Abstract
The December, 2019 coronavirus disease outbreak has seen many countries ask people who have potentially come into contact with the infection to isolate themselves at home or in a dedicated quarantine facility. Decisions on how to apply quarantine should be based on the best available evidence. We did a Review of the psychological impact of quarantine using three electronic databases. Of 3166 papers found, 24 are included in this Review. Most reviewed studies reported negative psychological effects including post-traumatic stress symptoms, confusion, and anger. Stressors included longer quarantine duration, infection fears, frustration, boredom, inadequate supplies, inadequate information, financial loss, and stigma. Some researchers have suggested long-lasting effects. In situations where quarantine is deemed necessary, officials should quarantine individuals for no longer than required, provide clear rationale for quarantine and information about protocols, and ensure sufficient supplies are provided. Appeals to altruism by reminding the public about the benefits of quarantine to wider society can be favourable.
Introduction
Quarantine is the separation and restriction of movement of people who have potentially been exposed to a contagious disease to ascertain if they become unwell, so reducing the risk of them infecting others.1 This definition differs from isolation, which is the separation of people who have been diagnosed with a contagious disease from people who are not sick; however, the two terms are often used interchangeably, especially in communication with the public.2 The word quarantine was first used in Venice, Italy in 1127 with regards to leprosy and was widely used in response to the Black Death, although it was not until 300 years later that the UK properly began to impose quarantine in response to plague.3 Most recently, quarantine has been used in the coronavirus disease 2019 (COVID-19) outbreak. This outbreak has seen entire cities in China effectively placed under mass quarantine, while many thousands of foreign nationals returning home from China have been asked to self-isolate at home or in state-run facilities.4 There are precedents for such measures. Citywide quarantines were also imposed in areas of China and Canada during the 2003 outbreak of severe acute respiratory syndrome (SARS), whereas entire villages in many west African countries were quarantined during the 2014 Ebola outbreak.
Key messages.
-
•
Information is key; people who are quarantined need to understand the situation
-
•
Effective and rapid communication is essential
-
•
Supplies (both general and medical) need to be provided
-
•
The quarantine period should be short and the duration should not be changed unless in extreme circumstances
-
•
Most of the adverse effects come from the imposition of a restriction of liberty; voluntary quarantine is associated with less distress and fewer long-term complications
-
•
Public health officials should emphasise the altruistic choice of self-isolating
Why is this Review needed?
Quarantine is often an unpleasant experience for those who undergo it. Separation from loved ones, the loss of freedom, uncertainty over disease status, and boredom can, on occasion, create dramatic effects. Suicide has been reported,5 substantial anger generated, and lawsuits brought6 following the imposition of quarantine in previous outbreaks. The potential benefits of mandatory mass quarantine need to be weighed carefully against the possible psychological costs.7 Successful use of quarantine as a public health measure requires us to reduce, as far as possible, the negative effects associated with it.
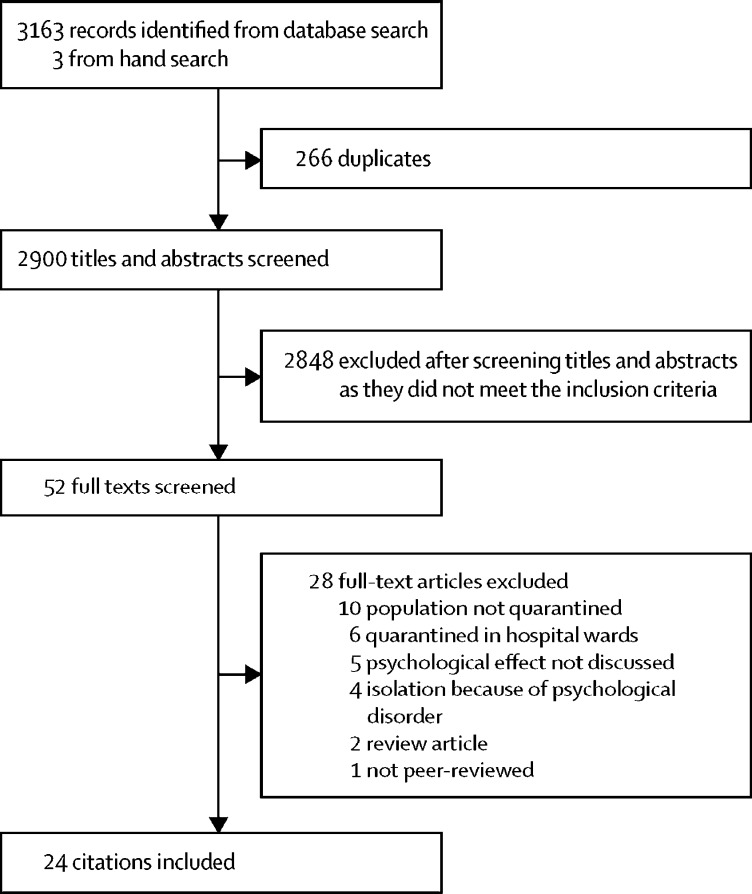
Given the developing situation with coronavirus, policy makers urgently need evidence synthesis to produce guidance for the public. In circumstances such as these, rapid reviews are recommended by WHO.8 We undertook a Review of evidence on the psychological impact of quarantine to explore its likely effects on mental health and psychological wellbeing, and the factors that contribute to, or mitigate, these effects. Of 3166 papers found, 24 are included in this Review (figure ). The characteristics of studies that met our inclusion criteria are presented in the table . These studies were done across ten countries and included people with SARS (11 studies), Ebola (five), the 2009 and 2010 H1N1 influenza pandemic (three), Middle East respiratory syndrome (two), and equine influenza (one). One of these studies related to both H1N1 and SARS.
Figure.
Screening profile
Table.
Study characteristics
| Country | Design | Participants | Quarantine period | Measures | |
|---|---|---|---|---|---|
| Bai et al (2004)9 | Taiwan | Cross-sectional | 338 hospital staff | 9 days because of contact with suspected SARS cases | Study-specific survey; SARS-related stress survey composed of acute stress disorder criteria according to the DSM-IV and related emotional and behavioural changes |
| Blendon et al (2004)10 | Canada | Cross-sectional | 501 Canadian residents | Length unclear; exposure to SARS | Study-specific survey |
| Braunack-Mayer et al (2013)11 | Australia | Qualitative | 56 school community members | Length unclear; H1N1 influenza | Interview |
| Caleo et al (2018)12 | Sierra Leone | Mixed methods | 1161 residents of a rural village; 20 of whom took part in an interview study | Length unclear; entire village on restricted movement because of Ebola | Interview |
| Cava et al (2005)13 | Canada | Qualitative | 21 Toronto residents | 5–10 days because of SARS contact | Interview |
| Desclaux et al (2017)14 | Senegal | Qualitative | 70 Ebola contact cases | 21 days because of Ebola contact | Interview |
| DiGiovanni et al (2004)15 | Canada | Mixed methods | 1509 Toronto residents | Duration of quarantine was the difference between the incubation period of SARS (taken as 10 days) and the time that had elapsed since their exposure to a SARS patient | Interviews, focus groups, and telephone polls |
| Hawryluck et al (2004)16 | Canada | Cross-sectional | 129 Toronto residents | Median of 10 days because of potential SARS exposure | IES-R to assess post-traumatic stress and CES-D to assess depression |
| Jeong et al (2016)17 | South Korea | Longitudinal | 1656 residents of four regions in Korea | 2 weeks because of contact with MERS patients | GAD-7 to assess anxiety and STAXI-2 to assess anger |
| Lee et al (2005)18 | Hong Kong (Special Administrative Region, China) | Mixed methods | 903 residents of Amoy Gardens (the first officially recognised site of community outbreak of SARS in Hong Kong) took surveys; 856 of whom were not diagnosed with SARS; 2 of whom were interviewed | Length unclear; residents of a SARS outbreak site | Study-specific survey |
| Liu et al (2012)19 | China | Cross-sectional | 549 hospital employees; 104 (19%) of whom had been quarantined | Length unclear; home or work quarantine because of potential SARS contact | CES-D to assess depressive symptoms and IES-R to assess post-traumatic stress symptoms |
| Marjanovic et al (2007)20 | Canada | Cross-sectional | 333 nurses | Length unclear; SARS exposure | MBI-GS to assess burnout; STAXI-2 to assess anger; six study-specific questions to assess avoidance behaviour |
| Maunder et al (2003)21 | Canada | Observational | Health-care workers (sample size unavailable) | 10 days voluntary quarantine because of potential SARS contact | Observations of health-care staff |
| Mihashi et al (2009)22 | China | Retrospective cross-sectional | 187 printing company workers, university faculty members and their families, and non-medicine students | Length unclear; citywide isolation because of SARS | GHQ-30 to assess psychological disorders |
| Pan et al (2005)23 | Taiwan | Observational | 12 college students | Length unclear; asked to limit interactions outside the home because of potential SARS contact | Observations of a support group for home-quarantined students |
| Pellecchia et al (2015)24 | Liberia | Qualitative | 432 (focus groups) and 30 (interviews) residents of neighbourhoods with incidence of Ebola | 21 days because neighbourhoods had epidemiological incidence of Ebola | Interviews and focus groups |
| Reynolds et al (2008)25 | Canada | Cross-sectional | 1057 close contacts of potential SARS cases | Mean 8·3 days; range 2–30 days because of contact with potential SARS cases | IES-7 to assess post-traumatic stress symptoms |
| Robertson et al (2004)26 | Canada | Qualitative | 10 health-care workers | 10 days home quarantine, or continually wearing a mask in the presence of others, or required to attend work but had to travel in their own vehicle and wear a mask, because of SARS exposure | Interviews |
| Sprang and Silman (2013)27 | USA and Canada | Cross-sectional | 398 parents | Length unclear; lived in areas severely affected by H1N1 or SARS | PTSD-RI Parent Version and PCL-C |
| Taylor et al (2008)28 | Australia | Cross-sectional | 2760 horse owners or those involved in horse industry | Several weeks because of equine influenza | K10 to assess distress |
| Wang et al (2011)29 | China | Cross-sectional | 419 undergraduates | 7 days; non-suspected H1N1 influenza cases | SRQ-20 to assess general mental health and IES-R to assess post-traumatic stress |
| Wester and Giesecke (2019)30 | Sweden | Qualitative | 12: six health-care workers who worked in west Africa during the Ebola outbreak and one close contact for each of them | 3 weeks because of working in west Africa during the Ebola crisis | Interview |
| Wilken et al (2017)31 | Liberia | Qualitative | 16 residents of villages who were quarantined | 21 days because of living in a village in which someone had died of Ebola | Interview |
| Wu et al (2008, 2009)32, 33 | China | Cross-sectional | 549 hospital employees | Length unclear; either because of SARS diagnosis, suspected SARS, or having had direct contact with SARS patients | 7 questions adapted from NHSDA to assess alcohol dependence and abuse; IES-R to assess post-traumatic stress symptoms; CES-D to assess depression |
| Yoon et al (2016)34 | South Korea | Psychological evaluation by professionals | 6231 Korean residents | Length unclear; placed in quarantine because of MERS | Questions such as ‘for the last 2 weeks or after being in quarantine, do you feel depressed or hopelessness? Do you feel loss of interest in any part of your life?’ |
SARS=severe acute respiratory syndrome. DSM-IV=Diagnostic and Statistical Manual of Mental Disorders-IV. IES-R=Impact of Event Scale-Revised. CES-D=Center for Epidemiologic Studies Depression scale. MERS=Middle East respiratory syndrome-related coronavirus. GAD-7=Generalised Anxiety Disorder-7. STAXI-2=State-Trait Anger Expression Inventory. MBI-GS= Maslach Burnout Inventory-General Survey. GHQ-30=General Health Questionnaire-30. IES-7=International Education Standard-7. PTSD-RI=Post-Traumatic Stress Disorder Reaction Index. PCL-C=PTSD Checklist-Civilian version. K10= Kessler 10 Psychological Distress Scale. SRQ-20=Self-Reporting Questionnaire-20. NHSDA=National Household Survey on Drug Abuse.
The psychological impact of quarantine
Five studies compared psychological outcomes for people quarantined with those not quarantined.9, 19, 27, 28, 33 A study9 of hospital staff who might have come into contact with SARS found that immediately after the quarantine period (9 days) ended, having been quarantined was the factor most predictive of symptoms of acute stress disorder. In the same study, quarantined staff were significantly more likely to report exhaustion, detachment from others, anxiety when dealing with febrile patients, irritability, insomnia, poor concentration and indecisiveness, deteriorating work performance, and reluctance to work or consideration of resignation. In another study,33 the effect of being quarantined was a predictor of post-traumatic stress symptoms in hospital employees even 3 years later. Approximately 34% (938 of 2760) of horse owners quarantined for several weeks because of an equine influenza outbreak reported high psychological distress during the outbreak, compared with around 12% in the Australian general population.28 A study27 comparing post-traumatic stress symptoms in parents and children quarantined with those not quarantined found that the mean post-traumatic stress scores were four times higher in children who had been quarantined than in those who were not quarantined. 28% (27 of 98) of parents quarantined in this study reported sufficient symptoms to warrant a diagnosis of a trauma-related mental health disorder, compared with 6% (17 of 299) of parents who were not quarantined. Another study19 of hospital staff examined symptoms of depression 3 years after quarantine and found that 9% (48 of 549) of the whole sample reported high depressive symptoms. In the group with high depressive symptoms, nearly 60% (29 of 48) had been quarantined but only 15% (63 of 424) of the group with low depressive symptoms had been quarantined.
All other quantitative studies only surveyed those who had been quarantined and generally reported a high prevalence of symptoms of psychological distress and disorder. Studies reported on general psychological symptoms,22 emotional disturbance,34 depression,16 stress,15 low mood,18 irritability,18 insomnia,18 post-traumatic stress symptoms25 (rated on Weiss and Marmar's Impact of Event Scale–Revised35), anger,20 and emotional exhaustion.21 Low mood (660 [73%] of 903) and irritability (512 [57%] of 903) stand out as having high prevalence.18
People quarantined because of being in close contact with those who potentially have SARS25 reported various negative responses during the quarantine period: over 20% (230 of 1057) reported fear, 18% (187) reported nervousness, 18% (186) reported sadness, and 10% (101) reported guilt. Few reported positive feelings: 5% (48) reported feelings of happiness and 4% (43) reported feelings of relief. Qualitative studies also identified a range of other psychological responses to quarantine, such as confusion,11, 12, 13, 23 fear,12, 13, 14, 15, 23, 24 anger,12, 13 grief,29 numbness,23 and anxiety-induced insomnia.14, 15
One study compared undergraduates who had been quarantined with those not quarantined immediately after the quarantine period and found no significant difference between the groups in terms of post-traumatic stress symptoms or general mental health problems.29 However, the entire study population were undergraduate students (who are generally young, and perhaps have fewer responsibilities than adults who are employed full-time) and thus it is possible that these conclusions cannot be generalised to the wider population.
Only one study17 compared psychological outcomes during quarantine with later outcomes and found that during quarantine, 7% (126 of 1656) showed anxiety symptoms and 17% (275) showed feelings of anger, whereas 4–6 months after quarantine these symptoms had reduced to 3% (anxiety) and 6% (anger).
Two studies reported on longer-term effects of quarantine. 3 years after the SARS outbreak, alcohol abuse or dependency symptoms were positively associated with having been quarantined in health-care workers.32 In a multivariate analysis,32 after controlling for demographic factors, having been quarantined and having worked in a high-risk location were the two types of exposure significantly associated with these outcomes (for quarantine: unadjusted mean ratio 0·45; 95% CI 1·02–2·65).
After quarantine, many participants continued to engage in avoidance behaviours. For health-care workers,20 being quarantined was significantly and positively associated with avoidance behaviours, such as minimising direct contact with patients and not reporting to work. A study25 of people quarantined because of potential SARS contact noted that 54% (524 of 1057) of people who had been quarantined avoided people who were coughing or sneezing, 26% (255) avoided crowded enclosed places, and 21% (204) avoided all public spaces in the weeks following the quarantine period. A qualitative study13 reported that several participants described long-term behavioural changes after the quarantine period, such as vigilant handwashing and avoidance of crowds and, for some, the return to normality was delayed by many months.
Prequarantine predictors of psychological impact
There was mixed evidence for whether participant characteristics and demographics were predictors of the psychological impact of quarantine. A study28 of horse owners quarantined because of equine influenza identified several characteristics associated with negative psychological impacts: younger age (16–24 years), lower levels of formal educational qualifications, female gender, and having one child as opposed to no children (although having three or more children appeared somewhat protective). However, another study16 suggested that demographic factors such as marital status, age, education, living with other adults, and having children were not associated with psychological outcomes.
Having a history of psychiatric illness was associated with experiencing anxiety and anger 4–6 months after release from quarantine.17 Health-care workers25 who had been quarantined had more severe symptoms of post-traumatic stress than members of the general public who had been quarantined, scoring significantly higher on all dimensions. Health-care workers also felt greater stigmatisation than the general public, exhibited more avoidance behaviours after quarantine, reported greater lost income, and were consistently more affected psychologically: they reported substantially more anger, annoyance, fear, frustration, guilt, helplessness, isolation, loneliness, nervousness, sadness, worry, and were less happy. Health-care workers were also substantially more likely to think they had SARS and to be concerned about infecting others. Conversely, one study16 suggested that health-care worker status was not associated with psychological outcomes.
Stressors during quarantine
Duration of quarantine
Three studies showed that longer durations of quarantine were associated with poorer mental health specifically, post-traumatic stress symptoms,16, 25 avoidance behaviours, and anger.20 Although the duration of the quarantine was not always clear, one study16 showed that those quarantined for more than 10 days showed significantly higher post-traumatic stress symptoms than those quarantined for less than 10 days.
Fears of infection
Participants in eight studies reported fears about their own health or fears of infecting others9, 13, 14, 16, 17, 21, 25, 26 and were more likely to fear infecting family members than those not quarantined.9 They also became particularly worried if they experienced any physical symptoms potentially related to the infection14 and fear that the symptoms could reflect having the infection continued to be related to psychological outcomes several months later.17 Conversely, one study11 found that although very few participants were extremely concerned about becoming infected or transmitting the virus to others, those who were concerned tended to be pregnant women and those with young children.
Frustration and boredom
Confinement, loss of usual routine, and reduced social and physical contact with others were frequently shown to cause boredom, frustration, and a sense of isolation from the rest of the world, which was distressing to participants.10, 11, 13, 14, 15, 16, 25, 26, 31 This frustration was exacerbated by not being able to take part in usual day-to-day activities, such as shopping for basic necessities16 or taking part in social networking activities via the telephone or internet.17
Inadequate supplies
Having inadequate basic supplies (eg, food, water, clothes, or accommodation) during quarantine was a source of frustration10, 31 and continued to be associated with anxiety and anger 4–6 months after release.17 Being unable to get regular medical care and prescriptions also appeared to be a problem for some participants.10
Four studies found that supplies from public health authorities were insufficient. Participants reported receiving their masks and thermometers late or not at all;13 food, water, and other items were only intermittently distributed;24 and food supplies took a long time to arrive.12 Although those quarantined during the Toronto SARS outbreak praised public health authorities for delivering kits of medical supplies at the beginning of the quarantine period, they did not receive groceries or other routine supplies needed for daily living.15
Inadequate information
Many participants cited poor information from public health authorities as a stressor, reporting insufficient clear guidelines about actions to take and confusion about the purpose of quarantine.11, 12, 13, 15, 24, 26 After the Toronto SARS epidemic, participants perceived that confusion stemmed from the differences in style, approach, and content of various public health messages because of poor coordination between the multiple jurisdictions and levels of government involved.15 Lack of clarity about the different levels of risk, in particular, led to participants fearing the worst.14 Participants also reported a perceived lack of transparency from health and government officials about the severity of the pandemic.11 Perhaps related to the lack of clear guidelines or rationale, perceived difficulty with complying with quarantine protocols was a significant predictor of post-traumatic stress symptoms in one study.25
Stressors postquarantine
Finances
Financial loss can be a problem during quarantine, with people unable to work and having to interrupt their professional activities with no advanced planning; the effects appear to be long lasting. In the reviewed studies, the financial loss as a result of quarantine created serious socioeconomic distress24 and was found to be a risk factor for symptoms of psychological disorders22 and both anger and anxiety several months after quarantine.17 One study28 found that respondents who were quarantined because of equine influenza, whose principal source of income was from a horse-related industry, were more than twice as likely to have high distress than those whose income was not from the industry. This finding is probably linked to economic effects but could also be related to disruption of social networks and loss of leisure activities. Notably, this study is exceptional in that occupation and exposure are confounded.
A study14 of people quarantined because of potential Ebola contact found that, although participants received financial assistance, some felt that the amount was insufficient and that it came too late; many felt wronged as the assistance they received did not cover their ongoing professional expenses. Many became dependent on their families to provide for them financially during quarantine which was often hard to accept and could cause conflicts. In one study,13 none of those quarantined in Toronto during SARS reported much financial hardship because employers or the government compensated them, but where that reimbursement was slow to arrive it caused those less financially well-off to struggle.
Potentially related to financial loss, participants with a combined annual household income of less than CAN$40 000 showed significantly higher amounts of post-traumatic stress and depressive symptoms.16 These symptoms are probably because those with lower incomes were more likely to be affected by the temporary loss of income than those with higher incomes.
People who are quarantined and have lower household incomes might require additional levels of support, along with those who lose earnings while in quarantine (ie, self-employed people who are unable to work or salaried staff who are unable to take paid leave). Financial reimbursements should be provided where possible and programmes developed to provide financial support throughout the quarantine period. Where appropriate, employers might also wish to consider proactive approaches that allow employees to work from home if they wish to, both to avoid financial loss and to stave off boredom, while being mindful that staff in these situations might not be at their most productive and might benefit more from remote social support from their colleagues.2
Stigma
Stigma from others was a major theme throughout the literature, often continuing for some time after quarantine, even after containment of the outbreak. In a comparison of health-care workers quarantined versus those not quarantined,9 quarantined participants were significantly more likely to report stigmatisation and rejection from people in their local neighbourhoods, suggesting that there is stigma specifically surrounding people who had been quarantined. Participants in several studies reported that others were treating them differently: avoiding them, withdrawing social invitations, treating them with fear and suspicion, and making critical comments.13, 14, 15, 16, 18, 21, 23, 24, 25, 26, 30, 31
Several health-care workers involved in the Ebola outbreak in Senegal reported that quarantine had led their families to consider their jobs to be too risky, creating intra-household tension.14 In the same study, three participants reported being unable to resume their jobs after surveillance ended because their employers expressed fear of contagion.
Those quarantined during the Ebola epidemic in Liberia reported that stigma could lead to disenfranchisement of minority groups in the community as families under quarantine were often said to belong to different ethnic groups, tribes, or religions and were perceived as dangerous because they were different.24 Perhaps because of this stigma, being quarantined led participants in this study to keep easily treatable, non-Ebola illnesses a secret and avoided seeking help.
General education about the disease and the rationale for quarantine and public health information provided to the general public can be beneficial to reduce stigmatisation, whereas more detailed information targeted at schools and workplaces might also be useful. It might also be that media reporting contributes to stigmatising attitudes in the general public; the media is a powerful influence on public attitudes and dramatic headlines and fear mongering have been shown to contribute to stigmatising attitudes in the past (eg, during the SARS outbreak).36 This issue highlights the need for public health officials to provide rapid, clear messages delivered effectively for the entire affected population to promote accurate understanding of the situation.
What can be done to mitigate the consequences of quarantine?
During major infectious disease outbreaks, quarantine can be a necessary preventive measure. However, this Review suggests that quarantine is often associated with a negative psychological effect. During the period of quarantine this negative psychological effect is unsurprising, yet the evidence that a psychological effect of quarantine can still be detected months or years later—albeit from a small number of studies17, 19— is more troubling and suggests the need to ensure that effective mitigation measures are put in place as part of the quarantine planning process.
In this regard, our results do not provide strong evidence that any particular demographic factors are risk factors of poor psychological outcomes after quarantine and therefore require specific attention. However, history of mental illness was only examined as a risk factor by one study. Previous literature suggests that psychiatric history is associated with psychological distress after experiencing any disaster-related trauma37, 38 and it is likely that people with pre-existing poor mental health would need extra support during quarantine. There also appeared to be a high prevalence of psychological distress in quarantined health-care workers, although there was mixed evidence as to whether this group were at higher risk for distress than non-health-care workers who were quarantined. For health-care workers, support from managers is essential in facilitating their return to work39 and managers should be aware of the potential risks for their staff who were quarantined so that they can prepare for early intervention.
Keep it as short as possible
Longer quarantine is associated with poorer psychological outcomes, perhaps unsurprisingly, as it stands to reason that the stressors reported by participants could have more of an effect the longer they were experienced for. Restricting the length of quarantine to what is scientifically reasonable given the known duration of incubation periods, and not adopting an overly precautionary approach to this, would minimise the effect on people. Evidence from elsewhere also emphasises the importance of authorities adhering to their own recommended length of quarantine, and not extending it. For people already in quarantine, an extension, no matter how small, is likely to exacerbate any sense of frustration or demoralisation.40 Imposing a cordon indefinitely on whole cities with no clear time limit (such as has been seen in Wuhan, China) might be more detrimental than strictly applied quarantine procedures limited to the period of incubation.
Give people as much information as possible
People who are quarantined often feared being infected or infecting others. They also often have catastrophic appraisals of any physical symptoms experienced during the quarantine period. This fear is a common occurrence for people exposed to a worrying infectious disease,41 and might be exacerbated by the often inadequate information participants reported receiving from public health officials leaving them unclear of the nature of the risks they faced and why they were being quarantined at all. Ensuring that those under quarantine have a good understanding of the disease in question, and the reasons for quarantine, should be a priority.
Provide adequate supplies
Officials also need to ensure that quarantined households have enough supplies for their basic needs and, importantly, these must be provided as rapidly as possible. Coordination for provision of supplies should ideally occur in advance, with conservation and reallocation plans established to ensure resources do not run out, which unfortunately has been reported.2
Reduce the boredom and improve the communication
Boredom and isolation will cause distress; people who are quarantined should be advised about what they can do to stave off boredom and provided with practical advice on coping and stress management techniques. Having a working mobile phone is now a necessity, not a luxury, and those stepping off a long flight to enter quarantine will probably welcome a charger or adaptor more than anything else.17 Activating your social network, albeit remotely, is not just a key priority, but an inability to do so is associated not just with immediate anxiety, but longer- term distress.2, 42 One study21 suggested that having a telephone support line, staffed by psychiatric nurses, set up specifically for those in quarantine could be effective in terms of providing them with a social network. The ability to communicate with one's family and friends is also essential. Particularly, social media could play an important part in communication with those far away, allowing people who are quarantined to update their loved ones about their situation and reassure them that they are well. Therefore, providing those quarantined with mobile phones, cords and outlets for charging devices, and robust WiFi networks with internet access to allow them to communicate directly with loved ones could reduce feelings of isolation, stress, and panic.2 Although this is possible to achieve in enforced quarantine, it could be more difficult to do in the case of widespread home quarantine; countries imposing censors on social media and messaging applications could also present difficulties in ensuring lines of communication between those quarantined and their loved ones.
It is also important that public health officials maintain clear lines of communication with people quarantined about what to do if they experience any symptoms. A phone line or online service specifically set up for those in quarantine and staffed by health-care workers who can provide instructions about what to do in the event of developing illness symptoms, would help reassure people that they will be cared for if they become ill. This service would show those who are quarantined that they have not been forgotten and that their health needs are just as important as those of the wider public. The benefits of such a resource have not been studied, but it is likely that reassurance could subsequently decrease feelings such as fear, worry, and anger.
There is evidence to suggest that support groups specifically for people who were quarantined at home during disease outbreaks can be helpful. One study23 found that having such a group and feeling connected to others who had been through the same situation could be a validating, empowering experience and can provide people with the support they might find they are not receiving from other people.
Health-care workers deserve special attention
Health-care workers themselves are often quarantined and this Review suggests they, like the general public, are negatively affected by stigmatising attitudes from others. None of the studies included in this Review focused on the perceptions of their colleagues, but this would be an interesting aspect to explore. It is also possible that health-care workers who are quarantined might be concerned about causing their workplaces to be understaffed and causing extra work for their colleagues21 and that their colleagues' perceptions could be particularly important. Being separated from a team they are used to working in close contact with might add to feelings of isolation for health-care workers who are quarantined. Therefore, it is essential that they feel supported by their immediate colleagues. During infectious disease outbreaks, organisational support has been found to be protective of mental health for health-care staff in general39 and managers should take steps to ensure their staff members are supportive of their colleagues who are quarantined.
Altruism is better than compulsion
Perhaps because of the difficulties of designing an appropriate study, no research was found which tested whether mandatory versus voluntary quarantine has a differential effect on wellbeing. In other contexts, however, feeling that others will benefit from one's situation can make stressful situations easier to bear and it seems likely that this is also true for home-based quarantine. Reinforcing that quarantine is helping to keep others safe, including those particularly vulnerable (such as those who are very young, old, or with pre-existing serious medical conditions), and that health authorities are genuinely grateful to them, can only help to reduce the mental health effect and adherence in those quarantined.19, 33 Notably, altruism has its limits if people are being asked to quarantine without adequate information on how to keep the people they live with safe. It is unacceptable to ask people to self-quarantine for the benefit of the community's health, when while doing so they might be putting their loved ones at risk.
What we do not know
Quarantine is one of several public health measures to prevent the spread of an infectious disease and as shown in this Review, has a considerable psychological impact for those affected. As such, there is a question as to whether other public health measures that prevent the need to impose quarantine (such as social distancing, cancellation of mass gatherings, and school closures) might be more favourable. Future research is needed to establish the effectiveness of such measures.
The strengths and limitations of this Review must be considered. Because of the time constraints of this Review given the ongoing coronavirus outbreak, the reviewed literature did not undergo formal quality appraisal. Additionally, the Review was limited to peer-reviewed publications and we did not explore potentially relevant grey literature. The recommendations we have made apply primarily to small groups of people in dedicated facilities and to some extent in self-isolation. Although we anticipate that many of the risk factors for poor psychosocial outcomes would be the same for larger containment processes (such as entire towns or cities), there are likely to be distinct differences in such situations that mean that the information presented in this Review should only be applied to such situations cautiously. Furthermore, potential cultural differences need to be considered. Although this Review cannot predict exactly what will happen or provide recommendations that will work for every future population that is quarantined, we have provided an overview of the key issues and how they could be rectified in the future.
There are also several limitations of the reviewed literature, which must be pointed out: only one study followed up participants over time, sample sizes were generally small, few studies directly compared participants quarantined with those not quarantined, conclusions based on certain study populations (eg, students) might not be generalisable to the wider public, and heterogeneity of outcome measures across studies make it difficult to make direct comparisons between studies. It is also worth pointing out that a minority of studies assessed symptoms of post-traumatic stress using measures designed to measure post-traumatic stress disorder, despite quarantine not being qualified as a trauma in the diagnosis for post-traumatic stress disorder in the Diagnostic and Statistical Manual of Mental Disorders 5.43
Strengths of this Review include the hand-searching of reference lists to identify any papers not found in the initial search, contacting authors who sent full-texts of papers which were not available in full online, and having multiple researchers carry out the screening to improve the rigour of the Review.
Conclusion
Overall, this Review suggests that the psychological impact of quarantine is wide-ranging, substantial, and can be long lasting. This is not to suggest that quarantine should not be used; the psychological effects of not using quarantine and allowing disease to spread might be worse.44 However, depriving people of their liberty for the wider public good is often contentious and needs to be handled carefully. If quarantine is essential, then our results suggest that officials should take every measure to ensure that this experience is as tolerable as possible for people. This can be achieved by: telling people what is happening and why, explaining how long it will continue, providing meaningful activities for them to do while in quarantine, providing clear communication, ensuring basic supplies (such as food, water, and medical supplies) are available, and reinforcing the sense of altruism that people should, rightly, be feeling. Health officials charged with implementing quarantine, who by definition are in employment and usually with reasonable job security, should also remember that not everyone is in the same situation. If the quarantine experience is negative, the results of this Review suggest there can be long-term consequences that affect not just the people quarantined but also the health-care system that administered the quarantine and the politicians and public health officials who mandated it.
Search strategy and selection criteria
Our search strategy was designed to inform this Review and a second review to be published elsewhere relating to adherence to quarantine. We searched Medline, PsycINFO, and Web of Science. The full list of search terms can be found in the appendix. In brief, we used a combination of terms relating to quarantine (eg, “quarantine” and “patient isolation”) and psychological outcomes (eg, “psych” and “stigma”). For studies to be included in this Review, they had to report on primary research, be published in peer-reviewed journals, be written in English or Italian (as these are the languages spoken by the current authors), include participants asked to enter into quarantine outside of a hospital environment for at least 24 hours, and include data on the prevalence of mental illness or psychological wellbeing, or on factors associated with mental illness or psychological wellbeing (ie, any predictors of psychological wellbeing during or after quarantine). The initial search yielded 3166 papers, of which 24 included relevant data and were included in this Review. The screening process is illustrated in the figure.
Acknowledgments
Acknowledgments
The research was funded by the National Institute for Health Research (NIHR) Health Protection Research Unit in Emergency Preparedness and Response at King's College London, in partnership with Public Health England, and in collaboration with the University of East Anglia and Newcastle University. The views expressed are those of the author(s) and not necessarily those of the National Health Service, NIHR, Department of Health and Social Care, or Public Health England.
Editorial note: the Lancet Group takes a neutral position with respect to territorial claims in the published table.
Contributors
GJR designed the search strategy with input from SKB, RKW, and LES. SKB, RKW, LES, and LW carried out the literature searches and screening, and any discrepancies were discussed with GJR and SW. SKB carried out the data extraction. SKB wrote the first draft of the review with input from RKW, LES, LW, SW, NG, and GJR.
Declaration of interests
We declare no competing interests.
Supplementary Material
References
- 1.Centers for Disease Control and Prevention Quarantine and isolation. 2017. https://www.cdc.gov/quarantine/index.html (accessed Jan 30, 2020).
- 2.Manuell M-E, Cukor J. Mother Nature versus human nature: public compliance with evacuation and quarantine. Disasters. 2011;35:417–442. doi: 10.1111/j.1467-7717.2010.01219.x. [DOI] [PubMed] [Google Scholar]
- 3.Newman K. Shutt up: bubonic plague and quarantine in early modern England. J Sol Hist. 2012;45:809–834. doi: 10.1093/jsh/shr114. [DOI] [PubMed] [Google Scholar]
- 4.Public Health England Novel coronavirus (2019-nCoV) – what you need to know. 2020. https://publichealthmatters.blog.gov.uk/2020/01/23/wuhan-novel-coronavirus-what-you-need-to-know/ (accessed Jan 31, 2020).
- 5.Barbisch D, Koenig KL, Shih FY. Is there a case for quarantine? Perspectives from SARS to Ebola. Disaster Med Public Health Prep. 2015;9:547–553. doi: 10.1017/dmp.2015.38. [DOI] [PubMed] [Google Scholar]
- 6.Miles SH. Kaci Hickox: public health and the politics of fear. 2014. http://www.bioethics.net/2014/11/kaci-hickox-public-health-and-the-politics-of-fear/ (accessed Jan 31, 2020). [DOI] [PubMed]
- 7.Rubin GJ, Wessely S. The psychological effects of quarantining a city. BMJ. 2020;368:m313. doi: 10.1136/bmj.m313. [DOI] [PubMed] [Google Scholar]
- 8.WHO Rapid reviews to strengthen health policy and systems: a practical guide. 2017. https://www.who.int/alliance-hpsr/resources/publications/rapid-review-guide/en/ (accessed Jan 31, 2020).
- 9.Bai Y, Lin C-C, Lin C-Y, Chen J-Y, Chue C-M, Chou P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv. 2004;55:1055–1057. doi: 10.1176/appi.ps.55.9.1055. [DOI] [PubMed] [Google Scholar]
- 10.Blendon RJ, Benson JM, DesRoches CM, Raleigh E, Taylor-Clark K. The public's response to severe acute respiratory syndrome in Toronto and the United States. Clin Infect Dis. 2004;38:925–931. doi: 10.1086/382355. [DOI] [PubMed] [Google Scholar]
- 11.Braunack-Mayer A, Tooher R, Collins JE, Street JM, Marshall H. Understanding the school community's response to school closures during the H1N1 2009 influenza pandemic. BMC Public Health. 2013;13:344. doi: 10.1186/1471-2458-13-344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Caleo G, Duncombe J, Jephcott F. The factors affecting household transmission dynamics and community compliance with Ebola control measures: a mixed-methods study in a rural village in Sierra Leone. BMC Public Health. 2018;18:248. doi: 10.1186/s12889-018-5158-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cava MA, Fay KE, Beanlands HJ, McCay EA, Wignall R. The experience of quarantine for individuals affected by SARS in Toronto. Public Health Nurs. 2005;22:398–406. doi: 10.1111/j.0737-1209.2005.220504.x. [DOI] [PubMed] [Google Scholar]
- 14.Desclaux A, Badji D, Ndione AG, Sow K. Accepted monitoring or endured quarantine? Ebola contacts' perceptions in Senegal. Soc Sci Med. 2017;178:38–45. doi: 10.1016/j.socscimed.2017.02.009. [DOI] [PubMed] [Google Scholar]
- 15.DiGiovanni C, Conley J, Chiu D, Zaborski J. Factors influencing compliance with quarantine in Toronto during the 2003 SARS outbreak. Biosecur Bioterror. 2004;2:265–272. doi: 10.1089/bsp.2004.2.265. [DOI] [PubMed] [Google Scholar]
- 16.Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. 2004;10:1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jeong H, Yim HW, Song Y-J. Mental health status of people isolated due to Middle East respiratory syndrome. Epidemiol Health. 2016;38:e2016048. doi: 10.4178/epih.e2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee S, Chan LY, Chau AM, Kwok KP, Kleinman A. The experience of SARS-related stigma at Amoy Gardens. Soc Sci Med. 2005;61:2038–2046. doi: 10.1016/j.socscimed.2005.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu X, Kakade M, Fuller CJ. Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Compr Psychiatry. 2012;53:15–23. doi: 10.1016/j.comppsych.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marjanovic Z, Greenglass ER, Coffey S. The relevance of psychosocial variables and working conditions in predicting nurses' coping strategies during the SARS crisis: an online questionnaire survey. Int J Nurs Stud. 2007;44:991–998. doi: 10.1016/j.ijnurstu.2006.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maunder R, Hunter J, Vincent L. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. 2003;168:1245–1251. [PMC free article] [PubMed] [Google Scholar]
- 22.Mihashi M, Otsubo Y, Yinjuan X, Nagatomi K, Hoshiko M, Ishitake T. Predictive factors of psychological disorder development during recovery following SARS outbreak. Health Psychol. 2009;28:91–100. doi: 10.1037/a0013674. [DOI] [PubMed] [Google Scholar]
- 23.Pan PJD, Chang S-H, Yu Y-Y. A support group for home-quarantined college students exposed to SARS: learning from practice. J Spec Group Work. 2005;30:363–374. [Google Scholar]
- 24.Pellecchia U, Crestani R, Decroo T, Van den Bergh R, Al-Kourdi Y. Social consequences of Ebola containment measures in Liberia. PLoS One. 2015;10:e0143036. doi: 10.1371/journal.pone.0143036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reynolds DL, Garay JR, Deamond SL, Moran MK, Gold W, Styra R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol Infect. 2008;136:997–1007. doi: 10.1017/S0950268807009156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Robertson E, Hershenfield K, Grace SL, Stewart DE. The psychosocial effects of being quarantined following exposure to SARS: a qualitative study of Toronto health care workers. Can J Psychiatry. 2004;49:403–407. doi: 10.1177/070674370404900612. [DOI] [PubMed] [Google Scholar]
- 27.Sprang G, Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med Public Health Prep. 2013;7:105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- 28.Taylor MR, Agho KE, Stevens GJ, Raphael B. Factors influencing psychological distress during a disease epidemic: data from Australia's first outbreak of equine influenza. BMC Public Health. 2008;8:347. doi: 10.1186/1471-2458-8-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang Y, Xu B, Zhao G, Cao R, He X, Fu S. Is quarantine related to immediate negative psychological consequences during the 2009 H1N1 epidemic? Gen Hosp Psychiatry. 2011;33:75–77. doi: 10.1016/j.genhosppsych.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 30.Wester M, Giesecke J. Ebola and healthcare worker stigma. Scand J Public Health. 2019;47:99–104. doi: 10.1177/1403494817753450. [DOI] [PubMed] [Google Scholar]
- 31.Wilken JA, Pordell P, Goode B. Knowledge, attitudes, and practices among members of households actively monitored or quarantined to prevent transmission of Ebola virus disease–Margibi County, Liberia: February–March 2015. Prehosp Disaster Med. 2017;32:673–678. doi: 10.1017/S1049023X17006720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu P, Liu X, Fang Y. Alcohol abuse/dependence symptoms among hospital employees exposed to a SARS outbreak. Alcohol Alcohol. 2008;43:706–712. doi: 10.1093/alcalc/agn073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu P, Fang Y, Guan Z. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. 2009;54:302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yoon MK, Kim SY, Ko HS, Lee MS. System effectiveness of detection, brief intervention and refer to treatment for the people with post-traumatic emotional distress by MERS: a case report of community-based proactive intervention in South Korea. Int J Ment Health Syst. 2016;10:51. doi: 10.1186/s13033-016-0083-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weiss DS, Marmar CR. The impact of event scale – revised. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. Guildford Press; New York: 1997. pp. 399–411. [Google Scholar]
- 36.Person B, Sy F, Holton K. Fear and stigma: the epidemic within the SARS outbreak. Emerg Infect Dis. 2004;10:358–363. doi: 10.3201/eid1002.030750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alvarez J, Hunt M. Risk and resilience in canine search and rescue handlers after 9/11. J Trauma Stress. 2005;18:497–505. doi: 10.1002/jts.20058. [DOI] [PubMed] [Google Scholar]
- 38.Cukor J, Wyka K, Jayasinghe N. Prevalence and predictors of posttraumatic stress symptoms in utility workers deployed to the World Trade Center following the attacks of September 11, 2001. Depress Anxiety. 2011;28:210–217. doi: 10.1002/da.20776. [DOI] [PubMed] [Google Scholar]
- 39.Brooks SK, Dunn R, Amlôt R, Rubin GJ, Greenberg N. A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. J Occup Environ Med. 2018;60:248–257. doi: 10.1097/JOM.0000000000001235. [DOI] [PubMed] [Google Scholar]
- 40.Rona RJ, Fear NT, Hull L. Mental health consequences of overstretch in the UK armed forces: first phase of a cohort study. BMJ. 2007;335:603. doi: 10.1136/bmj.39274.585752.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rubin GJ, Harper S, Williams PD. How to support staff deploying on overseas humanitarian work: a qualitative analysis of responder views about the 2014/15 West African Ebola outbreak. Eur J Psychotraumatol. 2016;7:30933. doi: 10.3402/ejpt.v7.30933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rubin GJ, Brewin CR, Greenberg N, Simpson J, Wessely S. Psychological and behavioural reactions to the bombings in London on 7 July 2005: cross sectional survey of a representative sample of Londoners. BMJ. 2005;331:606. doi: 10.1136/bmj.38583.728484.3A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.American Psychiatric Association . Diagnostic and statistical manual of mental disorders: DSM-5. American Psychiatric Association; Arlington, VA: 2013. [Google Scholar]
- 44.Hull HF. SARS control and psychological effects of quarantine, Toronto, Canada. Emerging Infectious Diseases. 2005;11:354–355. doi: 10.3201/eid1102.040760. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.