Abstract
Despite the mandated use of standard precaution guidelines to limit infection transmission in health‐care settings, adherence by health‐care professionals is suboptimal. There is currently no psychometrically‐validated scale to assess influences on workers' adherence. After the data collection was conducted, Michinov et al. (2016) published a questionnaire to determine sociocognitive determinants of adherence to Standard Precautions. The aim of the present study was to develop and test the psychometric properties of such a scale. Forty nine items were derived from interviews with 29 nurses and tested across two studies. Study 1 was a repeated‐measures survey using principal components analysis with data from 363 participants; a 29 item, five factor solution was extracted with good to acceptable internal reliabilities (α = .61–.85). Data from 122 of the original participants retested at 4 weeks showed intraclass correlations of .69–.84. Study 2, which was 6 months later, used confirmatory factor analysis with data from a second sample of 384 participants, and supported the five factor structure of leadership, justification, culture/practice, contextual cues, and judgement. The Factors Influencing Adherence to Standard Precautions Scale has good psychometric properties and stability across time and samples. The scale is suitable for use with nurses, and its validation with other health‐care professionals and trainees is important in order to tailor effective interventions to promote adherence.
Keywords: adherence, infection prevention and control, scale development, standard precautions, validation
1. INTRODUCTION
Infection control measures have been present in various forms since early Greek and Roman times (Smith, Watkins, & Hewlett, 2012). The identification of AIDS caused by HIV in the early 1980s prompted the introduction of more specific infection control measures, namely universal precaution guidelines (UP) (Centers for Disease Control, 1982, 1985, 1987), to protect health‐care workers. In 1996, UP were revised and renamed standard precaution guidelines (SP) (Garner, 1996). Lam (2011) highlighted the importance of the revisions, which outline specific criteria to be followed to prevent cross‐contamination of disease between patients and health‐care workers. The original guidelines have been revised several times, usually in reaction to identified risk factors. For example, respiratory hygiene/cough etiquette and safe injection practices were included in 2003–2004 to protect workers against the possible transmission of the coronavirus during the SARS epidemic, as well as the continued outbreaks of hepatitis B and C (Siegel, Rhinehart, Jackson, & Chiarello, 2007).
The guidelines emphasize that the use of SP is the foundation for preventing the cross‐transmission of infectious agents between patients and health‐care workers, and that they need to be supplemented, when needed, with additional transmission‐based precautions. Health‐care institutions are required to mandate the use of SP, but despite policies and procedures to enforce their use, health‐care workers’ adherence to SP remains poor. Adherence to SP ranges from a low of 19.5% in the years immediately following their introduction (Kelen et al., 1990), to the most recent figures of 57.4 and 69.4% among nurses in Hong Kong and Brazil, respectively (Lam, 2014; Pereira, Lam, Chan, Malaguti‐Toffano, & Gir, 2015), to 81% of staff whom Tait, Voepel‐Lewis, Tuttle, and Malviya (2000) surveyed working with patients known to be HIV positive/hepatitis B virus positive. Adherence figures also vary with respect to specific aspects of SP, such as handwashing (19%) (Askarian, McLaws, & Meylan, 2007) and the use of protective eyewear (52%) (Madan, Rentz, Wahle, & Flint, 2001) and gloves for cannulation (54%) (Zhang, Lee, & Knott, 2014).
In an integrative review, Valim, Marziale, Richart‐Martínez, and Sanjuan‐Quiles (2014) identified 18 measures designed to evaluate levels of compliance and adherence (terms they used interchangeably) with infection control practices. They emphasized that most of those measures assessed adherence/non‐adherence rates, and recommended that “further research [to] assess the variables that influence adherence to SP” (p. 1516). Attempts to date to determine the reasons for non‐adherence to SP among health‐care workers have typically used only single items (Lam, 2014; Rabaud et al., 2000; Valim, Marziale, Richart‐Martínez, & Sanjuan‐Quiles, 2014) or observational and anecdotal accounts. These latter accounts indicate that a lack of knowledge, lack of or inadequate supplies, time pressure, confidence in their own skills, the organizational climate, and forgetfulness are among the factors that staff have cited as their reasons for non‐adherence (Efstathiou, Papastavrou, Raftopoulos, & Merkouris, 2011b; Hills & Wilkes, 2003; Reda, Fisseha, Mengistie, & Vandeweerd, 2010). Furthermore, Efstathiou et al. (2011b) highlighted that most studies discussing non‐adherence to Standard Precautions “studied only one or limited aspects of SP, mainly hand hygiene” (p. 2). Some attempts to broaden the range of factors argued to assess adherence to SP can be found in the work of Osborne (2003) and Cheung et al. (2015); however, neither study provided detailed items nor any psychometric data beyond Cronbach's alpha. It is important, therefore, to develop and psychometrically validate a scale that systematically assesses a range of factors influencing adherence or non‐adherence to SP. The aim of the present study was to develop and validate such a scale. We report on two studies designed to achieve this aim.
2. METHODS
2.1. Study design
Two studies are reported in the current paper. Study 1 involved the development of items, followed by a two phase, repeated‐measures study, conducted via an online survey to assess the factor structure of the new scale items, and secondly, to test the stability of those factors over a 4 week period. Six months later, study 2 was conducted, which involved a second online survey to confirm the factors extracted from the data in study 1.
2.2. Scale development
Step 1 involved interviews with 29 nurses to elicit the reasons they considered influence staff adherence or lack of adherence to SP (Bouchoucha & Moore, 2018). Forty nine questions were written based upon these interview data. In step 2, three experienced clinicians – a nurse practitioner, a nurse educator, and an infection control nurse consultant – were invited to review the questions for face validity, to ensure that the items were written in plain language and clearly understandable by clinicians. No changes were recommended at this stage. The questions (e.g. I am more likely to wear personal protection equipment if it is located nearby patients, I assess what is wrong with a patient before deciding whether or not to implement SP) were answered on a five point Likert scale, where 0 = not at all and 4 = very much, as per Nunnally's (1967) suggestions on the use of Likert scales.
2.3. Study 1
2.3.1. Psychometric properties
In study 1, the construct validity and internal consistency of the scale items were tested using exploratory factor analysis and Cronbach's alpha with 363 nurse participants, followed by 4 week test–retest reliabilities with 122 nurses from the original sample who agreed to be followed up.
2.4. Participants
Participants were required to be nurses registered to practice. Complete data were available from 363 participants (49 males, 314 females) at time 1 (T1). There was no gender difference with respect to age (female mean age = 44.36 years, standard deviation [SD] = 9.66; male mean age = 41.94 years, SD = 10.36; independent t‐test t 361 1.61, P = .362).
Of this sample, 262 participants agreed to participate in a test–retest phase 4 weeks later (time 2/T2), but only 122 (88 females) of these 262 participants actually completed the questionnaire at T2. Their ages ranged from 27 to 64 years (mean = 45.18 years, SD = 8.81). There was no gender difference with respect to age among these 122 participants (female mean age = 45.37, SD = 8.74; 12 males, mean = 43.64, SD = 9.66; independent t‐test t 120 .70, P = .484, two tailed).
Most of the 363 (62.6%) participants surveyed at T1 reported that they worked full time. The majority of nurses worked in critical care areas (intensive care, coronary care, and high‐dependency units, 51.6%), 11.8% worked in the emergency department, 8.2% in medical care, 4.4% in surgical care, while the balance was variously employed in community, aged care education, or clinical management. Due to the means of data collection, it was not possible to calculate a response rate for T1, but 33.6% of T1 participants responded at T2.
2.5. Procedure
Participants were recruited by two means: The Northern Territory (NT, Australia) Department of Health Principal Nurse Advisor emailed an invitation to all nursing staff in the NT, and the Australian College of Critical Care Nurses also emailed an invitation to their members.
Participants were given a link to the website on which the questionnaire could be found, as well as a printable plain language statement that provided details of the study, indicated that participation was voluntary, and that the data collected were anonymous. Participants were advised that submission of the completed questionnaire would constitute their informed consent, and that they could exit the study at any time by closing their Web browser.
At T1, participants provided their demographic data, a unique identifier by which to match T2 data, and completed the 49 items written to assess the Factors Influencing Adherence to Standard Precautions Scale (FIASPS). Upon completion of the questionnaire, participants had two options: they could simply submit the completed survey or submit the survey and then indicate their agreement to participate in the retest phase of the study 4 weeks later. A separate file was generated for those who indicated their willingness to participate at T2 for them to record the date and their email address for follow up 4 weeks later. One month later, an email thank you and a link to the second survey were sent to each of the 262 T1 participants who had indicated their intention to participate in the second phase, although only 122 responded. Participants' demographic data and their identifier codes were used to match respondents at T2 to their T1 data. At no time was it possible to match email addresses to the data.
2.6. Ethics
Ethical approval for the conduct of these studies was obtained from the NT Department of Health, the Menzies School of Health Research Human Research Ethics Committee (no. HREC‐1601) and Charles Darwin University Human Research Ethics Committee approval (no. H11111).
2.7. Sample size and data analyses
Sample size recommendations for principal component analysis (PCA) vary widely from a minimum of 100 cases (Hair, Black, Babin, & Anderson, 2010) to 300 cases (Tabachnick & Fidell, 2013). Others have focused on the ratio of cases to variables from 3:1, 6:1, up to 20:1; however, Hogarty, Hines, Kromrey, Ferron, and Mumford (2005) found no evidence that these ratios had an effect on factor recovery. The use of statistics, such as the Kaiser–Meyer–Olkin (KMO) test, Bartlett's test of sphericity, and Cattell's scree test, are often the preferred indicators of the data's suitability for factor analysis (Gorsuch, 1983; Tabachnick & Fidell, 2013), and these indicators are employed in the present study.
The data were analyzed using SPSS (version 24). The factor structure and reliability of the scale items were investigated using PCA, Cronbach's alpha, and intraclass correlations (ICC) to determine the retest coefficients for the extracted factors.
3. RESULTS
3.1. Study 1: Exploratory factor analysis
Responses to the scale items were submitted to the PCA with oblique rotation to determine the underlying factor structure. Inspection of box plots, skewness, kurtosis, and Shapiro–Wilk statistics revealed approximate normality for all items. The KMO measure of sampling adequacy (.796) and Bartlett's test of sphericity (χ2 300 = 2413.02, P < .001) both indicated the factorability of the correlation matrix (Hair Jr et al., 2010; Tabachnick & Fidell, 2013). The initial PCA revealed two factors that explained ≥5% of the variance, but Cattell's scree plot, Tabachnick and Fidell (2013) criterion of choice, suggested the presence of four or five factors.
After successive iterations and the removal of 19 items that failed to load on any factor equal or greater than .45 (contributing 20% to the factor) (DeVellis, 2012; Hair Jr et al., 2010), simple independent structure was achieved with a five factor solution. These five factors explained 45% of the variance and were labelled leadership (6 items), justification (8 items), contextual cues (6 items), culture/practice (5 items), and judgement (5 items). Internal reliability analyses revealed that each item contributed to alpha across four scales; however, one item on the justification factor was removed as it decreased the alpha, leaving seven items to load on justification. Internal reliabilities were good to acceptable (Loewenthal, 2004), with Cronbach's alphas ≥.61. The final instrument comprised 29 items.
A second PCA was run and replicated the five factor structure with this reduced number of items, explaining approximately 48% of the variance. The factor loadings, reliability coefficients, intercorrelations, eigenvalues, percentages of the variance explained, and descriptive statistics for each factor are presented in Table 1.
Table 1.
Five factor principal component analysis of the Factors Influencing Adherence to Standard Precautions Scale
| Item | Factor | ||||
|---|---|---|---|---|---|
| Justification | Leadership | Contextual cues | Culture/practice | Judgement | |
| I don't wear gloves as I cannot feel veins | .78 | ||||
| I am clumsier when I wear gloves and risk having to repeat the procedure | .69 | ||||
| Wearing gloves makes it more difficult to palpate veins when practicing venepuncture or cannulation | .66 | ||||
| I am less likely to wear gloves as I was taught procedures without them | .64 | ||||
| I don't need to wear gloves when taking blood/cannulating as I am skilled at what I do | .60 | ||||
| It is my choice to not wear gloves when taking blood/cannulating as I am only putting myself at risk | .59 | ||||
| Some procedures I learnt without personal protective equipment and I continue to perform these without | .58 | ||||
| I feel the need to confront people I see not adhering to standard precautions | .86 | ||||
| When I witness others non‐adherence with standard precautions, I use that as an education opportunity | .84 | ||||
| I feel comfortable challenging nurses or doctors when I see them not adhering to standard precautions | .76 | ||||
| I use role‐modelling to increase use of standard precautions | .75 | ||||
| I have a responsibility to encourage people to protect themselves | .64 | ||||
| If people see me practicing standard precautions, they will do the same | .56 | ||||
| I am more likely to wear personal protective equipment if they are located near patients | .69 | ||||
| I am more likely to wear personal protective equipment if I see my colleagues wearing them | .69 | ||||
| A potential exposure to contaminants will trigger my use of standard precautions | .56 | ||||
| I am more careful if I know that a patient has a blood‐borne pathogen | .55 | ||||
| I am more likely to follow standard precautions if I am dealing with needles | .53 | ||||
| I am more likely to follow standard precautions if I am dealing with sharp instruments | .49 | ||||
| The culture of my organization allows for people not to follow standard precaution guidelines (R) | .72 | ||||
| In some workplaces it is standard practice not to follow guidelines (R) | .67 | ||||
| Most nurses typically adhere to standard precautions | .57 | ||||
| People interpret standard precaution guidelines differently (R) | .55 | ||||
| Most doctors typically adhere to standard precautions | .49 | ||||
| I am able to decide whether or not to use personal protective equipment based on the clinical risks to me | .68 | ||||
| I am educated and able to weigh up risks/benefits of not using standard precautions when needed | .63 | ||||
| The more experienced I become at my job, the more likely I am to be able to decide when I need to use standard precautions | .58 | ||||
| My assessment of a patient's status will indicate if I need to follow standard precautions guidelines | .56 | ||||
| I assess what is wrong with a patient before deciding whether or not to implement standard precautions | .56 | ||||
| Eigenvalue | 4.90 | 3.14 | 2.23 | 1.90 | 1.57 |
| %variance explained | 16.90 | 10.83 | 7.70 | 6.54 | 5.41 |
| Correlation matrix (weighted scores) | |||||
| Justification | 1 | ||||
| Leadership | −.21 | 1 | |||
| Contextual cues | −.15 | .04 | 1 | ||
| Culture/practice | −.10 | .07 | −.01 | 1 | |
| Judgement | −.21 | .02 | .18 | .03 | 1 |
| Mean | 5.12 | 17.25 | 13.01 | 12.00 | 6.58 |
| Standard deviation | 4.85 | 4.97 | 5.87 | 3.35 | 4.61 |
| Cronbach's α | .79 | .85 | .71 | .61 | .67 |
Note: No items cross‐loaded on any factor >.25. R = Reverse coded item.
3.2. Temporal stability over 4 weeks
Prior to assessing the temporal stability of the factors, it was important to determine if there was any systematic effect at T1 between the 122 participants who participated in the retest phase of the study and those who did not. A multivariate analysis of variance was conducted to test this proposition using the summated factor scores at T1 as the dependent variables and participants' retested/not retested at T2 as two levels of the independent variable. There was no significant difference between these two groups (Pillai's trace F 5, 251 = 2.11, P = .065, partial η 2 = .04 on T1 data).
ICC were used to test the stability of scores on the five factor over the 4 week period between T1 and T2 testing for these 122 persons (Table 2). All ICC were significant and ranged in magnitude from .69 to .84, which Cicchetti (1994) considered good to excellent.
Table 2.
Means, standard deviations, and intraclass correlations of the five factors of the Factors Influencing Adherence to Standard Precautions Scale for the 122 participants who completed times 1 and 2
| Factors | Means (SD) | Intraclass correlations (r) | |
|---|---|---|---|
| Time 1 | Time 2 | Times 1–Time 2 | |
| Leadership | 17.69 (4.86) | 17.71 (4.43) | .84* |
| Justification | 4.90 (4.78) | 4.98 (4.84) | .84* |
| Contextual cues | 12.52 (6.22) | 11.66 (6.48) | .77* |
| Culture/practice | 11.74 (3.47) | 12.11 (3.13) | .80* |
| Judgement | 6.27 (4.48) | 5.45 (3.95) | .69* |
P < 0.001. SD = standard deviation.
3.3. Study 2: Confirmatory factor analysis
A second study was conducted 6 months later with a different sample in order to validate the factor structure of the FIASPS developed in study 1.
3.4. Participants
Participants were again nurses registered to practice. Complete data were available from 384 participants (53 males, 331 females). There was no gender difference with respect to age (female mean age = 44.00 years, SD = 9.65; male mean age = 42.19 years, SD = 10.21; independent t‐test t 382 1.25, P = .209).
The majority of participants (63%) reported that they worked full time. As in the previous sample, the majority of nurses worked in critical care areas (intensive care, coronary care, and high‐dependency units, 49%), 12.5% worked in the emergency department, 5.7% in medical care, 2.6% in surgical care, while the balance were variously employed in community, aged care education, or clinical management.
3.5. Procedure
Volunteers were recruited as in study 1. The anonymity of the data precluded us from determining if any persons had also participated in study 1. Participants were asked to provide demographic data on their age and sex, and to complete the FIASPS developed in study 1.
3.6. Data analysis and sample size
Confirmatory factor analysis (CFA) (AMOS, version 7) was used to determine the stability of the factor structure in this second sample. Sample sizes for CFA are based on the number of parameters to be estimated, ranging from five to 20 cases per parameter (Tabachnick & Fidell, 2013). In the current study, using a ratio of 5:1, a sample of 300 was considered adequate.
3.7. Findings
The inspection of histograms, box plots, skewness, kurtosis, and Shapiro–Wilk statistics revealed approximate normality across all items. The independent χ2 (χ2 indep300 = 2474.19, P < .001) indicated that associations were present among the variables and supported their suitability for CFA. The χ2 (χ2 365 = 566.24, P < .001) and the goodness‐of‐fit indices supported the fit of the data to the five factor structure: χ2/degrees of freedom = 1.55, goodness of fit index (GFI) = .907, adjusted GFI = .889, incremental fit index = .923, Tucker–Lewis index = .913, comparative fit index = .922, root mean square error of approximation = .038, and standardized root mean square residual = .054.
Each variable loaded onto its hypothesized factor, and the intercorrelations among factors were acceptable (r = .04–.54) confirming their independence. The standardized factor loadings (β) and interfactor correlations (r) are shown in Figure 1.
Figure 1.
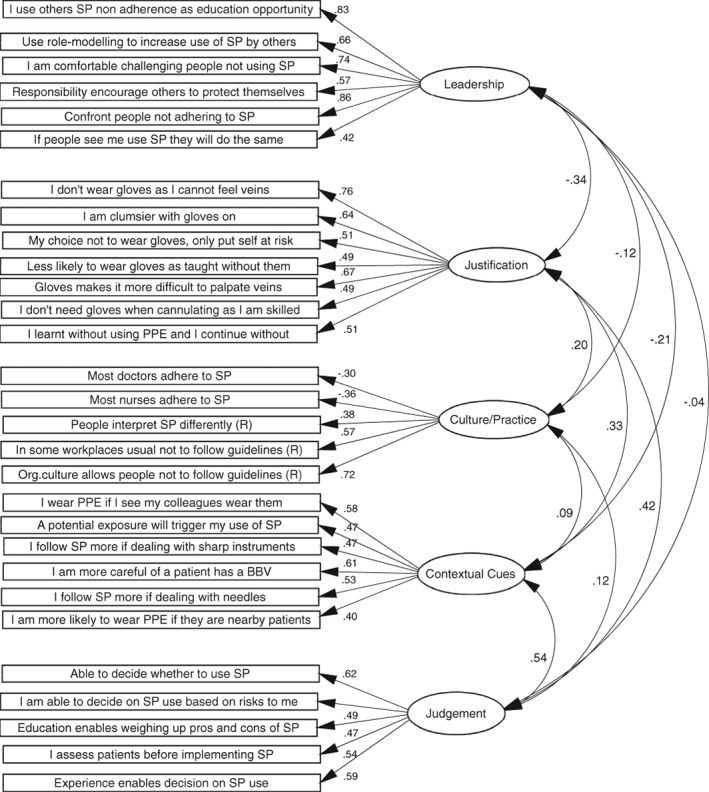
Confirmatory factor structure of the Factors Influencing Adherence to Standard Precautions Scale. BBV = blood‐borne virus; PPE = personal protective equipment; R = reverse coded Item; SP = standard precaution guidelines
4. DISCUSSION
The aim of these two studies was to develop and validate a scale designed to assess the factors influencing health‐care workers' adherence to SP in a large sample of nurses. A series of items was written following initial interviews with 29 nursing staff to reflect factors that might influence adherence to SP. These items were reviewed by experts to ensure that they were couched in plain language, clearly understandable by clinicians, and had face validity.
Analysis of the scale data in study 1 revealed five independent factors: judgement, leadership, culture/practice, contextual cues, and justification, which explained a substantial 48% of the variance. The temporal stability of these factors over a 4 week interval using ICC was acceptable for leadership, justification, contextual cues, and culture/practice (all >.78), although the ICC for judgement was moderate (.69). It might be that participants reflected on their own practices during the 4 week interval, and at least some of the participants reconsidered their ability to judge patients and situations (e.g. I am [not] able to decide whether or not to use personal protective equipment [PPE] based on clinical risks to me) as a function of raised awareness from participation in the initial phase of the study.
In study 2, conducted 6 months later, the construct validity of the five factor scale was confirmed using a CFA in a second sample of 384 registered nurses. A discussion of the factors follows.
The judgement factor reflects nurses making an assessment of the situation and of the patient (e.g. I am able to decide whether or not to use personal protective equipment based on the clinical risks to me). Such judgements are outside the guidelines. Furthermore, nurses who make these judgements not only ignore patient safety but might also be perceived as having some level of invincibility, that is, they will not be at risk. A sense of invincibility has been linked with risk‐taking behavior in the leisure context (Roberts & Kennedy, 2006; Wickman & Koniak‐Griffin, 2013), and it might be that those exhibiting this personality trait might also exhibit it in other areas, including the workplace. This factor aligns with Efstathiou et al.’s (2011b) finding that nurses who failed to follow some or all of the guidelines stated they did so because they had confidence in their capabilities and enough experience to make a judgement about the situation. It is encouraging that the mean score on this factor in the current sample was reasonably low (mean = 6.58, range 0–20).
The leadership factor encompasses items related to staff confronting others they observed not adhering to SP (e.g. I feel the need to confront people I see not adhering to standard precautions), as well as staff modelling the use of SP with the aim of promoting their use by others. This proactive approach can be likened to a type of informed leadership. The emergence of this factor supports the work of Neves et al. (2011), who showed that leadership and good supervision influenced adherence to SP. Both of these dimensions are in the spirit of Lymer, Richt, and Isaksson's (2004) findings, which showed that leadership and supervision have an impact on adherence to SP through increases in the safety culture of the workplace. Leadership was also a component of Efstathiou, Papastavrou, Raftopoulos, and Merkouris's (2011a) findings that senior nurses influenced more junior members of the nursing staff by their proactive behaviors. Conversely, junior nurses were less likely to adopt SP if witnessing one of their supervisors not following the guidelines. In the current sample, the average score for leadership was high (mean = 17.25, range 0–24), suggesting that nurses in our sample were willingly to confront those not adhering to standards, as well as modelling appropriate behaviors.
The organizational culture and practice factor relates to issues within the organization itself that promote or hinder the use of SP (e.g. The culture of my organization allows for people [not] to follow standard precaution guidelines [reverse coded to demonstrate a positive culture]). It includes items addressing professional practice, in particular, whether or not it is usual practice to follow SP in the organization. While encouraging, the mean rating on the culture factor in the current sample was moderate (mean = 12.00, range 0–20). Past research from Lymer, Richt, and Isaksson (2004) found that the organizational culture was important in promoting adherence to the guidelines. While the leadership factor extracted from the current data measures the impact of an individual's leadership and supervision, the culture/practice subscale is directed more at people's perceptions of the organizational climate as a reinforcement, or not, of SP use. Clearly, it is important for the organization to establish expectations that staff will adhere to SP, and furthermore, to ensure that these expectations are met.
The contextual cues factor contains items that can be seen to act as cues to action. For example, the proximity of personal protective equipment might act as a cue to its use, even in emergency situations; likewise, staff awareness of a patient's status with respect to a blood‐borne virus (BBV) might also be a determinant, as would knowing that the organizational culture supports SP use. Such cues seem to encourage individuals to adopt SP and might lead to the behaviors becoming habitual, that is, behavior repeated until it has become more or less automatic (Nilsen, Roback, Brostrom, & Ellstrom, 2012). Certainly, Neal, Wood, Wu, and Kurlander (2011) showed that habits can be activated directly by contextual cues that are outside the individual's overt sense of awareness, although this factor was not highly endorsed by current participants (mean = 13.01, range 0–24). The presence of positive or negative cues, such as knowledge of a patient's BBV status or lack of available PPE, has been described previously as factors influencing adherence to SP (Cutter & Jordan, 2012; Madan, Raafat, Hunt et al., 2002; Tait et al., 2000; Wu et al., 2008), although using one's knowledge of a patient's status to decide whether or not to use SP is against the basic premise of mandated SP use.
The justification factor relates to the reasons participants cited to rationalize their non‐adherence to SP, and pleasingly, the mean in this sample was low (mean = 5.12, range 0–28). For instance, not using gloves was justified on the basis that their use makes for a more clumsy execution of the task, that staff had trained for tasks without using gloves, and that wearing gloves reduces tactile feelings. These comments support Cutter and Jordan's (2012), Gammon, Morgan‐Samuel, and Gould's (2008), and Tait et al.’s (2000) research, where they reported that staff refrained from using PPE, such as gloves, due to their perception that PPE interfered with their skilled delivery of clinical procedures or increased their workload due to a need to repeat procedures. Interestingly, in a study of cannulation failure rates, Zhang, Lee, and Knott (2014) found no difference in whether or not participants used gloves, suggesting that glove use did not impede the administrator's skill, thus negating this justification. However, they did find that participants who did not use gloves reported more incidents related to significant blood spillage than those who did use gloves.
4.1. Limitations
The current findings would be enhanced by the assessment of convergent validity with a like measure. There is a possibility of response bias among the participants, and further, some participants might have responded to both studies. Despite these limitations and the need to replicate the findings across a range of health‐care settings, the results indicate that the FIASPS is a psychometrically‐robust scale that is stable over a 4 week period and across samples.
4.2. Implications
The FIASPS provides a validated instrument to ascertain the factors that influence adherence to SP among nurses. It would be suitable to determine the effectiveness of current nursing curricula around the delivery of infection prevention and control content, specifically the implementation of SP. Results from studies with nurse trainees, especially those on placement, would enable educational experts to review and strengthen curricula to take into account the psychosocial factors that are shown to affect behaviors and application of the guidelines, in addition to providing students with knowledge of the guidelines.
4.3. Conclusion
The current studies have yielded a robust measure of the factors influencing adherence to SP: judgement, leadership, culture/practice, contextual cues, and justification, which addresses a gap in the literature. Past research has focused largely on levels of adherence to SP, rather than addressing factors that might influence their use. This latter is important if behavioral and attitudinal changes are to be achieved and the risk of infection to both patients and staff reduced.
In summary, the FIASPS presents a novel means for researchers and clinicians to evaluate at least some of the factors influencing adherence to SP among nurses. Further research is required to validate its use with health‐care trainees and workers in both educational and health‐care settings. The results of such assessments can inform the design of specific interventions at individual and organizational levels to enhance health‐care workers’, and particularly trainees’, adherence to SP.
AUTHOR CONTRIBUTIONS
Study design: S.B. and K.M.
Data collection: S.B.
Data analysis: S.B. and K.M.
Revisions for important intellectual content: S.B. and K.M.
ACKNOWLEDGMENTS
The authors thank the participating nurses and the Australian College of Critical Care Nurses for distributing the survey.
Bouchoucha SL, Moore KA. Factors Influencing Adherence to Standard Precautions Scale: A psychometric validation. Nurs Health Sci. 2019;21:178–185. 10.1111/nhs.12578
[Correction added on November 9, 2018 after first online publication: ‘Minichov et al. (2016)’ has been corrected to ‘Michinov et al. (2016)’ in abstract section and in the reference list.]
REFERENCES
- Askarian, M. , McLaws, M. L. , & Meylan, M. (2007). Knowledge, attitude, and practices related to standard precautions of surgeons and physicians in university‐affiliated hospitals of Shiraz, Iran. International Journal of Infectious Diseases, 11(3), 213–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouchoucha, S. L. , & Moore, K. A. (2018). Infection prevention and control: Who is the judge, you or the guidelines? Journal of Infection Prevention, 19(3), 131–137. 10.1177/1757177417738332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control . (1982). Acquired immune deficiency syndrome (AIDS): Precautions for clinical and laboratory staffs. Morbidity and Mortality Weekly Report, 31(43), 577–580. [PubMed] [Google Scholar]
- Centers for Disease Control . (1985). Recommendations for preventing transmission of infection with human T‐Lymphotropic Virus Type III/Lymphadenopathy‐associated virus in the workplace. Mortality and Morbidity Weekly Report, 34(45), 682–695. [PubMed] [Google Scholar]
- Centers for Disease Control . (1987). Recommendations for prevention of HIV transmission in healthcare settings. Mortality and Morbidity Weekly Report, 36(S), 3–18. [Google Scholar]
- Cheung, K. , Chan, C. K. , Chang, M. Y. , Chu, P. H. , Fung, W. F. , Kwan, K. C. , … Mak, H. M. (2015). Predictors for compliance of standard precautions among nursing students. American Journal of Infection Control, 43(7), 729–734. 10.1016/j.ajic.2015.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutter, J. , & Jordan, S. (2012). Inter‐professional differences in compliance with standard precautions in operating theatres: A multi‐site, mixed methods study. International Journal of Nursing Studies, 49(8), 953–968. [DOI] [PubMed] [Google Scholar]
- DeVellis, R. (2012). Scale development ‐ Theory and application. London: Sage. [Google Scholar]
- Efstathiou, G. , Papastavrou, E. , Raftopoulos, V. , & Merkouris, A. (2011a). Compliance of Cypriot nurses with standard precautions to avoid exposure to pathogens. Nursing & Health Sciences, 13(1), 53–59. [DOI] [PubMed] [Google Scholar]
- Efstathiou, G. , Papastavrou, E. , Raftopoulos, V. , & Merkouris, A. (2011b). Factors influencing nurses' compliance with Standard Precautions in order to avoid occupational exposure to microorganisms: A focus group study. BMC Nursing, 10(1), 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gammon, J. , Morgan‐Samuel, H. , & Gould, D. (2008). A review of the evidence for suboptimal compliance of healthcare practitioners to standard/universal infection control precautions. Journal of Clinical Nursing, 17(2), 157–167. 10.1111/j.1365-2702.2006.01852.x [DOI] [PubMed] [Google Scholar]
- Garner, J. S. (1996). Guidelines for isolation precautions in hospitals. Infection Control and Hospital Epidemiology, 17(1), 13–21. [DOI] [PubMed] [Google Scholar]
- Gorsuch, R. L. (1983). Factor analysis. Hillsdale, NJ: Erlbaum. [Google Scholar]
- Hair, J. F., Jr. , Black, W. C. , Babin, B. J. , & Anderson, R. E. (2010). Multivariate data analysis: A global perspective (7th ed.). Sydney, Australia: Pearson. [Google Scholar]
- Hills, S. , & Wilkes, L. (2003). Occupational exposure of nurses working in high risk areas: An Australian study. Australian Journal of Advanced Nursing, 21(1), 28–34. [Google Scholar]
- Hogarty, K. , Hines, C. , Kromrey, J. , Ferron, J. , & Mumford, K. (2005). The quality of factor solutions in exploratory factor analysis: The influence of sample size, communality, and overdetermination. Educational and Psychological Measurement, 65(2), 202–226. [Google Scholar]
- Kelen, G. D. , DiGiovanna, T. A. , Celentano, D. D. , Kalainov, D. , Bisson, L. , Junkins, E. , … Quinn, T. C. (1990). Adherence to universal (barrier) precautions during interventions on critically ill and injured emergency department patients. Journal of Acquired Immune Deficiency Syndromes, 3(10), 987–994. [PubMed] [Google Scholar]
- Lam, S. C. (2011). Universal to standard precautions in disease prevention: Preliminary development of compliance scale for clinical nursing. International Journal of Nursing Studies, 48(12), 1533–1539. 10.1016/j.ijnurstu.2011.06.009 [DOI] [PubMed] [Google Scholar]
- Lam, S. C. (2014). Validation and cross‐cultural pilot testing of compliance with standard precautions scale: Self‐administered instrument for clinical nurses. Infection Control and Hospital Epidemiology, 35(5), 547–555. [DOI] [PubMed] [Google Scholar]
- Loewenthal, K. M. (2004). An introduction to psychological tests and scales (2nd ed.). Hove: Psychology Press. [Google Scholar]
- Lymer, U. B. , Richt, B. , & Isaksson, B. (2004). Blood exposure: Factors promoting health care workers' compliance with guidelines in connection with risk. Journal of Clinical Nursing, 13(5), 547–554. [DOI] [PubMed] [Google Scholar]
- Madan, A. K. , Raafat, A. , Hunt, J. P. , Rentz, D. , Wahle, M. J. , & Flint, L. M. (2002). Barrier precautions in trauma: Is knowledge enough? Journal of Trauma‐Injury Infection & Critical Care, 52(3), 540–543. [DOI] [PubMed] [Google Scholar]
- Madan, A. K. , Rentz, D. E. , Wahle, M. J. , & Flint, L. M. (2001). Non compliance of health care workers with universal precautions during trauma resuscitations. Southern Medical Journal, 94(3), 277–280. [PubMed] [Google Scholar]
- Michinov, E. , Buffet‐Bataillon, S. , Chudy, C. , Constant, A. , Merle, V. , & Astagneau, P. (2016). Sociocognitive determinants of self‐reported compliance with standard precautions: Development and preliminary testing of a questionnaire with French health care workers. American Journal of Infection Control, 44(1), 14–19. 10.1016/j.ajic.2015.07.041 [DOI] [PubMed] [Google Scholar]
- Neal, D. T. , Wood, W. , Wu, M. , & Kurlander, D. (2011). The pull of the past: When do habits persist despite conflict with motives? Personality and Social Psychology Bulletin, 37(11), 1428–1437. 10.1177/0146167211419863 [DOI] [PubMed] [Google Scholar]
- Neves, H. C. C. , Souza, A. C. S. e. , Medeiros, M. , Munari, D. B. , Ribeiro, L. C. M. , & Tipple, A. F. V. (2011). Safety of nursing staff and determinants of adherence to personal protective equipment. Revista Latino‐Americana de Enfermagem, 19(2), 354–361. [DOI] [PubMed] [Google Scholar]
- Nilsen, P. , Roback, K. , Brostrom, A. , & Ellstrom, P.‐E. (2012). Creatures of habit: Accounting for the role of habit in implementation research on clinical behaviour change. Implementation Science, 7(1), 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunnally, J. (1967). Psychometric theory. New York, NY: McGraw‐Hill. [Google Scholar]
- Osborne, S. (2003). Influences on compliance with standard precautions among operating room nurses. American Journal of Infection Control, 31(7), 415–423. [DOI] [PubMed] [Google Scholar]
- Pereira, F. M. V. , Lam, S. C. , Chan, J. H. M. , Malaguti‐Toffano, S. E. , & Gir, E. (2015). Difference in compliance with standard precautions by nursing staff in Brazil versus Hong Kong. American Journal of Infection Control, 43(7), 769–772. 10.1016/j.ajic.2015.03.021 [DOI] [PubMed] [Google Scholar]
- Rabaud, C. , Zanea, A. , Mur, J. M. , Blech, M. F. , Dazy, D. , May, T. , & Guillemin, F. (2000). Occupational exposure to blood: Search for a relation between personality and behavior. Infection Control and Hospital Epidemiology, 21(9), 564–574. [DOI] [PubMed] [Google Scholar]
- Reda, A. A. , Fisseha, S. , Mengistie, B. , & Vandeweerd, J.‐M. (2010). Standard precautions: Occupational exposure and behavior of health care workers in Ethiopia. PLoS One, 5(12), e14420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts, S. T. , & Kennedy, B. L. (2006). Why are young college women not using condoms? Their perceived risk, drug use, and development vulnerability may provide important clues to sexual risk. Archives of Psychiatric Nursing, 20(1), 32–40. [DOI] [PubMed] [Google Scholar]
- Siegel, J. D. , Rhinehart, E. , Jackson, M. , & Chiarello, L. (2007). Guidelines for isolation precaution: Preventing transmission of infectious agents in healthcare settings. Atlanta, GA: Centers for Disease Control; Retrieved from http://www.cdc.gov/ncidod/dhqp/pdf/isolation2007.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, P. W. , Watkins, K. , & Hewlett, A. (2012). Infection control through the ages. American Journal of Infection Control, 40(1), 35–42. [DOI] [PubMed] [Google Scholar]
- Tabachnick, B. G. , & Fidell, L. S. (2013). Using multivariates statistics (7th ed.). Boston, MA: Pearson. [Google Scholar]
- Tait, A. R. , Voepel‐Lewis, T. , Tuttle, D. B. , & Malviya, S. (2000). Compliance with standard guidelines for the prevention of occupational transmission of bloodborne and airborne pathogens: A survey of postanesthesia nursing practice. The Journal of Continuing Education in Nursing, 31(1), 38–44. [Google Scholar]
- Valim, M. D. , Marziale, M. H. P. , Richart‐Martínez, M. , & Sanjuan‐Quiles, A. (2014). Instruments for evaluating compliance with infection control practices and factors that affect it: An integrative review. Journal of Clinical Nursing, 23(11–12), 1502–1519. [DOI] [PubMed] [Google Scholar]
- Wickman, M. E. , & Koniak‐Griffin, D. (2013). Invincibility fable: Tool development to measure invincibility. Journal of Pediatric Nursing, 28(6), 575–584. 10.1016/j.pedn.2012.05.007 [DOI] [PubMed] [Google Scholar]
- Wu, S. , Li, L. , Wu, Z. , Cao, H. , Lin, C. , Yan, Z. , … Cui, H. (2008). Universal precautions in the era of HIV/AIDS: Perception of health service providers in Yunnan, China. AIDS and Behavior, 12(5), 806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, M. , Lee, M. , & Knott, S. (2014). Is clinical performance adversely affected by wearing gloves during paediatric peripheral intravenous cannulation? Emergency Medicine Australasia, 26, 455–460. 10.1111/1742-6723.12277 [DOI] [PubMed] [Google Scholar]


