Abstract
Rationale and objectives To see whether net mortalities increase during and after reductions in medical services, either at average weekends, or at Christmas when pressure from illness is unusually high.
Methods (1) Paired t‐tests to compare mean daily deaths and hospital admissions during and after weekends (Saturday–Tuesday) with means for the week, in south‐east England; (2) Linear regressions to see whether trends of daily deaths change when admissions are reduced at Christmas.
Results Neither mean daily all‐cause, respiratory or ischaemic heart deaths exceeded weekly averages during weekends, or during Saturday–Monday or Saturday–Tuesday, despite falls in daily elective and daily emergency hospital admissions at weekends that averaged 61–72% and 14–22%, respectively. During 19–24 December, daily deaths were above annual means, respiratory deaths by 49% (29, 1–58), but elective admissions fell and although emergency admissions tended to rise, total admissions rose only for respiratory disease, and only by 33% (376, −47 to 799). On Christmas Day (25 December), even emergency admissions fell sharply below previous trends, respiratory emergency admissions by 18% (P < 0.01). Respiratory deaths alone then immediately increased (P < 0.01) above trend, by 5.9% (5.8 deaths/day) on 26 December and by 12.9% (12.9) on 27 December.
Conclusions No adverse effect on mortality was apparent within 2 days from reduction in medical services at weekends. However, respiratory deaths accelerated sharply after reduction in elective and emergency admissions at Christmas, when rates of infection and mortality from respiratory disease were high. Implications for medical services during respiratory epidemics are discussed.
Keywords: coronary, elective, emergency, hospital admissions, mortality, respiratory
Introduction
There is little information on whether the reduction of hospital and other medical services during weekends (Fullerton & Crawford 1999), or other public holidays, has adverse consequences on short‐term mortality. The present study analyses changes in cause‐specific mortalities and hospital admissions during and for 2 days after weekends and Christmas. The hypothesis was that reduced medical services in holiday periods might be able to handle everyone requiring rapid lifesaving treatment if they happened at a time of average demand, such as average weekends, but not when demand is raised by respiratory epidemics and other illness. Such demand could be expected to be high at Christmas with the onset of winter. Separate analyses were made for all‐causes, respiratory disease, and ischaemic heart disease, and also for elective and emergency admissions to National Health Service hospitals in South‐east England.
Increased mortality during the weekend has been reported only for regions with high rates of acute alcohol poisoning at weekends (Chenet et al. 1998, , 2001) Increases in mortality on Mondays have often been reported, particularly from coronary heart disease (e.g. Peckova et al. 1999; Evans et al. 2000), but might result from people who live alone dying at weekends but not being found until Monday; or from quiet lifestyle at weekends delaying some deaths until after the weekend. We therefore looked first for any net increases in mean daily deaths during and for 2 days after weekends, which could be attributed to cutbacks in admissions at weekends.
We then looked for changes in daily mortality following sharp reductions of admissions at Christmas. Low temperature then can be expected to increase illness and mortality (Bull & Morton 1975; Eurowinter Group 1997; Donaldson & Keatinge 1997). Respiratory infections by influenza and respiratory syncytial virus are high at that time (http://www.phls.co.uk/topicsaz/index.htm). Haemoconcentration resulting from cold stress (Keatinge et al. 1984; Neild et al. 1994), and increased blood fibrinogen resulting from respiratory infections (Woodhouse et al. 1994), both tend to increase ischaemic heart deaths. Mortality was rising linearly before Christmas, and the rate of rise was analysed for any abrupt change that would give evidence of a specific effect of reduced admissions on Christmas Day.
Methods
Daily finished consultant episodes for emergency and elective admissions to National Health Service hospitals in south‐east England were provided by the Department of Health for 1 April 1989 to 31 March 2001. South‐east England for the year starting 1992 (1 April) or earlier was designated as the area controlled by health authorities of East Anglia, north‐west Thames, north‐east Thames, south‐west Thames, south‐east Thames, and Oxford; for 1993–98 as the regions of Anglia and Oxford, north Thames and south Thames; and for 1999–2000 as the eastern, London and south‐east regions. For the year starting 1994 or earlier, admissions were broken down by primary diagnosis using the ninth International Disease Classification (ICD9) and thereafter by the 10th ICD (ICD10), for ischaemic heart disease (ICD9 410.0–414.9 and ICD10 I20–I25), respiratory disease (460.0–519.9 and J00–J99); influenza (487.0–487.9 and J10–J11), and all‐cause (0–999.9 and A00–Y34). The deaths certified as influenza provide a marker for much larger numbers of deaths secondary to influenza (Donaldson & Keatinge 2002)
Daily deaths for these years in South‐east England (standard region) were supplied by the Office of National Statistics. This region comprised Greater London, Hertfordshire, Essex, Kent, East and West Sussex, Hampshire, Surrey, Berkshire, Oxfordshire, Buckinghamshire and Bedfordshire, and approximately matched the area for hospital admissions. Cause of death was coded using ICD9 except for January 2001 for which ICD10 was used. Standard adjustments were made for the change in coding practice in 1993. Temperatures were daily values from London Heathrow, provided by the Royal Meteorological Office.
Some discontinuities in the admissions data were apparently caused by minor changes in local boundaries, hospital capacities and admission policies. These could not be satisfactorily adjusted for by trend analysis or in other ways. As key comparisons used pairs of data each separated by only a few days, or sequences of data lasting only a few days, the discontinuities will have had little overall effect on them.
For effects of weekends, we compared by paired t‐tests the means of daily mortalities and admissions during weekends with means for the whole of the same week (Saturday–Friday). This analysis was repeated for Saturday–Monday and then for Saturday–Tuesday instead of the weekend.
This simple approach could not be used to assess changes at Christmas, as mortalities were rising systematically before Christmas. Nor could time series analysis be used, because of variable day of week effects during days close to Christmas Day. We accordingly analysed the most recent 7 years starting 1 February (1990, 1994 and 1996, 1997, 1998, 1999, 2000), in which every day of the week occurred only once on Christmas Day, and on each other date in the Christmas period. As the mean mortalities and admissions for these years rose linearly in the days before Christmas; linear regression was used to assess their trends, and to determine significances of deviations from them on and after Christmas Day. Ninety‐nine per cent probability was taken as significant.
Results
Weekends
Deaths from all‐causes, respiratory, and ischaemic heart disease (Fig. 1), were slightly reduced on Sundays, respectively, by 1.6% (−7.7, −10.8 to −4.6, mean and 99% confidence limits for change in deaths per day), by 1.9% (−1.1, −2.0 to −0.1) and by 2.0% (−2.1, −3.3 to −1.9) compared to their whole week averages. Ischaemic heart mortality was also reduced on Saturdays, by 1.9% (−2.0, −3.4 to −0.5) below the whole week average. Small increases in mortality on Monday (Fig. 1), particularly for ischaemic heart disease, largely balanced but never exceeded these falls. Mean mortalities from each cause over the entire period of either Saturday–Sunday, Saturday–Monday, or Saturday–Tuesday accordingly never exceeded the whole week averages (Table 1).
Figure 1.
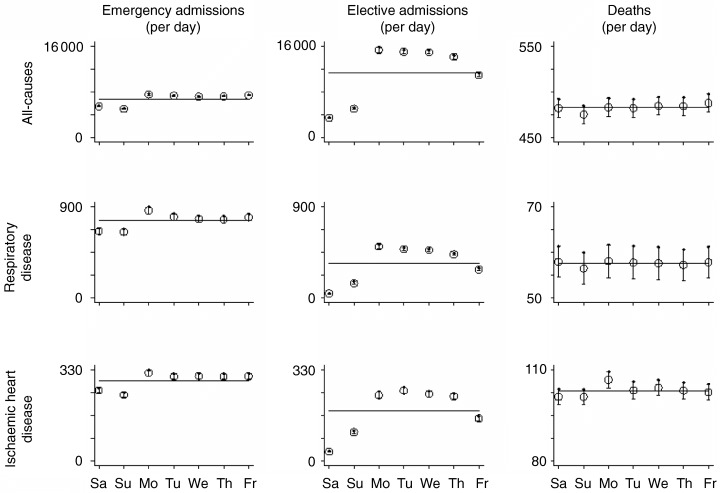
Deaths, and elective and emergency admissions, by day of week. Error bars give 99% confidence limits.
Table 1.
Mean daily deaths (Saturday to Sunday, Saturday to Monday and Saturday to Tuesday)
| Whole week | Saturday to Sunday | Saturday to Monday | Saturday to Tuesday | |
|---|---|---|---|---|
| All‐cause | 483 (473, 492) | 479 (469, 488) | 480 (471, 490) | 481 (471, 490) |
| Difference from whole week | −4.1 (−6.7, −1.5) | −2.6 (−4.5, −0.7) | −2.1 (−3.5, −0.7) | |
| Respiratory disease | 58 (54, 61) | 57 (54, 61) | 57 (54, 61) | 58 (54, 61) |
| Difference from whole week | −0.36 (−1.15, 0.44) | −0.06 (−0.65, 0.53) | 0.00 (−0.44, 0.45) | |
| Ischaemic heart disease | 103 (101, 106) | 101 (99, 104) | 103 (101, 105) | 103 (101, 105) |
| Difference from whole week | −2.0 (−2.9, −1.1) | −0.14 (−0.80, 0.52) | −0.07 (−0.57, 0.43) |
Values are means (99% confidence limits); significance of differences calculated from data paired within each week.
Admissions fell greatly at weekends (Fig. 1). Elective admissions per day over Saturday‐Sunday for all‐causes fell by 62% (−7013, −7161 to −6865 mean and 99% confidence limits for change in admissions per day) compared to the whole week average, those for respiratory disease fell by 72% (−244, −250 to −238), and those for ischaemic heart disease by 61% (−110, −114 to −105). Emergency admissions per day over Saturday‐Sunday for all‐causes were reduced by 22% (−1487, −1511 to −1463) compared to the whole week average, those for respiratory disease by 14% (−108, −114 to −102), and those for ischaemic heart disease by 15% (−44, −46 to −42). Emergency admissions rose on Mondays to their highest points of the week, but totals of elective or emergency admissions for all of these causes over Saturday–Monday, or Saturday–Tuesday, remained well below their whole week averages (Fig. 1).
Increasing illness and restriction of admissions in the days before Christmas Day
Deaths, particularly respiratory and influenza deaths, rose during cold weather in December (Fig. 2). The rise was briefly checked with a few days of warm weather in early December, but after 14th December mean daily temperature remained low, in a narrow band of 4.1–6.3°C, until the end of the month, and deaths rose linearly until Christmas Day. During the 6 days before Christmas, 19–24 December, daily deaths from all‐causes, respiratory and ischaemic heart disease, respectively, averaged 22%, 50%, and 24% above (P < 0.01) annual means (Fig. 2, Table 2). However, during these days, elective all‐cause, respiratory and ischaemic heart admissions were all greatly reduced compared to annual means (P < 0.01), respectively, by 27%, by 49%, and by 49%. Emergency admissions tended to be raised, but only emergency respiratory admissions were significantly above annual mean (P < 0.01), by 71%. The total of elective + emergency admissions for all‐causes was below annual mean by 15% (−2655, −4791 to −520); total respiratory admissions tended to rise, but only by 33% (376, −47 to 799), while total ischaemic heart admissions fell by 18% (−88, −134 to −42); values in brackets are means and 99% confidence limits for admissions per day.
Figure 2.
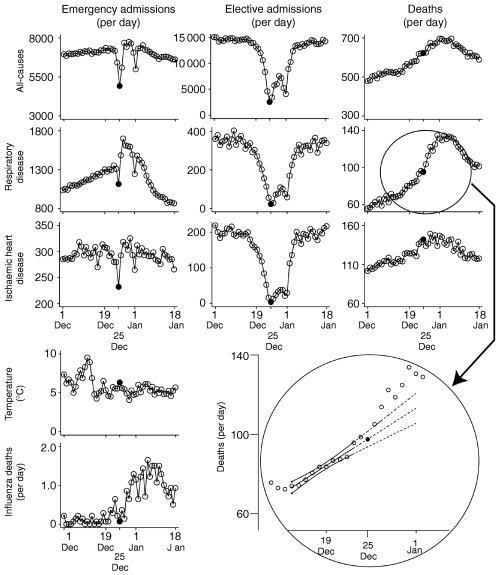
Daily deaths and hospital admissions during the Christmas period. Linear regression with 99% confidence limits on expanded scale insert is based on data of 14–23 December inclusive. Points for each date are means for 7 years on which each day of week was represented once (see Methods). Solid circles are Christmas Day.
Table 2.
Daily deaths and admissions 19–24 December compared to whole year
| Deaths | Elective admissions | Emergency admissions | |
|---|---|---|---|
| All‐cause | |||
| Throughout year | 483 (458, 507) | 11310 (9764, 12857) | 6749 (6104, 7395) |
| 19–24 December | 589 (482, 696) | 8281 (5601, 10962) | 7124 (6290, 7957) |
| Difference from whole year | 106 (16, 196) | −3029 (−4734, −1325) | 374 (−319, 1067) |
| Respiratory disease | |||
| Throughout year | 58 (49, 66) | 337 (297, 377) | 763 (696, 830) |
| 19–24 December | 87 (51, 123) | 171 (824, 258) | 1304 (842, 1767) |
| Difference from whole year | 29 (1, 58) | −166 (−234, −97) | 541 (131, 952) |
| Ischaemic heart disease | |||
| Throughout year | 103 (88, 119) | 181 (113, 248) | 293 (199, 386) |
| 19–24 December | 128 (103, 154) | 93 (37, 148) | 294 (195, 392) |
| Difference from whole year | 25 (6, 44) | −88 (−129, −48) | 1 (−15, 16) |
Values are means (99% confidence limits); significance of differences calculated from data paired within each year.
Changes on and immediately after 25 December
After a linear rise from 14 December to 23 December, there was a sharp reduction in all emergency admissions on Christmas Day, sometimes starting the previous day (Fig. 2). Compared to the previous linear trends, emergency admissions for all‐causes were reduced on 25 December by 33% or 2406 per day (P < 0.01), for ischaemic heart disease by 21% or 61 per day (P < 0.01), and for respiratory emergency admissions by 18% or 242 per day (P < 0.01).
Daily deaths from all of these causes also rose linearly from 14 December to 23 December, and up to and including 25 December After the reduced admissions that day, respiratory deaths alone rose significantly, on 26 December to 5.9% (5.8 per day, P < 0.01) above the linear trend, on 27 December to 12.9% (12.9 per day, P < 0.01) above it, and remained above trend for several further days (Fig. 2).
Admissions for all of these causes again fell briefly on 1 January, New Year's Day (Fig. 2); the wave of illness was then passing its peak, presumably because of rising immunity to the respiratory infections.
Discussion
The main findings are: (1) Elective admissions were reduced around 50% and emergency admissions around 20% at weekends. However, neither mean daily deaths from all‐causes, respiratory or ischaemic heart disease increased, either during weekends or during the weekends plus either 1 or 2 days following them; (2) Cold weather in the days leading up to Christmas was associated with increased illness and mortality, particularly from respiratory infections, but elective admissions for each cause fell, and only emergency admissions for respiratory disease increased significantly above annual mean, presumably reflecting recognition by health staff of need for urgent admission of acute respiratory cases. Even emergency admissions for respiratory disease were sharply reduced on Christmas Day and respiratory deaths then increased above trend on the next and subsequent days. This increase was too rapid in its early stages to be attributable to spread of infection at Christmas Day gatherings. Pulmonary symptoms resulting from infection by rhinoviruses, coronaviruses and respiratory syncytial viruses only start 3 days, and symptoms of influenza 2–4 days, after infection (Tyrrell et al. 1993; Isaacs 1996). The cutback in hospital admissions, and probably in other medical services, on Christmas Day provides the most likely explanation for the acceleration of deaths immediately afterwards.
The fact that large cutbacks in admissions at average weekends were not associated with any net increase in deaths during and for 2 days after the weekend is evidence that virtually all patients with acute, treatable illnesses which were life threatening in the short term were still admitted at weekends. The cutbacks in admissions at weekends were apparently successfully confined to patients without such pressing need for treatment. We know of no estimate of the overall proportion of admissions made up of such patients, although 1–20% of admissions to British hospitals have been judged inappropriate to the nature and severity of the patient's illness and the facilities of the hospital, and therefore unlikely to benefit the patient, rapidly or otherwise (Anderson et al. 1988; Victor & Khakoo 1994; Smith et al. 1997; McDonough et al. 2000). The selective admission of seriously ill people at weekends can incidentally explain high hospital mortality reported among people admitted at weekends (Bell & Redelmeier 2002), without needing to attribute that mortality to deficiencies in hospital treatment at weekends.
The fact that the increase in deaths after Christmas was confined to respiratory disease can be explained by the particularly high level of respiratory infection at the time, and by the fact that antibiotics, oxygen therapy and positive pressure ventilation can be lifesaving in acute respiratory failure, and can be given most quickly and effectively to patients who are already in hospital. The cutbacks in hospital admissions at that time may be partly because of patients’ choice, although it seems unlikely that many people acutely ill with respiratory infections would refuse admission in order to spend Christmas at home. Action to reduce cold stress, particularly outdoors, could reduce both the respiratory and other illness in cold weather (Keatinge 1987; Eurowinter Group 1997). Immunization against respiratory syncytial virus, in addition to current immunization against influenza (Treanor & Falsey 1999), may also have scope to do so. However, the main implication of the present results is that any major respiratory epidemic is likely to require a large number of admissions to beds with facilities for managing respiratory failure, if unnecessary deaths are to be avoided. Current epidemics of respiratory infections are minor compared to the influenza epidemics of 1970s, but the recent appearances of the Fuji strain of influenza, and of severe acute respiratory syndrome (SARS), have raised the possibility that a new virus may produce another large epidemic of respiratory disease before natural or artificial immunity to it can be established.
References
- Anderson P., Meara J., Brodhurst S., Attwood S., Timbrell M. & Gatherer A. (1988) Use of hospital beds: a cohort study of admissions to a provincial teaching hospital. British Medical Journal 297, 919–912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell C.H. & Redelmeier D.A. (2002) Mortality among patients admitted to hospitals on weekdays as compared with weekends. New England Journal of Medicine 345, 663–668. [DOI] [PubMed] [Google Scholar]
- Bull G.M. & Morton J. (1975) Seasonal and short term relationships of temperature with deaths from myocardial and cerebral infarction. Age Aging 4, 19–30. [DOI] [PubMed] [Google Scholar]
- Chenet L., Britton A., Kalediene R. & Petrauskiene J. (2001) Daily variations in deaths in Lithuania: the possible contribution of binge drinking. International Journal of Epidemiology 30, 743–748. [DOI] [PubMed] [Google Scholar]
- Chenet L., McKee M., Leon D., Shkolnikov V. & Vassin S. (1998) Alcohol and cardiovascular mortality in Moscow: new evidence of a causal association. Journal of Epidemiology and Community Health 52, 772–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donaldson G.C. & Keatinge W.R. (1997) Early increases in ischaemic heart disease mortality dissociated from, and later changes associated with, respiratory mortality after cold weather in south‐east England. Journal of Epidemiology and Community Health 51, 643–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donaldson G.C. & Keatinge W.R. (2002) Excess winter mortality: influenza or cold stress? British Medical Journal 324, 89–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eurowinter Group (1997) Cold exposure and winter mortality from ischaemic heart disease, cerebrovascular disease, respiratory disease, and all‐causes in warn and cold regions of Europe. Lancet 395, 1341–1346. [PubMed] [Google Scholar]
- Evans C., Chalmers J., Capewell S., Redpath A., Finlayson A., Boyd J., Pell J., McMurray J., Macintyre K. & Graham L. (2000) ‘I don’t like Mondays’– day of the week of coronary heart disease deaths in Scotland: study of routinely collected data. British Medical Journal 320, 218–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fullerton K.J. & Crawford V.L.S. (1999) The winter bed crisis – quantifying seasonal effects on hospital bed usage. Quarterly Journal of Medicine 92, 199–206. [DOI] [PubMed] [Google Scholar]
- Isaacs D. (1996) Section 7.10.1: Respiratory tract viruses In Oxford Textbook of Medicine (eds Weatherall D.J., Ledingham & J.G.G. D.A. Warrell), p. 338 Oxford University Press, Oxford. [Google Scholar]
- Keatinge W.R. (1987) Seasonal mortality among elderly people with unrestricted home heating. Geriatrics Digest 5, 23–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keatinge W.R., Coleshaw S.R.K., Cotter F., Mattock M., Murphy M. & Chelliah R. (1984) Increases in platelet and red cell counts, blood viscosity, and arterial pressure during mild surface cooling: factors in mortality from coronary and cerebral thrombosis in winter. British Medical Journal 289, 1405–1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonough M., Smith D.H. & Goddard M. (2000) Measuring appropriate use of acute beds. A systematic review of methods and results. Health Policy 53, 157–184. [DOI] [PubMed] [Google Scholar]
- Neild P.J., Syndercombe‐Court D., Keatinge W.R., Donaldson G.C., Mattock M. & Caunce M. (1994) Cold‐induced increases in erythrocyte count, plasma cholesterol and plasma fibrinogen of elderly people without comparable rise in protein C or factor X. Clinical Science 86, 43–48. [DOI] [PubMed] [Google Scholar]
- Peckova M., Fahrenbruch C.E., Cobb L.A. & Hallstrom A.P. (1999) Weekly and seasonal variation in the incidence of cardiac arrests. American Heart Journal 137, 512–515. [DOI] [PubMed] [Google Scholar]
- Smith H.E., Pryce A., Carlisle L., Jones J.M., Scarpello J. & Pantin C. (1997) Appropriateness of acute medical admissions and length of stay. Journal of Royal College of Physicians of London 5, 527–553. [PMC free article] [PubMed] [Google Scholar]
- Treanor J. & Falsey A. (1999) Respiratory viral infections in the elderly. Antiviral Research 44, 79–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyrrell D.A., Cohen S. & Schlarb J.E. (1993) Signs and symptoms in common colds. Epidemiology and Infection 111, 143–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victor C. & Khakoo A. (1994) Is hospital the right place? A survey of ‘inappropriate’ admissions to an inner London NHS trust. Journal of Public Health Medicine 3, 286–290. [PubMed] [Google Scholar]
- Woodhouse P.R., Khaw K.‐T., Plummer M., Foley A. & Meade T.W. (1994) Seasonal variations of plasma fibrinogen and factor VII activity in the elderly: winter infections and death from cardiovascular disease. Lancet 343, 435–439. [DOI] [PubMed] [Google Scholar]


