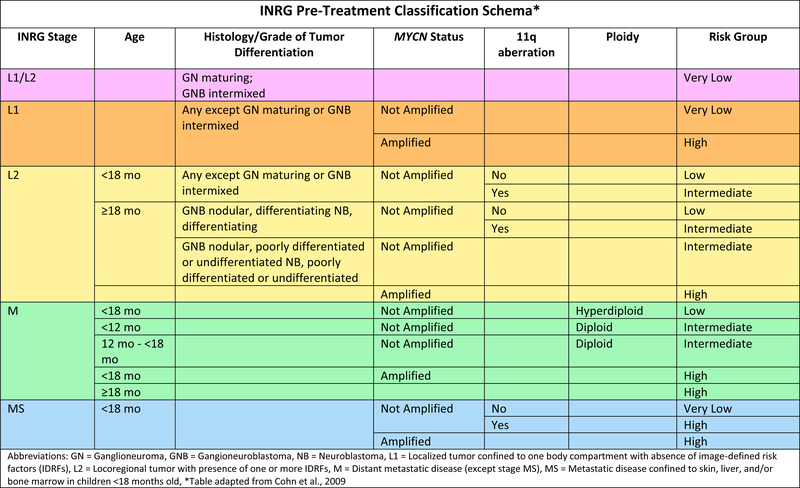
Neuroblastoma risk stratification utilizes age, stage, histology, MYCN gene amplification status, tumor cell ploidy, and segmental chromosomal abnormalities (Cohn et al., 2009). The International Neuroblastoma Risk Group (INRG) classification system stratifies patients into low-, intermediate-, and high-risk groups. Low- and intermediate-risk patients have excellent outcomes and current clinical trials aim to reduce therapy-related toxicities. High-risk neuroblastoma survival remains poor, necessitating new and improved treatment (Pinto et al., 2015).
Clinics and pathology
DISEASE
Localization: Adrenal medulla (50%) and para- and pre-vertebral sympathetic ganglia and paraganglia: cervical (5%), thoracic (15%), retroperitoneal (25%), and pelvic (5%).
Metastatic disease: In 50% of patients, metastatic tumor spread is found at diagnosis. Common sites of metastases are: bone marrow, bones, lymph nodes, liver, and skin. A unique pattern of metastatic spread is found in low-risk infants with favorable prognosis (stage MS).
Clinical Symptoms: The presenting clinical symptoms depend on the primary tumor location as well as the regional and metastatic dissemination. An abdominal tumor can be associated with discomfort, pain, digestive problems, and/or a palpable mass. Thoracic tumors are either found coincidentally or may cause respiratory distress, dysphagia, and circulatory problems. Cervical neuroblastomas can cause damage to the cervical ganglion, leading to Horner’s syndrome. Dumbbell tumors affecting the spinal cord and nerve roots can cause radicular pain, paraplegia, and dysfunction of bladder or bowel. Metastatic disease to the bone marrow or bleeding into a large primary tumor can cause anemia and thrombocytopenia. Bone metastases can cause pain, leading to limping or refusal to bear weight. Periorbital bone lesions may cause proptosis and bruising (“raccoon eyes”). Liver infiltration can lead to coagulopathy and jaundice. Systemic symptoms such as fever and weight loss may be present. Release of catecholamines by neuroblastoma tumors can cause tachycardia, hypertension, and flushing. Paraneoplastic presentations occur in a small percent of neuroblastoma patients, including opsoclonus myoclonus syndrome (OMS) and diarrhea caused by the secretion of vasoactive intestinal peptide (VIP). Symptoms of OMS include fast, uncontrolled, horizontal and vertical eye movements, as well as involuntary muscle twitching, occasionally with ataxia.
Differential diagnosis: The differential diagnosis varies based on tumor location and clinical presentation. For those with abdominal tumors, Wilms tumor and hepatoblastoma can be considered. Other thoracic tumors such as lymphoma and germ cell tumors will generally present in the anterior mediastinum whereas neuroblastoma will present in the posterior mediastinum along the sympathetic ganglia. Neuroblastoma metastatic to the bone should be differentiated from osteosarcoma, Ewing sarcoma, and chondrosarcoma. Bone marrow involvement should be distinguished from leukemia or lymphoma. OMS can occur with other conditions such as hepatoblastoma, infection, toxin exposures, and metabolic derangements.
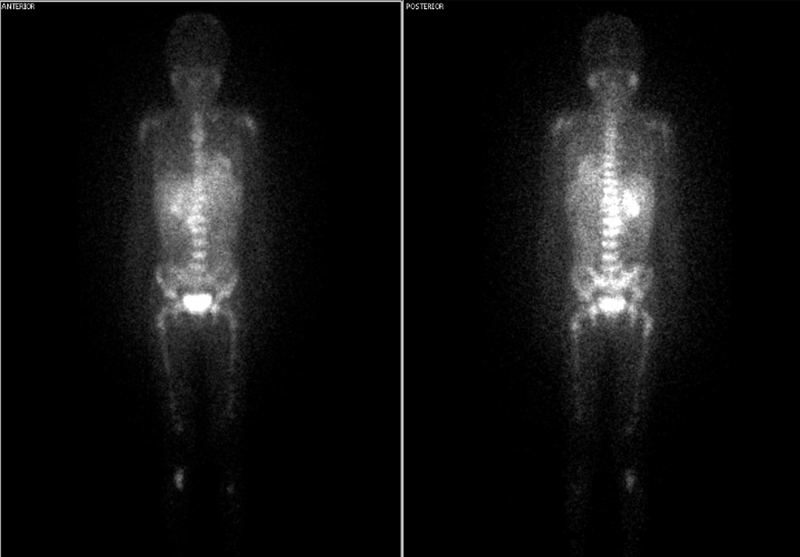
Diagnosis: All patients being evaluated for neuroblastoma should have a history and physical exam. Routine blood tests include blood counts, chemistries, and a hepatic panel. Measurement of the urinary catecholamine metabolites vanillylmandelic acid (VMA) and homovanillic acid (HVA) can help confirm a diagnosis. Confirmation of disease requires biopsy (of either primary tumor or bone marrow) and histologic evaluation. For tumor staging, CT or MRI of the primary tumor and nodal sites of metastatic disease is indicated. Patients should undergo I123 meta-iodobenzylguanidine (MIBG) scintigraphy (Figure 1) or PET if MIBG non-avid to evaluate for metastatic bone disease, as well as bilateral bone marrow aspirates and biopsies to determine involvement of that site.
Figure 1:
I123 meta-iodobenzylguanidine MIBG scan (Figure 1) of newly diagnosed patient with neuroblastoma. Bright white areas indicate area of neuroblastoma primary in the right adrenal gland with numerous bone and bone marrow metastases.
EMBRYONIC ORIGIN:
Neural crest cells of the sympathetic lineage (sympathetic neuronal precursor cells).
ETIOLOGY:
Most neuroblastomas occur sporadically, with only 1–2% occurring in families in an autosomal dominant pattern (Matthay et al., 2016).
EPIDEMIOLOGY:
Neuroblastoma is the most frequently diagnosed tumor in infancy and the most common cancer diagnosed within the first year of life. These tumors account for 7–10% of all childhood cancers. The incidence, which is almost uniform in industrialized countries, is 5–10 per million children per year. The median age at diagnosis is approximately 17 months. 50% of patients are diagnosed by the age of 2, and 90% of patients are diagnosed before 6 years of age.
PATHOLOGY:
The International Neuroblastoma Pathology Classification (INPC - Shimada system) groups neuroblastic tumors into four histopathologic categories according to the degree of cellular differentiation into ganglionic cells, ‘organoid’ maturation with the development of a Schwann cell stroma, and co-existence of clones of different maturity or of distinct aggressiveness:
-
–
Neuroblastoma (Schwannian stroma-poor)
-
–
Ganglioneuroblastoma, intermixed (Schwannian stroma-rich)
-
–
Ganglioneuroma (Schwannian stroma-dominant), maturing subtype OR Ganglioneuroblastoma, well differentiated (Schwannian stroma-rich)
-
–
Ganglioneuroblastoma, nodular (composite)
Two of these categories are further divided into subgroups according to cellular differentiation signs, i.e. Neuroblastoma into: undifferentiated, poorly differentiated and differentiating; and Ganglioneuroblastoma into maturing and mature. The degree of differentiation and stromal component of tumors can be used for prognostic assessment. Additionally, the age of the patient at diagnosis (below 1.5, between 1.5 and 5 years or over 5 years) is included as well as the number of mitotic and karyorrhectic (apoptotic) cells in the category of Neuroblastoma and the nodular part of Ganglioneuroma nodular.
Favorable features include:
Poorly differentiated or differentiating neuroblastoma, low or intermediate mitosis-karyorrhexis index (MKI), and age ≤ 1.5 years
Differentiating neuroblastoma, low MKI, and age 1.5 to 5 years
Ganglioneuroblastoma, intermixed
Ganglioneuroma
Unfavorable features include:
Undifferentiated tumor or high MKI tumor
Poorly differentiated tumor or intermediate MKI tumor in patients age 1.5 to 5 years
Patients ≥ 5 years with any grade of differentiation or MKI class
Nodular ganglioneuroblastoma
Prognostic Factors:
As neuroblastoma is a heterogeneous disease, risk stratification according to clinical features of the patient and biologic features of the tumor has allowed for an accurate assessment of prognosis and risk-adapted therapy. To facilitate clinical research and improve the outcome of children with neuroblastoma, investigators from the major cooperative groups developed a consensus pre-treatment International Neuroblastoma Risk Group (INRG) classification system. The task force collected data on 36 prognostic variables on 8,800 children enrolled on cooperative group studies and identified the seven factors that were highly statistically significant and also considered clinically relevant (Figure 2, Cohn et al., 2009).
Figure 2:
INRG Pre-Treatment Classification Schema (adapted from Cohn et al., 2009)
- Tumor Stage:
-
○Stage L1: Locoregional tumor not involving vital structures as defined by the image-defined risk factors (IDRF) and confined to one body part
-
○Stage L2: Locoregional tumor with presence of one or more IDRF
-
○Stage M: Distant metastatic disease (except Stage MS)
-
○Stage MS: Metastatic disease confined to skin, liver, and/or bone marrow
-
○
Age at diagnosis – Age <18 months at diagnosis is favorable
Pathologic risk classification – Categorized into favorable and unfavorable based on cell differentiation, schwannian cell content in stroma, MKI, and age at diagnosis
Cytogenetics and molecular genetics – Cytogenetic and molecular characteristics known to correlate with poor prognosis include MYCN amplification, ploidy, and 11q aberration
OTHER FEATURES:
Somatic Genomic Variations:
Multiple somatically acquired genomic alterations that contribute to tumorigenesis and progression of disease have been described. Somatic changes in the tumor genome such as gene mutations, loss or gain of alleles, and variations in ploidy have been identified as important factors in the development of neuroblastoma and contribute to its diverse phenotype.
TREATMENT:
Patients with low-risk neuroblastoma are often managed with surgical resection or, as is being evaluated in an ongoing clinical trial (NCT01728155), observation alone. Intermediate-risk patients are treated with chemotherapy (number of cycles is dependent on prognostic markers) and surgical resection of the primary tumor (Twist et al., 2019). Low- and intermediate-risk neuroblastomas have excellent outcomes and clinical trials aim to reduce therapy-related toxicities (Pinto et al., 2015). High-risk standard-of-care treatment consists of three treatment blocks. The first block, induction, includes high-dose chemotherapy and resection of the primary tumor. The second block is consolidation, which consists of tandem courses of myeloablative dose chemotherapy with autologous stem-cell rescue and external-beam radiotherapy (Park et al., 2019). Lastly, post-consolidation therapy includes anti–ganglioside 2 (GD2) immunotherapy with cytokines and cis-retinoic acid (Yu et al., 2010). Current clinical trials are evaluating the addition of MIBG therapy to induction (NCT01175356), anti–GD2 to induction chemotherapy (NCT01857934), or removing IL2 from immunotherapy and altering chemotherapy regimens (NCT01704716). Refractory and relapsed neuroblastoma is common in high-risk patients, indicating the need for further research on acquired drug and/or clonal resistance. While many patients can be salvaged with combination chemotherapy and anti-GD2 antibody (Mody et al., 2017), the long-term outcomes of relapsed neuroblastoma remain dismal.
Neuroblastoma mass screening:
Neuroblastoma mass screening was attempted in order to identify patients in a preclinical stage with the intention to decrease mortality. The results obtained by these efforts indicated that while the incidence of low-risk neuroblastoma increased dramatically, there was no decrease in the incidence or mortality of high-risk disease, suggesting that screening was ineffective and that low-risk and high-risk neuroblastoma are two biologically independent entities.
EVOLUTION:
Special features:
As demonstrated by mass screening efforts, neuroblastoma tumors range from indolent masses that may never be detected to rapidly growing and aggressive tumors. Spontaneous regression (without cytotoxic treatment) can be observed in neuroblastoma diagnosis within the first 18 months of life, even with metastatic disease. These tumor cells are characterized by distinct genomics. Spontaneous maturation of neuroblastoma into ganglioneuroblastoma and ganglioneuroma can be observed. These neuroblastic/ ganglionic cells share genetic characteristics with spontaneously regressing neuroblastomas. Moreover, such tumor cells are capable of recruiting non-neoplastic Schwann cells from the tumor adjacent tissue.
Genetics
NOTE:
Heredity:
Most cases of neuroblastoma develop sporadically, but familial neuroblastoma accounts for 1–2% of all cases (Matthay et al., 2016). Familial neuroblastoma presents at a younger age, and there is often a family history of the same tumor. Its inheritance pattern is most often autosomal dominant with incomplete penetrance.
PHOX2B: Loss-of-function mutations in paired-like homeobox 2B (PHOX2B) were the first discovered neuroblastoma predisposition genes. PHOX2B mutations are responsible for of 6–10% of familial neuroblastoma cases. These mutations also occur in approximately 2% of sporadic neuroblastoma cases (Trochet et al., 2004).
ALK: In 2008, the anaplastic lymphoma kinase gene (ALK) was identified as the major familial neuroblastoma predisposition gene (Mosse et al., 2008). Three missense mutations in in ALK (R1192P, R1275Q, G1128A) were found to be present in most familial neuroblastoma cases identified. ALK mutations are also present in 10–12% of cases of sporadic neuroblastoma.
KIF1Bβ: KIF1Bβ is a tumor suppressor gene that is likely involved in the development of neural crest tumors. Germline mutations in KIF1Bβ have been found in patients who have developed neuronal tumors, including neuroblastoma and pheochromocytoma (Schlisio et al., 2008; Barr et al., 2018).
Other cancer predisposition syndromes: While the mutations in PHOX2B, ALK, and KIF1Bβ are specific for predisposition to developing neuroblastoma, there are several syndromes that can lead to the development of neuroblastoma including RAS pathway mutations (Costello syndrome, Noonan syndrome, neurofibromatosis type 1, and congenital central hypoventilation syndrome), Li-Fraumeni syndrome, ROHHAD, Beckwith-Wiedemann syndrome, Weaver syndrome, and Familial Paraganglioma/Pheochromocytoma.
Sporadic (Nonfamilial) Neuroblastoma:
Sporadic neuroblastoma is recognized to be a complex genetic disease. Large genome-wide association studies (GWAS) have identified common single nucleotide polymorphisms that influence neuroblastoma susceptibility and phenotype.
BARD1 contains one of the most replicated signals. It has generally been thought of as a tumor suppressor, but in neuroblastoma, risk alleles are associated with increased expression of BARD1β, which promotes growth (Capasso et al., 2009).
LMO1 is a neuroblastoma oncogene and polymorphisms in the gene are associated with the development of high risk, clinically aggressive disease (Wang et al., 2011).
LIN28B polymorphisms are strongly correlated to with predisposition to high-risk neuroblastoma. Variants in HACE1, TP53 have also been identified (Diskin et al., 2012).
Variants in DUSP12 (1q23), HSD17B12 (11p11), DDX4/IL31RA (5q11.2) are associated with low-risk neuroblastoma (Nguyen et al., 2011).
Variants in CASC15, NBAT1 (6p22) influence susceptibility to high-risk neuroblastoma (Russell et al., 2015).
Polymorphisms in KIF15 are associated with the development of MYCN amplified neuroblastoma (Hungate et al., 2017) and those in MMP20 are associated with somatic 11q deletion (Chang et al., 2017).
Cytogenetics
NOTE:
Whole chromosome involvement: Ploidy (DNA index) is a significant prognostic marker of patient outcome, and it is a component of the INRG classification system. Hyperdiploid tumors (DNA index > 1) occur in about 66% of patients with neuroblastoma and are associated with lower risk disease and favorable outcomes (Look et al., 1991).
Segmental chromosomal aberrations: Tumors with segmental and subsegmental chromosomal aberrations have been found to be associated with high-risk disease. Additionally, new segmental aberrations have often been found at time of relapse. The most common alterations are gain of chromosomes 2p, which is the location of the MYCN oncogene; 17q gain; 1p loss of heterozygosity (LOH); and 11q loss (Bown 2001; Schleiermacher et al., 2012). 1p LOH is found primarily in MYCN amplified tumors whereas loss of 11q is correlated with non-MYCN amplified high-risk disease (Maris et al., 2000; Depuydt et al., 2018).
MYCN: The MYCN oncogene on chromosome 2p24 encodes a transcription factor that is known to cause malignant transformation. Amplification of the MYCN gene is noted in 20% of all primary neuroblastoma tumors. It is present in 50% of all high-risk tumors, and it is associated with aggressive disease and poor prognosis (Brodeur et al., 1984). MYCN amplification is used as a biomarker for risk stratification in the INRG classification system (Cohn et al., 2009).
17q gain: The gain of the distal portion of chromosome 17q is the most common copy number aberration in neuroblastoma. It is present in 50% of primary neuroblastomas, primarily those that are otherwise classified as high-risk (Bown et al., 1999).
1p LOH: LOH at chromosome 1p36 correlates with MYCN-amplification, metastatic disease, and older age. It is present in 23–35% of primary neuroblastoma tumors (Maris et al., 2000).
11q Loss occurs in about 33% of neuroblastomas, primarily non-MYCN-amplified, high-risk tumors. Despite significant research efforts, no confirmed driver tumor suppressors have been identified on 1p or 11q (Attiyeh et al., 2005).
Genes involved and proteins
NOTE:
Somatic Mutations
ALK: Genetic missense alterations (most commonly at R1275, F1174, and F1245) or gene amplification events within anaplastic lymphoma kinase (ALK) can occur. It is the gene that is most commonly mutated in neuroblastoma and inhibition of ALK signaling with crizotinib or newer generation ALK inhibitors are being tested in late phase trials (Bresler et al., 2014).
ATRX: Loss-of-function mutations or deletions in the RNA helicase alpha-thalassemia/mental retardation syndrome X-linked (ATRX) have been observed in neuroblastoma (10% of cases) and are often found in older patients (age at diagnosis >5). ATRX plays a role in chromatin remodeling, nucleosome assembly, and telomere maintenance. ATRX mutations are mutually exclusive with MYCN-amplification and TERT mutations (Pugh et al., 2013).
TERT: Genomic rearrangements in telomerase reverse transcriptase (TERT), a target of MYCN, can lead to neuroblastoma. It has been proposed that all neuroblastomas need a pathway to activate TERT or bypass the pathway via ATRX mutation (Valentijn et al., 2015).
GENE NAME : ALK (Anaplastic Lymphoma Kinase)
LOCATION : 2p23.1
NOTE: The major cause of familial neuroblastoma is heritable gain-of-function mutations of ALK. ALK mutations are also present in 10–12% of cases of sporadic neuroblastoma. It is the gene that is most commonly mutated in neuroblastoma and inhibition of ALK signaling with crizotinib or newer generation ALK inhibitors are being tested in late phase trials.
PROTEIN DESCRIPTION : Cell surface receptor tyrosine kinase
GERMINAL MUTATIONS : Three missense mutations in in ALK ( R1192P, R1275Q, G1128A) were found to be present in most familial neuroblastoma cases
SOMATIC MUTATIONS: Genetic missense alterations (most commonly at R1275, F1174, and F1245) or gene amplification events
GENE NAME : MYCN (v-myc myelocytomatosis viral related oncogene, neuroblastoma derived (avian))
LOCATION : 2p24.3
NOTE : Amplification of the MYCN gene is noted in 20% of all primary neuroblastoma tumors. It is present in 50% of all high-risk tumors, and it is associated with aggressive disease and poor prognosis (Brodeur et al., 1984). MYCN amplification is used as a biomarker for risk stratification in the INRG classification system.
PROTEIN DESCRIPTION : Nuclear protein; helix-loop-helix and a leucine zipper domain; transcription factor
SOMATIC MUTATION: Copy Number Variation Amplification
GENE NAME : ATRX (alpha-thalassemia/mental retardation syndrome X-linked)
LOCATION : Xq21.1
NOTE : Loss-of-function mutations or deletions in ATRX have been observed in neuroblastoma (10% of cases) and are often found in older patients (age at diagnosis >5 years). ATRX plays a role in chromatin remodeling, nucleosome assembly, and telomere maintenance. ATRX mutations are mutually exclusive with MYCN-amplification and TERT mutations.
PROTEIN DESCRIPTION : RNA helicase
SOMATIC MUTATIONS: Loss of function alterations (mutations, multi-exon deletions)
GENE NAME : TERT (telomerase reverse transcriptase)
LOCATION : 5p15.33
NOTE : Genomic rearrangements in TERT, a target of MYCN, can lead to neuroblastoma. It has been proposed that all neuroblastomas need a pathway to activate TERT or bypass the pathway via ATRX mutation.
PROTEIN DESCRIPTION : Subunit of the enzyme telomerase
SOMATIC MUTATIONS: Rearrangements and copy number mutations
Acknowledgments
This research was supported in part by the NIH Grant K08CA226237 (MAA). The contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
References
- Attiyeh EF, London WB, Mosse YP, et al. “Chromosome 1p and 11q deletions and outcome in neuroblastoma.” N Engl J Med 2005; 353(21): 2243–53. PMID [DOI] [PubMed] [Google Scholar]
- Barr EK and Applebaum MA. “Genetic Predisposition to Neuroblastoma.” Children (Basel) 2018; 5(9). PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bown N “Neuroblastoma tumour genetics: clinical and biological aspects.” J Clin Pathol 2001; 54(12): 897–910. PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bown N, Cotterill S, Lastowska M, et al. “Gain of chromosome arm 17q and adverse outcome in patients with neuroblastoma.” N Engl J Med 1999; 340(25): 1954–61. PMID [DOI] [PubMed] [Google Scholar]
- Bresler SC, Weiser DA, Huwe PJ, et al. “ALK mutations confer differential oncogenic activation and sensitivity to ALK inhibition therapy in neuroblastoma.” Cancer cell 2014; 26(5): 682–94. PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodeur GM, Seeger RC, Schwab M, et al. “Amplification of N-myc in untreated human neuroblastomas correlates with advanced disease stage.” Science 1984; 224(4653): 1121–4. PMID [DOI] [PubMed] [Google Scholar]
- Capasso M, Devoto M, Hou C, et al. “Common variations in BARD1 influence susceptibility to high-risk neuroblastoma.” Nat Genet 2009; 41(6): 718–23. PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang X, Zhao Y, Hou C, et al. “Common variants in MMP20 at 11q22.2 predispose to 11q deletion and neuroblastoma risk.” Nat Commun 2017; 8(1): 569. PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohn SL, Pearson AD, London WB, et al. “The International Neuroblastoma Risk Group (INRG) classification system: an INRG Task Force report.” J Clin Oncol 2009; 27(2): 289–97. PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohn SL, Pearson AD, London WB, et al. “The International Neuroblastoma Risk Group (INRG) classification system: an INRG Task Force report.” J Clin Oncol 2009; 27(2): 289–97. PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depuydt P, Boeva V, Hocking TD, et al. “Genomic Amplifications and Distal 6q Loss: Novel Markers for Poor Survival in High-risk Neuroblastoma Patients.” J Natl Cancer Inst 2018. PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diskin SJ, Capasso M, Schnepp RW, et al. “Common variation at 6q16 within HACE1 and LIN28B influences susceptibility to neuroblastoma.” Nat Genet 2012; 44(10): 1126–30. PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hungate EA, Applebaum MA, Skol AD, et al. “Evaluation of Genetic Predisposition for MYCN-Amplified Neuroblastoma.” J Natl Cancer Inst 2017; 109(10). PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Look AT, Hayes FA, Shuster JJ, et al. “Clinical relevance of tumor cell ploidy and N-myc gene amplification in childhood neuroblastoma: a Pediatric Oncology Group study.” J Clin Oncol 1991; 9(4): 581–91. PMID [DOI] [PubMed] [Google Scholar]
- Maris JM, Weiss MJ, Guo C, et al. “Loss of heterozygosity at 1p36 independently predicts for disease progression but not decreased overall survival probability in neuroblastoma patients: a Children’s Cancer Group study.” J Clin Oncol 2000; 18(9): 1888–99. PMID [DOI] [PubMed] [Google Scholar]
- Matthay KK, Maris JM, Schleiermacher G, et al. “Neuroblastoma.” Nat Rev Dis Primers 2016; 2: 16078. PMID [DOI] [PubMed] [Google Scholar]
- Mody R, Naranjo A, Van Ryn C, et al. “Irinotecan-temozolomide with temsirolimus or dinutuximab in children with refractory or relapsed neuroblastoma (COG ANBL1221): an open-label, randomised, phase 2 trial.” Lancet Oncol 2017; 18(7): 946–57. PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosse YP, Laudenslager M, Longo L, et al. “Identification of ALK as a major familial neuroblastoma predisposition gene.” Nature 2008; 455(7215): 930–5. PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen le B, Diskin SJ, Capasso M, et al. “Phenotype restricted genome-wide association study using a gene-centric approach identifies three low-risk neuroblastoma susceptibility Loci.” PLoS Genet 2011; 7(3): e1002026. PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park JR, Kreissman SG, London WB, et al. “Effect of Tandem Autologous Stem Cell Transplant vs Single Transplant on Event-Free Survival in Patients With High-Risk Neuroblastoma: A Randomized Clinical Trial.” JAMA 2019; 322(8): 746–55. PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto NR, Applebaum MA, Volchenboum SL, et al. “Advances in Risk Classification and Treatment Strategies for Neuroblastoma.” J Clin Oncol 2015; 33(27): 3008–17. PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pugh TJ, Morozova O, Attiyeh EF, et al. “The genetic landscape of high-risk neuroblastoma.” Nat Genet 2013; 45(3): 279–84. PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell MR, Penikis A, Oldridge DA, et al. “CASC15-S Is a Tumor Suppressor lncRNA at the 6p22 Neuroblastoma Susceptibility Locus.” Cancer Res 2015; 75(15): 3155–66. PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schleiermacher G, Mosseri V, London WB, et al. “Segmental chromosomal alterations have prognostic impact in neuroblastoma: a report from the INRG project.” Br J Cancer 2012; 107(8): 1418–22. PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlisio S, Kenchappa RS, Vredeveld LC, et al. “The kinesin KIF1Bbeta acts downstream from EglN3 to induce apoptosis and is a potential 1p36 tumor suppressor.” Genes Dev 2008; 22(7): 884–93. PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trochet D, Bourdeaut F, Janoueix-Lerosey I, et al. “Germline mutations of the paired-like homeobox 2B (PHOX2B) gene in neuroblastoma.” American journal of human genetics 2004; 74(4): 761–4. PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twist CJ, Naranjo A, Schmidt ML, et al. “Defining Risk Factors for Chemotherapeutic Intervention in Infants With Stage 4S Neuroblastoma: A Report From Children’s Oncology Group Study ANBL0531.” J Clin Oncol 2019; 37(2): 115–24. PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valentijn LJ, Koster J, Zwijnenburg DA, et al. “TERT rearrangements are frequent in neuroblastoma and identify aggressive tumors.” Nat Genet 2015; 47(12): 1411–4. PMID [DOI] [PubMed] [Google Scholar]
- Wang K, Diskin SJ, Zhang H, et al. “Integrative genomics identifies LMO1 as a neuroblastoma oncogene.” Nature 2011; 469(7329): 216–20. PMID [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu AL, Gilman AL, Ozkaynak MF, et al. “Anti-GD2 antibody with GM-CSF, interleukin-2, and isotretinoin for neuroblastoma.” N Engl J Med 2010; 363(14): 1324–34. PMID [DOI] [PMC free article] [PubMed] [Google Scholar]