Abstract.
Existing guidelines recommend long-term follow-up of childhood cancer survivors (CCS). However, in Japan, transitional care for CCS has not been established. To ascertain the current status in Japan, and to cultivate a better understanding, a questionnaire survey was conducted on transitional care in CCS, and adolescent and young adult (AYA) cancer survivors. Questionnaires were distributed to 183 councilors (137 institutions) of the Japanese Society for Pediatric Endocrinology. A total of 131 responses, representative of 174 councilors, were obtained. The response rate was 95%. Among the respondents, 91% had experience in medical care for cancer patients, while 63% had experience in transitional care; however, the number of patients referred to adult clinics was small. Further, 89% acknowledged the availability of adult endocrinologists who were willing to accept these patients; although their numbers were insufficient. Pediatric endocrinologists highlighted difficulties in medical examinations concerning infertility, obesity, pregnancy/delivery, and gonadal dysfunction, in that order. Staff and time shortages were listed as some of the challenges faced by medical staff, while multisystem morbidity was listed for patients. This nationwide questionnaire survey revealed that Japanese pediatric endocrinologists require cooperation between related departments and collaborative infrastructure to develop transitional care for cancer survivors.
Keywords: transition, childhood cancer survivor, adolescent and young adult, pediatric endocrinologist, questionnaire survey
Introduction
Due to improvements in the treatment and prognosis of cancer, the number of cancer survivors has increased (1). “Childhood cancer survivors (CCS)” and “adolescent and young adult (AYA) cancer survivors” are known to be at risk of various complications, e.g., second cancer, cardiovascular, endocrine, pulmonary, or neurological problems (2,3,4,5,6). The Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers, issued by the Children’s Oncology Group, are recognized as very useful resources for healthcare providers (7). Endocrine abnormalities were reported in more than 50% of CCS (8,9,10,11,12). Therefore, the CCS Committee of the Japanese Society for Pediatric Endocrinology (JSPE) issued a follow-up guide regarding CCS care (13). Health problems may occur long after cancer therapy, and therefore survivors need to be carefully examined. Recently, “transitional care” has been recognized as an important issue (14, 15). However, limited surveys on the endocrine abnormalities of CCS has been conducted in Japan. Therefore, appropriate evaluation and treatment for adult survivors of childhood or AYA cancer are still insufficient.
The aim of the present study was to gather the opinions of pediatric endocrinologists and reveal current clinical practice, to facilitate the development of transitional care for cancer survivors.
Participants and Methods
Questionnaires were sent to 183 councilors who are members of the JSPE. The questionnaire consisted of 17 closed-ended questions regarding the professional background of respondents, their experiences with transitional care in childhood and AYA cancer patients, their opinions regarding transition, and a free-entry section for personal opinions on future development plans for transitional care (Table 1). If multiple councilors belonged to one institution, an elected representative was permitted to present their opinions. The non-anonymous, self-reported questionnaire form was sent by surface mail, and responses were collected in a return envelope. The survey lasted from October to December 2018.
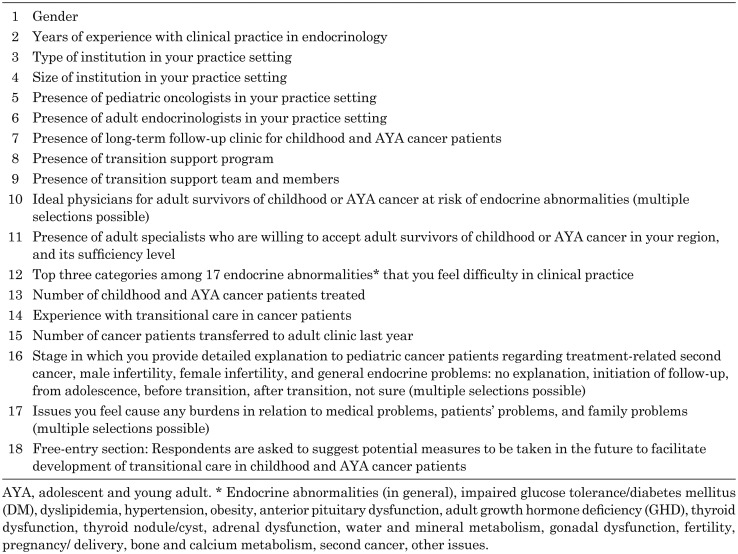
Table 1. Questionnaire.
This study was approved by the Ethics Committee of Osaka University Hospital (approval No. 18120). It was conducted as a joint study of the CCS Committee of the JSPE, the Research for Promotion of Cancer Control Program, and “Research Group for the Development of Comprehensive Care Program for Adolescents and Young Adults with Cancer” (organizer: Chikako Shimizu).
Results
Status of questionnaire responses
Questionnaires were sent to 183 councilors (137 institutions) who are members of the JSPE. A total of 131 valid responses, representative of 174 councilors, were obtained. The response rate from councilors was 95.1% (174/183).
Background of respondents
(Table 2)
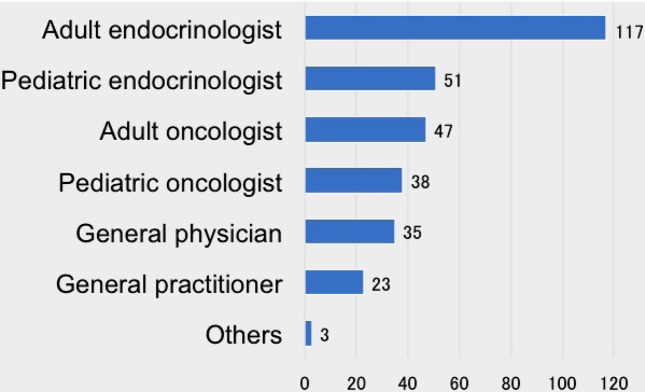
Table 2. Attributes of respondents and their clinical practice status (n = 131).
The gender of 131 respondents was 102 (77.9%) males and 29 (22.1%) females. Among the respondents, 60% had over 20 yr of clinical practice in endocrinology. Most were practicing in university hospitals (40.5%, n = 53) or general hospitals (37.4%, n = 49), with 54.2% (n = 71) responding that their institution had over 500 beds, and 32.1% (n = 42) indicating 100–499 beds, which shows that the majority of respondents were practicing in large-scale institutions. Nearly half of the respondents (45.8%, n= 60) worked in the Kanto-Shinetsu region of Japan. Others worked in the regions of Hokkaido 10 (7.6%), Tohoku 5 (3.8%), Tokai-Hokuriku 12 (9.1%), Kinki 16 (12.2%), Chugoku-Shikoku 12 (9.2%), Kyusyu 15 (11.5%), and abroad 1 (0.8%).
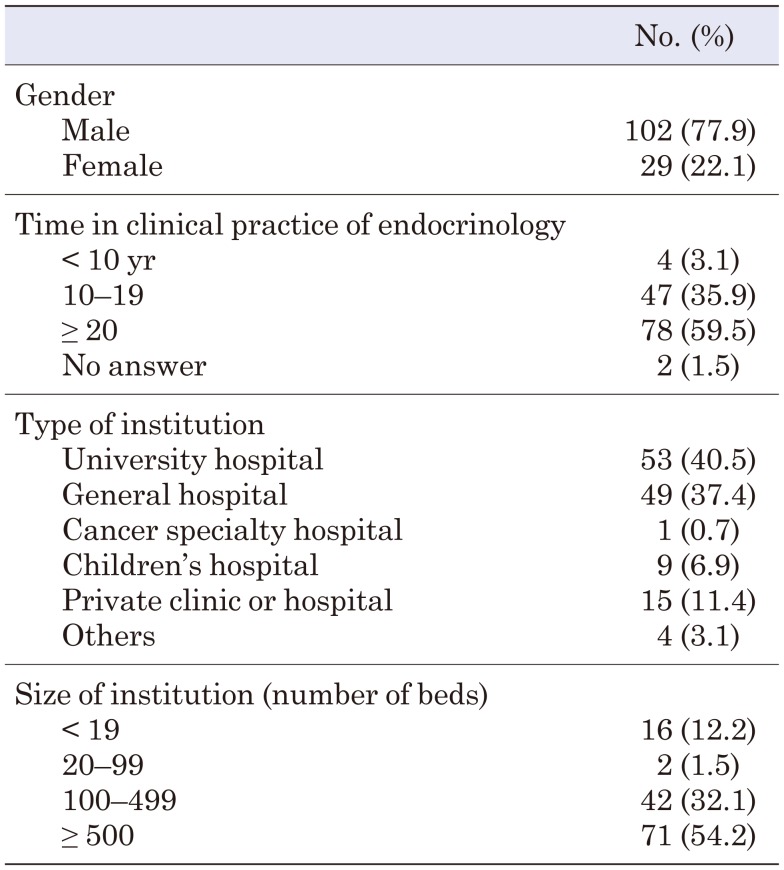
Status of respondents’ institutions
Half of the respondents (n= 65) stated that pediatric oncologists were present in their institutions, and 64.9% (n = 85) stated the presence of adult endocrinologists. A long-term follow-up clinic for cancer survivors existed in 43.5% (n = 57) of the institutions, whereas transition support programs for cancer patients (7.6%, n = 10) and transition support teams (6.9%, n = 9) were apparently insufficient (Fig. 1). Transition support teams, that support transitional care from pediatric to adult patient clinics among 9 affirmative respondents, consisted of pediatric oncologists (n = 9), pediatric endocrinologists (n = 9), adult endocrinologists (n = 4), adult oncologists (n = 3), nurses (n = 9), social workers (n = 6), clinical psychologists (n = 3), neurosurgeons (n = 2), pharmacists (n = 1), support school teachers (n = 1), public health nurses (n = 1), and peer supporters (n = 1).
Fig. 1.
Presence in the respondents’ institutions: (A) Long-term follow-up clinic for cancer survivors; (B) Transition support program; (C) Transition support team (n = 131).
Twelve respondents working at pediatric cancer center hospitals reported that their institution had pediatric oncologists, whereas adult endocrinologists existed only in 66.7% (n = 8) of these hospitals. A long-term follow-up clinic was present in all institutions, whereas transition support programs (41.7%, n = 5) and transition support teams (33.3%, n = 4) were also insufficient.
Clinical practice status of respondents
Experience in medical care for cancer patients: Regarding the respondents’ experience in medical care for childhood or AYA cancer patients, 90.9% (n = 119) of respondents answered affirmatively (Table 3). This result showed that most physicians had significant clinical practice with respect to managing cancer survivors. In addition, 62.6% (n = 82) of respondents answered that they had experience with transitional care. However, the number of patients transferred to adult patient clinics the previous year was small.
Table 3. Experience in medical care for childhood or AYA cancer patients.
Opinions regarding transitional care for cancer survivors
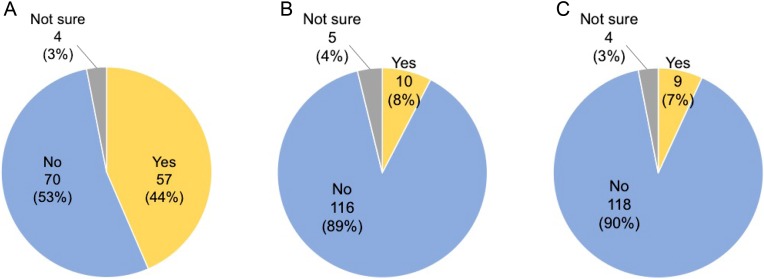
Regarding the ideal types of physicians for adult survivors of childhood or AYA cancer at risk of endocrine abnormalities, 89.3% (n = 117) of respondents selected adult endocrinologists (Fig. 2). This was much higher than the rates for pediatric endocrinologists 38.9% (n = 51), adult oncologists 35.9% (n = 47), and pediatric oncologists 29.0% (n = 38). This result showed that most of the respondents were aware of the importance of adult patient specialists.
Fig. 2.
Ideal physicians for adult survivors of childhood or AYA cancer at risk of endocrine abnormalities. Multiple selections were possible for this question (n = 131).
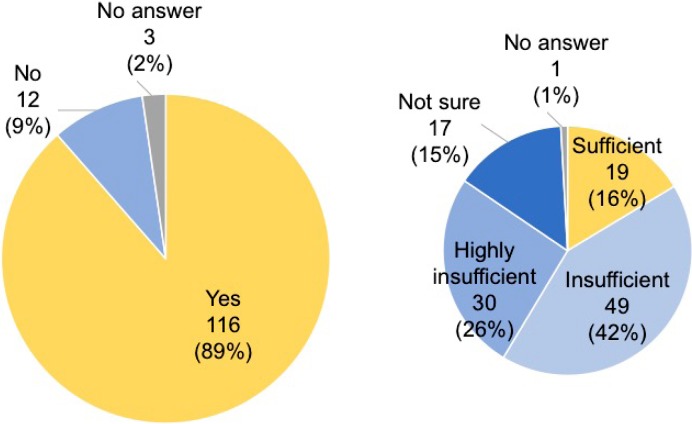
With respect to the presence of adult specialists willing to accept these patients in their region, 88.5% (n = 116) of respondents answered “yes”, while 9.2% (n = 12) answered “no” (Fig. 3). On the other hand, only 16.4% (n = 19) among these 116 affirmative responses were sufficient, while about two-thirds (68.1%, n = 79) of respondents were “insufficient” (42.2%, n = 49) or “highly insufficient” (25.9%, n = 30).
Fig. 3.
Existence of adult specialists willing to accept adult survivors of childhood or AYA cancer (left) (n = 131) and its sufficiency level (right) (n = 116).
Difficulties in the management of cancer patients
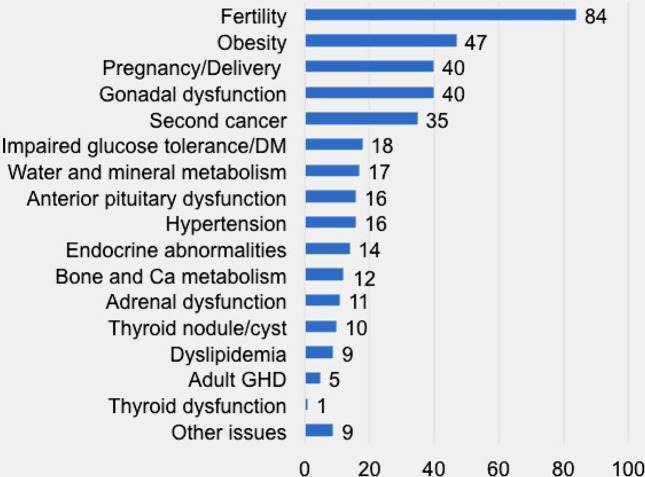
For the request to “Select three categories that you feel difficulties among 17 endocrine abnormalities”, respondents selected fertility (n = 84), obesity (n = 47), pregnancy and delivery (n = 40), gonadal dysfunction (n = 40), and second cancer (n = 35), in that order (Fig. 4). In total, 47 concrete examples were described.
Fig. 4.
Difficulty in management of childhood and AYA cancer patients. The respondents selected three answers for this question (n = 131).
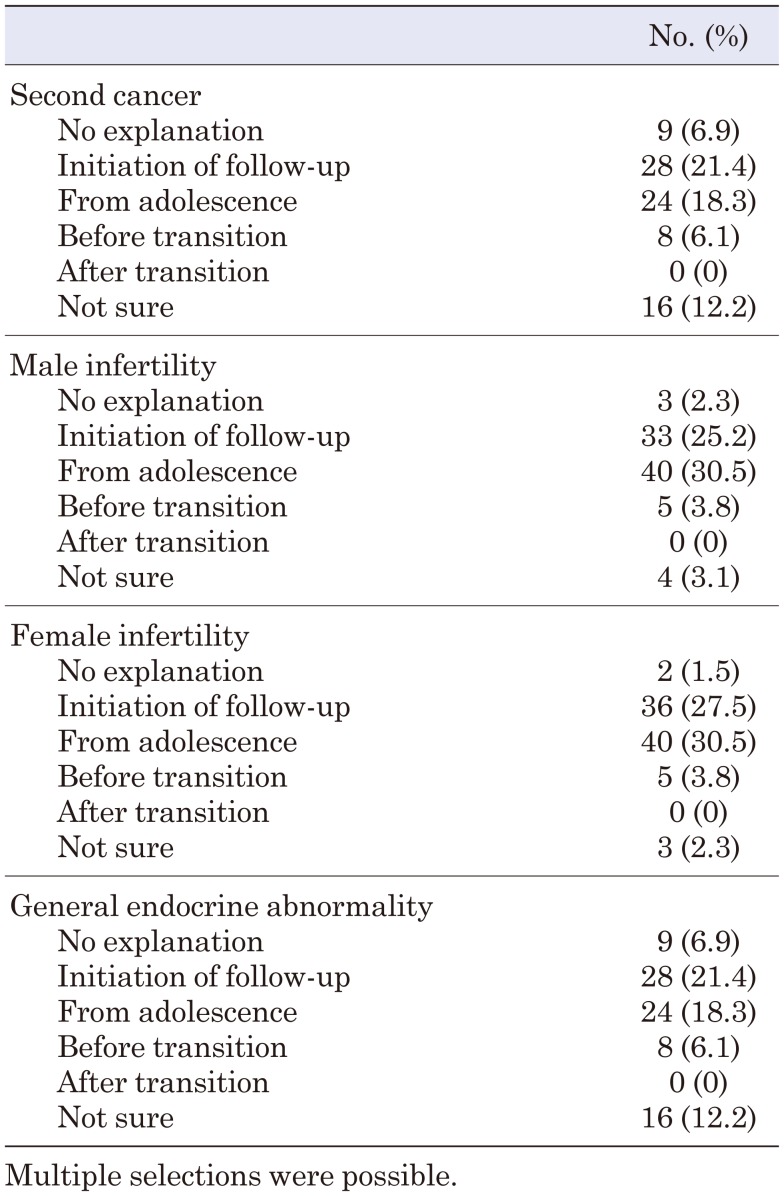
Stages in which physicians provide detailed explanations to patients
For the question, “When do you provide detailed explanations to pediatric cancer patients regarding treatment-related health problems (second cancer, infertility, and general endocrine problems), most of the respondents selected at “initiation of follow-up”, or “from adolescence”, regardless of the type of health problem (Table 4).
Table 4. Stage in which respondents provide detailed explanations to pediatric cancer patients (n = 131).
Experience with difficult situations in follow-up of AYA patients
Perceived issues regarding clinical practice for cancer patients were reported as staff and time shortages (n = 71); lack of definition of the roles of staff in medical examinations (n = 60); insufficient knowledge regarding cancer and therapy (n = 53); different patient-physician relationships in pediatric and adult clinics (n = 49); insufficient medical information, including that regarding cancer treatment and prognosis (n = 48); insufficient knowledge regarding late effects and follow-up (n = 46); insufficient explanation by oncologists (n = 43); and lack of clinical practice (n = 39).
Perceived issues regarding patients’ problems were reported as multisystem morbidity (specialization in medical care) (n = 86); financial burdens (n = 86); time related burdens (n = 82); infertility (n = 77); lack of awareness regarding health-related issues (n = 70); failure to recognize the importance of follow-up (n = 66); poor diligence during therapy, including discontinuation of drugs (n = 54); risk of relapse and second cancer (n = 52); and lack of awareness regarding cancer itself (n = 39).
Perceived issues regarding family problems were related to parents (e.g., overprotection and excessive control) (n = 95); pediatric cancer patients (e.g., immaturity) (n = 35); and partners (e.g., lack of empathy) (n = 28).
Opinions in the free-entry section
Among respondents, 87 (66.4%) provided comments in the free-entry section, in which they listed various problems. Poor communication between endocrinologists and oncologists, lack of information about cancer treatments, difficulties in clinical care due to insufficient explanation and lack of understanding, lack of financial support for long-term follow-up, and regional differences between rural areas and cities are some of the challenges of transitional care.
The respondents listed suggestions that included further education for physicians, collaboration between healthcare providers, training programs for coordinators, information sharing, financial support for follow-up, education programs for patients, psychological support, and socio-economical support in education and employment.
Discussion
We conducted a questionnaire survey regarding transitional care in CCS and AYA cancer survivors. The high response rate for the present survey indicates that Japanese pediatric endocrinologists are concerned about transition care issues. A large proportion of respondents had long-term experience, which suggests that the survey results obtained from the JSPE councilors reflected the country’s situation and opinions among practitioners, based on the actual experience of senior physicians in Japan.
“Transitional care” has recently been recognized as an important issue in America and Europe (14, 15), and also in Japan (16, 17). In 2013, the Ministry of Health, Labour, and Welfare in Japan established a research committee, focusing on issues related to social, educational, and medical support for adult patients with childhood-onset chronic diseases (APCCD). Also, the Japan Pediatric Society established a committee for the healthcare transition of APCCD and summarized their statements (18).
Healthcare transition from childhood to adulthood is required to ensure continuity of care for an increasing number of CCS cases. Based on our survey, pediatric oncologists existed in half of the respondents’ institutions; however, transition support programs and support teams were apparently insufficient. Most adult survivors of childhood or AYA cancer have not received outpatient follow-up care, resulting in insufficient clinical data on their long-term prognosis in Japan. Unfortunately, there are no prospective nationwide survey on long-term prognosis of CCS in Japan. However, a nationwide cancer registration system has started since 2016; therefore, precise data will be published in the future.
In the survey results, most physicians considered adult endocrinologists as most suitable for adult cancer survivors, while the numbers of physicians willing to accept these patients were insufficient. Since pediatric and adult specialists are not always available at the same institution, consensus guidelines are needed to ensure the same level of medical care is provided.
Pediatric endocrinologists rated fertility as the most difficult challenge in the management of cancer survivors. Gonadal dysfunction, subfertility, and premature ovarian insufficiency have been recognized as important issues for CCS (19,20,21). Therefore, we conducted other nationwide surveys to reveal current clinical practice among pediatric endocrinologists, to investigate issues and unmet needs associated with fertility in CCS (22, 23). Pediatric endocrinologists had anxieties regarding their cancer patients’ infertility and the risk of miscarriage, premature birth, and delivery problems. Only a limited number of endocrinologists had experience with managing childbirth and fertility preservation.
Most physicians had significant clinical practice with respect to managing cancer survivors. However, the number of patients transferred to adult clinics was small. One of the reasons cited was “dropped out from the outpatient clinic” (24). Lack of awareness on the importance of follow-up, due to insufficient explanation and lack of understanding was suggested. For early detection and early intervention of health-related problems, effective transition and long-term follow-up are essential (25, 26).
Nearly half of the respondents answered that they had provided detailed explanation to the patients regarding potential risk of late effects at initiation of follow-up or from adolescence. One of the characteristics of pediatric cancer is that patients may live long after the treatment. They therefore might later forget the precise explanation about cancer and its treatment. Also, since the patients are immature, they cannot fully understand the explanation provided, and explanations about cancer are often not provided to pediatric patients themselves. Patient-physician relationships in pediatric and adult clinics were different. Pediatric patients have lower self-management ability and tend to depend on the physicians mentally even if they grow up. Therefore, detailed explanations should be provided to the patients themselves at an appropriate time, i.e., before transition (6, 7).
In the free-entry section, respondents pointed out numerous problems and suggestions. The most common suggestion was to establish a more collaborative infrastructure. Implementing these opinions will result in a better understanding of transitional care. Systematic support programs and collaborative support teams are necessary for smooth transition. The current state of medical care is largely regional and facility-dependent; therefore, a nationwide approach is required.
This survey revealed an urgency to resolve problems concerning transitional care in cancer survivors and ask for understanding of related departments. It would be effective to hold training programs for medical staffs and lectures open to the public at annual meetings of related medical societies.
This study had a high response rate and reflected the opinions of pediatric endocrinologists with abundant clinical experience. However, there were some limitations in this questionnaire survey; for instance, we could not gather information from institutions that did not have a councilor. Similar studies in larger scale should be performed from the viewpoints of adult physicians.
Conclusion
In this nationwide questionnaire survey, Japanese pediatric endocrinologists highlighted the necessity for inter-disciplinary communication amongst healthcare providers.
Acknowledgements
We would like to thank all the councilors, who are members of the JSPE, for their contribution to this questionnaire survey. This work was supported by a Grant-in-Aid for Scientific Research (Japan Society for the Promotion of Science) (No. 18K07842). The authors declare no conflict of interests.
References
- 1.Cancer Information Service. Cancer Statistics in Japan’ 2018. https://ganjoho.jp/en/professional/statistics/brochure/2018_en.html (accessed August 16, 2019).
- 2.Bhakta N, Liu Q, Ness KK, Baassiri M, Eissa H, Yeo F, et al. The cumulative burden of surviving childhood cancer: an initial report from the St Jude Lifetime Cohort Study (SJLIFE). Lancet 2017;390: 2569–82. doi: 10.1016/S0140-6736(17)31610-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hudson MM, Armenian SH, Armstrong GT, Chow EJ, Henderson TO. Optimization of health and extension of lifespan through childhood cancer survivorship research. J Clin Oncol 2018;36: 2133–4. doi: 10.1200/JCO.2018.79.0477 [DOI] [PubMed] [Google Scholar]
- 4.Flerlage JE, Metzger ML, Bhakta N. The management of Hodgkin lymphoma in adolescents and young adults: burden of disease or burden of choice? Blood 2018;132: 376–84. doi: 10.1182/blood-2018-01-778548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bright CJ, Reulen RC, Winter DL, Stark DP, McCabe MG, Edgar AB, et al. Risk of subsequent primary neoplasms in survivors of adolescent and young adult cancer (Teenage and Young Adult Cancer Survivor Study): a population-based, cohort study. Lancet Oncol 2019;20: 531–45. doi: 10.1016/S1470-2045(18)30903-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coccia PF, Pappo AS, Beaupin L, Borges VF, Borinstein SC, Chugh R, et al. Adolescent and young adult oncology, Version 2.2018, NCCN Clinical practice guidelines in oncology. J Natl Compr Canc Netw 2018;16: 66–97. doi: 10.6004/jnccn.2018.0001 [DOI] [PubMed] [Google Scholar]
- 7.Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers. Version 5.0. - October 2018. http://www.survivorshipguidelines.org (accessed August 16, 2019).
- 8.Chemaitilly W, Sklar CA. Endocrine complications in long-term survivors of childhood cancers. Endocr Relat Cancer 2010;17: R141–59. doi: 10.1677/ERC-10-0002 [DOI] [PubMed] [Google Scholar]
- 9.Brignardello E, Felicetti F, Castiglione A, Chiabotto P, Corrias A, Fagioli F, et al. Endocrine health conditions in adult survivors of childhood cancer: the need for specialized adult-focused follow-up clinics. Eur J Endocrinol 2013;168: 465–72. doi: 10.1530/EJE-12-1043 [DOI] [PubMed] [Google Scholar]
- 10.Mostoufi-Moab S, Seidel K, Leisenring WM, Armstrong GT, Oeffinger KC, Stovall M, et al. Endocrine abnormalities in aging survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol 2016;34: 3240–7. doi: 10.1200/JCO.2016.66.6545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chemaitilly W, Sklar CA. Childhood cancer treatments and associated endocrine late effects: a concise guide for the pediatric endocrinologist. Horm Res Paediatr 2019;91: 74–82. doi: 10.1159/000493943 [DOI] [PubMed] [Google Scholar]
- 12.Miyoshi Y, Ohta H, Hashii Y, Tokimasa S, Namba N, Mushiake S, et al. Endocrinological analysis of 122 Japanese childhood cancer survivors in a single hospital. Endocr J 2008;55: 1055–63. doi: 10.1507/endocrj.K08E-075 [DOI] [PubMed] [Google Scholar]
- 13.Childhood Cancer Survivor Committee of the Japanese Society for Pediatric Endocrinology. Physician’s follow-up guide for childhood cancer survivors - 2011. http://jspe.umin.jp/medical/gui.html (accessed August 16, 2019).
- 14.American Academy of PediatricsAmerican Academy of Family PhysiciansAmerican College of Physicians-American Society of Internal Medicine. A consensus statement on health care transitions for young adults with special health care needs. Pediatrics 2002;110: 1304–6. [PubMed] [Google Scholar]
- 15.Mazur A, Dembinski L, Schrier L, Hadjipanayis A, Michaud PA. European Academy of Paediatric consensus statement on successful transition from paediatric to adult care for adolescents with chronic conditions. Acta Paediatr 2017;106: 1354–7. doi: 10.1111/apa.13901 [DOI] [PubMed] [Google Scholar]
- 16.Kubota M. Care continuity for patients during transition from childhood to adulthood-the perspective of pediatrician. Nihon Rinsho 2010;68: 145–50 (in Japanese). [PubMed] [Google Scholar]
- 17.Ishizaki Y, Higashino H, Kaneko K.Promotion of the transition of adult patients with childhood-onset chronic diseases among pediatricians in Japan. Front Pediatr 2016; 4:111. eCollection 2016. [DOI] [PMC free article] [PubMed]
- 18.Yokoya S, Ochiai R, Kobayashi N, Komatsu Y, Mashiko T, Mizuguchi M, et al. Statement of health care transition of patients with childhood-onset chronic diseases. J Jap Pediatr Soc 2014;118: 98–116. [Google Scholar]
- 19.Skinner R, Mulder RL, Kremer LC, Hudson MM, Constine LS, Bardi E, et al. Recommendations for gonadotoxicity surveillance in male childhood, adolescent, and young adult cancer survivors: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group in collaboration with the PanCareSurFup Consortium. Lancet Oncol 2017;18: e75–90. doi: 10.1016/S1470-2045(17)30026-8 [DOI] [PubMed] [Google Scholar]
- 20.van Dorp W, Mulder RL, Kremer LC, Hudson MM, van den Heuvel-Eibrink MM, van den Berg MH, et al. Recommendations for premature ovarian insufficiency surveillance for female survivors of childhood, adolescent, and young adult cancer: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group in Collaboration With the PanCareSurFup Consortium. J Clin Oncol 2016;34: 3440–50. doi: 10.1200/JCO.2015.64.3288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van Dorp W, Haupt R, Anderson RA, Mulder RL, van den Heuvel-Eibrink MM, van Dulmen-den Broeder E, et al. Reproductive function and outcomes in female survivors of childhood, adolescent, and young adult cancer: a review. J Clin Oncol 2018;36: 2169–80. doi: 10.1200/JCO.2017.76.3441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miyoshi Y, Yorifuji T, Horikawa R, Takahashi I, Nagasaki K, Ishiguro H, et al. Gonadal function, fertility, and reproductive medicine in childhood and adolescent cancer patients: a national survey of Japanese pediatric endocrinologists. Clin Pediatr Endocrinol 2016;25: 45–57. doi: 10.1297/cpe.25.45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miyoshi Y, Yorifuji T, Horikawa R, Takahashi I, Nagasaki K, Ishiguro H, et al. Childbirth and fertility preservation in childhood and adolescent cancer patients: a second national survey of Japanese pediatric endocrinologists. Clin Pediatr Endocrinol 2017;26: 81–8. doi: 10.1297/cpe.26.81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Okumura MJ, Hersh AO, Hilton JF, Lotstein DS. Change in health status and access to care in young adults with special health care needs: results from the 2007 national survey of adult transition and health. J Adolesc Health 2013;52: 413–8. doi: 10.1016/j.jadohealth.2012.08.005 [DOI] [PubMed] [Google Scholar]
- 25.Davis AM, Brown RF, Taylor JL, Epstein RA, McPheeters ML. Transition care for children with special health care needs. Pediatrics 2014;134: 900–8. doi: 10.1542/peds.2014-1909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhou H, Roberts P, Dhaliwal S, Della P. Transitioning adolescent and young adults with chronic disease and/or disabilities from paediatric to adult care services - an integrative review. J Clin Nurs 2016;25: 3113–30. doi: 10.1111/jocn.13326 [DOI] [PMC free article] [PubMed] [Google Scholar]