The confirmed and suspected cases of the 2019 novel coronavirus disease (COVID‐19) have increased not only in Wuhan, Hubei Province, but also China and the world. Enormous demand for handling the COVID‐19 outbreak challenged both the health care personnel and the medical supply system. In West China Hospital, emergency department (ED) undertook the mission of clinical reception, primary diagnosis, and interim treatment for the suspected cases of COVID‐19.
The pathogen of COVID‐19, severe acute respiratory syndrome coronavirus 2, was confirmed to have human‐to‐human transmission.1 Therefore, COVID‐19 has expanded the infection risk from Wuhan to cities throughout China and even the world via case transportation.2 Providing qualified personal protection equipment (PPE) to health care personnel plays an essential role in avoiding occupational exposure and infection. U.S. Centers for Disease Control and Prevention for COVID‐19 infection control of health care personnel recommended gloves, gowns, respiratory protection, and eye protection as standardized PPE.3 However, protective clothing, N95 respirators, and goggles are not commonly used in clinical practice and hence are not in bulk stock. This brief report aims to present our interim hospital management measures on the health care personnel protection in West China Hospital under the condition of intense workload and PPE supply shortage after the outbreak of COVID‐19.
We retrospectively reviewed the daily ED visits and PPE supply records from January 13 to February 1, 2020. The fever visits at the ED soared from January 20 to January 25. The ratio of fever patients at the ED exploded to a peak of over 40% on January 25 and then fluctuated at about 30% (Figure 1A). Protective clothing, N95 respirators, and goggles could only ensure the daily supply for < 15% ED personnel (Figure 1B). However, West China Hospital adopted a series of measures to achieve “zero infection” among health care personnel.
First, the online clinic was set to facilitate the patient triage (Figure 1C). Through free online consultation, the hospital preliminarily judged the treatment urgency, recommended nonemergency patients to delay hospital appointments or visit other nonantiepidemic hospitals, provided low‐suspected patients treatment instruction when self‐isolating at home, and invited high‐suspected patients to the Fever Clinic via the green channel. The online clinic effectively alleviated the ED workload and facilitated early detection of potential cases.
Second, the interim visit triage and ED region separation were established (Figure 1D). The assigned personnel conducted preexamination and triage to divide visits into low‐suspected, high‐suspected, and other patients and required different patients to follow the specified routines to enter ED and separate the intra‐ED space into high‐risk and low‐risk regions. For suspected cases, the hospital assigned an independent fever clinic room, fever observation room, and CT examination room. Cases confirmed through qRT‐PCR and/or CT were transferred to quarantine ward while excluded patients went to other departments or back home. The ED region separation triage system reduced the cross‐infection by restricting the activity ranges of both patients and ED personnel.
Third, the ED requirement had the highest priority. The hospital established a capable command system, implemented effective coordination mechanisms,4 provided the ED with PPE and medical devices preferentially, equipped the triage and high‐risk‐region personnel with standardized personal protection, withdrew or postponed nonurgent appointments and operations, and dispatched aid personnel from other departments to ED. These measures concentrated the limited supply through the hospital on the staff who mostly needed protection.
Figure 1.
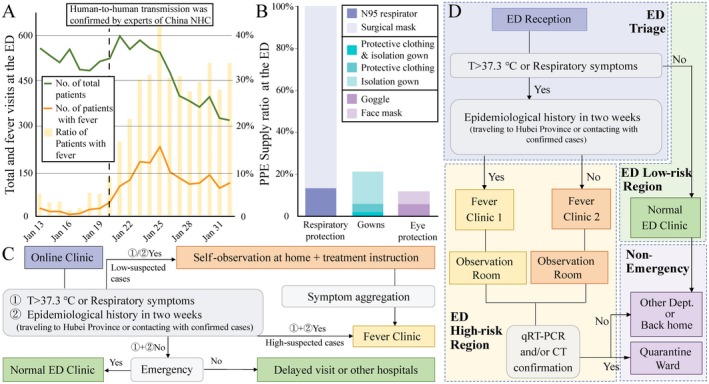
ED workload, PPE shortage, and hospital management plan during the COVID‐19 epidemic. (A) The daily number and ratio of fever visits at the ED from January 13 to February 1, 2020. (B) The PPE supply ratio at the ED of West China Hospital on January 25. (C) The illustration of online clinic triage of West China Hospital. (D) The illustration of ED triage and region separation. NHC = National Healthcare Commission; T = temperature.
Emergency‐ and disaster‐preparedness was an important issue and a global problem. Most hospitals could not maintain their routine work for a week due to the disaster‐related resource shortage.5 A previous review highlighted the challenge of the emergency ordering of standardized PPE supply.6 The hospital invested greater efforts to establish an emergency management system based on the anticipated hazard.7 However, the unpredictable epidemic rendered the interim PPE preparedness impossible, especially for less‐used PPE, protective clothing, and N95 respirators in daily work. It might be more practical to prepare a flexible hospital contingency plan than abundant PPE preparedness.
Our hospital adopted interim measures, including online consultation, region separation, and epidemic priority, to alleviate the pressure in the clinical work, reduce the cross‐infection, and strengthen the protection of high‐risk staff. Our hospital held the “zero infection” record, which was far lower than the simultaneous outside‐Hubei mean level of 3.4% in late January.8 The zero infection indicated the flexibility and validity of our interim hospital management strategy.
However, there were still some limitations. First, the supply protocol compromised the health protection of low‐risk personnel without standardized PPE. Second, the interim management strategies could not resist large‐scale outbreak and long‐term PPE shortage. Nevertheless, our management strategies, as a temporary emergency plan, created the biggest benefits of extremely limited resources to meet the emergency need. The long‐term solution should be a sustainable supply chain. Fortunately, the government of China recovered the PPE production supply in February, which alleviated the supply shortage significantly.
In conclusion, the hospital emergency management plan of West China Hospital could alleviate the ED workload, protect health care personnel, and control the cross‐infection during the COVID‐19 epidemic. We advocate that every hospital should create the contingency plan suited to their conditions.
We acknowledge the colleagues at Emergency Department of West China Hospital and also all the colleagues combating COVID‐19.
Academic Emergency Medicine 2020;27:309–311.
YC, QL, and JC contributed equally to this work.
The authors have no relevant financial information or potential conflicts to disclose.
Authors’ contributions: YC—conception, literature search, figures, data analysis, data interpretation, writing, and final approval; QL—conception, data collection, data analysis, data interpretation, and final approval; JC—conception, data collection, data analysis, data interpretation, and final approval; XG—writing, major revision, and final approval; CM—major revision and final approval; HY—major revision and final approval; ZC—conception, data interpretation, writing, and final approval; CL—conception, major revision, and final approval; LL—supervision, major revision, and final approval.
Contributor Information
Zihang Chen, Email: ianchan_0704@hotmail.com.
Chunjie Li, Email: lichunjie07@qq.com.
Longjiang Li, Email: muzili63@163.com.
References
- 1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Du Z, Wang L, Cauchemez S, et al. Risk for transportation of 2019 novel coronavirus disease from Wuhan to other cities in China. Emerg Infect Dis 2020;26 10.3201/eid2605.200146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. US Centers for Disease Control and Prevention . Interim Infection Prevention and Control Recommendations for Patients with Confirmed 2019 Novel Coronavirus (2019‐nCoV) or Patients Under Investigation for SARS‐CoV‐2 in Healthcare Settings. Atlanta, GA: US Centers for Disease Control and Prevention, 2020. Available at: https://www.cdc.gov/coronavirus/SARS-CoV-2/hcp/infection-control.html. Accessed February 3, 2020. [Google Scholar]
- 4. Li Y, Wang H, Jin XR, et al. Experiences and challenges in the health protection of medical teams in the Chinese Ebola treatment center, Liberia: a qualitative study. Infect Dis Poverty 2018;7:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Vick DJ, Wilson AB, Fisher M, et al. Assessment of community hospital disaster preparedness in New York State. J Emerg Manag 2018;16:213–27. [DOI] [PubMed] [Google Scholar]
- 6. Patel A, D'Alessandro MM, Ireland KJ, et al. Personal protective equipment supply chain: lessons learned from recent public health emergency responses. Health Secur 2017;15:244–52. [DOI] [PubMed] [Google Scholar]
- 7. Naser WN, Ingrassia PL, Aladhrae S, et al. A study of hospital disaster preparedness in South Yemen. Prehosp Disaster Med 2018;33:133–8. [DOI] [PubMed] [Google Scholar]
- 8. The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team . The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID‐19) — China, 2020. China CDC Weekly 2020;2:113–22. [PMC free article] [PubMed] [Google Scholar]


