Abstract
The authors assessed the risks of drug-related death, suicide, and homicide after release from New York City jails in 155,272 people who were incarcerated anytime from 2001 through 2005 and examined whether the mortality rate was associated with homelessness. Using jail records matched with death and single-adult homeless registries in New York City, they calculated standardized mortality ratios (SMRs) and relative risks. After adjustment for age, sex, race, and neighborhood, the risks of drug-related death and homicide in formerly incarcerated persons were 2 times higher than those of New York City residents who had not been incarcerated in New York City jails during the study period. These relative risks were greatly elevated during the first 2 weeks after release (for drug-related causes, SMR = 8.0, 95% confidence interval (CI): 5.2, 11.8; for homicide, SMR = 5.1, 95% CI: 3.2, 7.8). Formerly incarcerated people with histories of homelessness had higher rates of drug-related death (RR = 3.4, 95% CI: 2.1, 5.5) and suicide (RR = 2.1, 95% CI: 1.2, 3.4) than did persons without such histories. For individuals who died of drug-related causes, longer jail stays were associated with a shorter time until death after release. These results suggest that jail- and community-based interventions are needed to reduce the excess mortality risk among formerly incarcerated people.
Keywords: cause of death, homeless persons, mortality, urban population
Several studies have shown a high risk of death due to drug overdose, suicide, or homicide among former inmates who had recently been released from prisons (1–4). Some researchers have implicated loss of physiologic tolerance to drugs as a contributing factor to overdose (1, 3, 5). Decreased tolerance due to the limited availability of drugs during incarceration may increase the risk of fatal overdose after release (1, 6). Other investigators have suggested that community reentry hurdles could contribute to this excess risk (7, 8).
Despite evidence of an elevated risk of death in inmates after release from prisons, little is known about the risk of death among people released from jails, which release almost 10 times as many people as do prisons annually in the United States (7, 9–11). The risk of death from selected causes might be different for people released from jails rather than prisons because jails house people charged with (or convicted of) less serious crimes for shorter periods of time than do prisons. In addition, people incarcerated in jails have a high likelihood of entering homeless shelters after release (12, 13). The cycle is associated with substance use and mental illness, which are risk factors for premature death (12, 13). Finally, previous studies have not accounted for incomes or neighborhoods of residence. Most people in jail come from low-income neighborhoods, a fact that might independently affect mortality risk. The purpose of the present study was to assess the risks of suicide, homicide, and drug-related deaths after release from New York City (NYC) Department of Correction jails, especially immediately after release, and to examine how homelessness influenced these risks.
MATERIALS AND METHODS
Study population
This retrospective cohort study included people who were 16–89 years of age and spent at least 1 night during an incarceration in a NYC Department of Correction jail from January 1, 2001, through December 31, 2005 (n = 244,298). Analyses were restricted to 200,493 people who were released from NYC jails into the community. Individuals with missing residence information (n = 45,213) were excluded to allow us to conduct analyses that accounted for potential confounding by neighborhood effects. We excluded 7 people because their death was before their last discharge date, and yet they were not on the list of people known to have died in jail. Further, we excluded 1 person for whom we were missing the last discharge date. The final data set contained 155,272 people. This study was determined by the NYC Department of Health and Mental Hygiene Institutional Review Board to be an epidemiologic investigation not subject to institutional board review.
Data sources and matching procedures
In the present study, we matched jail records to records of death and single-adult homeless shelter use that occurred in 2001–2005 using the NYC Department of Health and Mental Hygiene Vital Statistics registry and the NYC Department of Homeless Services single-adult homeless registry. We performed probabilistic matching of these databases using QualityStage software (IBM Corporation, Armonk, New York). The likelihood that records from different registries described the same person was estimated based on agreement or disagreement of key variables, including first and last name, birth date, sex, and Social Security Number; this likelihood was denoted as a weight. We reviewed a randomly selected sample of potential matches and reached consensus on the threshold weight above which all potential match sets were accepted as true matches.
Study variables
Using death records, we defined the underlying cause of death for each decedent using codes from the International Classification of Diseases, Tenth Revision (14) as follows: for suicide, codes X60–X84 and X87.0; for homicide, codes X85-Y09 and Y87.1; and for drug-related death, codes F11-F16, F18-F19, X40-X42, and X44. People released from jail who died from any other cause of death (59% of all deaths; chronic diseases, n = 269; infectious diseases, n = 265; and other, n = 142) were censored at the time of death, as our study focused on external causes of death. From 1991 through 2006, most accidental drug-related deaths were misclassified as death due to chronic drug use. Thus, we combined “mental and behavioral disorders due to psychoactive substance abuse” with “accidental poisoning by the use of psychoactive substances, excluding alcohol and tobacco” to form a single category of “deaths due to drug use” (14).
We reviewed jail records for demographic and incarceration characteristics of persons included in the study. To describe the periods of incarceration, we used the cumulative number of days spent in jail (≤4 vs. ≥5 days), the frequency of incarceration (1 vs. ≥2 times), and 2 types of criminal charges: violent crimes (e.g., assault, murder, harassment, resisting arrest, and hazing) and drug-related crimes (e.g., drug sales and possession). We defined 42 NYC neighborhoods using the United Hospital Fund’s designations, which aggregate adjoining zip codes (15), and categorized neighborhoods into low-, middle-, and high-income groups based on the tertiles of the percentage of residents living below 200% of the federal poverty level according to the US Census 2000 (15, 16). We also used data from the Department of Homeless Services to include a variable that indicated at least 1 night spent in a NYC single-adult homeless shelter in 2001–2005.
Statistical analysis
Person-years at risk of death after incarceration.
Person-years were calculated to account for the amount of time at risk of death from selected causes. For people who had been released from jail, we defined person-years as the total number of days in the study period during which they were not incarcerated during 2001–2005, including days between each discharge and the subsequent incarceration, the end of the study period, or death. To approximate person-years for NYC residents who had not been incarcerated in NYC jails during 2001–2005 (hereafter referred to as nonincarcerated NYC residents), we multiplied the NYC population counts from the US Census 2000 by 5 (16) and subtracted the total person-years of formerly incarcerated people. The US Census count was used to represent the estimated aggregate populations in 2001–2005 because intercensal estimates were not available for persons who were 16 years of age or 85–89 years of age.
Mortality rates.
We calculated mortality rates by dividing the number of deaths by the number of person-years. To calculate the number of deaths among nonincarcerated NYC residents, we subtracted the total number of deaths among formerly incarcerated people from the total number of deaths among NYC residents within each age, sex, race, and neighborhood category.
Standardized mortality ratio and multivariate regression analysis.
We calculated standardized mortality ratios (SMRs) to examine the relative risk of death between formerly incarcerated people and nonincarcerated NYC residents. Multiplying age-, sex-, race-, and neighborhood-specific rates of death for nonincarcerated NYC residents by the person-years of formerly incarcerated people in corresponding strata yielded the expected number of deaths. SMR was the ratio of the observed number of deaths to the expected number of deaths. Because SMR was derived from stable mortality rates of NYC residents, a small number of deaths would not affect its reliability (2, 17). We used the Poisson method to compute 95% confidence intervals for SMRs.
Using data from the cohort of formerly incarcerated persons only, we performed 3 Poisson regression analyses to test the associations between mortality rates and demographic characteristics, the incarceration experience, and/or the use of homeless shelters. Variables were included in the models based on their associations with death among former prisoners (1–4). To account for under- and overdispersion, which produce erroneous standard errors, we adjusted the 95% confidence interval for the relative risk using the Pearson chi-squared coefficient divided by the degrees of freedom as an estimate of the dispersion parameter. We performed additional multivariate analyses to test whether decreased drug tolerance could contribute to a fatal overdose. Increased time in jail during the last incarceration before death was used as a proxy of decreased drug tolerance, and its correlation with time between release and death was calculated using a negative binomial regression model.
Non-Hispanic whites, younger people, and persons who had stayed in a homeless shelter were more likely to have missing residence information. To assess possible bias from excluding people for whom we did not have residence information, we conducted a sensitivity analysis in which we repeated all analyses using a data set that included people for whom we did not have residence information (n = 200,483). The direction and strength of the relations were very similar for the 2 data sets.
All P values were 2-sided. Analyses were conducted using SAS, version 9.2 (SAS Institute, Inc., Cary, North Carolina).
RESULTS
Formerly incarcerated people were more likely to be younger, male, and non-Hispanic black than were members of the overall NYC population and residents of the poorest NYC neighborhood (South Bronx) (Table 1). In 2001–2005, 51% of the study population had been incarcerated multiple times. The study cohort spent a cumulative average of 55 days in jail (median = 8 days), and 10% stayed in a NYC single-adult homeless shelter for at least 1 night.
Table 1.
Characteristics of the Study Population, New York City, 2001–2005
| Formerly Incarcerated People | New York City Residentsa | New York City Residents From the Poorest Neighborhooda,b | ||||
|---|---|---|---|---|---|---|
| No. | %c | No. | %c | No. | %c | |
| Total | 155,272 | 6,231,402 | 349,120 | |||
| Demographic characteristics | ||||||
| Age, years | ||||||
| 16–24 | 49,324 | 32 | 1,009,654 | 16 | 75,140 | 22 |
| 25–34 | 41,498 | 27 | 1,368,021 | 22 | 78,448 | 22 |
| 35–44 | 41,968 | 27 | 1,263,280 | 20 | 75,314 | 22 |
| 45–54 | 18,049 | 12 | 1,012,385 | 16 | 52,151 | 15 |
| 55–64 | 3,799 | 2 | 683,454 | 11 | 34,992 | 10 |
| 65–89 | 634 | 0 | 894,608 | 14 | 33,075 | 9 |
| Sex | ||||||
| Female | 18,111 | 12 | 3,332,730 | 53 | 194,327 | 56 |
| Male | 137,161 | 88 | 2,898,672 | 47 | 154,793 | 44 |
| Race/ethnicityd | ||||||
| Non-Hispanic white | 13,489 | 9 | 2,364,340 | 38 | 6,024 | 2 |
| Non-Hispanic black | 84,228 | 54 | 1,448,587 | 23 | 114,989 | 33 |
| Hispanic | 52,666 | 34 | 1,564,069 | 25 | 216,463 | 62 |
| Asian | 1,277 | 1 | 631,192 | 10 | 4,035 | 1 |
| Other | 3,416 | 2 | 223,214 | 4 | 7,609 | 2 |
| Neighborhood income | ||||||
| Low | 86,554 | 56 | 1,920,897 | 31 | 349,120 | 100 |
| Middle | 50,724 | 33 | 2,527,319 | 41 | ||
| High | 17,994 | 12 | 1,783,186 | 29 | ||
| Incarceration characteristics | ||||||
| No. of times incarcerated | ||||||
| 1 | 76,475 | 49 | ||||
| 2–3 | 49,008 | 32 | ||||
| ≥4 | 29,789 | 19 | ||||
| Cumulative days of incarceration | ||||||
| ≤3 | 45,800 | 30 | ||||
| 4–25 | 40,914 | 26 | ||||
| ≥26 | 68,558 | 44 | ||||
| Most frequent type of chargese | ||||||
| Violence | 57,210 | 37 | ||||
| Drug sales or drug possession | 61,171 | 39 | ||||
| Homeless shelter registrant, 2001–2005f | 16,216 | 10 | ||||
Restricted to people who were 16–89 years of age.
People living in the South Bronx (United Hospital Fund’s neighborhood designations 105, 106, and 107), which is the New York City neighborhood with the highest percent of people living in poverty (42%) according to the US Census 2000.
Percentages may not add to 100 because of rounding.
There were 196 formerly incarcerated people for whom race/ethnicity data were missing.
Categories are not mutually exclusive; one can receive multiple charges.
Anyone who spent at least 1 night in a New York City single-adult homeless shelter from 2001 through 2005.
Overall, the cohort of formerly incarcerated persons spent 379,363 person-years in the community after release, and 1,149 died during the study period. There were 219 drug-related deaths, 219 homicides, and 35 suicides. Rates of drug-related death and homicide were approximately 6 times higher in formerly incarcerated people than in nonincarcerated NYC residents and 2–3 times higher than in nonincarcerated people from the poorest NYC neighborhood (Figure 1). Suicide rates were not significantly different among these 3 groups.
Figure 1.
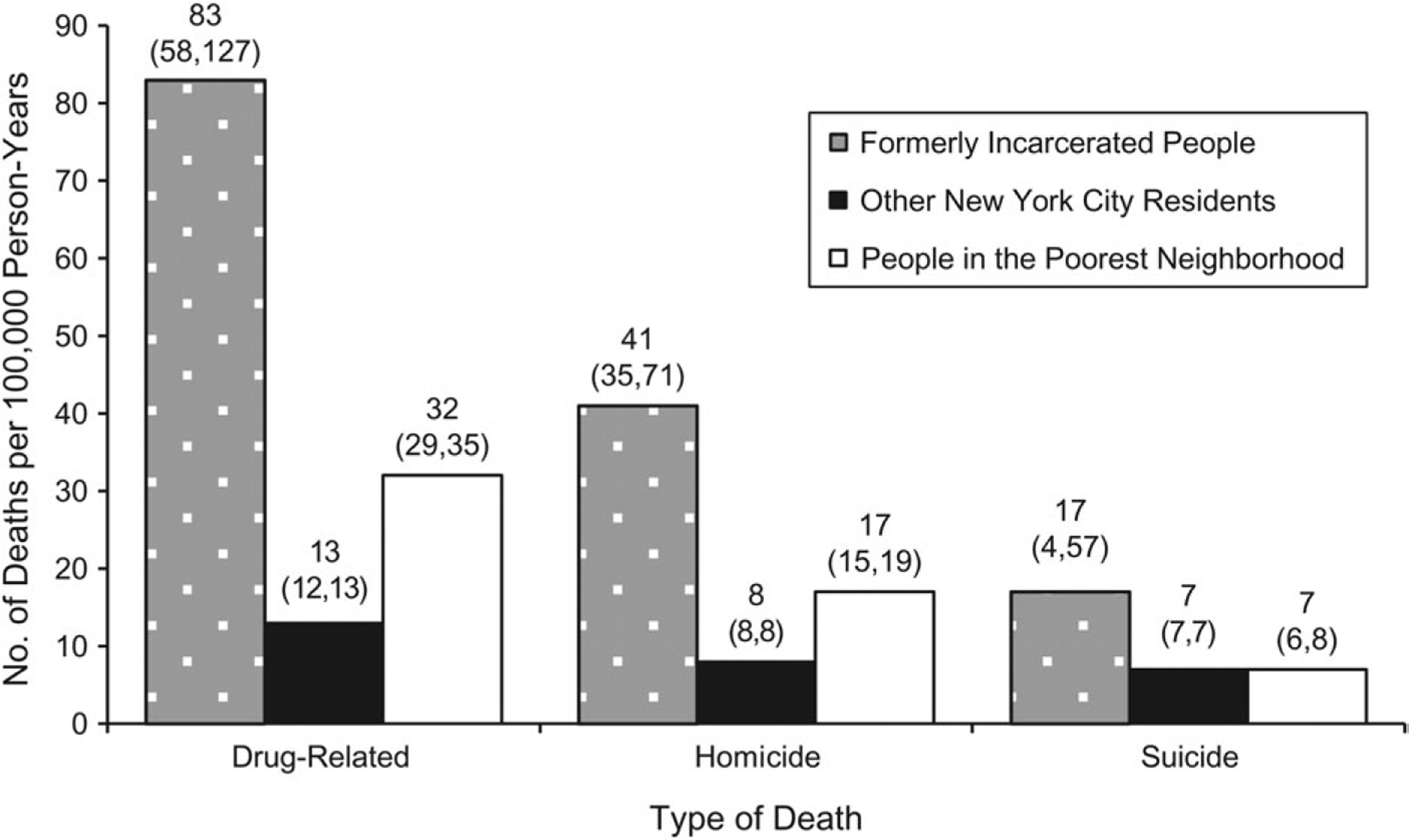
Age-standardized rates of death (deaths per 100,000 person-years) from suicide, homicide, and drug-related causes, New York City, 2001–2005. Persons living in the poorest neighborhood included New York City residents living in the South Bronx (United Hospital Fund’s neighborhood designations 105, 106, and 107). The South Bronx is the New York City neighborhood with the highest percent of people living in poverty (42%) according to the US Census 2000.
Comparisons with nonincarcerated people: SMR analysis
After adjustment for age, sex, race, and neighborhood, the risks of drug-related death and homicide were 2.2 times (95% CI: 1.9, 2.5) and 1.7 times (95% CI: 1.5, 2.0) higher, respectively, in formerly incarcerated people than in nonincarcerated NYC residents (Table 2). The SMRs for drug-related deaths and homicides during the first 2 weeks after release were 8.0 (95% CI: 5.2, 11.8) and 5.1 (95% CI: 3.2, 7.8), respectively. The SMR for suicide was not statistically significant during the immediate post-release period. During the entire post-release period, formerly incarcerated non-Hispanic whites had a high risk of suicide (SMR = 2.6, 95% CI: 1.4, 4.5) and drug-related death (SMR = 5.2, 95% CI: 4.0, 6.6), whereas non-Hispanic blacks (SMR = 1.7, 95% CI: 1.4, 2.0) and Hispanics (SMR = 2.1, 95% CI: 1.6, 2.8) had a higher risk of homicide (Table 2). The highest risk of death from drug-related causes (SMR = 8.6, 95% CI: 3.7, 16.9) and suicide (SMR = 9.7, 95% CI: 2.0, 28.3) was among white women. Formerly incarcerated people from low- or middle-income neighborhoods were 2 times more likely to die from homicide than were their nonincarcerated NYC counterparts. In high-income neighborhoods, the risk of drug-related death was greater (SMR = 3.3, 95% CI: 2.2, 4.9) in formerly incarcerated people than in nonincarcerated NYC residents. A similar pattern of smaller magnitude was seen in low-income neighborhoods (SMR = 1.7, 95% CI: 1.4, 2.0).
Table 2.
Observed Number of Deaths and Standardized Mortality Ratios by Time After Release and Demographic Characteristics Among People Released From Jails, New York City, 2001–2005
| Variable | Type of Death | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Drug-Related | Homicide | Suicide | |||||||
| No. of Deaths | SMR | 95% CI | No. of Deaths | SMR | 95% CI | No. of Deaths | SMR | 95% CI | |
| Total | 219 | 2.2 | 1.9, 2.5 | 219 | 1.7 | 1.5, 2.0 | 35 | 1.0 | 0.7, 1.4 |
| Time after release, weeks | |||||||||
| 1–2 | 25 | 8.0 | 5.2, 11.8 | 21 | 5.1 | 3.2, 7.8 | 1 | 0.9 | 0.02, 5.1 |
| 3–4 | 12 | 4.2 | 2.1, 7.3 | 12 | 3.1 | 1.6, 5.5 | 3 | 2.9 | 0.6, 8.5 |
| 5–6 | 10 | 3.7 | 1.8, 6.8 | 7 | 1.9 | 0.8, 4.0 | 2 | 2.1 | 0.2, 7.4 |
| 7–8 | 5 | 2.0 | 0.6, 4.6 | 9 | 2.6 | 1.2, 5.0 | 1 | 1.1 | 0.03, 6.1 |
| ≥9 | 167 | 1.9 | 1.6, 2.2 | 170 | 1.5 | 1.3, 1.8 | 28 | 0.9 | 0.6, 1.3 |
| Age, years | |||||||||
| 16–24 | 9 | 2.2 | 1.0, 4.2 | 92 | 1.6 | 1.3, 2.0 | 12 | 1.4 | 0.7, 2.4 |
| 25–34 | 31 | 2.3 | 1.5, 3.2 | 74 | 1.9 | 1.5, 2.3 | 9 | 0.9 | 0.4, 1.7 |
| 35–44 | 90 | 2.1 | 1.7, 2.6 | 36 | 1.6 | 1.2, 2.3 | 9 | 0.9 | 0.4, 1.7 |
| 45–54 | 76 | 2.1 | 1.7, 2.7 | 15 | 2.1 | 1.2, 3.4 | 2 | 0.3 | 0.04, 1.2 |
| 55–64 | 11 | 2.4 | 1.2, 4.3 | 2 | 2.0 | 0.2, 7.1 | 2 | 2.4 | 0.3, 8.6 |
| 65–89 | 2 | 9.5 | 1.2, 34.4 | 0 | 1 | 5.0 | 0.1, 27.9 | ||
| Sex | |||||||||
| Female | 39 | 5.9 | 4.2, 8.1 | 6 | 2.1 | 0.8, 4.6 | 5 | 3.5 | 1.2, 8.3 |
| Male | 180 | 1.9 | 1.6, 2.2 | 213 | 1.7 | 1.5, 2.0 | 30 | 0.9 | 0.6, 1.2 |
| Race/ethnicity | |||||||||
| Non-Hispanic white | 63 | 5.2 | 4.0, 6.6 | 3 | 0.9 | 0.2, 2.7 | 13 | 2.6 | 1.4, 4.5 |
| Non-Hispanic black | 81 | 1.4 | 1.1, 1.8 | 166 | 1.7 | 1.4, 2.0 | 9 | 0.5 | 0.2, 0.9 |
| Hispanic | 72 | 2.4 | 1.9, 3.0 | 50 | 2.1 | 1.6, 2.8 | 13 | 1.3 | 0.7, 2.2 |
| Asian | 0 | 0 | 0 | ||||||
| Other | 3 | 1.6 | 0.3, 4.6 | 0 | 0 | ||||
| Neighborhood income | |||||||||
| Low | 117 | 1.7 | 1.4, 2.0 | 143 | 1.7 | 1.4, 2.0 | 19 | 1.0 | 0.6, 1.5 |
| Middle | 75 | 3.4 | 2.7, 4.3 | 65 | 1.8 | 1.4, 2.3 | 11 | 0.9 | 0.5, 1.7 |
| High | 27 | 3.3 | 2.2, 4.9 | 11 | 1.7 | 0.9, 3.1 | 5 | 1.1 | 0.4, 2.6 |
Abbreviations: CI, confidence interval; SMR, standardized mortality ratio.
Comparisons among formerly incarcerated people: multivariate regression analysis
Compared with the mortality rate in formerly incarcerated persons 5 weeks after release or later, the mortality rate during the first 2 weeks was 3.8 times higher for drug-related causes (95% CI: 1.9, 7.7) and 2.9 times higher for homicide (95% CI: 2.3, 3.7) (Table 3). Non-Hispanic white race/ethnicity and older age were associated with a high risk of drug-related death, whereas non-Hispanic black and Hispanic race/ethnicity and younger age were associated with a high risk of homicide. Homicide rates increased as neighborhood-of-residence income decreased. Formerly incarcerated people who used homeless shelters had higher rates of drug-related death (relative risk (RR) = 3.4, 95% CI: 2.1, 5.5) and suicide (RR = 2.1, 95% CI: 1.2, 3.4) than those who did not use homeless shelters. Deaths in this population often did not occur during shelter stays. Persons charged with a violent crime were more likely to die from suicide than were those who faced other charges (RR = 2.3, 95% CI: 1.5, 3.5). Formerly incarcerated people who spent more than 4 cumulative days in jail were more likely to die from homicide (RR = 1.5, 95% CI: 1.2, 1.8) and suicide (RR = 2.0, 95% CI: 1.2, 3.3) than were persons who were detained for 4 days or fewer.
Table 3.
Adjusted Relative Risks From Multivariate Poisson Regressionsa for Mortality Rates Among People Released From Jails, New York City, 2001–2005
| Type of Death | ||||||
|---|---|---|---|---|---|---|
| Variable | Drug-Related | Homicide | Suicide | |||
| RR | 95% CI | RR | 95% CI | RR | 95% CI | |
| Time after release | ||||||
| 1–2 weeks | 3.8 | 1.9, 7.7 | 2.9 | 2.3, 3.7 | 1.0 | 0.3, 3.1 |
| 3–4 weeks | 2.0 | 0.7, 5.2 | 1.8 | 1.3, 2.5 | 3.1 | 1.6, 6.2 |
| Four or more days spent in jail | 1.1 | 0.6, 2.0 | 1.5 | 1.2, 1.8 | 2.0 | 1.2, 3.3 |
| Two or more incarcerations | 0.9 | 0.5, 1.6 | 1.2 | 1.0, 1.4 | 1.0 | 0.7, 1.6 |
| Type of crime | ||||||
| Drug-related | 1.5 | 0.9, 2.4 | 1.2 | 1.0, 1.3 | 0.3 | 0.2, 0.5 |
| Violence | 0.8 | 0.5, 1.3 | 1.2 | 1.0, 1.3 | 2.3 | 1.5, 3.5 |
| Age ≥33 years | 5.9 | 3.0, 11.7 | 0.5 | 0.4, 0.5 | 0.7 | 0.5, 1.1 |
| Race | ||||||
| Non-Hispanic black | 0.2 | 0.1, 0.3 | 6.5 | 3.6, 11.9 | 0.1 | 0.1, 0.2 |
| Hispanic | 0.3 | 0.2, 0.6 | 3.0 | 1.6, 5.6 | 0.2 | 0.1, 0.4 |
| Non-Hispanic Asian | ||||||
| Other | 0.2 | 0.0, 1.7 | ||||
| Male sex | 0.8 | 0.5, 1.5 | 4.8 | 3.1, 7.3 | 0.7 | 0.4, 1.2 |
| At least 1 night spent in a homeless shelter | 3.4 | 2.1, 5.5 | 0.5 | 0.4, 0.7 | 2.1 | 1.2, 3.4 |
| Neighborhood income | ||||||
| Middle | 1.0 | 0.6, 1.6 | 0.8 | 0.7, 1.0 | 0.7 | 0.5, 1.1 |
| High | 0.7 | 0.4, 1.6 | 0.5 | 0.3, 0.7 | 0.7 | 0.4, 1.2 |
Abbreviations: CI, confidence interval; RR, relative risk.
The reference categories were 5 weeks or more since release, less than 4 days spent in jail, 1 incarceration, no drug-related crimes, no violent crimes, age less than 33 years, non-Hispanic white race, female sex, no time spent in a homeless shelter, and low-income neighborhood.
Among the 219 persons who died from drug-related causes, spending more time in jail was associated with a lower predicted mean number of days between release and death (Table 4). For example, those who spent 91 days or more in jail had a mean predicted time to death of 189 days, compared with 425 days among those who spent fewer than 4 days in jail (P = 0.004). Having had multiple incarcerations was associated with a shorter time to death (RR = 0.7, 95% CI: 0.5, 0.9).
Table 4.
Predicted Mean Time Between Release and Death Among Formerly Incarcerated People Released From Jails Who Died of Drug-Related Causes, by Time Spent in Jail During the Last Incarceration, New York City, 2001–2005a
| Time Spent in Jail During the Last Incarceration, days | Predicted Mean, daysb | 95% Change Confidence in Predicted Interval for Mean Change in Predicted Mean | P Valuec | |
|---|---|---|---|---|
| <4 (n = 74) | 425.1 | 0 | Reference | |
| 4–14 (n = 53) | 330.8 | −22.2 | −48.5, 17.6 | 0.234 |
| 15–30 (n = 29) | 241.8 | −43.1 | −65.2, −7.0 | 0.024 |
| 31–60 (n = 23) | 246.4 | −42.1 | −66.2, −0.7 | 0.047 |
| 61–90 (n = 16) | 235.3 | −44.7 | −71.1, 5.9 | 0.074 |
| ≥91 (n = 24) | 188.7 | −55.6 | −74.3, −23.4 | 0.004 |
Results were from the negative binomial regression model, with days between release and death as the dependent variable. Covariates included time spent in jail during the last incarceration, sex, age at death, race/ethnicity, and the number of times incarcerated. Among all covariates, time spent in jail during the last incarceration and number of times incarcerated were significantly associated with the dependent variable.
Predicted mean was computed holding the other covariates at their mean.
Two-sided chi-squared test for the difference in mean days between release and death compared with the reference.
DISCUSSION
In a large retrospective cohort of formerly incarcerated adults, we identified patterns of elevated mortality risk due to drug use and homicide. Our findings were similar to those from previous studies among newly released prisoners in the United States, United Kingdom, and Australia (1, 3, 18–20). Specifically, we found that formerly incarcerated people in NYC were 8 times more likely to die of drug-related causes and 5 times more likely to die from homicide during the first 2 weeks after release than were nonincarcerated NYC residents in the same 2-week period. The overall risk of suicide was not elevated after release, but excess risk was found among non-Hispanic white women and homeless individuals. The elevated risk of drug-related death among formerly incarcerated people was most evident during the first 2 weeks after release. Although we found a negative association between the length of jail stay and time to death, the time to death for persons who spent longer periods in jail was too long to support the hypothesis that decreased drug tolerance during incarceration contributes to fatal overdose shortly after release.
Similar to what was found in a previous study (1), we found an excess risk of homicide among formerly incarcerated people, which suggested that they might be exposed to violent environments after release. This exposure might be explained by the relation between neighborhood deprivation and high homicide rates (21). Yet, excess risk was found even after accounting for the neighborhood of residence, implying that there might be other contributing factors. More research on the interplay between environmental, social, and personal risk factors is warranted.
In the present study, suicide risk was not elevated in the immediate post-release period, results which differ from previous studies of former prisoners (1, 4). This contradiction could possibly be attributed to differential consequences of long-term incarceration in prisons. However, the low number of suicides in our study limited our ability to conduct analyses by length of detention. Our finding that rates of drug-related death and suicide were higher among formerly incarcerated people who had used single-adult homeless shelters than among those who had not builds on previous studies that showed that substance use and mental illness contribute to the risk of incarceration and homelessness (13, 22). Populations with histories of both events might have a higher likelihood of not only experiencing but also dying from substance use.
Non-Hispanic whites had disproportionately higher risks of drug-related death and suicide, whereas elevated risk of homicide was found only among non-Hispanic black and Hispanic men. Some of these racial/ethnic differences were consistent with a previous finding (3, 23). However, the homicide risk found in our study differs from that in a North Carolina study in which the SMR for homicide was greater among white former prisoners than among black former prisoners (SMR = 6.7 vs. SMR = 2.7) (23). This may stem from differences in characteristics between NYC and North Carolina residents or between former prisoners and people released from jail.
Neighborhood income was associated with excess homicide risk among formerly incarcerated people. This builds on other work that showed a disparity in mortality rates between higher- and lower-income neighborhoods (24) and may reflect environmental factors, such as limited jobs and housing, that could impact trends in criminal activities (7). Beyond the neighborhood, there seems to be an additive effect of incarceration on mortality risk. Even among people from the low-income NYC neighborhoods, the homicide risk was almost 2 times greater than that among nonincarcerated people of the same age, sex, and race/ethnicity from those neighborhoods.
The present study has several limitations. We could not distinguish accidental drug-related death from death due to chronic drug use because of coding misclassification in the Vital Statistics registry (25), nor could we determine the drugs or circumstances involved in the overdoses. Death counts might have been underestimated because we did not include deaths that occurred outside NYC. Our neighborhood measure for formerly incarcerated people came from Department of Correction admission records. There could have been misclassification due to potential relocation after release. In addition, our neighborhood poverty variable might not capture individuals living in smaller poor areas within a large United Hospital Fund neighborhood with less poverty. Homelessness data were limited to single adults who had used a shelter for at least 1 night during the study period. Finally, at the time of data collection, electronic records of substance use and mental health diagnosis were not available, limiting our ability to analyze the role of depression and other clinical antecedents of excess mortality risk.
Our study demonstrates that for people released from NYC jails, the immediate post-release period may be a particularly vulnerable time and carry an excess risk of drug-related death and homicide. Racial, socioeconomic, and housing-related disparities in mortality rates persist. People incarcerated in NYC jails routinely undergo assessments to identify mental illness, suicide risk, and substance use disorders. Specifically, jail-based interventions include mental health counseling and therapy, suicide prevention screening and observation, opioid maintenance therapy and detoxification, substance use treatment, harm-reduction counseling, and linkages to community services. The present study highlights the importance of those interventions and the need for such programs to continue in the community after release.
We have several recommendations regarding preventing post-release homicide and drug overdose. Drug counseling and therapy initiated during incarceration should be maintained after release via increased collaboration with community partners, as these programs may reduce the risk of overdose (26, 27). A holistic framework that combines pharmacotherapy, harm reduction, and psychosocial development, as well as involvement with family and community, may be most effective (27). Post-release employment and supportive housing with drug treatment could also facilitate community reentry and decrease exposure to mortality risk factors (27, 28). Additional jail- and community-based strategies should be identified to decrease the risk of homicide and drug-related death among people released from NYC jails, particularly during the first few weeks after release.
ACKNOWLEDGMENTS
The authors thank Regina Zimmerman, Wenhui Lee, and Joseph Kennedy for their help with the mortality analysis; Tejinder Singh for data checking; Daliah Heller and Denise Paone for their help with the overdose analysis; Jisen Ho for data matching; Dova Marder and Eileen Lynch for their help with the homeless analysis; and Lorna Thorpe for her helpful comments on this study.
Abbreviations:
- CI
confidence interval
- NYC
New York City
- RR
relative risk
- SMR
standardized mortality ratio
Footnotes
This work was presented in part at the American Public Health Association 138th Annual Meeting & Exposition, November 6–10, 2010, Denver, Colorado (abstract 215374).
Conflict of interest: none declared.
Contributor Information
Sungwoo Lim, New York City Department of Health and Mental Hygiene, New York, New York.
Amber Levanon Seligson, New York City Department of Health and Mental Hygiene, New York, New York.
Farah M. Parvez, New York City Department of Health and Mental Hygiene, New York, New York The National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention, Atlanta, Georgia.
Charles W. Luther, SUNY Downstate Medical Center, New York, New York
Maushumi P. Mavinkurve, New York City Department of Health and Mental Hygiene, New York, New York
Ingrid A. Binswanger, University of Colorado School of Medicine and Denver Health Medical Center, Denver, Colorado
Bonnie D. Kerker, New York City Department of Health and Mental Hygiene, New York, New York
REFERENCES
- 1.Binswanger IA, Stern MF, Deyo RA, et al. Release from prison: a high risk of death for former inmates. N Engl J Med. 2007;356(2):157–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pratt D, Piper M, Appleby L, et al. Suicide in recently released prisoners: a population-based cohort study. Lancet. 2006; 368(9530):119–123. [DOI] [PubMed] [Google Scholar]
- 3.Farrell M, Marsden J. Acute risk of drug-related death among newly released prisoners in England and Wales. Addiction. 2008;103(2):251–255. [DOI] [PubMed] [Google Scholar]
- 4.Kariminia A, Law MG, Butler TG, et al. Suicide risk among recently released prisoners in New South Wales, Australia. Med J Aust. 2007;187(7):387–390. [DOI] [PubMed] [Google Scholar]
- 5.White JM, Irvine RJ. Mechanisms of fatal opioid overdose. Addiction. 1999;94(7):961–972. [PubMed] [Google Scholar]
- 6.Darke S, Ross J, Zador D, et al. Heroin-related deaths in New South Wales, Australia, 1992–1996. Drug Alcohol Depend. 2000;60(2):141–150. [DOI] [PubMed] [Google Scholar]
- 7.Freudenberg N, Daniels J, Crum M, et al. Coming home from jail: the social and health consequences of community reentry for women, male adolescents, and their families and communities. Am J Public Health. 2005;95(10):1725–1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van Olphen J, Freudenberg N, Fortin P, et al. Community reentry: perceptions of people with substance use problems returning home from New York City jails. J Urban Health. 2006;83(3): 372–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hammett TM, Harmon MP, Rhodes W. The burden of infectious disease among inmates of and releases from US correctional facilities, 1997. Am J Public Health. 2002;92(11): 1789–1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Office of Justice Statistics. Jail Inmates at Midyear 2007. Washington, DC: Department of Justice; 2008; (http://bjs.ojp.usdoj.gov/content/pub/pdf/jim07.pdf). (Accessed March 8, 2010). [Google Scholar]
- 11.Office of Justice Statistics. Prison Inmates at Midyear 2007. Washington, DC: Department of Justice; 2008; (http://bjs.ojp.usdoj.gov/content/pub/pdf/pim07.pdf). (Accessed March 8, 2010). [Google Scholar]
- 12.Caton CLM, Domiguez B, Schanzer B, et al. Risk factors for long-term homelessness: findings from a longitudinal study of first-time homeless single adults. Am J Public Health. 2005; 95(10):1753–1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Greenberg GA, Rosenheck RA. Jail incarceration, homelessness, and mental health: a national study. Psychiatr Serv. 2008; 59(2):170–177. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization. International Statistical Classification of Diseases and Related Health Problems Tenth Revision. Geneva, Switzerland: World Health Organization; 2006. (http://www.who.int/classifications/apps/icd/icd10online). (Accessed June 5, 2009). [Google Scholar]
- 15.United Hospital Fund. United Hospital Fund Neighborhoods. New York, NY: United Hospital Fund; 2008. (http://www.nyc.gov/html/doh/downloads/pdf/data/appb.pdf). (Accessed June 5, 2009). [Google Scholar]
- 16.US Census Bureau. United States Census 2000 Summary File 3. Washington, DC: US Census Bureau; 2000. (http://www.census.gov/census2000/sumfile3.html). (Accessed June 5, 2009). [Google Scholar]
- 17.Breslow NE, Day NE. Indirect standardization and multiplicative models for rates, with reference to the age adjustment of cancer incidence and relative frequency data. J Chronic Dis. 1975;28(5–6):289–303. [DOI] [PubMed] [Google Scholar]
- 18.Bird SM, Hutchinson SJ. Male drugs-related deaths in the fortnight after release from prison: Scotland, 1996–99. Addiction. 2003;98(2):185–190. [DOI] [PubMed] [Google Scholar]
- 19.Stewart LM, Henderson CJ, Hobbs MS, et al. Risk of death in prisoners after release from jail. Aust N Z J Public Health. 2004;28(1):32–36. [DOI] [PubMed] [Google Scholar]
- 20.Merrall EL, Kariminia A, Binswanger IA, et al. Meta-analysis of drug-related deaths soon after release from prison. Addiction. 2010;105(9):1545–1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morenoff JD, Sampson RJ, Raudenbush SW. Neighborhood inequality, collective efficacy, and the spatial dynamics of urban violence. Criminology. 2001;39(3):517–560. [Google Scholar]
- 22.McNiel DE, Binder RL, Robinson JC. Incarceration associated with homelessness, mental disorder, and co-occurring substance abuse. Psychiatr Serv. 2005;56(7):840–846. [DOI] [PubMed] [Google Scholar]
- 23.Rosen DL, Schoenbach VJ, Wohl DA. All-cause and cause-specific mortality among men released from state prison, 1980–2005. Am J Public Health. 2008;98(12):2278–2284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karpati AM, Bassett MT, McCord C. Neighbourhood mortality inequalities in New York City, 1989–1991 and 1999–2001. J Epidemiol Community Health. 2006;60(12):1060–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.New York City Department of Health and Mental Hygiene. Summary of Vital Statistics 2007: The City of New York. New York, NY: Office of Vital Statistics; (http://www.nyc.gov/html/doh/downloads/pdf/vs/2007sum.pdf). (Accessed February 22, 2010). [Google Scholar]
- 26.Pelissier B, Wallace S, O’Neil JA, et al. Federal prison residential drug treatment reduces substance use and arrests after release. Am J Drug Alcohol Abuse. 2001;27(2):315–337. [DOI] [PubMed] [Google Scholar]
- 27.World Health Organization. Prevention of Acute Drug-Related Mortality in Prison Populations During the Immediate Post-Release Period: 2010. Geneva, Switzerland: World Health Organization; 2010. (http://www.euro.who.int/__data/assets/pdf_file/0020/114914/E93993.pdf.) (Accessed October 18, 2011). [Google Scholar]
- 28.Jails Freudenberg N., prisons, and the health of urban populations: a review of the impact of the correctional system on community health. J Urban Health. 2001;78(2):214–235. [DOI] [PMC free article] [PubMed] [Google Scholar]


