Abstract
The novel coronavirus pneumonia, namely COVID-19, has become a global public health problem. Previous studies have found that air pollution is a risk factor for respiratory infection by carrying microorganisms and affecting body's immunity. This study aimed to explore the relationship between ambient air pollutants and the infection caused by the novel coronavirus. Daily confirmed cases, air pollution concentration and meteorological variables in 120 cities were obtained from January 23, 2020 to February 29, 2020 in China. We applied a generalized additive model to investigate the associations of six air pollutants (PM2.5, PM10, SO2, CO, NO2 and O3) with COVID-19 confirmed cases. We observed significantly positive associations of PM2.5, PM10, NO2 and O3 in the last two weeks with newly COVID-19 confirmed cases. A 10-μg/m3 increase (lag0–14) in PM2.5, PM10, NO2, and O3 was associated with a 2.24% (95% CI: 1.02 to 3.46), 1.76% (95% CI: 0.89 to 2.63), 6.94% (95% CI: 2.38 to 11.51), and 4.76% (95% CI: 1.99 to 7.52) increase in the daily counts of confirmed cases, respectively. However, a 10-μg/m3 increase (lag0–14) in SO2 was associated with a 7.79% decrease (95% CI: −14.57 to −1.01) in COVID-19 confirmed cases. Our results indicate that there is a significant relationship between air pollution and COVID-19 infection, which could partially explain the effect of national lockdown and provide implications for the control and prevention of this novel disease.
Keywords: Air pollution, Novel coronavirus pneumonia, COVID-19, Generalized additive model
Graphical abstract
Highlights
-
•
There was a significant relationship between air pollution and COVID-19 infection after controlling for confounding factors.
-
•
Positive associations of PM2.5, PM10, CO, NO2 and O3 with COVID-19 confirmed cases were observed.
-
•
However, SO2 was negatively associated with the number of daily COVID-19 confirmed cases.
1. Introduction
A novel coronavirus disease, namely COVID-19, was first detected in Wuhan city, China in December 2019 (Lu et al., 2020; Xu et al., 2020). In subsequent months, it spread rapidly to the rest of China, which has later become a global public health problem (Chen et al., 2020a; Gilbert et al., 2020; Sohrabi et al., 2020). COVID-19 is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Dong et al., 2020; Sohrabi et al., 2020; Zhou et al., 2020). Generally, most SARS-CoV-2 infected patients have mild symptoms including fever, dry cough, and sore throat (Huang et al., 2020; Sohrabi et al., 2020). However, some patients could have severe and even fatal complications such as Acute Respiratory Distress Syndrome (ARDS) (Chen et al., 2020b; Sohrabi et al., 2020).
To control the spread of COVID-19, various studies have been conducted to explore important factors affecting the transmission of SARS-CoV-2. Several early studies have demonstrated that human-to-human contact could increase the risk of COVID-19 infection (Chan et al., 2020; Li et al., 2020; Wang et al., 2020). Besides, population mobility has a significant effect on the COVID-19 epidemic (Kraemer et al., 2020). In addition, a recent study has shown an association of ambient temperature with the infection of COVID-19 (Xie and Zhu 2020). However, the impact of short-term exposure to air pollution lacks careful consideration.
Previous studies have suggested that ambient air pollutants are risk factors for respiratory infection by carrying microorganisms to make pathogens more invasive to humans and affecting body's immunity to make people more susceptible to pathogens (Becker and Soukup, 1999; Cai et al., 2007; Horne et al., 2018; Xie et al., 2019; Xu et al., 2016). Since COVID-19 is a respiratory disease and SARS-CoV-2 could remain viable in aerosols for hours (van Doremalen et al., 2020), it is interesting to investigate the effect of air pollution on COVID-19 infection. To provide useful implications for the control and prevention of this novel coronavirus disease, we aimed to explore the relationship between concentrations of six air pollutants and daily confirmed COVID-19 cases in 120 cities in China.
2. Materials and methods
2.1. Study area
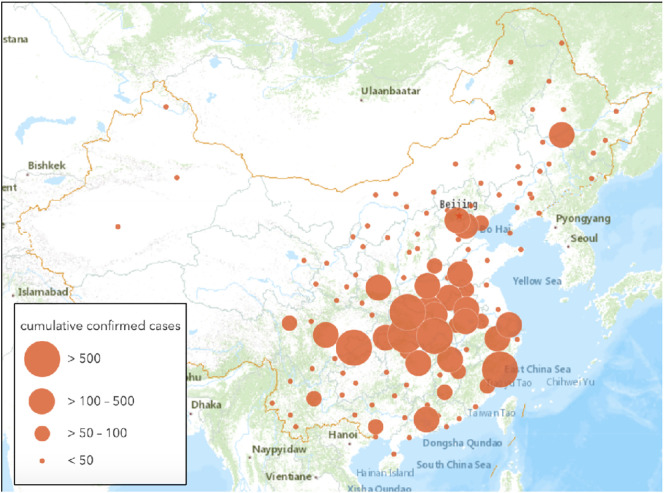
This study included 120 cities (4 municipalities and 116 prefecture-level cities) in the geographic regions of 83.4° to 131.6° east longitude and 20.0° to 51.4° north latitude (Fig. 1 ). According to the National Health Commission, 79,968 COVID-19 confirmed cases have been identified in the whole of China as of February 29, 2020. Our studied cities covered 70% of confirmed cases. We focused our analysis on these 120 cities because of the limitation of the meteorological data and the air pollution data we have obtained.
Fig. 1.
Locations of 120 cities and cumulative COVID-19 confirmed cases in each city as of February 29, 2020.
2.2. Data collection
Daily confirmed new cases for each city between January 23, 2020 and February 29, 2020 were obtained from the reports released by local health commissions on the official websites. We set January 23, 2020 (i.e., the date of lockdown in Wuhan) as the starting point of our study period to minimize the potential inclusion of imported cases from Wuhan.
Air pollution data were collected from an online platform (https://www.aqistudy.cn) monitoring and analyzing the air quality. Daily concentrations of six air pollutants were measured, including particles with diameters ≤2.5 μm (PM2.5), particles with diameters ≤10 μm (PM10), sulfur dioxide (SO2), carbon monoxide (CO), nitrogen dioxide (NO2), and ozone (O3).
Meteorological data on daily mean temperature, relative humidity, air pressure, and wind speed during the study period were obtained from the National Meteorological Information Center (http://data.cma.cn).
2.3. Statistical analysis
The generalized additive model (GAM) is a useful method to examine the effects of meteorological factors and air pollution on health outcomes (Lin et al., 2018; Ma et al., 2020; Peng et al., 2006; Talmoudi et al., 2017; Yang et al., 2020). As demonstrated by previous studies, the effect of air pollution can last for several days (Lin et al., 2018; Myung et al., 2019; Xie et al., 2019; Yang et al., 2020). In addition, an incubation period of 1 to 14 days for COVID-19 was reported by the National Health Commission in China. So, it is a reasonable choice to apply a moving-average approach to capture the cumulative lag effect of ambient air pollution (Duan et al., 2019; Li et al., 2018; Yang et al., 2020). Thus, in this study, we used the GAM with a Gaussian distribution family to estimate the associations between the moving average concentrations of air pollutants (lag0–7, lag0–14, lag0–21) and daily COVID-19 confirmed cases (Hastie, 2017; Liu et al., 2020). Specifically, we examined the effects of six air pollutants in six separate models (i.e., single-pollutant models) to reduce the collinearity since some of these pollutants were highly correlated (Chen et al. 2018; Dastoorpoor et al., 2019; Phosri et al., 2019). The basic model was defined as follows:
Here, log(y it) indicates the log-transformed COVID-19 counts reported on day t in city i (added 1 to avoid taking the logarithm of 0) (Liu et al., 2020; Xie and Zhu, 2020). a is the intercept. Z il denotes the linear term of (l + 1)-day moving average concentration of air pollutant (lag0-l) in city i (Chen et al. 2018; Phosri et al., 2019). Meteorological factors during the same period were controlled for the possible confounding effect, including mean temperature (tem il), relative humidity (rhu il), air pressure (prs il) and wind speed (win il). s(∙) is the smooth function (thin plate spline function with the maximum 3 degrees of freedom) of a certain meteorological factor (Liu et al., 2020; Wang et al., 2018; Xie and Zhu, 2020). log(y i, t−1) indicates the log-transformed COVID-19 counts reported on day t-1 in city i to account for the potential serial correlation in our data (Liu et al., 2020). In addition, we included city fixed effects (city i) to control for time-invariant city characteristics such as population size and density, and we also included day fixed effects (day t) to control for unobserved factors affecting all cities in each day such as national lockdown (Amuakwa-Mensah et al., 2017; Lu and Lu, 2017).
Two sensitivity analyses were conducted. First, since the number of confirmed cases in Wuhan city (the worst-hit region in China) was much larger than that in other cities, we excluded Wuhan from our data to test the robustness of our findings. Second, we applied two-pollutant models to examine whether the significant results from single-pollutant models were robust after controlling for other pollutants in the basic model (Chen et al. 2018; Phosri et al., 2019).
All analyses in this study were conducted using the “mgcv” package (version 1.8–28) in R statistical software (version 3.5.2). The statistical tests were two-sided, and p < 0.05 was considered statistically significant. Effect estimates were showed as percentage change (%) in daily COVID-19 confirmed cases per unit increase in pollutant concentration (i.e., 10 μg/m3 increase in PM2.5, PM10, SO2, NO2, O3 or 1 mg/m3 increase in CO).
3. Results
3.1. Descriptive analysis
Table 1 shows the statistics for daily COVID-19 confirmed cases, concentration of air pollution, and meteorological variables. During the observation period, this study included over 58,000 cases with an average of 12.94. Average daily concentrations of PM2.5, PM10, SO2, CO, NO2 and O3 were 46.43 μg/m3, 62.97 μg/m3, 12.23 μg/m3, 0.85 mg/m3, 19.28 μg/m3 and 78.22 μg/m3, respectively. The average of daily mean temperature, relative humidity, air pressure and wind speed were 2.82 °C, 67.25%, 964.08 hPa and 2.11 m/s, respectively.
Table 1.
Descriptive statistics of daily confirmed new cases, concentration of air pollution, and meteorological variables across all cities and days.
| Mean (SD) | Min | Max | |
|---|---|---|---|
| Daily confirmed cases | 12.94 (228.96) | 0 | 13,436 |
| PM2.5 (μg/m3) | 46.43 (38.55) | 2 | 554 |
| PM10 (μg/m3) | 62.97 (49.76) | 4 | 632 |
| SO2 (μg/m3) | 12.23 (9.90) | 2 | 87 |
| CO (mg/m3) | 0.85 (0.47) | 0.1 | 7.4 |
| NO2 (μg/m3) | 19.28 (11.87) | 2 | 86 |
| O3 (μg/m3) | 78.22 (20.58) | 11 | 152 |
| Mean temperature (°C) | 2.82 (10.11) | −33.8 | 26.5 |
| Relative humidity (%) | 67.25 (17.42) | 17 | 100 |
| Air pressure (hPa) | 964.08 (76.15) | 668.1 | 1039 |
| Wind speed (m/s) | 2.11 (1.19) | 0 | 15.4 |
Table 2 presents the spearman correlation coefficients between air pollutants and meteorological variables. Air pollutants had significant correlations with each other and all of them were correlated with mean temperature and relative humidity. SO2, CO and O3 were negatively correlated with air pressure, while PM2.5 and NO2 had positive correlations with air pressure. All of these air pollutants were significantly correlated with wind speed except for SO2.
Table 2.
Spearman correlation coefficients between air pollutants and meteorological variables across all cities and days.
| PM2.5 | PM10 | SO2 | CO | NO2 | O3 | Mean temperature | Relative humidity | Air pressure | Wind speed | |
|---|---|---|---|---|---|---|---|---|---|---|
| PM2.5 | 1.00 | |||||||||
| PM10 | 0.91⁎ | 1.00 | ||||||||
| SO2 | 0.37⁎ | 0.45⁎ | 1.00 | |||||||
| CO | 0.69⁎ | 0.62⁎ | 0.39⁎ | 1.00 | ||||||
| NO2 | 0.64⁎ | 0.65⁎ | 0.52⁎ | 0.63⁎ | 1.00 | |||||
| O3 | 0.13⁎ | 0.19⁎ | 0.11⁎ | −0.04⁎ | 0.08⁎ | 1.00 | ||||
| Mean temperature | −0.13⁎ | −0.17⁎ | −0.52⁎ | −0.09⁎ | −0.18⁎ | 0.08⁎ | 1.00 | |||
| Relative humidity | 0.08⁎ | −0.08⁎ | −0.41⁎ | 0.12⁎ | −0.07⁎ | −0.40⁎ | 0.34⁎ | 1.00 | ||
| Air pressure | 0.07⁎ | 0.02 | −0.21⁎ | −0.04⁎ | 0.04⁎ | −0.04⁎ | 0.15⁎ | 0.27⁎ | 1.00 | |
| Wind speed | −0.21⁎ | −0.13⁎ | −0.03 | −0.22⁎ | −0.22⁎ | 0.04⁎ | −0.07⁎ | −0.13⁎ | 0.12⁎ | 1.00 |
p < 0.05.
3.2. Relationship between air pollution and COVID-19 confirmed cases
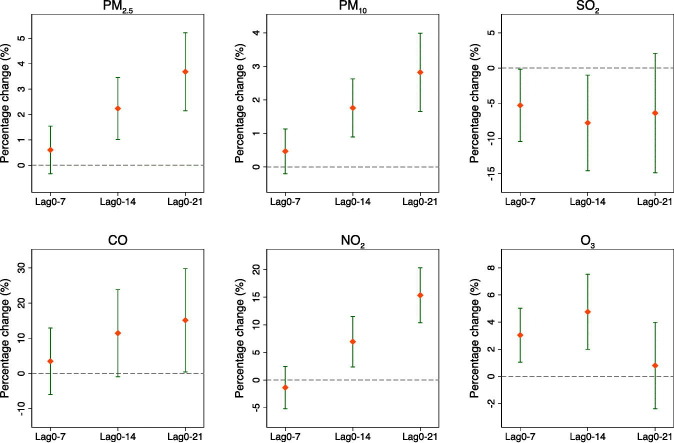
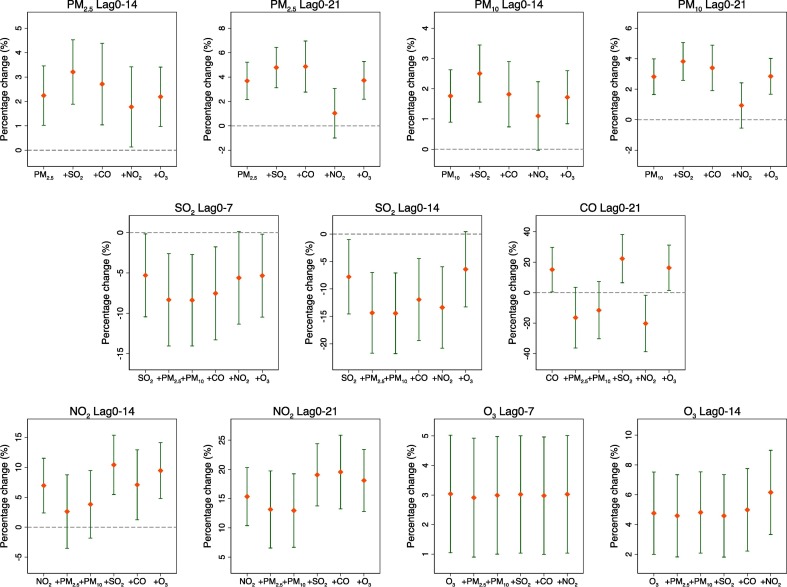
Fig. 2 plots the moving average lag effects (lag0–7, lag0–14, lag0–21) of different air pollutants on daily confirmed cases of COVID-19 in single-pollutant models. We observed significantly positive associations of PM2.5, PM10, CO, NO2 and O3 with COVID-19 confirmed cases. For example, a 10-μg/m3 increase (lag0–14) in PM2.5, PM10, NO2, O3 and 1-mg/m3 increase in CO (lag0–21) was associated with a 2.24% (95% CI: 1.02 to 3.46), 1.76% (95% CI: 0.89 to 2.63), 6.94% (95% CI: 2.38 to 11.51), 4.76% (95% CI: 1.99 to 7.52) and 15.11% (95% CI: 0.44 to 29.77) increase in the daily counts of COVID-19 confirmed cases, respectively. However, SO2 was negatively associated with COVID-19 confirmed cases at lag0–7 (percentage change = −5.30%, 95% CI: −10.44 to −0.16) and lag0–14 (percentage change = −7.79%, 95% CI: −14.57 to −1.01).
Fig. 2.
Percentage change (%) and 95% CI of daily COVID-19 confirmed cases associated with a unit increase in pollutant concentration using single-pollutant models. Units are 10 μg/m3 increase in PM2.5, PM10, SO2, NO2, O3 and 1 mg/m3 in CO.
3.3. Sensitivity analysis
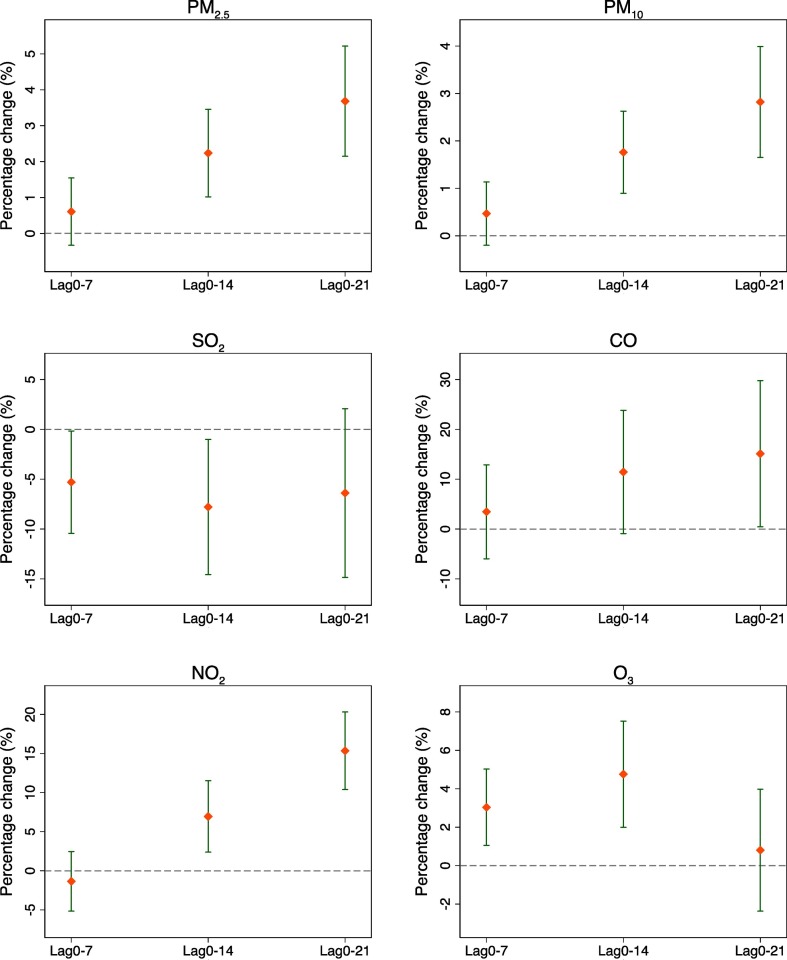
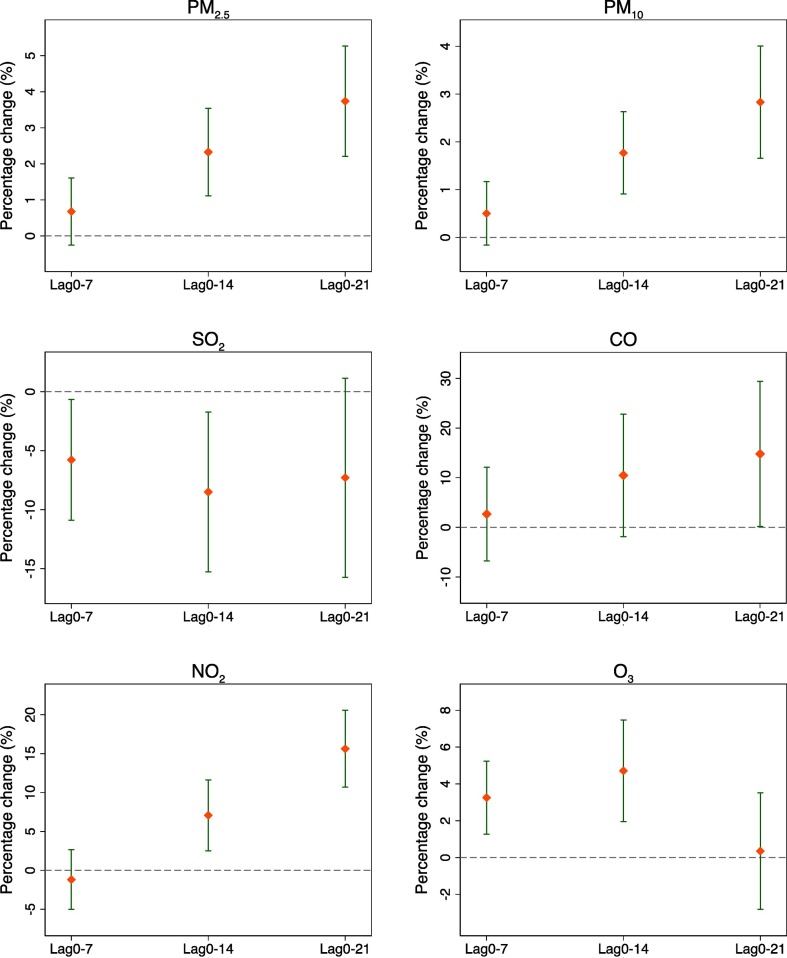
In the first sensitivity analysis, the relationship between COVID-19 confirmed cases and air pollution was robust after excluding Wuhan from our data (Fig. 3 ). Fig. 4 shows the results of two-pollutant models. For PM2.5 and PM10, the effects on COVID-19 confirmed cases became insignificant only when controlling for NO2. For SO2, the association could not remain significant after adding NO2 or O3 into the model. For CO, its effect was robust only when SO2 or O3 was included in the model. For NO2, the effect estimate did not alter much after the inclusion of SO2, CO or O3. The association of O3 with daily confirmed cases of COVID-19 remained robust after adjustment for other air pollutants.
Fig. 3.
Percentage change (%) and 95% CI of daily COVID-19 confirmed cases associated with a unit increase in pollutant concentration using single-pollutant models after excluding Wuhan. Units are 10 μg/m3 increase in PM2.5, PM10, SO2, NO2, O3 and 1 mg/m3 in CO.
Fig. 4.
Percentage change (%) and 95% CI of daily COVID-19 confirmed cases associated with a unit increase in pollutant concentration using single and two-pollutant models. Units are 10 μg/m3 increase in PM2.5, PM10, SO2, NO2, O3 and 1 mg/m3 in CO.
4. Discussion
In this paper, we used a generalized additive model to explore the relationship between ambient air pollutants and daily COVID-19 confirmed cases. We found significantly positive associations of PM2.5, PM10, CO, NO2 and O3 with COVID-19 confirmed cases, while SO2 was negatively associated with the number of daily confirmed cases. These findings could provide evidence that air pollution is an important factor in COVID-19 infection.
As demonstrated by previous literature, air pollution is also closely related to respiratory infection caused by other microorganisms (Chauhan and Johnston, 2003; Ciencewicki and Jaspers, 2007; Mehta et al., 2013). So, we compared our main findings with previous studies to find similarities and differences. Horne et al. (2018) reported that short-term exposure to higher PM2.5 was associated with more healthcare encounters for acute lower respiratory infection by a case-crossover design. Xie et al. (2019) also found a significant association of atmospheric particulate matter (PM2.5 and PM10,) and hospitalizations for respiratory disease using a distributed lag nonlinear model. A time-series analysis conducted in Thailand observed that PM10, SO2, CO, NO2 and O3 were significantly related to increased risk of respiratory hospital admissions (Phosri et al., 2019). A literature review also showed that exposure to SO2, CO and NO2 was harmful to our health and increased the risk of respiratory disease (Chen et al., 2007). Overall, all of the six air pollutants could be risk factors in respiratory infection. However, our results are different from previous studies since we observed a negative relationship between SO2 and COVID-19 confirmed cases. The virucidal property of SO2 may be a possible reason (Berendt et al., 1971, Berendt et al., 1972), and additional research is needed to determine the biological mechanisms behind this phenomenon.
Our study has some implications for the control and prevention of COVID-19. First, governments and the public should pay more attention to regions with high concentrations of PM2.5, PM10, CO, NO2 and O3, since these regions may suffer more serious COVID-19 epidemic. In other words, reducing air pollutants (not include SO2) could be a useful way to control COVID-19 infection. Additionally, it is noteworthy that SO2 has a negative association with COVID-19 confirmed cases, and further laboratory research needs to be conducted to elucidate the underlying mechanism.
Our study has several limitations. First, we only focused on the association between air pollutants and COVID-19 confirmed cases and not the causal effect of air pollution on COVID-19 infection. Second, our data did not include gender- or age-specific confirmed cases, so we could not conduct subgroup analyses. Third, our findings were not globally representative since cities of other countries were not included in this study. Future studies are needed to overcome these limitations.
5. Conclusion
Our study suggests that there is a statistically significant relationship between air pollution and COVID-19 infection. Short-term exposure to higher concentrations of PM2.5, PM10, CO, NO2 and O3 is associated with an increased risk of COVID-19 infection. However, short-term exposure to a higher concentration of SO2 is related to the decreased risk of COVID-19 infection. Further laboratory studies are needed to explore the underlying mechanisms.
CRediT authorship contribution statement
Yongjian Zhu: Data curation, Writing - original draft, Visualization, Investigation. Jingui Xie: Conceptualization, Methodology, Supervision. Fengming Huang: Validation, Investigation. Liqing Cao: Validation, Writing - review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This research was supported by the National Natural Science Foundation of China (grant no. 71571176).
Editor: Jianmin Chen
References
- Amuakwa-Mensah F., Marbuah G., Mubanga M. Climate variability and infectious diseases nexus: evidence from Sweden. Infect. Dis. Model. 2017;2:203–217. doi: 10.1016/j.idm.2017.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker S., Soukup J.M. Exposure to urban air particulates alters the macrophage-mediated inflammatory response to respiratory viral infection. J. Toxicol. Environ. Health Part A. 1999;57:445–457. doi: 10.1080/009841099157539. [DOI] [PubMed] [Google Scholar]
- Berendt R.F., Dorsey E.L., Hearn H.J. Virucidal properties of light and SO2 II. Effect of a low gas concentration on aerosolized virus. Proc. Soc. Exp. Biol. Med. 1971;138:1005–1008. doi: 10.3181/00379727-138-36038. [DOI] [PubMed] [Google Scholar]
- Berendt R.F., Dorsey E.L., Hearn H.J. Virucidal properties of light and SO2 I. Effect on aerosolized Venezuelan equine encephalomyelitis virus. Proc. Soc. Exp. Biol. Med. 1972;139:1–5. doi: 10.3181/00379727-139-36063. [DOI] [PubMed] [Google Scholar]
- Cai Q.-C., Lu J., Xu Q.-F., Guo Q., Xu D.-Z., Sun Q.-W., Yang H., Zhao G.-M., Jiang Q.-W. Influence of meteorological factors and air pollution on the outbreak of severe acute respiratory syndrome. Public Health. 2007;121:258–265. doi: 10.1016/j.puhe.2006.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan, J.F.-W., Yuan, S., Kok, K.-H., To, K.K.-W., Chu, H., Yang, J., Xing, F., Liu, J., Yip, C.C.-Y., Poon, R.W.-S., 2020. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 395, 514-523. 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed]
- Chauhan A.J., Johnston S.L. Air pollution and infection in respiratory illness. Br. Med. Bull. 2003;68:95–112. doi: 10.1093/bmb/ldg022. [DOI] [PubMed] [Google Scholar]
- Chen T.-M., Kuschner W.G., Gokhale J., Shofer S. Outdoor air pollution: nitrogen dioxide, sulfur dioxide, and carbon monoxide health effects. Am J Med Sci. 2007;333:249–256. doi: 10.1097/MAJ.0b013e31803b900f. [DOI] [PubMed] [Google Scholar]
- Chen C., Liu C., Chen R., Wang W., Li W., Kan H., Fu C. Ambient air pollution and daily hospital admissions for mental disorders in Shanghai. China. Sci. Total Environ. 2018;613:324–330. doi: 10.1016/j.scitotenv.2017.09.098. [DOI] [PubMed] [Google Scholar]
- Chen H., Guo J., Wang C., Luo F., Yu X., Zhang W., Li J., Zhao D., Xu D., Gong Q. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395:809–815. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., Qiu Y., Wang J., Liu Y., Wei Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciencewicki J., Jaspers I. Air pollution and respiratory viral infection. Inhal. Toxicol. 2007;19:1135–1146. doi: 10.1080/08958370701665434. [DOI] [PubMed] [Google Scholar]
- Dastoorpoor M., Sekhavatpour Z., Masoumi K., Mohammadi M.J., Aghababaeian H., Khanjani N., Hashemzadeh B., Vahedian M. Air pollution and hospital admissions for cardiovascular diseases in Ahvaz. Iran. Sci. Total Environ. 2019;652:1318–1330. doi: 10.1016/j.scitotenv.2018.10.285. [DOI] [PubMed] [Google Scholar]
- Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan Y., Liao Y., Li H., Yan S., Zhao Z., Yu S., Fu Y., Wang Z., Yin P., Cheng J. Effect of changes in season and temperature on cardiovascular mortality associated with nitrogen dioxide air pollution in Shenzhen. China. Sci. Total Environ. 2019;697:134051. doi: 10.1016/j.scitotenv.2019.134051. [DOI] [PubMed] [Google Scholar]
- Gilbert M., Pullano G., Pinotti F., Valdano E., Poletto C., Boëlle P.-Y., d'Ortenzio E., Yazdanpanah Y., Eholie S.P., Altmann M. Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study. Lancet. 2020;395:871–877. doi: 10.1016/S0140-6736(20)30411-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hastie T.J. Routledge; 2017. Generalized Additive Models, Statistical Models in S; pp. 249–307. [Google Scholar]
- Horne B.D., Joy E.A., Hofmann M.G., Gesteland P.H., Cannon J.B., Lefler J.S., Blagev D.P., Korgenski E.K., Torosyan N., Hansen G.I. Short-term elevation of fine particulate matter air pollution and acute lower respiratory infection. Am. J. Respir. Crit. Care Med. 2018;198:759–766. doi: 10.1164/rccm.201709-1883OC. [DOI] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer M.U., Yang C.-H., Gutierrez B., Wu C.-H., Klein B., Pigott D.M., du Plessis L., Faria N.R., Li R., Hanage W.P. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020 doi: 10.1126/science.abb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Wang X.-L., Zheng X. Impact of weather factors on influenza hospitalization across different age groups in subtropical Hong Kong. Int. J. Biometeorol. 2018;62:1615–1624. doi: 10.1007/s00484-018-1561-z. [DOI] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Ren R., Leung K.S., Lau E.H., Wong J.Y. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. New Engl. J. Med. 2020 doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin H., Tao J., Kan H., Qian Z., Chen A., Du Y., Liu T., Zhang Y., Qi Y., Ye J. Ambient particulate matter air pollution associated with acute respiratory distress syndrome in Guangzhou, China. J. Expo. Sci. Environ. Epidemiol. 2018;28:392. doi: 10.1038/s41370-018-0034-0. [DOI] [PubMed] [Google Scholar]
- Liu K., Hou X., Ren Z., Lowe R., Wang Y., Li R., Liu X., Sun J., Lu L., Song X. Climate factors and the East Asian summer monsoon may drive large outbreaks of dengue in China. Environ. Res. 2020;109190 doi: 10.1016/j.envres.2020.109190. [DOI] [PubMed] [Google Scholar]
- Lu S.F., Lu L.X. Do mandatory overtime laws improve quality? Staffing decisions and operational flexibility of nursing homes. Manag. Sci. 2017;63:3566–3585. doi: 10.1287/mnsc.2016.2523. [DOI] [Google Scholar]
- Lu H., Stratton C.W., Tang Y.W. Outbreak of pneumonia of unknown etiology in Wuhan China: the Mystery and the Miracle. J. Med. Virol. 2020 doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y., Zhao Y., Liu J., He X., Wang B., Fu S., Yan J., Niu J., Zhou J., Luo B. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan. China. Sci. Total Environ. 2020;138226 doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta S., Shin H., Burnett R., North T., Cohen A.J. Ambient particulate air pollution and acute lower respiratory infections: a systematic review and implications for estimating the global burden of disease. Air Qual. Atmos. Health. 2013;6:69–83. doi: 10.1007/s11869-011-0146-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myung W., Lee H., Kim H. Short-term air pollution exposure and emergency department visits for amyotrophic lateral sclerosis: a time-stratified case-crossover analysis. Environ. Int. 2019;123:467–475. doi: 10.1016/j.envint.2018.12.042. [DOI] [PubMed] [Google Scholar]
- Peng R.D., Dominici F., Louis T.A. Model choice in time series studies of air pollution and mortality. J. Roy. Stat. Soc. Ser. A. (Stat. Soc.) 2006;169:179–203. doi: 10.1111/j.1467-985X.2006.00410.x. [DOI] [Google Scholar]
- Phosri A., Ueda K., Phung V.L.H., Tawatsupa B., Honda A., Takano H. Effects of ambient air pollution on daily hospital admissions for respiratory and cardiovascular diseases in Bangkok, Thailand. Sci. Total Environ. 2019;651:1144–1153. doi: 10.1016/j.scitotenv.2018.09.183. [DOI] [PubMed] [Google Scholar]
- Sohrabi C., Alsafi Z., O’Neill N., Khan M., Kerwan A., Al-Jabir A., Iosifidis C., Agha R. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int. J. Surg. 2020 doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talmoudi K., Bellali H., Ben-Alaya N., Saez M., Malouche D., Chahed M.K. Modeling zoonotic cutaneous leishmaniasis incidence in central Tunisia from 2009-2015: forecasting models using climate variables as predictors. PLoS Negl. Trop. Dis. 2017;11 doi: 10.1371/journal.pntd.0005844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., Tamin A., Harcourt J.L., Thornburg N.J., Gerber S.I. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. New Engl. J. Med. 2020 doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang P., Goggins W.B., Chan E.Y. A time-series study of the association of rainfall, relative humidity and ambient temperature with hospitalizations for rotavirus and norovirus infection among children in Hong Kong. Sci. Total Environ. 2018;643:414–422. doi: 10.1016/j.scitotenv.2018.06.189. https://doi.org/10.1016/j.scitotenv.2018.06.189. [DOI] [PubMed] [Google Scholar]
- Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., Wang B., Xiang H., Cheng Z., Xiong Y. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan. China. JAMA. 2020 doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J., Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020;138201 doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J., Teng J., Fan Y., Xie R., Shen A. The short-term effects of air pollutants on hospitalizations for respiratory disease in Hefei. China. Int. J. Biometeorol. 2019;63:315–326. doi: 10.1007/s00484-018-01665-y. [DOI] [PubMed] [Google Scholar]
- Xu Q., Li X., Wang S., Wang C., Huang F., Gao Q., Wu L., Tao L., Guo J., Wang W. Fine particulate air pollution and hospital emergency room visits for respiratory disease in urban areas in Beijing, China, in 2013. PLoS One. 2016;11 doi: 10.1371/journal.pone.0153099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C., Liu S., Zhao P., Liu H., Zhu L. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020 doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Z., Hao J., Huang S., Yang W., Zhu Z., Tian L., Lu Y., Xiang H., Liu S. Acute effects of air pollution on the incidence of hand, foot, and mouth disease in Wuhan. China. Atmos. Environ. 2020;225:117358. doi: 10.1016/j.atmosenv.2020.117358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., Xiang J., Wang Y., Song B., Gu X. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]