Abstract
In developing countries acute infectious diarrhoea remains one of the leading causes of death among young children, especially those under 1 year of age. In contrast, in industrialized nations the death rate is very low, although the disease is an important cause of morbidity and consumes substantial healthcare costs. A variety of viral, bacterial and parasitic organisms have been implicated in the pathogenesis of acute diarrhoea. The primary objectives of treatment of acute infectious diarrhoea are correction of dehydration with oral replacement therapy (ORT) and maintenance of good nutritional status via food intake. With regards drug therapy antimicrobial agents are not usually recommended since the disease is generally self‐limiting. Racecadotril is powerful and selective enkephalinase inhibitor and has emerged as a promising drug in the antisecretory therapy of acute infectious diarrhoea in children.
Conclusion: There is encouraging evidence that treatment with racecadotril can provide clinically relevant symptomatic relief by reducing the severity and duration of diarrhoeal episodes. The drug is well tolerated and has a favourable safety profile. However, further comparative studies and cost‐effectiveness analyses are needed to define the position of the drug in the management of diarrhoeal illness in children.
Keywords: Antisecretory therapy, Diarrhoea, Racecadotril, Rehydration therapy

INTRODUCTION
Acute diarrhoea is one of the most common causes of morbidity and mortality in children worldwide, and it remains a major public health challenge especially in developing countries where it is a leading cause of death (1). This is despite the fact that in the past couple of decades improvements have been made with respect to the widespread distribution and use of oral rehydration solutions, increased rates of breastfeeding and better sanitation and hygiene; all of which have contributed to a reduction in disease burden (2).
The incidence of the disease varies largely according to geography, with an estimated incidence between 1.3 and 2.3 episodes of diarrhoea per child per year in industrialized countries compared with 3–9 episodes per child per year in the developing world (3). Estimates of mortality in developing countries based on studies published between 1992 and 2000 showed a median mortality of 4.9 children per 1000 per year in the first 5 years of life. Overall, in this cohort of children, diarrhoea accounted for 21% of all deaths, which represents between 1.5 and 2.5 million deaths per year, and the risk is greatest among children under 1 year of age (3). In contrast, deaths from diarrhoea are uncommon in industrialized countries, but the disease remains an important cause of morbidity and incurs substantial healthcare costs (4). It has been estimated that 1 in 40–50 children <5 years of age with serogroup A rotavirus infection requires hospital admission for the control of diarrhoea or treatment of related complications (5, 6). In addition to the direct health burden, consequences of diarrhoea include possible malnutrition, diminished growth and impaired cognitive development (7, 8).
Causative agents
A variety of bacterial, viral and parasitic organisms have been implicated in the pathogenesis of acute infectious diarrhoea. About 50–80% of episodes are caused by viruses, most notably rotaviruses or noroviruses, which are the leading cause of severe, dehydrating gastroenteritis among children (9, 10). Children infected with rotavirus may experience 10–20 bowel movements per day and vomiting for periods of 24 h or longer; consequently, dehydration is a major concern. Young children are particularly at risk of dehydration because of their higher surface‐to‐volume ratio, higher metabolic rate, smaller fluid reserves and their dependency on others for fluid intake. Rotavirus illness is difficult to prevent because it is easily transmitted (e.g. between family members in the home, and between children in preschool or day‐care settings); furthermore, children can be infected more than once (11). Therefore, implementing a vaccination program to protect against more severe subsequent infections represents an ideal means of preventing moderate‐to‐severe rotavirus infections.
Other viral agents include human caliciviruses (noroviruses), accounting for 4–19% of episodes of acute gastroenteritis in young children (12). Enteric adenoviruses and astroviruses are associated with approximately 2–12% of episodes of gastroenteritis (2). Several other enteric viruses, including coronaviruses, toroviruses and picobirnaviruses have been detected in children with diarrhoea, but their aetiological role is poorly defined.
Children in developing countries are exposed to a wide range of bacterial enteric pathogens and suffer numerous episodes of diarrhoeal illness as a result. Enterotoxigenic Escherichia coli, Campylobacter and Shigella species are the agents most commonly identified. The presence of specific virulent characteristics defines five classes of diarrhoeagenic E. coli: enterotoxigenic E. coli (ETEC), enteropathogenic E. coli (EPEC), enteroinvasive E. coli (EIEC), enterohaemorrhagic E. coli (EHEC) and enteroaggregative E. coli (EAEC) (13). In addition, Vibrio cholerae, Salmonella species (S. enteritidis, S. typhimurium) and Yersinia enterocolitica are other bacterial causes of acute infectious diarrhoea in children.
Although viral and bacterial agents are responsible for the majority of diarrhoeal illness, parasitic agents account for a small proportion of cases. Giardia lamblia, Cryptosporidium parvum, Entamoeba histolytica, Blastocystis hominis and Ascaris lumbricoides are the parasites that are most commonly associated with diarrhoea in children (14).
Pathogenic mechanisms
The initial event in the pathogenesis of acute infection is the ingestion of the offending organism, which colonizes the intestinal epithelium and adheres to enterocytes. Rotavirus and other intestinal viruses penetrate into the cytosol of enterocytes in the small bowel. Different pathways are involved depending upon the pathogen, including an effacement–attachment process in the small bowel, invasion of the epithelial layer of the intestinal mucosa usually occurring in the colon, or production of an enterotoxin. A simplified schematic representation of the pathogenetic mechanism of acute infectious diarrhoea is shown in Figure 1. For example, diarrhoea caused by invasive bacteria such as Shigella spp. is due to the failure of the colon to reabsorb water entering into the colon from the ileus.
Figure 1.
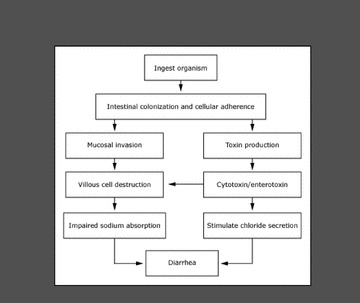
Pathogenic mechanism of acute infectious diarrhoea.
Enteric viruses cause diarrhoea through different mechanisms, including interference with gastrointestinal motility or damaging the intestinal epithelium and reducing brush border enzymes. The reduction in enzyme levels results in a failure to metabolize dietary carbohydrates with consequent osmotic diarrhoea. As shown in Figure 2, once rotavirus enters the small intestine, it attaches to glycolipids on the surface of the mature villous tip cells that line the small intestine. The virus invades the villous tip cells, causing villous atrophy, loss of digestive enzymes and a reduction of absorption. Once the villi become blunted, the resulting malabsorption of carbohydrates results in diarrhoea, which persists until the villi are regenerated. In addition, the nonstructural protein (NSP4) has been shown to act as a viral enterotoxin contributing to the pathogenic mechanisms of diarrhoea (15).
Figure 2.
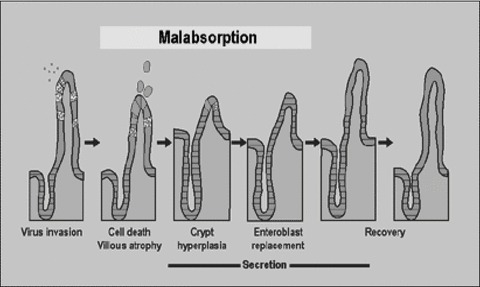
Mechanism of acute diarrhoeal illness caused by rotavirus.
Enteric bacteria induce clinical disease via the production of toxins and invasion of the enteric mucosa. Some agents, such as V. cholerae and ETEC, release enterotoxins that cause diarrhoea by activation of secretory mechanisms in the intestinal mucosa. In secretory diarrhoea no morphologic epithelial injury is present. Other bacterial agents, including Shigella spp., Campylobacter jejuni, Salmonella spp., Yersinia enterocolitica, EIEC, as well as the protozoa E. histolytica produce cytotoxins that lead to destruction of the intestinal epithelium, resulting in inflammatory diarrhoea. The diarrhoeal stools contain mucus, exudate and bleed and the release of inflammatory mediators stimulates fluid secretion. Hypermotility also results in diarrhoeal fluid losses. Hormones involved in hypermotility of acute infectious gastroenteritis include motilin, neurotensin, cholecystokinin and vasoactive intestinal peptide (VIP). Finally, some enteric pathogens can penetrate the intestinal mucosa and disseminate through the regional lymphatic system to enter the bloodstream, resulting in systemic manifestations.
Acute diarrhoea usually manifests as an increase in the frequency or volume of stool. Liquid faeces (like ‘dirty water’) are characteristic of secretory diarrhoea. Patients with enteroinvasive diarrhoea present with expulsion of faeces with mucus and blood. Expulsion of lumpy, acid faeces is observed in viral diarrhoea. In parasitic diarrhoea (Giardia lamblia), yellow doughy faeces are accompanied by a prominent and tympanic abdomen and abdominal pain. Fever is a common occurrence and usually is associated with invasive pathogens. Vomiting is observed more frequently in viral diarrhoea. However, determining the causative agent of diarrhoea in an individual patient based on clinical grounds alone is usually difficult (2). Differences in clinical findings according to the causative organisms are summarized in Table 1.
Table 1.
Differential diagnosis of acute infectious diarrhoea in children according to causative agents
| Clinical data | Rotavirus | Salmonella | Campylobacter | Shigella | Yersinia |
|---|---|---|---|---|---|
| Age | <2 years | Any | <5 years | Any | Any |
| Fever | Mild | Variable | Mild | Common | Common |
| Vomiting | Very frequent | Frequent | Sometimes | Sometimes | Sometimes |
| Abdominal pain | Mild | Moderate | Intense | Intense | Intense |
| Faeces | Watery | Loose, mucous and blood | Loose, mucous and blood | Loose, mucous and blood | Loose, mucous and blood |
Breastfeeding reduces the risk of infections such as diarrhoea and consequently, it also lowers healthcare costs as a result of a decreased rate of hospitalization for infectious diseases, including acute gastroenteritis and respiratory tract infections (16, 17). Human milk enhances the infant's immature immune system and strengthens host defence mechanisms against infectious agents. It achieves this through provision of bioactive factors, specific nutritional components, growth factors, nucleotides, colony stimulating factors, lactoferrin and cytokines all of which are present in breast milk (18). In addition, other constituents of breast milk promote gastrointestinal mucosal maturation, decrease the incidence of infection, alter gut microflora and have immunomodulatory and anti‐inflammatory properties (19, 20).
Management of the morbidity associated with diarrhoeal illness in children, and reducing the risk of death, is highly dependent on making a timely and accurate assessment of the status of hydration, followed by prompt institution of appropriate treatment. Clinical signs of dehydration are detailed in Table 2. Knowledge of the physiology of fluid balance, particularly intestinal electrolyte and nutrient transport, provides a basis for understanding the mechanisms of acute diarrhoeal disease and the rationale for oral rehydration therapy. Water absorption occurs primarily in the small intestine, driven by osmotic gradients that depend on the transport of the electrolytes sodium and chloride, as well as nutrients such as glucose and amino acids. Sodium, glucose and several amino acids are absorbed through the apical membranes of intestinal epithelial cells by a sodium‐dependent nutrient cotransporter system. Sodium is then transported from the cell across the basolateral membrane to the extracellular space by the enzyme Na+/K+‐ATPase. This enzyme utilizes energy to reduce the intracellular sodium concentration, which produces a negative extracellular electrical charge. The resultant electrochemical gradient facilitates sodium absorption by the epithelial cell, which drives the sodium‐dependent nutrient cotransporters. The anion chloride is absorbed to maintain electrical neutrality across the epithelium, and water is passively absorbed in response to the transport of these electrolytes and nutrients. Successful oral rehydration therapy with balanced sugar–salt solutions depends upon these simple physiologic principles.
Table 2.
Clinical signs of dehydration
| Sign | Severity of dehydration | ||
|---|---|---|---|
| Mild | Moderate | Severe | |
| Pulse | Normal | Fast | Fast‐weak |
| Blood pressure | Normal | Reduced | Reduced |
| Diuresis | Reduced | Very reduced | Oligoanuria |
| Oral mucosa | Pasty | Dry | Very dry |
| Fontanelle | Normal | Sunken | Very sunken |
| Eyes | Normal | Sunken | Very sunken |
| Skin | Normal | Cold | Acrocyanosis |
| Weight loss | |||
| Small children | <5% | 5–10% | >10% |
| Older children | <3% | 3–7% | >7% |
Rehydration therapy
Oral rehydration therapy (ORT) is designed to replace and maintain fluid levels through the administration of specially formulated oral rehydration solutions (ORS), combined with continued age‐appropriate nutrition (21, 22). ORT is now well accepted as a clinically efficacious and cost‐effective treatment option for the management of acute infectious gastroenteritis.
Although the secretory nature of diarrhoea results in substantial loss of water and electrolytes, an intact Na‐coupled solute cotransporter system allows efficient reabsorption of salt and water. Water passively follows the osmotic gradient generated by the transcellular transport of electrolytes and nutrients. Thus, the coupled transport of sodium and glucose molecules at the intestinal brush border is an essential requirement for ORS to work. Cotransport across the luminal membrane is facilitated by the protein, sodium‐glucose cotransporter 1 (SGLT1). Once in the enterocyte, the transport of glucose into the blood is facilitated by GLUT2 (glucose transporter type 2) in the basolateral membrane. Na+/K+‐ATPase provides the electrochemical gradient that drives the process. This mechanism remains intact, even in patients with severe diarrhoea (23).
The optimal osmolarity of ORS, determined by the concentration of sodium and glucose, has been reevaluated because clinical research has shown that children treated with an ORS of lower osmolarity had measurable reductions in stool output and vomiting, and less need for intravenous rehydration compared with children treated with the standard ORS (24, 25). The composition of the reduced osmolarity ORS, as recommended by WHO and the United Nations Children's Fund (UNICEF) (26) and the European Society for Pediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) (27) compared with the original ORS introduced in 1975, is shown in Table 3. Appropriate treatment for children with diarrhoea and dehydration includes the following principles (21, 27):
Table 3.
Composition of oral rehydration solutions
| WHO, 1975 | ESPGHAN, 1992 | WHO, 2002 | |
|---|---|---|---|
| Glucose, mmol/L | 111 | 74–111 | 75 |
| Sodium, mmol/L | 90 | 60 | 75 |
| Potassium, mmol/L | 20 | 20 | 20 |
| Chloride, mmol/L | 80 | 60 | 65 |
| Base, mmol/L | 30 | 10 (citrate) | 30 |
| Osmolarity, mosm/L | 331 | 225–260 | 245 |
-
1
ORS should be employed for rehydration using a hypotonic solution (60 mmol/L sodium)
-
2
Oral rehydration should be performed rapidly within 3–4 h
-
3
With regards realimentation, depending on age, an unrestricted diet is recommended as soon as dehydration is corrected
-
4
Breastfeeding should be continued
-
5
For formula fed babies, diluted formula is not recommended and special formula is usually not necessary
-
6
Additional ORS should be administered for ongoing losses caused by the diarrhoea
-
7
No unnecessary laboratory tests or medication should be administered.
The child with mild‐to‐moderate dehydration should receive 50–00 mL/kg of ORS over 3–4 h, administered at a rate of 75 mL/kg of body weight/h (e.g. 1 tea spoon = 5 mL, 1 tea spoon/min = 300 mL/h). Replacement fluids can be estimated at approximately 10 mL/kg for each stool and 2 mL/kg for each episode of emesis. This should be followed by additional ORS as needed to replace ongoing losses caused by vomiting and diarrhoea. Rehydration through a nasogastric tube can be particularly useful in emergency department setting, where rapid correction of hydration might prevent hospitalization. In this regard it is generally well tolerated, more cost‐effective, and associated with fewer complications than the alternative of intravenous infusion therapy (28). In a survey of 290 emergency paediatricians in Spain, 73.8% used a nasogastric tube to improve tolerance of ORT in the management of severe vomiting (29).
Despite the fact that the American Academy of Pediatrics (AAP) (1) and the Centers for Disease Control and Prevention (CDC) (6) have published practice parameters for the management of acute gastroenteritis, and both organizations recommend ORT as the preferred approach for treating mild‐to‐moderate dehydration caused by vomiting or diarrhoea, studies show that ORT continues to be underused globally (30, 31). A systematic review of 14 randomized controlled trials to compare ORT and intravenous therapy concluded that there were no clinically important differences between ORT and intravenous therapy in terms of efficacy and safety (32). In a review of 17 trials comparing oral and intravenous rehydration in children with gastroenteritis, it was calculated that only one in every 25 children (95% CI 14–100) would fail to respond to ORT and then require subsequent intravenous therapy (33). An algorithm for the management of acute diarrhoeal disease in children is shown in Figure 3.
Figure 3.
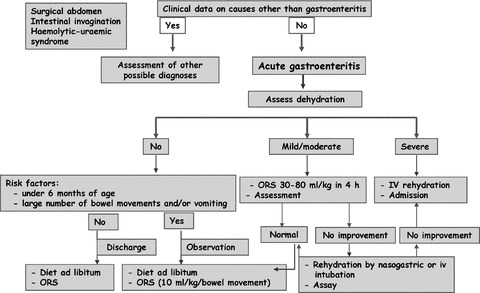
Therapeutic strategies in children presenting with acute diarrhoeal disease.
In order to supply a greater number of glucose molecules for cotransport of sodium without causing osmotic overload, an oral rehydration salt solution in which glucose (20 g/L) is replaced by 50–80 g/L of rice powder (with the electrolytes remaining unchanged) has been proposed to reduce stool output and duration of diarrhoea in patients with acute watery diarrhoea. Results from a systematic review indicates that the rice‐based oral rehydration appears to be effective in reducing stool output in patients with cholera, but it was not effective in infants and children with noncholera diarrhoea (34). Other strategies, including supplementation of ORS with partially hydrolyzed guar gum (35) and amylase‐resistant starch (36) (substances thought to generate short‐chain fatty acids in the colon and these accelerate colonic sodium and fluid absorption) have been shown to reduce stool output and the duration of diarrhoea. Moreover, addition of recombinant human lactoferrin and lysozyme to a rice‐based oral rehydration solution had beneficial effects in children with acute diarrhoea (37). Dietary management with a rice‐based diet containing either cooked green banana or pectin, in addition to their known colonotrophic effects, reduced the amount of stool, the need for ORS, and the duration of diarrhoea. It is thought that this effect was mediated by improvement of small intestinal permeability (38, 39).
Probiotics (microbial food components, which when administered in adequate amounts, confer a health benefit on the host due to antibacterial activity and immunostimulant capacity), appear to be a useful adjunct to rehydration therapy. Results of two systematic reviews (40, 41) and one meta‐analysis (42) of randomized controlled trials comparing probiotic therapy with placebo or nonprobiotic agents demonstrated a clinically significant benefit in terms of a reduction of diarrhoea, particularly with Lactobacillus GC. This was despite a large heterogeneity in the trials included in these analyses. However, the authors of these studies concluded that more research is needed to confirm the use of particular probiotic regimens in specific patient groups. Moreover, it has been argued that the beneficial effects of probiotics appear to be limited to a modest decrease in the duration of diarrhoea. In fact, in children less than 2 years of age with moderate to severe dehydrating diarrhoea, ORT plus Lactobacillus rhamnosus CG was no more effective than placebo in reducing the duration or severity of diarrhoea. This suggests that intestinal colonization must occur before benefits of probiotics can be realized (43). In a recent study, the probiotic yeast Saccharomyces boulardii administered as an adjuvant to ORS in ambulatory care in children less than 2 years old with mild or moderate acute diarrhoea decreased the duration of diarrhoea, accelerated recovery and reduced the risk of prolonged diarrhoea (44).
In summary, the optimal management of mild‐to‐moderately dehydrated children in Europe (45) should consist of (a) oral rehydration with a hypoosmolar glucose‐based 60 mmol/L sodium solution over 3–4 h and (b) rapid reintroduction of normal feeding thereafter. At all times, breastfeeding should be continued. Supplementation with ORS to compensate for fluid and electrolyte loss in the stool during continued diarrhoea, as clinically indicated, will further prevent the onset of dehydration. The use of lactose‐free formulae in the vast majority of children appears to be unjustified. Interestingly, results of a multicentre study performed in 29 European countries to determine how closely current treatment of acute gastroenteritis complicated by mild–to‐moderate dehydration compares with the ESPGHAN recommendations (46), revealed that a minority of physicians follow the guidelines regarding the use of rapid oral rehydration over 3–4 h, the inadequacy of lactose‐free formulae, and the use of ORS to minimize the effects from ongoing fluid loss‐associated watery diarrhoea.
Antisecretory treatment: racecadotril
The primary objectives of treatment of acute infectious diarrhoea are correction of dehydration with ORT and maintenance of good nutritional status via food intake (both milk and solids should not be withheld during diarrhoeal disease). Antimicrobial agents are not usually recommended for the routine treatment of acute diarrhoeal illness. Most episodes caused by bacteria and parasites are self‐limiting and can be managed effectively with ORS and adequate food intake. It has been shown that the return to usual eating habits reduces the abnormal increase in intestinal permeability that occurs in gastroenteritis, and may also enhance enterocytes regeneration and promote recovery of disaccharides in the brush border membrane.
A variety of nonspecific antidiarrhoeal agents (e.g. kaolin), antimotility agents (e.g. loperamide), antisecretory agents (e.g. bismuth salicylate) and toxin absorbents (e.g. cholestyramine, aluminium salts) have been used for the treatment of diarrhoea, especially in older children. Concerns regarding disadvantages, especially the possible masking of the severity of fluid loss into the intestine, and side effects have been expressed.
Racecadotril (acetorphan), an enkephalinase inhibitor, represents a promising new approach to the treatment of diarrhoea. The mechanism of action of racecadotril is shown in Figure 4. Water and electrolyte transport in the intestinal mucosa is regulated by local messengers (neuropeptides, amines, eicosanoids). Most of them act via the mediation of cyclic adenosine monophosphate (cAMP), activating or inhibiting its production from adenosine triphosphate. An increase in cAMP is induced by endogenous (e.g. VIP, PGE2) or exogenous agents (e.g. V. cholerae, E. coli toxins) and leads to net hypersecretion of water and electrolytes. Opiate neuropeptides are localized in the intestine myenteric and submucosal plexuses, where they modulate motility (mu receptors) and secretion (delta receptors). Activation of mu receptors prolongs intestinal transit while activation of delta receptors reduces intestinal secretion of water and electrolytes. Enkephalins activate delta receptors and inhibit adenylcyclase, thus facilitating a decrease in cAMP levels with a consequent reduction in water and electrolyte secretion. This antisecretory action, however, is brief because enkephalins are rapidly degraded by the membrane peptidase enkephalinase. Racecadotril is a prodrug that is rapidly hydrolysed in man into the active metabolite tiorphan, which is a powerful and selective enkephalinase inhibitor. Thus, the antisecretory action of enkephalins is prolonged in the presence of tiorphan (47, 48). Furthermore, unlike opiates and loperamide, racecadotril does not act on mu receptors and therefore it does not prolong intestinal transit, nor does it favour bacterial growth in the small intestine (49).
Figure 4.
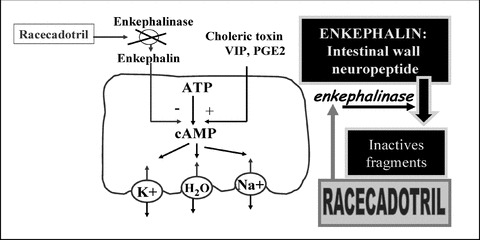
Mechanism of action of racecadotril.
Studies in children
Turk et al. (50) in a multicentre, parallel‐group, double‐blind, placebo‐controlled study compared racecadotril (1.5 mg/kg) with loperamide (0.03 mg/kg) three times daily in 102 children, aged 2–10 years, who were suffering from acute diarrhoea. No significant differences were found in faecal output or duration of diarrhoea. However, there were differences in tolerance, with a lower incidence of constipation and fewer associated treatment modifications in the racecadotril group. The authors concluded that racecadotril and loperamide were equally effective in treating acute diarrhoea in these children, and racecadotril had a superior tolerability and safety profile.
Salazar‐Lindo et al. (51) reported results from a double‐blind, randomized, placebo‐controlled study involving 135 boys (3–35 months of age) who had watery diarrhoea of 5 days duration. Sixty‐eight received racecadotril (1.5 mg/kg every 8 h) and 67 placebo, in addition to ORS. Children treated with racecadotril had significantly lower 48‐h stool output both in the intent‐to‐treat data set (45.6% reduction with racecadotril) and in the rotavirus‐positive subgroup (46.3% reduction with racecadotril). In patients positive for rotavirus, the duration of diarrhoea was significantly shorter compared with placebo (median 30 h vs. 90 h; p = 0.0001). The intake of ORS was significantly lower in the racecadotril group than in the placebo group (p < 0.001). Racecadotril was well tolerated with only seven patients reporting adverse effects, all of which were mild and transient. This study showed that in young boys with acute watery diarrhoea, racecadotril was an effective and well‐tolerated treatment.
Cézard et al. (52) published findings from a multicentre, double‐blind, parallel‐group, placebo‐controlled study in 172 infants aged 3 months–4 years who were hospitalized for acute diarrhoea. All received ORT, and 89 were treated with racecadotril (1.5 mg/kg every 8 h) and 83 with placebo. Children treated with racecadotril had significantly lower 24‐h and 48‐h faecal output, duration of diarrhoea, ORS intake, and incidence of dehydration. The efficacy of the drug was independent of the presence of rotavirus. Tolerability was good in both groups of children. This study confirmed the efficacy (up to 50% reduction in stool output) and tolerability of racecadotril as adjuvant therapy to ORS in the treatment of severe diarrhoea in infants and children.
Cojocaru et al. (53) compared racecadotril plus rehydration with rehydration alone in 166 children aged 3 months to 3 years who had acute diarrhoea and who were evaluated in the emergency department. Irrespective of the type of rehydration (oral or intravenous), the group treated with racecadotril had significantly lower faecal output and a faster recovery. Furthermore, the children receiving racecadotril needed fewer additional emergency department visits to manage the current bout of diarrhoea. This study confirmed the efficacy of racecadotril as adjuvant therapy to oral and intravenous rehydration in the treatment of acute diarrhoea, and it had the significant advantage of reducing the number of follow‐up visits to the emergency department before a full recovery was achieved.
A recent systematic review of randomized controlled trials compared racecadotril with placebo or no intervention as an adjunct to ORT in children with acute diarrhoea (54). Racecadotril, reduced the duration of acute diarrhoea and stool volume in children aged 3–48 months. The latter outcome is particularly important since quantitative diarrhoea criteria are recommended by the WHO for the evaluation of therapeutic agents in the management of this disorder (55). None of the studies revealed any significant adverse effects resulting from the administration of racecadotril, although some minor adverse effects were observed. These results apply primarily to hospitalized children; the efficacy of the racecadotril may be different for other subgroups (e.g. outpatients compared with in‐patients). The authors of the review concluded that, in three relatively small randomized controlled trials (51, 52, 53) with some methodological problems, racecadotril was effective in reducing the volume and frequency of stool output and in reducing the duration of diarrhoea (particularly in infants with rotavirus).
CONCLUSION
Racecadotril is a promising antisecretory drug that exerts its antidiarrhoeal effects by inhibiting intestinal enkephalins. Data from studies carried out in children provide evidence of the effectiveness of racecadotril in reducing stool output and the duration of diarrhoea in acute gastroenteritis. The drug is well tolerated and has shown a favourable safety profile. However, more studies are needed to assess the cost‐effectiveness of racecadotril and also its efficacy and tolerability relative to other treatment options.
ACKNOWLEDGEMENTS
We thank Marta Pulido, MD, for her contribution in the preparation of this article.
References
- 1. American Academy of Pediatrics . Practice parameter: the management of acute gastroenteritis in young children. Pediatrics 1996; 97: 424–35. [PubMed] [Google Scholar]
- 2. Podewils LJ, Mintz ED, Nataro JP, Parashar UD. Acute, infectious diarrhea among children in developing countries. Semin Pediatr Infect Dis 2004; 15: 155–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kosek M, Bern C, Guerrant RL. The global burden of diarrhoeal disease, as estimated from studies published between 1992 and 2000. Bull World Health Org 2003; 81: 197–204. [PMC free article] [PubMed] [Google Scholar]
- 4. Glass RI, Lew JF, Gangarosa RE, LeBaron CW, Ho MS. Estimates of morbidity and mortality rates for diarrheal diseases in American children. J Pediatr 1991; 118: S27–S33. [DOI] [PubMed] [Google Scholar]
- 5. Van Damme P, Giaquinto C, Huet F, Gothefors L, Maxwell M, Van Der Wielen M. REVEAL Study Group . Multicenter prospective study of the burden of rotavirus acute gastroenteritis in Europe, 2004–2005: the REVEAL study. J Infect Dis 2007; 195(Suppl 1): S4–16. [DOI] [PubMed] [Google Scholar]
- 6. Duggan C, Santosham M, Glass RI. The management of acute diarrhea in children: oral rehydration, maintenance, and nutritional therapy. Centers for Disease Control and Prevention. MMWR Recomm Rep 1992; 41(RR‐16): 1–20. [PubMed] [Google Scholar]
- 7. Niehaus M, Moore S, Patrick P, Derr LL, Lorntz B, Lima AA, et al Early childhood diarrhea is associated with diminished cognitive function 4 to 7 years later in children in a northeast Brazilian shantytown. Am J Trop Med Hyg 2002; 65: 590–93. [DOI] [PubMed] [Google Scholar]
- 8. Lorntz B, Soares AM, Moore SR, Pinkerton R, Gansneder B, Bovbjerg VE, et al Early childhood diarrhea predicts impaired school performance. Pediatr Infect Dis J 2006; 25: 513–20. [DOI] [PubMed] [Google Scholar]
- 9. Kapikian AZ, Wyatt RG, Dolin R, Thornhill TS, Kalica AR, Chanock RM. Visualization by immune electron microscopy of a 27‐nm particle associated with acute infectious nonbacterial gastroenteritis. J Virol 1972; 10: 1075–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bishop RF, Davidson GP, Holmes IH, Ruck BJ. Virus particles in epithelial cells of duodenal mucosa from children with acute non‐bacterial gastroenteritis. Lancet 1973; 2: 1281–3. [DOI] [PubMed] [Google Scholar]
- 11. Velasquez F, Matson D, Calva J. Rotavirus infection in infants as protection against subsequent infections. N Engl J Med 1996; 335: 1022–28. [DOI] [PubMed] [Google Scholar]
- 12. Dove W, Cunliffe NA, Gondwe JS, Broadhead RL, Molyneux ME, Nakagomi O, et al Detection and characterization of human caliciviruses in hospitalized children with acute gastroenteritis in Blantyre, Malawi. J Med Virol 2005; 77: 522–27. [DOI] [PubMed] [Google Scholar]
- 13. Bischoff C, Lüthy J, Altwegg M, Baggi F. Rapid detection of diarrheagenic E. coli by real‐time PCR. J Microbiol Methods 2005; 61: 335–41. [DOI] [PubMed] [Google Scholar]
- 14. Carvalho‐Costa FA, Gonçalves AQ, Lassance SL, De Albuquerque CP, Leite JP, Bóia MN. Detection of Cryptosporidium spp and other intestinal parasites in children with acute diarrhea and severe dehydration in Rio de Janeiro. Rev Soc Bras Med Trop 2007; 40: 346–8. [DOI] [PubMed] [Google Scholar]
- 15. Anderson EJ, Weber SG. Rotavirus infection in adults. Lancet Infect Dis 2004; 4: 91–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Quigley MA, Kelly YJ, Sacker A. Breastfeeding and hospitalization for diarrheal and respiratory infection in the United Kingdom millennium cohort study. Pediatrics 2007; 119: e837–42. [DOI] [PubMed] [Google Scholar]
- 17. Paricio Talayero JM, Lizán‐García M, Otero Puime A, Benlloch Muncharaz MJ, Beseler Soto B, Sánchez‐Palomares M, et al Full breastfeeding and hospitalization as a result of infections in the first year of life. Pediatrics 2006; 118: e92–9. [DOI] [PubMed] [Google Scholar]
- 18. Böttcher MF, Fredriksson J, Hellquist A, Jenmalm MC. Effects of breast milk from allergic and non‐allergic mothers on mitogen‐ and allergen‐induced cytokine production. Pediatr Allergy Immunol 2003; 14: 27–34. [DOI] [PubMed] [Google Scholar]
- 19. Koletzko B, Aggett PJ, Bindels JG, Bung P, Ferré P, Gil A, et al Growth, development and differentiation: a functional food science approach. Br J Nutr 1998; 80: S5–45. [DOI] [PubMed] [Google Scholar]
- 20. Oddy WH. The impact of breastmilk on infant and child health. Breastfeed Rev 2002; 10: 5–18. [PubMed] [Google Scholar]
- 21. King CK, Glass R, Bresee JS, Duggan C. Managing acute gastroenteritis among child. Oral rehydration, maintenance, and nutritional therapy. MMWR Recomm Rep 2003; 52(RR‐16): 1–16. [PubMed] [Google Scholar]
- 22. Fontaine O, Garner P, Bhan MK. Oral rehydration therapy: the simple solution for saving lives. BMJ 2007; 334(Suppl 1): s14. [DOI] [PubMed] [Google Scholar]
- 23. Acra SA, Ghishan GK. Electrolyte fluxes in the gut and oral rehydration solutions. Pediatr Clin North Am 1996; 43: 433–49. [DOI] [PubMed] [Google Scholar]
- 24. Hahn S, Kim Y, Garner P. Reduced osmolarity oral rehydration solution for treating dehydration due to diarrhoea in children: systematic review. BMJ 2001; 323: 81–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hahn S, Kim Y, Garner P. Reduced osmolarity oral rehydration solution for treating dehydration caused by acute diarrhoea in children. Cochrane Database Syst Rev 2002; (1): CD002847. [DOI] [PubMed] [Google Scholar]
- 26. World Health Organization . Oral rehydration salts (ORS): a new reduced osmolarity solution. Geneva , Switzerland : World Health Organization; 2002. [Google Scholar]
- 27. Recommendations for composition of oral rehydration solutions for the children of Europe. Report of an ESPGHAN Working Group. J Pediatr Gastroenterol Nutr 1992; 14: 113–5. [PubMed] [Google Scholar]
- 28. Nager AL, Wang VJ. Comparison of nasogastric and intravenous methods of rehydration in pediatric patients with acute dehydration. Pediatrics 2002; 109: 566–72. [DOI] [PubMed] [Google Scholar]
- 29. Sociedad Española deUrgencias dePediatría . Oral rehydration in pediatric emergencies. A Spanish survey. An Pediatr (Barc) 2004; 60: 243–8. [DOI] [PubMed] [Google Scholar]
- 30. Ozuah P, Avner J, Stein R. Oral rehydration, emergency physicians, and practice parameters: a national survey. Pediatrics 2002; 109: 259–61. [DOI] [PubMed] [Google Scholar]
- 31. Bender BJ, Ozuah PO. Intravenous rehydration for gastroenteritis: how long does it really take? Pediatr Emerg Care 2004; 20: 215–8. [DOI] [PubMed] [Google Scholar]
- 32. Bellemare S, Hartling L, Wiebe N, Russell K, Craig WR, McConnell D, et al Oral rehydration versus intravenous therapy for treating dehydration due to gastroenteritis in children: a meta‐analysis of randomised controlled trials. BMC Medicine 2004; 2: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hartling L, Bellemare S, Wiebe N, Russell K, Klassen TP, Craig W. Oral versus intravenous rehydration for treating dehydration due to gastroenteritis in children. Cochrane Database Syst Rev 2006; CD004390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Fontaine O, Gore SM, Pierce NF. Rice‐based oral rehydration solution for treating diarrhoea. Cochrane Database Syst Rev 2000; CD001264. [DOI] [PubMed] [Google Scholar]
- 35. Alam NH, Meier R, Schneider H, Sarker SA, Bardhan PK, Mahalanabis D, et al Partially hydrolyzed guar gum‐supplemented oral rehydration solution in the treatment of acute diarrhea in children. J Pediatr Gastroenterol Nutr 2000; 31: 503–7. [DOI] [PubMed] [Google Scholar]
- 36. Raghupathy P, Ramakrishna BS, Oommen SP, Ahmed MS, Priyaa G, Dziura J, et al Amylase‐resistant starch as adjunct to oral rehydration therapy in children with diarrhea. J Pediatr Gastroenterol Nutr 2006; 42: 362–8. [DOI] [PubMed] [Google Scholar]
- 37. Zavaleta N, Figueroa D, Rivera J, Sánchez J, Alfaro S, Lönnerdal B. Efficacy of rice‐based oral rehydration solution containing recombinant human lactoferrin and lysozyme in Peruvian children with acute diarrhea. J Pediatr Gastroenterol Nutr 2007; 44: 258–64. [DOI] [PubMed] [Google Scholar]
- 38. Rabbani GH, Teka T, Zaman B, Majid N, Khatun M, Fuchs GJ. Clinical studies in persistent diarrhea: dietary management with green banana or pectin in Bangladeshi children. Gastroenterology 2001; 121: 554–60. [DOI] [PubMed] [Google Scholar]
- 39. Rabbani GH, Teka T, Saha SK, Zaman B, Majid N, Khatun M, et al Green banana and pectin improve small intestinal permeability and reduce fluid loss in Bangladeshi children with persistent diarrhea. Dig Dis Sci 2004; 49: 475–84. [DOI] [PubMed] [Google Scholar]
- 40. Allen SJ, Okoko B, Martinez E, Gregorio G, Dans LF. Probiotics for treating infectious diarrhoea. Cochrane Database Syst Rev 2004; CD003048. [DOI] [PubMed] [Google Scholar]
- 41. Szajewska H, Mrukowicz JZ. Probiotics in the treatment and prevention of acute infectious diarrhea in infants and children: a systematic review of published randomized, double‐blind, placebo‐controlled trials. J Pediatr Gastroenterol Nutr 2001; 33(Suppl 2): S17–S25. [DOI] [PubMed] [Google Scholar]
- 42. Van Niel CW, Feudtner C, Garrison MM, Christakis DA. Lactobacillus therapy for acute infectious diarrhea in children: a meta‐analysis. Pediatrics 2002; 109: 678–84. [DOI] [PubMed] [Google Scholar]
- 43. Costa‐Ribeiro H, Ribeiro TC, Mattos AP, Valois SS, Neri DA, Almeida P, et al Limitations of probiotic therapy in acute, severe dehydrating diarrhea. J Pediatr Gastroenterol Nutr 2003; 36: 112–15. [DOI] [PubMed] [Google Scholar]
- 44. Villarruel G, Rubio DM, Lopez F, Cintioni J, Gurevech R, Romero G, et al Saccharomyces boulardii in acute childhood diarrhoea: a randomized, placebo‐controlled study. Acta Paediatr 2007; 96: 538–41. [DOI] [PubMed] [Google Scholar]
- 45. Walker‐Smith JA, Sandhu BK, Isolauri E, Banchini G, Van Caillie‐Bertrand M, Dias JA, et al Guidelines prepared by the ESPGAN Working Group on Acute Diarrhoea. Recommendations for feeding in childhood gastroenteritis. J Pediatr Gastroenterol Nutr 1997; 24: 619–20. [DOI] [PubMed] [Google Scholar]
- 46. Szajewska H, Hoekstra JH, Sandhu B. On behalf of The Working Group on acute Diarrhoea of the European Society for Paediatric gastroenterology, hepatology, and nutrition. J Pediatr Gastroenterol Nutr 2000; 30: 522–7. [DOI] [PubMed] [Google Scholar]
- 47. Matheson AJ, Noble S. Racecadotril. Drugs 2000; 59: 829–37. [DOI] [PubMed] [Google Scholar]
- 48. Schwartz JC. Racecadotril: a new approach to the treatment of diarrhoea. Int J Antimicrob Agents 2000; 14: 75–9. [DOI] [PubMed] [Google Scholar]
- 49. Maldonado J. New perspectives on acute diarrhea in the breastfed infant: racecadotril. Ars Pharm 2006; 47: 251–63. [Google Scholar]
- 50. Turck D, Berard H, Fretault N, Lecomte JM. Comparison of racecadotril and loperamide in children with acute diarrhoea. Aliment Pharmacol Ther 1999; 13(Suppl 6): 27–32. [DOI] [PubMed] [Google Scholar]
- 51. Salazar‐Lindo E, Santisteban‐Ponce J, Chea‐Woo E, Gutierrez M. Racecadotril in the treatment of acute watery diarrhea in children. N Engl J Med 2000; 343: 463–7. [DOI] [PubMed] [Google Scholar]
- 52. Cézard JP, Duhamel JF, Meyer M, Pharaon I, Bellaiche M, Maurage C, et al Efficacy and tolerability of racecadotril in acute diarrhea in children. Gastroenterology 2001; 120: 799–805. [DOI] [PubMed] [Google Scholar]
- 53. Cojocaru B, Bocquet N, Timsit S, Wille C, Boursiquot C, Marcombes F, et al Effect of racecadotril in the management of acute diarrhea in infants and children. Arch Pediatr 2002; 9: 774–9. [DOI] [PubMed] [Google Scholar]
- 54. Szajewska H, Ruszczyński M, Chmielewska A, Wieczorek J. Systematic review: racecadotril in the treatment of acute diarrhoea in children. Aliment Pharmacol Ther 2007; 26: 807–13. [DOI] [PubMed] [Google Scholar]
- 55. World Health Organization . The rational use of drugs in the management of acute diarrhoea in children. Geneva , Switzerland : World Health Organization; 1990. [Google Scholar]


