Abstract
Although maternal and child mortality are on the decline in southeast Asia, there are still major disparities, and greater equity is key to achieve the Millennium Development Goals. We used comparable cross-national data sources to document mortality trends from 1990 to 2008 and to assess major causes of maternal and child deaths. We present inequalities in intervention coverage by two common measures of wealth quintiles and rural or urban status. Case studies of reduction in mortality in Thailand and Indonesia indicate the varying extents of success and point to some factors that accelerate progress. We developed a Lives Saved Tool analysis for the region and for country subgroups to estimate deaths averted by cause and intervention. We identified three major patterns of maternal and child mortality reduction: early, rapid downward trends (Brunei, Singapore, Malaysia, and Thailand); initially high declines (sustained by Vietnam but faltering in the Philippines and Indonesia); and high initial rates with a downward trend (Laos, Cambodia, and Myanmar). Economic development seems to provide an important context that should be coupled with broader health-system interventions. Increasing coverage and consideration of the health-system context is needed, and regional support from the Association of Southeast Asian Nations can provide increased policy support to achieve maternal, neonatal, and child health goals.
This is the second in a Series of six papers about health in southeast Asia
Introduction
Southeast Asia has achieved substantial reductions in child and maternal mortality over the past two decades, but these achievements are unevenly distributed among and within the countries in the region. Of the ten countries in the Association of Southeast Asian Nations (ASEAN), only three have infant and child mortality rates below ten per 1000 livebirths—Brunei, Singapore, and Malaysia. Infant and under-5 mortality in Thailand and Vietnam have declined substantially to below 15 per 1000 livebirths within the past two decades, but the Philippines and Indonesia have seen a levelling off in rates to between 30 and 50 per 1000 livebirths. Myanmar, Cambodia, and Laos still have mortality levels of 50–70 per 1000 livebirths in 2008, which are similar to the rates of their neighbours from more than two decades ago, and rank among the highest for Asia.1
The UN estimates that every year about 350 000 women die as a result of pregnancy or childbirth,2 as do nearly 9 million children younger than 5 years.3 Worldwide, in 2008, about 18 000 maternal2 and 400 000 child3 deaths were in southeast Asia. Laos and Cambodia are among seven countries with the highest maternal mortality ratios outside of sub-Saharan Africa, and Indonesia is one of 11 countries that account for 65% of all maternal deaths worldwide.2 Although southeast Asia as a region might achieve the reductions in child mortality set by the UN Millennium Development Goal 4 (MDG4), Cambodia and Myanmar have been rated as having insufficient progress.4 Declines in mortality rates in Indonesia, Laos, and the Philippines are also faltering. Similarly, although all countries in the region are reporting declines in maternal deaths (towards MDG5), the rates of decline for Indonesia, the Philippines, and Myanmar have notably slowed.
Key messages.
-
•
Southeast Asia has sustained substantial reductions in maternal, neonatal, and child mortality since 1990, but this progress has been uneven. Mortality reductions in some countries have been the result of trajectories of rapid decline that started long before the Millennium Development Goals (MDGs) were developed in 1990. Others have succeeded in improving progress since the 1990s, but some countries continue to struggle.
-
•
Causes of death suggest a mortality transition in maternal deaths in the region. Child deaths are mainly attributable to the persistence of neonatal causes along with key preventable factors in the postneonatal period.
-
•
Disparities in intervention coverage are most acute in countries with the lowest intervention coverage overall.
-
•
Despite the variations in achievements, some countries are notable success stories. Suggested key factors include the ability to link maternal, neonatal, and child health interventions to broader health-system investments and to target access to rural and disadvantaged populations.
-
•
Increasing coverage to 60% will have a substantial effect on maternal deaths caused by unsafe abortion, hypertensive diseases, and postpartum haemorrhage and on neonatal deaths caused by pneumonia, sepsis, and birth asphyxia. Although there might not be quick solutions for maternal, neonatal, and child health in the region, coordinated expansion of proven effective interventions can contribute to improved reductions in mortality.
-
•
There is a need for stronger regional cooperation through the Association of Southeast Asian Nations to provide support to countries that need to accelerate progress to meet the MDGs.
Southeast Asia as a region has received little attention in recent efforts to revitalise and strengthen the policy agenda of the Partnership for Maternal, Newborn and Child Health, despite the complexity of national trends, including the substantial burden of morbidity and mortality in several countries and the existence of documented successes.5 As the economies of southeast Asia become more integrated with each other, there is an increasing need to assess and resolve the deficiencies in this agenda and to identify policy options for sustaining, if not accelerating, the pace of reduction in mortality.
Effective and affordable technology to reduce most maternal, neonatal, and child deaths is available,6, 7, 8, 9 so why has progress been so uneven? We focus on a region, collectively the ninth largest economy in the world, whose performance and achievements are often hidden by larger countries such as India or China, as well as by the UN agency groupings of the region that do not take into account historical and geopolitical ties within southeast Asia.10 In this paper, we critically review the region's achievements in reducing maternal and child mortality and highlight key factors that explain the successes and challenges in reaching these goals during competing worldwide, regional, and national health problems. We first report on patterns of mortality reduction within southeast Asia and major causes of maternal and child deaths in the context of MDG4 and MDG5. We investigate two country cases to highlight the notable variations in mortality reduction. Finally, we use an analysis of the deaths that could be averted through expanded coverage to identify more effective approaches for improving maternal, neonatal, and child health in southeast Asia.
Country-specific estimates on mortality rates
For the ten countries discussed in this paper, we reviewed estimates from national data sources and country Ministries of Health, as well as from the Demographic and Health Surveys and Multiple Indicator Cluster Surveys. We also reviewed estimates from international data sources from UNICEF, WHO, and the Institute for Health Metrics and Evaluation (webappendix pp 1–2). We present country-specific estimates on maternal, neonatal, and under-5 mortality rates from recent UN MDG reports,2, 3 as these estimates enable cross-country comparisons on trends in mortality using replicable estimation methods that reduce sources of non-sampling error. These estimates tend to be more conservative in the rate of decline than estimates from the Institute for Health Metrics and Evaluation. On the basis of increasing awareness of the burden of neonatal mortality, we sought comparable estimates of trends that separated neonatal (death within the first 28 days after birth) and postneonatal (death between 28 days and 1 year after birth) mortality. As UN models do not have neonatal time trends for all countries in the region, we report estimates from the Institute for Health Metrics and Evaluation.11 We report estimates on causes of neonatal and child deaths on the basis of standardised methods for estimating the distribution of causes of child deaths.12 We compiled estimates of causes of maternal deaths from Countdown 2015 country reports4 and WHO.13 We evaluated data from the Demographic and Health Surveys14 and Multiple Indicator Cluster Surveys15, 16 to assess existing intervention coverage within the region, with these data sources providing the ability to disaggregate coverage estimates by wealth quintile and rural or urban status17, 18, 19, 20 to establish the country average of coverage and to assess the programme coverage in disadvantaged populations by economic status and geography. We calculated regional estimates using country-level data from the specific source cited, unless otherwise indicated.
Analysis of the effect of interventions
To test the contribution of health-sector inputs to mortality reductions, we selected Thailand and Indonesia as case studies, as high (Thailand) and lower (Indonesia) achievers, and we focused on maternal and neonatal mortality as outcomes sensitive to health-system development. We used national data for these case studies to extend the analysis to the period before the MDG baseline year (1990).21, 22 We fitted data to a quadratic equation:
and to a linear equation:
to establish whether declines in maternal mortality could be attributed to programme changes or temporal trends, where MMR is the maternal mortality ratio and NMR is the neonatal mortality rate.
Using the Lives Saved Tool (LiST), we calculated potential deaths that could be averted through increasing population coverage of the interventions proven to be effective in reducing maternal, neonatal, and child mortality.23, 24 LiST operates within the Spectrum modelling platform, by the Futures Group, initially developed to project demographic change and complemented by modules to model the effect of family planning and HIV/AIDS interventions.25 The model yields estimates of deaths averted by cause and intervention for user-specified intervention coverage levels, based on inputs of demographic projections, numbers of maternal and child deaths, data on the distribution of deaths by cause, intervention effectiveness, and data on local health status.7, 26, 27, 28 The platform has been used previously for analysis of effect of intervention packages on maternal and child survival in South Africa29 and sub-Saharan Africa,30 but this is one of the first uses in southeast Asia. For this analysis, we assessed all the maternal, neonatal, and child health interventions included in LiST.31 The interventions and the estimates of their effectiveness are provided in webappendix pp 3–8. Values for the effectiveness of interventions were developed through a standardised review process using established criteria to identify which interventions to include on the basis of levels of evidence.31 The analysis was done for all ten countries and then for three subgroups of countries on the basis of observed patterns of mortality reduction: subgroup 1 (Brunei, Singapore, Malaysia, Thailand); subgroup 2 (the Philippines, Indonesia, Vietnam); and subgroup 3 (Laos, Cambodia, Myanmar). We assessed potential lives saved at three hypothetical coverage levels: 60%, 90%, and 99%.
Patterns of mortality reduction
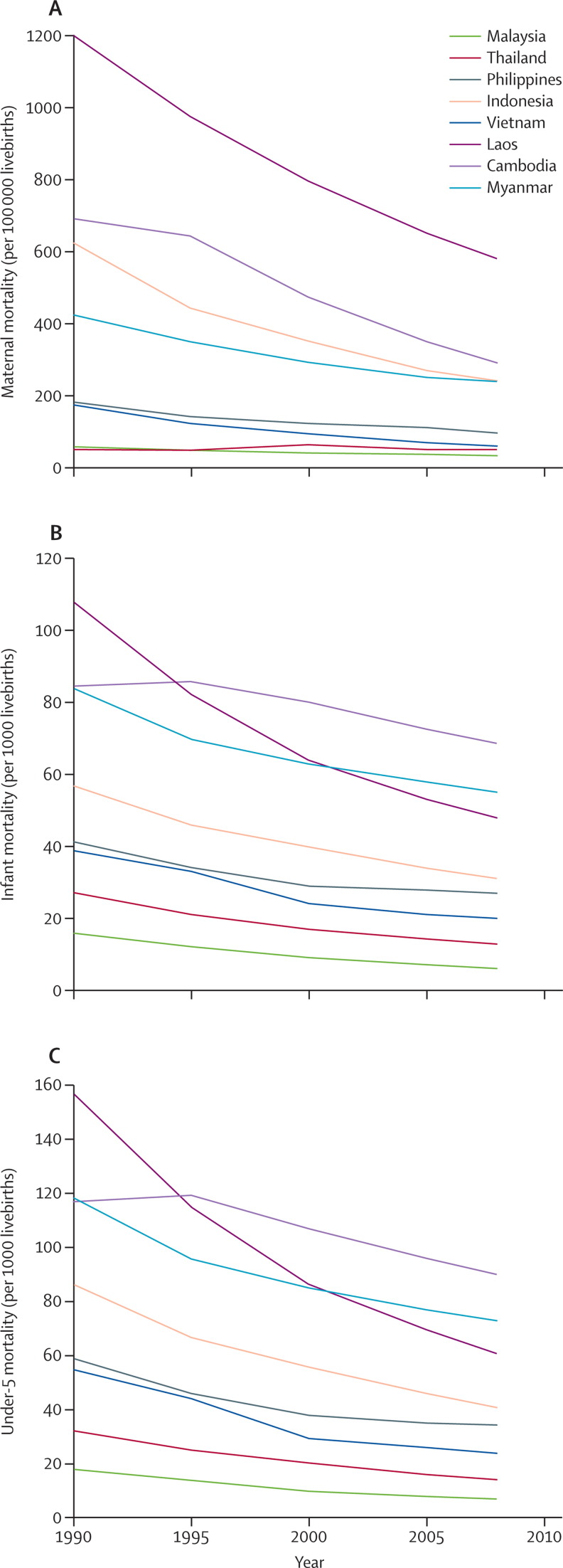
Reductions in maternal, infant, and child mortality in southeast Asia are indicative of the diversity of this region, presenting three divergent patterns (figure 1 , data not shown for Brunei and Singapore as these countries are considered to be more developed and where MDG goals might not be as relevant).10, 32 The first pattern reflects countries achieving low rates of mortality between 1990 (the MDG baseline year) and 2008 in Brunei, Singapore, Malaysia, and Thailand. In 1990, maternal mortality ratios in these countries were well below 100 per 100 000 livebirths, and infant and under-5 mortality rates were already at or below 20 per 1000 livebirths. These countries, the most economically advanced in the region, have also invested in their health systems over time.
Figure 1.
Trends in maternal (A), infant (B), and under-5 (C) mortality in southeast Asia (1990–2008)
A second, less distinct, pattern, seen in the Philippines, Indonesia, and Vietnam, starts with relatively high mortality rates and ratios in 1990, fairly large initial reductions (except for the maternal mortality ratio in Indonesia) that somewhat faltered after 2000 in Indonesia and the Philippines. By contrast, there were accelerated reductions in mortality in Vietnam during this period, with mortality rates and ratios beginning to come close to those of Thailand.
The third pattern, observed in Laos, Cambodia, and Myanmar has very high levels at the beginning of 1990, followed by sustained reductions from 1990 to 2005, with the exception of Cambodia's maternal mortality ratio.33 These three countries, which are on the UN list of least developed countries, continue to report high rates of maternal, infant, and child mortality.
Plotting maternal mortality reductions against gross national income per capita (webappendix p 9) indicates that, although countries with high maternal mortality achieved reductions in mortality as their gross national income per capita increased, some of the most notable declines in mortality took place earlier than the rapid rise in gross national income. The rapid reductions in maternal mortality in Thailand occurred before 1990. As maternal mortality declined to levels around 100, smaller reductions take place even as gross national income continues to improve. Similar patterns are evident for infant and under-5 mortality versus gross national income per capita plots (webappendix pp 10–11).
Neonatal and postneonatal mortality reductions
Separating infant mortality reduction between 1990 and 2010 into neonatal and postneonatal (webappendix p 12) indicates that the largest declines in infant mortality over time were mainly attributable to substantial postneonatal mortality reductions, as seen in Malaysia, Thailand, and Vietnam. The Philippines and Indonesia had reductions in neonatal and postneonatal mortality similar to that in Laos, Cambodia, and Myanmar. Although starting with comparably lower baseline mortality levels in 1990, rates of decline in the Philippines and Indonesia were not sufficiently accelerated since the development of the MDGs. Reductions in infant mortality in Brunei and Singapore stem from larger proportions of decline in neonatal deaths, a pattern similar to other high-income countries.34
Other than Brunei and Singapore, the slower rates of decline for neonatal mortality for the other eight of the ten ASEAN countries is a cause for concern. Interventions for reducing neonatal mortality are more closely linked to maternal interventions in terms of policy and programme implementation and might not be as noticeably tracked towards their effect on under-5 mortality. The Philippines, which is deemed to be on target for MDG4 in achieving reductions in child mortality,4 has the lowest reduction in neonatal mortality in the region—lower than that for Cambodia or Myanmar, which have been identified as having insufficient progress towards achieving MDG4.
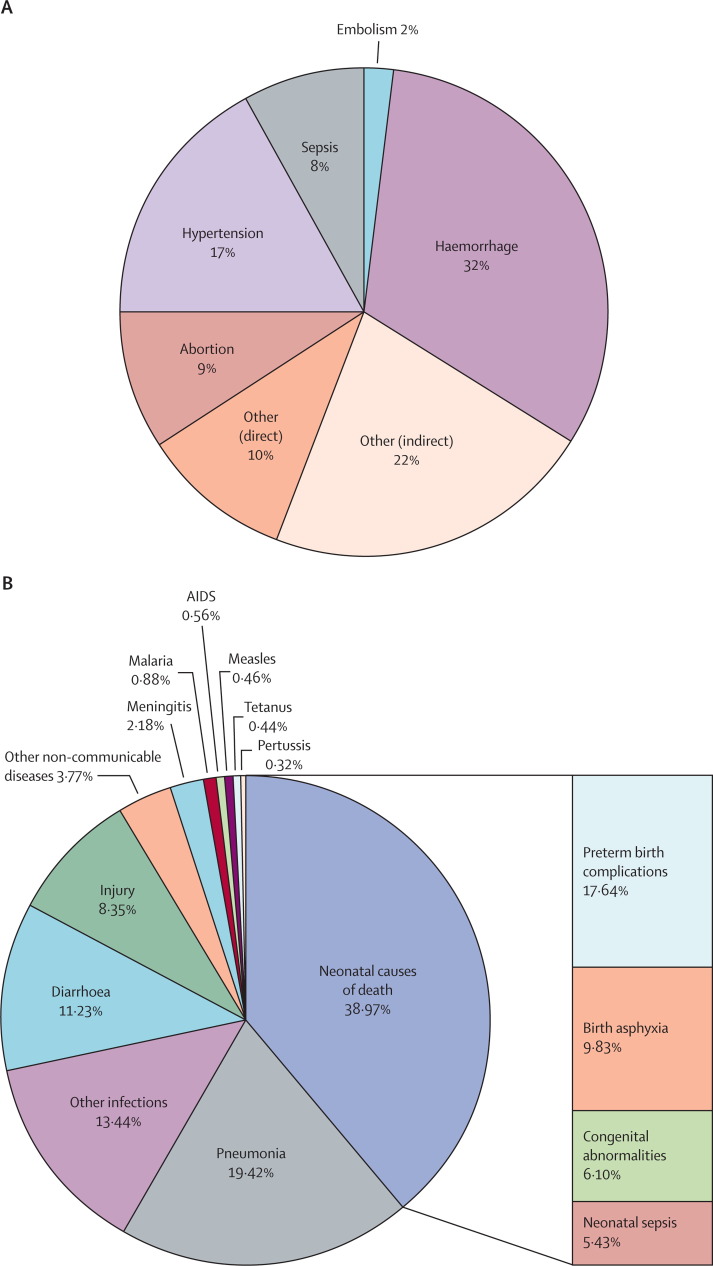
Causes of mortality
The distribution of maternal mortality causes (figure 2A ) is indicative of the substantial variations in health status and health-system development seen within the region. Haemorrhage is a leading cause of death, probably indicative of delays in attaining emergency obstetric care. Hypertensive disorders contribute to about one in every six maternal deaths in southeast Asia and suggest a different causal pathway more similar to that in developed country settings. The proportion of other indirect causes might indicate the still-substantial burden of infectious disease within the region and the effect of malaria and HIV on maternal health.33 Unsafe abortion is a factor in almost 10% of maternal deaths. These patterns reflect a causal transition in maternal mortality as the overall risk of maternal death declines and these causes will affect the extent to which interventions, both as single modalities or included in a package, can be predicted to avert deaths.13
Figure 2.
Causes of maternal (A) and child (B) deaths in southeast Asia
Data for maternal deaths are from UN MDG southeast Asia, 2010, including from ten ASEAN countries and Timor Leste (data not broken down to country level). Data for child deaths are from Black et al.12 ASEAN=Association of Southeast Asian Nations.
Different rates of reduction in child mortality can be attributed partly to variations in causes of death (figure 2B). Neonatal problems, such as preterm complications, contributed to about 40% of child mortality, accounting for the single largest proportion of preventable deaths, even as several ASEAN countries are successfully reducing their postneonatal and child mortality burdens. Infectious diseases, including pneumonia and diarrhoea, still account for almost half of the deaths in children, indicating substantial scope for continued reductions in child mortality.12
Within-country disparities in intervention coverage
Inequalities are substantial across countries in the region, but also within countries, as indicated by the current variation in intervention coverage by income and by rural or urban subgroups (webappendix pp 13–15). Disparities exist in antenatal care coverage, use of skilled birth attendance, and diphtheria, polio, tetanus, and measles vaccination together with use of oral rehydration therapy, which are all key to the development of a continuum of care.4, 8
With regard to overall programme coverage, Laos has a substantially lower coverage than that of other countries in the region and is far from a 60% coverage level, even for the wealthier groups. Antenatal care coverage is the most widespread, being close to or above 90%, in countries other than Laos and Cambodia, for the wealthier and urban areas. This disparity suggests that there is scope to effectively increase prenatal interventions that can avert maternal deaths. Vaccination coverage varies widely between and within countries, although several countries in the region are eligible for funds from the Global Alliance for Vaccines and Immunisation and have received substantial financial and policy support that is likely to lead to increases in vaccination coverage over time.
Laos and Cambodia have the greatest disparities in programme coverage. In Cambodia, vaccination levels for the wealthiest quintile are similar to those of the other southeast Asia countries, matching those of Indonesia's highest quintile. However, the coverage in the poorest households in Cambodia is almost 40% lower than that for the wealthiest households, resulting in a large equity gap in immunisation levels. The countries shown in the figures in webappendix pp 13–15 indicate relatively low coverage of skilled birth attendance (except Thailand and Vietnam) with inequality particularly acute in the Philippines, Laos, and Cambodia. Differences in skilled birth attendance between urban and rural Laotian populations are the largest among the six countries included in this comparison. Skilled birth attendance could be viewed as one indicator of broader health-system development, and the generally low coverage coupled with a high extent of inequality highlights the need for more comprehensive and coordinated health system improvements in the region overall.5 These patterns also point to the necessity of targeting the most vulnerable populations and maintaining attention to equity while increasing programme coverage.35
Case studies: Thailand and Indonesia
To understand potential determinants of mortality reduction, we look in more depth at two countries with different experiences of lowering mortality. The reduction in the maternal mortality in Thailand began in the 1960s (webappendix p 16) at a time when skilled birth attendants, mostly midwives, were systematically trained and deployed to community hospitals.36, 37, 38 At the time of Alma-Ata in 1978, Thailand's maternal mortality ratio was already below 200 and continued to drop even further in the 1980s as the economy improved and a health-care insurance programme for low-income populations was introduced along with specific safe motherhood interventions. Another round of health-system reforms and maternal, neonatal, and child health interventions were introduced in the early 2000s, including universal health coverage.
Coordinated health policy support through successive national plans provided a context and investments to stimulate structural, financial, and social capacities to deliver services, particularly in the district health system.21, 39, 40 Mandatory rural service for medical graduates provided a stable human resource base within community hospitals.36
Using a log linear model, no single programme could explain the decline in maternal mortality between 1960 and 1995, suggesting that the accelerated decline might be attributable to several developments. However, model fit after the 1997 economic crisis was not as good compared with earlier time periods. There was an increase in maternal mortality from 1997 to 2000, followed by a steady decline. This decline was in parallel with economic recovery and the introduction of universal health insurance coverage, the provincial Maternal and Child Health Board groups, the Healthy Thailand programme, and the Saiyairak programme.21, 39, 40 For this short period, assessment of the effect of any intervention programmes is difficult.
The systematic deployment of community-based health personnel took place in Indonesia41 about a decade later than in Thailand in the 1970s. Major, targeted, safe motherhood initiatives were introduced in the late 1980s, but by that time the maternal mortality ratio of Indonesia was about nine times higher than that of Thailand (webappendix pp 16–17).14, 22 A village midwife programme was implemented between 1989 and 1996, but the comparatively rapid training and deployment of 54 000 village midwives might have compromised quality of care.41
Access to care in Indonesia varies by rural or urban geography, income, and level of education. Unlike in Thailand, where the provision of skilled birth attendants was followed by increased facility and referral level capacities, in Indonesia not all health centres can provide basic obstetric care. About 40% of district hospitals do not have an obstetrician,41 indicating limited provision of the 24-h continuum of care necessary for dealing with emergency situations. A fragmented and devolved health system has challenged the capacity to sustain a comprehensive and concerted focus on maternal and child health.
Reductions in neonatal mortality (webappendix p 18) for the two countries mirror reductions in maternal mortality. Interventions to reduce neonatal mortality need more from health systems than either a maternal or child programme alone.34 In Thailand, neonatal interventions have been linked with maternal programmes,36, 39, 40 but this association has not been documented in Indonesia.
Maternal and neonatal mortality reductions in Thailand and Indonesia occurred in the context of rapid economic growth in both settings along with widespread increases in education levels and in sex equity.42 Although these factors might have affected levels of success, other determinants of mortality have been involved. Policy implementation in Thailand has been multi-sectoral, involving royalty and different ministries, including the National Health Security Office, which is responsible for health financing, especially universal coverage of health insurance. Investments in primary health care in the 1970s have led to benefits in the long term.5 However, geographic and demographic context also probably have a role. At the time of its rapid maternal mortality reduction in the 1970s, Thailand had a smaller, more circumscribed population compared with the larger and more dispersed Indonesian population, and this difference might have been an important factor in establishing physical access—a basic requirement for programme coverage.
LiST analysis
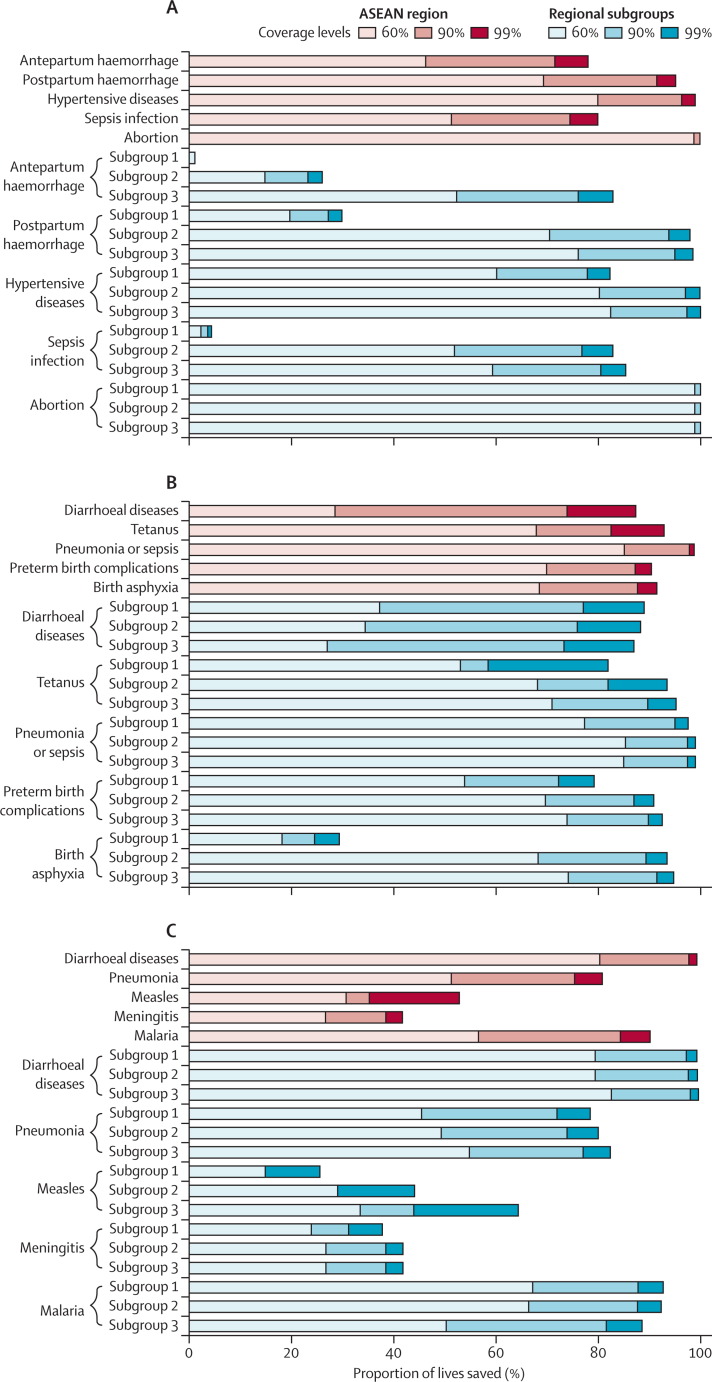
We investigated the potential effects of expanding programme coverage through a LiST analysis of the ASEAN region as a whole, and for subgroups on the basis of the mortality reduction patterns described earlier. We provide percentages rather than absolute numbers, as these estimates should be interpreted with caution in the context of local data.
The LiST analysis is under development as a measure for assessing and evaluating the benefits and limitations of interventions. Several of the interventions cited and used have been recently reviewed in depth25, 43 and used for regional estimates.44, 45 These estimates are the best point estimates for the effect of interventions, and, although these have been validated against actual observed mortality effects in the neonatal period,30 they still need prospective validation for programme-based effectiveness.
ASEAN regional averages are closer to those of subgroups 2 and 3 (as defined earlier), which consist of the bulk of the population and the higher mortality rates (figure 3A ). Although differences in maternal deaths averted across the groups are substantial, common trends across the region highlight crucial gaps. Expanding coverage of interventions for hypertensive disease in pregnancy and safe management of abortions, for example, will reduce maternal deaths substantially throughout the region, and addressing postpartum haemorrhage causes will largely reduce deaths for subgroups 2 and 3 but not subgroup 1.
Figure 3.
Maternal (A), neonatal (B), and child (C) deaths averted at 60, 90, and 99% coverage of interventions for the ASEAN region and regional subgroups as defined by mortality reduction patterns
Subgroup 1=Brunei, Singapore, Malaysia, and Thailand; subgroup 2=the Philippines, Indonesia, and Vietnam; and subgroup 3=Laos, Cambodia, and Myanmar. ASEAN=Association of Southeast Asian Nations.
Counterpart calculations were made for neonatal and child mortality (figure 3B and C). Interventions for birth asphyxia are more likely to avert deaths in subgroups 2 and 3 than in subgroup 1. The high proportion of neonatal and child deaths averted through interventions for infectious diseases in all subgroups is indicative that infectious disease remains a challenge for the region as a whole.12, 46
To focus on universal coverage, which is receiving greater attention in other health-policy settings,47 we report the deaths that could be averted at 99% programme coverage. At the regional level, universal basic obstetric care coverage will save about one in five mothers (table ), but with universal comprehensive obstetric care coverage, more than half of maternal deaths would be averted. Almost all these lives saved would be in subgroups 2 and 3 for which current levels of coverage for these services are low (webappendix pp 13–15). Because there is already good access to basic and comprehensive obstetric care for subgroup 1, the deaths averted from these interventions are minimal. By contrast, basic postabortion case management will save a higher proportion of mothers in subgroup 1 but more deaths will actually be averted in subgroups 2 and 3. The fewer lives saved in subgroup 1 with comprehensive abortion versus basic abortion care might be because the access to comprehensive obstetric care that could be used for abortion management in this group is already high.
Table.
Percentage of deaths averted with 99% coverage of selected interventions for the ASEAN region and for subgroups, as defined by mortality reduction patterns
| Level of evidence* | Subgroup 1 | Subgroup 2 | Subgroup 3 | ASEAN region | |
|---|---|---|---|---|---|
| Maternal deaths averted (%) | |||||
| Basic emergency obstetric care (clinic) | Moderate | 0·05 | 19·4 | 21·5 | 19·0 |
| Comprehensive emergency obstetric care | High | 1·6 | 55·1 | 55·6 | 52·9 |
| Basic postabortion case management | Moderate | 8·8 | 5·8 | 5·8 | 5·9 |
| Comprehensive postabortion case management | High | 12·1 | 6·5 | 6·5 | 6·7 |
| Neonatal deaths averted (%) | |||||
| Basic emergency obstetric care (clinic) | Moderate | 0·03 | 11·7 | 17·2 | 12·8 |
| Comprehensive emergency obstetric care | Moderate | 0·1 | 22·8 | 31·1 | 24·1 |
| Antenatal corticosteroids for preterm labour | High | 7·3 | 20·1 | 17·2 | 18·5 |
| Kangaroo care | Moderate | 20·3 | 20·6 | 16·8 | 19·4 |
| Child (including postneonatal) deaths averted (%) | |||||
| Use of safe water connection in the home | Moderate | 3·1 | 13·4 | 11·3 | 12·3 |
| Pneumococcal vaccine | High | 2·9 | 9·8 | 7·6 | 8·7 |
| Pneumonia case management (oral antibiotics) | High | 5·7 | 19·0 | 15·9 | 17·4 |
| Zinc for diarrhoea treatment | High | 1·2 | 5·0 | 3·9 | 4·4 |
Examples were selected for cases in which interventions might make the biggest differences and that indicate an approach to the use of LiST analysis. Level of evidence based on Grading of Recommendations Assessment, Development and Evaluation (GRADE) assessment using the Child Health Epidemiology Reference Group (CHERG) methods.23, 28 Subgroup 1=Brunei, Singapore, Malaysia, and Thailand; subgroup 2=the Philippines, Indonesia, and Vietnam; and subgroup 3=Laos, Cambodia, and Myanmar. ASEAN=Association of Southeast Asian Nations.
Universal basic obstetric care will avert about one in five neonatal deaths in subgroup 3, whereas comprehensive obstetric care will save almost twice as many lives as basic care will for the region as a whole, but particularly for subgroups 2 and 3. However, even at 99% coverage the maximum proportion of neonates that could be saved with either of these interventions does not go beyond a third of deaths, indicating the need for other interventions such as those that take into account prematurity through antenatal steroids and providing Kangaroo care.48
Interventions directed towards infectious diseases such as diarrhoea and pneumonia will, likewise, affect postneonatal and child deaths mostly in subgroups 2 and 3. A small but noticeable effect on death in subgroup 1 might also be apparent when coverage increases to 99%. Preventive measures such as improving access to safe water can contribute substantially to mortality reduction, averting more deaths than would pneumococcal vaccination in all the subgroups.
Conclusions
Despite substantial improvements in maternal, neonatal, and child health since 1990, most notably in Malaysia, Thailand, and Vietnam, high mortality, poor coverage, and high inequity continue to challenge other countries in the region, such as Laos, Cambodia, and Myanmar. Improvements in the first three countries seem to be attributable to socioeconomic progress and a consistent policy focus on maternal and child health programmes and coordinated health-system components,49, 50, 51 notably a stable and strategically deployed health workforce coupled with supportive finance mechanisms in Malaysia and Thailand. The importance of favourable health systems is highlighted by the case study in Thailand, which indicates that mortality reductions have taken place at modest levels of economic growth and that no single factor or intervention could account for these reductions. The case study in Indonesia indicates how similar interventions used in a setting with different system capacities and geopolitical features can result in different outcomes.
Thus, although the LiST analysis can estimate the potential effect of interventions given with maximum levels of coverage, the case studies caution us that improving health outcomes is not just about increasing the amount of money spent on health. Instead, targeted and sustained interventions to reduce the barriers that prevent the most vulnerable population groups from accessing the interventions they crucially need should be ensured in the long term. For example, the LiST analysis indicates that providing basic and comprehensive emergency obstetric care has the potential to avert half of all maternal deaths and about one in six neonatal deaths in Laos, Cambodia, and Myanmar. However, prevention of these deaths might be possible only if care coverage is rapidly expanded in low-income and rural populations, possibly through sustained donor investments, given the low levels of domestic health spending. In the Philippines and Indonesia, the two most populous countries in the region, regaining momentum in mortality reduction alongside substantial geographic and cultural access challenges might mean improving access to services through more equitable financing schemes.47
Despite the varying agendas that countries of the region might need to adopt to complete the unfinished maternal, neonatal, and child health agenda, our findings indicate important areas of common ground. Many key interventions to reduce child deaths have been implemented at the community level throughout southeast Asia, but necessary health-service investments that will enable the countries of the region to reduce maternal and neonatal deaths have yet to be fully considered. Access to safe abortion services and management of hypertensive disorders during pregnancy will prevent maternal deaths from these causes from Brunei to Myanmar. Similarly, all countries in the region recognise space for expanding coverage of crucial neonatal interventions to prevent preterm births and neonatal deaths from infection.
Our study has several limitations. We have used estimates of mortality reduction from UN agencies that might not match national estimates and that use different methods; however, these estimates are preferred for cross-country analysis. These estimates for southeast Asia are still mainly derived from household surveys and subject to potential error from under-reporting and misclassification of deaths. Only five of the ten countries discussed have vital registration systems, and not all these systems have valid registration of causes of death.2 There is an acute need for better data in Laos and Myanmar, particularly on maternal mortality, but the pioneering work in maternal death audits in Malaysia provides a potential model for the region.52
The selection of data sources was mainly affected by the availability of comparable, reliable data across all the ASEAN countries. For example, although we used the more inclusive gross national income per capita for webappendix pp 9–11, this measurement was not consistently available for the case studies, hence the use of gross domestic product for Thailand and Indonesia.
We were not able to disaggregate LiST estimates into relevant national subgroups by wealth or by rural or urban status. This non-separation is important because the poor populations are likely to have higher mortality rates and lower levels of intervention coverage than the wealthier groups, which could affect estimates.43 Data limitations restricted our ability to develop this analysis, even as a test case. We have also not analysed the costs involved in extending coverage, which we hope to develop in a future study.
Since its formation in 1967, ASEAN has positioned itself as an important hub for economic and socio-cultural cooperation. Infectious diseases have thus far commanded much of ASEAN's attention in health matters. Recently, regional focus has begun to shift to other health issues. The ASEAN Strategic Framework on Health Development 2010–2015,53 which focuses on access to health-care services in addition to communicable diseases and pandemic preparedness, has also gained regional support.
Given the economic vigour of ASEAN, regional cooperation in health might be key to motivating less-developed members to focus on maternal, neonatal, and child health. The pivotal role of ASEAN in stimulating and channelling international financial aid to tsunami-devastated Indonesia in 2004 and cyclone-stricken Myanmar in 2008 testifies to the power of this promise—the goodwill and experience of working with each other in disaster situations can be harnessed for the health and wellbeing of mothers and children in the region.54, 55
But how should this aid be used? The experience of the ASEAN, as discussed in this paper, suggests that effective interventions to curb maternal and child mortality need to be deployed to actively target the disadvantaged populations who are most affected by unsafe abortion, hypertensive diseases, postpartum haemorrhage, pneumonia, sepsis, and birth asphyxia. Far from expecting coverage of these programmes to passively diffuse to the very poor, governments must innovatively combine health interventions with non-health programmes such as micro-finance schemes and conditional cash transfer mechanisms that have proven successful in other settings.56, 57
Achievement of the MDGs worldwide will not happen without individual country efforts. As the donor community focuses its attention on the burdens of Africa and south Asia, ASEAN countries must provide support to each other. Examples of such support mechanisms already in place include financial cooperation through the ASEAN surveillance process, which is an early warning system to keep track of macroeconomic trends and to provide early detection of any adverse development. For public health, the ASEAN SARS Containment Information Network exemplifies how member countries share essential information, best practices, and new findings for severe acute respiratory syndrome. However, ASEAN has yet to develop initiatives for maternal, neonatal, and child health, which could be developed through sharing information and best practices (possibly starting by resolving the absence of comparable data across countries); financial cooperation efforts could be linked to outcomes, and the attainment of MDGs for member countries behind target could be made an ASEAN priority.
Search strategy and selection criteria
We searched the Demographic and Health Surveys (Cambodia 2000 and 2005; Indonesia 1987, 1991, 1994, 2002–03, and 2007; Philippines 1993, 1998, 2003, and 2008; and Vietnam 1997 and 2002),14 Multiple Indicators Cluster Surveys,15, 16 data banks of regional and global finance institutions such as the Asian Development Bank and the World Bank,17, 18, 19, 20, 32 the Millennium Development Goals surveillance data sources4 and publications of the UN agencies, mainly UNICEF,3, 15 and WHO1, 2, 40 from 1960 to October, 2010. We used the following search terms: “Asia”, “Asia and Pacific”, “Southeast Asia”, “SEA”, “Association of Southeast Asian Nations”, and “ASEAN” (for geographic location); “Cambodia”, “Indonesia”, “Lao PDR”, “Laos”, “Malaysia”, “Myanmar”, “Philippines”, “Thailand”, and “Vietnam” (our countries of interest); “(maternal OR child OR neonatal) AND (health OR health care)”, “(health OR mortality) AND (pregnancy OR pregnant)”, and “(health OR mortality) AND (maternal OR neonatal OR infant OR child OR under 5 years” (for health conditions); “health systems”, “health financing”, “leadership”, “governance”, “information systems”, “delivery and organization of services”, “regulation of health products”, “human resources” (for health systems); “maternal mortality ratio”, “infant mortality rate”, “neonatal mortality rate”, “under 5 mortality rate”, “skilled birth attendance”, “antenatal care”, “prenatal care”, “immunization”, “maternal and child nutrition”, and “causes of maternal, infant and child mortality” (for mortality and health programme indicators); and “gross domestic product”, “GDP”, “GDP per capita”, “national health accounts”, “NHA”, “public and private health expenditures”, and “(out-of-pocket OR OOP) health expenditures” (for finance). These data are complemented by nationally representative data and international journal publications. Specific country data were further verified and updated by members of the writing team. We also searched PubMed from 1960 to October, 2010, for peer-reviewed journals for pertinent articles on maternal and child health and the region, and cross-referenced WHO, UNICEF, the World Bank, and the Asian Development Bank. No initial language exclusion was applied in searching; for full-text papers, English and the languages of the authors (Thai, Bahasa, Malay, Chinese, Filipino, and Burmese) were used.
Acknowledgments
Acknowledgments
This paper is part of a Series funded by the China Medical Board, Rockefeller Foundation, and Atlantic Philanthropies. The authors thank the following individuals for their assistance: Virasakdi Chongsuvivatwong, Edward McNeil (Epidemiology Unit, Faculty of Medicine, Prince of Songkla University, Thailand), Marian Valera, Bryan Lim, Joan Javellana-Ottao (University of the Philippines, National Institutes of Health), and Arjumand Rizvi (Aga Khan University, Pakistan).
Contributors
CSA, RF, GLK, TTH, TL, and EA contributed to the conception, design, and acquisition of data for the first draft. TL, EA, and GLK contributed to the acquisition, analysis, and interpretation of data for the case studies. ZB, RF, and CSA contributed to the acquisition, analysis, and interpretation of data for the LiST analysis. CSA and RF were responsible for the overall analysis and interpretation of data. All authors contributed to the drafting and critical review of the paper.
Conflicts of interest
CSA is employed by the University of the Philippines, National Institutes of Health and has received consultancy fees from projects with the Philippine government, UNICEF, United States Agency for International Development, and WHO Regional Office for the Western Pacific. GLK has received consultancy fees from the Institute of Gerontology, Universiti Putra Malaysia, International Life Sciences Institute SEA, SEAMEO TROPMED Regional Centre for Community Nutrition, and is employed by the International Medical University, Malaysia. All other authors have no conflicts of interest.
Web Extra Material
References
- 1.WHO . World health statistics 2010. World Health Organization; Geneva: 2010. [Google Scholar]
- 2.WHO . Trends in maternal mortality: 1990–2008. World Health Organization; Geneva: 2010. [Google Scholar]
- 3.UNICEF Levels and trends in child mortality, Report 2010. Estimates developed by the UN Inter-agency Group for Child Mortality Estimation. United Nations Children's Fund, 2010. http://www.unicef.gr/pdfs/UNICEF_Levels_and_Trends_in_Child_mortality.pdf (accessed Nov 22, 2010).
- 4.Countdown to 2015. Maternal, Newborn and Child Health. 2010 country profiles. http://www.countdown2015mnch.org/reports-publications/2010-country-profiles (accessed May 12, 2010).
- 5.Rohde J, Cousens S, Chopra M. 30 years after Alma-Ata: has primary health care worked in countries? Lancet. 2008;372:950–961. doi: 10.1016/S0140-6736(08)61405-1. [DOI] [PubMed] [Google Scholar]
- 6.Campbell OMR, Graham WJ, Lancet Maternal Survival Series steering group Strategies for reducing maternal mortality: getting on with what works. Lancet. 2006;368:1284–1299. doi: 10.1016/S0140-6736(06)69381-1. [DOI] [PubMed] [Google Scholar]
- 7.Darmstadt GL, Bhutta ZA, Cousens S, Adam T, Walker N, de Bernis L, Lancet Neonatal Survival Steering Team Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet. 2005;365:977–988. doi: 10.1016/S0140-6736(05)71088-6. [DOI] [PubMed] [Google Scholar]
- 8.Kerber KJ, de Graft-Johnson JE, Bhutta ZA, Okong P, Starrs A, Lawn JE. Continuum of care for maternal, newborn, and child health: from slogan to service delivery. Lancet. 2007;370:1358–1369. doi: 10.1016/S0140-6736(07)61578-5. [DOI] [PubMed] [Google Scholar]
- 9.Bhutta ZA, Ali S, Cousens S. Interventions to address maternal, newborn, and child survival: what difference can integrated primary health care strategies make? Lancet. 2008;372:972–989. doi: 10.1016/S0140-6736(08)61407-5. [DOI] [PubMed] [Google Scholar]
- 10.Chongsuvivatwong V, Phua KH, Yap MT. Health and health-care systems in southeast Asia: diversity and transitions. Lancet. 2011 doi: 10.1016/S0140-6736(10)61507-3. published online Jan 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rajaratnam J, Marcus J, Flaxman A. Neonatal, postnatal, childhood, and under-5-mortality for 187 countries, 1970–2010: a systematic analysis of progress towards Millennium Development Goal 4. Lancet. 2010;375:1988–2007. doi: 10.1016/S0140-6736(10)60703-9. [DOI] [PubMed] [Google Scholar]
- 12.Black R, Cousens S, Johnson H. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375:1969–1987. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 13.Khan KS, Wojdyla D, Say L, Gülmezoglu AM, Van Look PFA. WHO analysis of causes of maternal death: a systematic review. Lancet. 2006;367:1066–1074. doi: 10.1016/S0140-6736(06)68397-9. [DOI] [PubMed] [Google Scholar]
- 14.Measure DHS. Demographic and Health Surveys. http://www.measuredhs.com (accessed April 27, 2010).
- 15.UNICEF Multiple Indicator Cluster Surveys. UNICEF. http://www.childinfo.org/mics.html (accessed July 4, 2010).
- 16.National Statistics Office Monitoring the situation of children and women. Thailand multiple indicator cluster survey December 2005–February 2006 Final Report. http://www.unicef.org/thailand/MICS_Final_Report2.pdf (accessed Sept 20, 2010).
- 17.Gwatkin D, Rutstein S, Johnson K, Suliman E, Wagstaff A, Amouzou A. Socio-economic differences in health, nutrition, and population in Cambodia. The World Bank; Washington, DC: 2007. [PubMed] [Google Scholar]
- 18.Gwatkin D, Rutstein S, Johnson K, Suliman E, Wagstaff A, Amouzou A. Socio-economic differences in health, nutrition, and population in Indonesia. The World Bank; Washington, DC: 2007. [PubMed] [Google Scholar]
- 19.Gwatkin D, Rutstein S, Johnson K, Suliman E, Wagstaff A, Amouzou A. Socio-economic differences in health, nutrition, and population in the Philippines. The World Bank; Washington, DC: 2007. [PubMed] [Google Scholar]
- 20.Gwatkin D, Rutstein S, Johnson K, Suliman E, Wagstaff A, Amouzou A. Socio-economic differences in health, nutrition, and population in Vietnam. The World Bank; Washington, DC: 2007. [PubMed] [Google Scholar]
- 21.Bureau of Policy and Strategy, Ministry of Public health . In: Thailand Health Profile 2005–2007. Wibulpolprasert S, editor. The War Veterans Organization of Thailand Printing Press; Bangkok: 2007. http://www.moph.go.th/ops/thp/index.php?option=com_content&task=view&id=6&Itemid=2&lang=en (accessed Nov 22, 2010). [Google Scholar]
- 22.Ministry of Health, Indonesia. National Health Surveys 1980–2008. Jakarta, Indonesia.
- 23.Plosky WD, Stover J, Winfrey B. The Lives Saved Tool. A computer program for making child and maternal survival projections. UNICEF. 2009. http://www.jhsph.edu/bin/i/x/list_manual.pdf (accessed Nov 22, 2010).
- 24.Department of International Health LiST: The Lives Saved Tool—an evidence-based tool for estimating intervention impact. Johns Hopkins University. http://www.jhsph.edu/dept/ih/IIP/list/index.html (accessed Oct 30, 2010).
- 25.Stover J, McKinnon R, Winfrey B. Spectrum: a model platform for linking impact of maternal and child survival intervention with AIDS, family planning and demographic projections. Int J Epidemiol. 2010;39(suppl 1):i7–i10. doi: 10.1093/ije/dyq016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jones G, Steketee RW, Black RE, Bhutta ZA, Morris SS. The Bellagio Child Survival Study Group. How many child deaths can we prevent this year? Lancet. 2003;362:65–71. doi: 10.1016/S0140-6736(03)13811-1. [DOI] [PubMed] [Google Scholar]
- 27.Bhutta ZA, Ahmad T, Black RE, for the Maternal and Child Undernutrition Study Group What works? Interventions for maternal and child undernutrition and survival. Lancet. 2008;371:417–440. doi: 10.1016/S0140-6736(07)61693-6. [DOI] [PubMed] [Google Scholar]
- 28.Boschi-Pinto C, Young M, Black RE. The child health epidemiology reference group reviews of the effectiveness of interventions to reduce maternal, neonatal and child mortality. Int J Epidemiol. 2010;39(suppl 1):i3–i6. doi: 10.1093/ije/dyq018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chopra M, Daviaud E, Pattinson B, Fonn S, Lawn JE. Saving the lives of South Africa's mothers, babies, and children: can the health system deliver? Lancet. 2009;374:835–846. doi: 10.1016/S0140-6736(09)61123-5. [DOI] [PubMed] [Google Scholar]
- 30.Friberg IK, Kinney MV, Lawn JE. Sub-Saharan Africa's mothers, newborns, and children: how many lives could be saved with targeted health interventions? PLoS Med. 2010;7:e1000295. doi: 10.1371/journal.pmed.1000295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Walker N, Fischer-Walker C, Bryce J, Bahl R, Cousens S, CHERG Review Groups on Intervention Effects Standards for CHERG reviews of intervention effects on child survival. Int J Epidemiol. 2010;39(suppl 1):i21–i31. doi: 10.1093/ije/dyq036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.World Bank World Development Indicators database. http://siteresources.worldbank.org/DATASTATISTICS/Resources/GNIPC.pdf (accessed Sept 27, 2010).
- 33.Hogan M, Foreman K, Naghavi M. Maternal mortality for 181 countries, 1980–2008: a systematic analysis of progress towards Millennium Development Goal 5. Lancet. 2010;375:1609–1623. doi: 10.1016/S0140-6736(10)60518-1. [DOI] [PubMed] [Google Scholar]
- 34.Lawn JE, Cousens S, Zupan J, Lancet Neonatal Survival Steering Team 4 million neonatal deaths: When? Where? Why? Lancet. 2005;365:891–900. doi: 10.1016/S0140-6736(05)71048-5. [DOI] [PubMed] [Google Scholar]
- 35.Boerma JT, Bryce J, Kinfu Y, Axelson H, Victora CG, Countdown 2008 Equity Analysis Group Mind the gap: equity and trends in coverage of maternal, newborn and child health services in 54 Countdown countries. Lancet. 2008;371:1259–1267. doi: 10.1016/S0140-6736(08)60560-7. [DOI] [PubMed] [Google Scholar]
- 36.Wibulpolprasert S. Community financing: Thailand experience. Health Policy Plan. 1991;6:354–360. [Google Scholar]
- 37.Van Lerberghe W, De Brouwere V. Of blind alleys and things that have worked: history's lessons on reducing maternal mortality. Studies Health Serve Organ Policy. 2001;17:7–33. [Google Scholar]
- 38.Bureau of Policy and Strategy. Ministry of Public Health . Health policy in Thailand. Ministry of Public Health; Nonthaburi: 2009. http://bps.ops.moph.go.th/webenglish/Health%20Policy%209.pdf (accessed Nov 22, 2010). [Google Scholar]
- 39.Pramualratana P, Wibulpolprasert S. Health insurance systems in Thailand. Health System Research Institute; Nonthaburi: 2002. http://ihppthaigov.net/publication/attachbook/92/chapter3.pdf (accessed Nov 22, 2010). [Google Scholar]
- 40.SEARO WHO. Improving maternal, newborn and child health in the South-East Asia Region. Data source: Basic indicators: health situation in south-east Asia, World Health Organization, South-East Asia Region, 2004.
- 41.Azwar A. Evolution of safe-motherhood policies in Indonesia. Initiative for Maternal Mortality Programme Assessment (IMMPACT), Country Co-ordinating Group & Technical Partners Meeting, Aberdeen, UK, January 2004.
- 42.Gakidou E, Cowling K, Lozano R, Murray CJL. Increased educational attainment and its effects on child mortality in 175 countries between 1970 and 2009: a systematic analysis. Lancet. 2010;376:959–974. doi: 10.1016/S0140-6736(10)61257-3. [DOI] [PubMed] [Google Scholar]
- 43.Victora CG. Commentary: LiST: using epidemiology to guide child survival policymaking and programming. Int J Epidemiol. 2010;39(suppl 1):i1–i2. doi: 10.1093/ije/dyq044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bryce J, Friberg I, Kraushaar D. LiST as a catalyst in program planning: experiences from Burkina Faso, Ghana and Malawi. Int J Epidemiol. 2010;39(suppl 1):i40–i47. doi: 10.1093/ije/dyq020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hazel E, Gilroy K, Friberg I. Comparing modelled to measured mortality reductions: applying the Lives Saved Tool to evaluation data from the Accelerated Child Survival Programme in West Africa. Int J Epidemiol. 2010;39(suppl 1):i32–i39. doi: 10.1093/ije/dyq019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Coker RJ, Hunter BM, Rudge JW, Liverani M, Hanvoravongchai P. Emerging infectious diseases in southeast Asia: regional challenges to control. Lancet. 2011 doi: 10.1016/S0140-6736(10)62004-1. published online Jan 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tangcharoensathien V, Patcharanarumol W, Ir P. Health-financing reforms in southeast Asia: challenges in achieving universal coverage. Lancet. 2011 doi: 10.1016/S0140-6736(10)61890-9. published online Jan 25. [DOI] [PubMed] [Google Scholar]
- 48.Victora CG, Rubens CE, the GAPPS Review Group Global report on preterm birth and stillbirth (4 of 7): delivery of interventions. BMC Pregnancy Childbirth. 2010;10(suppl 1):S4. doi: 10.1186/1471-2393-10-S1-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Limwattananon S, Tangcharoensathien V, Prakongsai P. Equity in maternal and child health in Thailand. Bull World Health Organ. 2010;88:420–427. doi: 10.2471/BLT.09.068791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.UN Country Team Malaysia Malaysia, Successes and challenges, Kuala Lumpur: United Nations Development Programme. 2005. http://www.undp.org.my/mdgs/malaysia-mdg-report (accessed Nov 22, 2010).
- 51.Health Policy and Strategy Institute Measuring health systems performance in Vietnam: results from eight provincial health systems assessments. http://www.healthsystems2020.org/content/resource/detail/2515/ (accessed Sept 25, 2010).
- 52.Abu Bakar S, Mathews A, Jegasothy R, Ali R, Kandiah N. Strategy for reducing maternal mortality. Bull World Health Organ. 1999;77:190–193. [PMC free article] [PubMed] [Google Scholar]
- 53.Association of Southeast Asian Nations Joint Statement of the 10th ASEAN Health Ministers Meeting Singapore. 22 July 2010. http://www.aseansec.org/24938.htm (accessed Oct 30, 2010).
- 54.ASEAN Regional Programme for Disaster Management A regional strategy for disaster reduction. http://www.aseansec.org/18455.htm (accessed Nov 22, 2010).
- 55.Tripartite Core Group; the Government of the Union of Myanmar. the United Nations. and the Association of Southeast Asian Nations Post-Nargis Joint Assessment (PONJA) July 2008. http://www.aseansec.org/21765.pdf (accessed Nov 22, 2010).
- 56.Ahmed MU, Islam SK, Quashem A, Ahmed N, CGAP Working Group on Microinsurance Health microinsurance: a comparative study of three examples in Bangladesh. Good and Bad Practices. 2005 case study 13. [Google Scholar]
- 57.Fiszbein A, Schady N, Ferreira F. Conditional cash transfers: reducing present and future poverty. The World Bank; Washington, DC: 2009. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.