Supplemental Digital Content is available in the text.
Abstract
Background:
The treatment of breast ptosis and gland hypoplasia in a single surgery is a challenging procedure and the result is less predictable. In this surgery, the complications mainly concern the prosthesis, such as implant deflation, capsular contracture, palpability, or malposition. We, therefore, propose a different and new technique that avoids breast prosthesis, combining mastopexy and autologous augmentation with fat grafts.
Methods:
Combined mastopexy and autologous fat graft augmentation (lipopexy) was performed in women affected by breast ptosis and asymmetric breast or hypomastia. The breast lift technique was determined due to the ptosis level. The process of fat grafting was executed according to the PureGraft and, in some cases, to GID System, to Celution System or Carraway’s techniques.
Results:
Thirty-four patients affected by breast ptosis and hypomastia underwent lipopexy from January 2010 to May 2017. The mean volume of adipose tissue injected for each breast was 225.98 ml. After surgery, the patients were followed for an average of 22.8 months. A mild ptosis relapse with partial fat absorption was observed in 4 cases (11.76%) and the presence of oily cysts was diagnosed in 2 patients (5.88%). One severe complication was recorded (hematoma drainage). All the patients healed uneventfully in 2 weeks.
Conclusions:
This technique allows the surgeon to distribute the desired fat volume along the breasts, avoids implants, and displayed stable results. This treatment has been demonstrated not to interfere with follow-up breast imaging. We, therefore, consider lipopexy a valuable and safe alternative to mastopexy and mild to moderate breast volume augmentation.
INTRODUCTION
The combination of breast ptosis and gland hypoplasia or breast asymmetry is a common condition that often occurs after pregnancies, lactation, and weight fluctuations.1
Although several techniques have been described to effectively correct these situations individually, treatment in a single surgery remains challenging. In fact, several parameters should be considered and combined in the same procedure, such as the amount of lift and augmentation, breast size and shape, symmetry, and the nipple/areola size and position. Moreover, the surgeon should perform in a single surgery the whole procedure considering the modifications of the parameters, in order to produce a harmonic and stable result.2,3
Several techniques have been proposed to overcome these problems and standardize the results. These techniques include procedural algorithms,4,5 a combination of previously known techniques,6 or customized procedures.7
However, the combination of mastopexy and augmentation is more difficult and the result is less predictable. As reported by Spear,3 the combination of these 2 procedures into 1 surgery “makes the other more difficult.” The most important matter of concern is the implant position. In fact, the soft tissue dissection required for its placement and the stress produced by the added volume could lead to soft tissue complications such as loss of nipple, skin flaps, loss of sensation, implant exposure, or infection.3 Although the incidence of these complications in the combined procedure is low, the majority of complications are implant-related (eg, implant deflation, capsular contracture, palpability or malposition).8,9
We propose a different technique that overcomes these issues, combining mastopexy and autologous augmentation with fat grafts in the same procedure. Although several techniques of breast augmentation with autologous adipose grafts have been described,10–13 the literature about techniques that combine adipose grafting with mastopexy is lacking. In this article, we aim to evaluate the effectiveness of our technique and the stability of the results over time.
MATERIALS AND METHODS
Inclusion Criteria
The aim of lipopexy is to achieve a satisfactory breast augmentation and mastopexy during a single procedure. This objective is realistic when the following criteria are fulfilled:
Patient is a woman aged 18 years or older
Breast ptosis is graded according to Regnault’s classification15
Patient desires a mild to moderate cosmetic breast augmentation or has the need of a breast symmeterization.
General adiposity is reasonably compatible with the desired augmentation.
Data Collection
Combined simultaneous mastopexy and augmentation with autologous fat graft (lipopexy) were performed from January 2010 to May 2017 in women affected by breast ptosis and asymmetry, accompanied by hypoplasia in several cases. A detailed summary of cases is reported in Table 1. Age, BMI, grade of ptosis, amount of suctioned fat, and amount of adipose graft were recorded. A single senior surgeon performed all surgeries.
Table 1.
Individual Patient Parameters
| Age | BMI | Breast Ptosis Grade | Type of Mastopexy | Fat Tissue Harvested (ml) | Fat Tissue Transferred Right Breast (ml) | Fat Tissue Transferred Left Breast (ml) | Fat Refinement Technique | Complications | P.R. | |
|---|---|---|---|---|---|---|---|---|---|---|
| B.D.L | 48 | 25.71 | Severe | Anchor | 3,000 | 200 | 200 | Carraway | — | P.R. |
| A.E.M.S | 58 | 24.61 | Mild | Periareolar | 2,650 | 350 | 300 | PureGraft | — | — |
| A.A. | 62 | 21.3 | Mild | Periareolar | 1,900 | 135 | 135 | Carraway | — | — |
| G.R.S | 21 | 20.2 | Mild | Periareolar | 2,100 | 260 | 160 | Carraway | — | — |
| B.M. | 23 | 24.21 | Moderate | Periareolar | 2,650 | 510 | 330 | PureGraft | — | P.R. |
| Q.F. | 45 | 23.25 | Moderate | Periareolar | 4,500 | 330 | 380 | GID | — | — |
| D.A. | 57 | 21.09 | Mild | Vertical | 1,950 | 0 | 250 | GID | — | P.R. |
| C.P. | 34 | 18.75 | Moderate | Vertical | 1,100 | 150 | 175 | Carraway | — | — |
| R.A. | 44 | 18.21 | Mild | Vertical | 1,300 | 165 | 200 | Carraway | N.L. | — |
| R.M. | 37 | 20.2 | Moderate | Vertical | 2,500 | 280 | 50 | Carraway | N.L. | P.R. |
| C.L. | 37 | 20.06 | Moderate | Vertical | 1,800 | 140 | 230 | PureGraft | — | — |
| F.A. | 40 | 19.96 | Moderate | Vertical | 2,500 | 270 | 0 | PureGraft | — | — |
| P.C. | 31 | 23.71 | Moderate | Vertical | 3,900 | 220 | 300 | GID | — | — |
| G.M.A | 21 | 20.58 | Moderate | Vertical | 2,300 | 210 | 60 | GID | — | — |
| G.E. | 59 | 26.22 | Severe | Vertical | 2,600 | 290 | 150 | Carraway | N.L. | — |
| V.S. | 32 | 20.43 | Moderate | Vertical | 800 | 70 | 225 | Carraway | — | — |
| V.A.M. | 37 | 22.58 | Moderate | Vertical | 1,050 | 195 | 155 | PureGraft | H.E. | — |
| S.A. | 37 | 21.26 | Severe | Vertical | 3,550 | 0 | 250 | Carraway | — | — |
| C.C. | 49 | 23.88 | Mild | Vertical | 4,150 | 200 | 200 | Carraway | — | — |
| S.M. | 42 | 25.26 | Severe | Vertical | 4,600 | 300 | 100 | Carraway | — | — |
| O.A. | 20 | 17.9 | Moderate | Vertical | 1,800 | 180 | 150 | Celution | — | — |
| C.M.G. | 44 | 23.18 | Moderate | Vertical | 3,650 | 230 | 250 | Carraway | — | — |
| C.B. | 55 | 23.53 | Moderate | Vertical | 450 | 0 | 40 | Carraway | — | — |
| A.R. | 20 | 28.34 | Moderate | Vertical | 5,000 | 150 | 300 | GID | — | — |
| F.An. | 46 | 37.18 | Severe | Vertical | 3,800 | 240 | 100 | GID | — | — |
| B.Mi. | 33 | 25.15 | Moderate | Vertical | 2,000 | 230 | 90 | Celution | — | — |
| L.G.D. | 34 | 20.2 | Moderate | Vertical | 1,100 | 80 | 40 | PureGraft | — | — |
| S.F. | 40 | 22.65 | Moderate | Vertical | 1,770 | 278 | 260 | Celution | — | — |
| L.M. | 20 | 24.17 | Moderate | Anchor | 4,950 | 180 | 100 | Carraway | — | — |
| L.A. | 39 | 28.34 | Moderate | Periareolar | 5,000 | 425 | 315 | Celution | O.C. | — |
| P.S. | 39 | 24.84 | Moderate | Vertical | 1,600 | 210 | 290 | Carraway | — | — |
| D.S. | 38 | 21.26 | Mild | Periareolar | 2,700 | 325 | 405 | Celution | O.C. | — |
| C.M. | 37 | 27.4 | Mild | Periareolar | 4,540 | 365 | 315 | Celution | N.L. | — |
| C.Pa. | 40 | 25.32 | Mild | Periareolar | 2,500 | 440 | 350 | Celution | — | — |
P.R., protheses removed; H.E., hematoma evacuation; N.L., new lipofilling; O.C., oily cyst.
Technique
The patient is marked preoperatively in a standing position. The surgeon should mark the median line, suprasternal notch, inframammary folds, and midclavicular lines. The nipple-suprasternal notch distance and the nipple-inframammary fold distance are measured and recorded. The new location of the NAC is marked on the midclavicular line.17
We prefer a periareolar breast lift for mild ptosis. In case of moderate or severe breast ptosis and marked cutaneous laxity, a superior pedicle breast reduction is preferred. The markings should include the areas to fill with adipose tissue. In this context, the patient should express her desires concerning augmentation to identify and mark those areas that need more filling. The donor sites and the amount of adipose graft should be decided preoperatively and discussed with the patient.
We divide the procedure into 2 steps. During the first step, we harvest the adipose tissue. In this phase, the operatory field generally includes abdomen, flanks, and thighs. Other areas could be employed as an adipose tissue donor site if greater amounts are required. Finally, if the patient wishes to remove the excess of fat tissue of different specific regions, this could also be evaluated. In a second phase, the field is extended to the thorax and mastopexy is performed. Breast lift is performed according to a standard periareolar18 or superior pedicle mastopexy19 as above mentioned, with a vertical or an anchor scar design. The adipose tissue is grafted during the procedure, usually when the mastopexy of the breast is outlined.
Adipose Graft
In a first phase, the adipose tissue is harvested. During fat processing, the mastopexy is performed. When the shape of the breast is outlined, the adipose tissue is grafted. This occurs in the periareolar technique just before the securing of the NAC to the new level. In the superior pedicle mastopexy technique, the graft is performed before anchoring the gland to the pectoral fascia. The harvest and graft of the autologous fat tissue is described in the following paragraphs.
A tumescent solution of saline composed by 0.5% lidocaine and 1:200.000 epinephrine is infiltrated in the donor site with a Lamis infiltrator. Usually abdomen and thigh are preferred, although several donor sites could be employed. The adipose tissue is then harvested with a 3-mm blunt Mercedes cannula into 10-ml Luer-Lok syringes. In our experience, 70–500 ml are required for each breast. Usually the surgeon should consider harvesting at least 3 times the amount desired for grafting. When the required quantity of fat is harvested, the procedure may continue as a standard liposuction. The adipose graft refinement has been developed according to the PureGraft system in some cases and GID System, Celution System, or Carraway technique in the rest of them. The different techniques of fat refinement were related to the moment when the surgery were performed. We have been switching from one technique to another trying to reach the one with the best results in terms of fat reabsorption. With all of these techniques, in our hands, we were able to obtain a fat reabsorption rate of 30% or less. Before infiltration, a percutaneous release of soft tissues with an 18-G needle is performed in case of need to remove scar retractions (if any) and to create a proper chamber for fat grafting (Fig. 1). Alternatively, in cases of breast hypoplasia, the soft tissue release with an 18-G needle aims to expand the affected quadrants and to allow a harmonic breast augmentation. The processed adipose tissue is injected with the following proportions into 4 sites, in this order:
Fig. 1.

Percutaneous aponeurotomy with an 18G needle.
40% intramuscular (pectoralis major) (Fig. 2)
10% under the pectoralis fascia (Fig. 3)
50% subcutaneous (Fig. 4)
Fig. 2.
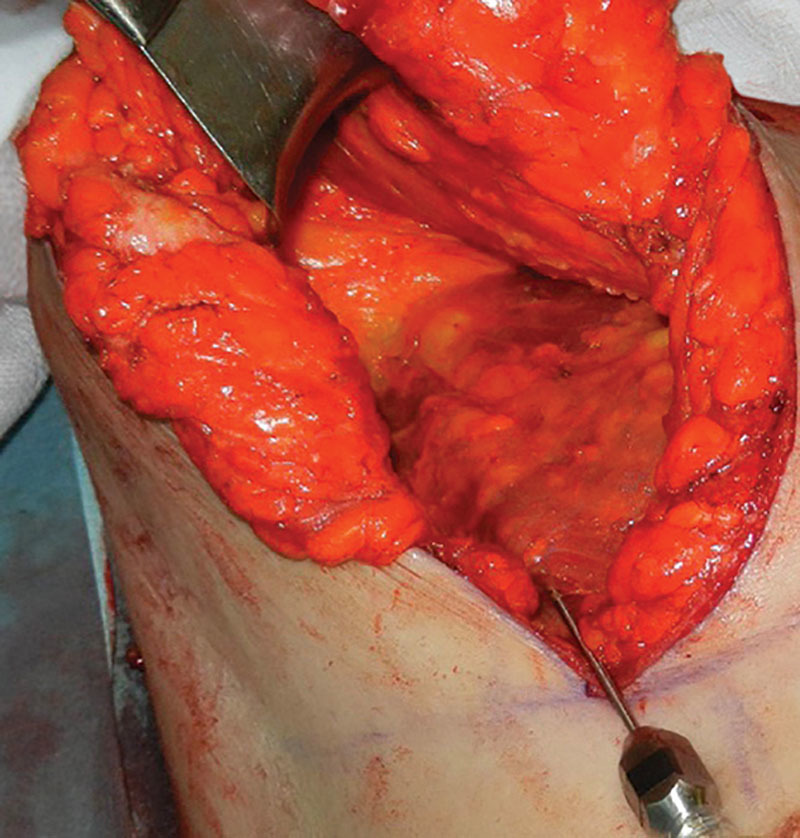
The adipose graft is placed under the pectoralis major and intramuscular.
Fig. 3.
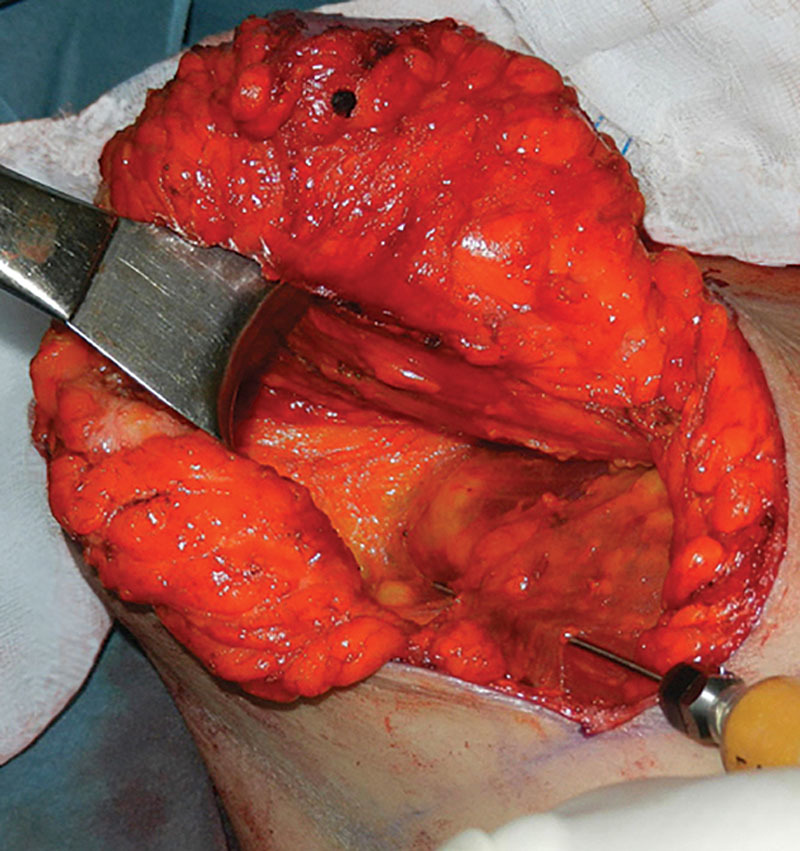
The graft is placed under the pectoralis major fascia.
Fig. 4.

The graft is placed in the subcutaneous tissue.
The distribution inside each breast should be performed according to the preoperative planning and patient desires. The distribution of the graft into 4 areas maximizes grafts take and produces a natural breast appearance.
Postoperative Clinical Evaluation
The evaluation of the graft take is still an open issue. Several studies show a variable graft take using subjective evaluations, ranging from 20% to 90%.25–30 Among objective measurements, CT is more precise in distinguishing fat density over MRI. However, in our case series, the adipose tissue is grafted in 4 different layers (subpectoral, intramuscular, subfascial, subcutaneous) and the objective measurement of the graft take is difficult even with CT. Therefore, a subjective analysis of the grafted fat was performed in all cases by the senior surgeon.
The following parameters were therefore evaluated:
Ptosis relapse. Any case affected by postoperative ptosis with >1 cm of cutaneous ptosis relapse and >2 cm of glandular ptosis relapse was recorded.
Any postoperative modifications of the breast shape were recorded.
Adipose graft stability and resorption. Resorption of the adipose graft was evaluated subjectively. Any case of incomplete take of the graft (approximately inferior to 70% of the injected volume) was recorded.
Stability of the correction of breast hypoplasia. The senior author performs the evaluation clinically. Any modification of the result in the postoperative is carefully recorded.
RESULTS
From January 2010 to May 2017, lipopexy was performed on 34 patients. The mean age of the case series is 39 years old (20–62) with a mean BMI of 23.26 (17.90–37.18). Lipopexy was secondary in 4 patients (12%) who previously underwent breast augmentation with implants. In those patients, the prostheses were totally removed and the breasts’ volume was maintained due to the fat grafting.
The periareolar technique was performed in 9 patients (26%) (Fig. 5), 23 patients (68%) underwent a breast lift with superior pedicle with vertical incision, and in 2 patients (5.88%) with severe breast ptosis and marked cutaneous laxity an anchor fashion scar was executed (See figure, Supplemental Digital Content 1, which displays a patient who underwent a liposuction of 2,500 ml from the peri-trochanteric, abdominal, flanks, and knees. Intraoperative and postoperative views are shown, http://links.lww.com/PRSGO/B255). (See figure, Supplemental Digital Content 2, which displays a patient who was affected by asymmetry and ptosis with left breast bigger and more ptotic than right breast, http://links.lww.com/PRSGO/B256).
Fig. 5.
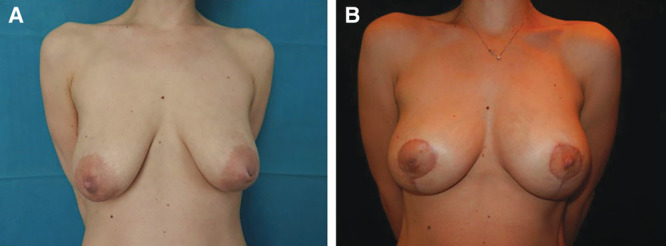
Asymmetric breast ptosis. A, S.V., 32-year-old patient, 20.4 BMI, affected by breast ptosis, volume asymmetry (greater volume on the right side) and bilateral inverted nipple. The sternal notch–right nipple measured 23.5 cm while the sternal notch–left nipple 22.5. The inframammary fold–nipple distance measured 7.5 cm on the right side and 7 cm on the left side. The patient underwent a liposuction of 800 ml from the peri-trochanteric area and lipopexy. A superior pedicle pexy was combined to a breast augmentation with fat graft (70 ml on the right side and 225 ml on the left side). The inverted nipple was corrected bilaterally. B, Postoperative result after 5 months.
The mean volume of adipose tissue harvested was 2,598 ml. After processing the fat, a mean volume of 225 ml (40–510 ml) was grafted on each breast. After surgery, the patients were followed for an average of 22.8 months (6–41).
The graft take was considered superior to 70% in all cases, according to the subjective evaluation of the senior author, based on clinical examination and photographs taken in a standardized manner. One major complication was recorded, an acute postoperative hematoma that needed to be drained in the operation room. All the patients healed uneventfully in 2 weeks. A cutaneous ptosis relapse (>1 cm of cutaneous ptosis relapse) and a partial fat reabsorption were observed in 4 cases (11%). Those complications were solved with another adipose graft under local anesthesia 6 months after the surgery. In 2 cases (5%), the presence of oily cysts was diagnosed using an ultrasonography device, and aspirated using an 18-G needle, with no signs of relapse in the follow-up.
DISCUSSION
The combination of augmentation and breast lift in a single procedure has widely been discussed. This surgery, formerly described by Gonzalez-Ulloa,26 was customized and modified by several authors.4,6,7,12
This kind of surgery raises 2 main difficulties:
The surgeon should manage and combine 2 distinct techniques into a single procedure, also combining a greater number of parameters and variables that could interfere with each other.
The implant stresses and compresses those soft tissues that are already kept under tension by the mastopexy. This could produce ischemic complications and raise the infection rate.
Our technique lets the surgeon perform the breast lift without introducing the variables related to the implant size. In fact, the adipose graft is performed along with mastopexy. Breast augmentation with fat graft is versatile, because the whole volume can be precisely distributed along the breasts, correcting even minimal preexisting or technique-related imperfections, fitting to each case. The fat graft is performed in 4 different layers: subpectoral, intramuscular, subfascial, and subcutaneous. The surgeon can thus adjust the fat distribution among and inside the 4 infiltration layers.
The aim of lipopexy is to correct the ptosis and achieve a satisfactory breast augmentation in one procedure. The latter often requires the employment of a silicone implant. However, several authors have recently described techniques for breast augmentation with autologous fat transfer. The limitations of these procedures concern the amount of fat graft that could be transferred to the breast to achieve a satisfactory augmentation. In fact, the adipocyte is able to survive in the first 2 days by imbibition from the surrounding tissues until new vascular connections are established.27 The graft of large quantities of adipose tissue could then produce large necrotic areas, cellulitis, cysts, and calcifications. Several solutions have been proposed to allow the graft of large quantities of adipose tissue to the breast. According to Serra-Renom,28 the graft could be divided in more surgeries. Khouri describes the preexpansion of the recipient site with the Brava technique and the uniform fat deposition in droplets (called “microribbons”).29,30
We propose instead the uniform deposition of adipose tissue in several layers (subpectoral, intramuscular, subfascial, subcutaneous). This procedure increases the graft take because it minimizes the accumulation of huge volumes of adipose tissue in a limited space and maximizes the interface with the recipient site and the vascularization of the graft.29,31 Our technique allows the surgeon to perform discrete augmentations (mean breast augmentation of 225 ml) in 1 surgical time without any treatment or pre-expansion of the breast.
Breast augmentation with fat grafting displays several early and late complications (eg infection, liponecrotic cysts, fat necrosis, and calcifications) and the results are less reproducible than those achieved with an implant. Nevertheless, the adipose graft, once taken, is virtually permanent, requires a less invasive procedure, and avoids the typical side effects of implants and foreign bodies (eg capsular contracture, rippling, rupture, displacement, extrusion, deformity).11,32
According to our experience, great volumes of adipose tissue may be grafted in a single surgery. Literature confirms higher fat survival when larger volumes are injected.33 In our case series, an average of 225 ml were injected for each breast. A good graft take was observed in all patients, with a stable result. The radiologic results of breast fat grafting have not been demonstrated to interfere with the mammographic follow-up. Fat grafting usually produces less benign microcalcifications than a common reduction mammoplasty.14 However, these alterations can be detected by follow-up imaging procedures.34 In our case series, we did not observe the occurrence of new calcifications after the procedure. The safety of fat grafting in breast lipomodelling has been demonstrated by Delay et al35 in an observational study at 10-years postoperatively. However, according to our technique, the adipose graft is positioned in the subcutaneous, sub-fascial, and intra-pectoral areas, minimizing alterations and contact with the mammary gland. Limits of the procedure are the availability of adipose tissue in patients with low BMI and the volume injected for each procedure.
CONCLUSIONS
Several authors have addressed the combination of mastopexy and breast augmentation in one procedure with several techniques. According to our lipopexy technique, an optimal and stable result could be achieved in selected patients, without the need of breast protheses.
Supplementary Material
Footnotes
Published online 25 February 2020.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Goldwyn R. Plastic and Reconstructive Surgery of the Breast. 1979Boston: Little, Brown and Company. [Google Scholar]
- 2.Spear SL, Pelletiere CV, Menon N. One-stage augmentation combined with mastopexy: aesthetic results and patient satisfaction. Aesthetic Plast Surg. 2004;28:259–267. [DOI] [PubMed] [Google Scholar]
- 3.Spear S. Augmentation/mastopexy: “surgeon, beware.” Plast Reconstr Surg. 2003;112:905–906. [DOI] [PubMed] [Google Scholar]
- 4.Parsa AA, Jackowe DJ, Parsa FD. A new algorithm for breast mastopexy/augmentation. Plast Reconstr Surg. 2010;125:75e–77e. [DOI] [PubMed] [Google Scholar]
- 5.Cárdenas-Camarena L, Ramírez-Macías R; International Confederation for Plastic Reconstructive and Aesthetic Surgery; International Society of Aesthetic Plastic Surgery; Iberolatinoamerican Plastic Surgery Federation; Mexican Association of Plastic Esthetic and Reconstructive Surgery; Western Mexican Association of Plastic, Esthetic and Reconstructive Surgery; Jalisco College of Plastic Surgeons. Augmentation/mastopexy: how to select and perform the proper technique. Aesthetic Plast Surg. 2006;30:21–33. [DOI] [PubMed] [Google Scholar]
- 6.Ceydeli A, Freund RM. “Tear-drop augmentation mastopexy”: a technique to augment superior pole hollow. Aesthetic Plast Surg. 2003;27:425–32; discussion 433. [DOI] [PubMed] [Google Scholar]
- 7.Eisenberg T. Simultaneous augmentation mastopexy: a technique for maximum en bloc skin resection using the inverted-T pattern regardless of implant size, asymmetry, or ptosis. Aesthetic Plast Surg. 2012;36:349–354. [DOI] [PubMed] [Google Scholar]
- 8.Stevens WG, Freeman ME, Stoker DA, et al. One-stage mastopexy with breast augmentation: a review of 321 patients. Plast Reconstr Surg. 2007;120:1674–1679. [DOI] [PubMed] [Google Scholar]
- 9.Stevens WG, Stoker DA, Freeman ME, et al. Is one-stage breast augmentation with mastopexy safe and effective? A review of 186 primary cases. Aesthet Surg J. 2006;26:674–681. [DOI] [PubMed] [Google Scholar]
- 10.Kamakura T, Ito K. Autologous cell-enriched fat grafting for breast augmentation. Aesthetic Plast Surg. 2011;35:1022–1030. [DOI] [PubMed] [Google Scholar]
- 11.Rosing JH, Wong G, Wong MS, et al. Autologous fat grafting for primary breast augmentation: a systematic review. Aesthetic Plast Surg. 2011;35:882–890. [DOI] [PubMed] [Google Scholar]
- 12.Illouz YG, Sterodimas A. Autologous fat transplantation to the breast: a personal technique with 25 years of experience. Aesthetic Plast Surg. 2009;33:706–715. [DOI] [PubMed] [Google Scholar]
- 13.Eaves FF, III, Haeck PC, Rohrich RJ. ASAPS/ASPS Position statement on stem cells and fat grafting. Plast Reconstr Surg. 2012;129:285–287. [DOI] [PubMed] [Google Scholar]
- 14.Rubin JP, Coon D, Zuley M, et al. Mammographic changes after fat transfer to the breast compared with changes after breast reduction: a blinded study. Plast Reconstr Surg. 2012;129:1029–1038. [DOI] [PubMed] [Google Scholar]
- 15.Regnault P. Breast ptosis. Definition and treatment. Clin Plast Surg. 1976;3:193–203. [PubMed] [Google Scholar]
- 16.von Heimburg D. Refined version of the tuberous breast classification. Plast Reconstr Surg. 2000;105:2269–2270. [DOI] [PubMed] [Google Scholar]
- 17.PITANGUY I. A new technic of plastic surgery of the breast. Study of 245 consecutive cases and presentation of a personal technic. Ann Chir Plast. 1962;7:199–208. [PubMed] [Google Scholar]
- 18.de Benito J, Sanza IF. Periareolar techniques for mammary reduction and elevation. Aesthetic Plast Surg. 1993;17:311–316. [DOI] [PubMed] [Google Scholar]
- 19.Lejour M, Abboud M, Declety A, et al. Reduction of mammaplasty scars: from a short inframammary scar to a vertical scar. Ann Chir Plast Esthet. 1990;35:369–379. [PubMed] [Google Scholar]
- 20.Boschert MT, Beckert BW, Puckett CL, Concannon MJ. Analysis of lipocyte viability after liposuction. Plast Reconstr Surg. 2002;109(2):761–765; discussion 766–767. [DOI] [PubMed] [Google Scholar]
- 21.Boyce RG, Nuss DW, Kluka EA. The use of autogenous fat, fascia, and nonvascularized muscle grafts in the head and neck. Otolaryngol Clin North Am. 1994;27:39–68. [PubMed] [Google Scholar]
- 22.Jackson IT, Simman R, Tholen R, et al. A successful long-term method of fat grafting: recontouring of a large subcutaneous postradiation thigh defect with autologous fat transplantation. Aesthetic Plast Surg. 2001;25:165–169. [DOI] [PubMed] [Google Scholar]
- 23.Matsudo PK, Toledo LS. Experience of injected fat grafting. Aesthetic Plast Surg. 1988;12:35–38. [DOI] [PubMed] [Google Scholar]
- 24.Nguyen A, Pasyk KA, Bouvier TN, et al. Comparative study of survival of autologous adipose tissue taken and transplanted by different techniques. Plast Reconstr Surg. 1990;85:378–386. [PubMed] [Google Scholar]
- 25.Rohrich RJ, Sorokin ES, Brown SA. In search of improved fat transfer viability: a quantitative analysis of the role of centrifugation and harvest site. Plast Reconstr Surg. 2004;113:391–395. [DOI] [PubMed] [Google Scholar]
- 26.Gonzalez-Ulloa M. Correction of hypotrophy of the breast by means of exogenous material. Plast Reconstr Surg Transplant Bull. 1960;25:15–26. [DOI] [PubMed] [Google Scholar]
- 27.Smahel J. Experimental implantation of adipose tissue fragments. Br J Plast Surg. 1989;42:207–211. [DOI] [PubMed] [Google Scholar]
- 28.Serra-Renom JM, Munoz-Olmo J, Serra-Mestre JM. Breast reconstruction with fat grafting alone. Ann Plast Surg. 2011;66:598–601. [DOI] [PubMed] [Google Scholar]
- 29.Khouri RK, Eisenmann-Klein M, Cardoso E, et al. Brava and autologous fat transfer is a safe and effective breast augmentation alternative: results of a 6-year, 81-patient, prospective multicenter study. Plast Reconstr Surg. 2012;129:1173–1187. [DOI] [PubMed] [Google Scholar]
- 30.Khouri RK, Rigotti G, Cardoso E, et al. Megavolume autologous fat transfer: part I. Theory and principles. Plast Reconstr Surg. 2014;133:550–557. [DOI] [PubMed] [Google Scholar]
- 31.Rigotti G. Discussion: The volumetric analysis of fat graft survival in breast reconstruction. Plast Reconstr Surg. 2013;131:192–193. [DOI] [PubMed] [Google Scholar]
- 32.Stutman RL, Codner M, Mahoney A, et al. Comparison of breast augmentation incisions and common complications. Aesthetic Plast Surg. 2012;36:1096–1104. [DOI] [PubMed] [Google Scholar]
- 33.Choi M, Small K, Levovitz C, et al. The volumetric analysis of fat graft survival in breast reconstruction. Plast Reconstr Surg. 2013;131:185–191. [DOI] [PubMed] [Google Scholar]
- 34.Pierrefeu-Lagrange AC, Delay E, Guerin N, et al. Radiological evaluation of breasts reconstructed with lipomodeling. Ann Chir Plast Esthet. 2006;51:18–28. [DOI] [PubMed] [Google Scholar]
- 35.Delay E, Garson S, Tousson G, et al. Fat injection to the breast: technique, results, and indications based on 880 procedures over 10 years. Aesthet Surg J. 2009;29:360–376. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


