Abstract
Introduction
Intra-abdominal hypertension (IAH) is a well-known phenomenon in critically ill patients. Effects of a moderately elevated intra-abdominal pressure (IAP) on lung mechanics are still not fully analyzed. Moreover, the optimal positive end-expiratory pressure (PEEP) in elevated IAP is unclear.
Methods
We investigated changes in lung mechanics and transformation in histological lung patterns using three different PEEP levels in eighteen deeply anesthetized pigs with an IAP of 10 mmHg. After establishing the intra-abdominal pressure, we randomized the animals into 3 groups. Each of n = 6 (Group A = PEEP 5, B = PEEP 10 and C = PEEP 15 cmH2O). End-expiratory lung volume (EELV/kg body weight (bw)), pulmonary compliance (Cstat), driving pressure (ΔP) and transpulmonary pressure (ΔPL) were measured for 6 hours. Additionally, the histological lung injury score was calculated.
Results
Comparing hours 0 and 6 in group A, there was a decrease of EELV/kg (27±2 vs. 16±1 ml/kg; p<0.05) and of Cstat (42±2 vs. 27±1 ml/cmH2O; p<0.05) and an increase of ΔP (11±0 vs. 17±1 cmH2O; p<0.05) and ΔPL (6±0 vs. 10±1 cmH2O; p<0.05). In group B, there was no significant change in EELV/kg (27±3 vs. 24±3 ml/kg), but a decrease in Cstat (42±3 vs. 32±1 ml/cmH20; p<0.05) and an increase in ΔP (11±1 vs. 15±1 cmH2O; p<0.05) and ΔPL (5±1 vs. 7±0 cmH2O; p<0.05). In group C, there were no significant changes in EELV/kg (27±2 vs. 29±3 ml/kg), ΔP (10±1 vs. 12±1 cmH2O) and ΔPL (5±1 vs. 7±1 cmH2O), but a significant decrease of Cstat (43±1 vs. 37±1 ml/cmH2O; p<0.05). Histological lung injury score was lowest in group B.
Conclusions
A moderate elevated IAP of 10 mmHg leads to relevant changes in lung mechanics during mechanical ventilation. In our study, a PEEP of 10 cmH2O was associated with a lower lung injury score and was able to overcome the IAP induced alterations of EELV.
Introduction
The interactions between the abdominal and the thoracic compartments represent a challenge for ICU physicians [1, 2]. Approximately 50% of intra-abdominal pressure (IAP) is transmitted to the intrathoracic compartment [3–6]. It therefore has a direct impact on functional residual capacity (FRC), end-expiratory lung volume (EELV), driving pressure (ΔP) and transpulmonary pressure (ΔPL). Almost half of the patients admitted to the ICUs worldwide develop intra-abdominal hypertension (IAH). Two-thirds of these cases were already present on the day of ICU admission [7]. An elevated IAP can be classified as follows: 1. intra-abdominal hypertension (IAH) with an IAP above 12 mmHg and 2. abdominal compartment syndrome with an IAP above 20 mmHg [8, 9]. Both are an independent risk factor for organ failure and mortality in the ICU [1, 7].
Clinical studies on critically ill patients identified an average IAP of 10 mmHg in supine position [1, 10, 11]. Moderate elevated IAP also occurs in obesity, pregnancy and during anesthesia [12–14]. The role of this moderate elevated IAP on lung mechanics and potential organ failure is yet not fully analysed.
We therefore analysed the effect of a moderate elevated IAP of 10 mmHg on lung mechanics in a porcine model up to 6 hours. To investigate the consequences of different PEEP levels, we used three levels of PEEP (5, 10, 15 cmH2O). The hypothesis in our study was that a PEEP of 10 cmH2O in moderate elevated IAP (10 mmHg) is protective by reducing lung injury and preserving the EELV during mechanical ventilation.
Materials and methods
Animal preparation and instrumentation
The protocol was approved by the responsible committee for animal research (Regierungspräsidium Karlsruhe, No. 35–9185.81/G-161/17). The animals were kept within the interfacultary biomedical faculty of the university of Heidelberg and were provided by a local pig breeder. All proceedings were in accordance with animal welfare notes regulated by German law. After overnight fasting with free access to water, 18 female domestic pigs were anaesthetized intramuscularly in combination with 7 mg/kg Azaperon (Stresnil®, Lilly, Bad Homburg, Germany), 8 mg/kg Ketaminhydrochlorid 10% (Ketamin10%®, Bremer Pharma, Warburg, Germany) and 0.3 mg/kg Midazolam (Midazolam, Hameln Pharma, Hameln, Germany). Anaesthesia was maintained by continuous infusion of 6 mg/kg/h Ketanest S (Pfizer Pharma, Berlin, Germany), 3.6 mg/kg/h Midazolam and 10–30 mg/kg/h Propofol 2% (Propofol, Fresenius Kabi, Bad Homburg, Germany). There was no use of neuromuscular blockers. Adequacy of the depth of anaesthesia was regularly assessed by absence of spontaneous breathing efforts and lack of muscle tone.
After induction of anaesthesia the pigs were tracheotomised and ventilated with an intensive care ventilator (Carescape R860, GE Healthcare, Madison, USA) using an inspiratory oxygen concentration (FiO2) of 0.4 in a pressure-controlled mode with volume guaranty. Also, a tidal volume of 8 ml/kg body weight, an inspiration/expiration ratio of 1:2 and a PEEP of 5 cmH2O was provided.
A 5F thermistor-tipped catheter (PiCCO®, Pulsion Medical systems, Feldkirchen, Germany) and a central venous catheter (Logicath, Smiths Medical, Grasbrunn, Germany) were inserted with ultrasound guidance. Crystalloid solution (Sterofundin ISO, Braun, Melsungen, Germany) was infused to keep the study population hemodynamically stable during the experiment. A polyethylene catheter (Nutrivent multifunction nasogastric catheter, Sidam, San Glacomo Roncole, Italy) was used to measure esophageal pressure. Appropriate catheter position was confirmed as previously described [15].
After a midline laparotomy a large intra-abdominal balloon (200-litre weather balloon, Stratoflight, Blomberg, Germany) was placed in the peritoneal cavity. Correct position in all abdominal quadrants was ensured by visual inspection and partial inflation. The abdomen was carefully closed. A urine catheter was placed in the bladder.
Measurements and calculations
Peak inspiratory airway pressure (PInsp), PEEP, inspiratory esophageal pressure (PEsInsp) and end-expiratory esophageal pressure (PEsExp) were recorded from the ventilator. ΔP and ΔPL were calculated as previously described [16]. Transpulmonary inspiratory pressure (TPPInsp) was calculated as TTPInsp = PInsp—PEsInsp and transpulmonary expiratory pressure (TPPExp) as TPPExp = PEEP—PEsExp. CStat was measured by the ventilator during an inspiratory hold. Elastance of the respiratory system (ERS) was calculated as ERS = (PInsp—PEEP) / VT, chest wall elastance (ECW) as ECW = (PEsInsp—PEsExp) / VT and elastance of the lung (EL) as EL = ERS—ECW.
We measured EELV bedside as previously described [17] without interrupting mechanical ventilation on the designated PEEP level. CI (cardiac index) was calculated with the PiCCO® System. End-expiratory IAP (IAPEndex) was measured as recommended [18, 19] and zeroed at midaxillary level [20]. P/F ratio was calculated based on the ratio of partial arterial pressure of oxygen to FiO2.
Experimental protocol
Data were assessed after a 30 minutes stabilization period (H0). The abdominal balloon was then filled with water up to an IAPEndex of 10 mmHg. We randomized into group A (n = 6) with a PEEP of 5, group B (n = 6) = PEEP 10 and group C (n = 6) = PEEP 15 cmH2O for 6 hours (H6) (Fig 1).
Fig 1. Experimental model study protocol.
After instrumentation and a 30-min stabilization period animals underwent measurements at H0 with PEEP 5 and no elevated intraabdominal pressure (IAP). Thereafter the intraabdominal balloon was filled with water up to an IAP of 10 mmHg. Animals were randomized afterwards to the three different groups with group A: PEEP 5 cmH2O, group B: PEEP 10 cmH2O and group C: PEEP 15 cmH2O. The IAP was held at 10 mmHg for 6 hours.
At the end of the experimental protocol, the pigs were euthanized with an intravenous bolus of 200 mg Propofol followed by 40mmol potassium chloride. We exposed the complete right lung and regional lung samples were extracted to evaluate wet-dry weight ratio and to perform histological examination.
Histology
Samples from the anterior, medial and dorsal position of the medial lobe were selected and immediately fixed in formalin. After fixation, the tissue samples were dehydrated and embedded. The sections were stained with hematoxylin and eosin. A pathologist, blinded to the study variables, evaluated each sample histologically to determine a lung injury score. To quantify the extent of histologic lung injury the pathologist used a lung injury scoring system [21] (S1 Table). Five independent variables were scored to generate the lung injury score. The sum of each of the five independent variables were weighted according to the relevance for acute lung injury [21]. The resulting lung injury score ranges from 0 to 1. Zero represents minimal to no damage and 1 the worst damage possible.
Wet-dry weight ratio
Wet-dry weight ratio was measured in samples of the medial lobe. Samples were weighed, dried and then weighted again.
Statistical analysis
Sample size was calculated based on the expected alterations in EELV using data from previous studies performed in our lab.
Statistical analysis was performed using SPSS (Version 25). H0 values and lung injury score were analyzed using a one-way ANOVA. In case of significance a post hoc analyze with a correction for multiple tests were performed. We used ANCOVA for comparing H0 with H6 data with post hoc analysis. Data are expressed as mean ± SEM (standard error of the mean). For all tests, P ≤ 0.05 was considered statistically significant.
Results
We included 18 animals in this study with a weight of 47 ± 1 kg. There were no significant differences at H0 among the experimental groups with the exeption of the significant higher heart rate of group B compared to group A.
Lung mechanics, hemodynamic parameters and oxygenation
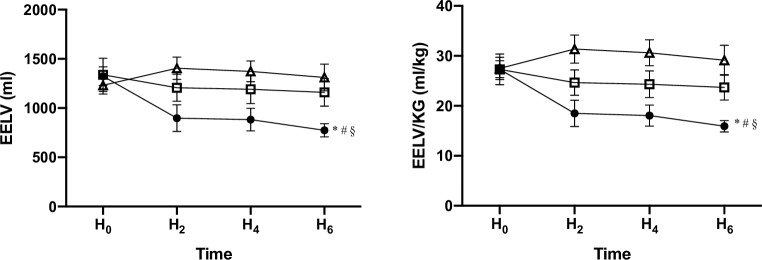
When compared with data at H0 we observed several alterations after 6 hours of mechanical ventilation (H6) (Table 1). In group A EELV (1323±95 vs. 774±67; p<0.05), EELV/kg bw (27±2 vs. 16±1 ml/kg; p<0.05) (Figs 2 and 3) and Cstat (42±2 vs. 27±1 ml/cmH2O; p<0.05) decreased (S1 Fig). The ΔP (11±0 vs. 17±1 cmH2O; p<0.05) and ΔPL (6±0 vs. 10±1 cmH2O; p<0.05) showed an increase (Figs 2 and 3). In group B EELV (1337±168 vs. 1159±140; p>0.05) and EELV/kg (27±3 vs. 24±3 ml/kg; p>0.05) were not influenced. Nonetheless a significant decrease in Cstat (42±3 vs. 32±1 ml/cmH2O; p<0.05) and an increase in ΔP (11±1 vs. 15±1 cmH2O; p<0.05) and ΔPL (5±1 vs. 7±0 cmH2O; p<0.05) could be observed. In group C EELV (1231±89 vs. 1310±135; p>0.05), EELV/kg (27±2 vs. 29±3 ml/kg; p>0.05), ΔP (10±1 vs. 12±1 cmH2O; p>0.05) and ΔPL (5±1 vs. 7±1 cmH2O; p>0.05) where not changed but a significant decrease of Cstat (43±1 vs. 37±1 ml/cmH2O; p<0.05) was found. The TPPInsp were different from H0 in group A and C (A: 6 ± 1 vs. 10 ± 1 cmH20, C: 6 ± 1 vs. 12 ± 2 cmH2O, p < 0.05) but not in group B (6 ± 1 vs. 7 ± 1 cmH2O, p > 0.05). The TTPEXP stayed unaffected between H0 and H6 (Table 1) (S2 Fig).
Table 1. Pulmonary and hemodynamic parameters in the setting of 6 hours mechanical ventilation with an intraabdominal pressure of 10 mmHg.
| group A | group B | group C | ||
|---|---|---|---|---|
| Weight (kg) | HO | 48±1 | 49±1 | 45±1 |
| IAP (mmHg) | HO | 3±0 | 2±1 | 2±0 |
| IAP (mmHg) | H6 | 10±0* | 10±0* | 10±0* |
| EELV | H0 | 1323±95 | 1337±168 | 1231±89 |
| EELV | H6 | 774±67* | 1159±140# | 1310±135§ |
| EELV/kg | H0 | 27±2 | 27±3 | 28±2 |
| EELV/kg | H6 | 16±1* | 24±3# | 29±3§$ |
| ΔP | H0 | 11±0 | 11±1 | 10±1 |
| ΔP | H6 | 17±1* | 15±1*# | 12±1§$ |
| ΔPL | H0 | 6±0 | 5±0 | 5±1 |
| ΔPL | H6 | 10±1* | 7±0* | 7±1 |
| TPPInsp | H0 | 7±1 | 6±1 | 6±1 |
| TPPInsp | H6 | 11±2* | 7±1 | 12±2* |
| TPPExp | H0 | 1±1 | 1±0 | 1±1 |
| TPPExp | H6 | 1±1 | 1±1 | 5±1 |
| CStat | H0 | 42±2 | 42±3 | 45±2 |
| CStat | H6 | 27±1* | 32±1*# | 37±1*§$ |
| ERS | H0 | 28±1 | 29±1 | 28±1 |
| ERS | H6 | 44±1* | 37±2*# | 32±1*§$ |
| ECW | H0 | 14±1 | 15±2 | 14±1 |
| ECW | H6 | 18±3 | 20±2 | 13±1 |
| EL | H0 | 14±1 | 13±1 | 13±2 |
| EL | H6 | 26±3* | 17±1* | 19±2 |
| HR | H0 | 79±9 | 113±9# | 85±9 |
| HR | H6 | 77±12 | 99±6 | 70±4 |
| MAP | H0 | 78±6 | 98±5 | 88±7 |
| MAP | H6 | 100±6* | 102±6 | 104±6 |
| P/F ratio | H0 | 452±25 | 425±20 | 505±24 |
| P/F ratio | H6 | 439±19 | 396±18 | 501±20$ |
| CI | H0 | 4.9±0.5 | 5.7±0.3 | 4.4±0.4 |
| CI | H6 | 4.3±0.4 | 4.9±0.3 | 3.6±0.2 |
EELV = end-expiratory lung volume (ml), EELV/kg = end-expiratory lung volume per kg bodyweight (ml/kg), ΔP = driving pressure (cmH2O), ΔPL = transpulmonary pressure (cmH2O), TPPInsp = inspiratory transpulmonary pressure (cmH2O), TPPExp = expiratory transpulmonary pressure (cmH2O), CStat = static pulmonary compliance (ml/cmH2O), ERS = Elastance of the respiratory system (cmH2O/ml), ECW = Elastance of the chest wall (cmH2O/ml), EL = lung elastance (cmH2O/ml), HR = heart rate (beats/min), MAP = mean arterial pressure (mmHg), P/F ratio = ratio between arterial pressure of oxygen and inspired oxygen concentration (mmHg), CI = cardiac index (l/min/m2)
* = P<0.05 HO vs. H6
# = p<0.05 group A vs. group B
§ = P<0.05 group A vs. group C
$ = p<0.05 group B vs. group C.
Fig 2. Alterations of end-expiratory lung volume in absolute values and in relation to body weight in response to an intraabdominal pressure of 10 mmHg over 6 hours mechanical ventilation.
 = group A with PEEP 5 cmH2O,
= group A with PEEP 5 cmH2O,  = group B with PEEP 10 cmH2O
= group B with PEEP 10 cmH2O  = group C with PEEP 15 cmH2O * = p<0.05 HO vs. H6, # = p<0.05 group A vs. group B, § = p<0.05 group A vs. group C. Mean values with SEM are illustrated.
= group C with PEEP 15 cmH2O * = p<0.05 HO vs. H6, # = p<0.05 group A vs. group B, § = p<0.05 group A vs. group C. Mean values with SEM are illustrated.
Fig 3. Alterations of driving pressure and transpulmonary pressure in response to an intraabdominal pressure of 10 mmHg over 6 hours mechanical ventilation.
 = group A with PEEP 5 cmH2O,
= group A with PEEP 5 cmH2O,  = group B with PEEP 10 cmH2O
= group B with PEEP 10 cmH2O  = group C with PEEP 15 cmH2O * = p<0.05 HO vs. H6, # = p<0.05 group A vs. group B, § = p<0.05 group A vs. group C, $ = p<0.05 group B vs. group C. Mean values with SEM are illustrated.
= group C with PEEP 15 cmH2O * = p<0.05 HO vs. H6, # = p<0.05 group A vs. group B, § = p<0.05 group A vs. group C, $ = p<0.05 group B vs. group C. Mean values with SEM are illustrated.
Mean values with SEM are illustrated.
At H6 we found a lower EELV/kg in group A (16±1 ml/kg) compared to group B (24±3 ml/kg) and C (29±3 ml/kg) (P<0.05) (Fig 2). Driving pressure decreased significantly with increasing PEEP (A: 17±1 cmH2O, B: 15±1 cmH2O, C: 12±1 cmH2O, p<0.05) (Fig 3).
Hemodynamic parameters and oxygenation are summarised in Table 1. We could not find a relevant alteration of cardiac index with higher PEEP nor was the P/F ratio significantly influenced.
Lung injury score and wet-dry weight ratio
The global lung injury score was lowest in group B (0.17±0.02) compared to group A (0.30±0.04) and group C (0.32±0.02) (p<0.05) (Fig 4). The wet-dry weight ratios were not different (S3 Fig).
Fig 4. Histologic assessment of lung injury.
Quantitative score for lung injury (from 0 = no damage to 1 = maximal alteration) calculated by the averaging score for five independent variables: neutrophils in the alveolar space, neutrophils in the interstitial space, hyaline membranes, proteinaceous debris filling the airspaces and alveolar septal thickening. Apical, medial, dorsal and global score (mean of scores for apical, medial and dorsal) are illustrated. # = p<0.05 group A vs. group B, § = p<0.05 group A vs. group C, $ = p<0.05 group B vs. group C. Mean values with SEM are illustrated.
Discussion
Main findings
The present animal study proved that even a moderate IAP of 10 mmHg caused changes in lung mechanics and a histological lung injury after 6 hours of ventilation. A PEEP of 10 cmH2O overcame the intra-abdominal pressure induced alterations of EELV and revealed the lowest lung injury score.
Alterations in lung mechanics
The main aim of our study was to describe the alterations in EELV, ΔP and ΔPL in a porcine model of moderately elevated IAP. These crucial parameters have an impact on the development or prevention of ventilator induced lung injury (VILI) [22, 23]. By implementing a water-filled balloon with an IAP of 10 mmHg for up to 6 hours, we detected a drop of EELV and EELV/kg bw with a PEEP of 5 cmH2O over time. In the two groups with a PEEP of 10 and 15 cmH2O, these reductions were not observed. PInsp did not rise proportionally to PEEP, which strongly suggests a regional recruitment due to an increasing PEEP. TPPInsp did not change significantly from H0 with a PEEP of 10 cmH2O in contrast to the groups with PEEP 5 and 15 cmH2O. The PEEP of 10 cmH2O did not affect TPPExp in significant manner. We interpret these results that the best compliance and lowest EL in this setting occurred with a PEEP of 10 cmH2O. These results extend those obtained by Cortes-Puentes et al. [24], which were able to reveal an unresponsive TPPExp with an increase of IAP. The authors argued that a rising IAP stiffens the chest wall, whereas aerated lung volume decreases, either due to derecruitment or a reduced stretch of air spaces that remain patent. Cortes-Puentes already showed that a PEEP of 10 cmH2O is able to restore FRC, which appears to be reduced above an IAP of over 10 mmHg. Compared to our study design the researchers used intra-abdominal air insufflation and modified IAP levels between zero and 35 cmH2O [24].
In our model with an IAP of 10 mmHg, ERS decreased with increasing PEEP, but ECW was the same in all groups. These findings are in line with studies in patients with ARDS. Krebs et al. applied different PEEP levels (up to 20 cmH2O) in 20 patients with ARDS; one half of the study population had IAH (with a mean IAP of 8 and 16 mmHg, respectively) [25]. PEEP was found to decrease ERS by decreasing EL without influencing ECW in both groups.
PEEP in elevated IAP
In the context of elevated IAP, the management of PEEP is still a contentious issue [26]. The TPPExp seems to be an important parameter. A negative TPPExp should be avoided in order to prevent lung collapse and to overcome intratidal recruitment/derecruitment [27]. By inflating an intra-abdominal balloon, Regli et al. analyzed different PEEP levels (5, 8, 12 and 15 cmH2O) unmatched to the level of IAP [28]. PEEP levels below the IAP were not able to prevent the decline of EELV. In a second study the same group now matched PEEP and IAP levels [29]. It must be noted that the authors found that EELV was preserved without any improvement in the P/F ratio. They argued that a reduction of cardiac output with higher PEEP levels is the main cause for the lack of improvement.
A human study in mechanically ventilated patients recently matched the PEEP to IAP. Only 10 of 18 patients tolerated this matched PEEP. In these 10 patients, the matched PEEP improved oxygenation but a PEEP matched 0.5 x IAP in cmH2O did not [30]. In our study, TPPExp was positive at all times and we were not able to find a relevant change in hemodynamic parameters. Neither could we find relevant alterations in P/F ratio between the groups or over time.
Histological lung injury
Acute lung injury (ALI) in humans is characterized by disruption of the alveolar-capillary membrane barrier, proteinaceous alveolar exudate and pulmonary edema. We used the recommended scoring system for ALI in animal studies [21]. The lung injury score (LIS) was significantly lower in the group with a PEEP of 10 cmH2O. PEEP of 10 cmH2O was probably more lung protective during the ventilation than a lower or higher PEEP. As mentioned previously neither P/F ratio nor cardiac index were relevantly different between the groups.
Alteration in the wet-dry weight ratio is a typical feature of VILI, caused by high tidal volumes, endotoxin or bacterial induced ALI [31]. As expected, the groups did not differ regarding the wet-dry weight ratio. We therefore presume that the observed differences in LIS were not caused by lung edema.
Experimental protocol
Some important aspects of our study differ from recent examinations and show the strength of the actual study.
1. We did not use an air inflated balloon to increase IAP. Instead we modified previously described methods to induce IAP [32, 33]. By installing water in a large 200-litre weather balloon, we aimed to simulate the leading cause of elevated IAP due to liquid ascites or oedematous tissue.
2. We only used a moderately elevated IAP of 10 mmHg and kept it for 6 hours. Since IAP is well known to be around 10 mmHg in critically ill patients [7, 10, 11] the investigation we present here therefore simulated a common scenario.
3. We tried to find the best PEEP in this setting. Therefore we matched PEEP and IAP levels based on the assumption that abdominal-thoracic transmission (ATT) is between 17 and 62% [3–6]. The ATT describes the percentage increase in thoracic pressures for each incremental increase of IAP.
Limitations
This is an animal study. The results therefore cannot be transferred to human patients without any restrictions. We only used an IAP of 10mmHg. Hence, it is unclear to what extent the above-mentioned PEEP matching to IAP is useful and would be tolerated at higher IAP values. Clinical scenarios rarely end at 6 hours in human subjects and extending IAP and the study for a prolonged period may also reveal a difference in optimal PEEP recommendations.
Conclusions
A moderately elevated IAP of 10 mmHg has already relevant effects on lung mechanics and on histological lung injury. Measuring bladder pressure should encourage the clinician to find the best PEEP in order to realize a safer ventilation strategy. In healthy porcine lungs with an IAP of 10 mmHg the application of a PEEP of 10 cmH2O overcame the intra-abdominal pressure induced alterations of EELV. A PEEP of 10 cmH2O revealed the lowest lung injury score.
Supporting information
(PDF)
Quantitative assessment for lung injury calculated by the averaging score for five independent variables and the resulting score (from 0 = no damage to 1 = maximal alteration).
(DOCX)
 = group A with PEEP 5 cmH2O,
= group A with PEEP 5 cmH2O,  = group B with PEEP 10 cmH2O
= group B with PEEP 10 cmH2O  = group C with PEEP 15 cmH2O * = p<0.05 HO vs. H6, # = p<0.05 group A vs. group B, § = p<0.05 group A vs. group C, $ = p<0.05 group B vs. group C. Mean values with SEM are illustrated.
= group C with PEEP 15 cmH2O * = p<0.05 HO vs. H6, # = p<0.05 group A vs. group B, § = p<0.05 group A vs. group C, $ = p<0.05 group B vs. group C. Mean values with SEM are illustrated.
(DOCX)
 = group A with PEEP 5 cmH2O,
= group A with PEEP 5 cmH2O,  = group B with PEEP 10 cmH2O
= group B with PEEP 10 cmH2O  = group C with PEEP 15 cmH2O * = p<0.05 HO vs. H6. Mean values with SEM are illustrated.
= group C with PEEP 15 cmH2O * = p<0.05 HO vs. H6. Mean values with SEM are illustrated.
(DOCX)
Mean values with SEM are illustrated.
(DOCX)
(XLSX)
Acknowledgments
We thank Daniel Kazdal, Mark Kriegsmann and Katarina Kriegsmann, Institute of Pathology, Heidelberg University Hospital, Heidelberg, Germany for the contribution in dyeing and scanning of the histological lung slices and Christopher Buesch, Institute for medical biometry and informatic, Heidelberg University Hospital, Heidelberg, Germany, for statistical advices.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Reintam Blaser A, Regli A, De Keulenaer B, Kimball EJ, Starkopf L, Davis WA, et al. Incidence, risk factors, and outcomes of intra-abdominal hypertension in critically ill patients-a prospective multicenter study (IROI Study). Crit Care Med. 2019;47(4):535–42. 10.1097/CCM.0000000000003623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pelosi P, Quintel M, Malbrain ML. Effect of intra-abdominal pressure on respiratory mechanics. Acta Clin Belg. 2007;62 Suppl 1:78–88. [DOI] [PubMed] [Google Scholar]
- 3.Malbrain ML, De Laet IE, De Waele JJ, Kirkpatrick AW. Intra-abdominal hypertension: definitions, monitoring, interpretation and management. Best Pract Res Clin Anaesthesiol. 2013;27(2):249–70. 10.1016/j.bpa.2013.06.009 [DOI] [PubMed] [Google Scholar]
- 4.Malbrain ML, Wilmer A. The polycompartment syndrome: towards an understanding of the interactions between different compartments! Intensive Care Med. 2007;33(11):1869–72. 10.1007/s00134-007-0843-4 [DOI] [PubMed] [Google Scholar]
- 5.Wauters J, Wilmer A, Valenza F. Abdomino-thoracic transmission during ACS: facts and figures. Acta Clin Belg. 2007;62 Suppl 1:200–5. [DOI] [PubMed] [Google Scholar]
- 6.Wauters J, Claus P, Brosens N, McLaughlin M, Hermans G, Malbrain M, et al. Relationship between abdominal pressure, pulmonary compliance, and cardiac preload in a porcine model. Crit Care Res Pract. 2012;2012:763181 10.1155/2012/763181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Malbrain ML, Chiumello D, Pelosi P, Bihari D, Innes R, Ranieri VM, et al. Incidence and prognosis of intraabdominal hypertension in a mixed population of critically ill patients: a multiple-center epidemiological study. Crit Care Med. 2005;33(2):315–22. 10.1097/01.ccm.0000153408.09806.1b [DOI] [PubMed] [Google Scholar]
- 8.Hedenstierna G, Larsson A. Influence of abdominal pressure on respiratory and abdominal organ function. Curr Opin Crit Care. 2012;18(1):80–5. 10.1097/MCC.0b013e32834e7c3a [DOI] [PubMed] [Google Scholar]
- 9.Rogers WK, Garcia L. Intraabdominal hypertension, abdominal compartment syndrome, and the open abdomen. Chest. 2018;153(1):238–50. 10.1016/j.chest.2017.07.023 [DOI] [PubMed] [Google Scholar]
- 10.Malbrain ML, Cheatham ML, Kirkpatrick A, Sugrue M, Parr M, De Waele J, et al. Results from the international conference of experts on intra-abdominal hypertension and abdominal compartment syndrome. I. Definitions. Intensive Care Med. 2006;32(11):1722–32. 10.1007/s00134-006-0349-5 [DOI] [PubMed] [Google Scholar]
- 11.Malbrain ML, Chiumello D, Cesana BM, Reintam Blaser A, Starkopf J, Sugrue M, et al. A systematic review and individual patient data meta-analysis on intra-abdominal hypertension in critically ill patients: the wake-up project. World initiative on abdominal hypertension epidemiology, a unifying project (WAKE-Up!). Minerva Anestesiol. 2014;80(3):293–306. [PubMed] [Google Scholar]
- 12.Malbrain ML, De Keulenaer BL, Oda J, De Laet I, De Waele JJ, Roberts DJ, et al. Intra-abdominal hypertension and abdominal compartment syndrome in burns, obesity, pregnancy, and general medicine. Anaesthesiol Intensive Ther. 2015;47(3):228–40. 10.5603/AIT.a2015.0021 [DOI] [PubMed] [Google Scholar]
- 13.Pelosi P, Ravagnan I, Giurati G, Panigada M, Bottino N, Tredici S, et al. Positive end-expiratory pressure improves respiratory function in obese but not in normal subjects during anesthesia and paralysis. Anesthesiology. 1999;91(5):1221–31. 10.1097/00000542-199911000-00011 [DOI] [PubMed] [Google Scholar]
- 14.Pelosi P, Croci M, Ravagnan I, Cerisara M, Vicardi P, Lissoni A, et al. Respiratory system mechanics in sedated, paralyzed, morbidly obese patients. J Appl Physiol. 1997;82(3):811–8. 10.1152/jappl.1997.82.3.811 [DOI] [PubMed] [Google Scholar]
- 15.Baydur A, Behrakis PK, Zin WA, Jaeger M, Milic-Emili J. A simple method for assessing the validity of the esophageal balloon technique. Am Rev Respir Dis. 1982;126(5):788–91. 10.1164/arrd.1982.126.5.788 [DOI] [PubMed] [Google Scholar]
- 16.Grieco DL, Chen L, Brochard L. Transpulmonary pressure: importance and limits. Ann Transl Med. 2017;5(14):285 10.21037/atm.2017.07.22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Olegard C, Sondergaard S, Houltz E, Lundin S, Stenqvist O. Estimation of functional residual capacity at the bedside using standard monitoring equipment: a modified nitrogen washout/washin technique requiring a small change of the inspired oxygen fraction. Anesth Analg. 2005;101(1):206–12. 10.1213/01.ANE.0000165823.90368.55 [DOI] [PubMed] [Google Scholar]
- 18.Malbrain ML, Deeren DH. Effect of bladder volume on measured intravesical pressure: a prospective cohort study. Crit Care. 2006;10(4):R98 10.1186/cc4962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kirkpatrick AW, Roberts DJ, De Waele J, Jaeschke R, Malbrain ML, De Keulenaer B, et al. Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the World Society of the Abdominal Compartment Syndrome. Intensive Care Med. 2013;39(7):1190–206. 10.1007/s00134-013-2906-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jakob SM, Knuesel R, Tenhunen JJ, Pradl R, Takala J. Increasing abdominal pressure with and without PEEP: effects on intra-peritoneal, intra-organ and intra-vascular pressures. BMC Gastroenterol. 2010;10:70 10.1186/1471-230X-10-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matute-Bello G, Downey G, Moore BB, Groshong SD, Matthay MA, Slutsky AS, et al. An official American Thoracic Society workshop report: features and measurements of experimental acute lung injury in animals. Am J Respir Cell Mol Biol. 2011;44(5):725–38. 10.1165/rcmb.2009-0210ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Slutsky AS, Ranieri VM. Ventilator-induced lung injury. N Engl J Med. 2013;369(22):2126–36. 10.1056/NEJMra1208707 [DOI] [PubMed] [Google Scholar]
- 23.Silva PL, Negrini D, Rocco PR. Mechanisms of ventilator-induced lung injury in healthy lungs. Best Pract Res Clin Anaesthesiol. 2015;29(3):301–13. 10.1016/j.bpa.2015.08.004 [DOI] [PubMed] [Google Scholar]
- 24.Cortes-Puentes GA, Gard KE, Adams AB, Faltesek KA, Anderson CP, Dries DJ, et al. Value and limitations of transpulmonary pressure calculations during intra-abdominal hypertension. Crit Care Med. 2013;41(8):1870–7. 10.1097/CCM.0b013e31828a3bea [DOI] [PubMed] [Google Scholar]
- 25.Krebs J, Pelosi P, Tsagogiorgas C, Alb M, Luecke T. Effects of positive end-expiratory pressure on respiratory function and hemodynamics in patients with acute respiratory failure with and without intra-abdominal hypertension: a pilot study. Crit Care. 2009;13(5):R160 10.1186/cc8118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Malbrain M. The saga continues: How to set best PEEP in intra-abdominal hypertension? J Crit Care. 2018;43:387–9. 10.1016/j.jcrc.2017.11.013 [DOI] [PubMed] [Google Scholar]
- 27.Fumagalli J, Berra L, Zhang C, Pirrone M, Santiago RRS, Gomes S, et al. Transpulmonary pressure describes lung morphology during decremental positive end-expiratory pressure trials in obesity. Crit Care Med. 2017;45(8):1374–81. 10.1097/CCM.0000000000002460 [DOI] [PubMed] [Google Scholar]
- 28.Regli A, Hockings LE, Musk GC, Roberts B, Noffsinger B, Singh B, et al. Commonly applied positive end-expiratory pressures do not prevent functional residual capacity decline in the setting of intra-abdominal hypertension: a pig model. Crit Care. 2010;14(4):R128 10.1186/cc9095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Regli A, Chakera J, De Keulenaer BL, Roberts B, Noffsinger B, Singh B, et al. Matching positive end-expiratory pressure to intra-abdominal pressure prevents end-expiratory lung volume decline in a pig model of intra-abdominal hypertension. Crit Care Med. 2012;40(6):1879–86. 10.1097/CCM.0b013e31824e0e80 [DOI] [PubMed] [Google Scholar]
- 30.Regli A, De Keulenaer BL, Palermo A, van Heerden PV. Positive end-expiratory pressure adjusted for intra-abdominal pressure—A pilot study. J Crit Care. 2018;43:390–4. 10.1016/j.jcrc.2017.10.012 [DOI] [PubMed] [Google Scholar]
- 31.Tsuno K, Miura K, Takeya M, Kolobow T, Morioka T. Histopathologic pulmonary changes from mechanical ventilation at high peak airway pressures. Am Rev Respir Dis. 1991;143(5 Pt 1):1115–20 [DOI] [PubMed] [Google Scholar]
- 32.Mutoh T, Lamm WJ, Embree LJ, Hildebrandt J, Albert RK. Abdominal distension alters regional pleural pressures and chest wall mechanics in pigs in vivo. J Appl Physiol. 1991;70(6):2611–8. 10.1152/jappl.1991.70.6.2611 [DOI] [PubMed] [Google Scholar]
- 33.Regli A, De Keulenaer BL, Singh B, Hockings LE, Noffsinger B, van Heerden PV. The respiratory pressure-abdominal volume curve in a porcine model. Intensive Care Exp. 2017; 5(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]