Summary
Background
Ministers of health, donor agencies, philanthropists, and international agencies will meet at Bamako, Mali, in November, 2008, to review global priorities for health research. These individuals and organisations previously set health priorities for WHO, either through its regular budget or extra-budgetary funds. We asked what insights can be gained as to their priorities from previous decisions within the context of WHO.
Methods
We compared the WHO biennial budgetary allocations with the burden of disease from 1994–95 to 2008–09. We obtained data from publicly available WHO sources and examined whether WHO allocations varied with the burden of disease (defined by death and disability-adjusted life years) by comparing two WHO regions—Western Pacific and Africa—that are at differing stages of epidemiological transition. We further assessed whether the allocations differed on the basis of the source of funds (assessed and voluntary contributions) and the mechanism for deciding how funds were spent.
Findings
We noted that WHO budget allocations were heavily skewed toward infectious diseases. In 2006–07, WHO allocated 87% of its total budget to infectious diseases, 12% to non-communicable diseases, and less than 1% to injuries and violence. We recorded a similar distribution of funding in Africa, where nearly three-quarters of mortality is from infectious disease, and in Western Pacific, where three-quarters of mortality is from non-communicable disease. In both regions, injuries received only 1% of total resources. The skew towards infectious diseases was substantially greater for the WHO extra-budget, which is allocated by donors and has risen greatly in recent years, than for the WHO regular budget, which is decided on by member states through democratic mechanisms and has been held at zero nominal growth.
Interpretation
Decision makers at Bamako should consider the implications of the present misalignment of global health priorities and disease burden for health research worldwide. Funds allocated by external donors substantially differ from those allocated by WHO member states. The meeting at Bamako provides an opportunity to consider how this disparity might be addressed.
Funding
None.
Introduction
Bamako 2008, which will bring together ministers of health, science, and development from across the world, provides an opportunity to reassess global priorities for health research.1 Previous research into the allocation of funding for international development has identified three sources of priorities—recipient need, donor interests,2 and an exchange process by which specific ideas emerge in policy forums involving state and non-state participants and, through the interchange of ideas and preferences, are either dismissed or amplified.3 Evidence suggests that all these factors have a role in allocation of funding.
This process does not necessarily lead to the best possible allocation of resources. In one study comparing expenditure on individual communicable diseases with the burden of disease that they represent, the investigators noted that some diseases seem to be funded very generously whereas others seem to be neglected.4 This situation is self-sustaining. Donors and international agencies develop expertise in an area and, in the absence of unexpected events (such as the emergence of AIDS in the 1980s), they tend to continue providing funding as they have done in the past.
In the 4 years since these ministers last met in Mexico City to discuss global health priorities,5 many changes have arisen in both the threats to global health and in our understanding of them. Climate change and migration issues are now clearly on the global health agenda, as is the crucial importance of health-system strengthening as a prerequisite for delivering essential interventions. Another change is the increased recognition of the importance of non-communicable diseases, which were once thought to be largely the preserve of high-income countries but are now increasing in developing countries.6 Within this group of diseases, the extent of ill-health attributable to mental disorders is also, belatedly, attracting attention.
The pace and scale of these changes mean that the ministers attending Bamako 2008 will have much to discuss. But will their discussions lead to a real change in priorities? Funding for health research is often embedded within programmes addressing specific disorders. Expecting, for example, the Global Fund to fight AIDS, Tuberculosis and Malaria or GAVI alliance (formerly The Global Alliance for Vaccines and Immunization) to start funding research on diabetes or schizophrenia is unreasonable. Priorities for health research will continue mainly to be driven by broader global health priorities. To what extent have these health priorities adapted to the changing global situation?
Ideally, we would relate trends in total global expenditure on research to the burden that is attributable to different categories of disease. However, this approach is not possible for many reasons, including the vast diversity of research funders that are active in the health sector worldwide, each with their own accounting systems. As a result, several definitional problems arise, such as how to differentiate research within budgets and how to allocate expenditure to disease categories. Instead, we adopt a revealed preference approach, comparing allocations within the budget of WHO, which are decided by its member states (including both donor and recipient countries) acting through the World Health Assembly—a uniquely representative organisation, providing a forum for 193 governments to influence the global health agenda—with WHO's extra-budgetary resources, which are established by a much smaller group of donors (including governments of rich countries and philanthropists).7
We focus on the budget of WHO because, although it is only one of many sources of funds for global health and research, it has an important normative role. Furthermore, unlike many state and non-state donors, it has a global perspective and covers all aspects of human health. For both these reasons it provides a unique opportunity to understand the priority that is given to different disease categories worldwide.
Because the ministers and non-state bodies that affect the use of the WHO's regular and extra-budgetary funds will make up most participants at Bamako 2008, we believe that, unless conscious steps are taken to bring about change, the health priorities that underpin WHO's budget will probably be the same as those that will shape the health research priorities emerging from Bamako.
We focus on one of these emerging issues—non-communicable diseases. The growing importance of these diseases is undisputed. Health ministers have raised more than 40 resolutions on non-communicable disease at the World Health Assembly in recent decades. In 1996, a WHO committee examining priorities for research and development emphasised the need to direct increased investment at the challenge of non-communicable diseases8 whereas, 9 years later, WHO published what amounted to a call to action, drawing attention to the growing human and economic toll that these disorders create.9 In 2007, the World Health Assembly endorsed a global strategy on prevention and control of non-communicable diseases,10 after two major initiatives to tackle the determinants of these diseases—the Framework Convention on Tobacco Control11 and the Global Strategy on Diet, Physical Activity and Health.12 Subsequently, a series in The Lancet described a range of inexpensive interventions that could be scaled up to control non-communicable diseases.13, 14 In 2008, WHO endorsed a non-communicable disease action plan at the 61st World Health Assembly.15 But has this rhetoric been translated into a financial reality at WHO? If not, to do so will need a special effort by those who have contributed to the current situation to ensure that health research is more closely aligned with health needs when they meet at Bamako.
The aim of our study was to assess whether, the extent to which, and under what circumstances WHO's budget has responded to the burden of non-communicable disease.
Methods
Study design and data sources
We used WHO budget data to examine the distribution of health funds against the burden of disease for the budget cycles from 1994–95 to 2008–09 (a list of sources of WHO budget data is available from the corresponding author on request). Data for the global burden of disease were taken from the WHO World Health Report 200416 and from Mathers and Loncar's 2006 global burden of disease projections.17 We quantified burden of disease with use of deaths and disability-adjusted life years (DALYs), which provide an aggregate measure of years of life lost because of disability and premature death. The data sources and detailed calculations of these measures are described elsewhere.18 In brief, in this Article we used the WHO's three broad categories of International Classification of Diseases (ICD) codes that are used in the Global Burden of Disease project. Infectious disease refers to the type-I group of communicable, maternal, perinatal, and nutritional disorders (although not exclusively infectious diseases, these are overwhelmingly dominant, accounting for roughly four-fifths of this category, expressed both as burden of disease and WHO expenditure); non-communicable disease refers to the type-II cluster of chronic disorders; and injuries and violence consist of WHO's type-III cluster (WHO, 2004).
The table summarises how WHO's so-called areas of work, or aggregated budget lines, from the financial reports were matched to each of the infectious disease, chronic disease, and injury and violence burden of disease clusters. We identified 14 budget lines for infectious diseases, five for non-communicable diseases, and one for injuries and violence. For disease clusters such as nutrition and food safety that might have applied to infectious or non-communicable disease, we analysed the descriptions of the work in the WHO programme budget to identify the appropriate disease cluster. Webtables 1 and 2 provide more details of the disease classification.
Table.
Classification of WHO budget lines according to disease classification, 2006–07
| Budget lines | Percentage of total WHO budget | |
|---|---|---|
| Infectious disease | Communicable disease prevention and control, communicable disease research, epidemic alert and response, malaria, tuberculosis, HIV/AIDS, nutrition,* food safety, reproductive health, making pregnancy safer, child and adolescent health, immunisation and vaccine development, essential medicines, essential health technologies | 56·2% |
| Non-communicable disease | Surveillance, prevention, and management of chronic, non-communicable diseases; health promotion;† mental health and substance misuse; tobacco; health and environment† | 7·6% |
| Injuries and violence | Violence, injuries, and disabilities | 0·6% |
| Non-disease specific | Gender, women, and health; policy making for health in development; health system policies and service delivery; human resources for health; health financing and social protection; health information; evidence and research policy; emergency preparedness and response; WHO's core presence in countries; knowledge managements and information technology; planning, resource coordination, and oversight; human resources management in WHO; budget and financial management; infrastructure and logistics; governing bodies; external relations; direction | 35·6% |
WHO 2006 mid-term budget review (pages 57 and 64) describes this money related to group I causes (WHO 2006 mid-term budget review available at http://whqlibdoc.who.int/hq/2007/WHO_PRP_07.3_eng.pdf).
Details for health promotion and for health and environment available from WHO 2006 mid-term budget review (pages 44–47 and 58–61, respectively). Webtable 1 further disaggregates budget lines and funds allocated in 2006–07.
Roughly two-thirds of WHO's budget data were set aside for specific diseases in 2006–07. For areas of the budget in which diseases or risk factors were not specified, such as policy making in health and development, we assumed that the same distribution across disease clusters would apply as was noted with the disease-specific areas of work.
We undertook three subanalyses to characterise the relationship between WHO allocations and disease burden. First, we disaggregated the three broad disease clusters into more refined categories to plot WHO budget areas against their associated mortality and DALY burden. We then separately examined the budget in two WHO regions: the African region covering the African continent (apart from some countries bordering the Mediterranean); and the Western Pacific region, covering countries such as China, Australia, and the Pacific Islands. Because Africa has a high infectious disease and low non-communicable disease burden, and the Western Pacific has a low infectious disease and high non-communicable disease burden, we expected a substantially greater proportion of the budget for the Western Pacific region to be allocated to non-communicable diseases than in the African region.
Second, we investigated whether the WHO budget allocations varied according to the source of funds. WHO receives funds in two ways: from assessed contributions and voluntary contributions. Each of these sources is allocated in a different way. For assessed contributions, WHO member states deliberate at the World Health Assembly until a consensus is reached about how the money should be spent and a resolution approving the budget is passed unanimously. WHO member states pledge to commit a specified proportion of the total assessed contributions, which is calculated according to each country's wealth and population size. Conversely, voluntary contributions are allocated to programmes according to the preferences of the donors involved. Together, these two sources of funds constitute the WHO regular budget and its extra-budgetary funds, respectively. Third, because the low-income and middle-income member states, which are the main recipients of WHO funds, have a much greater role in determining the regular budget than the extra-budgetary health priorities, we compared whether the distribution of the regular budget more closely aligned with the burden of disease than did the extra-budgetary allocations.
In all cases, we used data from the latest available year of the WHO financial reports and the WHO global burden of disease estimates.
Role of the funding source
No funding was involved in this study. All authors had full access to all the data in the study (which are publicly available) and had final responsibility for the decision to submit for publication.
Results
In 2006–07, WHO allocated 87% of its total budget to infectious diseases, 12% to non-communicable diseases, and less than 1% to injuries and violence.
We next disaggregated the broad disease clusters using the budget groups that could be matched to the burden of disease in terms of numbers of deaths and DALYs. The available disease-specific groups included malnutrition; malaria; tuberculosis; injuries; HIV/AIDS; child and maternal causes; communicable diseases excluding HIV/AIDS, tuberculosis, and malaria; and non-communicable diseases. Webtable 2 further describes the budget groups that corresponded to each disease.
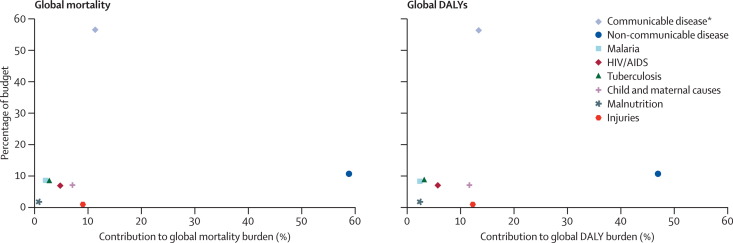
Figure 1 shows that WHO funds and disease burden were not correlated in 2004–05, irrespective of whether measured in terms of mortality or DALYs. Three-fifths of WHO funds were spent on communicable diseases excluding HIV, tuberculosis, and malaria, which accounted for roughly 11% of global mortality. Conversely, non-communicable disease accounted for more than half of global mortality and almost half of global DALYs, but received roughly a tenth of all WHO funds. We recorded a similar disparity with injuries, which claimed 9% of global mortality and 12% of global DALYs, but received less than 1% of global funds.
Figure 1.
Relation between WHO budget allocations and the global burden of disease, 2004–05
Data for global mortality and disability-adjusted life years (DALY) are from the WHO Global Burden of Disease, 2002 edition. DALYs are the sum of years of life lost because of premature mortality and years of life lost because of disability. *Communicable diseases excluding HIV, tuberculosis, and malaria.
Further inspection of the WHO budget showed that the resources used for communicable diseases excluding HIV, tuberculosis, and malaria were mainly driven by WHO extra-budgetary funds for immunisation and vaccine development. WHO's regular budget allocated US$14·3 million to this area of work, corresponding to 6% of WHO's regular budget. By contrast, WHO's extra-budgetary funds allocated $512·4 million, roughly 36 times as much as in the regular budget, corresponding to about 30% of WHO's extra-budgetary allocations for infectious disease control.
Although Bamako 2008 is a conference about the global health research agenda, it does explicitly focus on Africa, which is justifiable in view of the scale of both poverty and disease in that continent. For the same reason, international development assistance understandably concentrates on Africa and, within it, on the leading causes of disease. However, other regions worldwide still have a substantial burden of poverty and disease, although less than that in Africa. One such region is the Western Pacific region as defined by WHO, where almost three-quarters of all deaths are attributable to non-communicable diseases. In Africa, the burden of disease is almost the reverse: less than a quarter of mortality is from non-communicable diseases, and roughly three-quarters is from infectious diseases. Does WHO allocate a substantially greater fraction of the available funds to non-communicable diseases in the Western Pacific region than in the African region?
Figure 2 shows the distribution of WHO's budgetary allocations across the three major burden of disease clusters in the African and Western Pacific regions in 2004–05. In both regions, the resources were heavily skewed toward infectious diseases. In the African region, infectious diseases received almost all funds, with non-communicable diseases and injuries receiving very small proportions of the overall funds allocated by WHO to the region. The trend for the Western Pacific region was nearly the same (figure 2).
Figure 2.
Relation between WHO budget allocations and the burden of disease in Africa and Western Pacific regions
WHO allocations are from 2004–05 budget cycle. Data for global mortality and disability-adjusted life year (DALY) are from the WHO Global Burden of Disease, 2002 edition. DALYs are the sum of years of life lost because of premature mortality and years of life lost because of disability. Data do not equal 100% because of rounding errors.
To further investigate whether the recorded mismatch between the disease burden and allocated funds can be attributed to the differential allocation of assessed contributions, which are decided on by member states, and voluntary contributions, which are determined by donors, we compared the distribution of each.
WHO's budget has nearly doubled in recent years, from $2·3 billion in 2000–01 to $4·2 billion in 2008–09, with almost all the growth occurring in WHO's extra-budgetary funds, which have risen from 25% of the budget in 1971 to more than 75% in 2008. Much of this growth has been driven by increasing funding from countries from the Organisation for Economic Co-operation and Development (OECD) and, in recent years, from private philanthropic foundations, such as the Bill & Melinda Gates Foundation. Since these foundations have increased the contribution to WHO's budget, the private for-profit sector's direct contribution to WHO's extra-budgetary funds has dropped substantially, from 5% in 2000–01 to less than 1% in 2006–07.
Figure 3 shows the sources of WHO's extra-budgetary funds in 2006–07. Most funds come from member states, and, as shown in webtable 3, more than four-fifths of this money is donated by high-income countries that are not substantial recipients of the funds. Of the other sources, the three highest contributors were the UN, the Bill & Melinda Gates Foundation, and the European Commission, together contributing half the funds from sources other than those received directly from member states (the first and last of these contributors are essentially conduits for funds from member states). 15 years ago, direct funding by member states accounted for roughly four-fifths of extra-budgetary funds. Nowadays that amount has fallen to 40%, with the greatest rises coming from UN organisations (21% in 2006–07 versus 5% in 1992–93) and public and private foundations such as the Gates Foundation and Rotary International (15% in 2006–07).7 Webtable 3 shows the ten member states and the ten non-member states that contributed the most to WHO's extra-budgetary funds.
Figure 3.
WHO budget sources, 2006–07
The WHO regular budget is assessed from member states on the basis of country wealth and population size and allocated by all member states. The WHO extra-budget comes from voluntary contributions and is allocated by the donors themselves. Data are from the mid-term A60/30 report and Director-General Reports in 2006 and 2008. Sources for WHO financial data are available from the author on request. NGOs=non-governmental organisations.
As noted earlier, whether funds from the regular budget and extra-budgetary funds are allocated differently can provide important insights into the priorities of different decision makers. WHO's regular budget was much more closely aligned with the actual global burden of disease than were the extra-budgetary funds. Of WHO's regular budget, 61% of funds were allocated to infectious diseases, whereas 38% were allocated to non-communicable diseases and roughly 1% to injuries. Of the WHO's extra-budgetary funds, 91% went to infectious disease, 8% to non-communicable disease, and about 1% to injuries. In both cases, injuries received a substantially lower share than would be expected from the amount of mortality and disability that they cause (see webappendix 1 for more details of trends in WHO extra-budget allocations).
Discussion
Our analysis of the WHO budget has shown several disparities. First, the health priorities expressed by the world's health ministries—through their decisions at the World Health Assembly about WHO's regular budget, and those of the international donor community, which are expressed by the international donor community through its contributions to WHO's extra-budgetary funds—give greater weight to a death from an infectious disease than to one from a non-communicable disease. Deaths from injuries are given even less weight. Second, and very importantly, the regular budget of WHO is actually more closely aligned with the burden of disease than are extra-budgetary funds. The regular budget indicates the views of all countries whereas extra-budgetary funds are driven by the wealthy donor countries, industry, and philanthropists. The obvious implication is that extra-budgetary funds are misaligned with the health needs of the main recipients of WHO's activities.
Our analysis has several important limitations. First, we assumed that several of the areas of WHO's work that were not associated with specific diseases, such as emergency preparedness and response, reflected the distribution of funds to areas that were defined by specific diseases. However, after we inspected the descriptions in the WHO workplans of how the funds within these areas were spent, we believe that our calculations of the resources provided for communicable diseases are conservative. When we used different assumptions about the distribution of funds within these non-disease-specific areas, the overall patterns that we recorded did not change.
Second, we took the current burden of disease as our basis for comparison. Clearly, other factors are also important. One is the potential for rapid spread or economic effect. These considerations obviously apply to diseases such as severe acute respiratory syndrome (SARS) and avian influenza, thus justifying expenditure on them even though the current burden of disease attributable to them is zero for SARS and negligible for avian influenza from a global perspective. Some other infectious diseases share this potential, such as cholera, but most do not, either because they are limited geographically by the distribution of vectors or other factors, or because effective control programmes are already in place. Another consideration is the economic burden of disease. The WHO Commission on Macroeconomics and Health drew attention to the economic effects of the common diseases afflicting the poorest countries in sub-Saharan Africa, which are dominated by infections.19 However, evidence is growing for the substantial economic consequences of non-communicable diseases.20, 21 The diseases do not seem to differ substantially with regard to their effect on the economy.
Furthermore, a range of factors also need to be considered in prioritising health resources that are not directly related to health. For example, funding for HIV/AIDS has clearly benefited from the existence of powerful advocates in developed countries in a way that diseases such as filariasis or schistosomiasis have not. Funding for measures to combat bioterrorism are also part of a broader geopolitical agenda. However, although arguably idealistic, it is reasonable to argue that such considerations should play less of a part in organisations such as WHO.
A third limitation is that we have used available data for the global burden of disease that, for most low-income and middle-income countries, are based on estimates. Growing evidence from sentinel surveillance sites suggests that the burden of non-communicable diseases is somewhat greater than was previously thought.6, 22, 23 Inaccurate assessments of the true burden of disease could skew the allocations made by decision makers. However, this underreporting for our analysis would mean that WHO allocations are even more misaligned with the true burden than our data suggest.
Finally, we are using data for allocation of resources for health in general to infer the preferences that are likely to underpin the debate about priorities for health research at Bamako. However, the aim is not to produce an accurate estimate of the existing distribution of funds for health research but rather to enable those involved in priority setting to engage in an informed debate about the consequences of decisions that they have made previously, and to consider whether they feel that these consequences reflect their intentions.
In the future, analysis of WHO's budget priorities will become increasingly difficult because, similar to other international organisations, it has introduced new international accounting standards, shifting from cash accounting to an accrual accounting. It has also combined injuries and non-communicable diseases together in its work plans. Structural breaks in recording such as these complicate comparisons over time.
Despite these limitations, our findings are robust when the analyses are repeated with use of different measures of disease burden, including years of healthy life lost and years of potentially productive life years lost (data not shown), as well as premature mortality and years of life lost because of disability (webappendix 2). The pattern is consistent in regions of the world that have a quite different burden of disease, in this case Africa and the Western Pacific, providing further evidence that the health prioritisation process is driven by factors other than need.
We provide here a picture of the real health priorities of decision makers. True commitment can only be judged by the decision to spend money. Although the past few years have seen a series of high-profile statements seeming to prioritise non-communicable diseases—including the decision, for the first time ever, to invoke WHO's treaty-making powers to tackle the epidemic of tobacco-related disease—these statements have only resulted in a small shift in resources. These findings are relevant to the discussions that will take place at Bamako. Obviously, identification of priorities for research differs in important aspects from that for deciding on health policy. It would be inappropriate for global health priorities to be driven solely by the burden of disease, and a need for cross-cutting work—eg, on strengthening health systems—clearly exists. Yet equally, the appropriateness of whether global health priorities and the burden of disease should be so misaligned needs to be considered. The same principle holds for health research. Many of those present at Bamako will, entirely justifiably, be advocating for greater support for what they consider to be the most important diseases, which risks perpetuating the status quo.
Research needs to be undertaken on how to prevent and manage non-communicable diseases in resource-poor settings. Research in rich countries has identified the core principles involved, but solutions cannot simply be transposed to poor countries.24 For example, although the principles of managing type 1 diabetes in childhood are well known, many health systems remain unable to provide even the most basic care that is needed to allow children affected by this disease to survive.25 However, this tenet should not be seen as an argument for a rapid shift in priorities. In many countries there would simply be insufficient absorptive capacity. Instead, sustained investment in the capacity to undertake and implement research is needed, with South–South partnerships (ie, between institutions in developing countries) when possible.
In this Article we have sought to shed some light on the results of previous decisions made by those who will be at Bamako. We hope that this analysis will be useful as they look to the future.
Contributors
DS conceived the idea for the paper and developed it in discussions with MM, HR, and LK. HR collected the data, and HR and DS analysed the data. DS prepared the initial draft, which was revised by MM and commented on by HR and LK.
Conflict of interest statement
As of October, 2008, MM is chair of WHO's European Advisory Committee on Health Research, in which capacity he will be attending the Bamako conference. All other authors declare that they have no conflict of interest.
Web Extra Material
Trends in WHO extra-budgetary allocations, from 2000–01 to 2008–09
Replications with alternative burden of disease metrics
Classification of WHO areas of work by disease cluster in 2006–07
Classifications of areas of work and disease categories, 2004–05 (used in figure 1)
Sources of WHO extra-budgetary contributions, 2006–07
References
- 1.Ijsselmuiden C, Matlin SA, Maïga AH, on behalf of the Steering Committee of the 2008 Global Ministerial Forum on Research for Health From Mexico to Mali: a new course for global health. Lancet. 2008;371:91–93. doi: 10.1016/S0140-6736(08)60080-X. [DOI] [PubMed] [Google Scholar]
- 2.Maizels A, Nissanke MK. Motivations for aid in developing countries. World Dev. 1984;12:879–900. [Google Scholar]
- 3.Keck ME, Sikkink K. Activists beyond borders: advocacy networks in international politics. Cornell University Press; Ithaca, NY: 1998. [Google Scholar]
- 4.Shiffman J. Donor funding priorities for communicable disease control in the developing world. Health Policy Plan. 2006;21:411–420. doi: 10.1093/heapol/czl028. [DOI] [PubMed] [Google Scholar]
- 5.WHO Report from the Ministerial Summit on Health Research, Mexico City, November, 2004: 16–20. http://www.who.int/rpc/summit/en/index7.html (accessed May 27, 2008).
- 6.Tollman SM, Kahn K, Sartorius B, Collinson MA, Clark SJ, Garenne ML. Implications of mortality transition for primary health care in rural South Africa: a population-based surveillance study. Lancet. 2008;372:893–901. doi: 10.1016/S0140-6736(08)61399-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vaughan JP, Mogedal S, Stein-Erik K, Lee K, Walt G, de Wilde K. Financing the World Health Organization: global importance of extra-budgetary funds. Health Policy. 1996;35:229–245. doi: 10.1016/0168-8510(95)00786-5. [DOI] [PubMed] [Google Scholar]
- 8.Godal T, Jamison DT, Tulloch J. Investing in health research and development. WHO; Geneva: 1996. [Google Scholar]
- 9.WHO . Preventing chronic diseases: a vital investment. World Health Organization; Geneva: 2005. [Google Scholar]
- 10.WHO . World Health Assembly 53.17. Global strategy on prevention and control of non-communicable diseases. World Health Organization; Geneva: 2000. [Google Scholar]
- 11.WHO . Framework Convention on Tobacco Control. World Health Organization; Geneva: 2003. http://www.who.int/tobacco/framework/en/ (accessed Sept 12, 2008). [Google Scholar]
- 12.WHO . Global Strategy on Diet, Physical Activity and Health. 57th World Health Assembly. World Health Organization; Geneva: 2004. http://www.who.int/gb/ebwha/pdf_files/WHA57/A57_R17-en.pdf (accessed Oct 6, 2008). [Google Scholar]
- 13.Asaria P, Chisholm D, Mathers C, Ezzati M, Beaglehole R. Chronic disease prevention: health effects and financial costs of strategies to reduce salt intake and control tobacco use. Lancet. 2007;370:2044–2053. doi: 10.1016/S0140-6736(07)61698-5. [DOI] [PubMed] [Google Scholar]
- 14.Lim SS, Gaziano TA, Gakidou E. Prevention of cardiovascular disease in high-risk individuals in low-income and middle-income countries: health effects and costs. Lancet. 2007;370:2054–2062. doi: 10.1016/S0140-6736(07)61699-7. [DOI] [PubMed] [Google Scholar]
- 15.WHO . Prevention and control of noncommunicable diseases: implementation of the global strategy: report by the Secretariat to the 61st World Health Assembly. World Health Organization; Geneva: 2008. [Google Scholar]
- 16.WHO . World Health Report—changing history. World Health Organization; Geneva: 2004. http://www.who.int/whr/2004/en/ (accessed Sept 12, 2008). [Google Scholar]
- 17.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Murray CJL, Salomon JA, Mathers CD, Lopez AD, editors. Summary measures of population health: concepts, measurements, ethics, and applications. WHO; Geneva: 2002. [Google Scholar]
- 19.WHO Commission on Macroeconomics and Health, Macroeconomics and health: investing in health for economic development, report of the Commission on Macroeconomics and Health, chaired by Jeffrey Sachs. Commission on Macroeconomics and Health; Geneva: 2001. [Google Scholar]
- 20.Suhrcke M, McKee M, Sauto Arce R, Tsolova S, Mortensen J. The contribution of health to the economy in the European Union. European Commission; Brussels: 2005. [DOI] [PubMed] [Google Scholar]
- 21.Stuckler D. Population causes and consequences of leading chronic diseases: a comparative analysis of prevailing explanations. Milbank Q. 2008;86:273–326. doi: 10.1111/j.1468-0009.2008.00522.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thorogood M, Connor M, Tollman S, Hundt G Lewando, Fowkes G, Marsh J. A cross-sectional study of vascular risk factors in a rural South African population: data from the Southern African Stroke Prevention Initiative (SASPI) BMC Public Health. 2007;7:326. doi: 10.1186/1471-2458-7-326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bovet P, Ross AG, Gervasoni JP. Distribution of blood pressure, body mass index and smoking habits in the urban population of Dar es Salaam, Tanzania, and associations with socioeconomic status. Int J Epidemiol. 2002;31:240–247. doi: 10.1093/ije/31.1.240. [DOI] [PubMed] [Google Scholar]
- 24.McKee M, Ricciardi W. Towards Bamako: a European perspective on the global health research agenda. Eur J Public Health. 2008;18:107–108. doi: 10.1093/eurpub/ckm115. [DOI] [PubMed] [Google Scholar]
- 25.Beran D, Yudkin JS, de Courten M. Access to care for patients with insulin-requiring diabetes in developing countries: case studies of Mozambique and Zambia. Diabetes Care. 2005;28:2136–2140. doi: 10.2337/diacare.28.9.2136. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trends in WHO extra-budgetary allocations, from 2000–01 to 2008–09
Replications with alternative burden of disease metrics
Classification of WHO areas of work by disease cluster in 2006–07
Classifications of areas of work and disease categories, 2004–05 (used in figure 1)
Sources of WHO extra-budgetary contributions, 2006–07