Abstract
Objectives: To estimate winter viral‐related morbidity and mortality in Tennessee nursing home residents during 4 consecutive years.
Design: A retrospective cohort study.
Setting: Three hundred eighty‐one Tennessee nursing homes.
Participants: Nursing home residents.
Measurements: Viral surveillance data were used to define three seasons: influenza (influenza and respiratory syncytial virus (RSV) cocirculating), RSV (RSV alone circulating), and non winter‐viral (neither virus circulating). Adjusted seasonal differences in rates of cardiopulmonary hospitalizations, antibiotic prescriptions, and deaths during these three seasons were calculated to estimate annual hospitalizations, courses of antibiotics, and deaths attributable to influenza and RSV from 1995 to 1999.
Results: Nursing home residents had 81,885 person‐years of follow‐up. In the 63% of residents with comorbid conditions that increase influenza morbidity, influenza infection contributed to an estimated average of 28 hospitalizations, 147 courses of antibiotics, and 15 deaths per 1,000 persons annually. Similarly, RSV accounted for an annual average of 15 hospitalizations, 76 courses of antibiotics, and 17 deaths per 1,000 persons. Influenza and RSV accounted for 7% of cardiopulmonary hospitalizations and 9% of total deaths in high‐risk residents during the 4 study years. Absolute morbidity and mortality were lower in residents without identified comorbid conditions but accounted for 15% of hospitalizations and 14% of deaths. These estimates depend on the assumption that morbidity and mortality from other respiratory viruses were distributed evenly between the three defined seasons.
Conclusion: Influenza and RSV substantially increased hospitalization rates, antibiotic use, and deaths in elderly nursing home residents each winter. These data should encourage persistent efforts toward disease prevention, and thoughtful study of vaccine development and delivery, diagnostic tools, and methods of prophylaxis and therapy.
Keywords: influenza, respiratory syncytial virus, aged persons, nursing homes
Outbreaks of influenza and respiratory syncytial virus (RSV)‐associated illness are common in nursing home settings. 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 In temperate climates like the United States, these two viruses are usually confined to winter and typically cause seasonal outbreaks of respiratory illness. 9 , 10 , 11 Nursing home residents are confined in close contact with one another and staff, presenting easy opportunity for viral spread. In addition, the high prevalence of comorbid conditions increases the risk of serious morbidity and mortality associated with influenza and RSV infections.
The effect of influenza and RSV in the nursing home population is incompletely described despite the fact that institutional outbreaks of influenza and RSV are well documented. Winter outbreaks result in attack rates of 10% to 40% for both viruses, RSV case‐fatality rates of 2% to 20%, and influenza case‐fatality rates of up to 55%. 2 , 5 , 8 , 12 , 13 , 14 , 15 , 16 , 17 One prospective study in a single nursing home over the 1989–90 winter season identified RSV as the most common viral cause of acute respiratory illness in residents. It was documented in 27% of respiratory illnesses and was more common than influenza. 18 To date, studies of nursing home patients have included only a small number of homes, usually over fewer than three winter seasons. Thus, such information about the effects of influenza and RSV may not be typical of morbidity in most nursing home residents during most years.
This study describes the first population‐based study of the effect of influenza and RSV specifically in the nursing home population. A retrospective cohort study of all persons residing in Tennessee nursing homes enrolled in the Tennessee Medicaid program was performed to determine rates of cardiopulmonary hospitalizations, antibiotic use, and deaths during 4 consecutive years, August 1995 through July 1999. The rates of these events due to influenza and RSV were estimated using active viral surveillance to determine times these viruses were circulating in Tennessee. Tennessee Medicaid is a joint federal‐state program that insures approximately 80% of persons residing in the 381 nursing homes in the state. Computerized medical data on this large population allowed quantifying the morbidity and mortality associated with influenza and RSV in the statewide nursing home population.
METHODS
Sources of Data
Linked Tennessee Medicaid files were used to define the cohort and identify outcomes of interest as previously described. 19 The enrollment file included age, sex, race, dates of enrollment, and date of death. The nursing home file included name and location of nursing home, defined as urban (Tennessee's four largest cities), other standard metropolitan statistical areas (SMSA), or rural (non‐SMSA), and dates of nursing home use. Pharmacy files provided records of all filled prescriptions. Inpatient files provided dates of all hospitalizations and International Classification of Diseases, Ninth Edition with Clinical Modifications (ICD‐9‐CM)‐coded discharge diagnoses.
Study Population
The study population included all persons enrolled in the Tennessee Medicaid program for at least 1 year from August 1, 1994, through July 31, 1999, who were nursing home residents. Persons younger than 65 were excluded because this population was small (16% of eligible person‐time) and demographically different (54% male, 39% in mental health facilities, 65% with no comorbid condition) from older residents. Persons entered the study on the first day after August 1, 1995, on which they were enrolled in Medicaid for at least 1 year and a nursing home resident. Persons were followed until loss of enrollment, movement out of the nursing home, or death or until July 31, 1999.
Viral Surveillance
The exposure, or season of viral activity, was defined based on active viral surveillance in middle Tennessee. Two sources of viral surveillance were used: all positive antigen tests and cultures for influenza, RSV, or parainfluenza viruses from the Vanderbilt University Hospital laboratory were identified, and a cohort of about 150 children, aged 5 and younger, were followed annually in the Vanderbilt Vaccine Clinic and cultured for these three viruses whenever they developed fever or respiratory symptoms. This hospital serves as a referral hospital for middle Tennessee for adults and children. By protocol, all children hospitalized for respiratory symptoms are cultured for RSV; cultures for other viruses are not consistently collected. Thus these data may not accurately reflect the actual level of individual viral activity.
Influenza season began the first day of 2 consecutive weeks with at least two influenza isolates per week and ended the last day of the 2 consecutive weeks with at least two influenza isolates per week. RSV season was similarly defined but excluded those dates classified as influenza season. In each of the 4 years, the dates of influenza season were completely encompassed by RSV season. Thus, all person time and events in the study occurred in one of three exposure periods: RSV season, when only RSV was circulating; influenza season, when both influenza and RSV were circulating; and non‐winter‐viral season, when neither RSV nor influenza was circulating.
Risk Groups
All person‐time and events after a medical encounter with diagnostic or procedure codes or filled prescriptions indicating selected comorbid conditions were classified as high risk, including (1) asthma or chronic lung disease (ICD‐9‐CM codes 277.0, 770.7, 491–496) or prescriptions filled for β‐agonists, theophylline, inhaled corticosteroids, ipratropium, cromolyn sodium, or leukotriene inhibitors; (2) diabetes mellitus (ICD‐9‐CM codes 250) or prescriptions filled for insulin or oral hypoglycemic agents; (3) chronic heart disease (ICD‐9‐CM codes 393–398, 402–404, 410–414, 415–417, 425, 428, 429, 745–747, except 747.5–747.9); (4) cancer/immunosuppressed (ICD‐9‐CM codes 140–208.9, except 173) or prescriptions filled for chemotherapeutic agents or 60 days of oral corticosteroids; (5) chronic renal or liver disease (ICD‐9‐CM codes 581–583, 585, 587, 571, 303 or dialysis procedure codes); and (6) human immunodeficiency virus (HIV) infection (ICD‐9‐CM code 042) or prescriptions filled for HIV medications. These comorbid conditions were chosen based on the current recommendations for influenza immunization. All other person‐time and events were classified as not high risk.
Study Outcomes
Study outcomes were cardiopulmonary hospitalizations (ICD‐9‐CM‐coded discharge diagnoses of pneumonia (480–486), influenza (487), acute respiratory conditions (460–466), other respiratory conditions (490–519), heart failure or myocarditis (422, 427, 428)); the number of outpatient antibiotic prescriptions filled; and death. Mortality data were obtained from linkage of Medicaid files to State of Tennessee death certificates for those deaths that occurred between 1995 and 1998. Mortality data for deaths in 1999 were not yet available from Tennessee and thus were obtained from the Medicaid database. During 3 years, 1995–98, when death certificates were available, Medicaid files captured 96% of the deaths that were linked to Tennessee death certificates each of the 3 years.
Statistical Analysis
The total person‐time and number of hospitalizations due to cardiopulmonary events were tabulated during influenza, RSV, and nonwinter seasons. All person‐time was grouped into strata based on risk status (no high‐risk and high‐risk condition). Within each risk group, rates of cardiopulmonary hospitalizations were calculated by dividing the risk‐group‐specific sum of all hospitalizations due to cardiopulmonary events by the risk‐group‐specific total person‐years during influenza, RSV, and non‐winter‐viral seasons. These and all other rates were expressed per 1,000 person‐years and were adjusted for the proportion of the year in each of the three specific seasons. Differences in hospitalization rates during influenza and RSV seasons were calculated as measures of influenza‐attributable risk. Similarly, the RSV‐attributable risk was calculated as the difference between these rates during the RSV and non‐winter‐viral seasons. Standardized rate differences were calculated as the weighted average of the strata‐specific differences in rates. Confidence intervals were computed based on large sample properties. 20 Similar analyses were performed for antibiotic courses and death rates.
RESULTS
Study Population
Residents in Tennessee's 381 nursing homes contributed 81,885 person‐years of follow‐up during the 4 study years. Twenty‐three percent of total person‐years occurred during influenza seasons when RSV was also circulating, 26% occurred during RSV seasons when only RSV was circulating, and 51% occurred during the remaining non‐winter‐viral seasons. Demographic characteristics of residents reflected a typical nursing home population; 73% were in intermediate care facilities, and 48% were in homes in rural locations (Table 1). The residents were predominantly women (79%) and white (83%), and 63% had at least one high‐risk condition. There were 402 cardiopulmonary hospitalizations, 2,416 courses of antibiotics, and 296 deaths per 1,000 person‐years.
Table 1.
Demographic Characteristics and Healthcare Use of Medicaid Enrollees Aged 65 and Older in 381 Tennessee Nursing Homes from 1995 to 1999
| Characteristic | Outcome |
|---|---|
| Total person years | 88,581 |
| Nursing home characteristics | |
| Percentage distribution of person‐time: | |
| Type of facility | |
| Intermediate care facility | 73 |
| Skilled nursing facility or general hospital | 26 |
| Mental health nursing facility | 1 |
| Facility location | |
| Urban | 26 |
| Other standard metropolitan statistical areas | 26 |
| Rural | 48 |
| Resident characteristics | |
| Percentage distribution of person‐time: | |
| Female | 79 |
| Male | 21 |
| White | 83 |
| Black | 17 |
| High risk | 63 |
| No high risk | 37 |
| Total number of events (events/1,000 person‐years) | |
| Cardiopulmonary hospitalizations | 32,881 (402) |
| Antibiotic courses | 87,585 (2,416) |
| Deaths | 22,041 (269) |
Viral Surveillance
The two viral surveillance systems detected 1,105 RSV culture or antigen‐positive tests and 235 influenza culture or antigen‐positive tests and 77 parainfluenza‐positive cultures during the 4 study years. The onset of RSV season ranged from mid‐September to early November and averaged 26 weeks in length. The onset of influenza season ranged from late November to early January and averaged 12 weeks in length. Influenza A H3N2 viruses circulated in all 4 years; in addition, influenza A H1N1 virus circulated in the first year, and influenza B viruses were detected in every year except 1997–98. There was a mean of 4.8 positive influenza tests per week during the influenza season. Only four (<2%) positive tests occurred outside this time. The average number of positive RSV tests was slightly higher in influenza season (11.2 per week) than in RSV season (9.6 per week). There were few positive RSV tests in non‐winter‐viral season (0.3 per week).
Seasonal Differences in Cardiopulmonary Hospitalizations
Cardiopulmonary hospitalization rates were consistently higher in influenza seasons than in non‐winter‐viral season and, except for the first year, higher in RSV seasons (Figure 1A). For the 4 years combined (Table 2), residents without and with identified high‐risk conditions both experienced similar seasonal increases in hospitalizations, with the peak during the portion of the year when both influenza and RSV were present. Influenza was associated with an estimated seven and 28 cardiopulmonary hospitalizations per 1,000 person‐years in those without and with high‐risk conditions, respectively. RSV was associated with an annual excess of six and 11 hospitalizations per 1,000 person‐years in these two strata. Together, influenza and RSV were responsible for 15% of hospitalizations in residents with no other defined high‐risk conditions and 7% in those in the high‐risk group.
Figure 1.
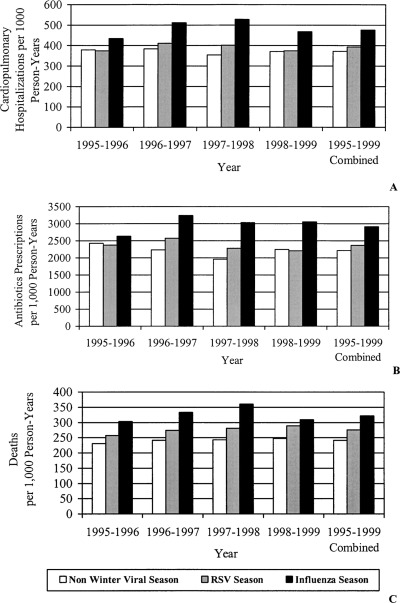
Rates of cardiopulmonary hospitalizations (A), antibiotic prescriptions (B), and deaths (C) by year, during non‐winter‐viral, respiratory syncytial virus (RSV), and influenza seasons. Panel A shows the number of cardiopulmonary hospitalizations per 1,000 person‐years. Panel B shows the number of antibiotic prescriptions per 1,000 person‐years. Panel C shows the number of deaths per 1,000 person‐years.
Table 2.
Influenza and Respiratory Syncytial Virus (RSV)‐Attributable Cardiopulmonary Hospitalizations (Events) by Risk Group, Tennessee Medicaid Nursing Home Residents from 1995 to 1999
| Rates, Events, and Person‐Years by Season | Total Rates, Events, and Person‐ Years | Estimated Annual Events Attributable to Winter Viruses per 1,000 Person‐Years* (95% Confidence Interval) | Percentage of Total Events Attributable to Winter Viruses † | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Risk Group | Influenza | RSV | Non‐winter viral | Influenza | RSV | Influenza | RSV | Both | |
| No high risk | 6.6 (4.1–9.2) | 6.0 (1.9–10.0) | 7.6 | 6.9 | 14.5 | ||||
| Hospitalizations per 1,000 person‐years | 113 | 87 | 74 | 88 | |||||
| Number of hospitalizations | 827 | 707 | 1,121 | 2,655 | |||||
| Person‐years | 7,310 | 8,075 | 15,112 | 30,497 | |||||
| High risk | 28.1 (23.4–32.9) | 11.4 (3.5–19.3) | 4.8 | 2.5 | 7.3 | ||||
| Hospitalizations per 1,000 person‐years | 707 | 571 | 545 | 588 | |||||
| Number of hospitalizations | 8,106 | 7,943 | 14,177 | 30,226 | |||||
| Person‐years | 11,459 | 13,901 | 26,029 | 51,389 | |||||
Values are weighted averages of annual excess events for a population of 1,000 persons within the specified age and risk group. The influenza excess events were calculated by multiplying the event rate difference between influenza and RSV by the proportion of overall study days in influenza season. The RSV excess events were calculated by multiplying the event rate difference between RSV and non‐winter‐viral season by the proportion of overall study days in RSV or influenza season (RSV circulated during both of these seasons). The weighted average difference in rates between influenza and RSV season and RSV season and non‐winter‐viral season were calculated with stratum‐specific person‐years in all seasons as weights; strata were defined by study year, race, sex, and nursing home location.
Percentage values are calculated by dividing the annual excess events attributable to influenza or RSV by the age and risk‐group specific total event rate.
Seasonal Differences in Antibiotic Courses
There was a consistent winter excess of antibiotic courses in both risk groups; the greatest antibiotic prescribing rate occurred when both influenza and RSV were circulating (Figure 1B, Table 3). The estimated numbers of excess antibiotic prescriptions during influenza season were 99 and 147 per 1,000 person‐years, for those without and with high‐risk conditions, respectively. RSV season was associated with an annual excess of 62 and 76 courses of antibiotics in those without and with high‐risk conditions. In both risk groups, 8% to 9% of all antibiotic courses were attributable to these two viruses.
Table 3.
Influenza and Respiratory Syncytial Virus (RSV)‐Attributable Antibiotic Courses (Events) by Risk Group, Tennessee Medicaid Nursing Home Residents from 1995 to 1999
| Risk group | Rates, Events, and Person‐Years by Season | Total Rates, Events, and Person‐Years | Estimated Annual Events Attributable to Winter Viruses per 1,000 Person‐Years* (95% Confidence Interval) | Percentage of Total Events Attributable to Winter Viruses † | |||||
|---|---|---|---|---|---|---|---|---|---|
| Influenza | RSV | Non‐winter viral | Influenza | RSV | Influenza | RSV | Both | ||
| No high risk | 99.0 (87.2–110.9) | 62.4 (43.4–81.3) | 5.3 | 3.3 | 8.6 | ||||
| Antibiotics per 1,000 person‐years | 2,263 | 1,844 | 1,716 | 1,881 | |||||
| Number of antibiotics | 16,543 | 14,889 | 25,927 | 57,359 | |||||
| Person‐years | 7,310 | 8,075 | 15,112 | 30,497 | |||||
| High risk | 146.6 (136.4–156.8) | 75.6 (58.7–92.5) | 5.4 | 2.8 | 8.2 | ||||
| Antibiotics per 1,000 person‐years | 3,331 | 2,674 | 2,503 | 2,734 | |||||
| Number of antibiotics | 38,166 | 37,176 | 65,158 | 30,226 | |||||
| Person‐years | 11,459 | 13,901 | 26,029 | 51,389 | |||||
Values are weighted averages of annual excess events for a population of 1,000 persons within the specified age and risk group. The influenza excess events were calculated by multiplying the event rate difference between influenza and RSV by the proportion of overall study days in influenza season. The RSV excess events were calculated by multiplying the event rate difference between RSV and non‐winter‐viral season by the proportion of overall study days in RSV or influenza season (RSV circulated during both of these seasons). The weighted average difference in rates between influenza and RSV season and RSV season and non‐winter‐viral season were calculated with stratum‐specific person‐years in all seasons as weights; strata were defined by study year, race, sex, and nursing home location.
Percentage values are calculated by dividing the annual excess events attributable to influenza or RSV by the age and risk‐group specific total event rate.
Seasonal Differences in Deaths
Seasonal death rates in the influenza and RSV seasons were consistently higher than death rates in non‐winter‐viral seasons and consistently peaked during influenza seasons (Figure 1C). It was estimated that influenza caused six and 15 deaths per 1,000 residents without and with high‐risk conditions, respectively (Table 4). Estimated mortality due to RSV was higher, 16 and 17 deaths per 1,000 in those without and with identified high‐risk conditions, respectively. In addition, these two winter viruses accounted for 14% and 9% of all deaths in nursing home residents in the two risk groups.
Table 4.
Influenza and Respiratory Syncytial Virus (RSV)‐Attributable Deaths (Events) by Risk Group, Tennessee Medicaid Nursing Home Residents from 1995 to 1999
| Rates, Events, and Person‐Years by Season | Total Rates, Events, and Person‐Years | Estimated Annual Events Attributable to Winter Viruses per 1,000 Person‐Years* (95% Confidence Interval) | Percentage of Total Events Attributable to Winter Viruses † | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Risk group | Influenza | RSV | Non‐winter viral | Influenza | RSV | Influenza | RSV | Both | |
| No high risk | |||||||||
| Deaths per 1,000 person‐years | 201 | 175 | 143 | 165 | 6.2 (2.7–9.8) | 16.3 (10.7–22.0) | 3.8 | 9.9 | 13.7 |
| Deaths | 1,467 | 1,411 | 2,153 | 5,031 | |||||
| Person‐years | 7,310 | 8,075 | 15,112 | 30,497 | |||||
| High risk | |||||||||
| Deaths per 1,000 person‐years | 400 | 335 | 298 | 331 | 14.5 (11.0–18.1) | 17.3 (11.5–23.3) | 3.4 | 5.2 | 8.6 |
| Deaths | 4,582 | 4,661 | 7,767 | 17,010 | |||||
| Person‐years | 11,459 | 13,901 | 26,029 | 51,389 | |||||
Values are weighted averages of annual excess events for a population of 1,000 persons within the specified age and risk‐group. The influenza excess events were calculated by multiplying the event rate difference between influenza and RSV by the proportion of overall study days in influenza season. The RSV excess events were calculated by multiplying the event rate difference between RSV and non‐winter‐viral season by the proportion of overall study days in RSV or influenza season (RSV circulated during both of these seasons). The weighted average difference in rates between influenza and RSV season and RSV season and non‐winter‐viral season were calculated with stratum‐specific person‐years in all seasons as weights; strata were defined by study year, race, sex, and nursing home location.
Percentage values are calculated by dividing the annual excess events attributable to influenza or RSV by the age and risk‐group specific total event rate.
DISCUSSION
This is the first population‐based study to quantify the morbidity and mortality associated with influenza virus or RSV in a statewide nursing home population. Previous population‐based studies did not specifically examine the nursing home population, and earlier studies based entirely on nursing homes evaluated only one or a few homes. Morbidity and mortality from influenza and RSV vary from year to year, from community to community, and from institution to institution, and an accurate estimate of disease burden requires temporal, geographic, and institutional breadth. These data, which included all nursing homes, more accurately reflect average risk over time; in any given year, a single nursing home could experience a large outbreak or no illness at all due to either of these viruses.
Cardiopulmonary hospitalizations are high in nursing home residents. Among the majority of residents who had at least one high‐risk condition, there was one hospitalization per year for every two residents. Although rates of cardiopulmonary hospitalizations were more than six times higher in residents with high‐risk conditions, the percentage of hospitalizations attributable to winter viruses was similar in both risk groups, at 5% to 15%. The absolute hospitalization rates and the approximately equal etiological contribution of RSV and influenza validate what others have found in national studies of the general population, using hospital discharge data, and prospective studies in single nursing homes or communities. 7 , 17 , 18 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 Recent surveillance data in communities confirm that influenza and RSV cause substantial morbidity in all age groups, with the contribution of each varying from year to year. 11
Nursing home residents were prescribed an average of 2.4 antibiotic courses per year. Influenza and RSV are important contributors to the large number of prescriptions filled, with the two viruses responsible for more than 8% of all courses of antibiotics in both risk groups. Perhaps most remarkably, between 9% and 14% of all deaths in persons residing in nursing homes were associated with the circulation of these two viruses. The etiological role of each virus in these deaths was virtually identical.
Another notable finding in this study was the overwhelming hospitalization, antibiotic use, and death rates of persons with chronic medical problems. Others have reported that persons with chronic illnesses are at significantly greater risk for influenza infection and its complications. 30 , 31 This study substantiates the finding and demonstrates the increase in hospitalization, antibiotic use, and death rates in high‐risk elderly during RSV season as well.
Regional viral surveillance was used for the middle Tennessee region, primarily in children, to define influenza and RSV seasons for all nursing homes in the state. Thus, these definitions are only approximate estimates of when the viruses were circulating in the state, but strong correlations between the timing of national and regional influenza viral activity and morbidity and mortality are well recognized. 10 , 30 National data indicate that RSV typically peaks in winter months, with widespread activity for up to 6 months, and that there are distinct regional patterns. 32 Thus, use of regional viral surveillance data in a largely pediatric population to define statewide viral activity is reasonable but likely results in some misclassification of seasons.
It was also assumed that influenza and RSV caused all excess cardiopulmonary hospitalizations, antibiotic courses, and deaths occurring during their respective seasons. This assumption requires that other viruses that cause respiratory illnesses, such as parainfluenza, coronavirus, and rhinovirus, were evenly divided throughout the three defined seasons and thus would not contribute to the seasonal differences in rates. This assumption is reasonable because influenza and RSV are the two main respiratory viruses with strong seasonal variations. 9 In addition, the surveillance data indicated that parainfluenza was most active in non‐winter‐viral months, which would result in an underestimation of the “excess” winter events when using non‐winter viral as the baseline. Neither coronavirus nor rhinovirus was included in the surveillance, and a differential distribution of these viruses could result in an over‐ or underestimation of the effects of influenza and RSV. Other winter factors, such as cold temperature and increased time indoors, would presumably not be important because nursing home residents encounter little seasonal environmental change.
The winter‐viral‐associated increase in hospitalization, antibiotic use, and death rates found in this study are particularly troublesome in light of the high rate of influenza vaccination in the nursing home population. During the time period of this study, estimates of influenza vaccination rates in nursing home residents were 64% to 83%. 33 , 34 Although continuing to improve vaccination rates may be helpful, future research efforts should focus on additional methods of reducing influenza disease such as increasing staff vaccination rates, improving detection and treatment of influenza outbreaks, and appropriate use of prophylactic measures.
In adults, RSV is difficult to diagnose, and treatment is largely supportive. There is currently no RSV vaccine licensed, although several RSV candidate vaccines are in human trials. Efforts at RSV prevention and detection are hindered by a low degree of suspicion for this illness in elderly adults. This lack of awareness may prove to be the greatest challenge to decreasing the effect of this illness.
The findings of this study have strong implications for future research efforts. The data reflect the need for continued study of influenza vaccine coverage, efficacy, and effectiveness and development and testing of candidate RSV vaccines in adults and children. Also, additional studies are needed to assess the role of education and other methods of prevention and treatment of illness due to both of these winter viruses in the nursing home population.
ACKNOWLEDGMENTS
The authors would like to thank Drs. Kathleen Neuzil, Tom Elasy, and James Powers for their helpful review of the manuscript and Cindy Naron and Angela Durham for editorial assistance.
This study was funded in part by a cooperative agreement with the Centers for Disease Control and Prevention UR6 CCU417579.
REFERENCES
- 1. Agius G, Dindinaud G, Biggar RJ et al An epidemic of respiratory syncytial virus in elderly people: Clinical and serological findings. J Med Virol 1990;30: 117–127. [DOI] [PubMed] [Google Scholar]
- 2. Drinka PJ, Gravenstein S, Krause P et al Outbreaks of influenza A and B in a highly immunized nursing home population. J Fam Pract 1997;45: 509–514. [PubMed] [Google Scholar]
- 3. Falsey AR. Noninfluenza respiratory virus infection in long‐term care facilities. Infect Control Hosp Epidemiol 1991;12: 602–608. [DOI] [PubMed] [Google Scholar]
- 4. Falsey AR. Respiratory syncytial virus infection in older persons. Vaccine 1998;16: 1775–1778. [DOI] [PubMed] [Google Scholar]
- 5. Goodman RA, Orenstein WA, Munro T et al Impact of influenza A in a nursing home. JAMA 1982;247: 1451–1453. [PubMed] [Google Scholar]
- 6. Libow L, Neufeld R, Olson E et al Sequential outbreak of influenza A and B in a nursing home: Efficacy of vaccine and amantadine. J Am Geriatr Soc 1996;44: 1153–1157. [DOI] [PubMed] [Google Scholar]
- 7. Mathur U, Bentley DW, Hall CB. Concurrent respiratory syncytial virus and influenza A infections in the institutionalized elderly and chronically ill. Ann Intern Med 1980;93: 49–52. [DOI] [PubMed] [Google Scholar]
- 8. Morens DM, Rash VM. Lessons from a nursing home outbreak of influenza A. Infect Control Hosp Epidemiol 1995;16: 275–280. [DOI] [PubMed] [Google Scholar]
- 9. Couch RB, Kasel JA, Glezen WP et al Influenza. Its control in persons and populations. J Infect Dis 1986;153: 431–440. [DOI] [PubMed] [Google Scholar]
- 10. Simonsen L, Clarke MJ, Williamson GD et al The impact of influenza epidemics on mortality: Introducing a severity index. Am J Public Health 1997;87: 1944–1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zambon MC, Stockton JD, Clewley JP et al Contribution of influenza and respiratory syncytial virus to community cases of influenza‐like illness: An observational study. Lancet 2001;358: 1410–1416. [DOI] [PubMed] [Google Scholar]
- 12. Coles FB, Balzano GJ, Morse DL. An outbreak of influenza A (H3N2) in a well immunized nursing home population. J Am Geriatr Soc 1992;40: 589–592. [DOI] [PubMed] [Google Scholar]
- 13. Drinka PJ, Krause P, Schilling M et al Report of an outbreak: Nursing home architecture and influenza‐A attack rates. J Am Geriatr Soc 1996;44: 910–913. [DOI] [PubMed] [Google Scholar]
- 14. Murayama N, Suzuki H, Arakawa M et al Two outbreaks of influenza A (H3N2) in a Japanese nursing home in the winter of 1996–97, with differing vaccine efficacy. Tohoku J Exp Med 1999;188: 289–298. [DOI] [PubMed] [Google Scholar]
- 15. Osterweil D, Norman D. An outbreak of an influenza‐like illness in a nursing home. J Am Geriatr Soc 1990;38: 659–662. [DOI] [PubMed] [Google Scholar]
- 16. Read CA, Mohsen A, Nguyen‐Van‐Tam JS et al Outbreaks of influenza A in nursing homes in Sheffield during the 1997–98 season: Implications for diagnosis and control. J Public Health Med 2000;22: 116–120. [DOI] [PubMed] [Google Scholar]
- 17. Sorvillo FJ, Huie SF, Strassburg MA et al An outbreak of respiratory syncytial virus pneumonia in a nursing home for the elderly. J Infect 1984;9: 252–256. [DOI] [PubMed] [Google Scholar]
- 18. Falsey AR, Treanor JJ, Betts RF et al Viral respiratory infections in the institutionalized elderly. Clinical and epidemiologic findings. J Am Geriatr Soc 1992;40: 115–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ray WA, Griffin MR. Use of Medicaid data for pharmacoepidemiology. Am J Epidemiol 1989;129: 837–849. [DOI] [PubMed] [Google Scholar]
- 20. Rothman KJ, Greenland S. Modern Epidemiology, 2nd Ed Philadelphia: Lippincott‐Raven, 1998. [Google Scholar]
- 21. Capewell A, Inglis JM, Williamson J. Respiratory syncytial virus infection in the elderly. BMJ (Clin Res ed.) 1984;288: 235–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. No authors listed. Respiratory syncytial virus infection in the elderly 1976–82. BMJ (Clin Res ed.) 1983;287: 1618–1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Morales F, Calder MA, Inglis JM et al A study of respiratory infections in the elderly to assess the role of respiratory syncytial virus. J Infect 1983;7: 236–247. [DOI] [PubMed] [Google Scholar]
- 24. Whimbey E, Ghosh S. Respiratory syncytial virus infections in immunocompromised adults. Curr Clin Top Infect Dis 2000;20: 232–255. [PubMed] [Google Scholar]
- 25. Falsey AR, Walsh EE. Respiratory syncytial virus infection in adults. Clin Microbiol Rev 2000;13: 371–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mlinaric‐Galinovic G, Falsey AR, Walsh EE. Respiratory syncytial virus infection in the elderly. Eur J Clin Microbiol Infect Dis 1996;15: 777–781. [DOI] [PubMed] [Google Scholar]
- 27. Glezen WP, Couch RB, Taber LH et al Epidemiologic observations of influenza B virus infections in Houston, Texas, 1976–77. Am J Epidemiol 1980;111: 13–22. [DOI] [PubMed] [Google Scholar]
- 28. Cameron AS, Roder DM, Esterman AJ et al Mortality from influenza and allied infections in South Australia during 1968–81. Med J Aust 1985;142: 14–17. [DOI] [PubMed] [Google Scholar]
- 29. Glezen WP, Decker M, Joseph SW et al Acute respiratory disease associated with influenza epidemics in Houston, 1981–83. J Infect Dis 1987;155: 1119–1126. [DOI] [PubMed] [Google Scholar]
- 30. Couch RB, Englund JA, Whimbey E. Respiratory viral infections in immunocompetent and immunocompromised persons. Am J Med 1997;102: 2–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Barker WH, Mullooly JP. Pneumonia and influenza deaths during epidemics: Implications for prevention. JAMA 1980;244: 2547–2549. [PubMed] [Google Scholar]
- 32. Centers for Disease Control and Prevention . Respiratory syncytial virus activity—United States 1999–2000 season. MMWR Morb Mortal Wkly Rep 2000;49: 1091–1093. [PubMed] [Google Scholar]
- 33. Advisory Committee on Immunization Practices . Prevention and control of influenza. MMWR Morb Mortal Wkly Rep 2001;50: 1–45.11215787 [Google Scholar]
- 34. Zadeh MM, Buxton BC, Thompson WW et al Influenza outbreak detection and control measures in nursing homes in the United States. J Am Geriatr Soc 2000;48: 1310–1315. [DOI] [PubMed] [Google Scholar]


