Abstract
Objectives
Helicobacter pylori stool antigen test (HpSAT) appropriateness was investigated by assessing its testing and positivity rates in Calgary, Canada.
Methods
The laboratory information system was accessed for all patients who received an HpSAT in 2018. Testing volume, test results, age, and sex of patients were collected. Sociodemographic risk factors and geospatial analysis were performed by matching laboratory data to the 2016 census data. Testing appropriateness was defined as a concordance between testing and positivity rates for each sociodemographic variable.
Results
In 2018, 25,518 H pylori stool antigen tests were performed in Calgary, with an overall positivity rate of 14.7%. Geospatial mapping demonstrated significant distribution variations of testing and positivity rates of HpSAT in the city. Certain sociodemographic groups studied (eg, recent immigrants) appeared to be appropriately tested (testing rate relative risk [RR] = 2.26, positivity rate RR = 4.32; P < .0001), while other groups (eg, male) may have been undertested (testing rate RR = 0.85, positivity rate RR = 1.14; P < .0001).
Conclusions
Determining concordance of testing and positivity rate of a laboratory test can be used for assessing testing appropriateness for other diseases in other jurisdictions. This study demonstrated some at-risk patients may be missed for H pylori testing.
Keywords: Helicobacter pylori, Stool antigen test (SAT), Census data, Geospatial mapping, Laboratory medicine
Helicobacter pylori is a gram-negative bacterium that infects the epithelial lining of the stomach and, as such, is the main cause of chronic gastritis.1 If left untreated, H pylori infections can lead to peptic ulcer disease and mucosal-associated lymphoid tissue lymphoma.2 The World Health Organization classifies H pylori as a type I carcinogen, as it is the causal agent for gastric carcinoma.3 Therefore, it is imperative that H pylori infections are diagnosed early and eradicated promptly, as appropriate intervention significantly decreases the risk of gastric carcinoma.4,5H pylori infections currently affect over half of the world’s population today. Typically, the prevalence of H pylori in resource-limited countries is higher than developed nations that have higher standards of living, access to cleaner sources of water, better hygiene, less crowded living conditions, and higher socioeconomic status.6-8 In Canada, the prevalence ranges between 15% and 95%, depending on which region, population, or testing methodology is under investigation.9-17 However, there are no published data to determine whether a general population that consists of a range of low and high risk of H pylori infections is appropriately tested.
In the United States, the American College of Gastroenterology and the Houston Consensus Conference both recommend testing H pylori in patients using noninvasive tests such as the H pylori stool antigen test (HpSAT) or urea breath test (UBT), or an invasive endoscopic biopsy in patients with active or previous peptic ulcer disease or dyspepsia.18,19 The Houston Consensus Conference further recommends testing H pylori infection in patients who are first-generation immigrants from high prevalence areas and patients of certain high-risk ethnic groups such as Latinos, African Americans, and Asian Americans.18 Similarly, in Alberta, Canada, the H pylori Primary Care Pathway also recommends patients without alarm features but with dyspepsia symptoms, current or past gastric or duodenal ulcers or upper gastrointestinal bleed, first-degree relative with a history of gastric cancer, and patients who are first-generation immigrants from Asia, Africa, and Central and South America be tested for H pylori using HpSAT or UBT.20 In January 2018, the Calgary zone implemented the HpSAT as the primary diagnostic test for H pylori infections. Guidelines and evidence support the use of this noninvasive diagnostic method.2,21-23 Therefore, this novel implementation provided an excellent opportunity to determine if the utilization of HpSAT testing is appropriate in an urban population with a diverse range of risk groups for H pylori infections.
The purpose of this study is to investigate whether the utilization of HpSAT is appropriate in an urban Canadian population by determining its testing and positivity rate at the geographic and sociodemographic levels. In this study, HpSAT testing is considered appropriate or inappropriate if there is a concordance or discordance between both testing and positivity rate of HpSAT, respectively.
Materials and Methods
Ethics Statement
Ethics approval for this study was received from the University of Calgary Conjoint Health Research Ethics Board (Ethics ID REB 13-0376).
Laboratory Data
Calgary Laboratory Services provides centralized laboratory services for the city of Calgary and surrounding areas in Alberta, performing on average 29 million tests annually for a catchment population of over 1.6 million individuals. All HpSAT tests are performed by the centralized regional Microbiology Laboratory. Each HpSAT encounter and test result for the 2018 calendar year were obtained from the laboratory information system (LIS). Thus, all patients of any age in Calgary and surrounding areas who had an HpSAT performed were represented in this cross-sectional observation study. Patients with missing information, such as age, sex, or Provincial Health Number (PHN), were excluded in the analysis. For each patient with multiple HpSATs performed for the 2018 calendar year, only the first test result was included to prevent skewing the data from patients who required confirmation of H pylori eradication after treatment.24
Census Data Linkage
To link laboratory data with Statistics Canada’s 2016 census data and Alberta Health Service’s data registries, patient PHN was used, as described previously.25-28 Briefly, individual-level sociodemographic variables, including date of birth, sex, and PHN, were collected for each patient from the LIS. Each patient’s postal code was then determined using PHNs from the Alberta Health Services Registry. The patient’s postal code allows for linkage of the patient’s HpSAT test results with the 2016 Canadian census dissemination area (CDA) in the city of Calgary. In Statistics Canada’s census data, CDAs exist as polygons that represent the smallest geographical units containing 400 to 700 individuals within each dissemination area throughout Canada.29 Potentially identifying information, including PHN, was removed for the analysis of this study. Patient data with missing PHN were excluded from the study as the PHN was required to link to the 2016 Canadian census. Group-level sociodemographic variables were then inferred from the CDA within the city of Calgary and were chosen for this study based on plausible associations with H pylori infections,7,30 which included recent immigrant status (defined as immigrating to Canada within the past 5 years), indigenous status (First Nations and Métis, the two largest indigenous populations in Calgary31), visible minorities (including Chinese, South Asian, and black, the three largest visible minority populations in Calgary31), median household income (MHI), employment rate, and education level (individuals with at least some university education). Each variable (age, sex, immigration status, ethnicity, socioeconomic status) was individually controlled for by holding all other variables constant as a reference. Therefore, each variable studied in this model has been adjusted for.
Geospatial Analysis
To investigate the geospatial distribution of testing and positivity rates of HpSAT for the patients tested for H pylori infections, the patients’ first HpSAT instance was plotted onto a map of Calgary for each of the CDA polygons and was graphically illustrated using ArcGIS v.10.3 (Esri) as described previously.26,28,32 Using hot spot analysis, the Getis-Ord Gi* statistic33 produced z scores and P values for each of the over 1,500 CDA polygons within Calgary, which determined statistically significant high or low testing or positivity rate for HpSAT in 90%, 95%, and 99% confidence levels within the CDAs.
Statistical Analysis
Testing rate for HpSAT was defined as the number of HpSAT tests performed (numerator) and the total number of patients in each CDA (denominator). The HpSAT positivity rate was calculated by dividing the total number of positive HpSAT results by the total number of HpSAT tests performed for the study period within each CDA.
A Poisson regression model (SAS version 9 software; SAS Institute) was performed to identify any statistically significant associations between the sociodemographic factors (independent variable) and the dependent variables of the proportion of HpSAT tests performed (HpSAT testing rate) or the proportion of positive HpSAT results (HpSAT positivity rate) per CDA. The sociodemographic associations were represented by the relative risk, where a value over 1.0 suggested the independent variable in question had a higher risk of being tested, or positive, for H pylori infections using HpSAT compared with its reference state. For individual-level variables, all age groups younger than 69 years and male sex were analyzed, with the reference states being age 70 years or older and female sex, respectively. Age was broken down into seven groups Table 1. Each group-level sociodemographic variable was compared with its respective reference state. For example, all indigenous populations from the 2016 census groups not included in the study were used as a reference for First Nations or Métis groups in this study. MHI was represented in units of $100,000 Canadian dollars (CAD). P < .05 was deemed statistically significant (SAS version 9 software). If both the testing and positivity rate of HpSAT were statistically significant for each sociodemographic variable, H pylori testing of patients from that sociodemographic group was considered appropriate if there was concordance of risk (eg, significantly high risk of being tested for [testing rate] and having a positive test result [positivity rate] for HpSAT).
Table 1.
Independent Associations of Sociodemographic Factors With Testing and Positivity Rates of Helicobacter pylori Stool Antigen Tests In Calgary, Canada, in 2018
| Sociodemographic Variables | Testing Rate | Positivity Rate | Concordance Between Testing and Positivity Ratesa | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Relative Risk | Confidence Limits | χ 2 | P Value | Relative Risk | Confidence Limits | χ 2 | P Value | ||
| Maleb | 0.85 | 0.82-0.87 | 126.58 | <.0001 | 1.14 | 1.08-1.21 | 19.42 | <.0001 | Discordant |
| Age, yc | |||||||||
| 0-14 | 0.30 | 0.26-0.34 | 294.14 | <.0001 | 0.91 | 0.71-1.17 | 0.55 | .4588 | — |
| 15-19 | 0.72 | 0.61-0.84 | 17.51 | <.0001 | 0.81 | 0.58-1.13 | 1.52 | .2176 | — |
| 20-29 | 0.54 | 0.49-0.59 | 177.32 | <.0001 | 1.25 | 1.04-1.49 | 5.88 | <.05 | Discordant |
| 30-39 | 0.71 | 0.65-0.76 | 74.7 | <.0001 | 1.53 | 1.32-1.77 | 32.48 | <.0001 | Discordant |
| 40-49 | 0.87 | 0.81-0.94 | 13.6 | <.001 | 1.51 | 1.29-1.76 | 26.95 | <.0001 | Discordant |
| 50-59 | 0.87 | 0.81-0.94 | 13.24 | <.001 | 1.33 | 1.15-1.55 | 14.24 | <.001 | Discordant |
| 60-69 | 1.08 | 1.00-1.16 | 4.17 | <.05 | 1.08 | 0.92-1.28 | 0.95 | .329 | — |
| Recent immigrant (within 5 years) | 2.26 | 1.25-4.09 | 7.21 | <.01 | 4.32 | 2.08-8.97 | 15.38 | <.0001 | Concordant |
| Aboriginal | |||||||||
| First Nations | 7.16 | 1.70-30.15 | 7.21 | <.01 | 98.28 | 0.75-12,803.61 | 3.41 | .0648 | — |
| Métis | 1.81 | 0.36-9.13 | 0.51 | .474 | 2.65 | 0.02-422.53 | 0.14 | .707 | — |
| Visible minority | |||||||||
| Chinese | 1.33 | 0.86-2.06 | 1.61 | .2043 | 2.24 | 1.30-3.85 | 8.5 | <.01 | — |
| South Asian | 1.36 | 1.04-1.78 | 5.08 | <.05 | 1.30 | 1.01-1.68 | 4.18 | <.05 | Concordant |
| Black | 2.20 | 1.12-4.33 | 5.28 | <.05 | 5.20 | 2.65-10.19 | 23.04 | <.0001 | Concordant |
| Median household income ($100,000) | 0.96 | 0.89-1.05 | 0.72 | .3977 | 0.84 | 0.75-0.96 | 6.97 | <.01 | — |
| Employment rate | 0.65 | 0.41-1.04 | 3.24 | .0718 | 0.73 | 0.47-1.14 | 1.94 | .1637 | — |
| Education level (at least some university) | 0.45 | 0.32-0.65 | 19.25 | <.0001 | 0.59 | 0.38-0.90 | 6.07 | <.05 | Concordant |
—, not significant.
aConcordance between statistically significant testing and positivity rate of the Helicobacter pylori stool antigen test for each sociodemographic variable.
bFemale was used as a reference group for male.
cAge group of 70 years or older was used as a reference group for all other age groups.
Results
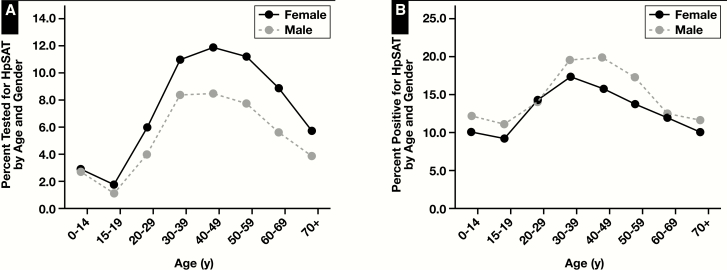
In 2018, 31,346 H pylori tests were performed in Calgary and surrounding areas, but three patients were excluded from the analysis, as their sex information was missing. Of the 31,343 unique patients who had their first H pylori test performed for the 2018 calendar year, 25,518 (81.4%) patients had an HpSAT performed, with the remainder having a UBT (n = 5,825). The overall positivity rate of HpSAT was 14.7% (females = 13.8%; males = 16.1%). Although there was a higher proportion of females being tested for H pylori infections using HpSAT for all age groups, there was a higher proportion of males with a positive HpSAT result in all age groups compared with females, except in the 20- to 29-year age group Figure 1.
Figure 1.
Although there were more females tested for Helicobacter pylori infections using the H pylori stool antigen test (HpSAT) regardless of age, there were more males with a positive test result: (A) Percent tested (total n = 25,518) for HpSAT and (B) percent positive of the patients tested for HpSAT (total n = 3,758) by age and sex in Calgary, Canada, in 2018.
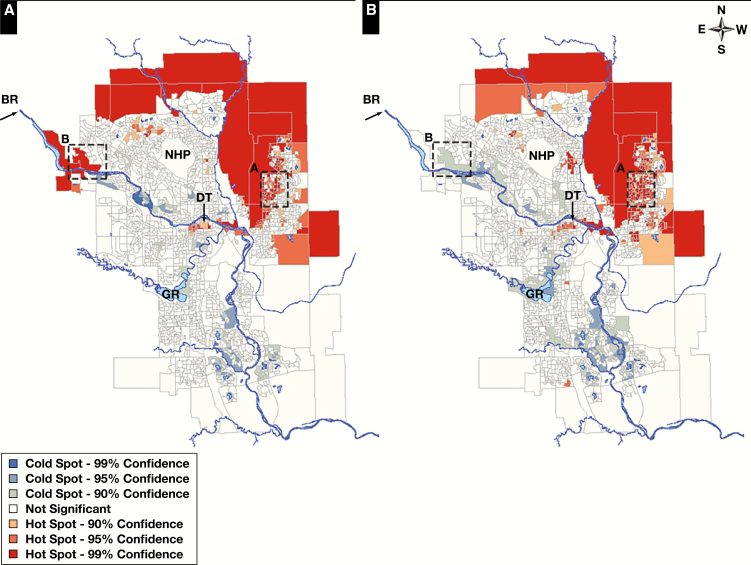
To investigate the geospatial distribution of patients being tested for and who had a positive test result for H pylori using HpSAT, testing and positivity rates for the patient’s first HpSAT encounter in Calgary in 2018 were analyzed geospatially Figure 2. There were significant geospatial variations of both testing and positivity rates for HpSAT during the study period. There was an alignment of statistically significant high testing rates with significantly high positivity rates, suggesting appropriate testing effort, within certain communities in the northeast (NE) quadrant of the city, east of downtown along the Bow River (BR), downtown area south of the BR, and some communities northwest (NW) of Nosehill Park. There was also an alignment of significantly low testing with low positivity rates within some of the communities in the NW quadrant of the city along the BR, in the far south communities along the BR, and surrounding the Glenmore Reservoir in the southwest (SW) quadrant of the city. A discordance between HpSAT testing and positivity rate, or poor testing effort, was observed in the communities in the westerly edge of the city along the BR, as HpSAT testing rate was significantly high, while positivity rate was significantly low (see Figure 2 for details).
Figure 2.
There were discernable geospatial variations in Helicobacter pylori stool antigen test (HpSAT) testing and positivity rates in Calgary, Canada. The city of Calgary is divided into four quadrants—northwest, northeast, southwest, and southeast (see compass on top-right corner for orientation)—where the intersection of the four quadrants is located at the center of downtown (DT). HpSAT testing rates (left) and HpSAT positivity rates (right) for the patient’s first HpSAT encounter in the 2018 calendar year for each census dissemination area in Calgary. Select examples of neighborhoods (dashed boxes) with an alignment (A) or a misalignment (B) between testing and positivity rates of HpSAT. Visually, it would appear there was an alignment of testing and positivity rates of HpSAT in numerous communities of Calgary. Red (statistically significant at 90% to 99% confidence, hot spot analysis) represents significantly high testing or positivity rates, and blue (statistically significant 90% to 99% confidence, cold spot analysis) represents significantly low testing or positivity rates. BR, Bow River; GR, Glenmore Reservoir; NHP, Nose Hill Park.
Sociodemographic risk associations were also investigated, where H pylori testing using HpSAT was defined as appropriate in this study if there was a concordance between statistically significant risk of being both tested (testing rate) and positive (positivity rate) for HpSAT per census dissemination area. All individual-level and group-level sociodemographic variables analyzed were adjusted for, thus making any significant associations an independent risk contribution. Inappropriate testing effort was found in sex, as there was a discordance between testing and positivity rates of HpSAT. Poisson regression revealed that males were significantly less likely to be tested for H pylori using HpSAT but had a markedly higher likelihood of having a positive test result compared with females per CDA. Misalignment between testing and positivity rate was also found in various age groups for HpSAT. During the study period, only those between 20 and 59 years of age were at a significantly higher risk of having a positive H pylori infection. However, anyone between birth and age 59 years was significantly less likely to be tested for H pylori infections, while those who were 60 years and older were significantly more likely to be tested using HpSAT (see Table 1 for details).
Poisson regression also revealed there were appropriate testing efforts for recent immigrants, visible minority South Asian individuals, and visible minority black individuals in this study as their significant risk of being tested for H pylori (HpSAT testing rate) mirrored their risk of being positive for infection (HpSAT positivity rates). Individuals who were indigenous First Nations in Calgary were also much more likely to be tested for H pylori infections using HpSAT compared with other indigenous groups and had a very high (but nonstatistically significant) likelihood of having a positive test result (see Table 1 for details).
Only those who had at least some university education were both significantly less likely to be tested for H pylori infections and less likely to have a positive HpSAT result, while employment had no effect on HpSAT testing and positivity rates. For every $100,000 CAD increase in median household income, the risk of having a positive HpSAT result decreased significantly by 16%. See Table 1 for more details of concordance or discordance between testing and positivity rates for each sociodemographic variable.
Discussion
To our knowledge, this is the first population-based study that provided evidence for appropriate or inappropriate testing for specific sociodemographic groups for a major infectious disease: H pylori infection. In this study, a method to determine whether HpSAT is used appropriately in a major urban population of over 1.6 million individuals in Calgary, Alberta, Canada, was presented. When laboratory data were linked with census data, geospatial analysis demonstrated significant variations of testing and positivity rates of HpSAT within the city but also displayed an alignment of testing effort within certain communities in the city. In Calgary, a high proportion of recent immigrants resides in the NE communities and in certain NW neighborhoods in the city, while a low proportion lives in the southern communities in Calgary.34 Depending on the country of origin, it is well established that recent immigrants are at a high risk for H pylori infections,6,7,30 and we observed that there is an appropriate testing effort for those residing in the NE communities, where there is a higher burden for disease. On the other hand, studies have found that those with a higher socioeconomic status, such as high levels of education, employment, and/or income, are at a lower risk of infection.8,30 In Calgary, certain SW and western quadrants of the city that tend to have a higher median household income and postsecondary education34 also have a significantly lower risk of having a positive HpSAT result. By mapping the patients’ postal codes with their test results, a bird’s-eye view of testing and positivity rates of HpSAT demonstrated an overall alignment between the two, suggesting testing effort is appropriate at the population level.
In the United States and Alberta, Canada, guidelines and consensus groups recommend patients without alarm features but with symptoms of dyspepsia or gastric peptic ulcers and who are first-generation immigrants from South or Central America, Africa, or Asia be tested for H pylori infection using HpSAT.18,20 Although geospatial analysis suggested HpSAT testing was appropriate for those who reside in neighborhoods with a high burden of disease, following an in-depth sociodemographic risk association analysis, results clearly showed that certain sociodemographic groups were appropriately tested as per practice recommendations (eg, those who recently immigrated to Canada, who identified as visible minority South Asian or visible minority black). This study also demonstrated those with at least some university education also appeared to be appropriately tested (ie, concordance between testing and positivity rates), while others may not be. For example, males and those between age 20 and 59 years were at risk for being undertested, so H pylori infection may be missed. None of the sociodemographic groups investigated appeared to be significantly overtested (ie, significant low positivity rate but high testing rate risk) for H pylori infections using HpSAT.
Studies find that adult men are at a higher risk of having an H pylori infection.35,36 Similarly, our study demonstrated that although females were more likely to be tested for an H pylori infection using HpSAT, males were at a significantly higher risk of having a positive HpSAT result. Studies have hypothesized that this may be due to women being more likely to seek health care earlier than men, are more likely to obtain antibiotics, and may be protected from infections due to a heightened immune response from estrogen.37,38 Although we observed this discordance between testing and positivity in males and females of all ages, males were less likely to be tested than females in our study, which may be due to men not visiting their primary care providers as often as women do, especially if they do not have multiple comorbidities.39,40 Perhaps there should be enhanced efforts of testing males for H pylori infections in Calgary if clinical indications are presented. It may be of interest in the future to match laboratory data with the patients’ visiting frequency to their primary care providers to verify if the lack of health care exposure is a major reason for increased risk of persistent infection.
Children in developed countries are less likely to have H pylori infections than children in resource-limited countries,8,41 which echoes what was observed in this study, as those younger than 20 years did not have a significantly high risk of being positive for H pylori. However, adults between 20 and 59 years of age were at a significantly higher risk of having a positive HpSAT result compared with the other age groups in Calgary. Similar to other studies,9,14 we also found that the risk of an H pylori infection increased with age in adults. In the population of Calgary, as age increased from 20 to 59 years, its positivity risk peaked in the 30- to 39-year age group. Unfortunately, the same age groups were also significantly less likely to be tested for H pylori infections, with those between ages 20 to 29 years being the least likely to be tested. This may not be due to physician ordering practices; rather, adult patients who are not elderly, who believe they are relatively healthy, and who do not have multiple comorbidities tend to not visit their primary care providers as often, comparatively.39,42,43 We remind physicians that patients of any age with a high pretest probability of H pylori infections should be tested early for prompt treatment.
In Canadian indigenous groups, the prevalence of H pylori infections ranges widely up to 95% and is region, population, and testing methodology specific.11,16,44,45 Here, we observed that although First Nations people who resided in Calgary were more likely to be tested, possibly due to their high risk of infection, they were not at a significantly higher risk of being H pylori positive (although the trend for a positive test result was present). This may be due to indigenous First Nations individuals living in a large urban center such as Calgary having easier access to health care and a higher socioeconomic status than those living in rural or remote communities in Canada,16,46 thereby decreasing their risk of having an H pylori infection through early detection and treatment. Also, possible cosegregation with other unmeasured socioeconomic or clinical variables may have resulted in a nonstatistically significant increase in the risk of having a positive HpSAT result.
Evidence suggests that those who are of Chinese descent are also at a high risk of developing H pylori infections.6,47 In Calgary, those who identified as visible minority Chinese may have been undertested using the HpSAT, as there was a discordance between a significantly high risk of positivity rate but a nonsignificant testing rate in this group. In Calgary, those who identified as visible minority South Asian and black were appropriately tested for H pylori infections, as supported by evidence of being at a higher risk of infection in other jurisdictions.6,7,47
There is a potential link between lower socioeconomic status and risk of developing H pylori infections due to poor hygiene, close living conditions, and poor nutrition.7,8 Similar to other review studies,7,30 our results also suggested that those with a higher socioeconomic status in terms of having had at least some university education or a high income were at a significantly lower risk of being H pylori positive, at 41% and 16% less risk, respectively. Although there are studies of health care occupational risks with acquiring an H pylori infection,48 we did not observe any significance in both testing and positivity rates of HpSAT in those who are employed compared with unemployed in this study.
Limitations
Although the stool antigen test was implemented in January 2018 as the primary diagnostic test for H pylori infections and confirmation of eradication, HpSAT was available for use prior to that in Calgary. Since we included only the first HpSAT encounter for each patient in the 2018 calendar year, we were not able to distinguish between which tests were used for diagnosis and which were used to confirm eradication following treatment. As such, the true-positive rate may be underestimated in this instance. However, when we included all HpSAT tests performed for the 2018 calendar year, only a small percentage of those tests was repeated for patients included in the study (8%; data not shown).
Moreover, the HpSAT testing rate may not be the true testing rate as there may be individuals who had an active H pylori infection but did not visit their doctor for a diagnosis. Conversely, patients may have received the laboratory requisition from their physician for HpSAT testing but did not drop off their stool sample to have the test performed. In future, it may be of value to match laboratory data (eg, HpSAT performed) with clinical data (eg, diagnosis of dyspepsia, peptic ulcer disease) to determine the frequency of HpSAT performed per diagnosis per patient.
As the laboratory data were matched with each patient’s postal code from the 2016 census data for the geospatial analysis, the statistically significant high/low testing or positivity rate for HpSAT represented the patient’s residential location at the time of the census rather than testing or physician ordering locations. Despite this limitation, there was still concordance between testing and positivity rates of HpSAT in the NE quadrants of the city, which has a proportionately higher percentage of recent immigrants living in those neighborhoods.34
Despite these limitations, we have demonstrated a method that can be applied to any laboratory test in any jurisdiction to assess testing appropriateness of infections or other diseases by using only secondary laboratory and public census data.
Conclusions
In this population-based study, there were statistically significant geospatial variations in both testing and positivity rates of HpSAT in a large Canadian urban center. Although geographically HpSAT appears to be appropriately tested in communities with a high or low burden of disease, it would appear that certain sociodemographic groups who would benefit from testing and subsequent treatment may be missed. We remind physicians that certain sociodemographic groups are at a higher risk for an H pylori infection and that there should be enhanced efforts to provide earlier diagnosis and eradication options for those patients. Results from this study may be useful to assist policy makers and primary care providers to strategize on enhanced screening approaches of high-risk sociodemographic groups and neighborhoods identified in this study. It may be of interest to analyze and compare results from this study with other jurisdictions across Canada using the same model, as the results shown here may be specific to this particular jurisdiction.
Acknowledgments
We thank the members of the research team who provided valuable insights and feedback for this study.
This study was supported by the Canadian Institutes of Health Research Foundation Scheme (RN254781-333204 to C.N.). The funding body did not have a role in the design of the study; in the collection, analysis, and interpretation of data; and in writing the manuscript.
References
- 1. Vogiatzi P, Cassone M, Luzzi I, et al. Helicobacter pylori as a class I carcinogen: physiopathology and management strategies. J Cell Biochem. 2007;102:264-273. [DOI] [PubMed] [Google Scholar]
- 2. Bjorkman DJ, Steenblik M. Best practice recommendations for diagnosis and management of Helicobacter pylori–synthesizing the guidelines. Curr Treat Options Gastroenterol. 2017;15:648-659. [DOI] [PubMed] [Google Scholar]
- 3. IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Schistosomes, Liver Flukes and Helicobacter Pylori. Lyon, France: International Agency for Research on Cancer; 1994. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, No. 61. [PMC free article] [PubMed] [Google Scholar]
- 4. Wong BC, Lam SK, Wong WM, et al. ; China Gastric Cancer Study Group Helicobacter pylori eradication to prevent gastric cancer in a high-risk region of China: a randomized controlled trial. JAMA. 2004;291:187-194. [DOI] [PubMed] [Google Scholar]
- 5. Wu CY, Kuo KN, Wu MS, et al. Early Helicobacter pylori eradication decreases risk of gastric cancer in patients with peptic ulcer disease. Gastroenterology. 2009;137:1641-1648.e1. [DOI] [PubMed] [Google Scholar]
- 6. Hooi JKY, Lai WY, Ng WK, et al. Global prevalence of Helicobacter pylori infection: systematic review and meta-analysis. Gastroenterology. 2017;153:420-429. [DOI] [PubMed] [Google Scholar]
- 7. Eusebi LH, Zagari RM, Bazzoli F. Epidemiology of Helicobacter pylori infection. Helicobacter. 2014;19(suppl 1):1-5. [DOI] [PubMed] [Google Scholar]
- 8. Khalifa MM, Sharaf RR, Aziz RK. Helicobacter pylori: a poor man’s gut pathogen? Gut Pathog. 2010;2:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Veldhuyzen van Zanten SJ, Pollak PT, Best LM, et al. Increasing prevalence of Helicobacter pylori infection with age: continuous risk of infection in adults rather than cohort effect. J Infect Dis. 1994;169:434-437. [DOI] [PubMed] [Google Scholar]
- 10. Pérez-Pérez GI, Bhat N, Gaensbauer J, et al. Country-specific constancy by age in cagA+ proportion of Helicobacter pylori infections. Int J Cancer. 1997;72:453-456. [DOI] [PubMed] [Google Scholar]
- 11. Bernstein CN, McKeown I, Embil JM, et al. Seroprevalence of Helicobacter pylori, incidence of gastric cancer, and peptic ulcer-associated hospitalizations in a Canadian Indian population. Dig Dis Sci. 1999;44:668-674. [DOI] [PubMed] [Google Scholar]
- 12. Sinha SK, Martin B, Sargent M, et al. Age at acquisition of Helicobacter pylori in a pediatric Canadian First Nations population. Helicobacter. 2002;7:76-85. [DOI] [PubMed] [Google Scholar]
- 13. Sinha SK, Martin B, Gold BD, et al. The incidence of Helicobacter pylori acquisition in children of a Canadian First Nations community and the potential for parent-to-child transmission. Helicobacter. 2004;9:59-68. [DOI] [PubMed] [Google Scholar]
- 14. Naja F, Kreiger N, Sullivan T. Helicobacter pylori infection in Ontario: prevalence and risk factors. Can J Gastroenterol. 2007;21:501-506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jones N, Chiba N, Fallone C, et al. ; Canadian Helicobacter Study Group Participants Helicobacter pylori in First Nations and recent immigrant populations in Canada. Can J Gastroenterol. 2012;26:97-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sethi A, Chaudhuri M, Kelly L, et al. Prevalence of Helicobacter pylori in a First Nations population in northwestern Ontario. Can Fam Physician. 2013;59:e182-e187. [PMC free article] [PubMed] [Google Scholar]
- 17. Colmers-Gray IN, Vandermeer B, Greidanus RI, et al. Helicobacter pylori status among patients undergoing gastroscopy in rural northern Alberta. Can Fam Physician. 2016;62:e547-e554. [PMC free article] [PubMed] [Google Scholar]
- 18. El-Serag HB, Kao JY, Kanwal F, et al. Houston consensus conference on testing for Helicobacter pylori infection in the United States. Clin Gastroenterol Hepatol. 2018;16:992-1002.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Randel A. H. pylori infection: ACG updates treatment recommendations. Am Fam Physician. 2018;97:135-137. [PubMed] [Google Scholar]
- 20. Alberta Health Services. Helicobacter pylori (H. pylori) primary care pathway. 2019. https://www.albertahealthservices.ca/assets/info/hp/sharp/if-hp-sharp-hpylori-pathway.pdf. Accessed November 18, 2019. [Google Scholar]
- 21. Falsafi T, Valizadeh N, Sepehr S, et al. Application of a stool antigen test to evaluate the incidence of Helicobacter pylori infection in children and adolescents from Tehran, Iran. Clin Diagn Lab Immunol. 2005;12:1094-1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gisbert JP, de la Morena F, Abraira V. Accuracy of monoclonal stool antigen test for the diagnosis of H. pylori infection: a systematic review and meta-analysis. Am J Gastroenterol. 2006;101:1921-1930. [DOI] [PubMed] [Google Scholar]
- 23. Fong E, Nguyen H, Kitt S, et al. 1995. Implementation of Helicobacter pylori stool antigen testing in a large metropolitan centre: a prospective comparative diagnostic trial. Open Forum Infect Dis. 2018;5(suppl 1):S580. [Google Scholar]
- 24. Towards Optimized Practice Working Group for H. pylori. Diagnosis and treatment of Helicobacter pylori infection in adults—clinical practice guideline. 2016. http://www.topalbertadoctors.org/download/362/h_pylori_guideline.pdf?_20160620094824. Accessed August 27, 2019. [Google Scholar]
- 25. de Koning L, Henne D, Woods P, et al. Sociodemographic correlates of 25-hydroxyvitamin D test utilization in Calgary, Alberta. BMC Health Serv Res. 2014;14:339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gorday W, Sadrzadeh H, de Koning L, et al. Association of sociodemographic factors and prostate-specific antigen (PSA) testing. Clin Biochem. 2014;47:164-169. [DOI] [PubMed] [Google Scholar]
- 27. Crouse A, Sadrzadeh SM, de Koning L, et al. Sociodemographic correlates of fecal immunotesting for colorectal cancer screening. Clin Biochem. 2015;48:105-109. [DOI] [PubMed] [Google Scholar]
- 28. Griener TP, Naugler C, Chan WW, et al. Sociodemographic correlates of urine culture test utilization in Calgary, Alberta. BMC Urol. 2018;18:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Statistics Canada. Dictionary, Census of Population, 2016—dissemination area (DA). 2016. https://www12.statcan.gc.ca/census-recensement/2016/ref/dict/geo021-eng.cfm. Accessed April 12, 2019. [Google Scholar]
- 30. Calvet X, Ramírez Lázaro MJ, Lehours P, et al. Diagnosis and epidemiology of Helicobacter pylori infection. Helicobacter. 2013;18(suppl 1):5-11. [DOI] [PubMed] [Google Scholar]
- 31. Statistics Canada. Calgary, CMA, Alberta (Code 325) (Table). National Household Survey (NHS) Profile. Ottawa, Canada: Statistics Canada; 2013. Cat No. 99-004-XWE. [Google Scholar]
- 32. Barber J, Guo M, Nguyen LT, et al. Sociodemographic correlates of clinical laboratory test expenditures in a major Canadian City. Am J Clin Pathol. 2017;148:91-96. [DOI] [PubMed] [Google Scholar]
- 33. Mitchell A, ed. The ESRI Guide to GIS Analysis: Volume 2. Spatial Measurements and Statistics. Redlands, CA: ESRI Press; 2005. [Google Scholar]
- 34. Naugler C, Zhang J, Henne D, et al. Association of vitamin D status with socio-demographic factors in Calgary, Alberta: an ecological study using Census Canada data. BMC Public Health. 2013;13:316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. de Martel C, Parsonnet J. Helicobacter pylori infection and gender: a meta-analysis of population-based prevalence surveys. Dig Dis Sci. 2006;51:2292-2301. [DOI] [PubMed] [Google Scholar]
- 36. Woodward M, Morrison C, McColl K. An investigation into factors associated with Helicobacter pylori infection. J Clin Epidemiol. 2000;53:175-181. [DOI] [PubMed] [Google Scholar]
- 37. Thompson AE, Anisimowicz Y, Miedema B, et al. The influence of gender and other patient characteristics on health care-seeking behaviour: a QUALICOPC study. BMC Fam Pract. 2016;17:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ferro A, Morais S, Pelucchi C, et al. Sex differences in the prevalence of Helicobacter pylori infection: an individual participant data pooled analysis (StoP Project). Eur J Gastroenterol Hepatol. 2019;31:593-598. [DOI] [PubMed] [Google Scholar]
- 39. Schlichthorst M, Sanci LA, Pirkis J, et al. Why do men go to the doctor? Socio-demographic and lifestyle factors associated with healthcare utilisation among a cohort of Australian men. BMC Public Health. 2016;16:1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Banks I. No man’s land: men, illness, and the NHS. BMJ. 2001;323:1058-1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Segal I, Otley A, Issenman R, et al. Low prevalence of Helicobacter pylori infection in Canadian children: a cross-sectional analysis. Can J Gastroenterol. 2008;22:485-489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Mäntyselkä P, Kumpusalo E, Ahonen R, et al. Pain as a reason to visit the doctor: a study in Finnish primary health care. Pain. 2001;89:175-180. [DOI] [PubMed] [Google Scholar]
- 43. Vegda K, Nie JX, Wang L, et al. Trends in health services utilization, medication use, and health conditions among older adults: a 2-year retrospective chart review in a primary care practice. BMC Health Serv Res. 2009;9:217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. McKeown I, Orr P, Macdonald S, et al. Helicobacter pylori in the Canadian arctic: seroprevalence and detection in community water samples. Am J Gastroenterol. 1999;94:1823-1829. [DOI] [PubMed] [Google Scholar]
- 45. Goodman KJ, Jacobson K, Veldhuyzen van Zanten S. Helicobacter pylori infection in Canadian and related Arctic Aboriginal populations. Can J Gastroenterol. 2008;22:289-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wei T, Hansen J, Office of Statistics and Information—Demography National Household Survey—Aboriginal People in Alberta: A Regional Perspective. Alberta, Canada: Alberta Government; 2016. http://www.finance.alberta.ca/aboutalberta/osi/census/2011/2011-national-household-survey-release1-Aboriginal-Peoples.pdf. Accessed April 12, 2019. [Google Scholar]
- 47. Goh KL, Parasakthi N. The racial cohort phenomenon: seroepidemiology of Helicobacter pylori infection in a multiracial South-East Asian country. Eur J Gastroenterol Hepatol. 2001;13:177-183. [DOI] [PubMed] [Google Scholar]
- 48. Magalhães Queiroz DM, Luzza F. Epidemiology of Helicobacter pylori infection. Helicobacter. 2006;11(suppl 1):1-5. [DOI] [PubMed] [Google Scholar]